Abstract
Introduction
After surgery for distal femur fractures in elderly patients, weight-bearing is commonly restricted. Immediate non-restrictive weight-bearing might have beneficial effects. There are no randomized studies on the topic. The purpose of this study was to compare the functional outcome between immediate full weight-bearing (FWB) as tolerated and partial weight-bearing (PWB) during the first 8 weeks following plate fixation of distal femur fractures in elderly patients.
Methods
Patients aged 65 years or older with distal femur fractures of AO/OTA types 33 A2, A3, B1, B2, C1, and C2 were included. Exclusion criteria were impaired cognitive function, concomitant injuries, or inability to follow the postoperative regimen. Internal fixation was achieved with an anatomical lateral distal femur plate applied as a strictly bridge-plating construct. The primary outcome measure was the function index of the short musculoskeletal functional assessment (SMFA) after 52 weeks from injury.
Results
Thirty-two patients were randomized to FWB (n = 11) or PWB (n = 21). After 16 and 52 weeks, there were no differences in the mean SMFA function index between FWB and PWB (36 vs 43, P = .42 and 52 vs 40, P = .18, respectively) nor in the mean EuroQol 5-dimension index or range of motion (ROM). Overall, the SMFA function index was higher at 52 weeks compared with before injury (44 vs 30, P = .001) as was the mean bothersome index (37 vs 21, P = .011). There was no clear difference in the occurrence of adverse events between the treatment groups.
Conclusions
There were no differences in functional outcome, adverse events, or ROM between immediate FWB and PWB following plate fixation for a distal femur fracture in elderly patients. A distal femur fracture has a negative effect on the functional status of elderly patients that persists at least up to 1 year following injury.
Keywords: distal femur fracture, geriatric trauma, weight-bearing, plate fixation, bridge-plating, functional outcome, rehabilitation
Introduction
The incidence of distal femur fractures is highest amongst the elderly. 1 Operative treatment is generally preferred over non-operative treatment 2 with plate fixation being a commonly used technique.3-5 There is no consensus on the most appropriate regimen for postoperative weight-bearing. Restricted weight-bearing is commonly recommended, presumably as it is thought to decrease the risk of treatment failures, but this assumption has not yet been proven. 6 According to a systematic review and meta-analysis by Koso et al., 7 the risk of revision following operative treatment of distal femur fractures was 6.4% for delayed and nonunion, and 3.6% for implant failure. Meanwhile, failure rates, in terms of nonunion or mechanical failures, of 5–7% have been reported with non-restrictive weight-bearing.8-10 The risk of nonunion and mechanical failure has been suggested to decline with increased age.4,11,12 When considering the optimal postoperative weight-bearing regimen for elderly patients, the risk of nonunion and mechanical failure has to be weighed against the potentially detrimental effects of immobilization. Elderly patients with distal femur fractures are frail, as emphasized by their high 1-year mortality rate 13 and restricted weight-bearing might increase mortality and harm bone healing and post-rehabilitation mobility.14-17 Elderly patients often cannot restrict weight-bearing consistently.18-21 It is, therefore, not clear that restricting weight-bearing is the most suitable postoperative rehabilitation strategy for elderly patients following a distal femur fracture. There has in recent years been a growing interest for less restrictive weight-bearing22,23 but randomized controlled trials (RCTs) comparing non-restrictive and restrictive weight-bearing strategies for distal femur fractures in elderly patients have not been published.
The purpose of this study was to compare the functional outcome between immediate full weight-bearing (FWB) and partial weight-bearing (PWB) during the first 8 weeks postoperatively in elderly patients treated with strict bridge-plating according to a standardized protocol.
Material and Methods
Trial Design and Eligibility Criteria
This study was a single-center, parallel, two-arm, RCT conducted at the Sahlgrenska University Hospital, Gothenburg, Sweden. The inclusion criteria were a traumatic fracture of the distal part of the femur of AO/OTA types A2, A3, B1, B2, C1, and C2 24 and age 65 years or older. Exclusion criteria were concurrent injury or any pre-existing condition that could considerably affect rehabilitation, preinjury inability to ambulate independently with or without walking aids (crutches or walker), inability to communicate in the Swedish language, severe cognitive impairment (6 points or fewer) according to the Short Portable Mental Status Questionnaire 25 , and open fractures of types II and III according to the Gustilo–Andersson classification. 26
Surgery
Surgery was carried out within 72 hours after admission. All patients underwent surgery according to a standardized protocol based on pre-existing routine. Procedures were done by 1 of 7 consultant orthopedic trauma surgeons. The written protocol was made readily available to the involved surgeons who were also briefed on its content. The surgical protocol included positioning the patient on a traction table and reducing the fracture using closed techniques such as traction, with the fracture dorsally supported by a femur-support (Figure 1). The limited skin incision could be extended to allow additional open reduction when necessary. A stainless-steel LCP® Distal Femur Plate (Synthes™, Oberdorf, Switzerland) was introduced under the fascia lata using a minimally invasive technique. A 13- or 15-hole plate was used depending on the length of the femur (Figure 2). The plate was fixed to bone with locking screws. Distally 5 bi-cortical screws were used. Proximally 4 screws were inserted through stab incisions, the most proximal of these was mono-cortical but the remaining screws were bi-cortical. Only a strictly bridge-plating construct was allowed, no screws or cerclage wires were used across the fracture site. A biplanar image intensifier was used to verify adequate fracture reduction and hardware positioning.
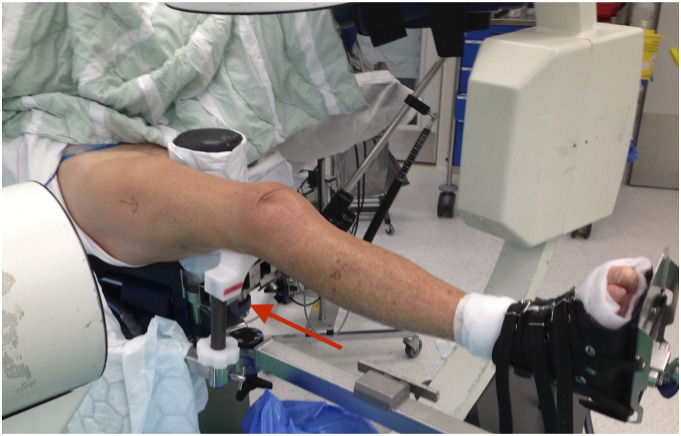
Figure 1.
The patient in the supine position on a traction table. The arrow indicates the femur-supporting device.
Figure 2.
