Abstract
BACKGROUND
Current equations for estimated glomerular filtration rate (eGFR) that use serum creatinine or cystatin C incorporate age, sex, and race to estimate measured GFR. However, race in eGFR equations is a social and not a biologic construct.
METHODS
We developed new eGFR equations without race using data from two development data sets: 10 studies (8254 participants, 31.5% Black) for serum creatinine and 13 studies (5352 participants, 39.7% Black) for both serum creatinine and cystatin C. In a validation data set of 12 studies (4050 participants, 14.3% Black), we compared the accuracy of new eGFR equations to measured GFR. We projected the prevalence of chronic kidney disease (CKD) and GFR stages in a sample of U.S. adults, using current and new equations.
RESULTS
In the validation data set, the current creatinine equation that uses age, sex, and race overestimated measured GFR in Blacks (median, 3.7 ml per minute per 1.73 m2 of body-surface area; 95% confidence interval [CI], 1.8 to 5.4) and to a lesser degree in non-Blacks (median, 0.5 ml per minute per 1.73 m2; 95% CI, 0.0 to 0.9). When the adjustment for Black race was omitted from the current eGFR equation, measured GFR in Blacks was underestimated (median, 7.1 ml per minute per 1.73 m2; 95% CI, 5.9 to 8.8). A new equation using age and sex and omitting race underestimated measured GFR in Blacks (median, 3.6 ml per minute per 1.73 m2; 95% CI, 1.8 to 5.5) and overestimated measured GFR in non-Blacks (median, 3.9 ml per minute per 1.73 m2; 95% CI, 3.4 to 4.4). For all equations, 85% or more of the eGFRs for Blacks and non-Blacks were within 30% of measured GFR. New creatinine–cystatin C equations without race were more accurate than new creatinine equations, with smaller differences between race groups. As compared with the current creatinine equation, the new creatinine equations, but not the new creatinine–cystatin C equations, increased population estimates of CKD prevalence among Blacks and yielded similar or lower prevalence among non-Blacks.
CONCLUSIONS
New eGFR equations that incorporate creatinine and cystatin C but omit race are more accurate and led to smaller differences between Black participants and non-Black participants than new equations without race with either creatinine or cystatin C alone. (Funded by the National Institute of Diabetes and Digestive and Kidney Diseases.)
THE GLOMERULAR FILTRATION RATE (GFR) is generally estimated from serum concentrations of endogenous filtration markers such as creatinine or cystatin C. During the past two decades, automated clinical laboratory reporting of GFR estimated with the use of creatinine (eGFRcr) has become widespread, coincident with increased awareness of chronic kidney disease (CKD) in the United States.1–4 Equations for estimated GFR (eGFR) incorporate demographic variables to explain variation in serum concentrations of endogenous filtration markers that are unrelated to GFR, thereby minimizing systematic errors in subgroups defined by these variables and systematic differences between groups.5 The current guideline-recommended approach is to use eGFRcr as the initial test in GFR evaluation, with an equation that includes race (Black vs. non-Black), because previous studies indicated a higher average serum creatinine level for the same measured GFR level in Black participants than in non-Black participants.5–7 Although not yet widely used, the serum cystatin C level is recommended for confirmatory testing of eGFR.8 The current equation for eGFR that uses serum cystatin C (eGFRcys) does not include race and has similar accuracy to eGFRcr. The current equation that uses both markers (eGFRcr-cys) is more accurate than either eGFRcr or eGFRcys but includes race.5,9
Inclusion of race in GFR estimating equations, along with other algorithms in medicine, is facing increasing scrutiny because race is a social and not a biologic construct; its inclusion ignores diversity within and among racial groups and may contribute to systemic racism in medicine.10–13 In response, some institutions omit Black race in computation of eGFR, thus assigning the value for non-Black persons to Black persons. However, the accuracy of this approach as compared with measured GFR has not been evaluated; it could lead to underestimates of measured GFR, with effects on clinical decision making and public health. This is particularly important given that Black Americans already bear a disproportionate burden of kidney failure.3 Systematic differences in GFR-based care could exacerbate health disparities.14–20
This study evaluated the accuracy of current guideline-recommended GFR estimating equations and compared them with new equations that do not use race. We also evaluated the effect of these equations on prevalence estimates for CKD and GFR stages used for clinical decisions among a representative sample of U.S. adults.
METHODS
STUDY OVERSIGHT
The study was conducted by the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI). The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, which had no role in the analysis of data, the preparation or approval of the manuscript, or the decision to submit the manuscript for publication. The authors vouch for the completeness and accuracy of the data and for the fidelity of the study to the statistical analysis plan. The institutional review boards at all participating institutions approved each study that was used as a data source, and the institutional review board at Tufts Medical Center approved the overall analyses.
EQUATIONS TO ESTIMATE GFR AND ACCURACY AS COMPARED WITH MEASURED GFR
Data Sources and Laboratory Methods
We pooled data from research studies and clinical populations in which GFR was measured with the use of urinary or plasma clearance of exogenous filtration markers (Table S1 and Fig. S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org).5,9 For development of new equations, we used the data sets previously used for development of current equations (development data sets): CKD-EPI 2009 for eGFRcr (10 studies, 8254 participants) and CKD-EPI 2012 for eGFRcys and eGFRcr-cys (13 studies, 5352 participants)5,9 (Table S2). For external validation, we used a new data set (CKD-EPI 2021), consisting of the CKD-EPI 2012 external validation data set and new studies (12 studies [7 new], 4050 participants) (validation data set), to compare the performance of current and new equations. All the participants were 18 years of age or older. Race was reported by the participant in most studies (Table S3) and was categorized as Black or non-Black (hereafter, race groups), consistent with current equations and the purposes of these analyses. Measurement of creatinine, cystatin C, and GFR followed previously reported methods.5,9,21,22
Development and Validation of Equations
Our goal was to compare the current CKD-EPI eGFRcr, eGFRcys, and eGFRcr-cys equations with equations developed with the use of two new approaches for GFR estimation that do not involve race.5,9 As we described previously, the current approach to the development of CKD-EPI equations has been to model eGFR with the use of least-squares linear regression to relate log-transformed measured GFR to log-transformed filtration markers, age, sex, and race with separate slopes for higher as compared with lower levels of creatinine and cystatin C.5,9 Race is an explanatory variable in the current eGFRcr and eGFRcr-cys equations but not in the current eGFRcys equation.
The first set of new equations uses the same coefficients for the intercept, age, sex and creatinine level as in the current eGFRcr and eGFRcr-cys equations but removes the Black race coefficient in computing eGFR, thereby assigning the eGFRcr and eGFRcr-cys values for non-Black persons to Black persons. For the second set of new equations, we fit new models using eGFRcr and eGFRcr-cys by means of the same regression function as the current equations but without inclusion of race as an explanatory variable. In total, we evaluated seven equations (three current and four new equations). Because all equations were developed by the CKD-EPI research group, we refer to them only by the filtration marker or markers (creatinine [eGFRcr], cystatin C [eGFRcys], or creatinine–cystatin C [eGFRcr-cys]) and the demographic factors (age, sex, and race [ASR] or age and sex [AS]) that were used in their development. We use the term non-Black (NB) to refer to ASR equations that were fit with a race term but in which the Black race coefficient was removed for computation of eGFR. Additional details are provided in the Methods section in the Supplementary Appendix.
