Version Changes
Revised. Amendments from Version 1
The article was updated and revised based on the reviewer’s comments. We have included references to support the previous statement regarding the virus's origin. We used one of the most comprehensive and reliable peer-reviewed scientific articles we could find. Similarly, we also updated in-text citations to support our earlier claim of the mutation of the virus. Other significant revisions include relocating some of the earlier statements to complement our claims better. For example, we placed QGIS right next to ESRI ArcGIS as both are GIS-based platforms. Previously QGIS was placed with RStudio as both are open-source software. In addition, we updated our discussion section to include the use of epidemiological models to forecast the spread of the virus within a geographic context. Lastly, we emphasized the data management practices and why future syntheses should investigate the data management strategies of human-based studies and emphasize ethical practices.
Abstract
Background: Geographic information science (GIS) has established itself as a distinct domain and incredibly useful whenever the research is related to geography, space, and other spatio-temporal dimensions. However, the scientific landscape on the integration of GIS in COVID-related studies is largely unknown. In this systematic review, we assessed the current evidence on the implementation of GIS and other geospatial tools in the COVID-19 pandemic.
Methods: We systematically retrieved and reviewed 79 research articles that either directly used GIS or other geospatial tools as part of their analysis. We grouped the identified papers under six broader thematic groups based on the objectives and research questions of the study- environmental, socio-economic, and cultural, public health, spatial transmission, computer-aided modeling, and data mining.
Results: The interdisciplinary nature of how geographic and spatial analysis was used in COVID-19 research was notable among the reviewed papers. Geospatial techniques, especially WebGIS, have even been widely used to visualize the data on a map and were critical to informing the public regarding the spread of the virus, especially during the early days of the pandemic. This review not only provided an overarching view on how GIS has been used in COVID-19 research so far but also concluded that geospatial analysis and technologies could be used in future public health emergencies along with statistical and other socio-economic modeling techniques. Our review also highlighted how scientific communities and policymakers could leverage GIS to extract useful information to make an informed decision in the future.
Conclusions: Despite the limited applications of GIS in identifying the nature and spatio-temporal pattern of this raging pandemic, there are opportunities to utilize these techniques in handling the pandemic. The use of spatial analysis and GIS could significantly improve how we understand the pandemic as well as address the underserviced demographic groups and communities.
Keywords: GIS, Coronavirus, COVID-19, Spatial analysis, Systematic review, Evidence-based practice
Introduction
COVID-19 has taken the world within a blink of an eye with a rapidly increasing confirmed cases and case-fatalities around the world 1 . After originating in the Hubei province of China in late December 2019, the World Health Organization (WHO) termed it an epidemic on January 29 2020 2 , named it COVID-19 on February 11, and declared it as a pandemic on March 11 3 . Although the first reported case was in China, and it was the epicenter of the pandemic 4 , the virus has mutated and changed transmission pattern several times since then 5 . Lately, the United States, parts of Europe, and countries in the Global South had been reporting the highest number of cases with a rapid increase in both confirmed cases and fatalities 1 .
The declaration of COVID-19 as a pandemic and subsequent lockdown at various levels, from the local city level to the country level, has a much broader impact on our surrounding environment compared to what we usually observe. Despite the availability of data, studies examining the impacts of this ongoing pandemic and enforced lockdowns using different geospatial analysis techniques is not substantial. However, the application of spatial analysis tools, techniques, and geographic information system (GIS) platforms provide the scientific community and the practitioners a wide range of benefits. These benefits include more straightforward and understandable visualization, real-time tracking of confirmed and reported case numbers 6 , contact tracing, spread direction, and also, to identify the hotspots to limit the dispersion and community spread 7, 8 . The application of GIS in public-health related issues is not something introduced during this pandemic. It was used by numerous studies in the past, long before the computerized GIS software was born in the mid-1960s 9 . Since then, GIS was extensively used in analyzing, visualizing, and detecting patterns of disease. A recent review found that among the included 869 studies, one-fourth of the studies used GIS techniques for mapping, especially infectious disease mapping 10 .
Different GIS software and methods have been implemented and widely accepted to prevent the transmission by imposing lockdowns and contact tracing. The best example of GIS application during this pandemic is the web-based near-real-time COVID dashboard created by the Johns Hopkins University 6, 11, 12 . Later the WHO and different local and regional governing bodies also followed the same direction 13 . The online dashboards have been a critical source of information during this pandemic. Although at the beginning the studies implementing or using GIS methods were more focused on visualizing or contact tracing, later, they moved on spatial analysis incorporating social, economic, environmental, and more sophisticated analytical tools as more data started to become available.
There have been attempts to review the studies regarding the application of geospatial analysis in COVID-19 related studies. Pardo et al. (2020) reviewed the studies that were focused on understanding the distribution patterns of the pandemic and identified such applications in six thematic groups 7 . Similar attempts were made by Kamel Boulous and Geraghty (2020) to review the web-based use of GIS technologies 8 . However, none of these approaches followed a systematic approach in selecting the articles, and the reviews were mostly incomprehensive.
Systematic reviews provide an organized, replicable, and methodologically synthesized landscape of evidence that may inform policymaking and practice. During this pandemic, the scarcity of evidence remains a major challenge for public policymaking, which necessitates a careful assessment of the growing body of literature on GIS and geospatial analyses. Also, systematically evaluated evidence is critical for the advancement of science as further primary studies or research syntheses can be informed by the findings of a systematic review. We acknowledged this knowledge gap and conceptualized this review to advance science and practice related to GIS and a wide range of geospatial techniques that are being used in this pandemic. The objective of this study is to conduct a systematic review of the implementation of GIS and other geospatial tools and technologies in COVID-19 related studies. We highlighted the works that used geospatial techniques as part of their analytical method and tried to provide pointers on how these techniques can be better used in times of future public health emergencies.
Methodology
Guideline and data sources
This systematic review was conducted using the reporting guidelines as stated in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement 14 . A protocol was prepared before conducting this review that was not registered with PROSPERO or any other organization. This protocol was uniformly followed by the reviewers at each stage of the review, which is available upon request. The data for this systematic review were retrieved from MEDLINE and Web of Science. Both databases have their own competitive advantages that provide a broader coverage of scholarly articles. MEDLINE is considered as the largest bibliographic databases for health sciences, whereas Web of Science provides access to journals from multiple scholarly disciplines. We used the following steps to identify relevant literature for this review. First, we used the following search query in each database: (“COVID-19” OR “2019-nCoV” OR “2019 coronavirus” OR “2019 novel coronavirus” OR “novel coronavirus” OR “SARS-CoV-2”) to identify COVID-19 related studies. Further, we used another search query to retrieve GIS-related studies as following: (“GIS” OR “ArcGIS” OR "Geographic information systems" OR "Geographic mapping" OR "Spatial analysis" OR "Geospatial analysis"). At the next step, we combined both these queries with “AND” operator to identify literature that is likely to contain studies referring to both these topics. Furthermore, as COVID-19-related literature is evolving rapidly, we also searched the Google Scholar database to identify studies that may align with the objective of this review. Also, we performed a reference searching and contacted subject matter experts for additional studies beyond the scope of the databases, if there were any. We limited the timeline for literature searching between 2019 and 2020 considering the origin of the outbreak in late 2019. The search was first conducted on May 7, 2020, and updated on June 28, 2020.
Eligibility criteria
Articles were considered eligible for this review if they were a) published in English language, b) available as peer-reviewed journal articles, c) the primary focus of the paper was on any aspect of the COVID-19 pandemic, d) demonstrated the applications of GIS or geospatial analyses. Any article that did not comply any of these criteria were excluded from this review. For example, non-English studies, articles that were not peer-reviewed (e.g., letters, editorials, comments), studies that did not focus on COVID-19, or did not use GIS or geospatial techniques (conceptual papers without providing any findings) were considered ineligible for inclusion.
Selection of studies and synthesis of evidence
All citations retrieved through database searching were imported in Endnote reference manager software for curating the collective bibliography. Further, this library was exported to Rayyan QCRI, a cloud-based software for citations screening and assessment. Two authors independently assessed each citation against the eligibility criteria stated above. At the end of the process, a third reviewer was consulted to review the conflicts and a consensus on inclusion or exclusion was made upon discussion. The full texts of the primarily selected articles were reviewed and reviewed by all authors.