A long spiral fracture of the distal femur fixed with a 15-hole plate. The osteosynthesis is done according to a strictly bridge-plating concept which results in a long working length. The image is digitally edited by merging 2 x-ray images.
Intervention: Full or Partial Weight-Bearing
Patients were randomized to either immediate FWB or PWB for the first 8 weeks postoperatively. The patients in both intervention groups received physiotherapy according to routine, including exercises that could be carried out in bed or while standing. They received thorough instructions from a physiotherapist on how to follow the allocated intervention. In the PWB group, weight-bearing was set to approximately 30% of body weight. Using a bathroom scale together with real-time visual feedback about weight-bearing, the physiotherapist trained the patient during the hospital stay. In the FWB group, patients could directly bear weight as tolerated. Patients in both groups could use whatever walking aids they needed postoperatively.
Assessment of Outcome
Patients were followed up at 8, 16, and 52 weeks. The primary outcome measure was the function index of the short musculoskeletal functional assessment (SMFA).27,28 The SMFA is a self-reported instrument which has been found to be valid for assessing the impact of musculoskeletal conditions on functional status. 29 The SMFA is composed of 2 indices: the bothersome index and function index. The latter has 4 categories: daily activities, emotional status, arm and hand function, and mobility. The range runs from 0 to 100 in each category and a higher score represents a greater impairment. Secondary outcome measures were the categories of the SMFA and the bothersome index, pain assessed in mm on a visual analog scale (VAS), ROM of the knee in degrees assessed with a goniometer, and the three-level EuroQol 5-dimension (EQ-5D) instrument. 30 The EQ-5D index was calculated as described by Dolan. 31 Preinjury patient-reported outcome was captured using the recall method referring to patients’ functional status during the last 7 days prior to the injury. Preinjury function was also assessed by the Function Recovery Score 32 and a basic three-level classification regarding general medical health and social situation. ROM was assessed by the first author who was not blinded to treatment allocation. The “time-up-go” (TUG) test at 16 weeks 33 was conducted by an experienced senior physiotherapist who was blinded to treatment allocation.
Sample Size
An estimate of the minimal important difference was not available for the SMFA function index before initiating the study. 29 A SD of 15 was considered reasonable. 34 A group size of 35 patients in each group was aimed for and would detect a 10-point difference with 80% power and alpha set at .05.
Randomization
Patients were randomized immediately after surgery. This option was chosen since randomizing applied to the postoperative treatment selection. Randomization prior to surgery would have entailed a risk of the surgical procedure being adapted to the allocated treatment group.
Statistical Methods
Analysis was performed in SPSS® Statistics version 26 (IBM®, Armonk, NY, USA). Continuous data are presented as mean and SD. For comparisons between groups, an independent samples t-test was used for continuous variables and Fisher’s exact test for categorical variables. For comparisons between different timepoints, a paired samples t-test was used. Statistical significance was set at P > .05.
Clinical Trial Registry
This study was entered (registration number 115861) on December 4, 2012, in the national clinical trial registry; The Healthcare Committee, Region Västra Götaland, Sweden.
Results
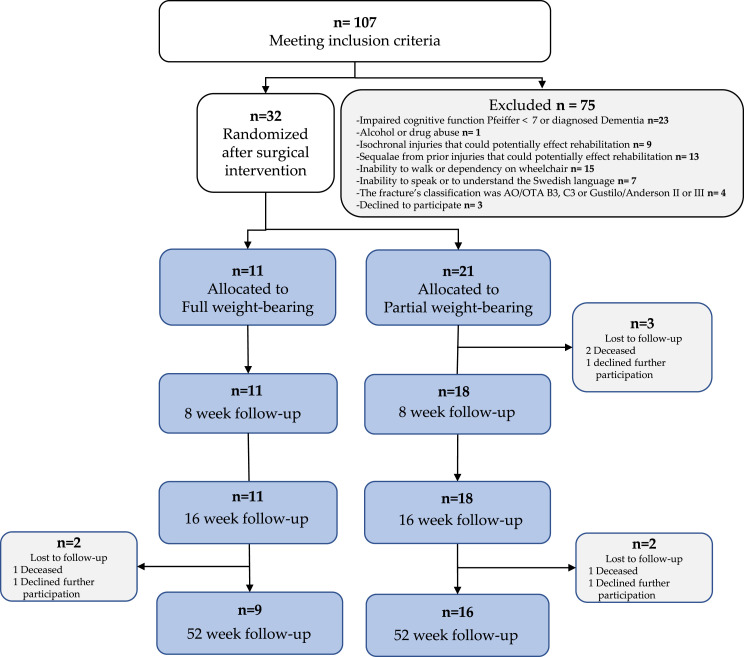
Between January 2013 and June 2016, 32 patients were enrolled in this study. Eleven patients were randomized to FWB and 21 patients to PWB, (Figure 3). Two patients in the PWB group died and 1 was lost to follow-up prior to follow-up at 8 weeks and were excluded from further analysis. There were thus 11 patients in the FWB group and 18 patients in the PWB group with data available from follow-ups who were included in the analysis.
Figure 3.
Flowchart showing the pathway of the patients through the study.
There were no statistically significant differences in demographic and clinical characteristics between the treatment groups except that the mean duration of surgery in minutes was shorter in the FWB group compared to the PWB group (Table 1).
Table 1.
Demographic and Treatment-Related Data.
| FWB | PWB | ||
|---|---|---|---|
| (n =11) | (n = 18) | P-value | |
| Age in years, mean (SD) | 79.2 (9) | 81.3 (8) | .55 a |
| Sex, n (%) | 1.0 b | ||
| Women | 10 (91) | 15 (83) | |
| BMI, mean (SD) | 27.6 (4.6) | 25.2 (4.2) | .15 a |
| ASA class, n (%) | .64 b | ||
| ASA I | 2 (18) | 1 (6) | |
| ASA II | 5 (45) | 8 (44) | |
| ASA III | 4 (36) | 9 (50) | |
| FRS, n (%) | .48 b | ||
| 90–100% | 9 (82) | 13 (72) | |
| 80–89% | 2 (18) | 1 (6) | |
| 70–79% | 0 (0) | 2 (11) | |
| Missing | 2 (11) | ||
| Medical general condition, n (%) | 1.0 b | ||
| A; No other injury or illness | 3 (27) | 4 (22) | |
| B; Isochronal injury or illness, not affecting rehabilitation | 4 (36) | 6 (33) | |
| C; Isochondral injury or illness, possibly affecting rehabilitation | 4 (36) | 8 (44) | |
| Social situation, n (%) | 1.0 b | ||
| Con with relatives, n (%) | |||
| A; More than once a week | 10 (91) | 15 (83) | |
| B; More than once a month | 1 (9) | 3 (17) | |
| C; Less that once a month | 0 (0) | 0 (0) | |
| Surgery, mean (SD) | |||
| Hours from injury to surgery | 34 (13) | 37 (21) | .61 a |
| Duration of surgery in minutes | 83 (21) | 104 (22) | .022 a |
| Blood loss in ml | 268 (184) | 275 (132) | .90 a |
ASA, American Society of Anesthesiologists Classification; BMI, Body mass index; FWB, Full Weight-Bearing; FRS, Function Recovery Scale; PWB, Partial Weight-Bearing.
aIndependent Sample t-test.
bFischer’s exact test.
