Abstract
Background:
Tearing and insufficiency of the ulnar collateral ligament (UCL) of the elbow result in valgus instability, which can lead to pain while throwing and decline in performance in overhead athletes.
Purpose:
To assess the clinical results of a modified UCL reconstruction technique using 1 bone hole in the ulna and 1 bone tunnel in the humerus in baseball players.
Study Design:
Case series; Level of evidence, 4.
Methods:
The inclusion criteria were medial elbow pain preventing effective playing, clinically medial elbow laxity, and magnetic resonance imaging results consistent with UCL injury. Patients who were engaged in other sports and in other positions in baseball except pitchers were excluded from this study. Our modified Tommy John procedure was performed via a muscle-splitting approach and an original single-bone-tunnel technique, using a suture anchor. After a minimum of 24 months, patients were evaluated using the Conway scale and the Timmerman-Andrews score.
Results:
Of 31 patients, 20 baseball pitchers (20 male: 5 high school, 5 collegiate, 8 nonprofessional, and 2 professional pitchers) were reviewed. The mean patient age at the time of operation was 21.9 years, and the mean postoperative follow-up period was 35.1 months (range, 24-66 months). The mean Timmerman-Andrews subjective score improved significantly from pre- to postoperatively (from 68.3 to 98.3; P < .05); the objective score also improved significantly (from 81.1 to 96.4; P = .01). No complications were detected at the latest follow-up. Overall, 19 patients were able to return to their preinjury level of sports or higher.
Conclusion:
UCL reconstruction with 1 bone hole in the ulna and 1 bone tunnel in the humerus demonstrated satisfactory results in baseball pitchers. Our modified technique was safe and achieved satisfactory clinical results, with a 95% rate of return to sports.
Keywords: autografts, elbow, ligaments, return to sport, suture anchors, throwing injury, UCL reconstruction
The ulnar collateral ligament (UCL), the medial ligamentous structure of the elbow joint, is composed of 3 substructures: the anterior, posterior, and transverse bundles. The anterior bundle functions as the primary stabilizer of the elbow joint against valgus stress. 8,15 During the acceleration phase of throwing, 64 N·m varus torque is estimated to result at the elbow joint. 14 The chronic repetitive trauma of throwing can result in injury or tear of this bundle. Injury to the UCL of the elbow results in valgus instability, which can cause pain during throwing and decline in performance.
Since Jobe et al 17,18 first reported on UCL reconstruction in overhead throwers in 1986 using a technique known as the figure-of-8 procedure, UCL reconstruction has been performed using a palmaris longus tendon autograft. In this method, detachment of the flexor-pronator muscles from their origin is mandatory for preparing the medial epicondyle. Simultaneously, the ulnar nerve is transferred as well. It has been reported that 62.5% of patients undergoing this surgery return to their preinjury level of sports. 9 Thompson et al 35 demonstrated better outcomes and fewer complications using a modified technique, which includes use of a muscle-splitting approach. Subsequently, a number of reports have depicted successful results using modified techniques or various devices with the original technique ¶ such as docking, 11,21,30 modified docking, 5,27 and DANE TJ techniques. 10
Since the original fixation with bone tunnels was developed by Jobe et al, 18 other fixation devices have been developed, including interference screws, 1,20,22,24 suture anchors, 16 and suspensory cortical buttons. 3,7 In terms of graft fixation to the bone, most of these techniques require a minimum of 1 bone tunnel in both the ulna and the humerus. Hechtman et al 15 demonstrated a UCL reconstruction technique using suture anchors at both of the insertion sites and reported no significant difference in the strength of reconstruction between suture anchors and bone tunnels.
The figure-of-8 procedure typically needs 3 bone tunnels in the humerus and 2 in the ulna; however, we have developed a modified figure-of-8 technique in which a suture anchor needs only 1 bone hole in the ulna. In addition, we have found that turning the graft back minimizes the number of bone holes in the medial epicondyle of the humerus without an implant. The purpose of this study was to assess the clinical results of our modified Tommy John procedure in high school, collegiate, and professional baseball pitchers. We hypothesized that with regard to the clinical results and rate of return to sports, our modified technique would show similar results in comparison with other methods.