In the development data sets, we assessed bias (systematic error) as the difference between measured GFR and eGFR and assessed model fit using root-mean-square error.5,9 In the validation data set, we assessed accuracy overall and within race groups as bias, percentage of estimates less than 30% different from measured GFR (P30, with 1−P30 corresponding to large errors that may be clinically significant), and agreement of eGFR with measured GFR categories using guideline-recommended GFR stages (<30, 30 to 44, 45 to 59, 60 to 89, and >90 ml per minute per 1.73 m2 of body-surface area).8 A P30 value of 80 to 90% is considered to be acceptable for GFR evaluation in many circumstances, and a P30 value of 90% or higher is preferred; these values correspond to approximately 60 to 70% agreement and more than 70% agreement of eGFR with measured GFR in GFR categories, respectively.5,8,9 We also focused on differential bias (systematic differences) between race groups because it could lead to systematic differences in treatment for the same measured GFR level. Confidence intervals for bias were calculated by means of bootstrap methods. We assessed accuracy in subgroups according to eGFR (as defined above), age (<40, 40 to 65, and >65 years), sex, and body-mass index (BMI, the weight in kilograms divided by the square of the height in meters: ≤25, 25 to <30, and ≥30).
In sensitivity analyses, we weighted the proportion of Black participants in the development data set from 0 to 100% to evaluate the effect on accuracy. In the validation data set, we calibrated measured GFR to account for differences between measurement methods as compared with the development data sets,5,9,23 and we compared equations that were developed by other research groups to estimate GFR in adults.24–28
ESTIMATION OF PREVALENCE OF CKD AND GFR STAGES IN U.S. ADULTS
We estimated CKD prevalence using data from 4563 participants from the 1999–2000 and 2001–2002 cycles of the National Health and Nutrition Examination Survey (NHANES) who were 20 years of age or older and had data available on serum creatinine or cystatin C levels (Tables S4 and S5).29 We used recommended NHANES methods for weighting and variance estimation.30–32 CKD was defined as an eGFR of less than 60 ml per minute per 1.73 m2 with the use of the equations described above or persistent albuminuria (urinary albumin-to-creatinine ratio [with albumin measured in milligrams and creatinine measured in grams] of >30) and the guideline-recommended GFR stages.8,29 We assessed the number of participants with CKD or an eGFR lower than key thresholds for clinical decision making (60, 45, and 30 ml per minute per 1.73 m2) as compared with the number of participants according to the current eGFRcr(ASR) equation. Prevalence estimates were applied to the 2019 U.S. Census estimate of 246.6 million adults 20 years of age or older. Additional details are provided in the Methods section in the Supplementary Appendix.
RESULTS
DEVELOPMENT OF EQUATIONS AND ACCURACY AS COMPARED WITH MEASURED GFR
Participants
Black participants made up 31.5% of the 2009 development data set, 39.7% of the 2012 development data set, and 14.3% of the 2021 validation data set; the mean (±SD) measured GFR in each overall data set was 67.6±39.6, 67.9±38.6, and 76.4±29.6 ml per minute per 1.73 m2, respectively (Table 1 and Fig. S2). Tables S6 through S9 show demographic and clinical characteristics within each study used as a data source.
Table 1.
Characteristics of the Participants in the Development and Validation Data Sets.*
| Characteristic | eGFRcr 2009 Development Data Set | eGFRcr-cys 2012 Development Data Set | 2021 Validation Data Set | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall (N = 8254) |
Black (N = 2601) |
Non-Black (N = 5653) |
Overall (N = 5352) |
Black (N = 2123) |
Non-Black (N = 3229) |
Overall (N = 4050) |
Black (N = 579) |
Non-Black (N = 3471) |
|
| Percent of overall population | 100 | 31.5 | 68.5 | 100 | 39.7 | 60.3 | 100 | 14.3 | 85.7 |
| Age — yr | 47.0±14.8 | 52.8±12.0 | 44.3±15.2 | 46.5±15.1 | 53.1±11.6 | 42.2±15.6 | 57.0±17.4 | 53.6±12.6 | 57.6±18.0 |
| Age category — no. (%) | |||||||||
| <40 yr | 2921 (35.4) | 397 (15.3) | 2524 (44.6) | 2008 (37.5) | 299 (14.1) | 1709 (52.9) | 715 (17.7) | 59 (10.2) | 656 (18.9) |
| 40–65 yr | 4309 (52.2) | 1807 (69.5) | 2502 (44.3) | 2625 (49.0) | 1463 (68.9) | 1162 (36.0) | 1989 (49.1) | 417 (72.0) | 1572 (45.3) |
| >65 yr | 1024 (12.4) | 397 (15.3) | 627 (11.1) | 719 (13.4) | 361 (17.0) | 358 (11.1) | 1346 (33.2) | 103 (17.8) | 1243 (35.8) |
| Female sex — no. (%) | 3606 (43.7) | 1026 (39.4) | 2580 (45.6) | 2245 (41.9) | 822 (38.7) | 1423 (44.1) | 1557 (38.4) | 140 (24.2) | 1417 (40.8) |
| BMI† | 28.2±6.1 | 30.6±6.7 | 27.2±5.5 | 28.3±6.3 | 30.8±6.9 | 26.6±5.2 | 26.9±5.0 | 28.0±6.0 | 26.8±4.8 |
| BMI category — no. (%)† | |||||||||
| <20 | 285 (3.5) | 60 (2.3) | 225 (4.0) | 214 (4.0) | 53 (2.5) | 161 (5.0) | 165 (4.1) | 23 (4.0) | 142 (4.1) |
| 20 to <25 | 2446 (29.6) | 457 (17.6) | 1989 (35.2) | 1585 (29.6) | 360 (17.0) | 1225 (37.9) | 1366 (33.8) | 173 (29.9) | 1193 (34.4) |
| 25 to <30 | 2923 (35.4) | 862 (33.1) | 2061 (36.5) | 1881 (35.2) | 686 (32.3) | 1195 (37.0) | 1623 (40.1) | 215 (37.2) | 1408 (40.6) |
| ≥30 | 2600 (31.5) | 1222 (47.0) | 1378 (24.4) | 1671 (31.2) | 1024 (48.2) | 647 (20.0) | 890 (22.0) | 167 (28.9) | 723 (20.9) |
| Diabetes — no. (%)‡ | 2406 (29.1) | 297 (11.4) | 2109 (37.3) | 1726 (32.2) | 199 (9.4) | 1527 (47.3) | 1357 (37.5) | 171 (33.4) | 1186 (38.2) |
| Kidney-donor candidates — no. (%) | 1030 (12.5) | 69 (2.7) | 961 (17.0) | 180 (3.4) | 10 (0.5) | 170 (5.3) | 459 (11.3) | 14 (2.4) | 445 (12.8) |
| Measured GFR — ml/min/1.73 m2 | 67.6±39.6 | 55.5±27.2 | 73.2±43.0 | 67.9±38.6 | 56.5±25.4 | 75.4±43.6 | 76.4±29.6 | 84.0±26.0 | 75.1±30.0 |
| Measured GFR category — no. (%) | |||||||||
| <30 ml/min/1.73 m2 | 1722 (20.9) | 513 (19.7) | 1209 (21.4) | 945 (17.7) | 331 (15.6) | 614 (19.0) | 254 (6.3) | 14 (2.4) | 240 (6.9) |
| 30 to <60 ml/min/1.73 m2 | 2334 (28.3) | 1026 (39.4) | 1308 (23.1) | 1765 (33.0) | 913 (43.0) | 852 (26.4) | 896 (22.1) | 84 (14.5) | 812 (23.4) |
| 60 to <90 ml/min/1.73 m2 | 1669 (20.2) | 793 (30.5) | 876 (15.5) | 1105 (20.6) | 679 (32.0) | 426 (13.2) | 1601 (39.5) | 240 (41.5) | 1361 (39.2) |
| ≥90 ml/min/1.73 m2 | 2529 (30.6) | 269 (10.3) | 2260 (40.0) | 1537 (28.7) | 200 (9.4) | 1337 (41.4) | 1299 (32.1) | 241 (41.6) | 1058 (30.5) |
| Creatinine — mg/dl | 1.66±1.16 | 1.86±1.09 | 1.56±1.18 | 1.57±0.93 | 1.74±0.85 | 1.45±0.97 | 1.16±0.70 | 1.16±0.56 | 1.16±0.72 |
| Cystatin C — mg/liter | NA | NA | NA | 1.43±0.71 | 1.49±0.63 | 1.39±0.76 | 1.18±0.55 | 1.05±0.41 | 1.20±0.57 |
Plus–minus values are means ±SD. Race was reported by the participants. To convert the values for glomerular filtration rate (GFR) to milliliters per second per square meter, multiply by 0.0167. To convert the values for serum creatinine to micromoles per liter, multiply by 88.4. Percentages may not total 100 because of rounding. Descriptive data according to the studies used for each data set are provided in Tables S6 through S8 in the Supplementary Appendix. The term eGFRcr denotes estimated GFR from creatinine equation, eGFRcr-cys estimated GFR from creatinine–cystatin C equation, and NA not applicable.
