Abstract
Ocular symptoms are a common reason for patients to present to the emergency department or to their primary care physician. Though often benign, these symptoms can also be an early manifestation of systemic disease. We report the case of a patient who presented to the emergency department with 1 week of rash followed by 2 days of fever, sore throat, chills, blurry vision and photophobia. His physical examination was notable for a desquamative rash over his tattoos, left-sided tonsillar exudate and pharyngeal oedema without lymphadenopathy. Biopsy of his tattoos revealed subepithelial non-caseating granulomas, confirming the diagnosis of tattoo granulomas with uveitis. The patient was started on corticosteroids and methotrexate and responded well to treatment. This case emphasises the importance of recognising ocular symptoms that are indicative of systemic disease and require further evaluation.
Keywords: ophthalmology, dermatology, rheumatology, immunology, primary care
Background
Tattoo granulomas are a well-described complication of tattoos. Though this type of complication was initially identified in the skin, the analogous condition of tattoo-associated uveitis was first described by Lubeck et al in 1952.1 Classically associated with systemic sarcoidosis and tattoo granulomas, it more frequently first presents in isolation or without evidence of systemic disease.2–4
Ocular symptoms are a common reason for patients to present to the emergency department or to their primary care physician.5 Though relatively minor conditions such as conjunctivitis, hordeolum or corneal abrasion are the most common diagnoses, ocular symptoms can also be an early manifestation of systemic disease and may require further evaluation.5 Since patients often first present in the primary care setting, it is essential to recognise ‘red flag’ symptoms indicative of severe disease.6
Case presentation
A male patient presented to the emergency department with 1 week of rash followed by 2 days of fever, sore throat, chills, blurry vision and photophobia. His medical history was significant for lower back pain treated with corticosteroid injections. His physical examination was notable for a desquamative rash over his tattoos, left-sided tonsillar exudate and pharyngeal oedema without lymphadenopathy. Ophthalmology was consulted and the ophthalmic examination was notable for bilateral anterior uveitis. Pupils, irides and intraocular pressures were normal. Dilated fundus examination was unremarkable. His best corrected visual acuity was 20/20 bilaterally. A review of systems elicited chronic back pain. He denied any trauma, gastrointestinal upset, joint pain, oral ulcers, sick contacts, sexual exposures, workplace exposures or travel. The patient was started on topical steroid drops 8×/day in both eyes, sent for diagnostic testing and seen in clinic for follow-up 1 week later. His examination at that time was unchanged.
Investigations
The patient’s diagnostic testing was notable for an ACE level of 86 nmol/mL/min, with the upper limit of normal being 40 nmol/mL/min. The erythrocyte sedimentation rate (ESR) and C reactive protein (CRP) level were also elevated. Complete blood count (ie, haemoglobin, hematocrit, white blood cell count and platelet count) and serum chemistry panel (ie, serum electrolytes, blood urea nitrogen and creatine) were within normal limits. A viral swab and COVID-19 test were negative. Blood cultures, fluorescent treponemal antibody absorption (FTA-ABS), human leucocyte antigen B27 (HLA-B27), interferon-gamma release assay (IGRA), Lyme antibodies, anti-herpes simplex virus (HSV) 1 and 2 antibodies, anti-varicella zoster (VZV) antibodies, chest radiography and pulmonary function testing were normal. Biopsy of the patient’s tattoos revealed subepithelial non-caseating granulomas (figure 1).
Figure 1.
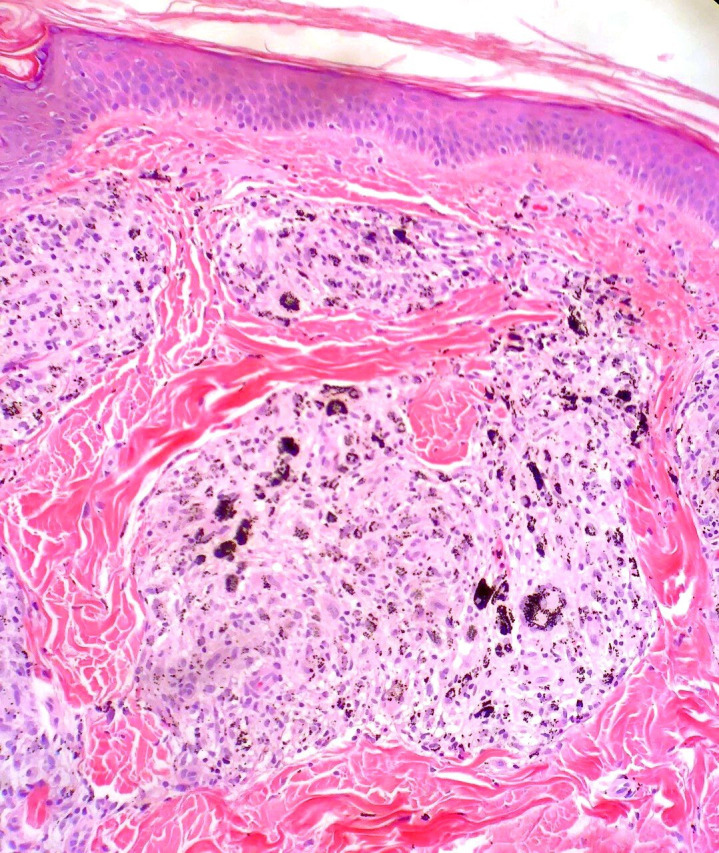
Skin punch biopsy demonstrating a non-caseating granuloma (H&E stain, objective magnification ×10).
