Abstract
Objective:
To compare the effects of sodium fluoride mouth rinse, casein phosphopeptide-amorphous calcium phosphate (CPP-ACP), and the microabrasion technique in treating white spot lesions.
Materials and Methods:
The study population consisted of 80 patients (46 females, 34 males; 966 affected teeth) who had developed multiple decalcified enamel lesions after fixed orthodontic therapy. The study population was divided into four groups of 20 patients each. The control group (group I) participants were to just brush their teeth, the fluoride group (group II) participants were instructed to use 20 ml of neutral 0.025% sodium fluoride rinse, the participants in the CPP-ACP group (group III) were instructed to use tooth mousse twice a day in addition to fluoride toothpaste for 6 months, and the participants in the microabrasion group (group IV) were to undergo treatment by the microabrasion technique, which is a commonly used mixture of 18% hydrochloric acid. Data were analyzed with the generalized linear mixed model and Tukey HSD at the P < .05 level.
Results:
The area of the white spot lesions decreased significantly in all groups. Inter group differences in the treatment success rates were significant. The highest success rate was observed for group IV (97%). The success rate of group III (58%) was significantly higher than that of groups II (48%) and I (45%).
Conclusions:
The use of CPP-ACP can be more beneficial than fluoride rinse for postorthodontic remineralization. Microabrasion is an effective treatment for cosmetic improvement of long-standing white spot lesions.
Keywords: Enamel demineralization, Fluoride, CPP-ACP, Microabrasion
INTRODUCTION
White spot lesions affect many orthodontic patients who show poor compliance with intratreatment oral hygiene and preventive advice.1,2 The presence of fixed orthodontic appliances further affects oral hygiene and makes the cleaning of teeth more difficult; hence, accumulation of plaque around brackets and bands increases, which causes enamel demineralization.3 In addition, factors such as appliance design, improper use of cement lute, salivary flow and composition, enamel susceptibility, and, of course, dietary practices greatly influence the development of white spot lesions.4 Estimates of the overall prevalence of white spot lesions arising during fixed appliance therapy range was widely from 2% to 96%.5
Restorative treatment is the conventional approach for treating white spot lesions; however, this technique has the disadvantage of being invasive.6 If salivary or plaque calcium, phosphate ions, and fluoride ions are present in adequate amounts, they can also promote the remineralization of previously demineralized enamel. Therefore, fluoride application can be used to promote remineralization after debonding.7 The use of casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) has been reported to induce remineralization because of its ability to stabilize calcium and phosphate in an amorphous state, preventing the accumulation of calcium phosphate to a critical amount that leads to precipitation.8,9 The potential of CPP-ACP in promoting remineralization was demonstrated in animal caries models in 1995, but it was used for the first time in treating white spot lesions in 2009.10 The use of the microabrasion technique was also advocated for the removal of postorthodontic demineralized white spot lesions.11 Microabrasion has long been widely used for the removal of superficial noncarious enamel defects.11,12 Recently, this conservative technique was advocated for the removal of white spot lesions as well.13
A review of the literature showed that there were no comparative studies on the different methods for treating white spot lesions. The purpose of this in vivo study was to determine the effectiveness of fluoride mouth rinse, CPP-ACP crème, and the microabrasion technique in reducing white spot lesions. The null hypothesis to be tested was that there is no statistically significant difference between the treatment and control groups.
MATERIALS AND METHODS
Potential study participants were selected by analyzing a database of patients with postorthodontic demineralized lesions who had undergone treatment at the Orthodontic Department of Dentistry, Faculty of Selçuk University, Konya, Turkey. Ethical approval for this study was obtained from the Selçuk University Meram Medicine Faculty Research Ethics Committee, and informed written consent was obtained from all the study participants.
Study Design
The study was an experimental prospective clinical controlled trial with four parallel groups. Participants who developed postorthodontic demineralized white spot lesions following fixed appliance therapy were offered the opportunity to enroll into the study and to join one of the groups (control group, fluoride rinsing group, CPP-ACP crème group, and microabrasion group). Initial photographic records of the participants who had enrolled in the study were obtained. The records were grouped according to the date of debonding. Inclusion criteria are listed in Table 1.
Table 1.
Inclusion Criteria
The power analysis was established by G*Power version 3.0.10 (Franz Faul Universitat, Kiel, Germany) software. Based on the 1∶1 ratio between groups, a sample size of 20 participants per group would give more than 80% power to detect significant differences with a 0.40 effect size and at the α = .05 significance level.