Methods
This study was performed with ethics committee approval from our institution. We retrospectively reviewed baseball pitchers who underwent UCL reconstruction. Between 2006 and 2011, a total of 31 consecutive patients were treated using UCL reconstruction by a single surgeon (K.S.). All patients had elbow pain at the medial side, which was related to UCL insufficiency or injury. On physical examination, they showed a positive sign of moving valgus stress test, pain with valgus stress, or unsatisfied performance in throwing. All patients underwent ultrasonography and magnetic resonance imaging (MRI) showing partial or complete tears (n = 15) and instability of the UCL (n = 16). Valgus instability of the throwing elbow was assessed with the elbow in 90° of flexion using ultrasonography and compared with that of the nonthrowing side. Before surgical treatment, all patients had undergone a minimum 12-week period of nonoperative therapy that included rest and physical therapy, a treatment that eventually failed for all patients. In all patients, cortisone and platelet-rich plasma were not administered before surgery. Written informed consent was obtained from all patients.
The indications for surgical reconstruction were persistent pain with valgus stress test, low performance in throwing, or inability to throw at the preinjury level without pain after nonoperative treatment for a minimum of 12 weeks.
Arthroscopic Assessment
Intra-articular assessment routinely was performed arthroscopically. In the anterior and posterior compartments, articular cartilage and synovium were evaluated via the lateral portal, transtriceps, and posteromedial portal, respectively. If pathologic conditions such as loose body and spurs were identified, they were removed via an arthroscopic procedure.
Operative Technique
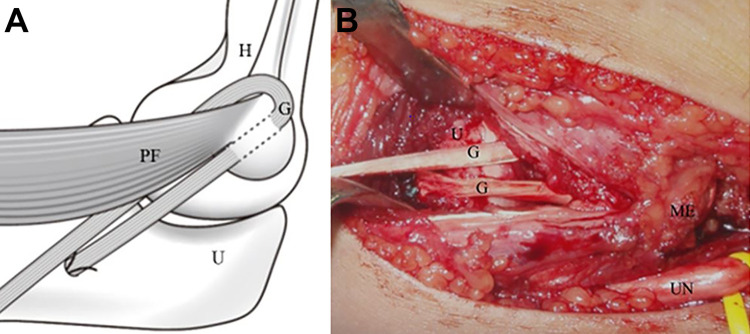
We used a modified technique based on the Tommy John procedure. The patient was placed in the supine position. The forearm was then positioned on the operating table. The palmaris longus tendon was harvested for the reconstruction as an autograft from the ipsilateral side in all patients. The graft was prepared to pass through the humeral bone tunnel and ulnar bone hole for the suture anchor using No. 2.0 nonabsorbable braided sutures fastened on 1 end. An oblique 6-cm incision was made precisely at the anterior proximal area of the medial epicondyle and swept distally. The medial antebrachial cutaneous nerve and ulnar nerve were identified for their protection. Dissection was performed down to the fascia covering the flexor-pronator mass. A muscle-splitting approach was used through the common flexor-pronator muscles in the anterior part of the flexor carpi ulnaris muscle. 31 A longitudinal split was made in the posterior part of the muscle to reach the anterior bundle of the UCL. After the exposure of that bundle, a longitudinal incision was made, identifying the joint line via a needle. Subsequently, at the anterior area of the sublime tubercle of the ulna, the bone hole for a suture anchor was created while protecting the ulnar nerve using a 3.2-mm drill. The first end of the graft was tied with the suture from the anchor, keeping the edge of its end inside the bone hole. The tunnel position at the humerus was located in the anterior part of the medial epicondyle. A longitudinal incision was made within the remaining UCL for the preparation of a humeral bone tunnel. That tunnel was created in the medial epicondyle using a 3.2-mm drill. The second end of the graft was passed through the bone tunnel in the humerus and then distally turned back (Figure 1).
Figure 1.
Passing of the graft through the bone tunnel at the humerus after fixation of 1 end of the graft at the ulna. The arrow indicates the bone hole for the suture anchor, and the arrowheads indicate the bone tunnel at the medial epicondyle. G, palmaris longus tendon graft; H, humerus; ME, medial epicondyle of the humerus; PF, pronator teres and flexor carpi ulnaris muscles; U, ulna.