Further, articles fulfilling all criteria for this review were retained and data were extracted using a predesigned extraction sheet in Microsoft Excel on the following variables:
a) publication details,
b) study objectives,
c) the sources of data,
d) countries of origin,
e) COVID-19 specific domain presented in the papers,
f) the use of GIS or geospatial analyses, and
g) the research outcomes or key findings of those studies.
The applications of GIS or geospatial analyses on COVID-19 studies were identified and narratively synthesized as major themes alongside tabulation of the key findings. A narrative synthesis is appropriate where quantitative or qualitative synthesis may not be feasible due to the methodological differences and other measures of heterogeneity across the included studies 15 . Moreover, quality appraisal or risk of bias assessment were not considered in this review due to a large volume of studies and profound heterogeneity in methodological approaches, data sources, measurements, types of applications adopted in different contexts, and research outcomes in respective studies.
Results
Summary and characteristics of reviewed articles
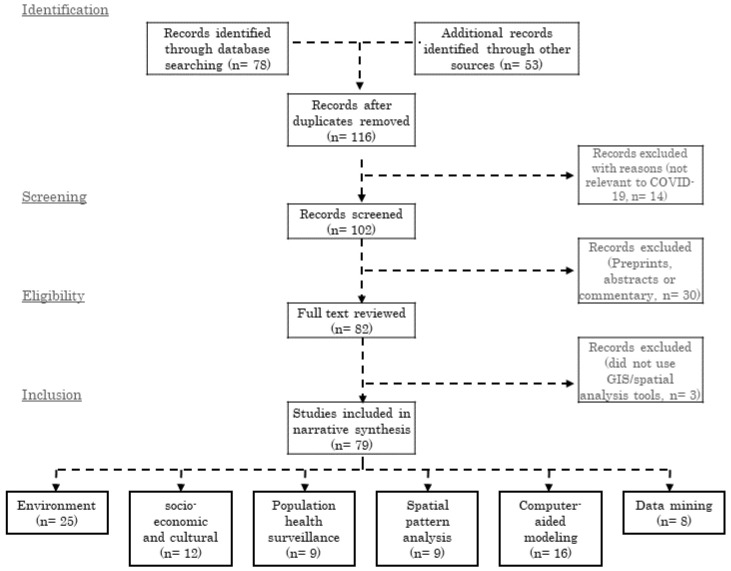
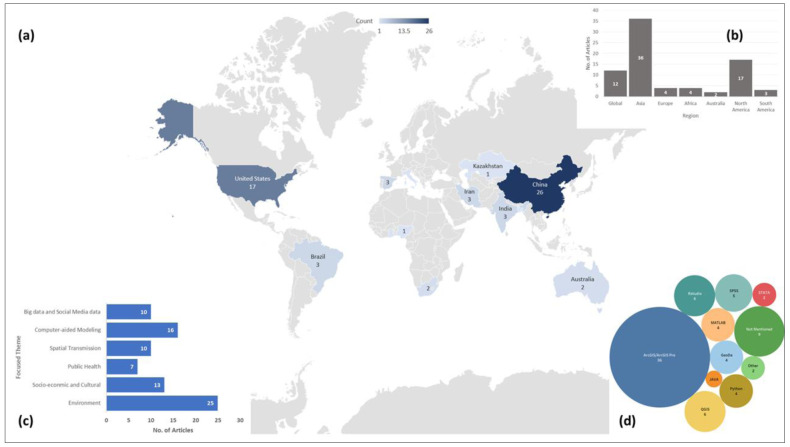
The PRISMA diagram for this review is shown in Figure 1. We found a total of 79 articles which met all the inclusion criteria. A PRISMA checklist enlisting the contents of this systematic review is available on Open Science Framework repository 16 . A summary of these 79 reviewed articles is listed in Extended data, Table 1 17 . The articles included in the review were published in a diverse group of journals, mostly in public health, urban planning, geography, and interdisciplinary journals. Although COVID-19 is more of a public health and welfare issue, these articles covered from public health issues to planning techniques, environmental concerns, and, most importantly, used geospatial analysis tools and techniques as part of their methods. In total, 32.9% of the articles (n=26) used China and 21.5% the United States (n=17) as their study site, which indicates to the disparity of the geographic coverage. Figure 2 shows the geographic distribution of the study area used in the 79 articles we included in our review. Wuhan, China, first reported COVID-19 cases, and the GIS has the highest number of confirmed cases, which also was reflected in the over-representation of these two countries in these articles. Africa and Europe had the lowest number of articles (n=4). Among these reviewed articles, 15% (n=12) worked on a global or multi-national scale. The global studies are more focused on mobility and how COVID-19 transmitted via airports and other human mobility 18– 20 .
Figure 1. GIS Applications in COVID-19 research literature search and evaluation for inclusion.
Figure 2.
( a) article count per country and geographic distribution of the study sites; ( b) number of articles in each continent based on study site along with Global scale studies; ( c) number of articles in each thematic groups used in this review; and ( d) bubble chart showing the frequency of each software or tool used for spatial analysis.
A wide range of geospatial tools were used in the reviewed articles. Most of these articles used regression analysis (n=18) and correlation analysis (n=11) for statistical analysis. Most prominently used spatial analysis was hotspot analysis using either kernel density function or other density techniques (n=16) followed by the spatial autocorrelation analysis using either global or local Moran’s Index (n=13) and proximity analysis (n=5). All the articles used different visualization techniques to display either the intermediate or the end products. Along with that, suitability analysis (n=3) and sensitivity analysis (n=4) were also used to find either access to hospitals or how the cases are distributed. One of the less frequently implemented but interesting technique was to track transmission patterns using the mobility data 8, 21, 22 . Similarly, remote sensing data was used for air quality and pollution measurement, but not that prominently (n=6). Nighttime imagery and solar radiation data were used by n=5 studies to compare the energy consumption differences between before and after pandemic situation.
ESRI ArcGIS is the most used platform (n=36) in these articles. QGIS, a free and open-source GIS software was also used in these reviewed articles (n=4). Other open-source platforms like RStudio, where spatial and statistical analysis can be done simultaneously, were often used as well (n=6). Apart from that, a couple of the studies developed their own platforms and one of the studies used GPS data. Most of these articles used COVID-19 confirmed cases as part of their analysis (n=77). In most cases, researchers used either WHO provided data or JHU provided data for the research purpose. As several spatial analysis was performed based on remotely sensed data, NASA and USGS satellite images were the primary source for those (n=5). Apart from that, the air quality index (AQI) was used in the articles focused on environmental analysis (n=8). As mentioned in the methodology, we did not assess the risk of bias among studies included in this review.
Thematic groups
The rapid diffusion of COVID-19 and data convenience had enforced the global scientific community to work more vigorously on geospatial analysis of this pandemic. These studies had focused on distinct aspects of the pandemic and have different inputs. The articles included in this review was divided into six thematic groups- environment (n=25), socio-economic and cultural (n=13), Population Health Surveillance (n=8), spatial transmission (n=9), computer-aided spatial and statistical analysis and modeling (n=17) and big data, social media and mobile data (n=10).
Environment . We found a total of 25 articles that emphasized the use of GIS and spatial analysis on environmental issues related to COVID-19 8, 19, 21– 43 . Although these studies had a similar research interest, they differ significantly based on the spatial scale- from global 23– 27 to regional 28, 29 , national 30– 38 and small local scale studies 39– 45 . Several works examined the relationship between different meteorological factors and the transmission potential of the virus. They included a diverse set of characteristics in the studies: temperature 21, 25– 27, 30, 31, 33, 35– 37, 39, 42, 44, 46 , humidity 21, 26, 27, 31, 33, 35– 37, 39, 44, 46 , precipitation 21, 39 , daylight hours 25, 46 , solar radiation 21, 31, 35 , and wind-speed 27, 33, 35, 39 . One primary hypothesis of these studies was that these climatic factors and the dispersion of COVID-19 are correlated. In an attempt to examine the hypothesis, statistical and geospatial analysis was used as a key analytical tool 25, 31, 39, 44 .