Overall, the distribution of AO/OTA fracture types was similar in both groups (Table 2). Four patients in each group had extra-articular type A fracture that extended substantially into the shaft. The occurrence of peri-implant fractures was high, 64% in the FWB group and 72% in the PWB group (Table 3).
Table 2.
AO/OTA Fracture Classification.
| FWB | PWB | |
|---|---|---|
| (n) | (n) | |
| AO/OTA fracture type | ||
| A, Extra-articular | 5 | 7 |
| B, Partial articular | 1 | 0 |
| C, Complete articular | 1 | 3 |
| V.3 B 1, Bed of or around stable implant TKR | 2 | 4 |
| V.3 C, Proximal to the implant and cement mantle TKR | 1 | 0 |
| IV.3 C a, Distal to a THR | 0 | 1 |
| V.3 D, Between THR and TKR, close to the knee | 1 | 3 |
AO/OTA, Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association; TKR, Total Knee Replacement; THR, Total Hip Replacement.
Table 3.
Distribution of Combinations of Peri-Implant Fractures.
| FWB | PWB | |
|---|---|---|
| (n) | (n) | |
| Peri-implant fractures | ||
| Single implant | ||
| THR | 0 | 3 |
| TKR | 2 | 4 |
| Hip ORIF | 3 | 3 |
| 2 implants | ||
| THR and TKR | 1 | 3 |
| TKR and Hip ORIF | 1 | 0 |
FWB, Full Weight-Bearing; PWB, Partial Weight-Bearing; THR, Total Hip Replacement; TKR, Total Knee Replacement; ORIF, Open reduction and internal fixation.
There were no statistically significant differences between the treatment groups in the means of the SMFA indices, EQ-5D index (Table 4), or ROM (Table 5) at any time point. When analyzing patients from both treatment groups with available data (n = 18) together, SMFA function and bothersome indices were higher at 1-year follow-up than before the injury (44 vs 30, P = .001 and 37 vs 21, P = .011, respectively).
Table 4.
Results of PROMs (EQ-5D and SMFA) at different time points (Preinjury, 8 weeks, 16 weeks and 52 weeks).
| Preinjury | 8 weeks | 16 weeks | 52 weeks | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FWB | PWB | FWB | PWB | FWB | PWB | FWB | PWB | |||||
| (n = 10) | (n = 18) | P-value | (n = 11) | (n = 12) | P-value | (n = 9) | (n = 15) | P-value | (n = 7) | (n = 12) | P-value | |
| EQ-5D, mean (SD) | ||||||||||||
| EQ-5D index | .72 (.30) | .63 (.32) | .64 | .55 (.23) | .51 (.28) | .70 | .59 (.29) | .54 (.23) | .66 | .61 (.20) | .64 (.20) | .72 |
| EQ-5D VAS | 74 (21) | 78 (15) | .45 | 53 (23) | 52 (24) | .92 | 71 (20) | 56 (23) | .15 | 54 (16) | 65 (21) | .32 |
| SMFA, mean (SD) | ||||||||||||
| Function index | 29 (23) | 35 (21) | .45 | 45 (17) | 47 (17) | .78 | 36 (23) | 43 (20) | .42 | 52 (19) | 40 (16) | .18 |
| Daily activity | 37 (33) | 44 (28) | .57 | 59 (23) | 70 (24) | .30 | 47 (28) | 58 (30) | .37 | 62 (28) | 51 (26) | .42 |
| Emotional status | 27 (24) | 31 (18) | .58 | 36 (18) | 43 (15) | .38 | 31 (23) | 39 (18) | .34 | 46 (11) | 41 (19) | .59 |
| Arm and hand function | 19 (23) | 24 (25) | .64 | 27 (26) | 20 (20) | .51 | 19 (27) | 19 (22) | .99 | 37 (29) | 19 (17) | .11 |
| Mobility | 30 (20) | 37 (20) | .31 | 51 (16) | 50 (21) | .85 | 41 (20) | 50 (22) | .32 | 50 (25) | 44 (18) | .54 |
| Bothersome index | 19 (21) | 28 (29) | .31 | 38 (18) | 41 (18) | .71 | 26 (21) | 37 (22) | .23 | 41 (17) | 35 (19) | .60 |
EQ-5D, EuroQol 5-Dimensions; FWB, Full Weight-Bearing; PROMs, Patient reported outcome measures; PWB, Partial Weight-Bearing; SMFA, Short musculoskeletal function assessment; VAS, Visual analog scale.
Table 5.
Range of Motion at 8, 16, and 52 weeks of Follow-Up.
| 8 weeks | 16 weeks | 52 weeks | |||||||
|---|---|---|---|---|---|---|---|---|---|
| FWB (n = 11) | PWB (n = 17) | P-value | FWB (n = 10) | PWB (n = 16) | P-value | FWB (n = 9) | PWB (n = 13) | P-value | |
| Range of knee motion in degrees, median (SD) | |||||||||
| Active flexion | 105 (14) | 100 (24) | .55 | 110 (10) | 106 (21) | .66 | 110 (18) | 110 (19) | .96 |
| Active extension | 0 (3) | 0 (5) | .37 | 2 (3) | 3 (5) | .32 | 1 (2) | 2 (6) | .49 |
FWB, Full Weight-Bearing; PWB, Partial Weight-Bearing.