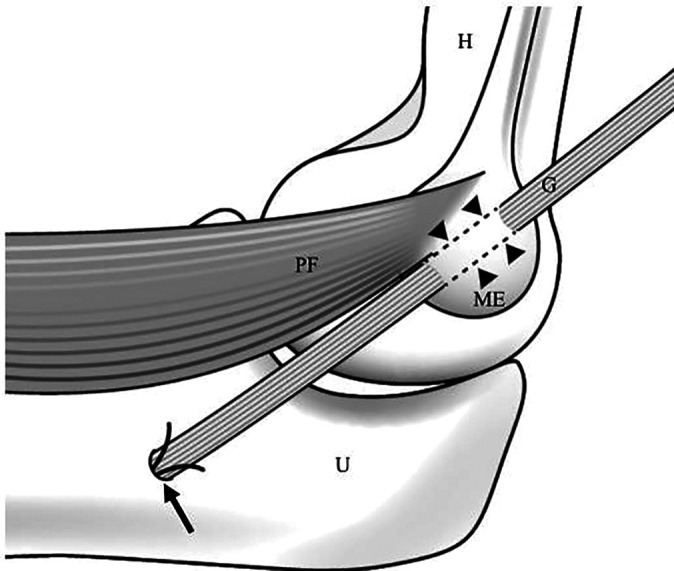
After the graft was folded, the folded end was passed underneath the pronator teres and the flexor carpi ulnaris muscles near their origin from the medial epicondyle (Figure 2).
Figure 2.
(A) Turn-back of the grosteophytes were removed arthroscopically underneath the pronator teres and the flexor carpi ulnaris muscles near the origin of the graft at the medial epicondyle. (B) Intraoperative photograph of the turn-back of the graft underneath the pronator teres and the flexor carpi ulnaris muscles near the origin of the graft at the medial condyle. G, palmaris longus tendon graft; H, humerus; ME, medial epicondyle of the humerus; PF, pronator teres and flexor carpi ulnaris muscles; U, ulna; UN, ulnar nerve.
The surgeon tensioned the graft, holding the patient’s arm at 30° of flexion while adding varus stress manually. The second end was tied around the first end of the graft and the distal remnant of the UCL at the ulna. Both ends of the graft were fixed using nonabsorbable sutures. After suturing, the excessive length of the graft was folded again in the proximal direction and was tied to the graft itself for reinforcement (Figure 3). Finally, sutures were added to reduce the gap between both sides of the grafts.
Figure 3.
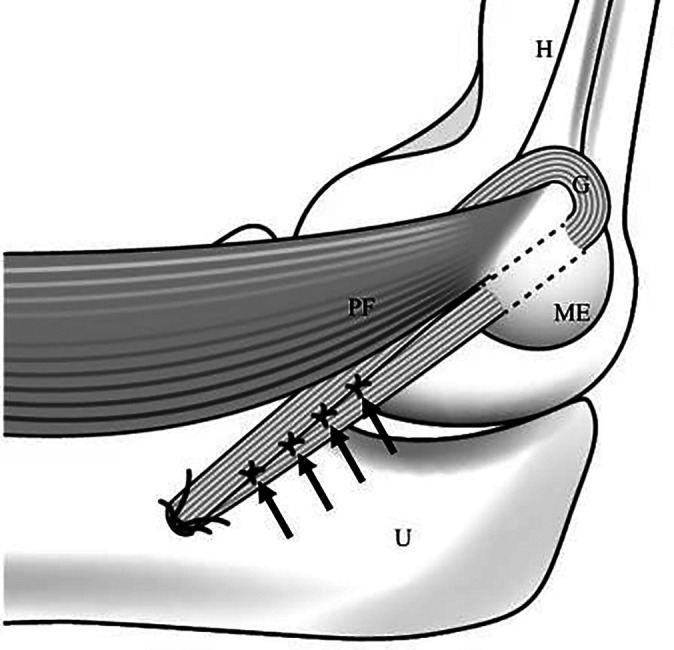
Suturing of the second end of the graft around the first end of the graft and additional suturing of the graft itself. The arrows indicate the interlaced sutures of the tendon graft sides. G, palmaris longus tendon graft; H, humerus; ME, medial epicondyle of the humerus; PF, pronator teres and flexor carpi ulnaris muscles; U, ulna.
Postoperative Therapy
The elbow was immobilized in a splint for 2 weeks at 60° of flexion. Then, the splint was transitioned to a hinged elbow brace so the patients could start passive and active assisted elbow flexion and extension without valgus stress. At 6 weeks after surgery, the hinged brace was removed, and strength training of the forearm and shoulder was allowed to start without valgus stress at the elbow. At 12 weeks after surgery, gradual progression of valgus stress was permitted to start during strength training. A throwing program began 16 weeks postoperatively. At 6 months after surgery, the patients were allowed to start pitching from the mound.
