Abstract
Objective:
To test the null hypothesis that the presence of alveolar defects (dehiscence and fenestration) was not different among patients with different vertical growth patterns.
Materials and Methods:
A total of 1872 teeth in 26 hyper-divergent (mean age: 24.4 ± 4.8 years), 27 hypo-divergent (mean age: 25.1 ± 4.5 years), and 25 normo-divergent (mean age: 23.6 ± 4.1 years) patients with no previous orthodontic treatment were evaluated using cone-beam computed tomography. Axial and cross-sectional views were evaluated with regard to whether dehiscence and/or fenestration on buccal and lingual surfaces existed or not. For statistical analysis, the Pearson chi-square test was used at a P < .05 significance level.
Results:
According to the statistical analysis, the hypo-divergent group (6.56%) had lower dehiscence prevalence than the hyper-divergent (8.35%) and normo-divergent (8.18%) groups (P = .004). Higher prevalences of dehiscence and fenestration were found on buccal sides in all vertical growth patterns. While fenestration was a common finding for the maxillary alveolar region, dehiscence was a common finding in the mandible in all groups.
Conclusion:
The null hypothesis was rejected. Although the prevalence of fenestrations was not different, significant differences for dehiscences were found in patients with different vertical growth patterns.
Keywords: Orthodontics, Cone-beam computed tomography, Fenestration, Dehiscence
INTRODUCTION
Orthodontic tooth movement is induced by mechanical stimuli and facilitated by remodeling of the periodontal ligament and alveolar bone. Absent or insufficient alveolar bone thickness is a complicating factor for orthodontic treatment.1 The biologic and biomechanical factors are closely related and determine the potential side effects of orthodontic treatment, such as external root resorption, gingival recession, dehiscence, and fenestration.2
The lack of facial or lingual cortical plates, which results in exposing the cervical root surface and affecting the marginal bone, represents an alveolar defect called dehiscence. When there is still some bone in the cervical region, the defect is termed fenestration.3
The occurrence of dehiscence and fenestration during orthodontic treatment depends on several factors, such as the direction of movement, the frequency and magnitude of orthodontic forces, and the volume and anatomic integrity of periodontal tissues.4 Before orthodontic treatment, alveolar morphology must be determined through imaging to avoid these problems.5
There are three basic types of facial vertical growth pattern: hypo-divergent (low angle), normo-divergent (average), and hyper-divergent (high angle) growth patterns.6 The hyper-divergent pattern is typified by excessive vertical facial growth. It is usually associated with anterior open bite and an increased sella-nasion (SN)–mandibular plane (MP) angle, gonial angle, and maxillary/mandibular planes angle.7 The hypo-divergent pattern is typified by reduced vertical growth. It is usually accompanied by deep anterior overbite, reduced facial heights, and reduced SN-MP angle.8 Between the two types lays the normo-divergent facial growth pattern. The relationship between bite force and craniofacial morphology has been investigated.9 The mean bite force in the molar region was reported to be twice as great for normo-divergent subjects as compared with hyper-divergent subjects, while hypo-divergent subjects have still higher maximum forces than normo-divergent subjects.10
Imaging modalities, including periapical and panoramic radiographs, have been used in maxillofacial fields over the past few decades; however, entirely satisfactory results are not attainable. Until the introduction of computerized tomography (CT), visualization of dehiscences and fenestrations was not possible with traditional two-dimensional methods because of the superimposition of contralateral cortical bony or dental structures.11 The development of CT and especially cone-beam CT (CBCT) has provided the means with which to visualize these defects three dimensionally (3D).12 CBCT was specifically developed for the maxillofacial region to provide comparable images to conventional CT at a reduced radiation dose and cost.13 CBCT reconstructions have smaller voxels in comparison with conventional CT, which could be advantageous in obtaining more accurate 3D surface models of teeth crowns.14 However, CBCT subjective image quality is still inferior in comparison with that of conventional CT.15
Alveolar defects have been evaluated with CT,16,17 but few studies5 have compared the presence of alveolar defects in untreated subjects with different vertical growth patterns with CBCT. Thus, the aim of this study was to evaluate the presence of dehiscence and fenestration among different vertical growth patterns by means of CBCT.
