Abstract
Objectives:
The present study, building on cross-sectional research showing links between mothers’ sleep, stress, and parenting, used a longitudinal design to consider 1) the temporal direction of links between mothers’ sleep and stress, 2) whether mother sleep deficits predict change in parenting across time, and 3) whether mother sleep deficits mediate the inverse association between stress and positive parenting.
Design:
The study used repeated measures of stress, mother sleep, and positive parenting at toddler ages 30, 36, and 42 months.
Setting:
Data were collected at two sites, one in the Midwest and one in the East.
Participants:
413 mother-toddler pairs were followed. Mothers were mostly married, college educated, and middle class, but there was also considerable variability between families.
Measurements:
Stress was measured via parenting hassles, CHAOS, and role overload scales. Mother sleep was measured via actigraphy. Positive parenting was observed during the bedtime routine and rated using the HOME scale and other items.
Results:
Mother stress and sleep were inextricably linked across toddlerhood, and worse sleep was predictive of less observed positive parenting, even when controlling for prior levels of stress and parenting.
Conclusions:
Improving mothers’ sleep may be important in efforts to improve their parenting.
Keywords: sleep, parenting, stress, family systems, longitudinal, cross-lagged panel models
Sleep deficits have been shown to be associated with adults’ stress1 and poor cognitive and emotional functioning2. We found that sleep deficits in mothers of typically developing toddlers were concurrently associated with less observed positive parenting during the toddler’s bedtime routine, even controlling for the effects of sociodemographic risk factors, parenting stress, child misbehavior, hours worked outside the home, and number of children in the home3. We now can address these questions in a longitudinal design, which allows us to consider, in addition to the question of concurrent linkage, whether: 1. the effects between stress and sleep have a temporal order, 2. mother sleep deficits predict change in parenting across time, and 3. mother sleep deficits mediate the inverse association between stress and positive parenting.
Mothers of Toddlers
During the early childhood years, mothers, on average, tend to be more directly involved in their children’s lives and more sensitive to problem behavior and other stressors, compared to fathers.4 Additionally, mothers are more likely to experience sleep disruptions in relation to their child’s sleep disruptions, while father sleep is less strongly associated with child sleep.5 Mothers, therefore, were the particular focus of the present study, which was conducted across toddlerhood, a developmental period known for increases in child willfulness in addition to changes in sleep, particularly decreases in daytime sleep6, night wakings7, and total sleep.8 Mothers of toddlers likely face high levels of parental stress and sleep deficits that could affect their parenting behavior.
Mothers’ Sleep
There is abundant and important research on the sleep and functioning of mothers of infants9 and mothers of chronically ill children10. Research on the sleep of parents of typically developing children after infancy is comparatively scarce, but it is growing11. Cross-sectional studies show that the timing, duration, and quality of child sleep are significantly related to the timing, duration, and quality of mother sleep12. Mothers’ insomnia is linked with higher levels of household chaos and child neglect, even when socioeconomic status, depression, and relationship status are controlled13. Parents’ fatigue has also been shown to be associated with higher levels of parenting stress, hostility, and irritability, as well as with lower levels of parental warmth, self-efficacy, and satisfaction in the parenting role14. Notably, these associations between parent sleep/fatigue with parent functioning have been based entirely on parent-report. To date, the only study to examine the links between actigraphically-measured sleep and daytime functioning in mothers of toddlers comes from our research group. We found that actigraphic measures of mother sleep deficits were not only associated with mother reports of parenting pressures, child misbehavior, and sociodemographic risk factors, but also were concurrently associated, inversely, with observed positive parenting above and beyond the effects of these three stress domains3. Longitudinal research is now necessary to determine: 1. the direction of effects between stress and sleep across time, 2. whether mother sleep deficits predict change in parenting across time, and 3. whether mother sleep deficits mediate the inverse association between stress and positive parenting.
The Present Study
This study used repeated measures of mother-reported stress, mothers’ actigraphic sleep, and observed positive parenting during the bedtime routine at toddler ages 30, 36, and 42 months. A cross-lagged panel model was conducted to model the levels of change mothers experienced across time relative to other mothers, and to test lead-lag associations between constructs across time.
We sought to examine temporal links between parents’ stress and sleep across toddlerhood. Research has shown that stress can result in poor and insufficient sleep. Experimentally induced stress15 and real-world stressors16 can reduce the duration and quality of sleep. For women in particular, lower socioeconomic status has been shown to be associated with fewer actigraphic sleep minutes17. Prior research has also shown that poor and insufficient sleep, in turn, can result in higher stress levels. Poor sleep quality increases morning cortisol and cholesterol levels, reflecting a physiological stress response18. Moreover, sleep loss has been shown to reduce the rate at which cortisol concentrations decline over the course of a day, resulting in relatively elevated levels of cortisol in the evening19. Sleep deficits also limit the regulatory functioning of the prefrontal cortex, resulting in increased negative emotionality, impulsivity, and sensitivity to low-level stressors20. Research on sleep deprived individuals responding to physical exercise21 and sleep deprived medical professionals responding to disruptive and unexpected events at work22 has shown that the heightened activation of stress systems following sleep loss is associated with stronger reactions to such challenges compared to milder appraisals of these challenges when the individuals are well-rested. Based on this extensive prior research on the connections between stress and sleep in adults and our previous cross-sectional findings with mothers of toddlers in particular3, we expected to find similar bidirectional links between mother stress and sleep spanning across a year of toddlerhood.
We also sought to longitudinally extend our prior cross-sectional research showing that poor and insufficient mother sleep was linked with less observed positive parenting during toddlers’ bedtime routines3. Other previous research examining links between stress and parenting showed that mothers returning home from stressful work days were more likely to show less positive parenting, rather than an increase in negative parenting23. Thus, we again examined the effects of stress and sleep on positive parenting, and we expected that mothers who experienced worse sleep would show less positive parenting across time, even with controls for prior levels of positive parenting, compared to mothers who experienced better sleep. Finally, we tested whether mother sleep deficits mediated the association between stress and observed positive parenting. We expected to find that mothers who endorsed higher levels of stress would experience worse sleep, which over time would result in less observed positive parenting.