In the 2012 development data set, data on body-mass index (BMI) were available for 5351 participants in the overall population, 2123 Black participants, and 3228 non-Black participants. In the 2021 validation data set, data on BMI were available for 4044 participants in the overall population, 578 Black participants, and 3466 non-Black participants.
In the 2021 validation data set, data on diabetes status were available for 3616 participants in the overall population, 512 Black participants, and 3104 non-Black participants.
Description of Current and New Equations
Table 2 shows the variables included in the current and new equations. By design, coefficients are the same for the ASR and ASR-NB equations except for the presence or absence of the Black race coefficient. All coefficients for the new AS equations differed from those for the current ASR and new ASR-NB equations (Table 2). For the same age, sex, and creatinine level, eGFRcr for Black participants was highest for the current ASR equation, lowest for the new ASR-NB equation, and intermediate for the new AS equation. For non-Black participants, eGFRcr was equal for the ASR and ASR-NB equations and higher for the AS equation (Fig. S3 and Table S10). Differences in eGFR values between race groups were smaller for new eGFRcr-cys equations than for new eGFRcr equations.
Table 2.
Current and New Equations to Estimate GFR.*
| Model; Name of Equation† | Intercept μ (95% CI) | Coefficients for Creatinine (95% CI)‡ | Coefficients for Cystatin C (95% CI)§ | Coefficient c for Age (95% CI) | Coefficient d for Female Sex (95% CI) | Coefficient e for Black Race (95% CI) | ||
|---|---|---|---|---|---|---|---|---|
| a 1 | a 2 | b 1 | b 2 | |||||
| 2009 CKD-EPI creatinine5; eGFRcr(ASR), current | 141 (139 to 144) |
F: −0.329 (−0.428 to −0.230); M: −0.411 (−0.508 to −0.314) |
−1.209 (−1.220 to −1.198) |
— | — | 0.9929 (0.9925 to 0.9933) |
1.018 (1.007 to 1.029) |
1.159 (1.144 to 1.170) |
| 2009 CKD-EPI creatinine5; eGFRcr(ASR-NB), new | 141 (139 to 144) |
F: −0.329 (−0.428 to −0.230); M: −0.411 (−0.508 to −0.314) |
−1.209 (−1.220 to −1.198) |
— | — | 0.9929 (0.9925 to 0.9933) |
1.018 (1.007 to 1.029) |
1 |
| 2021 CKD-EPI creatinine (2009 CKD-EPI creatinine fit without race); eGFRcr(AS), new | 142 (139 to 144) |
F: −0.241 (−0.344 to −0.138); M: −0.302 (−0.403 to −0.202) |
−1.200 (−1.211 to −1.189) |
— | — | 0.9938 (0.9935 to 0.9942) |
1.012 (1.000 to 1.023) |
— |
| 2012 CKD-EPI cystatin C9; eGFRcys(AS), current | 133 (130 to 136) |
— | — | −0.499 (−0.610 to −0.388) |
−1.328 (−1.344 to −1.312) |
0.9962 (0.9957 to 0.9966) |
0.932 (0.921 to 0.944) |
— |
| 2012 CKD-EPI creatinine–cystatin C9; eGFRcr-cys(ASR), current | 135 (132 to 137) |
F: −0.248 (−0.364 to −0.132); M: −0.207 (−0.308 to −0.107) |
−0.601 (−0.630 to −0.571) |
−0.375 (−0.477 to −0.274) |
−0.711 (−0.744 to −0.678) |
0.9952 (0.9948 to 0.9957) |
0.969 (0.958 to 0.980) |
1.080 (1.067 to 1.093) |
| 2012 CKD-EPI creatinine–cystatin C9; eGFRcr-cys(ASR-NB), new | 135 (132 to 137) |
F: −0.248 (−0.364 to −0.132); M: −0.207 (−0.308 to −0.107) |
−0.601 (−0.630 to −0.571) |
−0.375 (−0.477 to −0.274) |
−0.711 (−0.744 to −0.678) |
0.9952 (0.9948 to 0.9957) |
0.969 (0.958 to 0.980) |
1 |
| 2021 CKD-EPI creatinine–cystatin C (2012 CKD-EPI creatinine–cystatin C fit without race); eGFRcr-cys(AS), new | 135 (132 to 137) |
F: −0.219 (−0.336 to −0.101); M: −0.144 (−0.245 to −0.042) |
−0.544 (−0.572 to −0.515) |
−0.323 (−0.426 to −0.220) |
−0.778 (−0.809 to −0.746) |
0.9961 (0.9957 to 0.9965) |
0.963 (0.952 to 0.974) |
— |
The cells show coefficients to use in the following formula: . Here, κ is 0.7 for female participants and 0.9 for male participants, min indicates the minimum of Scr/κ and 1, and max indicates the maximum of Scr/κ and 1. The 2009 and 2012 models were developed previously. Sex differences for eGFRcr and eGFRcr-cys equations are modeled as sex-specific creatinine coefficients as well as female sex coefficients. CKD-EPI denotes Chronic Kidney Disease Epidemiology Collaboration, F female, and M male.
The equations are referred to by the filtration marker or markers (creatinine [eGFRcr], cystatin C [eGFRcys], or creatinine–cystatin C [eGFRcr-cys]) and the demographic factors (age, sex, and race [ASR] or age and sex [AS]) that were used in their development. Non-Black (NB) refers to equations in which the Black race coefficient was omitted in computation of the eGFR value.
The coefficient a1 is used for levels of creatinine less than or equal to 0.9 mg per deciliter for male participants and 0.7 mg per deciliter for female participants. The coefficient a2 is used for levels of creatinine greater than 0.9 mg per deciliter for male participants and 0.7 mg per deciliter for female participants.
The coefficient b1 is used for levels of cystatin C less than or equal to 0.8 mg per liter, and the coefficient b2 is used for levels greater than 0.8 mg per liter.
Bias in Equations Involving Black and Non-Black Participants in Development Data Sets
In the development data sets, the current eGFRcr(ASR) and eGFRcr-cys(ASR) equations were unbiased in both race groups (Fig. S4 and Table S11). The new ASR-NB equations underestimated measured GFR in Black participants. The new AS equations underestimated measured GFR in Black participants less than the ASR-NB equations but overestimated measured GFR in non-Black participants. Bias was smaller for new eGFRcr-cys equations than for corresponding new eGFRcr equations. In sensitivity analyses for the new AS equations, varying the proportion of Black participants in the development data sets changed the magnitude of the bias in each race group but not the differential bias between race groups and had less effect on the bias for eGFRcr-cys equations than on the bias for eGFRcr equations (Fig. S5 and Table S12).