MATERIALS AND METHODS
A power analysis established by G*Power Ver. 3.0.10 (Franz Faul, Universität Kiel, Kiel, Germany) software, based on a 1∶1 ratio among groups, and a sample size of 24 patients would give more than 75% (actual power = 0.7554) power to detect significant differences with 0.40 effect size and at the α = .05 significance level (critical χ2 = 11.0704; noncentrality parameter λ = 10.5600).
Permission was obtained from the University Human Research Regional Ethical Committee at Erciyes University after the Research Scientific Committee at the same institution had approved the experimental protocol. The patients were selected from the archives of the Oral and Maxillofacial Radiology Department and were called for a second intraoral examination. If the individuals met the inclusion criteria, they were informed about the research and usage purpose of their CBCT scans. Volunteers were asked to complete an informed consent form.
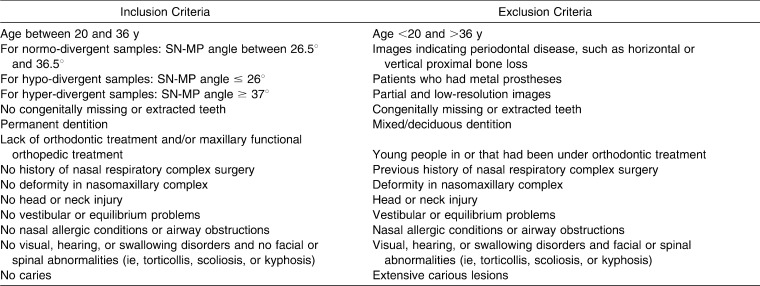
CBCTs of these patients had been taken at their usual records appointment as a part of the necessary radiographs; therefore, they were not unnecessarily subjected to additional radiation. The CBCT images of 78 patients (aged 20–36 years) were analyzed. All measurements were made by the same observer (F.I.U.), who is experienced in CBCT scans. The criteria for sample selection are presented in Table 1.
Table 1.
Criteria for Sample Selection
These scans were obtained using CBCT (iCAT®, Model 17–19, Imaging Sciences International, Hatfield, Pa) with a single 360° rotation and a voxel size of 0.3 mm at the following settings: the x-ray emission time was 3.5 seconds; exposures were made with 5.0 mA, 120 kV, and an exposure time of 4 seconds; and the axial slice thickness was 0.3 mm.
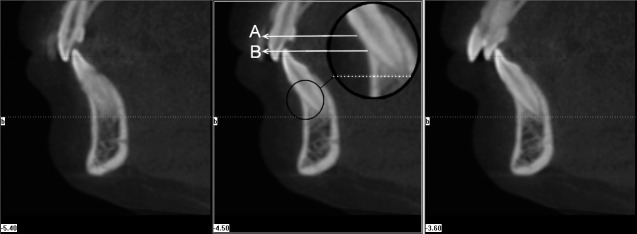
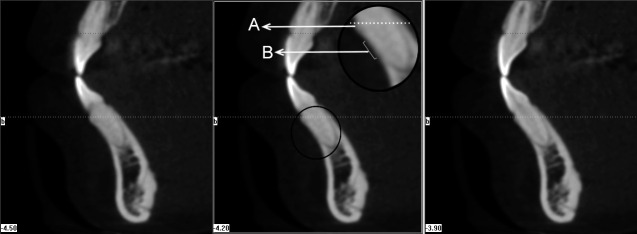
A total of 78 CT scans were obtained with the iCAT scanner (Imaging Sciences International) with a single 360° rotation. With iCAT software primary and secondary reconstructions of the data were performed. For the creation of 3D image projection with maximum intensity for making linear and angular measurements, secondary reconstructions were used. Each tooth root was evaluated in axial and cross-sectional slices at the buccal and lingual surfaces. An alveolar defect was identified when there was no cortical bone around the root in at least three sequential views. If the alveolar bone height was more than 2 mm from the cemento-enamel junction (Figure 1), it was classified as dehiscence. When the defect did not involve the alveolar crest (Figure 2), the case was classified as fenestration.18
Figure 1.