Method
Procedure
Three community samples were collected as part of a multi-site, longitudinal study, the Toddler Development Study. Recruitment was primarily through a database using county birth records and community outreach efforts, such as through the local Head Start agency and the Housing Authority. Advertisements, such as postcards, flyers, and social media postings, were also used. Compensation ($100 total per wave of assessment, approximately $25 per hour of participation) was provided, and transportation was offered. The local institutional review boards approved the study, and mothers provided informed consent.
At child ages 30, 36, and 42 months, mothers completed questionnaires pertaining to demographic information and stress. Mother-child dyads also participated in two home visits. At the initial home visit, mothers were given actigraphs to wear for one week. Within the next several days, two research assistants conducted a second home visit to observe parent-child interaction in the hour prior to the child’s bedtime.
The full sample, collapsed across the three subsamples, included 413 mother-child pairs at 30 months, 335 at 36 months, and 250 at 42 months. The first two samples were collected in a Midwestern town and were followed longitudinally from child age 30 to 36 to 42 months. The first sample completed fewer stress measures than the second and third samples, but had the same measures of parental sleep and parenting. Data collection for the first sample was completed in 2013. The second sample completed additional stress measures. Data collection for Sample 2 was completed in 2018. The third sample was collected in an Eastern city and was followed longitudinally from child age 30 to 36 months. Data collection for this sample was completed in 2016. The measures collected in the second and third samples were identical. Measures collected in each sample are listed in Table 1.
Table 1.
Descriptives
| Domain | Variable | Child Age |
N (%) | M | SD | Min | Max |
|---|---|---|---|---|---|---|---|
| Parenting | Pos. Parenting (z) | 30 | 386 (93) | .00 | 1.00 | −4.17 | 1.19 |
| Pos. Parenting (z) | 36 | 314 (76) | .00 | 1.00 | −4.53 | 2.38 | |
| Pos. Parenting (z)* | 42 | 231 (56) | .00 | 1.00 | −5.31 | 1.42 | |
| Stress | Parenting Hassles | 30 | 413 (100) | 39.58 | 8.33 | 13.00 | 68.00 |
| Parenting Hassles | 36 | 332 (80) | 40.04 | 8.09 | 19.00 | 63.00 | |
| Parenting Hassles* | 42 | 239 (58) | 40.14 | 7.81 | 14.00 | 66.00 | |
| CHAOS^ | 30 | 300 (73) | 3.65 | 2.97 | .00 | 14.00 | |
| CHAOS^ | 36 | 228 (55) | 4.00 | 2.85 | .00 | 14.00 | |
| CHAOS^* | 42 | 138 (33) | 4.21 | 3.03 | .00 | 13.00 | |
| Role Overload^ | 30 | 311 (75) | 4.37 | 1.06 | 1.33 | 7.00 | |
| Role Overload^ | 36 | 246 (60) | 4.49 | 1.00 | 2.17 | 6.50 | |
| Role Overload^* | 42 | 136 (33) | 4.42 | 1.06 | 2.33 | 6.83 | |
| Mother Sleep | Sleep Duration (z) | 30 | 360 (87) | .01 | .91 | −3.45 | 3.06 |
| Sleep Variability (z) | 30 | 360 (87) | .00 | .78 | −1.19 | 4.65 | |
| Sleep Activity (z) | 30 | 357 (86) | .04 | .84 | −1.35 | 3.57 | |
| Sleep Timing (z) | 30 | 359 (87) | −.02 | .94 | −3.10 | 4.03 | |
| Sleep Onset Latency | 30 | 353 (85) | 31.45 | 30.19 | .86 | 291.00 | |
| Sleep Duration (z) | 36 | 309 (75) | .05 | .91 | −3.33 | 2.57 | |
| Sleep Variability (z) | 36 | 308 (75) | −.06 | .75 | −1.25 | 3.46 | |
| Sleep Activity (z) | 36 | 307 (74) | .03 | .95 | −1.56 | 3.83 | |
| Sleep Timing (z) | 36 | 308 (75) | −.06 | .90 | −3.00 | 3.16 | |
| Sleep Onset Latency | 36 | 303 (73) | 31.56 | 29.58 | .50 | 324.83 | |
| Sleep Duration (z)* | 42 | 215 (52) | −.04 | .85 | −2.91 | 2.03 | |
| Sleep Variability (z)* | 42 | 215 (52) | .03 | .95 | −1.35 | 6.20 | |
| Sleep Activity (z)* | 42 | 215 (52) | −.04 | .92 | −1.38 | 3.76 | |
| Sleep Timing (z)* | 42 | 215 (52) | .05 | 1.01 | −4.32 | 4.47 | |
| Sleep Onset Latency* | 42 | 213 (51) | 27.95 | 23.59 | .75 | 182.33 | |
Note.
indicates that the measure was not collected for Sample 3.
indicates that the measure was not collected for Sample 1.
All percentages are based on the original sample size at the first wave of data collection (N = 413), although some missingness was planned at 42 months since these data were not collected for Sample 3. Pos. Parenting refers to the Observed Positive Parenting composite that was formed based on observed parental involvement and responsiveness during the home visit. CHAOS refers to the Confusion, Hubbub, and Order Scale26.
Participants
In the first sample, mothers were 19 to 48 years old (M = 32.91, SD = 5.69), and 58% of the target children were males. The family’s SES was calculated using the Hollingshead Four Factor Index24, an index which takes into account the parents’ educational attainment and occupational prestige, with both parents’ education and occupation scores equally informing estimates when both parents are employed, but with only one parent’s score informing estimates in families with a single parent or a couple with a non-employed partner. Based on the Hollingshead index, the sample was largely middle class (range = 14– 66, M = 47.29, SD = 14.96). Eighty-two percent of mothers were Caucasian, 7% were Hispanic, 3% were African American, and 8% identified as Asian American, American Indian, mixed race, or other. Seven percent of the mothers were single/never married, separated, or divorced. In 48% of the families, the target child was the only child. Thirty-four percent had two children in the home, while 18% had three to four children. Forty-one percent of mothers did not work outside the home.