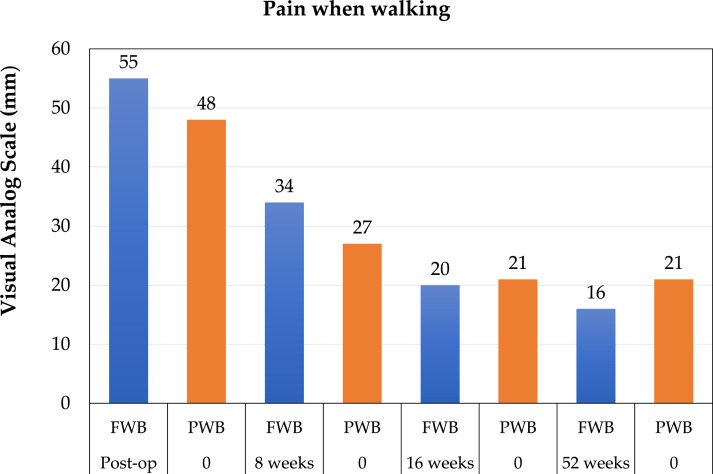
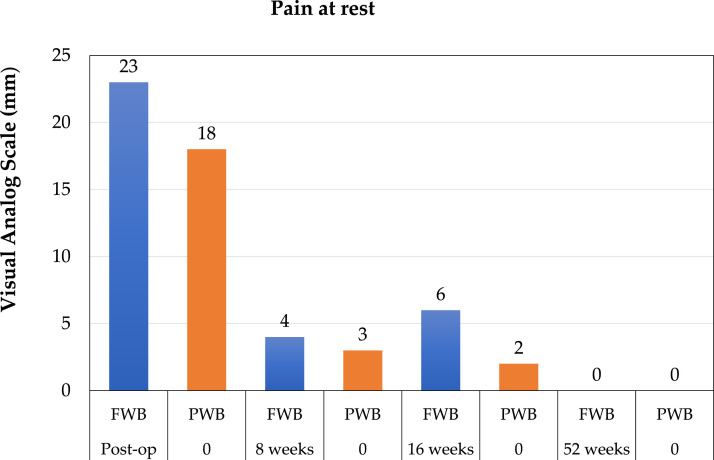
At the 1-year follow-up, there were no statistically significant differences between the treatment groups in mean pain (VAS) when walking (Figure 4) or at rest (Figure 5). The mean VAS scores were highest postoperatively but gradually declined over time in both treatment groups.
Figure 4.
Reported pain when walking, measured by Visual Analog Scale (VAS) during follow-up. FWB, Full Weight-Bearing; PWB, Partial Weight-Bearing.
Figure 5.
Reported pain while resting, measured by Visual Analog Scale (VAS) during follow-up. FWB, Full Weight-Bearing; PWB, Partial Weight-Bearing.
Results of the TUG test were available for 7 patients in each treatment group at 16 weeks of follow-up. Patients in the FWB group were somewhat faster compared to the PWB group (20.3 vs 25.4 seconds, respectively), although the difference was not statistically significant, P = .34. There was no difference in the mean length of hospital stay between the FWB group (14.6 days, SD 6.6) and the PWB group (14.3 days, SD 5.7), P = .87. However, all the patients in the FWB were discharged directly to their homes, whereas 3 patients in the PWB group were discharged to a permanent nursing home.
Adverse Events
There were few adverse events in overall terms and there was no clear difference in their pattern between the treatment groups (Table 6). There was one death in the FWB group and 3 in the PWB group. One patient in the PWB group died of pulmonary embolism while still in hospital, the other deaths occurred at 21, 182, and 364 days after surgery, none of them were directly related to the femur fracture or its treatment.
Table 6.
Patients With Adverse Advents.
| FWB (n) | PWB (n) | Treatment | Timepoint | Outcome | |
|---|---|---|---|---|---|
| Adverse events requiring major reoperation | |||||
| Proximal screw breakage adjacent to THR | 0 | 1 | Revision of proximal fixation with LAP | 4 months | Union |
| Deep infection | 0 | 1 | DAIR | 2 months | Infection eradication and union |
| Delayed union, due to undetected atypical fracture | 1 | 0 | Initially non-operative treatment but ultimately addition of lag screws | 14 months | Union |
| Adverse events requiring minor reoperation | |||||
| Independent new fracture of the lateral femur condyle, 1 week postoperatively | 0 | 1 | Screw removal distally | 8 months | United distal femur fracture, poor knee function |
| Screw tip protruding through the medial cortex of the femur condyle | 1 | 1 | Exchange to shorter screws | 2 and 5 months | Pain and discomfort subsided |
DAIR Debridement Antibiotics Implant Retention; FWB, Full Weight-Bearing; LAP, Lateral Attachment Plate; PWB, Partial Weight-Bearing; THR, Total Hip Replacement.
Discussion
The main finding of this randomized study is that, for elderly patients treated with plate fixation for a traumatic distal femur fracture, there was no difference in patient-reported outcome between the patients who were allowed immediate full weight-bearing and those who were assigned PWB during the initial 8 weeks after surgery.
To the best of our knowledge, no previous randomized studies compare different weight-bearing strategies for distal femur fractures. The results of the current study are, however, consistent with previous non-randomized studies which have not demonstrated a clear advantage of any weight-bearing strategy in terms of function35,36 or the occurrence of complications.8-(10)- PWB was the standard treatment locally when the study was started and was therefore chosen as the treatment with which to compare FWB. The weight-bearing strategies reported by previous studies vary considerably in the loading allowed but are collectively referred to here as those with restrictive or non-restrictive weight-bearing.
Two non-randomized comparative studies by Bruggers et al. 35 and Lieder et al. 36 found no difference in the results of Patient Reported Outcomes (PRO) between non-restrictive and restrictive weight-bearing strategies, consistent with the results of the current study. Lieder et al. compared weight-bearing as tolerated (n = 56) and touch-down weight-bearing (n = 79) following internal fixation of patients 60 years and older with type A distal femur fractures. The degree of weight-bearing was at the discretion of the surgeon. The presence of factors associated with an increased risk of failure, such as fracture comminution 37 and mal-reduction 38 might have affected group allocation which could explain the uneven distribution of fixation techniques between the treatment groups. In the weight-bearing as tolerated group, 50 of 56 were treated with an intramedullary nail but 46 of 79 in the touch-down weight-bearing group with a plate. However, Lieder et al. found no differences between the treatment groups in the mean Patient-Reported Outcomes Measurement Information System (PROMIS) scores, data which were collected by telephone.
Knee-specific PROMs might detect potential differences between weight-bearing strategies better than more generic instruments, such as the PROMIS or the SMFA used in the current study. Using the knee-specific Oxford knee score Bruggers et al. however, found no difference in mean scores at 6 weeks, 12 weeks, or 6 months between weight-bearing as tolerated (n = 11) and protective/non-weight-bearing (n = 35) in patients over 64 years of age treated with plate fixation. Again, treatment allocation was surgeon-based and potentially affected by risk factors for failure37,39 since patients with diabetes were completely absent and patients with overweight underrepresented in the weight-bearing as tolerated group.