Studies analyzing the effects of temperature, humidity, and solar radiation found that an association exists between the transmission of the virus and humidity. These studies claimed that humidity is directly associated with the transmission 31 , while temperature has no relation to the viruses diffusion 35, 37 . However, another study refuted these findings and claimed both temperature and average daylight hours are influencing the spread of the virus 25 . Other studies incorporated demographic variables as well as mobility and infections data with these meteorological factors to investigate how they are correlated with the COVID-19 outbreak 35 . Instead of concentration mapping, they showed the spatial distribution and sensitivity of each factor in the study area map and asserted that population density and human mobility among the provinces are directly influencing the accelerated diffusion of COVID-19 cases.
Statistical and spatial analysis and modeling were used in other studies to identify the association between COVID-19 and climatic factors to understand the spatial distribution pattern of COVID-19 cases 26, 44 and spatio-temporal prediction of the pandemic for a different period 36 . These studies concluded that without adequate and effective control measures, there is no evidence of humidity, and summer weather substantially limiting the pandemic growth 26 . Additionally, Pearson's correlation, generalized additive model, and regression models were also utilized in different studies to understand the influence of climate on the virus transmission. These works widely used GIS for mapping the observed and predicted COVID cases 30, 33 , mean temperature and humidity variation and correlation with COVID cases 27 . None of these studies found any evidence of slower COVID-19 transmission with the change of temperature and humidity.
Different countries around the world have enforced different lockdown strategies since mid-January, even before WHO declared COVID-19 as a pandemic. As a result of these lockdowns, and lowered human and industrial activities, a substantial decline in air pollution was noticed 23, 24, 28, 29, 34, 40, 41, 43 . Several studies had reported a significant reduction in NO 2, CO , and SO 2 concentration in the environment 23, 24, 28, 34, 40 . Studies reported significant improvement in AQI 39 and significant reductions in particulate matter (PM) concentrations 41 . Similar studies at a global scale reported a significant decrease in NO 2 concentration and minor decrease in CO concentration, and aerosol optical depth 23 .
Other studies identified a global reduction of environmental pollution by up to 30%, human mobility by up to 90% 24 , and vessel activities by up to 69% 29 . A study using satellite images to compare the pollutants concentration before, during, and after the Chinese Spring Festival observed that the usual trend of NO 2 and SO 2 concentrations decrease before the festival and increase afterwards was not noticed in 2020 34 . ArcGIS was extensively used in several studies to quantify the association between AQI and the distribution of COVID-19 cases 32, 33 . These studies claimed that air quality is a core driver of COVID-19 dispersion around the world, and the dispersion enhances in a temperature ranged from 10 to 20°C. ArcGIS was also used to perform sensitivity analysis, and for the calculation of Global Moran's I and LISA to analyze the impact of PM concentration in the air on the fatality rate in China 45 . The study concluded that the fatality rate is positively correlated with the pollutant concentrations in the air.
Socio-economic and cultural . In response to the coronavirus pandemic, alongside the booming clinical and public health research, social scientists are also retooling existing studies, methodologies, and data to understand the people's behavior responding to the pandemic and its impact on socio-economic and cultural settings around the globe. A total of 12 articles were identified that emphasized on socio-economic and cultural aspects in COVID-19 and used GIS 43– 54 . Researchers used gross domestic product (GDP), demographic and household compositions data, population density, and accessibility data 46 . Several researchers utilized existing social vulnerability index data and applied geospatial tools and techniques to examine the spatial pattern of COVID-19 emergence across different socio-cultural settings 47– 49 . Studies developed dot density and choropleth maps of COVID-19 cases and reported that population density diseases along with poverty and unemployment rates are the major indicators associated with a higher COVID-19 mortality rate 49 .
Different studies reported association among spatial distribution of the socioeconomic variables and the temporal progression of the pandemic using a regression model based spatio-temporal analysis. They noticed that per capita GIS and public transit access is closely related to COVID-19 incidence 46 . Using a similar analytical tool, another study estimated the association between virus infection and social vulnerability considering county-level socioeconomic data, demographic composition, disability and minority status, language, and housing and transportation database. The study concluded that the increase of COVID-19 cases is highly associated with minority status and language 47 . To understand the association between racial inequality and COVID-19 mortality, Kim and Bostwick (2020) utilized principal component analysis (PCA) and hotspot analysis in ArcGIS. The study reported that African American communities are the ones with the highest COVID-19 related deaths in the USA 48 . Other studies also used ArcGIS and regression analysis to investigate the spatial patterns of the COVID-19 in relation to socio-economic variables. This study used GIS to map the spatial aspects and disparities between metropolitan and nonmetropolitan communities and the regression analyses to test the hypotheses of positive correlations between COVID-19 incidence and mortality rates and socio-economic factors in the GIS 50 .
Proximity and hotspot analysis in GIS has become a widely used geospatial analysis technique in the social research to understand the feasibility of social distancing 51 , accessibility analysis of specific age group 52, 53 . Gibson and Rush (2020) calculated the distance to each dwelling's nearest neighbors to identify units that are unable to practice social distancing effectively. Dryhurst et al. (2020) developed a global risk perception index (R.P.I.) using a linear regression model and used GIS to plot the mean risk perception of COVID-19 in 10 countries 54 . Sarkar (2020) used ArcGIS to reclassify the administrative units of Bangladesh based on COVID-19 susceptibility using multicriteria analysis based pairwise comparison 55 . Cavalcante and Abreu (2020) applied Moran’s I and LISA to identify the type and degree of spatial clustering and scatter plots of socio-economic indicators 56 . Similarly, Exploratory Spatial Data Analysis (ESDA) technique was used to identify spatial relationships between the density of built heritage resources and Airbnb listings. Based on the calculation and mapping, they concluded that the distribution of Airbnb listings has a certain degree of spatial autocorrelation 57 .
Population health surveillance . From the first case in Wuhan to the global pandemic, an enormous number of public health studies have been conducted to help the policymakers to understand how best to manage the current and future public health responses. A total of nine articles were identified that emphasized public health issues and used GIS 50, 55– 62 . Multiple studies developed a multicriteria decision making index to assess the risk and resilience of the existing healthcare system. Requia et al. (2020) employed GIS techniques to construct a geodatabase comprising land use, income, population, health condition, number of hospital beds, and staff at the municipality scale. They predicted a deficit of 17 beds in Brazilian municipalities 55 . Similarly, Jovanović et al. (2020) developed a global index comprising of 57 indicators using ArcGIS-based network analysis for hospital accessibility and resilience mapping 58, 59 .
GIS was used to find out whether there is any association between orthopedic surgeons’ age and COVID-19 confirmed cases 60 . The study reported a spatial relationship between the number of cases and number of surgeons in a state. In a similar study, Ruthberg et al. (2020) studied the potential risk of otolaryngologists above age 60 due to COVID-19, where they used a heat map to show the state-wise potential risk zone using QGIS. The study indicated that New York, New Jersey, Massachusetts, and Michigan were the riskiest zone according to the ratio of the number of confirmed cases to the number of total ENT's over 60 61 . Kuupiel et al. (2020) calculated the distance from the primary healthcare (PHC) clinic as well as to the nearest health facility in ArcGIS to measure geographical accessibility (in terms of distance and time) to COVID-19 specialized hospital facilities in Ghana. The analysis reported that the current mean travel time (more than an hour) and distance (more than 35 kilometers) to PHC is significantly higher than the globally accepted standards 62 . Similar accessibility analysis was done in Australia using proximity analysis and hotspot analysis to measure travel time to the closest hospital facility for aged population resulted in a similar outcome as well 53 .
Ahmadi et al. (2020) developed an epidemic prediction model for spatial-temporal analysis to predict and estimate the number of patients and deaths at the end of pandemic (infected, cured, and dead cases). The study predicted that approximately 7900 and 4620 deaths would occur in Iran from May 13 to June 1, 2020, respectively, and then the curve will flatten 63 . To analyze the epidemiology of COVID-19, studies also utilized georeferencing. These studies first geocoded all COVID-19 cases and then joined them to the county layers by administrative codes in ArcGIS and afterwards, applied LISA. This study reported that the spatial clustering is not random and shows significant spatial heterogeneity in China 64 . A wastewater-based epidemiology (WBE) tool was proposed as a surveillance tool to monitor the COVID-19 pandemic 65 . The study used multiple variables to run the GIS-based hydraulic model and network analysis using the SWMM modeling environment and ArcGIS. The result effectively served as a justification to use WBE as a rapid and efficient tool to track COVID-19, which the authors claimed could be used with clinical testing to save billions of dollars 65 .