Postoperative Evaluation
All patients were available for follow-up. Preoperatively and at the final follow-up, clinical evaluation was performed using the Conway scale and the Timmerman-Andrews score. 36 The elbow range of motion and return to baseball pitching performance (ie, preinjury or higher level) were also assessed.
Statistical Analysis
Comparisons between preoperative and postoperative data were performed using a paired t test. Values of P < .05 were considered statistically significant. These statistical analyses were performed using R Version 1.33 (Saitama Medical Center, Jichi Medical University). 19 The post hoc power analysis was performed to evaluate power (1−β) using G*Power3 Version 3.1.9.2 statistical analysis software (Heinrich Heine University Duesseldorf), 12,13 with significance (α) set at .05.
Results
Of the 31 patients, 5 patients who were engaged in other sports (judo, javelin, and basketball) and 4 baseball players at other positions (2 catchers and 2 field players) were excluded from this study. A total of 22 pitchers met the inclusion criteria. Of these 22 baseball pitchers, 2 patients (9%) were lost to follow-up after 24 months. Thus, overall, 20 baseball pitchers were reviewed. All 20 patients were male, including 5 high school, 5 collegiate, 8 nonprofessional, and 2 professional pitchers. The average age at the time of the reconstruction was 21.9 years (range, 17-31 years). The mean postoperative follow-up period was 35.1 months (range, 24-66 months). The involved extremity was dominant in all cases. The dominant side in all of the patients were the same as throwing side.
There were no intraoperative complications, and all patients were available for follow-up at a mean of 35.9 months after surgery (range, 24-55 months). In 9 of these patients (45%), osteophytes were removed arthroscopically from the posteromedial margin of the olecranon, the edge of the coronoid process, or both. Loose bodies were removed in 7 patients (35%). The ulnar nerve was transposed subcutaneously in 3 patients (15%) because of preoperative ulnar nerve symptoms. A total of 19 patients (95%) returned to their preinjury level of sports or higher, indicated by an excellent grade on the Conway scale. Only 1 patient was not able to return to pitching at his preinjury level; he decided to stop playing baseball after graduating from college.
Significant improvement was shown in scores by using the Timmerman-Andrews 100-point subjective scoring system: a mean preoperative score of 68.3 (range, 60-85) and a mean postoperative score of 98.3 (range, 85-100) (P < .05). Furthermore, in terms of objective score, the preoperative score of 81.1 recovered to a postoperative score of 96.4, which was a significant difference (P < .01). By the grading scale of the Timmerman-Andrews total scoring system, the postoperative outcome was excellent in 18 patients (90%) and good in 2 patients (10%) at the final follow-up time. There were no postoperative infections or neurologic complications.
Discussion
In this study, we evaluated the clinical results and the rate of return to sports in baseball pitchers after UCL reconstruction with a modified figure-of-8 technique. The modification for this technique, which entails folding and passing the graft tendon underneath the pronator teres and the flexor carpi ulnaris muscles near the origin of the graft, minimized the number and size of tunnels in the medial epicondyle of the humerus. Additionally, the use of an ulnar suture anchor did not require a bone tunnel but rather required only a bone hole, which did not have an aperture at the opposite side of the cortex of the ulnar sublime tubercle. This modification also reduced exposure of the posterior part of the ulnar sublime tubercle and decreased detachment of the origin of the flexor digitorum superficialis and profundus muscles. In the clinical evaluation of this study, 95% of the pitchers (all except 1 patient) could return to their preinjury level of performance.
Since Jobe et al 18 initially demonstrated elbow UCL reconstruction, which has been called the figure-of-8 technique, multiple techniques and modifications have been described. 2,4,5,9 –11,16,21,27,30 In the figure-of-8 technique, 2 and 3 bone tunnels in the ulna and the humerus, respectively, are prepared for passing and fixing the graft. Rohrbough et al 30 described the revised procedure of UCL reconstruction as the docking technique. This procedure and the modified docking technique need 1 bone tunnel in the anterior and posterior parts of the sublime tubercle and a Y-shaped tunnel in the medial epicondyle for passing and fixing the grafts. 5,27,30 Additionally, the use of interference screws has made it possible to fix grafts using only 1 bone tunnel in each bone, providing sufficient strength for graft fixation. 1,20,22,24 In contrast, Hechtman et al 15 reported that use of a suture anchor, which does not need bone tunnels but requires a hole with 1 aperture, could be a less invasive surgery. In addition, biomechanically, no significant difference was shown in reconstruction strength with the use of bone anchors versus bone tunnels. 15 In our procedure, after the graft was passed through the bone hole in the medial condyle and turned back, the graft was fixed underneath the flexor muscle to avoid creating an additional bone hole in the humerus.