The mean scores of the SMFA function index were between 36 and 52 points after 4 and 12 months of follow-up in both treatment groups, indicating significant impairment. These values are comparable to a mean of 44 points on the SMFA function index reported by Shulman et al., 40 based on patients aged 65 years or older treated with a plate or intramedullary nail for AO type B or C femur fractures after 2.1 years of follow-up. These values, like those in the current study, imply considerable impairment. In the current study, both SMFA function and bothersome indices indicated significantly worse function at 1-year follow-up than before the injury. These findings emphasize that sustaining a distal femur fracture often substantially affects the life of elderly patients.
The main concern with nonrestrictive weight-bearing is a potential increase in the risk of failure in terms of nonunion with or without implant breakage. In a systematic review and meta-analysis on distal femur fractures, Koso et al., 7 reported an overall risk of revision for nonunion, delayed union, and mechanical failure of 10%. In another meta-analysis, Yoon et al. 41 estimated that approximately 5% of patients with distal femur fractures treated with locked compression plates or intramedullary nails develop nonunion. In the current study, there were few adverse events overall (Table 6), and no clear difference between FWB and PWB. This is consistent with 3 previous studies, which have found no increase in the occurrence of treatment failure for non-restrictive as compared to restrictive weight-bearing strategies (Table 7).10,36 Furthermore, there is no clear difference between cohort studies using non-restrictive weight-bearing8,9,42-44 and restrictive weight-bearing45-48 after internal fixation of distal femoral fractures, and treatment failures occurring with both types of strategies (Table 8).
Table 7.
Overview of Studies Comparing Restrictive and Non-restrictive Weight-Bearing Strategies for Distal Femur Fractures.
| First author | Year | Included in analysis (n) | Weight-bearing strategy (n) | Mean age (years) | Treatment (n) | AO classification (n) | Follow-up (months) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-restrictive | Restrictive | Treatment failure | ||||||||||||||||
| As tolerated | Early | Touch- down | Protective/non | Non | Plate | RIMN | A | B | C | Non-restrictive (n and %) | Restrictive (n and %) | |||||||
| Lieder et al. 36 | 2021 | 135 | 56 | 79 | 76 | 52 | 83 | 135 | 0 | 0 | 21 | 6 | 11% | 11 | 14% | |||
| Bruggers et al. 35 | 2020 | 46 | 11 | 35 | 75 | 46 | 37 | 2 | 7 | 12 | 0 | 2 | 6% | |||||
| Consigliere et al. 10 | 2019 | 51 | 19 | 32 | 64 | 51 | 13 | 3 | 20 | 3 | 0 | 2 | 6% | |||||
AO, Arbeitsgemeinschaft für Osteosynthesefragen; RIMN, reamed intramedullary nail;
Table 8.
Overview of results of cohort studies on distal femur fractures which specify type of weight-bearing strategy used.
| First author | Year | Included in analysis (n) | Weight-bearing strategy (n) | Mean age (years) | Treatment (n) | AO classification (n) | Follow-up (months) | Treatment failures (n and %) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-restrictive | Restrictive | ||||||||||||||
| As tolerated | Partial | Touch- down | Non | Plate | RIMN | A | B | C | |||||||
| Non-restrictive weight-bearing | |||||||||||||||
| Poole et al. 8 | 2017 | 127 | 107 | 73 | 127 | 107 | 4 | 16 | 4b | 5% | |||||
| Smith et al. 9 | 2016 | 54a | 54 | 74 | 54 | 12 | 4c | 7% | |||||||
| Doshi et al. 42 | 2013 | 24 | 24 | 73 | 24 | 20 | 1 | 3 | 15 | 0 | |||||
| Kanakaris et al. 44 | 2019 | 36 | 36 | 77 | 36 | 9 | 5 | 14% | |||||||
| Giddie et al. 43 | 2015 | 54 | 54 | 81 | 54 | 54 | 4 | 0 | |||||||
| Restrictive weight-bearing | |||||||||||||||
| Tank et al. 48 | 2016 | 67 | 67 | 55 | 67 | 16 | 1 | 50 | 10 | 11 | 16% | ||||
| Loosen et al. 46 | 2019 | 50 | 3 | 19 | 28 | 50 | 40 | 4 | 8 | 0 | |||||
| Khursheed et al. 45 | 2015 | 25 | 25 | 67 | 25 | 25 | 0 | ||||||||
| Patterson et al. 47 | 2020 | 78 | 78 | 60 | 78 | 38 | 41 | 25 | 3 | 4% | |||||
AO, Arbeitsgemeinschaft für Osteosynthesefragen; RIMN, Reamed intramedullary nail.
a54 fractures in 52 patients.
b4 of 85 with available data.
c3 implant failures and 1 nonunion.
In addition to potentially affecting function, different weight-bearing strategies might have other implications although data concerning distal femur fractures specifically is limited. From other studies it is, however, known that loading has a positive effect on fracture healing, 17 and muscle disuse has been found to cause rapid muscle atrophy and potentially loss of functional health.49,50 Studies on hip fractures have found that early weight-bearing decreases mortality15,16 and the occurrence of complications such as pneumonia 51 and pressure ulcers 15 while non-weight-bearing status compromises functional level. 52 It appears reasonable to infer that this also applies for distal femoral fractures 53 since, despite differences in biomechanics and treatment-related issues, patients with proximal femur fractures have demographics similar to those with distal femur fractures concerning age, co-morbidities, and risk of mortality.54,55
Summarizing the literature regarding the effect of weight-bearing on the outcome of distal femur fractures in elderly patients is difficult. This is in part due to the risk of bias and the limited number of patients in both the current and previous studies. Lieder et al. estimated that, based on their data, 574 patients would be required to detect a difference in the occurrence of major adverse events with a power of .8. 36 Interpretation of the literature would be facilitated by standardized weight-bearing protocols and consistent terminology. In addition, it would be useful if all studies on distal femur fractures would specify the weight-bearing strategy used, which is currently not the case.12,56-59
Based on available knowledge regarding the effects of restrictive and non-restrictive weight-bearing discussed in the preceding paragraphs, it seems reasonable to suggest non-restrictive weight-bearing for elderly patients with distal femur fractures. Non-restrictive weight-bearing might, however, not be appropriate for all patients. Therefore, patient factors, such as obesity and open fractures which have been associated with an increased risk of treatment failure,11,39 need to be considered when choosing weight-bearing strategy. Drawing firm conclusions about the most appropriate weight-bearing strategy for elderly patients following distal femur fractures must be deferred until large trials comparing restrictive and non-restrictive weight-bearing are available.