Spatial pattern analysis of COVID-19 . A total of nine articles were identified that emphasized on identifying the spatial transmission pattern analysis of COVID-19 15, 17, 20, 62– 67 . So far, only one study had used geospatial analysis to identify Spatio-temporal clusters and prediction modeling for COVID-19 transmission. They utilized the Poisson probability distribution model, Kernel density analysis, and space-time scanning analysis to identify high-risk Spatio-temporal clusters for transmission of COVID-19 in Brazil and detected active Spatio-temporal clusters comprising six municipalities in the south-central region of Brazil 66 . Only two studies so far studied how travel restrictions may have limited the epidemic trajectory. One of them developed a global model based on internationally reported cases and mobility data, to project the impact of travel limitations on the national and international spread of the epidemic and revealed that Wuhan travel ban only hindered the overall epidemic trajectory by 3 to 5 days in other cities of China but had a significant influence on the international scale dispersion 22 . Studies also estimated the probability of COVID-19 cases transportation before January 23 among 369 cities in China and reported that 130 cities in China have more than 50% chance of having a COVID-19 case imported from Wuhan 67 .
In a global study to identify geographic risks of COVID-19 transmission using online Rasch Modeling Algorithm, the authors reported that Iran, South Korea, Italy, Germany, Spain, China (Hubei), and France, are the top countries with higher outbreak potential respectively 68 . Other studies utilized accessibility analysis techniques to assess the spatial diffusion of COVID-19, using GIS-based origin, destinations, and frequencies mapping of public transportation from Wuhan. The study claimed that increase of COVID-19 cases has a direct relationship with the frequency of public transport from Wuhan 69 . Other studies utilized time-series analysis and plots to portray the spatial and temporal variation of COVID-19 cases in China and to elucidate the role of case importation in transmission in cities across China using spatial analysis 70 .
One other global study used GIS to visualize the worldwide distribution of air transport passengers from Wuhan and infected traveler’s ratio around the world 20 . Geo-referencing of confirmed cases also played an interesting role in the spatial pattern analysis studies. These studies measured and identified the regions that have a high risk of transmission at an early stage 71 . Similarly, a generalized linear regression model was used to analyze the spread and control of COVID-19 cases using case reports, and human movement data. This study utilized spatial distribution mapping of the travel movements from Wuhan to each province and modeled the spatial dispersal pattern of COVID-19 trajectories with or without Wuhan travel ban. They found that Wuhan shutdown delayed arrival of COVID-19 in other cities by around three days 19 .
Computer-aided spatial and statistical analysis and modeling . A substantial number of studies were found to apply computer-aided spatial and statistical analysis and modeling techniques in analyzing distinct aspects of COVID-19. A total of 16 articles were identified that emphasized on computer-aided spatial and statistical analysis and modeling in COVID-19 69– 84 . Most of these works were focused on analyzing the spatial distribution pattern of COVID-19 cases using the confirmed cases data 72– 78 , or news reports of COVID-19 cases as proxy data 79 . Most of the studies were focused on examining the spatial distribution and relationship between COVID-19 cases, deaths, and locations. Adekunle et al. (2020) examined the same relationship. They found a positive statistically significant relationship among spatial clusters, confirmed cases and potential deaths 72 . Another similar study in Hubei, China, demonstrated that the high-low cluster had no high-value incidence cluster where local Moran's I indicated that Hubei was the only province with High-Low aggregation 74 . Moran's I was applied in analyzing the spatial and temporal distribution of cases in Hubei province by other studies as well 77 .
Multiple studies examined the spatial and temporal distribution and modeled the trend of COVID-19 cases growth in ArcGIS and found that the highest risk place was those that had a high population inflow from Wuhan and Hubei province 75, 76 . Spatial modeling using Poisson space-time scan statistics to produce cluster mapping attempts also led to the proposal of first rapid surveillance to monitor the spread of COVID-19 73 . Miller et al. (2020) demonstrated the worldwide spatial distribution of COVID-19 cases using the heat map technique in GIS The map reported that China, Italy, Iran, and Spain were the highest affected countries till March 17, 2020, which was also visible by the JHU and WHO reported data 78 . Spatial panel data model used by Guliyev (2020) showed that the rate of deaths had a significant positive effect where the recovery rate had a negative with the confirmed COVID-19 cases 80 . Irvine et al. (2020) used a SEIR model to estimate the transmission rate within Immigration and Customs Enforcement detention facilities in the GIS and the impacts on the I.C.U. capacity 81 .
Bai (2020) used two different models, including SEIRD model and Agent-Based Model (A.B.M.) to simulate the COVID-19 spread. They found that A.B.M. could be more effective and it also could be a useful tool to figure out new effective strategies 82 . In a similar work, Mollalo et al. (2020) compared five different models to develop a spatial model of COVID-19 incidence rate considering 35 variables using geospatial software’s. The results showed that MGWR could be a better model as it was able explain 68.1% of the total variation of COVID-19 incidences in the GIS 83 . In a follow-up paper, the same authors used ANN to model the incidence rate of COVID-19 and used Moran's I index to create incidence hotspots. Out of included 57 variables, 10 variables found statistically significant in explaining the result 84 . A similar global scale study revealed that age and population density have a statistically significant relationship with the spatial distribution pattern of COVID-19 cases 85 .
Using Maxent based Ecological Niche Model, Ren et al. (2020) developed a potential risk zone map of China where population, public transportation demands, medical resources demands were used as explanatory variables. They suggested using this as an early forecasting model to predict the risk zone in China's other megacities 86 . Kanga et al. (2020), on the other hand, provided a useful recommendation to local authorities in India by using proximity-based hot spot analysis to map the risk zones with relevant preventative measures to mitigate the COVID-19 crisis 87 . Several other works were focused on suitability mapping with a focus to find a suitable location for the quarantine zone in Surat, India, using ArcGIS. The study revealed that the suitability analysis could help to control the spread as a prevention measure.
Data mining and COVID-19. We grouped the application of big data, social media data mining, and contact tracing through geospatial technologies together. Although very few studies attempted to incorporate those techniques in COVID-19 research, a total of eight articles were identified that emphasized on data mining, big data, and social media data use in COVID-19 62, 85– 91 . Data mining using unsupervised machine learning models were utilized in a study to analyze the twitter data and it reported tweets related to symptoms of users is associated with COVID-19 testing accessibility 66 . Studies also used nighttime light (NTL) data and AQI data to analyze the spatial and temporal pattern of COVID-19 and how that impacted human activities. The observation demonstrated that the NTL brightness and AQI value were much lower during the quarantine period in Mainland China 88 . Similarly, radar data was used to detect traffic patterns where the findings reported that the number of heavy vehicles movement in the region changed significantly after the COVID outbreak 89 .
Several studies used mobile sensor data or geodata for contact tracing as a surveillance strategy to monitor COVID-19 90– 92 . Wang et al. (2020) developed a Geo-AI based mini program within an instant messaging app (WeChat) to trace close contacts of all confirmed patients. The results showed that the program could analyze real-time data to trace the contacts, and those data could be used with other datasets to find out more useful information to reduce COVID-19 spread. Similarly, other studies also attempted to develop a smart contact tracing app using big data analytics 90 or using a mobile sensor-based contact tracing system to minimize the spread of COVID-19 91 . Using social media posts, Huang et al. (2020) examined the attributes of both suspected and confirmed COVID-19 cases who contacted with the symptoms. They used SPSS and ArcGIS for descriptive statistical analysis and spatial analysis, where they found that most of the patients seeking help were above 65 years old from Wuhan 93 .