Creatinine-Based eGFR in Validation Data Set
In the validation data sets, the current eGFRcr(ASR) equation overestimated measured GFR in Black participants by a median of 3.7 ml per minute per 1.73 m2 (95% confidence interval [CI], 1.8 to 5.4) and minimally overestimated measured GFR in non-Black participants by a median of 0.5 ml per minute per 1.73 m2 (95% CI, 0.0 to 0.9); the differential bias was 3.2 ml per minute per 1.73 m2 (95% CI, 1.3 to 5.0) (Fig. 1, Fig. S6, and Table 3). In a sensitivity analysis that was calibrated for differences in GFR measurement methods, the equation was unbiased in Black participants and underestimated measured GFR in non-Black participants, without a change in the differential bias (Figs. S7 and S8 and Table S13). The new eGFRcr(ASR-NB) equation underestimated measured GFR in Black participants (7.1 ml per minute per 1.73 m2; 95% CI, 5.9 to 8.8). The new eGFRcr(AS) equation underestimated measured GFR in Black participants (3.6 ml per minute per 1.73 m2; 95% CI, 1.8 to 5.5) and overestimated measured GFR in non-Black participants (3.9 ml per minute per 1.73 m2; 95% CI, 3.4 to 4.4). The differential bias was 7.6 ml per minute per 1.73 m2 for both new ASR-NB and AS equations. P30 was 85 to 90% for both race groups for all eGFRcr equations (Table 3). Agreement between GFR categories was 59 to 69% and was lower in Black participants than in non-Black participants for all eGFRcr equations, especially for the ASR-NB equation (Table 3 and Table S14).
Figure 1. Comparison of Measured GFR and Estimated GFR (eGFR) According to Race Group across Alternative GFR Estimating Equations.
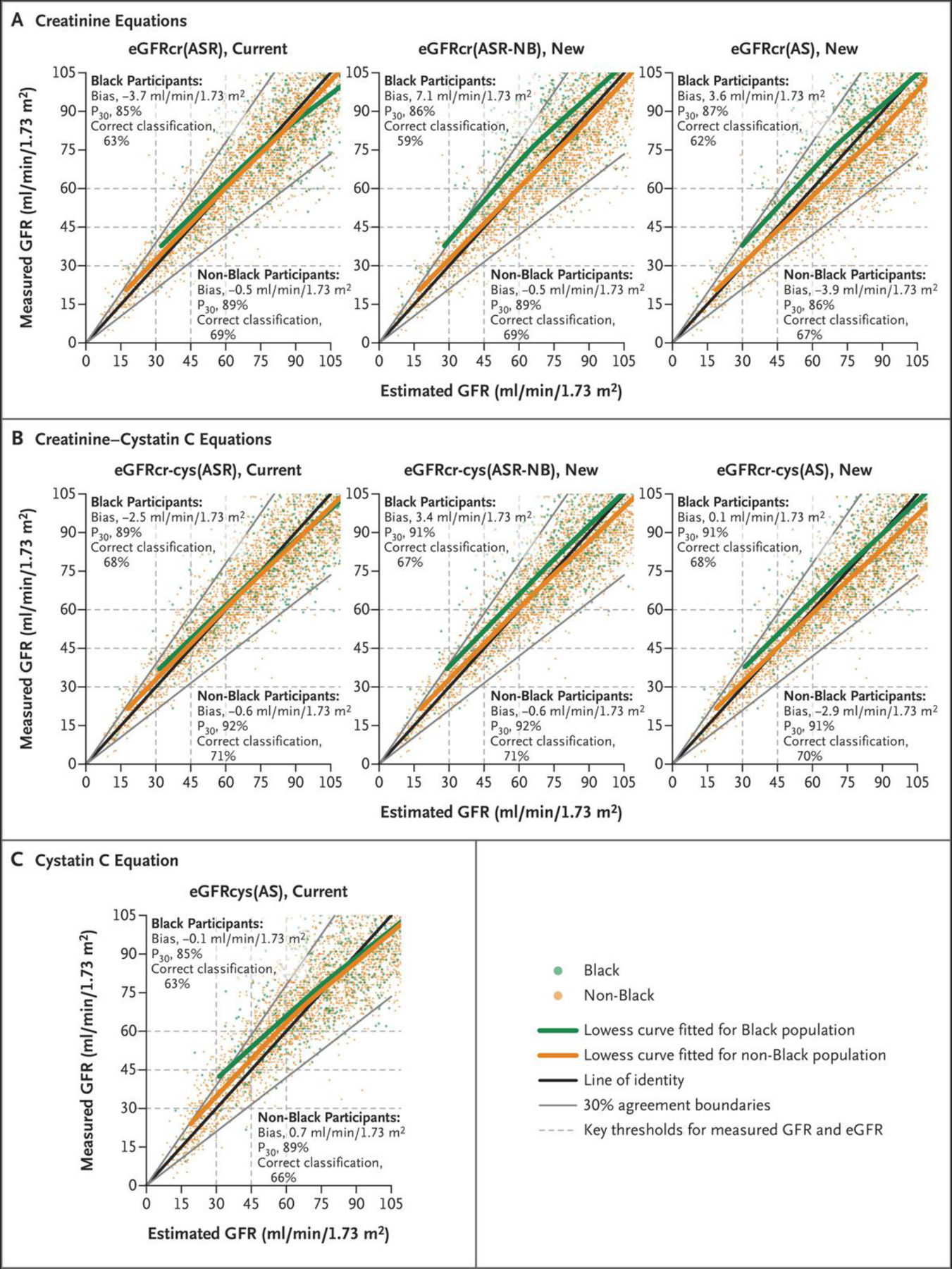
The equations are referred to by the filtration marker or markers (creatinine [eGFRcr], cystatin C [eGFRcys], or creatinine–cystatin C [eGFRcr-cys]) and the demographic factors (age, sex, and race [ASR] or age and sex [AS]) that were used in their development. Non-Black (NB) refers to equations in which the Black race coefficient was omitted in computation of the eGFR value. Data from the validation data set are shown. Data from the development data set are shown in Figure S4 in the Supplementary Appendix. Bias is defined as the median difference between measured GFR and eGFR. A positive sign indicates underestimation of measured GFR, and a negative sign indicates overestimation of measured GFR. P30 is the proportion of eGFR within 30% of measured GFR. Correct classification refers to agreement between measured GFR and eGFR categories of more than 90, 60 to 89, 45 to 59, 30 to 44, 15 to 29, and less than 15 ml per minute per 1.73 m2.
Table 3.