Limitations
Including eligible patients and implementing the study proved to be more difficult than expected. Unfortunately, the treatment groups were of unequal size, attributable to treatment allocation being done with simple randomization. Based on the inclusion rate and interim results, it was clear that obtaining a sizable cohort of patients would not be possible to accomplish within a reasonable timeframe. The study was therefore terminated. Unfortunately, the rate of discontinuation of RCTs may be as high as 43% with slow recruitment being the most common reason for discontinuation. 60 There are, however, no previous RCTs available on the topic and the data can be used for future meta-analysis and planning of future trials. There were only 4 patients with complete articular fractures which needs to be considered when interpreting the results. The follow-up did not extend beyond 1 year, in part as the advanced age and co-morbidities in the study population make a longer follow-up difficult. In addition, it appears plausible that a potential difference in function would make itself known during the first year of follow-up.
Conclusion
In this RCT, no difference was detected in functional outcome between FWB as tolerated and PWB during the first 8 weeks postoperatively in patients aged 65 years or older, treated with plate fixation for distal femur fractures. Treatment failures were not overrepresented in the FWB group. These results are consistent with previous non-randomized studies. Both the SMFA function and bothersome indices indicated worse function at 52 weeks as compared to before the injury, emphasizing the lasting impact distal femur fractures can have on the life of elderly patients.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research received no external funding. None of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article.
Clinical Trial Registry: This study was entered (registration number 115861) on December 4, 2012, in the national clinical trial registry; The Healthcare Committee, Region Västra Götaland, Sweden.
Ethical Considerations: This study was approved by the Regional Ethical Review Board in Gothenburg (entry number 008-12). All patients provided written informed consent to participate in the study.
ORCID iDs
Martin Paulsson https://orcid.org/0000-0002-7104-2262
Eythor Jonsson https://orcid.org/0000-0002-1975-1096
References
- 1.Elsoe R, Ceccotti AA, Larsen P. Population-based epidemiology and incidence of distal femur fractures. Int Orthop. 2018;42(1):191-196. doi: 10.1007/s00264-017-3665-1. [DOI] [PubMed] [Google Scholar]
- 2.Butt MS, Krikler SJ, Ali MS. Displaced fractures of the distal femur in elderly patients. Operative versus non-operative treatment. J Bone Joint Surg Br. 1996;78-B(1):110-114. [PubMed] [Google Scholar]
- 3.Nyholm AM, Palm H, Kallemose T, Troelsen A, Gromov K, DFDB collaborators . No association between surgical delay and mortality following distal femoral fractures. A study from the Danish fracture database collaborators. Injury. 2017;48(12):2833-2837. doi: 10.1016/j.injury.2017.10.022. [DOI] [PubMed] [Google Scholar]
- 4.Smith JRA, Halliday R, Aquilina AL, Morrison RJM, Yip GCK, McArthur J, et al. Distal femoral fractures: The need to review the standard of care. Injury. 2015;46(6):1084-1088. doi: 10.1016/j.injury.2015.02.016. [DOI] [PubMed] [Google Scholar]
- 5.Vestergaard V, Pedersen AB, Tengberg PT, Troelsen A, Schrøder HM. 20-year trends of distal femoral, patellar, and proximal tibial fractures: A Danish nationwide cohort study of 60,823 patients. Acta Orthop. 2020;91(1):109-114. doi: 10.1080/17453674.2019.1698148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Distal Femur (Thighbone) Fractures of the Knee. Orthoinfo. https://orthoinfo.aaos.org/en/diseases--conditions/distal-femur-thighbone-fractures-of-the-knee/. Accessed March 17, 2021.
- 7.Koso RE, Terhoeve C, Steen RG, Zura R. Healing, nonunion, and re-operation after internal fixation of diaphyseal and distal femoral fractures: A systematic review and meta-analysis. Int Orthop. 2018;42(11):2675-2683. doi: 10.1007/s00264-018-3864-4. [DOI] [PubMed] [Google Scholar]
- 8.Poole WEC, Wilson DGG, Guthrie HC, Bellringer SF, Freeman R, Guryel E, et al. ‘Modern’ distal femoral locking plates allow safe, early weight-bearing with a high rate of union and low rate of failure. Bone Joint J. 2017;99-B(7):951-957. doi: 10.1302/0301-620x.99b7.Bjj-2016-0585.R1. [DOI] [PubMed] [Google Scholar]
- 9.Smith WR, Stoneback JW, Morgan SJ, Stahel PF. Is immediate weight bearing safe for periprosthetic distal femur fractures treated by locked plating? A feasibility study in 52 consecutive patients. Patient Saf Surg. 2016;10:26. doi: 10.1186/s13037-016-0114-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Consigliere P, Iliopoulos E, Ads T, Trompeter A. Early versus delayed weight bearing after surgical fixation of distal femur fractures: A non-randomized comparative study. Eur J Orthop Surg Traumatol. 2019;29(8):1789-1794. doi: 10.1007/s00590-019-02486-4. [DOI] [PubMed] [Google Scholar]
- 11.Ricci WM, Streubel PN, Morshed S, Collinge CA, Nork SE, Gardner MJ. Risk factors for failure of locked plate fixation of distal femur fractures: An analysis of 335 cases. J Orthop Trauma. 2014;28(2):83-89. doi: 10.1097/BOT.0b013e31829e6dd0. [DOI] [PubMed] [Google Scholar]
- 12.Wenger D, Andersson S. Low risk of nonunion with lateral locked plating of distal femoral fractures-A retrospective study of 191 consecutive patients. Injury. 2019;50(2):448-452. doi: 10.1016/j.injury.2018.10.039. [DOI] [PubMed] [Google Scholar]
- 13.Wolf O, Mukka S, Ekelund J, Möller M, Hailer NP. How deadly is a fracture distal to the hip in the elderly? An observational cohort study of 11,799 femoral fractures in the Swedish Fracture Register. Acta Orthop. 2020;92:40-46. doi: 10.1080/17453674.2020.1831236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pfeufer D, Zeller A, Mehaffey S, Böcker W, Kammerlander C, Neuerburg C. Weight-bearing restrictions reduce postoperative mobility in elderly hip fracture patients. Arch Orthop Trauma Surg. 2019;139(9):1253-1259. doi: 10.1007/s00402-019-03193-9. [DOI] [PubMed] [Google Scholar]
