Introduction
Patients hospitalized with coronavirus disease 2019 (COVID-19) have demonstrated significant care needs after discharge, particularly among older adults and those with pre-admission frailty.1 Characteristics and outcomes of patients hospitalized with COVID-19 have been well described,2 but few studies have examined patterns in post-acute care (PAC) utilization over the course of a COVID-19 surge.3 Evaluating these trends may inform planning for future surges.
During the initial COVID-19 surge, PAC facilities and resources were limited due to lack of personal protective equipment, internal COVID-19 outbreaks, and staffing shortages. To address these shortages in Boston, Massachusetts, PAC sites for patients with COVID-19 were created, including Boston Hope Field Hospital4 and dedicated units at skilled nursing facilities (SNFs) in the community.5 We describe patterns in PAC utilization, including placement in PAC facilities (SNFs, long-term acute care (LTAC), and inpatient rehabilitation (IRF)) and referral to home health agencies (HHA) among patients age 50 years or older with COVID-19 at a tertiary-care 1,043 bed hospital in Massachusetts.
Methods
Patients age 50 or older with COVID-19 admitted during the 12-week (3/11/20–6/3/20) surge were included. Patients admitted from PAC facilities (including short-stay and long-term care) prior to their acute hospitalization were excluded. We used data from the MGH COVID-19 Data Registry6 and 4Next, a case management application, to evaluate trends in discharge disposition relative to the opening of dedicated COVID-19 PAC facilities.
Results
836 patients were included in the cohort. The mean age was 69 years. Most patients self-identified as white (44%) or Hispanic (30%), and 40% had limited English proficiency. While many were admitted from private homes (77%), a significant portion (13%) presented from assisted living facilities. Approximately one third (35%) of patients had an ICU stay, 85% of whom were intubated. The median LOS was eight days, and the mean LOS was 14.
Half of the patients (50%) were discharged to home, but less than one third of those discharged home (16% of total) received HHA services. Approximately one third (31%) were discharged to a PAC facility. The majority of PAC discharges (17% of total) were to LTACs as compared to SNFs (10% of total) and IRFs (4% of total).