Across the second two samples with complete stress measures, mothers were 21 to 50 years old (M = 32.70, SD = 5.03), and 49% of the target children were males. Based on the Hollingshead index, the sample was largely middle class (range = 13– 66, M = 47.71, SD = 13.36). Ninety percent of mothers were Caucasian, 4% were Hispanic, 3% were African American, and 3% identified as Asian American, American Indian, mixed race, or other. Fifteen percent of the mothers were single/never married, separated, or divorced. In 28% of the families, the target child was the only child. Forty percent had two children in the home, 29% had 3-4 children, and 3% had five or more children. Thirty-one percent of mothers did not work outside the home, and 28% worked 40 or more hours per week. The two sites of data collection for Samples 2 (site 1) and 3 (site 2) did not significantly differ in terms of mother age (M = 32.68, SD = 4.71 years for Sample 2, and M = 32.66, SD = 5.57 years for Sample 3) or family SES (M = 47.39, SD = 13.95 for Sample 2, and M = 48.36, SD = 12.11 for Sample 3). Similarly, these second two samples did not significantly differ from the first sample in terms of mother age (M = 32.91, SD = 5.69) or family SES (M = 47.29, SD = 14.96).
Measures
Stress.
Multiple indexes of parenting stress, including parenting hassles, household chaos, and role overload were collected in Samples 2 and 3. The first sample assessed only parenting hassles.
Parenting hassles.
In all three samples, mothers completed the Parenting Daily Events scale25, and the 16-item parenting tasks subscale was used for this study. Mothers rated the frequency (1 = never to 5 = constantly) and intensity (1 = no hassle to 5 = big hassle) of common parenting hassles, such as cleaning up messes and running errands. The sum of the items was used in all analyses (α = .81).
Household chaos.
In the second two samples, mothers completed the Confusion, Hubbub, and Order Scale (CHAOS)26. Mothers’ responses to 12 binary (1 yes/ 0 no) items, such as “You can’t hear yourself think in our home” and “It’s a real zoo in our home,” were summed (α = 0.79).
Role overload.
In the second two samples, mothers’ perceived role overload was assessed using the revised, 6-item Reilly Role Overload Scale27. Items included “I need more hours in the day to do all the things that are expected of me” and “There are times when I cannot meet everyone’s expectations” using a 7-point Likert-scale, ranging from never to always. The average per-item rating was used (α = .80).
Mother sleep.
In all samples and time points, mothers wore a watch-like actigraph on their non-dominant wrist for one week. The MicroMini Motionlogger from Ambulatory Monitoring, Inc. (AMI; Ardsley, NY) recorded minute-by-minute patterns of motor activity. Actigraph data were scored with the Motionlogger Analysis Software Package Action W-2 software (version 2.6.92) from AMI. The Cole-Kripke algorithm, which has been validated for adults and shown to provide reliable estimates of sleep indexes when averaged over at least five nights, was used to reduce the motion data into meaningful sleep variables28, 29. Wake time was recorded as the first minute that exceeded 50 movements and remained above that value for the rest of the morning. Mothers also completed daily diaries to record time in and out of bed as well as times when the actigraph was not worn.
Based on previous principal components analysis30, the large number of AW-2 actigraph variables were summarized into four composites. Composites were formed by standardizing the actigraphy variables (based on sleep data across all assessments) and averaging them. These four composites—sleep duration, sleep timing, sleep variability, and sleep activity—represent broad dimensions of actigraphy that are often examined in the sleep literature31. The actigraphy variables included in each composite are listed in Appendix A. Of note, the only diary reported variables included in the sleep composites were mother-reported bedtime and the standard deviation of bedtime. On average, based on our actigraphy data, the mothers slept for 8 hours (M = 454.26 minutes, SD = 53.86), experienced two prolonged night wakings (lasting five or more minutes) per night (M = 2.39 wakings, SD = 1.57), and went to bed around 11:30 PM (M = 23.60 in 24-hour time, SD = 1.15).
Observed Positive Parenting.
During the second home visit, two trained research assistants observed for approximately an hour before the toddler’s bedtime. All research assistants were thoroughly trained on the observation procedure using a comprehensive observation manual, training sessions with advanced lab coordinators before visiting homes, and a pairing procedure so that novice observers were accompanied by advanced observers for additional training purposes on home visits. Observers independently completed a Post-Observation Questionnaire (POQ)3 and two scales from the Home Observation for Measurement of the Environment inventory (HOME)32. The POQ used a 5-point Likert scale to assess responsiveness via 9 items, including “to what extent did this mother seem to enjoy accommodating herself to the child’s needs and wants” and “to what extent did both mother and child contribute reciprocally to their interactions”. The two HOME subscales used were responsivity (11 items) and parental involvement (5 items). Each subscale had binary yes (1) /no (0) and not applicable responses, and the sum of responses divided by the number of applicable items was used for each. Sample items include “mother responds to child’s vocalizations with a verbal response” for responsivity, and “mother tends to keep child within visual range and to look at him/her often” for parental involvement. The two observers’ ratings on the HOME and POQ subscales were averaged, and a single composite index of Observed Positive Parenting was formed because all three scales were conceptually related and significantly correlated, with correlation coefficients ranging from .34 to .653. Cronbach’s α for the full composite was 0.82, and inter-rater agreement on the composite was r = 0.57.
Analysis Plan
Structural Equation Modeling (SEM) was conducted in Mplus version 8.433. Full information maximum likelihood estimation (FIML), a robust estimation method when data are missing at random or completely at random, was used to address missingness. A portion of the sample (24%) involved planned missingness (i.e., were purposefully not assessed at all 3 ages), while other forms of missingness included participant unwillingness to have observers visit their home, failure to return questionnaire packets, refusal to wear actigraphs, actigraphic equipment failure, or attrition across time points when a family moved or was unable to be contacted. The data that were missing by design were considered to be missing completely at random34,35. Missingness for sleep and parenting data as a function of an auxiliary variable, family SES, was also tested. Mothers with usable actigraphic data had significantly higher SES (48.51 ± 13.13) compared with mothers without actigraphy data (43.30 ± 13.86), t(360) = 2.45, p = .02. However, mothers with parenting data were not quite as likely to be high on SES, with a nonsignificant difference on socioeconomic status for mothers with (48.11 ± 15.19) and without (42.89 ± 13.14) parenting data, t(386) = 1.60, p = .12. Maximum likelihood estimation with bootstrapping was used for the longitudinal mediation model.