Dehiscence: at least three sequential views (A indicates cemento-enamel junction; B, bone level).
Figure 2.
Fenestration: at least three sequential views (A indicates bone; B, fenestration area/cement of the root).
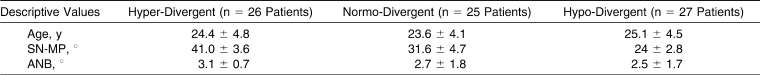
Subjects were divided into three groups with different vertical growth patterns in terms of SN-MP angle as a reference point to distinguish the vertical skeletal pattern. The SN-MP angle from 26.5° to 36.5° (normal range for the controls) denotes the normo-divergent group.19 The hypo-divergent and hyper-divergent groups include the subjects with SN-MP angles that are equal to or less than 26° and equal to or greater than 37°, respectively (Table 2).
Table 2.
Mean Values (±Standard Deviations) for Age, Sella-Nasion–Mandibular Plane (SN-MP) Angle, and ANB Angle in Patients with Different Vertical Growth Patterns
Statistical Analysis
All statistical analyses were performed with SPSS 15.0 (SPSS for Windows; SPSS Inc, Chicago, Ill). The normality test of Shapiro-Wilks and Levene's variance homogeneity test were applied to the data. The data were found to be normally distributed, and there was homogeneity of variance among the groups. Thus, the statistical evaluation was performed using parametric tests. Statistical comparisons of alveolar defects in subjects with different vertical growth patterns were undertaken by the Pearson chi-square test. When the P-value was less than .05, the statistical test was determined to be significant.
Methodological Error
To determine the intraoperator measurement reliability for CBCT measurements, 15 CBCT images were selected randomly and these were measured twice with a 4-week interval by the same observer. A Bland and Altman plot was applied to assess the repeatability. It was determined that the differences between the first and second measurements were not significant.
RESULTS
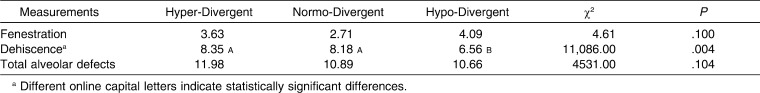
The distribution of alveolar defects for different vertical growth patterns are presented in Table 3. Fenestrations were observed in 3.63%, 2.71%, and 4.09% of subjects and dehiscences were observed in 8.35%, 8.18%, and 6.56% of subjects in the hyper-divergent, normo-divergent, and hypo-divergent subjects, respectively. While fenestrations were not statistically different among groups, dehiscences were more prevalent in hyper-divergent and normo-divergent patients (P = .004).
Table 3.
Distribution of Alveolar Defects for Different Vertical Growth Patterns
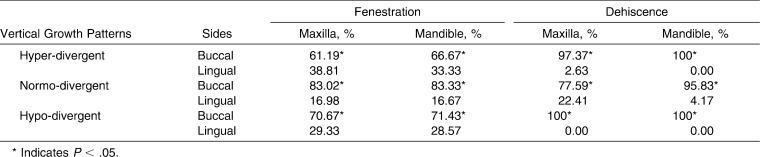
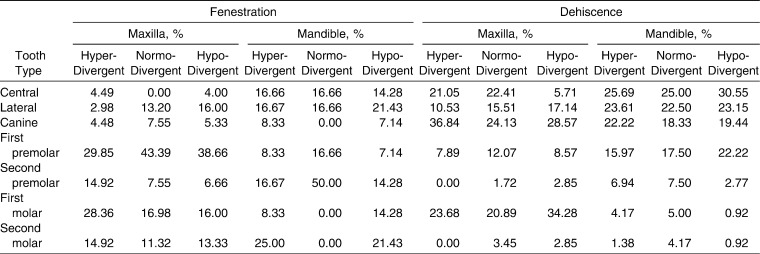
Alveolar defects (fenestration and dehiscence) in the maxilla and mandible were more predominant in buccal alveolar surfaces of all patients with different vertical growth patterns (Table 4). When teeth were evaluated individually, the majority of fenestrations in the maxilla were found on first premolars (hyper-divergent: 29.85%; normo-divergent: 43.39%; and hypo-divergent: 38.66%) and the majority of dehiscences in the mandible were found on central incisors (hyper-divergent: 25.69%; normo-divergent: 25%; and hypo-divergent: 30.55%) for all groups (Table 5).