In the figure-of-8 and docking procedures, fixation materials are not required. Instead, for graft passing, 4,9,11,27,30 the figure-of-8 technique requires double 3 mm–diameter and 4 mm–diameter holes in the ulna and the humerus, respectively. 4,9 In the docking and modified docking techniques, while a single 4 to 5 mm–diameter bone tunnel with 2 small apertures is created in the medial epicondyle, double 3 to 3.5 mm–diameter tunnels are prepared. 5,11,27,30 However, when interference screws are used, a 4.5 mm–diameter bone tunnel is needed on both sides. 20 In our procedure, using suture anchors made it possible to fix the graft using only 1 bone hole of 3.2-mm diameter in the humerus and 1 bone tunnel of 3.2-mm diameter in the ulna. This method could decrease the risk of medial epicondyle fracture. In addition, bone anatomic features differ among individual baseball players. 6 Therefore, it could be difficult to apply the same tunnel sizes and configurations to each athlete. Anatomic differences have been reported in the shoulders of the throwing side due to adaptive changes during growth and development. 33,34 Changes to the medial epicondyle of the throwing side also have been identified from youth to adolescent baseball players through the use of ultrasonography, radiography, or MRI. 23,26,28,37 Therefore, it is possible that similar adaptive changes may exist in the elbows of throwing athletes caused by the effects of repetitive throwing on the ulnar sublime tubercle. As a result, our modified technique could be an efficient surgical option in patients who have a small medial epicondyle.
To fix the graft during docking and figure-of-8 procedures, 2 apertures have to be prepared at the proximal area of the medial epicondyle. 4,9,11,27,30 Between these 2 apertures, a bone bridge with a minimum 5- to 10-mm margin is needed to resist valgus torque and support the graft itself until it is healed between the bone and tendon interface. In our technique, after the graft is passed through humeral bone tunnel, the graft goes through the layer between the flexor mass and the capsule of the elbow. This makes the anterior half of the medial epicondyle capable of supporting the graft. Moreover, the flexor mass was thought to play a role in preventing excessive movement of the graft around the medial epicondyle. Side-to-side suturing of the graft, after passing under the flexor mass, would reinforce the graft itself and avoid excessive slipping and movement of the graft.
In the ulnar sublime tubercle, 1 bone hole is necessary for inserting a suture anchor, and this tunnel does not violate the opposite cortex. It also does not require an aperture to pass the graft to the opposite side of the cortex and does not require exposing the posterior part of the sublime tubercle, which is near the path of the ulnar nerve. Moreover, while the graft is turned back anteriorly, the posterior side of the medial epicondyle, which is also close to the path of the ulnar nerve, does not have to be exposed excessively. These procedures for the ulnar nerve could be related to the absence of postoperative complications.
Several studies have demonstrated a rate of return to sports from 67.5% to 92% after the initial Jobe technique. # The docking technique and its modifications have shown high rates of return to sports, from 85% to 92%, in Major League Baseball players. 5,16,27 Moreover, 77% to 84% of high school and collegiate baseball players have been reported to return to baseball at the same or higher level. 25,29,32 The level of baseball pitching performance in our study was different from that reported in previous studies because we included both high school and professional players. However, our technique showed a 95% return to preinjury or higher level of sports. This technique can be considered highly reliable in baseball pitchers.
The present study has several limitations. First, this study was a retrospective study and did not have a control group. Second, the results of this study did not include detailed degrees of competitiveness or performance metrics. Third, the patient cohort was not uniform. Fourth, in terms of the technique, no biomechanical study was performed to test initial strength against valgus stress. Fifth, because the graft was passed between the flexor mass and the capsule to minimize the number and size of bone holes in the humerus, its effect on the flexor mass is unknown. However, we believe that graft passage underneath the flexor mass would also contribute to reinforcing and stabilizing the graft during the throwing motion. As a next step, we will evaluate the use of a revised fixation material, which has greater pullout strength and better healing potential and would improve the UCL reconstruction.