Differential diagnosis
Given the patient’s presenting symptoms of bilateral anterior uveitis, tattoo-associated rash, elevated ACE and history of chronic back pain, the differential diagnosis included viral uveitis, ankylosing spondylitis, Lyme disease and tattoo granulomas with uveitis. Lower on the differential were tuberculoid leprosy, tuberculosis and secondary syphilis.
Though the history of fever is consistent with viral uveitis, the dermatologic findings, normal intraocular pressures and negative HSV/VZV titers made this diagnosis less likely. Lower back pain with uveitis could be consistent with ankylosing spondylitis, though lower back pain is a very non-specific symptom. Negative HLA-B27 and a history of normal sacroiliac imaging made this diagnosis less likely. Given that the patient lived in an endemic area for Lyme disease and presented with symptoms consistent with early disseminated Lyme disease, serologic testing for Lyme disease was obtained and was found to be negative. Additionally, the localisation of the skin reactions to tattoo sites would not be consistent with Lyme disease.
Tuberculoid leprosy could also be consistent with this constellation of symptoms, tattoo reactions and non-caseating granulomas on biopsy; however, this was considered unlikely due to the low prevalence of leprosy in the USA and absence of travel history. Similarly, though tuberculosis and secondary syphilis can present with similar findings, the absence of travel history and sexual history, respectively, made these diagnoses unlikely. Tuberculosis was ruled out with a negative IGRA, and FTA-ABS was used to rule out syphilis.
The chronology of tattoo rash followed by fever and uveitis most favoured the diagnosis of tattoo granulomas with uveitis. The elevated ACE, ESR, and CRP, though non-specific, are also consistent with this diagnosis. Ultimately, the presence of non-caseating granulomas on skin biopsy and the positive response to immunosuppressive therapy made this the most likely diagnosis.
Outcome and follow-up
The patient was started on 40 mg of prednisone daily with improvement in his rash, photophobia and severity of ocular inflammation. He was referred to rheumatology for initiation of immunomodulatory treatment. The patient was subsequently started on 15 mg of methotrexate/week and tapered off oral steroids with good response to treatment. He was asymptomatic at his 2-month follow-up visit.
Discussion
Granulomatous inflammatory reactions are a well-described complication of tattoos and have a strong male preponderance.2 Granulomatous reactions can occur 6–20 months after initial tattooing and can affect multiple tattoos and scars.2 7 Skin manifestations include scattered papules or nodules, scaling, induration, pruritus and tenderness and are typically limited to the tattoo site.6 Although no clear trigger has been described, interferon therapy for hepatitis C, highly active antiretroviral therapy for HIV and influenza vaccination have been proposed as instigating factors.2 8 9 Proposed mechanisms include that a component in the tattoo ink induces either a foreign body or sarcoid-type reaction or that there is an allergic response secondary to a delayed-type hypersensitivity reaction.10–13
Although granulomatous reactions to tattoos are relatively common, ocular inflammation associated with tattoo granulomas is uncommon. In one retrospective chart review of patients with sarcoidosis and tattoo granulomas, 9% of cases displayed ocular inflammation.2 Ocular manifestations can present simultaneously with dermatologic manifestations or up to several months later.7 The most common ocular manifestation is anterior uveitis, though panuveitis, posterior uveitis, retinal vasculitis, cystoid macular oedema and lacrimal gland involvement have also been reported.2 4 Ocular signs and symptoms include ciliary flush, miosis, blurred vision, worsening eye pain and photophobia. If tattoo granulomas with uveitis are suspected, skin biopsy should be performed to confirm the diagnosis given the accessibility and ease of obtaining tissue.2 Further immunosuppressive or immunomodulatory treatment should be delayed if possible until after skin biopsy is obtained to increase diagnostic yield and to have pathologic confirmation of the diagnosis.
