Abstract
Background
Coronavirus disease 2019 (COVID-19) has been the most important global issue since December 2019. Although the clinical course of COVID-19 is known to be milder in children than in adults, associated hospitalizations among children have increased since the emergence of contagious severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants and the achievement of a high vaccination rate in adults. Considering these global and domestic situations, we believe that risk stratification in children with COVID-19 is urgently needed for decision making regarding hospitalization priority in children infected with SARS-CoV-2 and vaccination priority against COVID-19.
Methods
This systematic review and meta-analysis was performed by comprehensively searching the PubMed, EMBASE, Scopus and KoreaMed databases through August 25, 2021. The criteria for enrollment were “severe COVID-19” as poor outcomes (intensive care unit admission, invasive mechanical ventilation, and/or death) and underlying comorbidities before SARS-CoV-2 infection.
Results
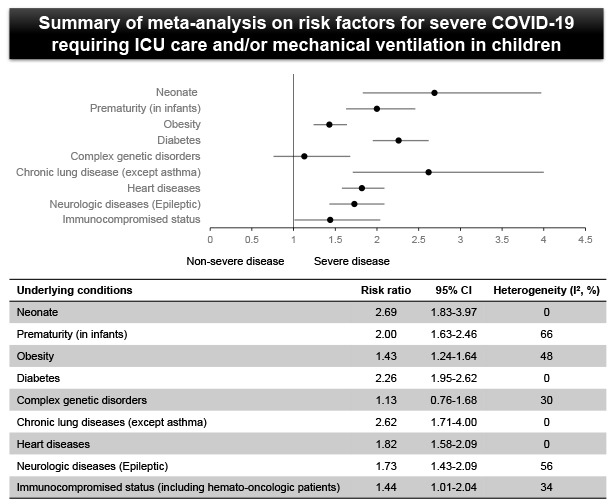
Among 872 screened studies, 17 articles were included in the systematic review, and 10 articles were included in the meta-analysis. Neonate (risk ratio [RR], 2.69; 95% confidence interval [CI], 1.83–3.97), prematurity in young infants (RR, 2.00; 95% CI, 1.63–2.46), obesity (RR, 1.43; 95% CI, 1.24–1.64), diabetes (RR, 2.26; 95% CI, 1.95–2.62), chronic lung disease (RR, 2.62; 95% CI, 1.71–4.00), heart disease (RR, 1.82; 95% CI, 1.58–2.09), neurologic disease (RR, 1.18; 95% CI, 1.05–1.33), and immunocompromised status (RR, 1.44; 95% CI, 1.01–2.04) were significant risk factors for severe COVID-19 in children. In the subgroup analysis, age younger than 3 months (RR, 0.26; 95% CI, 0.11–0.66), asthma (RR, 1.08; 95% CI, 0.98–1.20), and neurodevelopmental disorders (RR, 0.88; 95% CI, 0.75–1.04) were not risk factors for severe COVID-19.
Conclusion
Children with comorbidities such as obesity, diabetes, heart disease, chronic lung diseases other than asthma, seizure disorders, and an immunocompromised status had a high prevalence of severe COVID-19. Neonate and premature infants had a high risk of severe COVID-19. Defining the high-risk group for severe COVID-19 could help to guide hospital admission and priority for vaccination against SARS-CoV-2.
Keywords: COVID-19, Critical Illness, Children, Risk Factor, Meta-Analysis
Graphical Abstract
INTRODUCTION
Coronavirus disease 2019 (COVID-19) has dramatically increased the burden on healthcare worldwide since the initial identification of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in December 2019.1 Despite the global pandemic, children and adolescents have milder clinical presentations and more favorable outcomes than adults.2,3,4,5 However, some children experience a severe clinical course and even were deceased.2,6 Additionally, delayed hyperinflammatory shock conditions, defined as multisystem inflammatory syndrome in children (MIS-C), have been reported and threaten the health of children with COVID-19.7,8
Since July 7, 2021, the 4th epidemic wave of COVID-19 has been ongoing in South Korea. Approximately 2,000 cases are confirmed by the polymerase chain reaction method every day, and most of the patients, including asymptomatic children, are being treated in residential treatment centers or hospitals. Since the end of 2020, home care guidelines have been established mainly for children with asymptomatic or mild COVID-19 and their families, but the degree of implementation is insignificant.9,10 In addition, as in other countries,11 the proportion of children among confirmed COVID-19 cases has been increasing, possibly due to the balloon effect from COVID-19 vaccination in adults and increased circulation of the contagious SARS-CoV-2 delta variant.
In the early COVID-19 pandemic, a high-risk group of children was defined based on the data from other respiratory viral illness. Therefore, it is necessary to define children at high risk of severe COVID-19 based on the accumulated data thus far. Most children who have mild or asymptomatic COVID-19 can be safely managed in their own home. However, it is questionable whether children at risk of developing severe COVID-19 are monitored based on risk assessment in the current clinical field. In addition, Central Disease Control Headquarters of the Republic of Korea recently announced a plan to vaccinate children aged 12–17 years old against COVID-19. Children who have a possibility of progressing to severe COVID-19 should be the priority population for COVID-19 vaccination. Taken together, risk stratification in children is important for identifying high-risk groups for COVID-19, especially under limited healthcare resources. Therefore, we performed a systematic review and meta-analysis to identify children at high risk of severe COVID-19, with a focus on comorbidities and age.