Discussion
To the best of our knowledge, this is one of the first systematic reviews of the application of GIS and other geospatial technologies in COVID-19 related research. Our work does not only provide an overview of how GIS was used so far but also provides pointers on how GIS could be more efficiently used in COVID-19-related works and other public health issues in the coming days. The application of GIS technologies and spatial analysis has substantially influenced the understanding of COVID-19, not only for the scientific community but also for the policymakers, and for the public in building a long-term response to the ongoing pandemic 94 . Initially, spatial analysis techniques were used as part of predictive modeling to predicts the growth of COVID-19 cases 63 and to model the spatio-temporal variation of confirmed incidences 74 . With the increasing availability of COVID-19 data, a significant number of studies started to analyze the spatial transmission pattern and spread of the virus from Wuhan to other cities in China and the rest of the world 8, 18, 19, 22, 26, 67, 71, 89, 95 . Most of these early applications of GIS and spatial analysis were more focused on visualizing the COVID-19 confirmed cases as well as the distribution of cases among administrative units and countries. However, as time goes on and more data became available, more complex GIS tools come into play. Studies not only used GIS for analyzing different environmental aspects; they also used different earth observation data acquired by the European Space Agency (ESA) and NASA 23, 24, 28, 34 .
During the early days, one of the biggest discussions among the researchers was regarding the ability of meteorological factors to limit the spread of coronavirus. With the declaration of the pandemic and subsequent lockdown globally in early March, several studies used GIS and remotely sensed images to analyze the impacts of this lockdown on the environment, air quality, and other particulate matters 19, 23, 26 . Several studies evaluated that relationship with the help of spatial analytical tools, and most of these studies could not reach a valid conclusion where they could claim temperature or other climatic factors do limit the spread of the virus 23, 24, 27, 30 . Later application of GIS does not restrict itself in just visualizing. Instead, it was more used to spatial autocorrelation and clustering analysis, hotspot analysis, and suitability analysis to see whether any association exists among social and economic groups, any specific location or social group, and COVID-19 infection rate 55, 56, 59 . With the increasing confirmed cases around the world, different social-science studies analyzed the association among COVID-19 infection rate and social vulnerability, racial inequality, risk perception, resiliency, and settlement quality issues 44, 45, 47 . These studies also utilized GIS to identify any spatial patterns and autocorrelation with COVID-19. In the following days, different epidemiological models (i.e., COVID-19 Hospital Impact Model for Epidemics (CHIME)) were employed to forecast and map the spread of the virus within a geographic context, that enabled the policymakers to undertake informed interventions and allocate their resources accordingly 96, 97 .
We reviewed how GIS and spatial analysis techniques were used in the past COVID-19 related studies. We found that most of the included studies used GIS for visualizing the spatial distribution and pattern of COVID-19 spread, cluster analysis to identify the accumulation of cases, hot spot analysis to find out any outbreak, proximity analysis to evaluate the accessibility to the primary health care facilities. However, with time, studies focused on different models to predict or simulate various aspects of COVID-19 using geospatial techniques that were published as well. On that point of interest, GIS-based Maxent model, spatial data panel model, SEIR model, Agent-Based Model, GWR, MGWR, ANN were used in different studies 80– 84, 86 . However, we did not find any studies that used spatially explicit modeling to identify and predict the location of any potential outbreak in the future. One of the few positive aspects of COVID-19-related studies is the publicly available data, and the same was noticed in the review as well. We found that more than half of the studies used data from some form of government database followed by WHO database (n=12), different websites (n=12), JHU dashboard and Worldometers (n=9), Social media data (n=8), satellite images (n=7), primary survey (n=3) and mobile phone data (n=3).
Though COVID-19 related data is mostly publicly available, some studies reported data unavailability issues, especially in developing or less developed countries 32, 49, 84 . The major challenge of global or regional studies is the possibility of an under-reported number of confirmed cases, especially in low-income regions, because of the low detection coverage of COVID-19, which may skew the result. Most of the global or regional studies cannot incorporate the controlling measures imposed by different governments, which has significant impacts on the spread and infection incidences of COVID-19 cases. No consideration of government control measures and low testing issues is also a substantial limitation for modeling and prediction focused research which creates a biased result. Therefore, future studies should emphasize considering government control measures and policies in their modeling. Although contract tracing and data mining research has been proven to be useful in analyzing and forecasting the spatial pattern of COVID dispersion, no trace of any studies were found outside of China and the USA. That might be due to data unavailability and technological issues. Contract tracing in China was possible due to its government-backed app that gathers a user's information, including name, ID number, and health information and movement data. Two studies were conducted in China and Taiwan for smart contract tracing using mobile sensor data 90, 92 . Low or middle-income countries can adopt a GIS-based volunteered surveillance approach where peoples will share their information voluntarily to tackle the pandemic. So far, GIS has not been used much to track the transmission pattern and to predict the transmission. That is something that can be done at a global level to leverage GIS to predict not only the confirmed case numbers but also specific locations where the outbreak would happen with higher statistical precision 98 .
The findings of this review have profound implications for contemporary and future multidisciplinary scientific research, policymaking, and practice. The diverse use of GIS technologies in different overarching thematic areas of scientific research highlights the potential of incorporating methodological perspectives for solving complex research questions. This evolution is consistent with the emerging perspective that “one size does not fit all” and each unique scenario may require conceptual and empirical inputs from different disciplines for achieving a higher precision on research outcomes. Nonetheless, an increasing trend of integrating GIS technologies in studies that emphasized on multiple research objectives show how such technologies are being a part of the entire work rather than the only approach used in those research efforts. Thus, the use of GIS may improve other methodological measures and increase the scope of scientific exploration on a topic of interest.
The existing evidence highlights the use of GIS and other geospatial techniques for addressing research question; however, little evidence exists on how geospatial can be used for delivering digital interventions for individuals or target populations. Perhaps such technological innovations would take much time to appear, but precision sciences and their applications on personalizing user level platforms may bring such technologies closer to everyday practice. Moreover, a wide range of data sources used in different studies included in this review provide meaningful insights on how data from multiple can be harmonized and utilized in addressing population-based problems. Furthermore, integrating GIS in COVID-19 related research may enable real-time decision-making for preventing public health crises and deploying resources whenever required. A major lesson from existing studies is to developing local and global disaster preparedness plans that may enable policymakers and practitioners to leverage GIS-based advanced data analytics for mitigating large scale public health emergencies. More implementation research is needed to assess the scope of such multipronged yet coordinated response systems that may emerge in the post-pandemic world. Such initiatives may require strengthening technological capacities in low and middle-income countries that share a major proportion of global health problems yet have limited resources to address the same 99, 100 .
Despite notable strengths, this systematic review has several limitations that should be acknowledged and addressed in future research. First, the selection of databases and keywords could have excluded some studies that were indexed in other databases or used non-specified keywords, which were beyond the scope of this review. Adding more databases/conferences/journals could have improved the findings that were beyond the scope of this review. As more studies are being published and presented on geospatial aspects of COVID-19, future evidence syntheses should include additional sources whenever possible. Second, we focused on peer-reviewed publications and did not cover preprints that did not undergo peer-review; therefore, those studies are also excluded from this review, which may provide further insights on the evidence landscape. Third, the existing literature shows a high heterogeneity in the methods, data inputs, and research outcomes leading to a narrative synthesis. Fourth, we did not assess the quality of the studies and the risk of bias within and between the studies. We recommend that future evidence syntheses on specific GIS-related topics should assess the risk of bias among the scientific literature in those topics. Prospective evidence-based reviews may also consider the quantitative synthesis of homogenous studies on specific themes. This systematic review provides an inclusive and extensive synthesis of multidisciplinary research using GIS during COVID-19, which may inform future primary studies and advanced syntheses addressing the current limitations and improving the knowledge base in this domain. Our study also did not examine the data management practices in the reviewed studies. A huge concern in these studies is confidentiality. Therefore, we call for robust data management and sharing practices ensuring confidentiality and ethical use of data. Future such reviews could investigate the data collection and reporting strategies followed by the researchers.