Tattoo granulomas with uveitis are uncommon, but can be the first presenting symptom in patients with systemic sarcoidosis. For this reason, it is important to consider it in patients presenting with ocular symptoms, especially given the 10%–25% prevalence of cosmetic tattoos in western populations.9 Patients presenting with red eye and findings concerning for uveitis, such as worsening vision, severe pain and photophobia, should be asked about their tattoos. A careful history should be obtained along with a thorough physical examination including assessment of the skin, auscultation of the lungs and palpation for lymphadenopathy. Additionally, patients should undergo laboratory workup, pulmonary function testing and chest imaging. Whether tattoo granulomas are the trigger for systemic sarcoidosis or a manifestation of latent disease remains unknown, but the importance of physician awareness of this entity is key to ensuring a timely diagnosis and prompt treatment for patients.
Learning points.
Severe systemic diseases may first present with ocular symptoms.
It is essential to perform a complete physical examination, including dermatologic assessment, in patients who present with concerning eye symptoms.
Tattoo granulomas with uveitis can be the first presenting symptom in patients with systemic sarcoidosis and warrant a prompt systemic workup.
Footnotes
Contributors: AA-A reviewed the relevant literature and contributed to the preparation of the manuscript. NA participated in the initial evaluation of the patient and in the preparation of the manuscript. NK was involved in the evaluation of the patient and in the preparation of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Lubeck G, Epstein E. Complications of tattooing. Calif Med 1952;76:83. [PMC free article] [PubMed] [Google Scholar]
- 2.Kluger N. Tattoo-associated uveitis with or without systemic sarcoidosis: a comparative review of the literature. J Eur Acad Dermatol Venereol 2018;32:1852–61. 10.1111/jdv.15070 [DOI] [PubMed] [Google Scholar]
- 3.Klímová A, Heissigerová J, Říhová E, et al. Tattoo-associated uveitis. Cesk Slov Oftalmol 2017;73:30–3. [PubMed] [Google Scholar]
- 4.Moschos MM, Guex-Crosier Y. Retinal vasculitis and cystoid macular edema after body tattooing: a case report. Klin Monbl Augenheilkd 2004;221:424–6. 10.1055/s-2004-812815 [DOI] [PubMed] [Google Scholar]
- 5.Pflipsen M, Massaquoi M, Wolf S. Evaluation of the painful eye. Am Fam Physician 2016;93:991–8. [PubMed] [Google Scholar]
- 6.Ramanayake RPJC, Basnayake BMTK. Evaluation of red flags minimizes missing serious diseases in primary care. J Family Med Prim Care 2018;7:315–8. 10.4103/jfmpc.jfmpc_510_15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kluger N. Sarcoidosis on tattoos: a review of the literature from 1939 to 2011. Sarcoidosis Vasc Diffuse Lung Dis 2013;30:86–102. [PubMed] [Google Scholar]
- 8.Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med 2007;357:2153–65. 10.1056/NEJMra071714 [DOI] [PubMed] [Google Scholar]
- 9.Kluger N. Epidemiology of tattoos in industrialized countries. Curr Probl Dermatol 2015;48:6–20. 10.1159/000369175 [DOI] [PubMed] [Google Scholar]
- 10.Dickinson JA. Sarcoidal reactions in tattoos. Arch Dermatol 1969;100:315–9. 10.1001/archderm.1969.01610270057013 [DOI] [PubMed] [Google Scholar]
- 11.Mansour AM, Chan CC. Recurrent uveitis preceded by swelling of skin tattoos. Am J Ophthalmol 1991;111:515–6. 10.1016/S0002-9394(14)72395-5 [DOI] [PubMed] [Google Scholar]
- 12.Rorsman H, Brehmer-Andersson E, Dahlquist I, et al. Tattoo granuloma and uveitis. Lancet 1969;2:27–8. 10.1016/S0140-6736(69)92600-2 [DOI] [PubMed] [Google Scholar]
- 13.Ostheimer TA, Burkholder BM, Leung TG, et al. Tattoo-associated uveitis. Am J Ophthalmol 2014;158:637–43. 10.1016/j.ajo.2014.05.019 [DOI] [PubMed] [Google Scholar]