A total of 145 participants and their families provided consent for participation in our study. However, only 80 of the 145 participants actually attended their appointments. Twenty participants from every group participated and attended their appointments and thus helped complete the study. Appointments were given to all the participants except for those in the microabrasion group at 1-month intervals for checkup and administration of new agent.
Mouth Rinse Treatment
The fluoride rinse, neutral 0.025% sodium fluoride (Colgate Plax, Colgate-Palmolive, Herstal, Belgium), was given to each patient with instructions to use a measured quantity (20 ml accurately dispensed from the bottle dosimeter) for 30 seconds twice daily, after breakfast and before bedtime. The mouth rinse had an effective sodium-fluoride content of 100 ppm, as recommended by various authorities.14,15 Rinsing was done immediately after brushing with toothpaste containing fluoride. Eating and drinking were prohibited for 30 minutes after rinsing. The second set of records was obtained after a 6-month period, during which the participants were asked to follow the same mouth-rinsing regimen.
CPP-ACP Treatment
Participants applied the topical crème CPP-ACP (GC Tooth Mousse, Asia Pty. Ltd, Japan) to the tooth surfaces by using a clean finger twice a day, after brushing their teeth. A minimum of a pea-sized amount of crème was considered necessary for each dental arch. For areas that are difficult to reach (between the teeth), patients were advised to use an interproximal tooth-cleaning brush. The CPP-ACP crème was left undisturbed on the teeth by asking the participants to ensure that they kept their mouths open at least for 3 minutes after applying the crème. Eating and drinking were prohibited for 30 minutes after application.
Microabrasion Treatment
Appointments were scheduled for participants of the microabrasion group. Each patient underwent the procedure described by Welbury and Carter11 and Croll and Cavanaugh,12 which was performed by the same operator. Eighteen percent hydrochloric acid was mixed with fine pumice powder to obtain a slurry form. The affected teeth were cleaned slowly with pumice and water by using a rubber cup in a contra-angle handpiece. A rubber dam was used to isolate these teeth from the rest so as to eliminate the chemical effects of microabrasion. This mixture was applied to the buccal surface of each tooth to be treated. The slurry was agitated into the tooth surface for 30 seconds and then washed off with an air-water spray. The cycle of microabrasion procedure and washing was repeated three to four times on each affected tooth. The patients underwent four or five sessions of the microabrasion therapy at an interval of 2 weeks, as necessary.
Image Acquisition
The participants were examined while they were seated on a dental chair; the examinations were conducted when the participants had dry tooth surfaces after undergoing debonding procedure. All premolars, canines, and incisors of each participant were examined for the presence of white spot lesions. All the determined lesions were recorded, and preorthodontic treatment photographs were examined to ensure that no lesions were visible before the orthodontic treatment. In addition to photographic records of the debonding, standardized intraoral images were taken perpendicular to the affected surface of every tooth of each patient by using a digital camera (Nikon D80, Nikon Corporation, Tokyo, Japan). The images were taken after debonding and after 6 months of treatment for every group, except the microabrasion group; in this group, follow-up photographic records were taken after the patients' final microabrasion treatment. To avoid the potential side effect of light reflections, stable illumination with ring-flash and cross-polarizing filters was used.
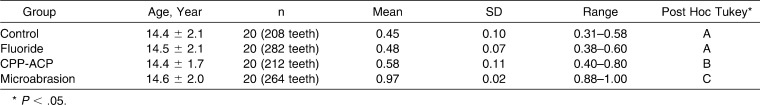
Image-processing software (AutoCAD-2011, Autodesk Inc, San Rafael, Calif) was used to quantify the size (in mm2) of the visible areas of the demineralized lesions and the size of the affected tooth's vestibular surface (Figure 1). After determination of both of these values, the area affected by demineralization was expressed as a percentage of the total tooth surface. The images were reanalyzed after a month to determine the reproducibility of the method. Thus, the extent of white spot lesion formation was determined. The severity of the lesion was scored from 1 to 3, similar to the system used by Curzon and Spector16 and listed in Table 2.
Figure 1.