Accuracy of Current and New Approaches for GFR Estimation as Compared with Measured GFR in the Validation Data Set.
| Filtration Marker and Equation* | Black Participants | Non-Black Participants | Difference between Black Participants and Non-Black Participants (95% CI)† |
|---|---|---|---|
| Bias: Median Difference between Measured GFR and eGFR (95% CI)‡ | |||
| milliliters per minute per 1.73 square meters | |||
| Creatinine | |||
| eGFRcr(ASR), current | −3.7 (−5.4 to −1.8) | −0.5 (−0.9 to 0.0) | −3.2 (−5.0 to −1.3) |
| eGFRcr(ASR-NB), new | 7.1 (5.9 to 8.8) | −0.5 (−0.9 to 0.0) | 7.6 (6.1 to 9.0) |
| eGFRcr(AS), new | 3.6 (1.8 to 5.5) | −3.9 (−4.4 to −3.4) | 7.6 (5.6 to 9.5) |
| Cystatin C | |||
| eGFRcys(AS), current | −0.1 (−1.5 to 1.6) | 0.7 (0.2 to 1.2) | −0.8 (−2.5 to 0.8) |
| Creatinine–cystatin C | |||
| eGFRcr-cys(ASR), current | −2.5 (−3.7 to −1.2) | −0.6 (−0.9 to −0.2) | −1.9 (−3.2 to −0.6) |
| eGFRcr-cys(ASR-NB), new | 3.4 (1.5 to 4.5) | −0.6 (−0.9 to −0.2) | 4.0 (2.6 to 5.3) |
| eGFRcr-cys(AS), new | 0.1 (−0.9 to 1.6) | −2.9 (−3.3 to −2.5) | 3.0 (1.6 to 4.4) |
| Agreement within 30% of Measured GFR (P30)§ | |||
| percent | percentage points | ||
| Creatinine | |||
| eGFRcr(ASR), current | 85.1 (82.2 to 87.9) | 89.5 (88.5 to 90.4) | −4.4 (−7.6 to −1.2) |
| eGFRcr(ASR-NB), new | 86.4 (83.4 to 89.1) | 89.5 (88.5 to 90.4) | −3.1 (−6.2 to 0) |
| eGFRcr(AS), new | 87.2 (84.5 to 90.0) | 86.5 (85.4 to 87.6) | 0.7 (−2.4 to 3.8) |
| Cystatin C | |||
| eGFRcys(AS), current | 84.6 (81.7 to 87.6) | 88.9 (87.9 to 89.9) | −4.3 (−7.5 to −1.1) |
| Creatinine–cystatin C | |||
| eGFRcr-cys(ASR), current | 88.6 (85.8 to 91.2) | 92.4 (91.5 to 93.2) | −3.8 (−6.7 to −0.9) |
| eGFRcr-cys(ASR-NB), new | 90.8 (88.4 to 93.1) | 92.4 (91.5 to 93.2) | −1.6 (−4.2 to 1) |
| eGFRcr-cys(AS), new | 90.5 (88.1 to 92.9) | 90.8 (89.9 to 91.8) | −0.3 (−3.0 to 2.4) |
| Percent Agreement between eGFR and Measured GFR Categories¶ | |||
| Creatinine | |||
| eGFRcr(ASR), current | 63.2 (59.3 to 67.1) | 68.5 (67.0 to 70.1) | −5.3 (−9.6 to −1) |
| eGFRcr(ASR-NB), new | 59.2 (55.2 to 63.2) | 68.5 (67.0 to 70.1) | −9.3 (−13.7 to −4.9) |
| eGFRcr(AS), new | 61.8 (57.9 to 65.8) | 66.7 (65.1 to 68.2) | −4.9 (−9.3 to −0.5) |
| Cystatin C | |||
| eGFRcys(AS), current | 62.5 (58.6 to 66.5) | 66.1 (64.5 to 67.7) | −3.6 (−8.0 to 0.8) |
| Creatinine–cystatin C | |||
| eGFRcr-cys(ASR), current | 67.9 (64.1 to 71.7) | 70.8 (69.3 to 72.4) | −2.9 (−7.1 to 1.3) |
| eGFRcr-cys(ASR-NB), new | 66.5 (62.6 to 70.3) | 70.8 (69.3 to 72.4) | −4.3 (−8.6 to 0) |
| eGFRcr-cys(AS), new | 68.4 (64.6 to 72.2) | 70.2 (68.6 to 71.7) | −1.8 (−6 to 2.4) |
The equations are referred to by the filtration marker or markers (creatinine [eGFRcr], cystatin C [eGFRcys], or creatinine–cystatin C [eGFRcrcys]) and the demographic factors (age, sex, and race [ASR] or age and sex [AS]) that were used in their development. Non-Black (NB) refers to equations in which the Black race coefficient was removed.
Difference between race groups was defined as the metric in Black participants minus non-Black participants. A negative sign for difference in bias indicates underestimation of measured GFR in Black participants relative to non-Black participants. A negative sign for P30 or GFR category agreement indicates less agreement in Black participants as compared with non-Black participants. Differences for agreement within 30% of measured GFR and for percent agreement between eGFR and measured GFR categories are expressed as percentage points.
Bias is defined as the median difference between measured GFR and eGFR. A positive sign indicates underestimation of measured GFR, and a negative sign indicates overestimation of measured GFR.
P30 is the proportion of eGFR within 30% of measured GFR.
Correct classification refers to agreement between measured GFR and eGFR categories of more than 90, 60 to 89, 45 to 59, 30 to 44, 15 to 29, and less than 15 ml per minute per 1.73 m2.
eGFR Based on Creatinine and Cystatin C in Validation Data Set
The current eGFRcr-cys(ASR) equation overestimated measured GFR in Black participants (2.5 ml per minute per 1.73 m2; 95% CI, 1.2 to 3.7) and minimally overestimated measured GFR in non-Black participants (0.6 ml per minute per 1.73 m2; 95% CI, 0.2 to 0.9). The differential bias was 1.9 ml per minute per 1.73 m2 (95% CI, 0.6 to 3.2). The new eGFRcr-cys(ASR-NB) and eGFRcr-cys(AS) equations had smaller bias in Black participants, similar bias in non-Black participants, and smaller differential bias than the corresponding new eGFRcr equations. P30 was greater than 90% for Blacks and non-Blacks, and agreement between GFR categories was 67 to 71% and more similar for Black and non-Black participants than with eGFRcr equations. The eGFRcys equation had minimal bias in both groups but lower P30 and lesser agreement for GFR categories than with the current and new eGFRcr-cys equations.
Results for bias and P30 were generally consistent across subgroups of eGFR, age, sex, diabetes status, and BMI (Fig. S7). Other eGFRcr or eGFRcr-cys equations that were developed previously in mainly White populations showed greater bias in Black participants (Table S13).
PREVALENCE OF CKD AND GFR STAGES ACCORDING TO EQUATION
Figure S10 shows the distribution of eGFR with the use of different equations. As compared with the current eGFRcr(ASR) equation, the estimated prevalence of CKD among Black persons was higher for the new eGFRcr(ASR-NB) and eGFRcr(AS) equations, but the estimated prevalence was lower among non-Black persons for the eGFRcr(AS) equation, mostly owing to differences in the prevalence of CKD stage G3 (GFR of 30 to 59 ml per minute per 1.73 m2) (Table 4 and Tables S15 and S16). With the use of the current eGFRcys equation, the estimated prevalence was similar to that for the current eGFRcr(ASR) equation among Black persons but was higher among non-Black persons. As compared with the current eGFRcr(ASR) equation, the new eGFRcr-cys equations had less effect on CKD prevalence than the new eGFRcr equations. For GFR thresholds, the new ASR-NB and AS equations moved more persons across higher GFR thresholds than across lower GFR thresholds (Table 4). Movement across the eGFR threshold of 60 ml per minute per 1.73 m2 was generally more frequent among Black persons than among non-Black persons and was less frequent with all eGFRcr-cys equations than with eGFRcr equations.
Table 4.