Conclusion
UCL reconstruction with 1 bone hole in the ulna and 1 bone tunnel in the humerus demonstrated satisfactory results in baseball pitchers. This technique would minimize the number and size of bone tunnels and holes in the humerus and ulna.
Footnotes
Final revision submitted September 18, 2020; accepted November 13, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Nagoya City University (study No. 1263).
References
- 1. Ahmad CS, Lee TQ, ElAttrache NS. Biomechanical evaluation of a new ulnar collateral ligament reconstruction technique with interference screw fixation. Am J Sports Med. 2003;31(3):332–337. [DOI] [PubMed] [Google Scholar]
- 2. Andrews JR, Timmerman LA. Outcome of elbow surgery in professional baseball players. Am J Sports Med. 1995;23(4):407–413. [DOI] [PubMed] [Google Scholar]
- 3. Armstrong AD, Dunning CE, Ferreira LM, Faber KJ, Johnson JA, King GJ. A biomechanical comparison of four reconstruction techniques for the medial collateral ligament-deficient elbow. J Shoulder Elbow Surg. 2005;14(2):207–215. [DOI] [PubMed] [Google Scholar]
- 4. Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28(1):16–23. [DOI] [PubMed] [Google Scholar]
- 5. Bowers AL, Dines JS, Dines DM, Altchek DW. Elbow medial ulnar collateral ligament reconstruction: clinical relevance and the docking technique. J Shoulder Elbow Surg. 2010;19(2)(suppl):110–117. [DOI] [PubMed] [Google Scholar]
- 6. Byram IR, Khanna K, Gardner TR, Ahmad CS. Characterizing bone tunnel placement in medial ulnar collateral ligament reconstruction using patient-specific 3-dimensional computed tomography modeling. Am J Sports Med. 2013;41(4):894–902. [DOI] [PubMed] [Google Scholar]
- 7. Camp CL, Bernard C, Benavitz B, Konicek J, Altchek DW, Dines JS. Reconstruction of the medial ulnar collateral ligament of the elbow: biomechanical comparison of a novel anatomic technique to the docking technique. Orthop J Sports Med. 2019;7(7):2325967119857592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ciccotti MG, Jobe FW. Medial collateral ligament instability and ulnar neuritis in the athlete’s elbow. Instr Course Lect. 1999;48:383–391. [PubMed] [Google Scholar]
- 9. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes: treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74(1):67–83. [PubMed] [Google Scholar]
- 10. Dines JS, ElAttrache NS, Conway JE, Smith W, Ahmad CS. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;35(12):2039–2044. [DOI] [PubMed] [Google Scholar]
- 11. Dodson CC, Thomas A, Dines JS, Nho SJ, Williams RJ III, Altchek DW. Medial ulnar collateral ligament reconstruction of the elbow in throwing athletes. Am J Sports Med. 2006;34(12):1926–1932. [DOI] [PubMed] [Google Scholar]
- 12. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. [DOI] [PubMed] [Google Scholar]
- 13. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. [DOI] [PubMed] [Google Scholar]
- 14. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23(2):233–239. [DOI] [PubMed] [Google Scholar]
- 15. Hechtman KS, Tjin ATEW, Zvijac JE, Uribe JW, Latta LL. Biomechanics of a less invasive procedure for reconstruction of the ulnar collateral ligament of the elbow. Am J Sports Med. 1998;26(5):620–624. [DOI] [PubMed] [Google Scholar]
- 16. Hechtman KS, Zvijac JE, Wells ME, Botto-van Bemden A. Long-term results of ulnar collateral ligament reconstruction in throwing athletes based on a hybrid technique. Am J Sports Med. 2011;39(2):342–347. [DOI] [PubMed] [Google Scholar]
- 17. Jobe FW, Nuber G. Throwing injuries of the elbow. Clin Sports Med. 1986;5(4):621–636. [PubMed] [Google Scholar]
- 18. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68(8):1158–1163. [PubMed] [Google Scholar]
- 19. Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48(3):452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kodde IF, Rahusen FT, Eygendaal D. Long-term results after ulnar collateral ligament reconstruction of the elbow in European athletes with interference screw technique and triceps fascia autograft. J Shoulder Elbow Surg. 2012;21(12):1656–1663. [DOI] [PubMed] [Google Scholar]