After addressing missingness and examining descriptives and bivariate correlations among all variables, Confirmatory Factor Analyses (CFAs) were conducted to form latent constructs for parental stress, mother sleep, observed positive parenting, individually, at child age 30 months. If the constructs were successfully formed, these constructs were then tested at the second two time points, 36 and 42 months, to evaluate time invariance in the measurement models. The fixed factor method of coding was used for the CFAs, meaning that the mean and variance of the latent factor were set to zero and one, respectively, which allows factor loadings to vary freely and promotes interpretability of findings.
After establishing measurement models, a cross-lagged panel model was conducted to test whether stress predicted subsequent poor mother sleep, while controlling for prior levels of mother sleep and while simultaneously testing the converse (poor mother sleep predicting subsequent stress controlling for prior stress). A panel model was also used to examine whether stress predicted later parenting behavior (controlling for prior levels of parenting) and whether individual differences in sleep mediated this association. To determine whether sleep mediated the effect of stress on later parenting behavior, the longitudinal mediation modeling approach recommended by Cole and Maxwell36 was used. The longitudinal mediation models examined whether (a) stress predicted subsequent sleep controlling for prior sleep, (b) sleep predicted later parenting behavior controlling for prior levels of parenting behavior, (c) stress predicted later parenting behavior (controlling for prior levels of sleep and parenting behavior), and (d) whether the effect of stress on later parenting behavior was mediated by sleep. The full models included other possible within- and across-construct covariances to account fully for the covariance structure. Indirect effects were tested by bootstrapping 95% confidence intervals (CIs) from 1,000 bootstrap samples.
Results
Descriptive statistics are reported in Table 1. Mothers’ perceptions of parenting hassles, household chaos, and role overload were selected to be tested in the CFA for parental stress because they have been well-established in previous research and were shown to converge in research from our project, with correlation coefficients ranging from .38 to .483 (Appendix B). The sleep construct, General Sleep Deficit, was also formed based on previous research3 in which the actigraphic composites of Sleep Duration, Timing, and Variability were shown to correlate (absolute r values ranged from .32 to .53), and a CFA was fit to the data at child age 30 months to form the General Sleep Deficit construct, which reflected shorter, later, and more variable sleep. This CFA was replicated and extended in the present study by testing the CFA at all time points (Appendix C). The remaining sleep composite, Sleep Activity, did not strongly correlate with General Sleep Deficit (r = .13) and did not converge in a latent construct. The parenting construct, Observed Positive Parenting (Appendix D), reflected maternal responsiveness and involvement observed during the home visit in the hour before the target child’s bedtime, and a composite based on these scales was used in previous research3.
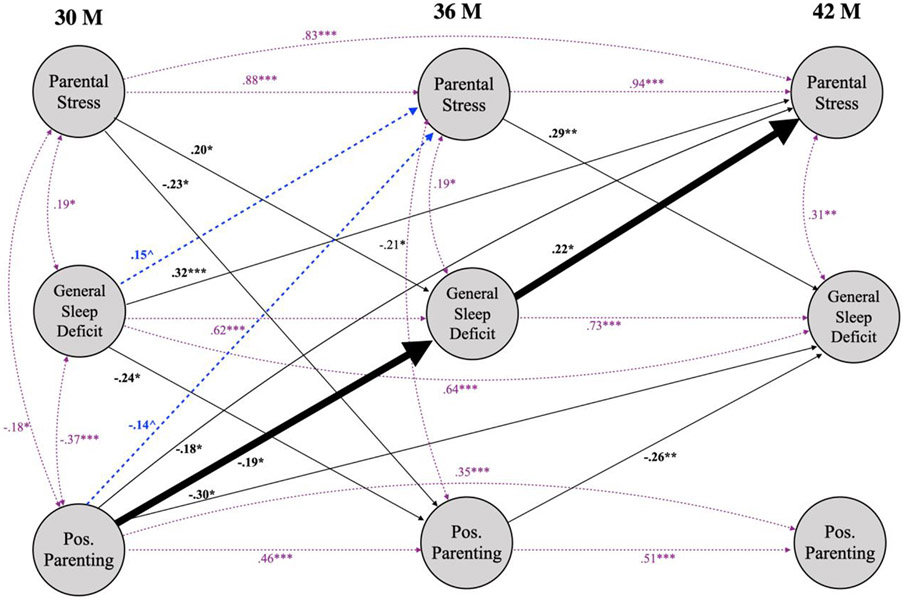
Cross-lagged Panel Model
After finalizing the latent constructs for stress, sleep, and parenting, a cross-lagged panel model was conducted (Figure 1). Four notable findings emerged. First, stress at child age 30 months was concurrently associated with General Sleep Deficit. General Sleep Deficit and stress were also both associated with less positive parenting at 30 months. Second, the model showed evidence for the hypothesized bidirectional links between stress and sleep deficits. Higher levels of mother-reported stress were predictive of worse sleep at 30 to 36 months and at 36 to 42 months. The reverse was also true; General Sleep Deficit was predictive of higher reports of stress 6 and 12 months later. In addition to these bidirectional links across time, stress and sleep deficits were concurrently linked at each age. The third notable finding from this model pertains to associations with positive parenting. Both stress and sleep deficits were predictive of less positive parenting 6 months later, even with autoregressive controls for prior parenting. Fourth, we found a significant mediation effect, although it was not the expected effect. We hypothesized that sleep deficits would mediate the link between stress and parenting. Although we found that stress predicted worse sleep from 30 to 36 months, the link between sleep deficits at 36 months and parenting at 42 months was not statistically significant, although it was in the expected (negative) direction (β = − 0.02). Instead of the hypothesized mediation effect, however, we found that more positive parenting at 30 months predicted fewer sleep deficits at 36 months, which in turn predicted lower levels of stress at 42 months.
Figure 1.
Stress, General Sleep Deficit, and Positive Parenting Cross-lagged Panel Model. χ2(351) = 3253.16, p = .00; RMSEA = 0.03; CFI = .96; ^ p < 0.10, * p < 0.05, ** p < 0.01, *** p < 0.001. Nonsignificant paths are not displayed. Circles represent latent constructs. Concurrent associations and autoregressive paths are displayed in lightweight, dotted lines. Cross-lagged paths that are trending towards significance are displayed by dashed lines. Significant, cross-lagged paths are displayed by black lines. The heavily weighted, black lines show the mediation effect. Pos. Parenting refers to the Observed Positive Parenting latent factor that was formed based on observed parental involvement and responsiveness during the home visit.