METHODS
Search strategy and study selection
A comprehensive search of the PubMed, EMBASE, Scopus, and KoreaMed databases was performed by two authors (Choi JH and Yun KW) between August 1, 2021, and August 25, 2021. The entry terms were (“risk factor” OR “severe” OR “outcome”) AND (“COVID-19” OR “SARS-CoV-2”) AND (“children” OR “pediatric”). We also performed manual searches of related bibliographies. We first screened the titles and abstracts of articles, and potentially relevant full-text articles were then independently reviewed by two authors (Choi SH and Yun KW) using the following inclusion criteria: 1) the rates of intensive care unit (ICU) admission, invasive mechanical ventilation, and/or death among children with COVID-19; 2) the inclusion of different age groups, particularly neonates and infants younger than 3 months of age; and 3) the prevalence of comorbidities including prematurity, obesity, diabetes, genetic disorders, neurologic disease, cardiac disease, lung disease, hemato-oncologic disease, and immunocompromised status. The following types of studies were excluded: 1) studies with combined COVID-19 and MIS-C results and 2) studies for which the full text was not accessible. No language restrictions were applied.
Data extraction and risk of bias assessment
Data from the included studies were extracted with standardized forms and were independently confirmed by all authors. For each article, the following information was collected: name of the first author; year of publication; study design; study location; study period; sample size; age; number of patients with COVID-19; numbers of patients with ICU admission, mechanical ventilation, and/or death; numbers of patients with specific comorbidities; and characteristics of the population (general, hospitalized, or with confirmed COVID-19).
None of the included studies had randomized controlled designs; therefore, the risk of bias was evaluated by the Risk of Bias Assessment Tool for Nonrandomized Studies (RoBANS).12 The RoBANS contains 6 domains: 1) selection of participants, 2) confounding variables, 3) measurement of exposure, 4) blinding of outcome assessments, 5) incomplete outcome data, and 6) selective outcome reporting. Each item was independently assessed by two reviewers (Choi SH and Choi JH), and disagreements were resolved by an arbitrator (Yun KW).
Data synthesis and statistical analysis
We conducted a meta-analysis to generate estimates of the relative risk of severe COVID-19 in children with specific comorbidities using Review Manager (RevMan) Version 5.4. We defined “severe COVID-19” as a case requiring ICU admission, invasive mechanical ventilation, and/or death. Hemodynamic support was included as “severe COVID-19” in 1 study due to the impossibility of separating it from other outcomes.13 Hospitalization was not included in the severe COVID-19 definition because hospital admission depends on the institutional policy and/or the corresponding physician’s subjective decision. Potential risk factors were limited to young age and underlying comorbidities. From the risk factors investigated in previous original and review articles, we reclassified underlying conditions into eight categories: young age (neonate or infant), prematurity, obesity, diabetes, complex genetic disorder, chronic lung disease (including asthma), heart disease (including congenital heart disease [CHD]), neurologic disease (including epilepsy and neurodevelopmental disorders), and immunocompromised status (including primary/secondary immune deficiency and hemato-oncologic disorders).14,15 We used a random-effects model for analysis if there was significant heterogeneity between studies. Meta-analysis was performed using a fixed-effect model if there was no heterogeneity between studies. To assess statistical heterogeneity, we used the I2 statistic, which is expressed as the percentage of total variation across studies. The impact of comorbidities is expressed by the risk ratio (RR) and 95% confidence interval (CI). Subgroup analyses were performed for some comorbidities if needed and when possible.
Ethics statement
Ethical approval was not necessary because this study was performed using data from published studies.
RESULTS
Literature search and study characteristics
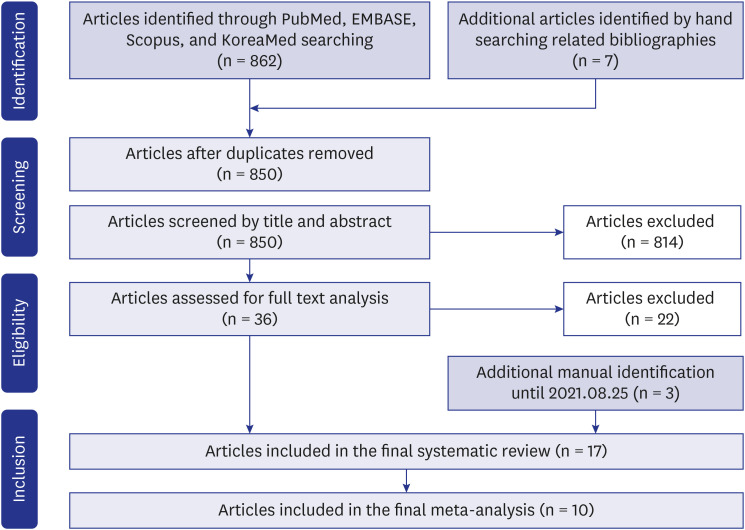
A total of 862 eligible articles were identified through initial screening, and 10 articles were further identified manually. During the review process, 855 of these articles were excluded; finally, 17 articles were included in the systematic review, and 10 articles were included in the meta-analysis (Fig. 1). The characteristics of the included studies and the corresponding risk factors are summarized in Table 1, and more detailed characteristics of the included studies are shown in Supplementary Tables 1, 2, 3. The results of the quality assessment of the individual studies are demonstrated in Supplementary Fig. 1.
Fig. 1. Flow diagram of the literature search.
Table 1. Characteristics and details of the included studies.