Estimated Prevalence of Chronic Kidney Disease and GFR Stages among U.S. Adults.*
| Equation† | Black Persons | Non-Black Persons | ||||
|---|---|---|---|---|---|---|
| No. in Millions | Weighted Percent | Change from eGFRcr(ASR)‡ | No. in Millions | Weighted Percent | Change from eGFRcr(ASR)‡ | |
| percent | percent | |||||
| Chronic kidney disease § | ||||||
| Creatinine | ||||||
| eGFRcr(ASR), current | 4.56±0.36 | 14.34±1.13 | Reference | 25.17±2.00 | 11.72±0.93 | Reference |
| eGFRcr(ASR-NB), new | 5.65±0.40 | 17.77±1.26 | 3.4±0.42 | 25.17±1.99 | 11.72±0.93 | 0 |
| eGFRcr(AS), new | 5.18±0.38 | 16.32±1.21 | 2.0±0.30 | 22.02±2.05 | 10.25±0.95 | −1.5±0.16 |
| Cystatin C | ||||||
| eGFRcys(AS), current | 4.52±0.42 | 14.23±1.32 | −0.1±0.45 | 28.57±2.14 | 13.30±1.00 | 1.6±0.57 |
| Creatinine–cystatin C | ||||||
| eGFRcr-cys(ASR), current | 4.33±0.37 | 13.63±1.15 | −0.7±0.25 | 25.55±2.05 | 11.89±0.95 | 0.2±0.31 |
| eGFRcr-cys(ASR-NB), new | 4.68±0.37 | 14.72±1.18 | 0.4±0.28 | 25.55±2.04 | 11.89±0.95 | 0.2±0.31 |
| eGFRcr-cys(AS), new | 4.42±0.38 | 13.92±1.19 | −0.4±0.28 | 23.72±2.09 | 11.04±0.97 | −0.7±0.32 |
| eGFR <60 ml/min/1.73 m 2 | ||||||
| Creatinine | ||||||
| eGFRcr(ASR), current | 2.08±0.18 | 6.54±0.56 | Reference | 14.75±0.89 | 6.86±0.41 | Reference |
| eGFRcr(ASR-NB), new | 3.32±0.24 | 10.43±0.76 | 3.9±0.46 | 14.75±0.89 | 6.86±0.41 | 0 |
| eGFRcr(AS), new | 2.72±0.18 | 8.55±0.56 | 2.0±0.26 | 11.34±0.78 | 5.28±0.36 | −1.6±0.16 |
| Cystatin C | ||||||
| eGFRcys(AS), current | 2.17±0.27 | 6.84±0.84 | 0.3±0.66 | 19.04±1.49 | 8.86±0.69 | 2.0±0.62 |
| Creatinine–cystatin C | ||||||
| eGFRcr-cys(ASR), current | 1.90±0.20 | 5.97±0.63 | −0.6±0.39 | 15.49±1.02 | 7.21±0.47 | 0.3±0.35 |
| eGFRcr-cys(ASR-NB), new | 2.30±0.21 | 7.24±0.65 | 0.7±0.37 | 15.49±1.02 | 7.21±0.47 | 0.3±0.35 |
| eGFRcr-cys(AS), new | 1.99±0.20 | 6.28±0.63 | −0.3±0.41 | 13.39±0.98 | 6.23±0.46 | −0.6±0.35 |
| eGFR <45 ml/min/1.73 m 2 | ||||||
| Creatinine | ||||||
| eGFRcr(ASR), current | 0.89±0.14 | 2.80±0.44 | Reference | 4.90±0.46 | 2.28±0.21 | Reference |
| eGFRcr(ASR-NB), new | 1.35±0.13 | 4.23±0.41 | 1.4±0.27 | 4.90±0.46 | 2.28±0.21 | 0 |
| eGFRcr(AS), new | 1.03±0.14 | 3.23±0.44 | 0.4±0.12 | 3.97±0.40 | 1.85±0.19 | −0.4±0.07 |
| Cystatin C | ||||||
| eGFRcys(AS), current | 1.05±0.13 | 3.32±0.41 | 0.5±0.23 | 8.09±0.75 | 3.76±0.35 | 1.5±0.24 |
| Creatinine–cystatin C | ||||||
| eGFRcr-cys(ASR), current | 0.91±0.12 | 2.85±0.37 | 0.1±0.18 | 5.61±0.50 | 2.61±0.23 | 0.3±0.09 |
| eGFRcr-cys(ASR-NB), new | 1.12±0.14 | 3.51±0.43 | 0.7±0.15 | 5.61±0.50 | 2.61±0.23 | 0.3±0.09 |
| eGFRcr-cys(AS), new | 0.99±0.12 | 3.12±0.36 | 0.3±0.21 | 5.01±0.48 | 2.33±0.22 | 0.1±0.10 |
| eGFR <30 ml/min/1.73 m 2 | ||||||
| Creatinine | ||||||
| eGFRcr(ASR), current | 0.45±0.08 | 1.40±0.25 | Reference | 1.10±0.22 | 0.51±0.10 | Reference |
| eGFRcr(ASR-NB), new | 0.57±0.09 | 1.79±0.29 | 0.4±0.12 | 1.10±0.22 | 0.51±0.10 | 0 |
| eGFRcr(AS), new | 0.49±0.09 | 1.54±0.27 | 0.1±0.07 | 0.81±0.16 | 0.38±0.08 | −0.1±0.04 |
| Cystatin C | ||||||
| eGFRcys(AS), current | 0.57±0.09 | 1.81±0.29 | 0.4±0.14 | 2.56±0.40 | 1.19±0.19 | 0.7±0.11 |
| Creatinine–cystatin C | ||||||
| eGFRcr-cys(ASR), current | 0.55±0.09 | 1.72±0.27 | 0.3±0.12 | 1.85±0.35 | 0.86±0.16 | 0.4±0.08 |
| eGFRcr-cys(ASR-NB), new | 0.57±0.09 | 1.80±0.28 | 0.4±0.13 | 1.85±0.35 | 0.86±0.16 | 0.4±0.08 |
| eGFRcr-cys(AS), new | 0.55±0.09 | 1.72±0.27 | 0.3±0.12 | 1.71±0.29 | 0.80±0.13 | 0.3±0.07 |
Plus–minus values are means ±SE.
The equations are referred to by the filtration marker or markers (creatinine [eGFRcr], eGFRcys [cystatin C], or creatinine–cystatin C [eGFRcr-cys]) and the demographic factors (age, sex, and race [ASR] or age and sex [AS]) that were used in their development. Non-Black (NB) refers to equations in which the Black race coefficient was removed.
Change was calculated as the difference in weighted percent from eGFRcr(ASR).
Chronic kidney disease was defined as a GFR of less than 60 ml per minute per 1.73 m2 or persistent albuminuria (urinary albumin-to-creatinine ratio [with albumin measured in milligrams and creatinine measured in grams] of >30).
DISCUSSION
National kidney disease organizations recommend replacement of current eGFR equations by equations that do not use race and that are accurate, inclusive, and standardized in every laboratory in the United States.33 A change in estimating equations could affect care of patients and estimates of the public health burden of CKD. In a large population of adults with or without CKD, we evaluated the accuracy with respect to measured GFR of new approaches without race (ASR-NB and AS) as compared with the currently recommended approach with race (ASR) and estimated their effects on the national prevalence of CKD and GFR stages. The new eGFRcr equations may introduce inaccuracies for both race groups and differences in eGFR between groups. The magnitude of these inaccuracies was generally smaller than the 30% margin of error, which is considered adequate for clinical decision making in many circumstances. However, the larger biases that were observed for the new eGFRcr equations in each race group and differential bias between groups led to differences in estimates of CKD prevalence and GFR stages. This could lead to systematic differences in care between race groups, especially at higher GFR. In contrast, new eGFRcr-cys equations minimized inaccuracy for both race groups, differences in eGFR between race groups, and differences in estimated CKD prevalence. More frequent use of eGFRcr-cys may improve the accuracy of CKD diagnosis and GFR staging while eliminating the use of race in GFR estimating equations.