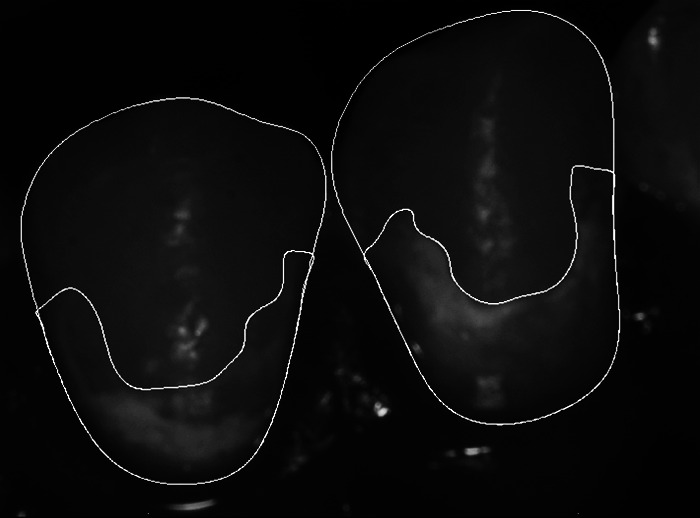
A white spot lesion outlined on the labial surface of affected tooth from a sample using the image analysis program.
Table 2.
The Lesion Was Scored for Each Third of the Vestibular Surface of Each Tooth as Followsa
We determined the extent of lesion formation again after the patients had completed their respective treatment regimens. The success rate of treatment for each tooth was determined by comparing the extent of white spot lesion formation before and after treatment by using the following formula:
 |
Statistical Analysis
All statistics were performed with SPSS version 17.0 (SPSS Inc, Chicago, Ill). The normality test of Shapiro-Wilks and the Levene's variance homogeneity test were applied to the data. The data were found normally distributed, and there was homogeneity of variance among the groups. Descriptive statistics were calculated for each of the groups tested. A paired-sample t-test was used to determine the differences in the mean changes within each treatment group. Statistical differences were checked by generalized linear mixed model (GLMM) for general groups, and after classification, if differences were found between the groups, the Tukey HSD multiple comparison test was used. Significance for all statistical tests was predetermined at P < .05.
RESULTS
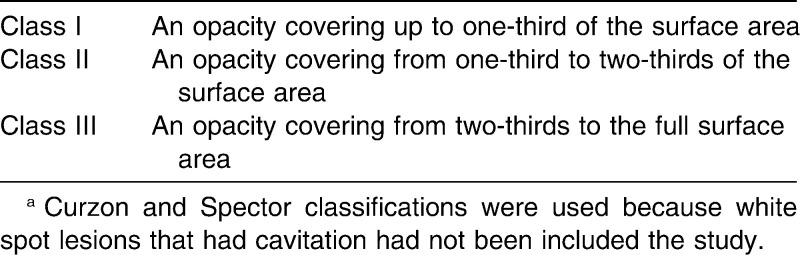
Descriptive statistics and comparison of the percentages of white spot lesions in the treatment and control groups are listed in Table 3. The mean degree of white spot lesion decreased during the follow-up period. According to the results of the paired-samples t-test, statistically significant differences were found between the pretreatment and posttreatment extent of white spot lesions. The difference was statistically significant at P < .001 for all groups.
Table 3.
Descriptive Statistics and Statistical Comparison of Pretreatment and Posttreatment White Spot Lesion Percentage (%)a
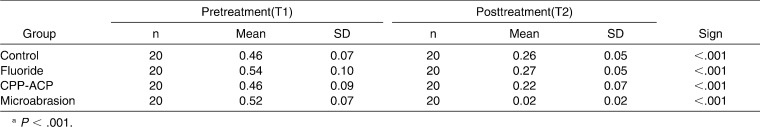
The descriptive statistics for success rates of the different treatments are listed in Table 4. The results of GLMM showed that differences between the four groups were significant (P < .001). Thus, our null hypothesis for this study was rejected. The Tukey HSD test showed that the success rate of group IV was the highest (P < .001). The next highest success rate was for group III (P < .05), which was higher than that of group II and group I. We found no significant differences between the success rates of treatment in groups I and II (P > .05).
Table 4.
Descriptive Statistics and Statistical Comparison of Success Rate (%)
The results of the GLMM indicated that differences between the groups (P < .001) and between lesion classes (P < .001) were significant, and there was interaction between the groups and classes (P < .001). Participant groups and lesion classes were then subjected to a post hoc test with the Tukey HSD adjustment to evaluate the reduction of white spot lesions during treatment. The descriptive statistics for success rates of treatment in the participant groups and lesion classes and their post hoc comparisons are listed in Table 5. The results of the reduction of white spot lesion, with standard deviations, are shown in Figure 2.
Table 5.
Descriptive Statistics and Statistical Comparison of Success Rate of Groups With Classes (%)
Figure 2.