| Studies | Study design | Location | Sample sizeb | Risk factors included | Analysis in this study | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | P | O | D | L | C | N | G | I | H | ||||||||||||||
| Zachariah et al. (2020) 17 | R/CS | USA | 50 | SR & MA | |||||||||||||||||||
| Chao et al. (2020) 26 | R/CS | USA | 67 | SR & MA | |||||||||||||||||||
| Swann et al. (2020) 21 | P/CO | UK | 580 | SR & MA | |||||||||||||||||||
| Götzinger et al. (2020) 20 | A/CO | Europe | 582 | SR & MA | |||||||||||||||||||
| Bellino et al. (2020) 16 | R/CO | Italy | 3,836 | SR & MA | |||||||||||||||||||
| Fisler et al. (2020) 31 | R/CO | USA | 77 | SR & MA | |||||||||||||||||||
| Ouldali et al. (2021) 13 | P/CS | France | 397 | SR & MA | |||||||||||||||||||
| Graff et al. (2021) 18 | R/CS | USA | 454 | SR & MA | |||||||||||||||||||
| Kompaniyets et al. (2021) 24 | R/CS | USA | 43,465 | SR & MA | |||||||||||||||||||
| Verma et al. (2021) 27 | R/CO | USA | 82 | SR & MA | |||||||||||||||||||
| Mithal et al. (2020) 19 | CC | USA | 18 | SR | |||||||||||||||||||
| Kanburoglu et al. (2020) 22 | P/CO | Turkey | 37 | SR | |||||||||||||||||||
| Wardell et al. (2020) 23 | CC | USA | 4 | SR | |||||||||||||||||||
| Cardona-Hernandez et al. (2021) 25 | R/CO | Multinationala | 16 | SR | |||||||||||||||||||
| Dannan et al. (2020) 28 | CC | UAE | 5 | SR | |||||||||||||||||||
| Madhusoodhan et al. (2021) 29 | R/CS | USA | 98 | SR | |||||||||||||||||||
| Barhoom et al. (2021) 30 | CC | Iran | 4 | SR | |||||||||||||||||||
A = age, P = prematurity, O = obesity, D = diabetes, L = chronic lung disease, C = cardiac disease, N = neurologic disease, G = complex genetic disease, I = immune-compromising disorder and/or immunosuppressive medication, H = hemato-oncologic disease, R/CS = retrospective cross-sectional, P/CO = prospective cohort, A/CO = ambispective cohort, R/CO = retrospective cohort, P/CS = prospective cross-sectional, CC = case series, SR = systematic review, MA = meta-analysis.
aChina, Italy, Spain, and USA; bNumber of enrolled children.
Systematic review and meta-analyses according to comorbidity
Young age
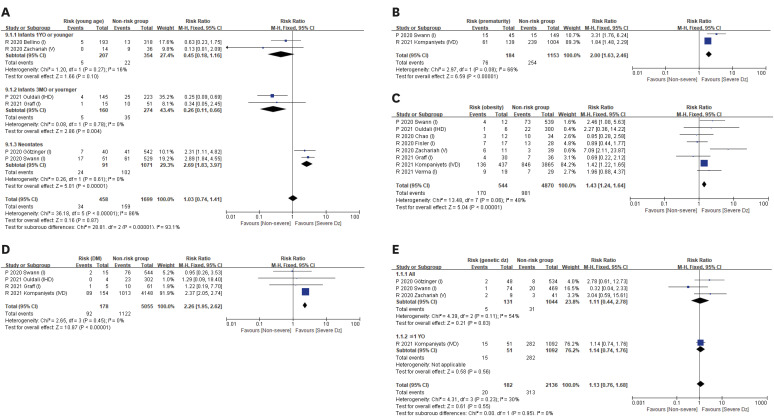
The impact of young age on the occurrence of severe COVID-19 was analyzed in 9 studies (Table 1). Two retrospective studies analyzing infants younger than 1 and 2 years of age showed a lower prevalence of severe COVID-19 in this age group than in other age groups, although the difference was nonsignificant.16,17 Additionally, in two other studies analyzing infants younger than 3 months of age, the prevalence of ICU admission was lower in this group than in the other age groups (RR, 0.26; 95% CI, 0.11–0.66).13,18 One case series report showed that no children required ICU care among 18 infants younger than 3 months of age.19 However, two multicenter studies in Europe showed that a higher prevalence of neonates required ICU admission than older patients, with odds ratios of 3.21 (95% CI, 1.36–7.66) and 5.06 (95% CI, 1.72–14.87), respectively.20,21 Two case series also reported that neonates had a high risk of severe COVID-19.22,23 Due to differences in outcomes according to age group classification in the included studies, young age did not seem to have an impact on the severity of COVID-19 according to the pooled meta-analysis (RR, 1.03; 95% CI, 0.74–1.41), but the subgroup analysis showed that neonates probably had an increased risk for severe COVID-19 compared with others (RR, 2.69; 95% CI, 1.83–3.97) (Fig. 2A).
Fig. 2. Meta-analysis of the impacts of 5 comorbidities on the severity of COVID-19 in children. (A) the impact of age. (B) the impact of prematurity. (C) the impact of obesity. (D) the impact of diabetes. (E) the impact of complex genetic disorders.
COVID-19 = coronavirus disease 2019, CI = confidence interval, RR = risk ratio, DM = diabetes mellitus, P = prospective study, R = retrospective study, I = intensive care unit care, V = mechanical ventilator support, D = death, H = hemodynamic support.
Prematurity
In two of the included studies, the effect of prematurity was evaluated among children younger than 1 and 2 years of age. In nationwide studies in the UK, the prevalence of ICU admission in premature and full-term infants with COVID-19 was 19.2% and 6.0%, respectively (P = 0.001).21 The prevalence of poor outcomes in premature COVID-19 infants was higher than that in full-term infants in the USA (RR, 1.84; 95% CI, 1.48–2.29).24 The impact of prematurity on severity in the included studies was evaluated among children younger than 1 year of age. In total, the risk of severe COVID-19 was higher in premature infants than in full-term infants (RR, 2.00; 95% CI, 1.63–2.46) (Fig. 2B).
Obesity
Analyses of the impact of obesity on COVID-19 severity were performed in 8 studies (Table 1). At the start of the pandemic in the UK, a prospective study including 580 children showed that obesity was related to prevalent ICU admission (RR, 2.46; 95% CI, 1.08–5.63).21 In a recent national surveillance study in the USA including 4,302 hospitalized children, obese patients with COVID-19 were at higher risk of severe clinical courses, including ICU admission, respiratory support, and death, than nonobese patients (adjusted RR [aRR], 1.42; 95% CI, 1.22–1.66).24 According to the analysis of the 8 included studies, obesity was found to be a risk factor for severe disease in COVID-19 patients (RR, 1.43; 95% CI, 1.24–1.64) (Fig. 2C).