- 15.Warren J, Sundaram K, Anis H, McLaughlin J, Patterson B, Higuera CA, et al. The association between weight-bearing status and early complications in hip fractures. Eur J Orthop Surg Traumatol. 2019;29(7):1419-1427. doi: 10.1007/s00590-019-02453-z. [DOI] [PubMed] [Google Scholar]
- 16.Atzmon R, Drexler M, Ohana N, Nyska M, Palmanovich E, Dubin J. The effect of postoperative weight-bearing status on mortality rate following proximal femoral fractures surgery [published ahead of print January 8, 2004]. Arch Orthop Trauma Surg. doi: 10.1007/s00402-020-03721-y. [DOI] [PubMed]
- 17.Windolf M, Ernst M, Schwyn R, Arens D, Zeiter S. The relation between fracture activity and bone healing with special reference to the early healing phase - A preclinical study. Injury. 2021;52(1):71-77. doi: 10.1016/j.injury.2020.10.050. [DOI] [PubMed] [Google Scholar]
- 18.Kammerlander C, Pfeufer D, Lisitano LA, Mehaffey S, Böcker W, Neuerburg C. Inability of older adult patients with hip fracture to maintain postoperative weight-bearing restrictions. J Bone Joint Surg Am. 2018;100(11):936-941. doi: 10.2106/jbjs.17.01222. [DOI] [PubMed] [Google Scholar]
- 19.Dabke HV, Gupta SK, Holt CA, O’Callaghan P, Dent CM. How accurate is partial weightbearing? Clin Orthop Relat Res 2004;421:282-286. doi: 10.1097/01.blo.0000127116.13377.65. [DOI] [PubMed] [Google Scholar]
- 20.Vasarhelyi A, Baumert T, Fritsch C, Hopfenmüller W, Gradl G, Mittlmeier T. Partial weight bearing after surgery for fractures of the lower extremity - Is it achievable? Gait Posture. 2006;23(1):99-105. doi: 10.1016/j.gaitpost.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 21.Kärrholm MTJ, Karrholm J. Low effectiveness of prescribed partial weight bearing. Continuous recording of vertical loads using a new pressure-sensitive insole. J Rehabil Med. 2001;33(1):42-46. doi: 10.1080/165019701300006533. [DOI] [PubMed] [Google Scholar]
- 22.Trompeter A. A call to arms: It’s time to bear weight!. Bone Joint J. 2020;102-b(4):403-406. doi: 10.1302/0301-620x.102b4.Bjj-2019-1482.R1. [DOI] [PubMed] [Google Scholar]
- 23.National Institute for Health Care and Excellance Guidance . Fractures (Non-complex): Assessment and Management. London: National Institute for Health and Care Excellence (UK). http://www.nice.org.uk (2016). [Google Scholar]
- 24.Meinberg E, Agel J, Roberts C, Karam M, Kellam J. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32(suppl 1):S1-S10. doi: 10.1097/BOT.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 25.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficits in the elderly. J Am Geriatr Soc. 1975;23:433-441. [DOI] [PubMed] [Google Scholar]
- 26.Gustilo R, Anderson J. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58(4):453-458. [PubMed] [Google Scholar]
- 27.Swiontkowski MF, Engelberg R, Martin DP, Agel J. Short musculoskeletal function assessment questionnaire: Validity, reliability and responsiveness. J Bone Joint Surg Am. 1999;81, 1245-1260. doi: 10.2106/00004623-199909000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Ponzer S, Skoog A, Bergström G. The Short Musculoskeletal Function Assessment Questionnaire (SMFA) cross-cultural adaptation, validity, reliability and responsiveness of the Swedish SMFA (SMFA-Swe). Acta Orthop Scand. 2003;74(6):756-763. doi: 10.1080/00016470310018324. [DOI] [PubMed] [Google Scholar]
- 29.Bouffard J, Bertrand-Charette M, Roy J-S. Psychometric properties of the Musculoskeletal Function Assessment and the Short Musculoskeletal Function Assessment: A systematic review. Clin Rehabil. 2016;30(4):393-409. doi: 10.1177/0269215515579286. [DOI] [PubMed] [Google Scholar]
- 30.Devlin NJ, Brooks R. EQ-5D and the EuroQol group: Past, present and future. Appl Health Econ Health Policy. 2017;15(2):127-137. doi: 10.1007/s40258-017-0310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35(11):1095-1108. [DOI] [PubMed] [Google Scholar]
- 32.Zuckerman JD, Koval KJ, Aharonoff GB, Skovron ML. A functional recovery score for elderly hip fracture patients: II. Validity and reliability. J Orthop Trauma. 2000;14(1):26-30. [DOI] [PubMed] [Google Scholar]
- 33.Bohannon RW. Reference values for the timed up and go test: A descriptive meta-analysis. J Geriatr Phys Ther. 2006;29(2):64-68. [DOI] [PubMed] [Google Scholar]
- 34.el Moumni M, Voogd EH, ten Duis HJ, Wendt KW. Long-term functional outcome following intramedullary nailing of femoral shaft fractures. Injury. 2012;43(7):1154-1158. doi: 10.1016/j.injury.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 35.Bruggers JJK, Tanner S, Israel H, Dawson S, Cannada L. Early weight bearing after distal femur fractures in the elderly: A prospective, cohort pilot study. J Orthop Exp Innovation 2020;(May). https://journaloei.scholasticahq.com/article/12620. [Google Scholar]
- 36.Lieder CM, Gaski GE, Virkus WW, Kempton LB. Is immediate weight-bearing safe after single implant fixation of elderly distal femur fractures? J Orthop Trauma. 2021;35(1):49-55. doi: 10.1097/BOT.0000000000001882. [DOI] [PubMed] [Google Scholar]
- 37.Wang MT, An VVG, Sivakumar BS. Non-union in lateral locked plating for distal femoral fractures: A systematic review. Injury. 2019;50(11):1790-1794. doi: 10.1016/j.injury.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 38.Peschiera V, Staletti L, Cavanna M, Saporito M, Berlusconi M. Predicting the failure in distal femur fractures. Injury. 2018;49(suppl 3):S2–S7. doi: 10.1016/j.injury.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 39.Rodriguez EK, Boulton C, Weaver MJ, Herder LM, Morgan JH, Chacko AT, et al. Predictive factors of distal femoral fracture nonunion after lateral locked plating: A retrospective multicenter case-control study of 283 fractures. Injury. 2014;45(3):554-559. doi: 10.1016/j.injury.2013.10.042. [DOI] [PubMed] [Google Scholar]