Uniform implementation by clinical laboratories of new GFR estimating equations without race will be essential for consistent care.4 Our results show that the new eGFRcr(ASR-NB) equation, as has been adopted by some institutions, could lead to large errors in GFR estimation in some Black persons — for example, as Hsu et al. now report in the Journal.34 The new eGFRcr(AS) equation may be more equitable than the new eGFRcr(ASR-NB) equation because it averages observed differences across all persons and may be more appropriate for the increasingly diverse U.S. population. As compared with the ASR-NB equation, the AS equation decreases the bias in Black persons but also introduces a bias in non-Black persons; the magnitude of the bias in each group reflects the proportion of Black participants included in the development data set, which emphasizes the importance of including diverse populations in these data sets.6,35,36
As compared with the current eGFRcr(ASR) equation, the new AS equation would have less effect than the new ASR-NB equation on the prevalence of CKD and GFR stages among Black persons but a greater effect among non-Black persons15,19,20 Assigning a lower eGFR to Black persons would increase the estimated prevalence of CKD among Black persons and could enable earlier diagnosis and treatment. However, it could also lead to potential overdiagnosis of CKD and missed opportunities for therapies that are contraindicated at a low GFR.15,19,20 Assigning a higher eGFR to non-Black persons would decrease the estimated prevalence of CKD and could lead to underdiagnosis of CKD and inappropriate exposure to interventions contraindicated at a lower GFR.
Increased use of estimating equations that incorporate cystatin C could mitigate limitations of the new eGFRcr(ASR-NB) and eGFRcr(AS) equations. The current eGFRcys(AS) equation is nearly unbiased in both race groups, but agreement with measured GFR is not as high as with new eGFRcr-cys equations, and the prevalence of CKD may be overestimated in non-Black persons. The new eGFRcr-cys equations had smaller differences in bias between race groups than the corresponding eGFRcr equations, with less effect on prevalence estimates for CKD and GFR stages than the corresponding eGFRcr equations. Enhanced systems for rapid, cost-effective measurement of cystatin C levels could facilitate its increased use.
The strengths of our study are its design, with separate large data sets that include both Black participants and non-Black participants for development and validation of new equations that eliminate race from GFR estimation. The limitations are that categorization of race into two groups does not adequately represent the diversity within and among racial groups, some of the included studies that were used in the development of the equations are old, and none were in representative populations. We had a smaller number of Black participants than non-Black participants in the validation set, so the estimates of accuracy may be less precise in Black persons, and we had an insufficient representation of racial and ethnic groups other than Black and White.37 We did not use the same data sets in the development of different eGFR equations, which could explain some of the difference in bias between those equations. The studies involved only ambulatory adult populations without serious coexisting conditions; thus, our results may not apply to patients in acute care settings.
We present new eGFRcr equations without race that would be considered sufficiently accurate for clinical practice in many circumstances but may lead to systematic differences in accuracy of eGFRcr between race groups, with implications for individual patients and public health. New eGFRcr-cys equations without race more accurately estimated measured GFR than equations with either the creatinine or cystatin C level alone and led to smaller differences from measured GFR between race groups. These data may inform ongoing discussions on eGFR equations for use in clinical practice, research, and public health.38
Supplementary Material
Acknowledgments
Drs. Inker, Eneanya, Crews, and Powe are members of the National Kidney Foundation–American Society of Nephrology Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Disease. The findings and conclusions in this report are those of the authors and do not represent the official position of the task force.
Supported by grants (R01DK097020 and 1R01DK116790) to Tufts Medical Center from the National Institute of Diabetes and Digestive and Kidney Diseases.
APPENDIX
The authors’ full names and academic degrees are as follows: Lesley A. Inker, M.D., Nwamaka D. Eneanya, M.D., M.P.H., Josef Coresh, M.D., Ph.D., Hocine Tighiouart, M.S., Dan Wang, M.S., Yingying Sang, M.S., Deidra C. Crews, M.D., Alessandro Doria, M.D., Ph.D., M.P.H., Michelle M. Estrella, M.D., M.H.S., Marc Froissart, M.D., Ph.D., Morgan E. Grams, M.D., M.H.S., Ph.D., Tom Greene, Ph.D., Anders Grubb, M.D., Ph.D., Vilmundur Gudnason, M.D., Ph.D., Orlando M. Gutiérrez, M.D., Roberto Kalil, M.D., Amy B. Karger, M.D., Ph.D., Michael Mauer, M.D., Gerjan Navis, M.D., Ph.D., Robert G. Nelson, M.D., Ph.D., Emilio D. Poggio, M.D., Roger Rodby, M.D., Peter Rossing, M.D., D.M.Sc., Andrew D. Rule, M.D., Elizabeth Selvin, Ph.D., M.P.H., Jesse C. Seegmiller, Ph.D., Michael G. Shlipak, M.D., M.P.H., Vicente E. Torres, M.D., Ph.D., Wei Yang, Ph.D., Shoshana H. Ballew, Ph.D., Sara J. Couture, M.P.H., Neil R. Powe, M.D., M.P.H., M.B.A., and Andrew S. Levey, M.D.
The authors’ affiliations are as follows: the Division of Nephrology (L.A.I., S.J.C., A.S.L.) and the Institute for Clinical Research and Health Policy Studies (H.T.), Tufts Medical Center, Tufts Clinical and Translational Science Institute, Tufts University (H.T.), the Section on Genetics and Epidemiology, Joslin Diabetes Center (A.D.), and the Department of Medicine, Harvard Medical School (A.D.) — all in Boston; the Renal-Electrolyte and Hypertension Division, Perelman School of Medicine (N.D.E.), and the Departments of Biostatistics, Epidemiology, and Informatics, Center for Clinical Epidemiology and Biostatistics (W.Y.), University of Pennsylvania, Philadelphia; the Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health and the Welch Center for Prevention, Epidemiology, and Clinical Research, Johns Hopkins Medical Institutions (J.C., D.W., Y.S., M.E.G., E.S., S.H.B.), the Division of Nephrology, Department of Medicine, Johns Hopkins University School of Medicine (D.C.C., M.E.G.), and the Department of Medicine, Division of Nephrology, University of Maryland School of Medicine (R.K.) — all in Baltimore; the Kidney Health Research Collaborative, San Francisco Veterans Affairs (VA) Medical Center and University of California, San Francisco (M.M.E., M.G.S.), the Division of Nephrology, Department of Medicine, San Francisco VA Health Care System and University of California, San Francisco (M.M.E.), and the Department of Medicine, Priscilla Chan and Mark Zuckerberg San Francisco General Hospital and University of California, San Francisco (N.R.P.) — all in San Francisco; the Clinical Trial Unit, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland (M.F.); the Division of Biostatistics, Department of Population Health Sciences, University of Utah Health, Salt Lake City (T.G.); the Department of Clinical Chemistry and Pharmacology, Institute of Laboratory Medicine, Lund University, Lund, Sweden (A.G.); the Faculty of Medicine, University of Iceland, Reykjavik, and the Icelandic Heart Association, Kopavogur — both in Iceland (V.G.); the Departments of Medicine and Epidemiology, University of Alabama at Birmingham, Birmingham (O.M.G.); the Departments of Laboratory Medicine and Pathology (A.B.K., J.C.S.), Pediatrics (M.M.), and Medicine (M.M.), University of Minnesota, Minneapolis, and the Division of Nephrology and Hypertension, Mayo Clinic, Rochester (A.D.R., V.E.T.) — all in Minnesota; the Faculty of Medical Sciences, University Medical Center Groningen, Groningen, the Netherlands (G.N.); the Chronic Kidney Disease Section, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Phoenix, AZ (R.G.N.); the Department of Nephrology and Hypertension, Glickman Urological and Kidney Institute, Cleveland Clinic, Cleveland (E.D.P.); Rush University Medical Center, Chicago (R.R.); and Steno Diabetes Center Copenhagen and the Department of Clinical Medicine, University of Copenhagen — both in Copenhagen (P.R.).
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank Shiyuan Miao, M.S. (Tufts Medical Center, Boston), for assistance with creating earlier versions of the figure.