Diabetes
Diabetes in relation to the severity of COVID-19 was analyzed in 4 studies. In a large retrospective study in the USA, children with type 1 diabetes who were hospitalized for COVID-19 developed more severe disease than nondiabetic children (aRR, 2.38; 95% CI, 2.06–2.76).24 However, two small studies showed that diabetic children with COVID-19 were not at high risk of ICU admission.18,21 In our meta-analysis, children with diabetes had a higher risk of severe COVID-19 than those without diabetes (RR, 2.26; 95% CI, 1.95–2.62) (Fig. 2D). Although excluded from the meta-analysis, a cohort study including 17,110 children with type 1 diabetes in 4 countries (China, Italy, Spain, and the USA) reported that children with severe COVID-19 were the only children to be admitted to the ICU to manage diabetic ketoacidosis through August 2020.25
Complex genetic disorders
Among the included studies, analyses of comorbidities, such as complex genetic disorders, on the severity of COVID-19 were performed in 4 studies. In these analyses, comorbidities such as congenital anomalies, chromosomal abnormalities, and genetic disorders were included. In total, genetic anomalies were not related to an increased risk of severe disease in children with COVID-19 (RR, 1.13; 95% CI, 0.76–1.68) (Fig. 2E).
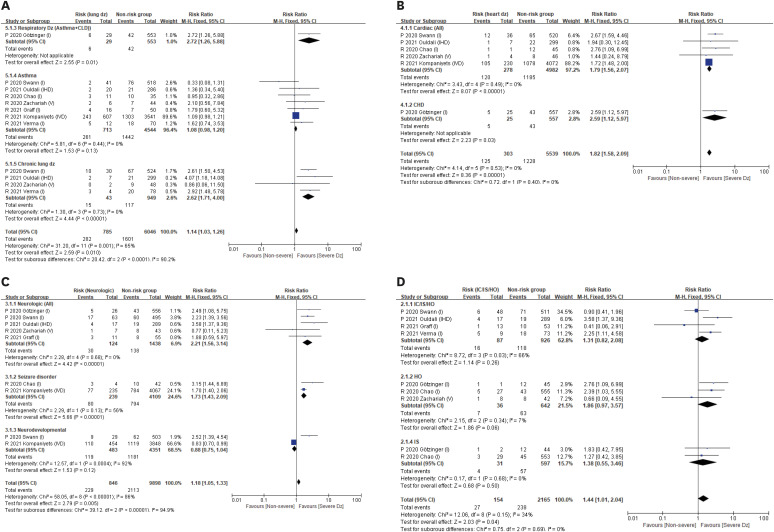
Chronic lung diseases and asthma
The impacts of chronic lung diseases, including asthma, on severe COVID-19 were analyzed in 8 studies. In total, the risk for severe COVID-19 was slightly increased in children with chronic lung diseases, including asthma (RR, 1.14; 95% CI, 1.03–1.26). However, in the subgroup analyses, children with chronic lung diseases other than asthma developed severe COVID-19 (RR, 2.62; 95% CI, 1.71–4.00), whereas those with asthma did not (RR, 1.08; 95% CI, 0.98–1.20) (Fig. 3A). Several studies have reported that the presence of asthma is not related to ICU admission for the management of COVID-19.21,26,27
Fig. 3. Meta-analysis of the impacts of 4 comorbidities on the severity of COVID-19 in children. (A) The impact of chronic lung disease and asthma. (B) The impact of heart disease. (C) The impact of neurologic disease. (D) The impact of immunocompromised status.
COVID-19 = coronavirus disease 2019, CI = confidence interval, RR = risk ratio, DM = diabetes mellitus, P = prospective study, R = retrospective study, I = intensive care unit care, V = mechanical ventilator support, D = death, H = hemodynamic support, CLD = chronic lung disease, CHD = congenital heart disease, IC = immunocompromising status, IS = immunosuppressant drug use, HO = hemato-oncologic disease.
Heart disease
Six studies that analyzed heart disease in relation to COVID-19 were included. In a prospective study in the UK, 15.4% (12/78) of children with any heart disease were admitted to the ICU after a diagnosis of COVID-19, and the prevalence was higher than those without heart disease (P = 0.002).21 Another study in Europe showed that 10.4% of children with CHD were admitted to the ICU, and the RR was 2.59 (95% CI, 1.12–5.97).20 In total, the prevalence of severe COVID-19 was significantly higher in children with cardiac disease, including CHD, than in those without cardiac disease (RR, 1.82; 95% CI, 1.58–2.09) (Fig. 3B).
Neurologic diseases
The impacts of neurologic diseases were analyzed in 7 studies. In the subgroup analysis of children with seizure disorder, the prevalence of severe COVID-19 was significantly higher in children with seizure disorder than in those without (RR, 1.73; 95% CI, 1.43–2.09) (Fig. 3D). Only neurodevelopmental disorders showed no effect on the risk of severe clinical illness in children with COVID-19 (RR, 0.88; 95% CI, 0.75–1.04).21,24 When total neurologic disorders were analyzed, the presence of a neurologic disorder had a significant relationship with severe COVID-19 (RR, 1.18; 95% CI, 1.05–1.33) (Fig. 3C). In conclusion, children with neurologic diseases, especially seizure disorders but not neurodevelopmental disorders, likely have a high risk of severe COVID-19.