Table 4.
Percentage of Fenestration and Dehiscence for Different Vertical Growth Patterns
Table 5.
Percentage of Alveolar Defects in Patients with Different Vertical Growth Patterns According to Tooth Type
DISCUSSION
CBCT has the potential to identify alveolar and periodontal defects without the distortion that is present in a panoramic radiograph,12 and CBCT enables clinicians to examine the shape and size of alveolar bones without the disadvantages associated with conventional radiographs.20 As compared with helical CT, CBCT requires less time for the images to be captured, which is useful for patients who are not comfortable or who are unable to keep still. In addition, the images generated via CBCT are less distorted and give practitioners a better understanding of the density of the bone being imaged.21 As a result of the high definition and sensitivity, dehiscence and fenestration could be determined with helical CT and CBCT.22 A spiral or helical CT uses more radiation and has higher costs than CBCT, and use of spiral and helical CT is limited for routine dental radiography.23
In this study, CBCT scans were used to judge alveolar bone measurements and bone defects by means of axial and cross-sectional sections. Leung et al.24 evaluated the accuracy and reliability of CBCT for measuring alveolar bone height and alveolar defects. They correlated direct measurements with CBCT. For bone margin measurements, the correlation coefficient between direct measurements and CBCT was 0.870. On the other hand, detection of fenestration and dehiscence is more prone to error. For dehiscence, both sensitivity and specificity were about 0.80. The diagnosis of alveolar defects using CT depends on length, the thickness of the alveolar cortical plate, and visualization of the periodontal ligament space.5 As these measurements are too small, scoring of these thicknesses as a defect could be the limitation of our study.
Menezes et al.25 found excellent interexaminer and intraexaminer reproducibility of buccal and lingual bone plate thickness measurements in CBCT images and demonstrated good precision for voxel dimensions of 0.2, 0.3, and 0.4 mm. In the current study, an 0.3-mm voxel size was used.
Hypo-divergent and hyper-divergent patterns represent two extremes of facial divergence. While hypo-divergent subjects present with thicker alveolar ridges,26 hyper-divergent subjects have thinner alveolar ridges, especially in the mandibular anterior region.1
Fenestrations are most commonly seen in the maxilla, particularly in the first molar and canine region. Dehiscences are found predominantly in the lower anterior region especially on buccal surfaces. It has been suggested27 that the presence of a narrow zone of attached gingiva, a high frenal attachment, and labially positioned teeth are often associated with these defects. Although Evangelista et al.5 reported that growth patterns do not affect the prevalence of alveolar defects, in the current study statistically significant dehiscences (P = .004) were found in hyper-divergent subjects. A possible reason for this situation is the thinner bone plates, especially in the mandibular anterior region.1,28 Dehiscences could be determined easily and are more accurate than determination of fenestration with CBCT. It is well known that the densities of cementum and bone are similar because of their comparable hydroxyapatite content.29 On the other hand, enamel has greater hydroxyapatite content. Drawing the attention of the investigator to this density difference may lead to overdetermination of dehiscence. Additionally, the bone margin has a certain thickness that can cause difficulty in selecting the point accurately for the measurement.24
The distance from the root apex to the external surface of buccal and lingual cortical bone is greater in hypo-divergent patients compared to hyper-divergent patients.30 Although hyper-divergent patients have thinner bone thickness, the same fenestration prevalence was observed in both groups. The thickness of bone plates at the level of the root apex could not be enough to create fenestration.