In the initial six weeks, 35% of the cohort was discharged to PAC facilities or home with HHA services (Figure A). This increased in concert with the opening of dedicated COVID-19 PAC sites, to 59% over the remainder of the surge. In the final weeks, when fewer patients with COVID-19 were discharged, nearly 60% were discharged PAC facilities and no patients were discharged home without HHA services. SNF referrals for all hospitalized patients peaked to an average of 15 referrals per patient from a pre-pandemic average of four (Figure B).
Figure.
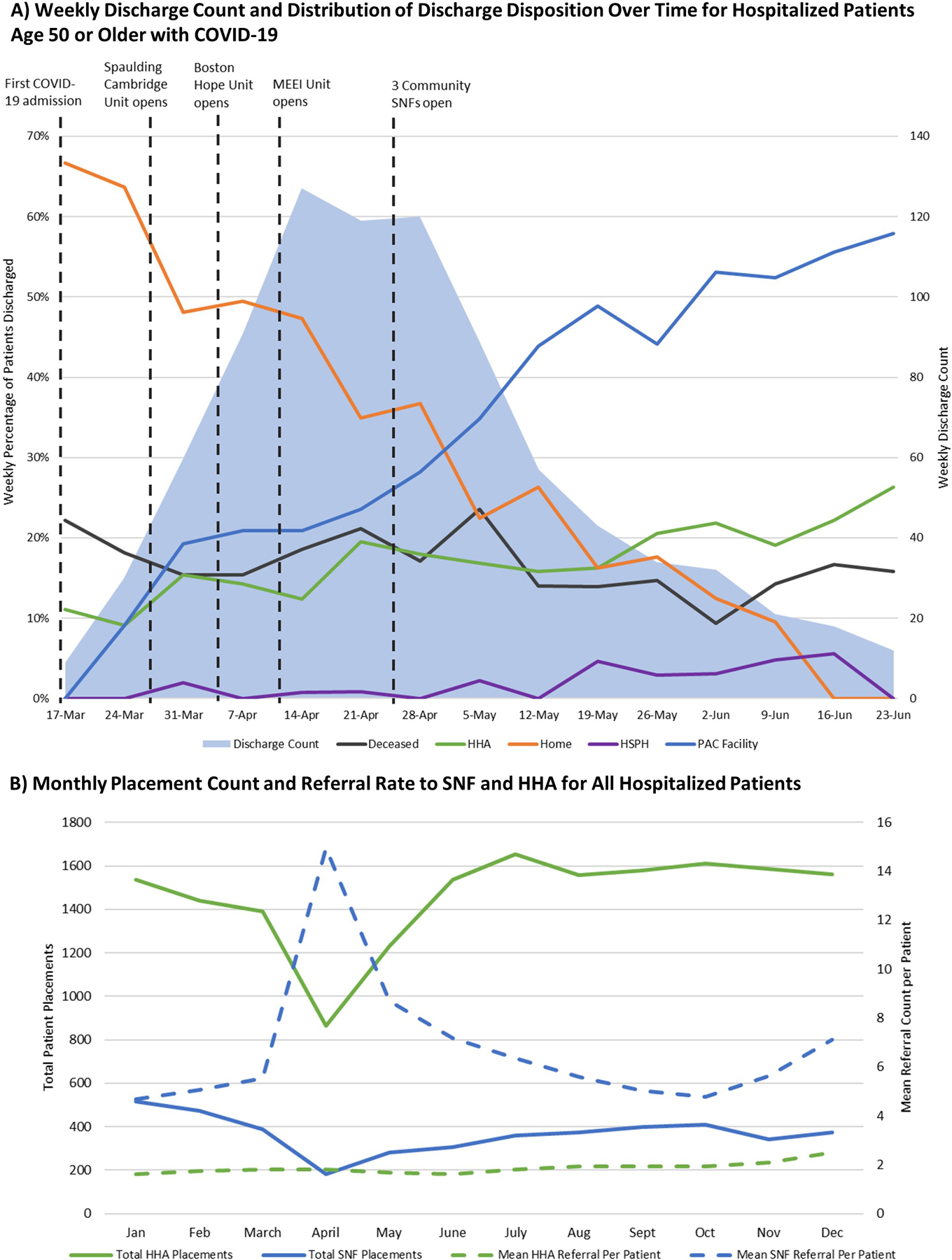
A) Weekly Discharge Count and Distribution of Discharge Disposition Over Time for Hospitalized Patients Age 50 or Older with COVID-19 shows the weekly discharge count and distribution of discharge disposition over time for admitted patients 50 years or older with COVID-19. The solid blue area represents the weekly discharge count and demonstrates the surge of COVID-19 cases. Each colored line represents the weekly percentage of discharged patients for each discharge disposition. The vertical dashed lines indicate relevant events including the date of the first admission of a patient with COVID-19 and the opening of dedicated PAC facilities for patients with COVID-19 in Boston, Massachusetts including units at Spaulding Hospital, Boston Hope Field Hospital, Massachusetts Eye and Ear Infirmary (MEEI) and three community SNFs.
B) Monthly Placement Count and Referral Rate to SNF and HHA for All Hospitalized Patients Shows the monthly average number of referrals made for SNF (blue dashed) and HHA (green dashed) and the monthly count of SNF (blue solid) and HHA (green solid) placements for all patients hospitalized during 2020.
Discussion
During this COVID-19 surge, hospitalized adults age 50 or older with COVID-19 faced significant PAC challenges including limited access and increased PAC needs. As the pandemic emerged, considerable attention was paid to anticipated acute inpatient needs, however, preparation for PAC use was less robust.7 Few facilities accepted patients with COVID-19 initially, and many were unable to operate at capacity.
Our referral findings suggest that access to SNFs was severely limited during the COVID-19 surge and that this improved over time as auxiliary discharge locations opened. In addition, strict admission requirements to LTAC and IRF8 were waived to facilitate movement of patients across the care spectrum as seen in our cohort.