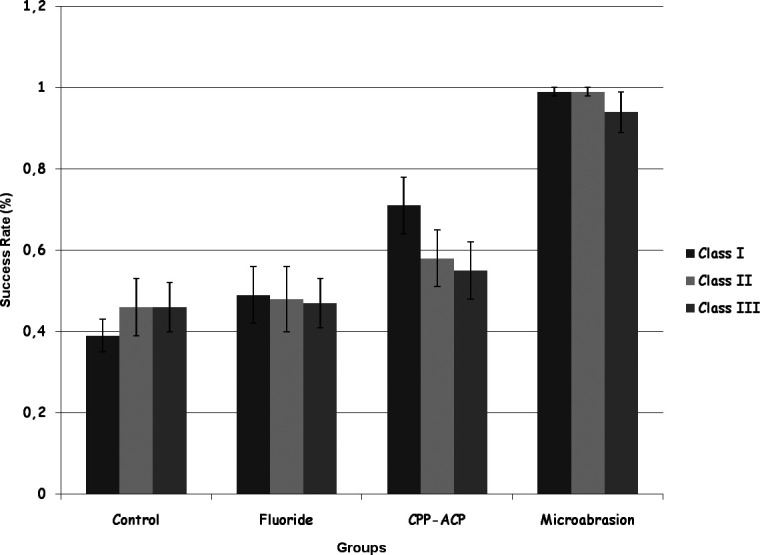
Histogram showing the success rates and standard deviations of groups and classes.
DISCUSSION
This study was performed to determine which treatment method is most successful in treating postorthodontic demineralized white spot lesions. The methods employed were fluoride mouth rinse, topical application of CPP-ACP, and microabrasion. The results of all the treatment groups were compared with those of a control group.
Accumulation of plaque and cariogenic microorganism around orthodontic appliances has been reported to increase significantly during orthodontic treatment. Removal of fixed orthodontic appliances results in substantial reduction of the levels of cariogenic challenge and facilitates subsequent remineralization of white spot lesions.17,18 The mineral content of dental enamel is in equilibrium with its environment, and saliva contains all the necessary elements for hydroxyapatite crystal growth. In the natural state, demineralization and remineralization take place continuously15; this equilibrium is restored following the completion of fixed orthodontic treatment. Good oral hygiene with a standard fluoridated dentifrice, used daily, is prescribed for the prevention of white spot lesions.19 The additional use of sodium fluoride rinses (twice daily) and CPP-ACP products can be effective in remineralizing the demineralized enamel.20 Reynolds21 reported that CPP-ACP, which is derived from milk casein, was capable of being absorbed through the enamel surface and could affect the demineralization-remineralization processes.
The results of this study showed that the size reduction of postorthodontic white spot lesions when using a low-fluoride mouth rinse was not significantly different from that in a control group. Fluoride mouth rinse was effective only on mild lesions. Other studies tried to determine the effect of fluoride mouth rinse on all types of white spot lesions and did not classify the lesions on the basis of their size. Willmot15 found no significant difference, while studies by Linton22 and Lagerweij et al.23 reported a therapeutic effect of low-fluoride mouth rinse. This can be explained by the mechanism by which fluoride takes effect. Small lesions are relatively shallow, and fluoride can therefore easily support remineralization.14,24 Although CPP-ACP generally supports the remineralization of white spot lesions better than fluoride mouth rinse does, the differences were not significant for moderate and severe lesions. CPP-ACP was found to be more effective in treating mild lesions than moderate and severe lesions. This could confirm the previously reported therapeutic effects of CPP-ACP products.9
The use of a slurry of hydrochloric acid and pumice in the microabrasion technique yielded dramatic cosmetic results.13 Microabrasion is an effective therapy for improving postorthodontic demineralized lesions.13 Initially, every clinician is wary of removing too much enamel material. The erosive and abrasive potential of the microabrasion procedure depends on several parameters, such as the acid used, its concentration and pH, abrasive medium, time of instrumentation, force applied, and revolutions per minute (rpm). Waggoner et al.25 reported an average removal of 12 µm of enamel material after the initial application and an average of 26 µm of enamel loss after each successive application when using 18% hydrochloric acid-pumice mixture. Murphy et al.13 showed 83% success in the reduction of white spot lesions by microabrasion. In our study, we achieved success rates of 99% for mild and moderate lesions and 94% for severe lesions. In the present study, the microabrasion method was applied a maximum of 5 times on each tooth. After treatment, a small affected area remained due to cavitation. We observed cavitation in some teeth during the procedure. Enamel from the more affected surface was more easily removed than from the other surface.