Discussion
Previous research has shown that actigraphic measures of mothers’ sleep deficits inversely predict positive parenting practices observed during the toddler’s bedtime period, above and beyond other forms of stress, including parenting pressures, child misbehavior, and sociodemographic risk factors like low socioeconomic status and single parenthood3. However, due to the cross-sectional nature of this previous research, the direction of associations between stress and sleep could not be clarified, and sleep deficits could not be shown to have a causal effect on parent behavior. The present study built on this previous research by 1) documenting bidirectional links between parental stress and sleep deficits across a year of toddlerhood, 2) showing that mother sleep deficits predicted change in parenting across time, and 3) establishing an unexpected mediation effect, with positive parenting during the toddler’s bedtime routine predicting better sleep, which in turn predicted less stress over time.
Summary of Findings
Evidence for bidirectional associations between stress and sleep emerged. Mothers who reported higher levels of stress tended to experience more sleep deficits later relative to less stressed mothers, and across time, mothers who experienced worse sleep tended to report more stress later relative to mothers who experienced better sleep. These bidirectional links show that stress and sleep continually and mutually influence one another across time. Thus, our hypothesis that mother sleep deficits play a part in the stress process, contributing to a vicious cycle in which stress results in insufficient sleep, which in turn leads to a greater perception of stress, was confirmed.
We also replicated and extended our previous result that mother sleep deficits predict less observed positive parenting during the pre-bedtime period3. In the present study, we found this result concurrently as well as across time from 30 to 36 months. Mothers who experienced higher levels of General Sleep Deficit at child age 30 months tended to show less positive parenting during the bedtime visit six months later compared to more well-rested mothers. Although both of these findings are promising, we did not find evidence in support of the hypothesized mediation effect with stress predicting poor sleep, which in turn was expected to predict less positive parenting. We did, however, find that observed positive parenting in the bedtime routine predicted better mother sleep six months later, which in turn predicted lower levels of perceived stress another 6 months later. Mothers who are highly responsive and involved during their child’s bedtime routine may prioritize sleep, practice good sleep hygiene, and promote children’s sleep, all of which could enable better mother sleep, which appears to have downstream positive effects on perceived stress. This speculative but theoretically plausible explanation requires further research. A systematic review37 has shown that positive affect in adults is longitudinally predictive of better sleep over time, potentially due to enhanced parasympathetic regulation38 and more frequent use of restorative health practices39. Such processes associated with positive affect, in addition to the positive consequences of positive parenting for the family system, may collectively contribute to the mediation effect found in the present study.
Limitations
Several limitations of this work should be considered. First, although the sample did have a meaningful range of stress, it was not a sample of highly sleep deprived and otherwise highly stressed mothers. This sample was also racially and ethnically homogeneous, and thus, the results may not generalize to mothers from racial or ethnic minority backgrounds. Additionally, our Hollingshead index of socioeconomic status is limited as it does not incorporate important factors, such as income to needs ratio and income stability40. Individual characteristics, such as mothers’ race, socioeconomic status, and temperament, may serve as important moderators of the links examined here and should be tested in future research41.
Second, the time scale that was used in this study, assessing mothers every six months, may not be fine-grained enough to detect within-person effects of sleep deficits on parent functioning. To better detect within-person effects, future research could examine mothers’ sleep the night before their parenting is observed.
A third limitation of this study was our sole focus on mothers of toddlers without consideration of fathers in the home. Several studies have demonstrated that mothers’ and fathers’ average stress ratings tend to be more similar than different4, but the consideration of fathers would be particularly useful for better understanding their contribution to parenting tasks, specifically positive parenting observed at bedtime and its downstream effects on sleep in the family system. Indeed, prior research examining both mother and father reports of family process in connection with toddler sleep has shown that fathers’ reports of relationship satisfaction and family functioning are inversely predictive of toddler sleep problems42, suggesting the key role that fathers play in affecting sleep in the family system.
Lastly, although we were specifically interested in the effects of stress and sleep on positive parenting, future research should also examine the effects of stress and sleep on the occurrence of negative forms of parenting. To get a valid, observational measure of dysfunctional parenting, it may be necessary to observe for much longer periods than we did. It was very rare to see truly negative parenting behavior, such as harsh scolding or spanking, during the home visits.
Conclusions
These limitations are offset by several strengths, particularly the use of a large, multi-site sample, a longitudinal design, well-validated actigraphic measures of sleep, and observed measures of parenting. The findings advance our understanding of how parental stress and sleep are interconnected for mothers across the toddlerhood period and how sleep can affect parenting. Prior to this study, the relevant research primarily relied upon mother reports in cross-sectional designs. Sleep deficits are a prevalent but relatively overlooked stressor. From previous research, we know that sleep deficits result in reduced productivity, poor health, irritability, decreased quality of life, and strained social interactions43. We now also know from this study that for mothers of toddlers, sleep deficits contribute to an overarching stress process and result in less positive parenting during a crucial time of day, their toddler’s bedtime routine.
Acknowledgments
The Toddler Development Study has been funded by grants MH099437 from the National Institute of Mental Health and HD073202 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Appendix
Appendix A.
Actigraphy variables included in composites
| Sleep Composite | Variable Descriptions |
|---|---|
| Sleep Duration | Average sleep period (minutes) |
| Average duration of time in bed (minutes) | |
| Average minutes asleep in bed | |
| Sleep Timing | Average time of midsleep (HH:MM in 24-hour time) |
| Average time of sleep onset (HH:MM in 24-hour time) | |
| Average bedtime (HH:MM in 24-hour time)* | |
| Sleep Variability | SD of time of sleep onset |
| SD of duration in bed | |
| SD of duration of sleep period | |
| SD of time of midsleep | |
| SD of bedtime* | |
| SD of minutes asleep in bed | |
| Sleep Activity | Average time (minutes) awake after sleep onset |
| SD of average minute to minute activity levels | |
| Average number of awakenings (lasting 5 minutes or more) | |
| Average duration (minutes) of longest wake episode (after sleep onset) |
Note.
bedtime variable was based on mother report of time in bed on the daily diary
Appendix B.