PAC needs remained high compared to a pre-pandemic baseline. For all-payer discharges in Massachusetts in 2016, 18% of all patients were discharged to PAC facilities9 as compared to 31% in our cohort. Early in the surge, most patients were discharged home without HHA services. Over time PAC resource utilization steadily rose. Mean Charlson Comorbidity Index scores and ICU stay rates remained stable over the surge (data not shown), suggesting unmet PAC needs early on.
Limited PAC access likely impacted hospital LOS, which was prolonged. We observed a mean LOS of 14 days compared to the average for all patients prior to the pandemic of eight days and an expected LOS for community acquired pneumonia of five days.10 These LOS results are similar to other published studies.2
This study is unique because it describes striking patterns of PAC utilization for a large cohort of patients over a COVID-19 surge. COVID-19 outbreaks are ongoing around the world, and this pandemic has demonstrated our population’s vulnerability to future pathogens. This work can inform surge planning and help systems optimize hospital outflow and PAC access, both critical for hospitals to simultaneously continue COVID-19 and non-COVID-19 related care.
Acknowledgements
The authors thank Helaine Rockett, MS, RD for data support, and Ryan Thompson MD for logistical support and guidance of this work.
Disclosures
Dr. Bassett is supported by the Weissman Family MGH Scholar Award (R01 AI042006-24S1) and the National Institutes of Health (NIH award K24AI141036). Dr. Baughman is supported by the Winickoff Scholars Program.
Sponsor’s Role
None of the study sponsors participated in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
Footnotes
Portions of the work presented in this paper have been previously presented as a poster at both the Society for General Internal Medicine Annual Meeting and at the Society for Hospital Medicine District 1 Regional Meeting. This paper has not been published previously.
Conflict of Interest
There are no financial or personal conflicts to declare.
Citations
- 1.Vilches-Moraga A, Price A, Braude P, et al. Increased care at discharge from COVID-19: The association between pre-admission frailty and increased care needs after hospital discharge; a multicentre European observational cohort study. BMC Med 2020. Doi: 10.1186/s12916-020-01856-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suleyman G, Fadel RA, Malette KM, et al. Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit. JAMA Netw Open. 2020;3(6):e2012270. doi: 10.1001/jamanetworkopen.2020.12270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Werner R, Bressman E. Trends in Post-Acute Care Utilization During the COVID-19 Pandemic. JAMDA 2021. Doi: 10.1016/j.jamda.2021.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baughman AW, Hirschberg RE, Lucas LJ, et al. Pandemic care through collaboration: lessons from a COVID-19 field hospital. J Am Med Dir Assoc 2020. Doi: 10.1016/j.jamda.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen A Spaulding Hospital in Cambridge Opens a Dedicated COVID-19 Recovery Unit. wbur.org. Available at: https://www.wbur.org/commonhealth/2020/03/30/spaulding-hospital-cambridge-covid-19-coronavirus-unit. Accessed March 2, 2021.
- 6.Bassett IV, Triant VA, Bunda BA, et al. MGH Covid-19 registry reveals two distinct populations of hospitalized patients by race and ethnicity. PLoS One 2020. Doi: 10.1371/journal.pone.0244270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maloney Matthew, Morley Ryan, Checketts Robert, et al. Planning for the Aftershock: a model of post-acute care needs for hospitalized COVID-19 patients. medRxiv 2020. Doi: 10.1101/2020.06.12.20129551. [DOI] [Google Scholar]
- 8.COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers. CMS. Available at: https://www.cms.gov/files/document/covid19-emergency-declaration-health-care-providers-fact-sheet.pdf. Accessed August 15, 2021. [Google Scholar]
- 9.2019 Annual Health Care Cost Trends Report. Massachusetts Health Policy Commission. Available at: https://www.mass.gov/doc/2019-cost-trends-report-chartpack/download. Accessed August 15, 2021
- 10.Ramirez JA, Wiemken TL, Peyrani P, et al. Adults hospitalized with pneumonia in the United States: incidence, epidemiology, and mortality. Clin Infect Dis 2017. Doi: 10.1093/cid/cix647. [DOI] [PubMed] [Google Scholar]