The thickness of bone plates at the cervical level and the middle third of the root is very similar in patients with different vertical growth patterns.31 Contrary to the findings of Ferreira et al.,31 greater dehiscence prevalence was observed in the present study at the cervical level in hyper-divergent samples. In hyper-divergent patients, the direction of condylar growth is mainly in the posterior direction and teeth are positioned inclined. On the other hand, hypo-divergent subjects generally show deep bite, and incisor angulation is steeper than in hyper-divergent subjects. Incisor inclination may affect the generation of alveolar defects.32 Future studies are needed in order to examine incisor inclination with regard to dehiscence and fenestration.
Nair et al.33 found no significant differences between the volumes of the maxilla and the mandible in hyper- and hypo-divergent skeletal patterns with CBCT. Either fenestration or dehiscence in the maxilla and mandible was more predominant in buccal root surfaces for all groups. Facial type may have an influence on the thickness of buccal and lingual bone plates. This condition can be attributed to thinner buccal plates when compared to lingual or palatal plates.
In accordance with the literature, the majority of fenestrations were found in the maxilla (around first premolars) and the majority of dehiscences were found in the mandible (around central incisors) in all groups.34 The possible reason for fenestrations at the first premolars could be the anatomical characteristics of the maxilla.35 The maxillary first premolars are located in an area that becomes narrower upwards.17 The incidence of dehiscence is positively correlated with thin alveolar bone.36 In the mandible, the bone becomes thinner from the posterior to the anterior region.37 Unless a proper orthodontic treatment plan is established, alveolar defects have the potential to create gingival recession or tooth mobility. Orthodontic mechanics per se may result in dehiscence and/or fenestration, based on the initial morphology of the alveolar bone as well as on the amount of tooth movement. Orthodontists must be aware of these predisposing factors, and movements in the labio-lingual direction should be limited.
In general, fenestrations are commonly observed in the maxilla, whereas dehiscences are more predominant in the mandibular arch. Further studies should be conducted to confirm and expand the results of the present study on anterior teeth and to determine the predictability of the detection of fenestrations of posterior teeth using CBCT scans.
CONCLUSIONS
A prevalence of dehiscences was found in all different vertical growth patterns.
Hypo-divergent subjects had less dehiscence prevalence than did the hyper-divergent and normo-divergent groups.
While fenestration was seen in the maxillary premolar region, dehiscence was seen in the mandibular anterior region.
REFERENCES
- 1.Handelman C. S. The anterior alveolus: its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod. 1996;66:95–109. doi: 10.1043/0003-3219(1996)066<0095:TAAIII>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Årtun J, Krogstad O. Periodontal status of mandibular incisors following excessive proclination: a study in adults with surgically treated mandibular prognathism. Am J Orthod Dentofacial Orthop. 1987;91:225–232. doi: 10.1016/0889-5406(87)90450-1. [DOI] [PubMed] [Google Scholar]
- 3.Lindhe J, Karring T, Araujo M. The anatomy of periodontal tissues. In: Lindhe J, Karring T, Lang N. P, editors. Clinical Periodontology and Implant Dentistry 4th ed. Copenhagen, Denmark: Blackwell Munksgaard; 2003. pp. 3–48. [Google Scholar]
- 4.Reitan F, Rygh P. Biomechanical principles and reactions. In: Graber T. M, Vandarsdall R. L, editors. Orthodontics Current Principles and Techniques 2nd ed. St Louis, Mo: Mosby-Year Book; 1994. pp. 96–192. [Google Scholar]