- 40.Shulman BS, Patsalos-Fox B, Lopez N, Konda SR, Tejwani NC, Egol KA. Do elderly patients fare worse following operative treatment of distal femur fractures using modern techniques? Geriatr Orthop Surg Rehabil. 2014;5(1):27-30. doi: 10.1177/2151458514525041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yoon B-H, Park IK, Kim Y, Oh H-K, Choo SK, Sung Y-B. Incidence of nonunion after surgery of distal femoral fractures using contemporary fixation device: A meta-analysis. Arch Orthop Trauma Surg. 2021;141(2):225-233. doi: 10.1007/s00402-020-03463-x. [DOI] [PubMed] [Google Scholar]
- 42.Doshi HK, Wenxian P, Burgula MV, Murphy DP. Clinical outcomes of distal femoral fractures in the geriatric population using locking plates with a minimally invasive approach. Geriatr Orthop Surg Rehabil. 2013;4(1):16-20. doi: 10.1177/2151458513496254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Giddie J, Sawalha S, Parker M. Retrograde nailing for distal femur fractures in the elderly. SICOT-J. Dec 1 2015;1:31. doi: 10.1051/sicotj/2015034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kanakaris NK, Obakponovwe O, Krkovic M, Costa ML, Shaw D, Mohanty KR, et al. Fixation of periprosthetic or osteoporotic distal femoral fractures with locking plates: A pilot randomised controlled trial. Int Orthop. 2019;43(5):1193-1204. doi: 10.1007/s00264-018-4061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Khursheed O, Wani MM, Rashid S, Lone AH, Manaan Q, Sultan A, et al. Results of treatment of distal extra: Articular femur fractures with locking plates using minimally invasive approach--experience with 25 consecutive geriatric patients. Musculoskeletal Surg. 2015;99(2):139-147. doi: 10.1007/s12306-014-0343-y. [DOI] [PubMed] [Google Scholar]
- 46.Loosen A, Fritz Y, Dietrich M. Surgical treatment of distal femur fractures in geriatric patients. Geriatr Orthop Surg Rehabil. 2019;10:215145931986072. doi: 10.1177/2151459319860723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Patterson BM, Breslin MA, Wadenpfuhl LK, Vallier HA. New versus old: 95 degree angled blade plate versus distal femoral locking plate. Injury. 2021;52, 1563, 1568. doi: 10.1016/j.injury.2020.11.060. [DOI] [PubMed] [Google Scholar]
- 48.Tank JC, Schneider PS, Davis E, Galpin M, Prasarn ML, Choo AM, et al. Early mechanical failures of the synthes variable angle locking distal femur plate. J Orthop Trauma. 2016;30(1):e7-e11. doi: 10.1097/bot.0000000000000391. [DOI] [PubMed] [Google Scholar]
- 49.Dirks ML, Wall BT, van de Valk B, Holloway TM, Holloway GP, Chabowski A, et al. One week of bed rest leads to substantial muscle atrophy and induces whole-body insulin resistance in the absence of skeletal muscle lipid accumulation. Diabetes. 2016;65(10):2862-2875. doi: 10.2337/db15-1661. [DOI] [PubMed] [Google Scholar]
- 50.Wall BT, Dirks ML, van Loon LJC. Skeletal muscle atrophy during short-term disuse: Implications for age-related sarcopenia. Ageing Res Rev. 2013;12(4):898-906. doi: 10.1016/j.arr.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 51.Kamel HK, Iqbal MA, Mogallapu R, Maas D, Hoffmann RG. Time to ambulation after hip fracture surgery: Relation to hospitalization outcomes. sciencesNov. 2003;58(11):M1042-M1045. doi: 10.1093/gerona/58.11.m1042. [DOI] [PubMed] [Google Scholar]
- 52.Ariza-Vega P, Jiménez-Moleón JJ, Kristensen MT. Non-weight-bearing status compromises the functional level up to 1 yr after hip fracture surgery. Am J Phys Med Rehabil. 2014;93(8):641-648. doi: 10.1097/PHM.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 53.Clement ND, Aitken SA, Duckworth AD, McQueen MM, Court-Brown CM. The outcome of fractures in very elderly patients. J Bone Joint Surg Br. 2011;93-B(6):806-810. doi: 10.1302/0301-620x.93b6.25596. [DOI] [PubMed] [Google Scholar]
- 54.Streubel PN, Ricci WM, Wong A, Gardner MJ. Mortality after distal femur fractures in elderly patients. Clin Orthop Relat Res. 2011;469(4):1188-1196. doi: 10.1007/s11999-010-1530-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Konda SR, Pean CA, Goch AM, Fields AC, Egol KA. Comparison of short-term outcomes of geriatric distal femur and femoral neck fractures: Results from the NSQIP database. Geriatr Orthop Surg Rehabil. 2015;6(4):311-315. doi: 10.1177/2151458515608225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Harvin WH, Oladeji LO, Della Rocca GJ, Murtha YM, Volgas DA, Stannard JP, et al. Working length and proximal screw constructs in plate osteosynthesis of distal femur fractures. Injury. 2017;48(11):2597-2601. doi: 10.1016/j.injury.2017.08.064. [DOI] [PubMed] [Google Scholar]
- 57.Kim S-M, Yeom J-W, Song HK, Hwang K-T, Hwang J-H, Yoo J-H. Lateral locked plating for distal femur fractures by low-energy trauma: What makes a difference in healing? Int Orthop. 2018;42(12):2907-2914. doi: 10.1007/s00264-018-3881-3. [DOI] [PubMed] [Google Scholar]
- 58.Kiyono M, Noda T, Nagano H, Maehara T, Yamakawa Y, Mochizuki Y, et al. Clinical outcomes of treatment with locking compression plates for distal femoral fractures in a retrospective cohort. J Orthop Surg Res. 2019;14(1):384. doi: 10.1186/s13018-019-1401-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee J-H, Park K-C, Lim S-J, Kwon K-B, Kim JW. Surgical outcomes of simple distal femur fractures in elderly patients treated with the minimally invasive plate osteosynthesis technique: Can percutaneous cerclage wiring reduce the fracture healing time? Arch Orthop Trauma Surg. 2020;140(10):1403-1412. doi: 10.1007/s00402-020-03385-8. [DOI] [PubMed] [Google Scholar]
- 60.Rosenthal R, Kasenda B, Dell-Kuster S, von Elm E, You J, Blümle A, et al. Completion and publication rates of randomized controlled trials in surgery. Annals of surgery. Jul 2015;262(1):68-73. doi: 10.1097/sla.0000000000000810. [DOI] [PubMed] [Google Scholar]