- 21. Koh JL, Schafer MF, Keuter G, Hsu JE. Ulnar collateral ligament reconstruction in elite throwing athletes. Arthroscopy. 2006;22(11):1187–1191. [DOI] [PubMed] [Google Scholar]
- 22. Large TM, Coley ER, Peindl RD, Fleischli JE. A biomechanical comparison of 2 ulnar collateral ligament reconstruction techniques. Arthroscopy. 2007;23(2):141–150. [DOI] [PubMed] [Google Scholar]
- 23. Lee YY, Yang TH, Huang CC, et al. Ultrasonography has high positive predictive value for medial epicondyle lesions among adolescent baseball players. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3261–3268. [DOI] [PubMed] [Google Scholar]
- 24. McAdams TR, Lee AT, Centeno J, Giori NJ, Lindsey DP. Two ulnar collateral ligament reconstruction methods: the docking technique versus bioabsorbable interference screw fixation—a biomechanical evaluation with cyclic loading. J Shoulder Elbow Surg. 2007;16(2):224–228. [DOI] [PubMed] [Google Scholar]
- 25. Osbahr DC, Cain EL, Jr, Raines BT, Fortenbaugh D, Dugas JR, Andrews JR. Long-term outcomes after ulnar collateral ligament reconstruction in competitive baseball players: minimum 10-year follow-up. Am J Sports Med. 2014;42(6):1333–1342. [DOI] [PubMed] [Google Scholar]
- 26. Otoshi K, Kikuchi S, Kato K, et al. Sufficient duration of off-season decreases elbow disorders in elementary school-aged baseball players. J Shoulder Elbow Surg. 2019;28(6):1098–1103. [DOI] [PubMed] [Google Scholar]
- 27. Paletta GA, Jr, Wright RW. The modified docking procedure for elbow ulnar collateral ligament reconstruction: 2-year follow-up in elite throwers. Am J Sports Med. 2006;34(10):1594–1598. [DOI] [PubMed] [Google Scholar]
- 28. Pennock AT, Pytiak A, Stearns P, et al. Preseason assessment of radiographic abnormalities in elbows of Little League Baseball players. J Bone Joint Surg Am. 2016;98(9):761–767. [DOI] [PubMed] [Google Scholar]
- 29. Petty DH, Andrews JR, Fleisig GS, Cain EL. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med. 2004;32(5):1158–1164. [DOI] [PubMed] [Google Scholar]
- 30. Rohrbough JT, Altchek DW, Hyman J, Williams RJ III, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002;30(4):541–548. [DOI] [PubMed] [Google Scholar]
- 31. Smith GR, Altchek DW, Pagnani MJ, Keeley JR. A. muscle-splitting approach to the ulnar collateral ligament of the elbow: neuroanatomy and operative technique. Am J Sports Med. 1996;24(5):575–580. [DOI] [PubMed] [Google Scholar]
- 32. Swindell HW, Trofa DP, Confino J, Sonnenfeld JJ, Alexander FJ, Ahmad CS. Performance in collegiate-level baseball players after elbow ulnar collateral ligament reconstruction. Orthop J Sports Med. 2020;8(4):2325967120913013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Takenaga T, Goto H, Tsuchiya A, et al. Relationship between bilateral humeral retroversion angle and starting baseball age in skeletally mature baseball players—existence of watershed age. J Shoulder Elbow Surg. 2019;28(5):847–853. [DOI] [PubMed] [Google Scholar]
- 34. Takeuchi S, Yoshida M, Sugimoto K, Tsuchiya A, Takenaga T, Goto H. The differences of humeral torsion angle and the glenohumeral rotation angles between young right-handed and left-handed pitchers. J Shoulder Elbow Surg. 2019;28(4):678–684. [DOI] [PubMed] [Google Scholar]
- 35. Thompson WH, Jobe FW, Yocum LA, Pink MM. Ulnar collateral ligament reconstruction in athletes: muscle-splitting approach without transposition of the ulnar nerve. J Shoulder Elbow Surg. 2001;10(2):152–157. [DOI] [PubMed] [Google Scholar]
- 36. Timmerman LA, Andrews JR. Arthroscopic treatment of posttraumatic elbow pain and stiffness. Am J Sports Med. 1994;22(2):230–235. [DOI] [PubMed] [Google Scholar]
- 37. Yoshizawa T, Okamoto Y, Tanaka K, et al. Normal imaging laterality on magnetic resonance imaging of the medial epicondyle of the elbow on the dominant side of adolescent male baseball players. Skeletal Radiol. 2018;47(9):1237–1244. [DOI] [PubMed] [Google Scholar]