REFERENCES
- 1.Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function — measured and estimated glomerular filtration rate. N Engl J Med 2006; 354: 2473–83. [DOI] [PubMed] [Google Scholar]
- 2.Levey AS, Coresh J, Tighiouart H, Greene T, Inker LA. Measured and estimated glomerular filtration rate: current status and future directions. Nat Rev Nephrol 2020; 16:51–64. [DOI] [PubMed] [Google Scholar]
- 3.Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2018 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2019;73: Suppl 1: A7–A8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller WG, Jones GRD. Estimated glomerular filtration rate: laboratory implementation and current global status. Adv Chronic Kidney Dis 2018; 25: 7–13. [DOI] [PubMed] [Google Scholar]
- 5.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150: 604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flamant M, Vidal-Petiot E, Metzger M, et al. Performance of GFR estimating equations in African Europeans: basis for a lower race-ethnicity factor than in African Americans. Am J Kidney Dis 2013; 62: 182–4. [DOI] [PubMed] [Google Scholar]
- 7.Lewis J, Agodoa L, Cheek D, et al. Comparison of cross-sectional renal function measurements in African Americans with hypertensive nephrosclerosis and of primary formulas to estimate glomerular filtration rate. Am J Kidney Dis 2001;38: 744–53. [DOI] [PubMed] [Google Scholar]
- 8.KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 2013; 3: 1–150. [DOI] [PubMed] [Google Scholar]
- 9.Inker LA, Schmid CH, Tighiouart H, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med 2012; 367: 20–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eneanya ND, Yang W, Reese PP. Re-considering the consequences of using race to estimate kidney function. JAMA 2019; 322: 113–4. [DOI] [PubMed] [Google Scholar]
- 11.Vyas DA, Eisenstein LG, Jones DS. Hidden in plain sight — reconsidering the use of race correction in clinical algorithms. N Engl J Med 2020; 383: 874–82. [DOI] [PubMed] [Google Scholar]
- 12.Warren E, Booker C, Wyden R, Lee B. Agency for Healthcare Research and Quality (AHRQ) requesting a review of the use of race-based clinical algorithms in standard medical practices Washington, DC: U.S. Congress, September 22, 2020. [Google Scholar]
- 13.Agarwal A Response to Chairman Neal re race and eGFR Washington, DC: American Society of Nephrology, 2020. [Google Scholar]
- 14.Levey AS, Tighiouart H, Titan SM, Inker LA. Estimation of glomerular filtration rate with vs without including patient race. JAMA Intern Med 2020; 180: 793–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed S, Nutt CT, Eneanya ND, et al. Examining the potential impact of race multiplier utilization in estimated glomerular filtration rate calculation on African-American care outcomes. J Gen Intern Med 2020; 36:464–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levey AS, Titan SM, Powe NR, Coresh J, Inker LA. Kidney disease, race, and GFR estimation. Clin J Am Soc Nephrol 2020; 15: 1203–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Powe NR. Black kidney function matters: use or misuse of race? JAMA 2020; 324:737–8. [DOI] [PubMed] [Google Scholar]
- 18.Shin J-I, Sang Y, Chang AR, et al. The FDA metformin label change and racial and sex disparities in metformin prescription among patients with CKD. J Am Soc Nephrol 2020; 31:1847–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diao JA, Inker LA, Levey AS, Tighi-ouart H, Powe NR, Manrai AK. In search of a better equation — performance and equity in estimates of kidney function. N Engl J Med 2021; 384: 396–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duggal V, Thomas I-C, Montez-Rath ME, Chertow GM, Kurella Tamura M. National estimates of CKD prevalence and potential impact of estimating glomerular filtration rate without race. J Am Soc Nephrol 2021; 32: 1454–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inker LA, Couture SJ, Tighiouart H, et al. A new panel estimated GFR, including β2-microglobulin and β-trace protein and not including race, developed in a diverse population. Am J Kidney Dis 2020; 77(5):673.e1–683.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karger AB, Eckfeldt JH, Rynders GP, et al. Long-term longitudinal stability of kidney filtration marker measurements: implications for epidemiological studies and clinical care. Clin Chem 2020;67: 425–33. [DOI] [PubMed] [Google Scholar]
- 23.Soveri I, Berg UB, Björk J, et al. Measuring GFR: a systematic review. Am J Kidney Dis 2014; 64: 411–24. [DOI] [PubMed] [Google Scholar]
- 24.Pottel H, Hoste L, Dubourg L, et al. An estimated glomerular filtration rate equation for the full age spectrum. Nephrol Dial Transplant 2016; 31: 798–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Björk J, Grubb A, Sterner G, Nyman U. Revised equations for estimating glomerular filtration rate based on the Lund-Malmö Study cohort. Scand J Clin Lab Invest 2011; 71:232–9. [DOI] [PubMed] [Google Scholar]
- 26.Pottel H, Björk J, Courbebaisse M, et al. Development and validation of a modified full age spectrum creatinine-based equation to estimate glomerular filtration rate: a cross-sectional analysis of pooled data. Ann Intern Med 2021; 174: 183–91. [DOI] [PubMed] [Google Scholar]
- 27.Grubb A, Horio M, Hansson L-O, et al. Generation of a new cystatin C-based estimating equation for glomerular filtration rate by use of 7 assays standardized to the international calibrator. Clin Chem 2014;60: 974–86. [DOI] [PubMed] [Google Scholar]
- 28.Pottel H, Delanaye P, Schaeffner E, et al. Estimating glomerular filtration rate for the full age spectrum from serum creatinine and cystatin C. Nephrol Dial Transplant 2017;32: 497–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey May 28, 2020. (https://www.cdc.gov/nchs/nhanes/index.htm).
- 30.Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA 2007;298:2038–47. [DOI] [PubMed] [Google Scholar]
- 31.Selvin E, Juraschek SP, Eckfeldt J, Levey AS, Inker LA, Coresh J. Calibration of cystatin C in the National Health and Nutrition Examination Surveys (NHANES). Am J Kidney Dis 2013; 61: 353–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Selvin E, Manzi J, Stevens LA, et al. Calibration of serum creatinine in the National Health and Nutrition Examination Surveys (NHANES) 1988–1994, 1999–2004. Am J Kidney Dis 2007; 50: 918–26. [DOI] [PubMed] [Google Scholar]
- 33.National Kidney Foundation, American Society of Nephrology. Removing race from estimates of kidney function March 9, 2021. (https://www.asn-online.org/about/press/releases/ASN_PR_20210309_Press_release_NKF_A.pdf).
- 34.Hsu C, Yang W, Parikh RV, et al. Race, genetic ancestry, and estimating kidney function in CKD. N Engl J Med 2021;385: 1750–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Levey AS, Tighiouart H, Inker LA. Improving glomerular filtration rate estimation — across the age and diversity spectrum. Ann Intern Med 2020; 174: 265–7. [DOI] [PubMed] [Google Scholar]
- 36.Levey AS, Tighiouart H, Simon AL, Inker LA. Comparing newer GFR estimating equations using creatinine and cystatin C to the CKD-EPI equations in adults. Am J Kidney Dis 2017; 70: 587–9. [DOI] [PubMed] [Google Scholar]
- 37.Stevens LA, Claybon MA, Schmid CH, et al. Evaluation of the Chronic Kidney Disease Epidemiology Collaboration equation for estimating the glomerular filtration rate in multiple ethnicities. Kidney Int 2011; 79: 555–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.National Kidney Foundation, American Society of Nephrology. Establishing a task force to reassess the inclusion of race in diagnosing kidney diseases July 2, 2020. (https://www.kidney.org/news/establishing-task-force-to-reassess-inclusion-race-diagnosing-kidney-diseases).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