Immunocompromised status (immunodeficiency, immunosuppressive drug use, and/or a hemato-oncologic disorder)
Immunocompromised hosts included children who were undergoing chemotherapy, used immunosuppressant drugs, or had immunodeficiency or a hemato-oncologic disorder. In our meta-analysis, the risk of severe COVID-19 was related to immunocompromised status (RR, 1.44; 95% CI, 1.01–2.04) (Fig. 3D). Among children with immunocompromised status, subgroup analysis was performed by dividing 3 groups: mixed group without detailed distinction, hemato-oncologic disorder group, and immunosuppressant drug user group. Contrary to the overall results, all detailed subgroup analyses showed that each immunocompromised status did not have increased risks of severe COVID-19. (Fig. 3D). Although a case series reported that all various immunocompromised patients had only mild symptoms,28 17.3% of children with oncology patients required ICU care in a cross-sectional study,29 and three of four pediatric hematopoietic stem cell transplantation recipients developed severe COVID-19 in a case series.30
DISCUSSION
This study investigated morbidities related to the severity of COVID-19 in children through a systematic review and meta-analysis to provide updated evidence of high-risk pediatric groups requiring COVID-19 vaccination priority and hospitalization when infected with SARS-CoV-2. The analysis included data from 17 studies, including several case series. The results of the meta-analysis showed that age younger than 1 month, prematurity in young infants, obesity, diabetes, chronic lung disease other than asthma, heart disease, seizure disorder, and immunocompromised status affected the severity of COVID-19 in children.
Central Disease Control Headquarters of the Republic of Korea defines infants younger than 3 months as a high-risk group for COVID-19.10 However, our subgroup analysis of infants younger than 3 months had low risks of severe COVID-19 (RR, 0.26; 95% CI, 0.11–0.66). Only neonates younger than 1 month of age had a high risk of severe COVID-19 (RR, 2.69; 95% CI, 1.83–3.97). Although neonates tended to be managed in the ICU regardless of clinical severity for close monitoring in the early COVID-19 pandemic, we recommend that the high-risk group should be reclassified from infants younger than 3 months to neonates based on this analysis.
In two selected studies, the impacts of prematurity were analyzed only in limited age groups, such as children younger than 1 year and 2 years.21,24 Each study revealed that prematurity was a risk factor for severe COVID-19 in the 1-year (RR, 3.31; 95% CI, 1.76–6.24) and 2-year (RR, 1.84; 95% CI, 1.48–2.29) groups. It is already well known that preterm infants have a higher prevalence of ICU admissions for respiratory illness than full-term infants.32,33 Although prematurity among children older than 2 years was not analyzed, the high impact of prematurity on severe COVID-19 identified in this study suggests that clinicians manage preterm infants with COVID-19 more carefully.
Obesity and diabetes are known to be risk factors for severe COVID-19-associated illness among adults.34,35 The high-risk tendency in obese populations has been explained by several mechanisms, such as immune dysfunction, altered pulmonary physiology, and high angiotensin converting enzyme 2 (ACE2) expression.36 Considering the risk of obesity, obese children with COVID-19 need close monitoring for clinical deterioration or progression to acute respiratory distress syndrome. Additionally, in obese children, lifestyle habit control and prevention through COVID-19 vaccination were emphasized.
Diabetes is a metabolic disorder resulting from impaired insulin secretion or insulin resistance and is known to be associated with a higher risk of acquiring infectious diseases. Insulin resistance seems to promote the synthesis of end-glycosylation products and stimulate proinflammatory cytokines and oxidative stress, resulting in a higher likelihood of infection and worse prognosis.37 Diabetes and hyperglycemia have been proven to be independent prognostic factors of morbidity and fatality in patients infected with SARS-CoV and MERS-CoV.38,39 In adults, diabetes has emerged as a major risk factor that increases severe illness and mortality in COVID-19 patients.40 The relationship between diabetes and severe COVID-19 was explained by overexpression of angiotensin converting enzyme 2.41 Although diabetes was identified as a risk factor in this study, this was mainly due to one large retrospective study.25 Interestingly other studies included in the analysis did not show a significant relationship between diabetes and severe COVID-19. This result was explained by many theories, such as the low incidence of COVID-19 in children due to strict quarantine policy, the relatively high controlled diabetes in children compared to adults, and the high proportion of type 1 diabetes in children. Diabetic children with COVID-19 should be monitored for future research.
Our analysis of heart disease as a risk factor contributing to severe COVID-19 included 652 COVID-19 children with heart disease, including CHD. A small number of patients with heart disease were included because active quarantine measures and a relatively short pandemic period prevented many children with heart disease from becoming infected with COVID-19. Respiratory syncytial virus (RSV) infection is an important risk factor for morbidity and mortality in children with CHD. A recent systematic review showed that a case fatality rate of up to 3% was associated with RSV infection in children with CHD.42 The persistent COVID-19 pandemic could have an effect similar to that of RSV in heart disease patients. From this point of view, children with heart disease should be considered a priority of COVID-19 vaccination. However, the increased prevalence of myocarditis after COVID-19 vaccination with the mRNA vaccine in adolescents aged 12–17 years should be considered in heart disease patients carefully.
Asthma, neurodevelopmental delay and complex genetic disorders, such as Down syndrome, have been considered risk factors for a severe clinical course in previous studies on endemic respiratory viruses.43,44 However, these comorbidities, which can be considered risk factors, had no effect on the risk of severe COVID-19 in our analysis. Asthma was considered one of the risk factors for severe COVID-19 during the early pandemic. However, an initial systematic review reported that the role of asthma as a risk factor in children with COVID-19 was unclear.45 In subsequent studies in adults, asthma was found to be a nonsignificant risk factor for poor outcomes in COVID-19 patients.46,47 All 6 studies in our analysis showed that children with asthma had no poor outcomes after COVID-19. The clinical association between asthma and severe COVID-19 has not been fully established, and type 2 airway inflammation and downregulation of ACE2 receptors in asthmatic patients could affect these results. Neurodevelopmental delay and complex genetic disorders require attention to interpretation because these groups consisted of heterogeneous diseases. Additionally, we cannot overlook the low incidence of COVID-19 in children due to strict quarantines, such as school closures. When there is a chance of SARS-CoV-2 infection after the normalization of daily life, children with these underlying comorbidities should be monitored carefully.