Conclusion
This systematic review evaluated the current literature on the use of GIS and geospatial analyses in the context of COVID-19 pandemic and explored the scope of integrating such techniques in the current research efforts as well as future research and practice. In the era of digital revolution, a growing need for exchanging technological advancements across scientific disciplines is widely acknowledged. The use of GIS and related technologies in COVID-19 pandemic exemplifies such integrations and provide scholarly perspectives on how complex societal and global issues can be understood using the existing tools. Moreover, such applications necessitate revisiting the current strengths and weaknesses of curating evidence across contexts. It is essential to strengthening institutional capacities to leverage GIS-related technologies in multipronged research and development that empower research communities to work together in this pandemic. Last but not least, future technological innovations should be grounded on the lessons learned during this pandemic to make such technologies readily available for facilitating robust research and decision-making that may improve population-level outcomes globally.
Data availability
Underlying data
All data underlying the results are available as part of the article and no additional data are required.
Extended data
Figshare: Application of geospatial techniques in COVID-19-related studies. https://doi.org/10.6084/m9.figshare.13229147.v2 17 .
This project contains a summary of the articles identified in this study. This includes a detailed breakdown of what methods used in the reviewed article, along with the data type, spatial analysis tool/techniques and the findings from the analysis.
Reporting guidelines
Open Science Framework: PRISMA checklist for ‘Applications of GIS and geospatial analyses in COVID-19 research: A systematic review’. https://doi.org/10.17605/OSF.IO/ZGMP8 101 .
Extended data are available under the terms of the Creative Commons Attribution 4.0 International license (CC-BY 4.0); the completed PRISMA checklist is available under the terms of the Creative Commons Zero "No rights reserved" data waiver (CC0 1.0 Public domain dedication).
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 2; peer review: 2 approved]
References
- 1. World Health Organization (WHO): Coronavirus disease 2019 (COVID-19): situation report, 201.2020a. Reference Source [Google Scholar]
- 2. McNeil MG, Jr: Coronavirus Has Become a Pandemic, W.H.O. Says.In The New York Times. ed. New York: The New York Times Company,2020. Reference Source [Google Scholar]
- 3. World Health Organization (WHO): Coronavirus disease 2019 (COVID-19): situation report, 250.2020b. [Google Scholar]
- 4. Allam Z: The First 50 days of COVID-19: A Detailed Chronological Timeline and Extensive Review of Literature Documenting the Pandemic. Surveying the Covid-19 Pandemic and its Implications. 2020;1–7. 10.1016/B978-0-12-824313-8.00001-2 [DOI] [Google Scholar]
- 5. Kannan SR, Spratt AN, Sharma K, et al. : Omicron SARS-CoV-2 variant: Unique features and their impact on pre-existing antibodies. J Autoimmun. 2022;126:102779. 10.1016/j.jaut.2021.102779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dong E, Du H, Gardner L: An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Franch-Pardo I, Napoletano BM, Rosete-Verges F, et al. : Spatial analysis and GIS in the study of COVID-19. A review. Sci Total Environ. 2020;739:140033. 10.1016/j.scitotenv.2020.140033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kamel Boulos MN, Geraghty EM: Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics.(in eng). Int J Health Geogr. 2020;19(1):8. 10.1186/s12942-020-00202-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. ESRI: History of GIS. (accessed July 29, 2020, 2020). Reference Source [Google Scholar]
- 10. Lyseen AK, Nøhr C, Sørensen EM, et al. : A Review and Framework for Categorizing Current Research and Development in Health Related Geographical Information Systems (GIS) Studies.(in eng). Yearb Med Inform. 2014;9(1):110–124. 10.15265/IY-2014-0008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hopkins J: CSSE Coronavirus COVID-19 Global Cases (dashboard).(accessed August 24, 2020). Reference Source [Google Scholar]
- 12. Hopkins J: CSSE GitHub–CSSEGISandData/COVID-19: Novel Coronavirus (COVID-19) Cases (data repository).(accessed August 9, 2020). Reference Source [Google Scholar]
- 13. Texas Department of State Health Services: Texas Case Counts- COVID-19. accessed. Reference Source [Google Scholar]
- 14. Liberati A, Altman DG, Tetzlaff J, et al. : The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 15. Popay J, Roberts H, Sowden A, et al. : Guidance on the conduct of narrative synthesis in systematic reviews A product from the ESRC methods programme. Version. 2006;1:b92. 10.13140/2.1.1018.4643 [DOI] [Google Scholar]
- 16. Ahasan R, Alam MS, Chakraborty T, et al. : GIS in COVID-19 research.2020. 10.17605/OSF.IO/ZGMP8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ahasan R, Alam MS, Chakraborty T, et al. : Application of geospatial techniques in COVID-19 related studies. figshare. Online resource.2020. 10.6084/m9.figshare.13229147.v2 [DOI] [Google Scholar]
- 18. Kraemer MUG, Yang CH, Gutierrez B, et al. : The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368(6490):493–497. 10.1126/science.abb4218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tian H, Liu Y, Li Y, et al. : An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368(6491):638–642. 10.1126/science.abb6105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Christidis P, Christodoulou A: The Predictive Capacity of Air Travel Patterns during the Global Spread of the COVID-19 Pandemic: Risk, Uncertainty and Randomness. Int J Environ Res Public Health. 2020;17(10):3356. 10.3390/ijerph17103356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pequeno P, Mendel B, Rosa C, et al. : Air transportation, population density and temperature predict the spread of COVID-19 in Brazil. PeerJ. 2020;8:e9322. 10.7717/peerj.9322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chinazzi M, Davis JT, Ajelli M, et al. : The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. 10.1126/science.aba9757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lal P, Kumar A, Kumar S, et al. : The dark cloud with a silver lining: Assessing the impact of the SARS COVID-19 pandemic on the global environment. Sci Total Environ. 2020;732:139297. 10.1016/j.scitotenv.2020.139297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Muhammad S, Long X, Salman M: COVID-19 pandemic and environmental pollution: a blessing in disguise? Sci Total Environ. 2020;728:138820. 10.1016/j.scitotenv.2020.138820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Iqbal MM, Abid I, Hussain S, et al. : The effects of regional climatic condition on the spread of COVID-19 at global scale. Sci Total Environ. 2020;739:140101. 10.1016/j.scitotenv.2020.140101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Baker RE, Yang W, Vecchi GA, et al. : Susceptible supply limits the role of climate in the early SARS-CoV-2 pandemic. Science. 2020;369(6501):315–319. 10.1126/science.abc2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wu Y, Jing W, Liu J, et al. : Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci Total Environ. 2020;729:139051. 10.1016/j.scitotenv.2020.139051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kanniah KD, Kamarul Zaman NAF, Kaskaoutis DG, et al. : COVID-19's impact on the atmospheric environment in the Southeast Asia region. Sci Total Environ. 2020;736:139658. 10.1016/j.scitotenv.2020.139658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Depellegrin D, Bastianini M, Fadini A, et al. : The effects of COVID-19 induced lockdown measures on maritime settings of a coastal region. Sci Total Environ. 2020;740:140123. 10.1016/j.scitotenv.2020.140123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Briz-Redón Á, Serrano-Aroca Á: A spatio-temporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Sci Total Environ. 2020;728:138811. 10.1016/j.scitotenv.2020.138811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Runkle JD, Sugg MM, Leeper RD, et al. : Short-term effects of specific humidity and temperature on COVID-19 morbidity in select US cities. Sci Total Environ. 2020;740:140093. 10.1016/j.scitotenv.2020.140093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Xu H, Yan C, Fu Q, et al. : Possible environmental effects on the spread of COVID-19 in China. Sci Total Environ. 2020;731:139211. 10.1016/j.scitotenv.2020.139211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zhang Z, Xue T, Jin X: Effects of meteorological conditions and air pollution on COVID-19 transmission: Evidence from 219 Chinese cities. Sci Total Environ. 2020;741:140244. 10.1016/j.scitotenv.2020.140244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fan C, Li Y, Guang J, et al. : The Impact of the Control Measures during the COVID-19 Outbreak on Air Pollution in China. Remote Sens. 2020;12(10):1613. 10.3390/rs12101613 [DOI] [Google Scholar]