Computer-assisted image analysis of photographic records is increasingly used in the evaluation of white spot lesion treatments.13,26 This digital system has many advantages: records are permanent and they can be examined later and reexamined multiple times, photographs can be digitized and classified independently by many examiners, and the severity of the lesion can be measured by measuring the colors' degree.26
A distinct disadvantage of fixed orthodontic therapy is the formation of decalcification, or white spot lesions, adjacent to brackets and the lack of oral hygiene during the course of the treatment. Although the present study showed a reduction in the area of the white spot lesions, it might also be interesting to investigate changes in the other characteristics of the lesions. A limitation of this study was that only the surface areas of the lesions were determined. Ideally, a future study should examine the surface areas of the white spot lesions along with their depth and softness.
Our findings provide some solutions regarding the ideal method for treating white spot lesions. Considering the limitations of our in vivo study, it can be inferred that microabrasion would be more beneficial than the other methods for treating patients with white spot lesions. Although CPP-ACP had side effects, it is better than fluoride mouth rinse, which also induces remineralization of white spot lesions. The use of topical fluoride would be ideal in poorly compliant patients who have not yet developed enamel lesions.4,7,15,20 The microabrasion method can minimize esthetic damage and prevent the need for future restorative intervention. However, further investigation of the clinical effectiveness of the microabrasion technique, CPP-ACP, fluoride mouth rinse, and other topical agents in white spot lesion treatment would be required to confirm these findings.
CONCLUSIONS
Considering the limitations of any in vivo study, the following clinical conclusions can be drawn.
The size of a white spot lesion can reduce over time; CPP-ACP and fluoride agents support increased remineralization of the demineralized enamel.
Microabrasion is the best method for the cosmetic treatment of these postorthodontic demineralized white spot lesions.
Acknowledgments
This study is produced from the PhD thesis of Mehmet Akin and supported by Selçuk University Research Projects (10202015).
REFERENCES
- 1.Gorelick L, Geiger A, Gwinnet A. J. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–98. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 2.Øgaard B. Prevalence of white spot lesions in 19 year olds: a study on untreated and orthodontically treated persons 5 years after treatment. Am J Orthod Dentofacial Orthop. 1989;98:423–437. doi: 10.1016/0889-5406(89)90327-2. [DOI] [PubMed] [Google Scholar]
- 3.Van Der Linden R. P, Dermaut L. R. White spot formation under orthodontic bands cemented with glass ionomer with or without fluor protector. Eur J Orthod. 1998;20:219–224. doi: 10.1093/ejo/20.3.219. [DOI] [PubMed] [Google Scholar]
- 4.Dijkman A, Arends J. Mineral distribution in human enamel after in-vivo demineralisation by dental plaque. In: Leach S. A, editor. Proceedings of Workshop; Antalya Turkey; 1985. Oxford: IRL Press; 1985. [Google Scholar]
- 5.Mizrahi E. Enamel demineralization following orthodontic treatment. Am J Orthod. 1982;82:62–67. doi: 10.1016/0002-9416(82)90548-6. [DOI] [PubMed] [Google Scholar]
- 6.Maltured M. I. Minimally invasive restorative dentistry: a biomimetic approach. Pract Proced Aesthet Dent. 2006;18:409–414. [PubMed] [Google Scholar]
- 7.Reynolds E. C, Cai F, Cochrane N. J, Shen P, Walker G. D, Morgan M. V, Reynolds C. Fluoride and casein phosphopeptide-amorphous calcium phosphate. J Dent Res. 2008;87:344–348. doi: 10.1177/154405910808700420. [DOI] [PubMed] [Google Scholar]
- 8.Rose R. K. Effects of an anticariogenic casein phosphopeptide on calcium diffusion in streptococcal model dental plaques. Arch Oral Biol. 2000;45:569–575. doi: 10.1016/s0003-9969(00)00017-0. [DOI] [PubMed] [Google Scholar]