- 5.Evangelista K, Vasconcelos K. F, Bumann A, Hirsch E, Nitka M, Silva M. A. G. Dehiscence and fenestration in patients with Class I and Class II Division 1 malocclusion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;138:133e1–133e7. doi: 10.1016/j.ajodo.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 6.Fields H. W, Proffit W. R, Nixon W. L, Phillips C, Stanek E. Facial pattern differences in long-faced children and adults. Am J Orthod. 1984;85:217–223. doi: 10.1016/0002-9416(84)90061-7. [DOI] [PubMed] [Google Scholar]
- 7.Cangialosi T. J. Additional criteria for sample division suggested. Am J Orthod Dentofacial Orthop. 1989;96:24A. doi: 10.1016/0889-5406(89)90248-5. [DOI] [PubMed] [Google Scholar]
- 8.Opdebeeck H, Bell W. H. The short face syndrome. Am J Orthod. 1978;73:499–511. doi: 10.1016/0002-9416(78)90240-3. [DOI] [PubMed] [Google Scholar]
- 9.Ingervall B, Helkimo E. Masticatory muscle force and facial morphology in man. Arch Oral Biol. 1978;23:203–206. doi: 10.1016/0003-9969(78)90217-0. [DOI] [PubMed] [Google Scholar]
- 10.Proffit W. R, Fields H. W, Nixon W. L. Occlusal forces in normal- and long-face adults. J Dent Res. 1983;62:566–570. doi: 10.1177/00220345830620051201. [DOI] [PubMed] [Google Scholar]
- 11.Lang N. P, Hill R. W. Radiographs in periodontics. J Clin Periodontol. 1977;4:16–28. doi: 10.1111/j.1600-051x.1977.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 12.Mengel R, Candir M, Shiratori K, Flores-de-Jacoby L. Digital volume tomography in the diagnosis of periodontal defects: an in vitro study on native pig and human mandibles. J Periodontol. 2005;76:665–673. doi: 10.1902/jop.2005.76.5.665. [DOI] [PubMed] [Google Scholar]
- 13.Quereshy F. A, Savell T. A, Palomo J. M. Applications of cone beam computed tomography in the practice of oral and maxillofacial surgery. J Oral Maxillofac Surg. 2008;66:791–796. doi: 10.1016/j.joms.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 14.Bartling S. H, Majdani O, Gupta R, et al. Large scan field, high spatial resolution flat-panel detector based volumetric CT of the whole human skull base and for maxillofacial imaging. Dentomaxillofac Radiol. 2007;36:317–327. doi: 10.1259/dmfr/19164138. [DOI] [PubMed] [Google Scholar]
- 15.Hassan B, Souza P. C, Jacobs R, Berti S. A, van der Stelt P. Influence of scanning and reconstruction parameters on quality of three-dimensional surface models of the dental arches from cone beam computed tomography. Clin Oral Invest. 2010;14:303–310. doi: 10.1007/s00784-009-0291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leung C. C, Palomo L, Griffith R, Hans M. G. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofacial Orthop. 2010;137:S109–S119. doi: 10.1016/j.ajodo.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 17.Garib D. G, Yatabe M. S, Ozawa T. O, Filho O. G. S. Alveolar bone morphology under the perspective of the computed tomography: defining the biological limits of tooth movement. Dent Press J Orthod. 2010;15:192–205. [Google Scholar]
- 18.Glover M. E. Periodontal plastic and reconstructive surgery. In: Rose L, Mealey B, Genco R, Cohen W, editors. Periodontics Medicine Surgery and Implants 1st ed. St Louis, Mo: Mosby; 2004. pp. 406–487. [Google Scholar]
- 19.Wada K. A study on the individual growth of maxillofacial skeleton by means of lateral cephalometric roentgenograms. J Osaka Univ Dent Soc. 1977;22:239–269. [Google Scholar]
- 20.Yamada C, Kitai N, Kakimoto N, et al. Spatial relationships between the mandibular central incisor and associated alveolar bone in adults with mandibular prognathism. Angle Orthod. 2007;77:766–772. doi: 10.2319/072906-309. [DOI] [PubMed] [Google Scholar]
- 21.Guttenberg S. A. Oral and maxillofacial pathology in three dimensions. Dent Clin N Am. 2008;52:843–873. doi: 10.1016/j.cden.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 22.Mol A, Balasundaram A. In vitro cone beam computed tomography imaging of periodontal bone. Dentomaxillofac Radiol. 2008;37:319–324. doi: 10.1259/dmfr/26475758. [DOI] [PubMed] [Google Scholar]