Generally, immunocompromised status was defined as a risk factor for severe respiratory viral disease in any age group. However, each subgroup (immunosuppressant drug use, immunodeficiency, and hemato-oncologic disease) analysis showed that all detailed statuses were not significant factors for severe COVID-19 in our study (Fig. 3C). This may be because immunocompromised status included heterogeneous disease groups. Additionally, most studies on the impact of hemato-oncologic disease have shown that the outcome of severe COVID-19 is ICU admission. ICU admission could have increased to monitor the clinical status due to hemato-oncologic disease itself, such as young age; therefore, data about respiratory support or mortality should be followed.
Among individuals with complex genetic disorders, individuals with Down syndrome receive slightly more attention because they have a longer life expectancy than individuals with other genetic disorders and are known to be at high risk of respiratory tract infections. In adults, Down syndrome patients with COVID-19 had more severe disease than those with other medical conditions.48 Several case reports emphasized careful monitoring and reported that children with Down syndrome developed severe COVID-19.49,50 We could not locate well-designed research focusing on children with Down syndrome. However, children with Down syndrome had comorbidities, such as cardiopathies, immunodeficiency, obesity, and diabetes, that were found to be related to severe COVID-19 in our analysis. Accordingly, it is necessary to monitor children with Down syndrome for COVID-19 more carefully.
Although excluded from our high-risk group analysis, MIS-C should be considered when analyzing the seriousness of COVID-19. A recent study analyzing 2,818 MIS-C cases in individuals less than 21 years of age reported that the odds of death were significant in persons aged 16–20 years (adjusted odds ratio [aOR], 6.8; 95% CI, 2.7–17.1), with neurologic disorders (aOR, 5.1; 95% CI, 1.9–14.1) and noncardiac congenital anomalies (aOR, 6.5; 95% CI, 2.6–16.0).51 However, MIS-C should be distinguished from severe COVID-19 in our analysis due to the characteristics of showing the clinical manifestations for a relatively long time after SARS-CoV-2 infection.
This study has some limitations. The nature of the included studies and the definition of comorbidities in the studies were heterogeneous. In several studies, patients in their early twenties, such as 21 years old, were included; however, we could not exclude those data because studies of only children under 18 years old are scarce. In most of the included studies, the number of enrolled children was so small, and there were only 4 studies with more than 500 subjects. In addition, the criteria for ICU admission might be different depending on the environment of each hospital. Finally, we could not evaluate the effect of combined comorbidities due to difficulty in detailed classification. Last, the current study was based on the limited number of published studies thus far regarding the risk factors for severe COVID-19 in children; therefore, this is a living systematic review. However, this systematic review and meta-analysis was strengthened by a comprehensive literature search and detailed classification of underlying comorbidities.
In conclusion, we recommend that children with comorbidities such as obesity, diabetes, heart disease, chronic lung diseases other than asthma, seizure disorder, and an immunocompromised status be classified as a high-risk population who should be considered for hospitalization when infected with SARS-CoV-2 and a priority population for COVID-19 vaccination. Additionally, neonates and preterm infants younger than 1 year of age should be included in the high-risk group for COVID-19 and receive active monitoring and management when infected. Children with underlying diseases determined to be nonsignificant risk factors in our analysis could be considered high-risk when their underlying conditions are unstable; therefore, they must be monitored carefully. Recently, several severe COVID-19 in Korean children were reported.52 We hope that risk stratification in children with COVID-19 can help clinicians manage patients and policymakers establish priority populations for COVID-19 vaccination.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Yun KW.
- Data curation: Choi JH, Choi SH.
- Formal analysis: Choi JH, Choi SH.
- Investigation: Choi JH, Choi SH, Yun KW.
- Methodology: Yun KW.
- Validation: Yun KW.
- Writing - original draft: Choi JH.
- Writing - review & editing: Choi SH, Yun KW.
SUPPLEMENTARY MATERIALS
Characteristics of the included studies in meta-analysis
Comorbidities and risk factors associated with severe COVID-19 in the studies including meta-analysis
Characteristics of the included studies in systematic reviews (excluding studies in meta-analysis)
Risk of bias of included studies in this meta-analysis.
References
- 1.World Health Organization. WHO coronavirus (COVID-19) dashboard. [Updated 2021]. [Accessed September 30, 2021]. https://covid19.who.int/
- 2.American Academy of Pediatrics. Children and COVID-19: state-level data report. [Updated 2021]. [Accessed September 30, 2021]. https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/
- 3.Han MS, Choi EH, Chang SH, Jin BL, Lee EJ, Kim BN, et al. Clinical characteristics and viral RNA detection in children with coronavirus disease 2019 in the Republic of Korea. JAMA Pediatr. 2021;175(1):73–80. doi: 10.1001/jamapediatrics.2020.3988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145(6):e20200702. doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 5.Borrelli M, Corcione A, Castellano F, Fiori Nastro F, Santamaria F. Coronavirus disease 2019 in children. Front Pediatr. 2021;9:668484. doi: 10.3389/fped.2021.668484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shekerdemian LS, Mahmood NR, Wolfe KK, Riggs BJ, Ross CE, McKiernan CA, et al. Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 2020;174(9):868–873. doi: 10.1001/jamapediatrics.2020.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Radia T, Williams N, Agrawal P, Harman K, Weale J, Cook J, et al. Multi-system inflammatory syndrome in children & adolescents (MIS-C): a systematic review of clinical features and presentation. Paediatr Respir Rev. 2021;38:51–57. doi: 10.1016/j.prrv.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toubiana J, Poirault C, Corsia A, Bajolle F, Fourgeaud J, Angoulvant F, et al. Kawasaki-like multisystem inflammatory syndrome in children during the COVID-19 pandemic in Paris, France: prospective observational study. BMJ. 2020;369:m2094. doi: 10.1136/bmj.m2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Korean Disease Control and Prevention Agency. A guidelines for COVID-19 self-treatment in children. [Updated 2021]. [Accessed September 30, 2021]. http://ncov.mohw.go.kr/shBoardView.do?brdId=2&brdGubun=28&ncvContSeq=4540 .