- 35. Ahmadi M, Sharifi A, Dorosti S, et al. : Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci Total Environ. 2020;729:138705. 10.1016/j.scitotenv.2020.138705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gupta S, Raghuwanshi GS, Chanda A: Effect of weather on COVID-19 spread in the US: A prediction model for India in 2020. Sci Total Environ. 2020;728:138860. 10.1016/j.scitotenv.2020.138860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Qi H, Xiao S, Shi R, et al. : COVID-19 transmission in Mainland China is associated with temperature and humidity: A time-series analysis. Sci Total Environ. 2020;728:138778. 10.1016/j.scitotenv.2020.138778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Arab-Mazar Z, Sah R, Rabaan AA, et al. : Mapping the incidence of the COVID-19 hotspot in Iran - Implications for Travellers. Travel Med Infect Dis. 2020;34:101630. 10.1016/j.tmaid.2020.101630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bashir MF, Ma B, Bilal, et al. : Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci Total Environ. 2020;728:138835. 10.1016/j.scitotenv.2020.138835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bao R, Zhang A: Does lockdown reduce air pollution? Evidence from 44 cities in northern China. Sci Total Environ. 2020;731:139052. 10.1016/j.scitotenv.2020.139052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mahato S, Pal S, Ghosh KG: Effect of lockdown amid COVID-19 pandemic on air quality of the megacity Delhi, India. Sci Total Environ. 2020;730:139086. 10.1016/j.scitotenv.2020.139086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Shahzad F, Shahzad U, Fareed Z, et al. : Asymmetric nexus between temperature and COVID-19 in the top ten affected provinces of China: A current application of quantile-on-quantile approach. Sci Total Environ. 2020;736:139115. 10.1016/j.scitotenv.2020.139115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kerimray A, Baimatova N, Ibragimova OP, et al. : Assessing air quality changes in large cities during COVID-19 lockdowns: The impacts of traffic-free urban conditions in Almaty, Kazakhstan. Sci Total Environ. 2020;730:139179. 10.1016/j.scitotenv.2020.139179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Liu J, Zhou J, Yao J, et al. : Impact of meteorological factors on the COVID-19 transmission: A multi-city study in China. Sci Total Environ. 2020;726:138513. 10.1016/j.scitotenv.2020.138513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Yao Y, Pan J, Wang W, et al. : Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chinese cities. Sci Total Environ. 2020;741:140396. 10.1016/j.scitotenv.2020.140396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Paez A, Lopez FA, Menezes T, et al. : A Spatio-Temporal Analysis of the Environmental Correlates of COVID-19 Incidence in Spain. Geogr Anal. 2020. 10.1111/gean.12241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Karaye IM, Horney JA: The Impact of Social Vulnerability on COVID-19 in the U.S.: An Analysis of Spatially Varying Relationships. Am J Prev Med. 2020;59(3):317–325. 10.1016/j.amepre.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kim SJ, Bostwick W: Social Vulnerability and Racial Inequality in COVID-19 Deaths in Chicago. Health Educ Behav. 2020;47(4):509–513. 10.1177/1090198120929677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ramírez IJ, Lee J: COVID-19 Emergence and Social and Health Determinants in Colorado: A Rapid Spatial Analysis. Int J Environ Res Public Health. 2020;17(11):3856. 10.3390/ijerph17113856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Zhang CH, Schwartz GG: Spatial Disparities in Coronavirus Incidence and Mortality in the United States: An Ecological Analysis as of May 2020. J Rural Health. 2020;36(3):433–445. 10.1111/jrh.12476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gibson L, Rush D: Novel Coronavirus in Cape Town Informal Settlements: Feasibility of Using Informal Dwelling Outlines to Identify High Risk Areas for COVID-19 Transmission From A Social Distancing Perspective. JMIR Public Health Surveill. 2020;6(2):e18844. 10.2196/18844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lakhani A: Introducing the Percent, Number, Availability, and Capacity [PNAC] Spatial Approach to Identify Priority Rural Areas Requiring Targeted Health Support in Light of COVID-19: A Commentary and Application. J Rural Health. 2021;37(1):149–152. 10.1111/jrh.12436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lakhani A: Which Melbourne Metropolitan Areas Are Vulnerable to COVID-19 Based on Age, Disability, and Access to Health Services? Using Spatial Analysis to Identify Service Gaps and Inform Delivery. J Pain Symptom Manage. 2020:60(1):e41–e44. 10.1016/j.jpainsymman.2020.03.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Dryhurst S, et al. : Risk perceptions of COVID-19 around the world. J Risk Res. 2020;23(7–8):994–1006. 10.1080/13669877.2020.1758193 [DOI] [Google Scholar]
- 55. Sarkar SK: COVID-19 Susceptibility Mapping Using Multicriteria Evaluation. Disaster Med Public Health Prep. 2020;14(4):521–537. 10.1017/dmp.2020.175 [DOI] [PubMed] [Google Scholar]
- 56. Cavalcante JR, Lopes de Abreu AdJ: COVID-19 in the city of Rio de Janeiro: spatial analysis of first confirmed cases and deaths. Epidemiol Serv Saude. 2020;29(3):e2020204. 10.5123/S1679-49742020000300007 [DOI] [PubMed] [Google Scholar]
- 57. Rubino I, Coscia C, Curto R: Identifying Spatial Relationships between Built Heritage Resources and Short-Term Rentals before the Covid-19 Pandemic: Exploratory Perspectives on Sustainability Issues. Sustainability. 2020;12(11):4533. 10.3390/su12114533 [DOI] [Google Scholar]
- 58. Requia WJ, Kondo EK, Adams MD, et al. : Risk of the Brazilian health care system over 5572 municipalities to exceed health care capacity due to the 2019 novel coronavirus (COVID-19). Sci Total Environ. 2020;730:139144. 10.1016/j.scitotenv.2020.139144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Jovanović A, Klimek P, Renn O, et al. : Assessing resilience of healthcare infrastructure exposed to COVID-19: emerging risks, resilience indicators, interdependencies and international standards. Environ Syst Decis. 2020;40;252–286. 10.1007/s10669-020-09779-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Jella TK, Acuña AJ, Samuel LT, et al. : Geospatial mapping of orthopaedic surgeons age 60 and over and confirmed cases of COVID-19. J Bone Joint Surg Am. 2020;102(12):1022–1028. 10.2106/JBJS.20.00577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ruthberg JS, Quereshy HA, Jella TK, et al. : Geospatial analysis of COVID-19 and otolaryngologists above age 60. Am J Otolaryngol. 2020;14(4):102514. 10.1016/j.amjoto.2020.102514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kuupiel D, Adu KM, Bawontuo V, et al. : Geographical accessibility to glucose-6-phosphate dioxygenase deficiency point-of-care testing for antenatal care in Ghana. Diagnostics (Basel). 2020;10(4):229. 10.3390/diagnostics10040229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ahmadi A, Fadai Y, Shirani M, et al. : Modeling and forecasting trend of COVID-19 epidemic in Iran until May 13, 2020. Med J Islam Repub Iran. 2020;34(1):27. 10.34171/mjiri.34.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Fan J, Liu X, Pan W, et al. : Epidemiology of Coronavirus Disease in Gansu Province, China, 2020. Emerg Infect Dis. 2020;26:1257–1265. 10.3201/eid2606.200251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hart OE, Halden RU: Computational analysis of SARS-CoV-2/COVID-19 surveillance by wastewater-based epidemiology locally and globally: Feasibility, economy, opportunities and challenges. Sci Total Environ. 2020;730:138875. 10.1016/j.scitotenv.2020.138875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Andrade LA, Gomes DS, Góes MAO, et al. : Surveillance of the first cases of COVID-19 in Sergipe using a prospective spatiotemporal analysis: the spatial dispersion and its public health implications. Rev Soc Bras Med Trop. 2020;53:e20200287. 