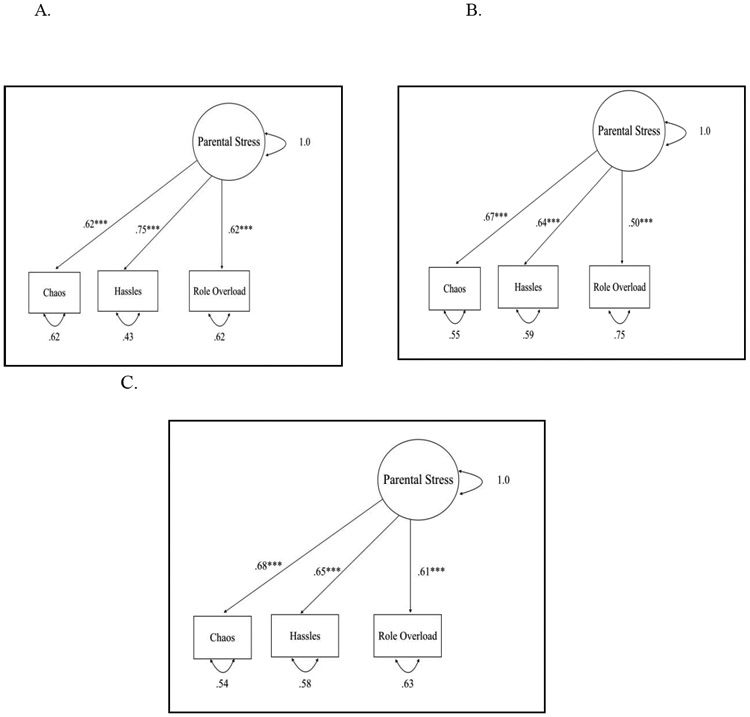
CFA for parental stress. A shows the CFA at the first time point, child age 30 months, B at 36 months, and C at 42 months. The fixed factor method of coding was used for each model, as this approach explicitly recognizes that the metric of the latent variable is arbitrary. Therefore, the variance of the construct is fixed to 1 so that the estimated latent factor relations can thereby be estimated in a standardized metric. ***. denotes significance at p < 0.001. CHAOS refers to the Confusion, Hubbub, and Order Scale26.
Appendix C.
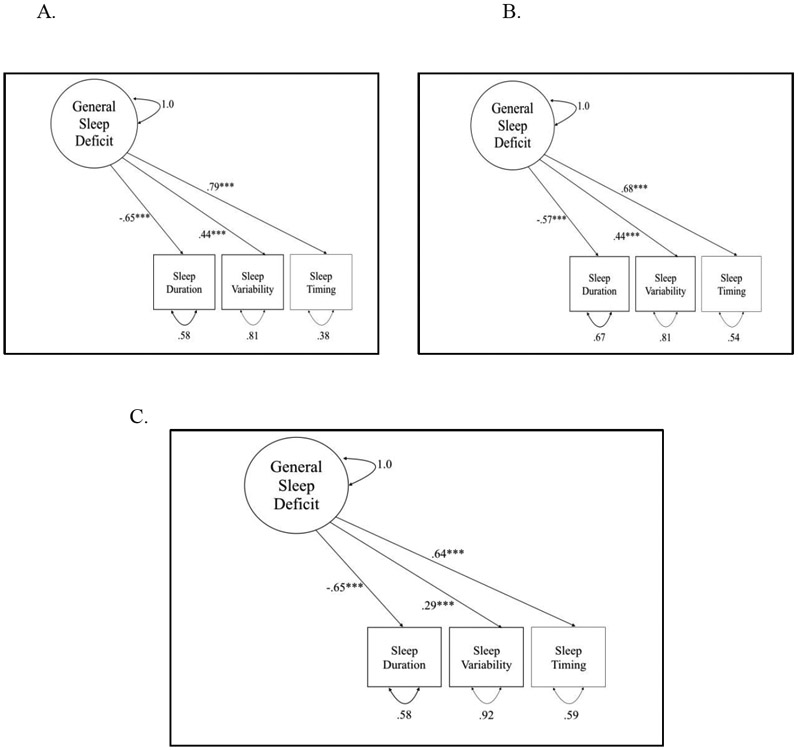
CFA for General Sleep Deficit. A shows the CFA at the first time point, child age 30 months, B at 36 months, and C at 42 months. The fixed factor method of coding was used for each model, as this approach explicitly recognizes that the metric of the latent variable is arbitrary. Therefore, the variance of the construct is fixed to 1 so that the estimated latent factor relations can thereby be estimated in a standardized metric. ***. denotes significance at p < 0.001.
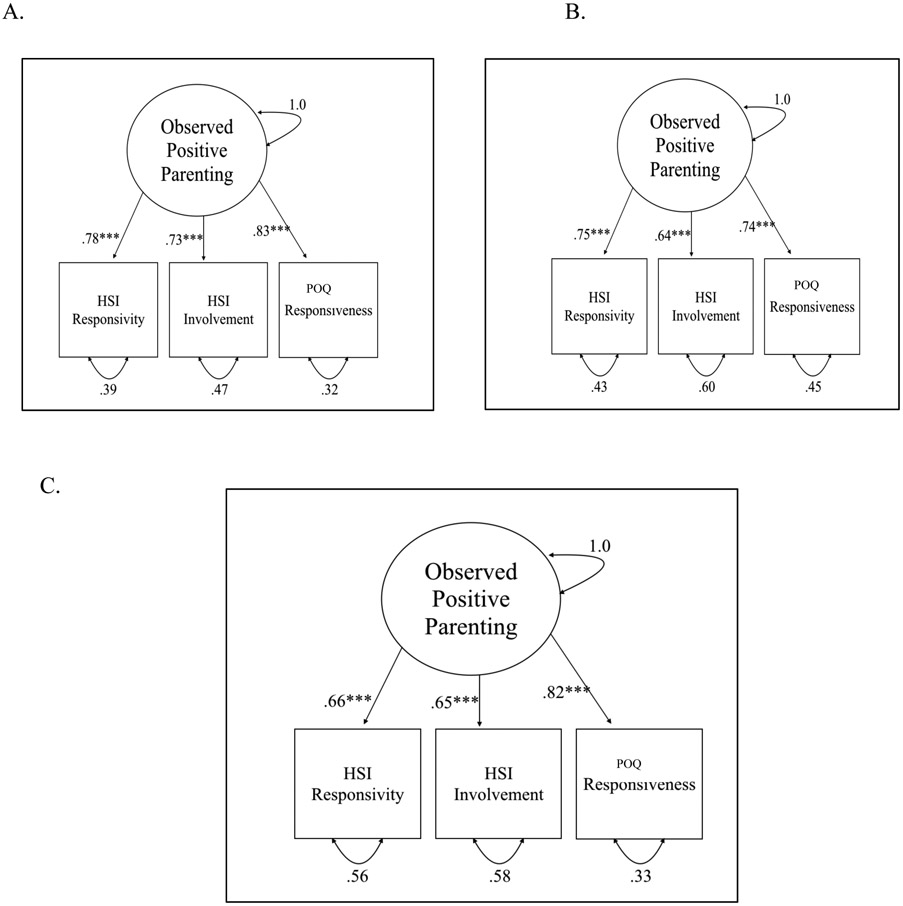
Appendix D.