- 10.Korean Disease Control and Prevention Agency. A guideline for COVID-19 self-treatment in children version 3-1. [Updated 2021]. [Accessed January 8, 2022]. http://ncov.mohw.go.kr/shBoardView.do?brdId=2&brdGubun=28&ncvContSeq=4627 .
- 11.Delahoy MJ, Ujamaa D, Whitaker M, O’Halloran A, Anglin O, Burns E, et al. Hospitalizations associated with COVID-19 among children and adolescents - COVID-NET, 14 States, March 1, 2020-August 14, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(36):1255–1260. doi: 10.15585/mmwr.mm7036e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66(4):408–414. doi: 10.1016/j.jclinepi.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 13.Ouldali N, Yang DD, Madhi F, Levy M, Gaschignard J, Craiu I, et al. Factors associated with severe SARS-CoV-2 infection. Pediatrics. 2021;147(3):e2020023432. doi: 10.1542/peds.2020-023432. [DOI] [PubMed] [Google Scholar]
- 14.Tsabouri S, Makis A, Kosmeri C, Siomou E. Risk factors for severity in children with coronavirus disease 2019: a comprehensive literature review. Pediatr Clin North Am. 2021;68(1):321–338. doi: 10.1016/j.pcl.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams N, Radia T, Harman K, Agrawal P, Cook J, Gupta A. COVID-19 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review of critically unwell children and the association with underlying comorbidities. Eur J Pediatr. 2021;180(3):689–697. doi: 10.1007/s00431-020-03801-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bellino S, Punzo O, Rota MC, Del Manso M, Urdiales AM, Andrianou X, et al. COVID-19 disease severity risk factors for pediatric patients in Italy. Pediatrics. 2020;146(4):e2020009399. doi: 10.1542/peds.2020-009399. [DOI] [PubMed] [Google Scholar]
- 17.Zachariah P, Johnson CL, Halabi KC, Ahn D, Sen AI, Fischer A, et al. Epidemiology, clinical features, and disease severity in patients with coronavirus disease 2019 (COVID-19) in a children’s hospital in New York city, New York. JAMA Pediatr. 2020;174(10):e202430. doi: 10.1001/jamapediatrics.2020.2430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Graff K, Smith C, Silveira L, Jung S, Curran-Hays S, Jarjour J, et al. Risk factors for severe COVID-19 in children. Pediatr Infect Dis J. 2021;40(4):e137–e145. doi: 10.1097/INF.0000000000003043. [DOI] [PubMed] [Google Scholar]
- 19.Mithal LB, Machut KZ, Muller WJ, Kociolek LK. SARS-CoV-2 infection in infants less than 90 days old. J Pediatr. 2020;224:150–152. doi: 10.1016/j.jpeds.2020.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4(9):653–661. doi: 10.1016/S2352-4642(20)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Swann OV, Holden KA, Turtle L, Pollock L, Fairfield CJ, Drake TM, et al. Clinical characteristics of children and young people admitted to hospital with COVID-19 in United Kingdom: prospective multicentre observational cohort study. BMJ. 2020;370:m3249. doi: 10.1136/bmj.m3249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kanburoglu MK, Tayman C, Oncel MY, Akin IM, Can E, Demir N, et al. A multicentered study on epidemiologic and clinical characteristics of 37 neonates with community-acquired COVID-19. Pediatr Infect Dis J. 2020;39(10):e297–e302. doi: 10.1097/INF.0000000000002862. [DOI] [PubMed] [Google Scholar]
- 23.Wardell H, Campbell JI, VanderPluym C, Dixit A. Severe acute respiratory syndrome coronavirus 2 infection in febrile neonates. J Pediatric Infect Dis Soc. 2020;9(5):630–635. doi: 10.1093/jpids/piaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kompaniyets L, Agathis NT, Nelson JM, Preston LE, Ko JY, Belay B, et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw Open. 2021;4(6):e2111182. doi: 10.1001/jamanetworkopen.2021.11182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cardona-Hernandez R, Cherubini V, Iafusco D, Schiaffini R, Luo X, Maahs DM. Children and youth with diabetes are not at increased risk for hospitalization due to COVID-19. Pediatr Diabetes. 2021;22(2):202–206. doi: 10.1111/pedi.13158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chao JY, Derespina KR, Herold BC, Goldman DL, Aldrich M, Weingarten J, et al. Clinical characteristics and outcomes of hospitalized and critically ill children and adolescents with coronavirus disease 2019 at a tertiary care medical center in New York city. J Pediatr. 2020;223:14–19.e2. doi: 10.1016/j.jpeds.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verma S, Lumba R, Dapul HM, Gold-von Simson G, Phoon CK, Lighter JL, et al. Characteristics of hospitalized children with SARS-CoV-2 in the New York city metropolitan area. Hosp Pediatr. 2021;11(1):71–78. doi: 10.1542/hpeds.2020-001917. [DOI] [PubMed] [Google Scholar]
- 28.El Dannan H, Al Hassani M, Ramsi M. Clinical course of COVID-19 among immunocompromised children: a clinical case series. BMJ Case Rep. 2020;13(10):e237804. doi: 10.1136/bcr-2020-237804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Madhusoodhan PP, Pierro J, Musante J, Kothari P, Gampel B, Appel B, et al. Characterization of COVID-19 disease in pediatric oncology patients: The New York-New Jersey regional experience. Pediatr Blood Cancer. 2021;68(3):e28843. doi: 10.1002/pbc.28843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barhoom D, Mohseni R, Hamidieh AA, Mohammadpour M, Sharifzadeh M, Navaeian A, et al. Clinical effects of COVID-19 on hematopoietic stem cell transplant outcomes in pediatric patients. Exp Clin Transplant. 2021;19(5):501–507. doi: 10.6002/ect.2020.0518. [DOI] [PubMed] [Google Scholar]