- 9.Shen P, Cai F, Nowicki A, Vincent J, Reynolds E. C. Remineralization of enamel subsurface lesions by sugar-free chewing gum containing casein phosphopeptide-amorphous calcium phosphate. J Dent Res. 2001;80:2066–2070. doi: 10.1177/00220345010800120801. [DOI] [PubMed] [Google Scholar]
- 10.Bailey D. L, Adams G. G, Tsao C. E, Hyslop A, Escobar K, Manton D. J, Reynolds E. C, Morgan M. V. Regression of post-orthodontic lesions by a remineralizing cream. J Dent Res. 2009;88:1148–1153. doi: 10.1177/0022034509347168. [DOI] [PubMed] [Google Scholar]
- 11.Welbury R. R, Carter N. E. The hydrochloric acid-pumice microabrasion technique in the treatment of post-orthodontic decalcification. Br J Orthod. 1993;20:181–185. doi: 10.1179/bjo.20.3.181. [DOI] [PubMed] [Google Scholar]
- 12.Croll T. P, Cavanaugh R. R. Enamel color modification by controlled hydrochloric acid-pumice abrasion. I. Technique and examples. Quintessence Int. 1986;17:81–87. [PubMed] [Google Scholar]
- 13.Murphy T. C, Willmot D. R, Rodd H. D. Management of postorthodontic demineralized white lesions with microabrasion: a quantitative assessment. Am J Orthod Dentofacial Orthop. 2007;131:27–33. doi: 10.1016/j.ajodo.2005.04.041. [DOI] [PubMed] [Google Scholar]
- 14.Ogaard B, Rolla G, Arends J, Ten Cate J. J. Orthodontic appliances and enamel demineralization part 2: prevention and treatment of lesions. Am J Orthod Dentofacial Orthop. 1988;93:123–128. doi: 10.1016/0889-5406(88)90360-5. [DOI] [PubMed] [Google Scholar]
- 15.Willmot D. R. White lesions after orthodontic treatment: does low fluoride make a difference. J Orthod. 2004;31:235–242. doi: 10.1179/146531204225022443. [DOI] [PubMed] [Google Scholar]
- 16.Curzon M. E, Spector P. C. Enamel mottling in a high strontium area of the U.S.A. community. Dent Oral Epidemiol. 1977;5:243–247. doi: 10.1111/j.1600-0528.1977.tb01648.x. [DOI] [PubMed] [Google Scholar]
- 17.Corbett J. A, Brown L. R, Keene H. J, Horton T. M. Comparison of Streptococcus mutans concentrations in non-bonded and bonded orthodontic patients. J Dent Res. 1981;60:1936–1942. doi: 10.1177/00220345810600120301. [DOI] [PubMed] [Google Scholar]
- 18.Mattingly J. A, Sauer G. J, Yancey J. M, Arnold R. R. Enhancement of Streptococcus mutans colonization by direct bonded orthodontic appliances. J Dent Res. 1983;62:1209–1211. doi: 10.1177/00220345830620120601. [DOI] [PubMed] [Google Scholar]
- 19.Bibby B. G. Test of the effect of fluoride-containing dentifrices on dental caries. J Dent Res. 1945;24:297–303. doi: 10.1177/00220345450240060301. [DOI] [PubMed] [Google Scholar]
- 20.Zahradnik R. T. Effect of fluoride rinses upon in vitro enamel remineralization. J Dent Res. 1980;59:1065–1066. doi: 10.1177/00220345800590061001. [DOI] [PubMed] [Google Scholar]
- 21.Reynolds E. C. The prevention of sub-surface demineralization of bovine enamel and change in plaque composition by casein in an intra-oral model. J Dent Res. 1987;66:1120–1127. doi: 10.1177/00220345870660060601. [DOI] [PubMed] [Google Scholar]
- 22.Linton J. L. Quantitative measurements of remineralization of incipient caries. Am J Orthod Dentofacial Orthop. 1996;110:590–597. doi: 10.1016/s0889-5406(96)80034-5. [DOI] [PubMed] [Google Scholar]
- 23.Lagerweij M. D, Damen J. J. M, Stookey G. K. Remineralisation of small lesions by fluoride. J Dent Res. 1997;76(Special issue):16. [Google Scholar]
- 24.Mizrahi E. Surface distribution of enamel opacities following orthodontic treatment. Am J Orthod. 1983;84:323–331. doi: 10.1016/s0002-9416(83)90348-2. [DOI] [PubMed] [Google Scholar]
- 25.Waggoner W. F, Johnston W. M, Schumann S, Schikowski S. Microabrasion of human enamel in vitro using hydrochloric acid and pumice. Pediatr Dent. 1989;11:319–323. [PubMed] [Google Scholar]
- 26.Benson P. E. Evaluation of white spot lesions on teeth with orthodontic brackets. Semin Orthod. 2008;14:200–208. [Google Scholar]