CFA for Observed Positive Parenting. A shows the CFA at the first time point, child age 30 months, B at 36 months, and C at 42 months. The fixed factor method of coding was used for each model, as this approach explicitly recognizes that the metric of the latent variable is arbitrary. Therefore, the variance of the construct is fixed to 1 so that the estimated latent factor relations can thereby be estimated in a standardized metric. ***. denotes significance at p < 0.001. HSI refers to HOME scale items. POQ refers to Post Observation Questionnaire.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Conflicts of Interest
We have no conflicts of interest to disclose.
References
- 1.Van Reeth O, Weibel L, Spiegel K, et al. : Physiology of sleep–interactions between stress and sleep: from basic research to clinical situations. Sleep Medicine Reviews 2000; 4: 201–219. doi: 10.1053/smrv.1999.0097 [DOI] [Google Scholar]
- 2.Walker MP, van Der Helm E: Overnight therapy? The role of sleep in emotional brain processing. Psychological Bulletin 2009; 135: 731–748. doi: 10.1037/a0016570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McQuillan ME, Bates JE, Staples AD, Deater-Deckard K: Maternal stress, sleep, and parenting. Journal of Family Psychology 2019; 33 (3), 349–359. doi: 10.1037/fam0000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McBride BB, Mills G: A comparison of mother and father involvement with their preschool age children. Early Childhood Research Quarterly 1994; 8: 457–477. doi: 10.1016/S0885-2006(05)80080-8 [DOI] [Google Scholar]
- 5.Zhang J, Li AM, Fok TF, Wing YK: Roles of parental sleep/wake patterns, socioeconomic status, and daytime activities in the sleep/wake patterns of children. Journal of Pediatrics 2010; 156 (4): 606–612. doi: 10.1016/j.jpeds.2009.10.036 [DOI] [PubMed] [Google Scholar]
- 6.Staples AD, Bates JE, Petersen IT: Bedtime routines in early childhood: Prevalence, consistency, and associations with nighttime sleep. Monographs of the Society for Research in Child Development 2015; 80 (1): 141–159. doi: 10.1111/mono.12149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaylor EE, Burnham MM, Goodlin-Jones BL, Anders TF: A longitudinal follow-up study of young children’s sleep patterns using a developmental classification system. Behavioral Sleep Medicine 2005; 3: 44–61. doi: 10.1207/s15402010bsm0301_6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galland BC, Taylor BJ, Elder DE, Herbison P: Normal sleep patterns in infants and children: A systematic review of observational studies. Sleep Medicine Reviews 2012; 16: 213–222. doi: 10.1016/j.smrv.2011.06.001 [DOI] [PubMed] [Google Scholar]
- 9.Sinai D, Tikotzky L: Infant sleep, parental sleep and parenting stress in families of mothers on maternity leave and in families of working mothers. Infant Behavior and Development 2012; 35: 179–186. doi: 10.1016/j.infbeh.2012.01.006 [DOI] [PubMed] [Google Scholar]
- 10.Meltzer LJ, Walsh CM: The impact of pediatric chronic illness on caregiver sleep and daytime functioning, in The Oxford Handbook of Infant, Child, and Adolescent Sleep and Behavior. Edited by Wolfson AR, Montgomery-Downs HE. New York, NY, Oxford University Press, 2013, pp. 140–149. [Google Scholar]
- 11.Meltzer LJ, Westin AM: Impact of child sleep disturbances on parent sleep and daytime functioning, in Sleep and Development: Familial and Socio-cultural Considerations. Edited by El-Sheikh M. New York, NY: Oxford University Press, 2011, pp. 113–131. doi: 10.1093/acprof:oso/9780195395754.003.0006 [DOI] [Google Scholar]
- 12.Kouros CD, El- Sheikh M: Within- family relations in objective sleep duration, quality, and schedule. Child Development 2017; 88(6): 1983–2000. doi: 10.1111/cdev.12667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gregory AM, Moffitt TE, Ambler A, Arseneault L, Houts RM, Caspi A: Maternal insomnia and children’s family socialization environment. Sleep 2012; 35: 579–582. doi: 10.5665/sleep [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chau V, Giallo R: The relationship between parental fatigue, parenting self-efficacy and behavior: Implications for supporting parents in the early parenting period. Child: Care, Health and Development 2015; 41(4): 626–633. doi: 10.1111/cch.12205 [DOI] [PubMed] [Google Scholar]
- 15.Gross RT, Borkovec TD: Effects of a cognitive intrusion manipulation on the sleep-onset latency of good sleepers. Behavior Therapy 1982; 13(1): 112–116. doi: 10.1016/S0005-7894(82)80054-3 [DOI] [Google Scholar]
- 16.Törnroos M, Hakulinen C, Hintsanen M, Puttonen S, Hintsa T, et al. : Reciprocal relationships between psychosocial work characteristics and sleep problems: A two-wave study. Work & Stress 2017; 31(1): 63–81. doi: 10.1080/02678373.2017.1297968 [DOI] [Google Scholar]
- 17.El-Sheikh M, Keiley M, Bagley EJ, Chen E: Socioeconomic adversity and women’s sleep: Stress and chaos as mediators. Behavioral Sleep Medicine 2015; 13(6): 506–523. doi: 10.1080/15402002.2014.940110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ekstedt M, Akerstedt T, Soderstrom M: Microarousals during sleep are associated with increased levels of lipids, cortisol, and blood pressure. Psychosomatic Medicine 2004; 66(6): 925–931. [DOI] [PubMed] [Google Scholar]