- 31.Fisler G, Izard SM, Shah S, Lewis D, Kainth MK, Hagmann SHF, et al. Characteristics and risk factors associated with critical illness in pediatric COVID-19. Ann Intensive Care. 2020;10(1):171. doi: 10.1186/s13613-020-00790-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tomashek KM, Shapiro-Mendoza CK, Davidoff MJ, Petrini JR. Differences in mortality between late-preterm and term singleton infants in the United States, 1995-2002. J Pediatr. 2007;151(5):450–456. doi: 10.1016/j.jpeds.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 33.Gunville CF, Sontag MK, Stratton KA, Ranade DJ, Abman SH, Mourani PM. Scope and impact of early and late preterm infants admitted to the PICU with respiratory illness. J Pediatr. 2010;157(2):209–214.e1. doi: 10.1016/j.jpeds.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wu ZH, Tang Y, Cheng Q. Diabetes increases the mortality of patients with COVID-19: a meta-analysis. Acta Diabetol. 2021;58(2):139–144. doi: 10.1007/s00592-020-01546-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kompaniyets L, Goodman AB, Belay B, Freedman DS, Sucosky MS, Lange SJ, et al. Body mass index and risk for COVID-19 related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March - December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(10):355–361. doi: 10.15585/mmwr.mm7010e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou Y, Chi J, Lv W, Wang Y. Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (COVID-19) Diabetes Metab Res Rev. 2021;37(2):e3377. doi: 10.1002/dmrr.3377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Knapp S. Diabetes and infection: is there a link?--A mini-review. Gerontology. 2013;59(2):99–104. doi: 10.1159/000345107. [DOI] [PubMed] [Google Scholar]
- 38.Yang JK, Feng Y, Yuan MY, Yuan SY, Fu HJ, Wu BY, et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med. 2006;23(6):623–628. doi: 10.1111/j.1464-5491.2006.01861.x. [DOI] [PubMed] [Google Scholar]
- 39.Banik GR, Alqahtani AS, Booy R, Rashid H. Risk factors for severity and mortality in patients with MERS-CoV: analysis of publicly available data from Saudi Arabia. Virol Sin. 2016;31(1):81–84. doi: 10.1007/s12250-015-3679-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sarkar S, Das D, Borsingh Wann S, Kalita J, Manna P. Is diabetes mellitus a wrongdoer to COVID-19 severity? Diabetes Res Clin Pract. 2021;178:108936. doi: 10.1016/j.diabres.2021.108936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Checchia PA, Paes B, Bont L, Manzoni P, Simões EA, Fauroux B, et al. Defining the risk and associated morbidity and mortality of severe respiratory syncytial virus infection among infants with congenital heart disease. Infect Dis Ther. 2017;6(1):37–56. doi: 10.1007/s40121-016-0142-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Galleguillos C, Galleguillos B, Larios G, Menchaca G, Bont L, Castro-Rodriguez JA. Down’s syndrome is a risk factor for severe lower respiratory tract infection due to respiratory syncytial virus. Acta Paediatr. 2016;105(11):e531–e535. doi: 10.1111/apa.13552. [DOI] [PubMed] [Google Scholar]
- 44.Pham H, Thompson J, Wurzel D, Duke T. Ten years of severe respiratory syncytial virus infections in a tertiary paediatric intensive care unit. J Paediatr Child Health. 2020;56(1):61–67. doi: 10.1111/jpc.14491. [DOI] [PubMed] [Google Scholar]
- 45.Castro-Rodriguez JA, Forno E. Asthma and COVID-19 in children: a systematic review and call for data. Pediatr Pulmonol. 2020;55(9):2412–2418. doi: 10.1002/ppul.24909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lovinsky-Desir S, Deshpande DR, De A, Murray L, Stingone JA, Chan A, et al. Asthma among hospitalized patients with COVID-19 and related outcomes. J Allergy Clin Immunol. 2020;146(5):1027–1034.e4. doi: 10.1016/j.jaci.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee SC, Son KJ, Han CH, Jung JY, Park SC. Impact of comorbid asthma on severity of coronavirus disease (COVID-19) Sci Rep. 2020;10(1):21805. doi: 10.1038/s41598-020-77791-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Malle L, Gao C, Hur C, Truong HQ, Bouvier NM, Percha B, et al. Individuals with Down syndrome hospitalized with COVID-19 have more severe disease. Genet Med. 2021;23(3):576–580. doi: 10.1038/s41436-020-01004-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Newman AM, Jhaveri R, Patel AB, Tan TQ, Toia JM, Arshad M. Trisomy 21 and coronavirus disease 2019 in pediatric patients. J Pediatr. 2021;228:294–296. doi: 10.1016/j.jpeds.2020.08.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kantar A, Mazza A, Bonanomi E, Odoni M, Seminara M, Verde ID, et al. COVID-19 and children with Down syndrome: is there any real reason to worry? Two case reports with severe course. BMC Pediatr. 2020;20(1):561. doi: 10.1186/s12887-020-02471-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bowen A, Miller AD, Zambrano LD, Wu MJ, Oster ME, Godfred-Cato S, et al. Demographic and clinical factors associated with death among persons <21 years old with multisystem inflammatory syndrome in children-United States, February 2020-March 2021. Open Forum Infect Dis. 2021;8(8):ofab388. doi: 10.1093/ofid/ofab388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee H, Choi S, Park JY, Jo DS, Choi UY, Lee H, et al. Analysis of critical COVID-19 cases among children in Korea. J Korean Med Sci. 2022;37(1):e13. doi: 10.3346/jkms.2022.37.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Characteristics of the included studies in meta-analysis
Comorbidities and risk factors associated with severe COVID-19 in the studies including meta-analysis
Characteristics of the included studies in systematic reviews (excluding studies in meta-analysis)
Risk of bias of included studies in this meta-analysis.