- 23.Mah J. K, Danforth R. A, Bumann A, Hatcher D. Radiation absorbed in maxillofacial imaging with a new dental computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:508–513. doi: 10.1016/s1079-2104(03)00350-0. [DOI] [PubMed] [Google Scholar]
- 24.Leung C. C, Palomo L, Griffith R, Hans M. G. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofacial Orthop. 2010;137:S109–S119. doi: 10.1016/j.ajodo.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 25.Menezes C. C. D, Janson G, Massaro C. D. S, Cambiaghi L, Garib D. G. Reproducibility of bone plate thickness measurements with cone-beam computed tomography using different image acquisition protocols. Dent Press J Orthod. 2010;15:143–149. [Google Scholar]
- 26.Gracco A, Lombardo L, Mancuso G, Gravina V, Siciliani G. Upper incisor position and bony support in untreated patients as seen on CBCT. Angle Orthod. 2009;79:692–702. doi: 10.2319/081908-437.1. [DOI] [PubMed] [Google Scholar]
- 27.Watson W. G. Expansion and fenestration or dehiscence. Editorial. Am J Orthod. 1980;3:330–332. doi: 10.1016/0002-9416(80)90086-x. [DOI] [PubMed] [Google Scholar]
- 28.Beckmann S. H, Kuitert R. B, Prahl-Andersen B, Segner D, The R. P. S, Tuinzing D. B. Alveolar and skeletal dimensions associated with lower face height. Am J Orthod Dentofacial Orthop. 1998;113:498–506. doi: 10.1016/s0889-5406(98)70260-4. [DOI] [PubMed] [Google Scholar]
- 29.Carranza F. A, Bernard G. W. The tooth-supporting structures. In: Newman M. G, Takei H. H, Carranza F. A, editors. Carranza's Clinical Periodontology 9th ed. Philadelphia, Pa: WB Saunders; 2002. pp. 36–57. [Google Scholar]
- 30.Tsunori M, Mashita M, Kasai K. Relationship between facial types and tooth and bone characteristics of the mandible obtained by CT scanning. Angle Orthod. 1998;68:557–562. doi: 10.1043/0003-3219(1998)068<0557:RBFTAT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Ferreira M. C, Garib D. G, Cotrim-Ferreira F. Padronização de um método para mensuração dastábuas ósseas vestibular e lingual dos maxilaresna tomografia computadorizada de feixe cônico (cone beam) Dent Press J Orthod. 2010;15:49e1–49e7. [Google Scholar]
- 32.Yu Q, Pan X. G, Ji G. P, Shen G. The association between lower incisal inclination and morphology of the supporting alveolar bone—a cone-beam CT study. Int J Oral Sci. 2009;4:217–223. doi: 10.4248/IJOS09047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nair R, Deguchi T. S, Li X, Katashiba S, Chan Y. H. Quantitative analysis of the maxilla and the mandible in hyper- and hypo-divergent skeletal class II pattern. Orthod Craniofac Res. 2009;12:9–13. doi: 10.1111/j.1601-6343.2008.01431.x. [DOI] [PubMed] [Google Scholar]
- 34.Rupprecht R. D, Horning G. M, Nicoll B. K, Cohen M. E. Prevalence of dehiscences and fenestrations in modern American skulls. J Periodontol. 2001;72:722–729. doi: 10.1902/jop.2001.72.6.722. [DOI] [PubMed] [Google Scholar]
- 35.Garib D. G, Henriques J. F, Janson G, Freitas M. R, Fernandes A. Y. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: a computed tomography evaluation. Am J Orthod Dentofacial Orthop. 2006;129:749–758. doi: 10.1016/j.ajodo.2006.02.021. [DOI] [PubMed] [Google Scholar]
- 36.Siriwat P. P, Jarabak J. R. Malocclusion and facial morphology: is there a relationship? An epidemiologic study. Angle Orthod. 1985;55:127–138. doi: 10.1043/0003-3219(1985)055<0127:MAFMIT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 37.Swasty D, Lee J. S, Huang J. C, Maki K, Gansky S. A, Hatcher D, Miller A. J. Anthropometric analysis of the human mandibular cortical bone as assessed by cone-beam computed tomography. J Oral Maxillofac Surg. 2009;67:491–500. doi: 10.1016/j.joms.2008.06.089. [DOI] [PubMed] [Google Scholar]