10.1590/0037-8682-0287-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Du Z, Wang L, Cauchemez S, et al. : Risk for transportation of coronavirus disease from Wuhan to other cities in China. Emerg Infect Dis. 2020;26(5):1049–1052. 10.3201/eid2605.200146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Jen TH, Chien TW, Yeh YT, et al. : Geographic risk assessment of COVID-19 transmission using recent data: An observational study. Medicine (Baltimore). 2020;99(24):e20774. 10.1097/MD.0000000000020774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Zheng R, Xu Y, Wang W, et al. : Spatial transmission of COVID-19 via public and private transportation in China. Travel Med Infect Dis. 2020;34:101626. 10.1016/j.tmaid.2020.101626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Kang D, Choi H, Kim JH, et al. : Spatial epidemic dynamics of the COVID-19 outbreak in China. Int J Infect Dis. 2020;96–102. 10.1016/j.ijid.2020.03.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Jia JS, Lu X, Yuan Y, et al. : Population flow drives spatio-temporal distribution of COVID-19 in China. Nature. 2020;582(7812):389–94. 10.1038/s41586-020-2284-y [DOI] [PubMed] [Google Scholar]
- 72. Adekunle IA, Onanuga A, Wahab O, et al. : Modelling spatial variations of coronavirus disease (COVID-19) in Africa. Sci Total Environ. 2020;729:138998. 10.1016/j.scitotenv.2020.138998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Desjardins M, Hohl A, Delmelle E: Rapid surveillance of COVID-19 in the United States using a prospective space-time scan statistic: Detecting and evaluating emerging clusters. Appl Geogr. 2020;118:102202. 10.1016/j.apgeog.2020.102202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Li H, Li H, Ding Z, et al. : Spatial statistical analysis of Coronavirus Disease 2019 (Covid-19) in China. Geospat Health. 2020;15(1). 10.4081/gh.2020.867 [DOI] [PubMed] [Google Scholar]
- 75. Ye L, Hu L: Spatiotemporal distribution and trend of COVID-19 in the Yangtze River Delta region of the People’s Republic of China. Geospat Health. 2020;15(1). 10.4081/gh.2020.889 [DOI] [PubMed] [Google Scholar]
- 76. Tang W, Liao H, Wang Z, et al. : The Changing Patterns of Coronavirus Disease 2019 (COVID-19) in China: A Tempogeographic Analysis of the Severe Acute Respiratory Syndrome Coronavirus 2 Epidemic. Clin Infect Dis. 2020;71(15):818–824. 10.1093/cid/ciaa423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Yang W, Deng M, Li C, et al. : Spatio-Temporal Patterns of the 2019-nCoV Epidemic at the County Level in Hubei Province, China. Int J Environ Res Public Health. 2020;17(7):2563. 10.3390/ijerph17072563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Miller LE, Bhattacharyya R, Miller AL: Spatial Analysis of Global Variability in Covid-19 Burden. Risk Manag Healthc Policy. 2020;13:519–522. 10.2147/RMHP.S255793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Thakar V: Unfolding Events in Space and Time: Geospatial Insights into COVID-19 Diffusion in Washington State during the Initial Stage of the Outbreak. ISPRS Int J Geoinf. 2020;9(6):382. 10.3390/ijgi9060382 [DOI] [Google Scholar]
- 80. Guliyev H: Determining the spatial effects of COVID-19 using the spatial panel data model. Spat Stat. 2020;100443. 10.1016/j.spasta.2020.100443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Irvine M, Coombs D, Skarha J, et al. : Modeling COVID-19 and Its Impacts on US Immigration and Customs Enforcement (ICE) Detention Facilities, 2020. J Urban Health. 2020;97(4):439–447. 10.1007/s11524-020-00441-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Bai S: Simulations of COVID-19 spread by spatial agent-based model and ordinary differential equations. International Journal of Simulation and Process Modelling. 2020;15(3):268–277. 10.1504/IJSPM.2020.10029411 [DOI] [Google Scholar]
- 83. Mollalo A, Vahedi B, Rivera KM: GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. Sci Total Environ. 2020;728:138884. 10.1016/j.scitotenv.2020.138884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Mollalo A, Rivera KM, Vahedi B: Artificial Neural Network Modeling of Novel Coronavirus (COVID-19) Incidence Rates across the Continental United States. Int J Environ Res Public Health. 2020;17(12):4204. 10.3390/ijerph17124204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Likassa HT: The Impacts of Covariates on Spatial Distribution of Corona Virus 2019 (COVID-19): What Do the Data Show through ANCOVA and MANCOVA?2020;4(2):141–148. Reference Source [Google Scholar]
- 86. Ren H, Zhao L, Zhang A, et al. : Early forecasting of the potential risk zones of COVID-19 in China's megacities. Sci Total Environ. 2020;729:138995. 10.1016/j.scitotenv.2020.138995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Kanga S, Meraj SG, Farooq M, et al. : Reporting the Management of COVID-19 Threat in India Using Remote Sensing and GIS-Based Approach. Geocarto Int. no. just-accepted:2020;1–6. 10.1080/10106049.2020.1778106 [DOI] [Google Scholar]
- 88. Liu Q, Sha D, Liu W, et al. : Spatiotemporal Patterns of COVID-19 Impact on Human Activities and Environment in Mainland China Using Nighttime Light and Air Quality Data. Remote Sens. 2020;12(10):1576. 10.3390/rs12101576 [DOI] [Google Scholar]
- 89. Tanveer H, Balz T, Cigna F, et al. : Monitoring 2011–2020 Traffic Patterns in Wuhan (China) with COSMO-SkyMed SAR, Amidst the 7th CISM Military World Games and COVID-19 Outbreak. Remote Sensing. 2020;12(10):1636. 10.3390/rs12101636 [DOI] [Google Scholar]
- 90. Chen CM, Jyan HW, Chien SC, et al. : Containing COVID-19 Among 627,386 Persons in Contact With the Diamond Princess Cruise Ship Passengers Who Disembarked in Taiwan: Big Data Analytics. J Med Internet Res. 2020;22(5):e19540. 10.2196/19540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Ekong I, Chukwu E, Chukwu M: COVID-19 Mobile Positioning Data Contact Tracing and Patient Privacy Regulations: Exploratory Search of Global Response Strategies and the Use of Digital Tools in Nigeria. JMIR Mhealth Uhealth. 2020;8(4):e19139. 10.2196/19139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Wang S, Ding S, Xiong L: A New System for Surveillance and Digital Contact Tracing for COVID-19: Spatiotemporal Reporting Over Network and GPS. JMIR Mhealth Uhealth. 2020;8(6):e19457. 10.2196/19457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Huang C, Xu X, Cai Y, et al. : Mining the Characteristics of COVID-19 Patients in China: Analysis of Social Media Posts. J Med Internet Res. 2020;22(5):e19087. 10.2196/19087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Rosenkrantz L, Schuurman N, Bell N, et al. : The need for GIScience in mapping COVID-19. Health & Place. 2020;67:102389. 10.1016/j.healthplace.2020.102389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Mo C, Tan D, Mai T, et al. : An analysis of spatiotemporal pattern for COIVD-19 in China based on space-time cube. J Med Virol. 2020;92(9):1587–1595. 10.1002/jmv.25834 [DOI] [PubMed] [Google Scholar]
- 96. Wang Z, Aydin O: Sensitivity Analysis for COVID-19 Epidemiological Models within a Geographic Framework.In Proceedings of the 1st ACM SIGSPATIAL International Workshop on Modeling and Understanding the Spread of COVID-19 (COVID-19).Association for Computing Machinery, New York, NY, USA,2020;11–14. 10.1145/3423459.3430755 [DOI] [Google Scholar]
- 97. Penn Healthcare: COVID-19 Hospital Impact Model for Epidemics (CHIME).2020. Reference Source [Google Scholar]
- 98. Ahasan R, Hossain MM: Leveraging GIS and spatial analysis for informed decision-making in COVID-19 pandemic. Health Policy Technol. 2021;10(1):7–9. 10.1016/j.hlpt.2020.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Hossain MM, Sharma R, Sultana A, et al. : Globalising artificial intelligence for improved clinical practice. Indian J Med Ethics. 2019;1–2. 10.20529/IJME.2019.074 [DOI] [PubMed] [Google Scholar]
- 100. Hossain MM, Tasnim T, Sharma R, et al. : Digital interventions for people living with non-communicable diseases in India: A systematic review of intervention studies and recommendations for future research and development. Digit Health. 2019;5:2055207619896153. 10.1177/2055207619896153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Ahasan R, Alam S, Chakraborty T, et al. : GIS in COVID-19 research.2020. 10.17605/OSF.IO/ZGMP8 [DOI] [PMC free article] [PubMed] [Google Scholar]