- 19.Leproult R, Copinschi G, Buxton O, Van Cauter E: Sleep loss results in an elevation of cortisol levels the next evening. Sleep 1997; 20(10): 865–870. [PubMed] [Google Scholar]
- 20.Minkel JD, Banks S, Htaik O, Moreta MC, Jones CW, McGlinchey EL, Dinges DF: Sleep deprivation and stressors: Evidence for elevated negative affect in response to mild stressors when sleep deprived. Emotion 2012; 12(5): 1015–1020. doi: 10.1037/a0026871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin BJ, Chen HI: Sleep loss and the sympathoadrenal response to exercise. Medicine & Science in Sports & Exercise 1984; 16 (1): 56–59. doi: 10.1249/00005768-198401000-00011 [DOI] [PubMed] [Google Scholar]
- 22.Zohar D, Tzischinsky O, Epstein R, Lavie P: The effects of sleep loss on medical residents’ emotional reactions to work events: a cognitive-energy model. Sleep 2005; 28(1): 47–54. [DOI] [PubMed] [Google Scholar]
- 23.Repetti RL, Wood J. Effects of daily stress at work on mothers' interactions with preschoolers. Journal of Family Psychology. 1997;11(1):90. [Google Scholar]
- 24.Hollingshead AB: Four-factor index of social status. New Haven, CT, Yale University, 1975. [Google Scholar]
- 25.Crnic KA, Greenberg MT: Minor parenting stresses with young children. Child Development 1990; 61(5): 1628–1637. doi: 10.1111/j.1467-8624.1990.tb02889.x [DOI] [PubMed] [Google Scholar]
- 26.Matheny AP, Wachs TD, Ludwig JL, Phillips K: Bringing order out of chaos: Psychometric characteristics of the Confusion, Hubbub, and Order Scale. Journal of Applied Developmental Psychology 1995; 16: 429–444. doi: 10.1016/0193-3973(95)90028-4 [DOI] [Google Scholar]
- 27.Thiagarajan P, Chakrabarty S, Taylor R: A confirmatory factor analysis of Reilly’s Role Overload Scale. Educational and Psychological Measurement 2006; 66:657–666. doi: 10.1177/0013164405282452 [DOI] [Google Scholar]
- 28.Acebo C, Sadeh A, Seifer R, Tzischinsky O, Wolfson AR, Hafer A, Carskadon MA: Estimating sleep patterns with activity monitoring in children and adolescents: How many nights are necessary for reliable measures? Sleep 1999; 22(1):95–103. doi: 10.1093/sleep/22.1.95 [DOI] [PubMed] [Google Scholar]
- 29.Cole RJ, Kripke DF, Gruen W, Mullaney DJ, Gillin JC: Automatic sleep/wake identification from wrist activity. Sleep 1992; 15(5):461–469. [DOI] [PubMed] [Google Scholar]
- 30.Staples AD, Bates JE, Petersen IT, McQuillan ME, Hoyniak C: Measuring sleep in young children and their mothers: Identifying actigraphic sleep composites. International Journal of Behavioral Development 2019; 43(3):278–285. doi: 10.1177/0165025419830236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meltzer LJ, Montgomery-Downs HE, Insana SP, Walsh CM: Use of actigraphy for assessment in pediatric sleep research. Sleep Medicine Reviews 2012; 16(5):463–475. doi: 10.1016/j.smrv.2011.10.00 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bradley RH, Caldwell BM: Home observation for measurement of the environment: A revision of the preschool scale. American Journal of Mental Deficiency 1979; 84(3), 235–244. [PubMed] [Google Scholar]
- 33.Muthen LK, Muthen BO: Mplus user’s guide. Eighth edition. Los Angeles, CA, Muthen & Muthen, 2019. [Google Scholar]
- 34.Little TD, Jorgensen TD, Lang KM, Moore EWG: On the joys of missing data. Journal of Pediatric Psychology 2013; 39(2): 151–162. doi: 10.1093/jpepsy/jst048 [DOI] [PubMed] [Google Scholar]
- 35.Schafer JL, Graham JW: Missing data: Our view of the state of the art. Psychological Methods 2002; 7:147 – 177. doi: 10.1037//1082-989X.7.2.147 [DOI] [PubMed] [Google Scholar]
- 36.Cole DA, Maxwell SE: Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology 2003; 112:558–577. doi: 10.1037/0021-843x.112.4.558 [DOI] [PubMed] [Google Scholar]
- 37.Ong AD, Kim S, Young S, Steptoe A: Positive affect and sleep: A systematic review. Sleep Medicine Reviews 2017; 35: 21–32. doi: 10.1016/j.smrv.2016.07.006 [DOI] [PubMed] [Google Scholar]
- 38.Lopez SJ, Snyder CR: The central role of the heart in generating and sustaining positive emotions. In McCraty R & Rees RA (Eds.), Oxford handbook of positive psychology 2009; (2nd ed., pp. 527–536). New York, NY: Oxford University Press. [Google Scholar]
- 39.Steptoe A, O'Donnell K, Marmot M, Wardle J: Positive affect, psychological well-being, and good sleep. Journal of Psychosomatic Research 2008; 64(4), 409–415. doi: 10.1016/j.jpsychores.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 40.Duncan GJ, Magnuson KA. Off with Hollingshead: Socioeconomic resources, parenting, and child development. Socioeconomic status, parenting, and child development. 2003:83–106. [Google Scholar]
- 41.DeJoseph ML, Sifre RD, Raver CC, Blair CB, Berry D. Capturing environmental dimensions of adversity and resources in the context of poverty across infancy through early adolescence: A moderated nonlinear factor model. Child Development. 2021; doi: 10.1111/cdev.13504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peltz JS, Rogge RD, Sturge-Apple ML, O'Connor TG, Pigeon WR. Reciprocal influences among family processes and toddlers’ sleep problems. Journal of Family Psychology. 2016. Sep;30(6):720. [DOI] [PubMed] [Google Scholar]
- 43.Gislason T, Almqvist M: Somatic diseases and sleep complaints. Acta Medica Scandinavica 1987; 221(5), 475–481. doi: 10.1111/j.0954-6820.1987.tb01283.x [DOI] [PubMed] [Google Scholar]