Abstract
Objective:
To conduct a prospective and randomized study of the efficiency of orthodontic treatment with self-ligating edgewise brackets (SL; Time2 brand, American Orthodontics) and conventional edgewise twin brackets (CE; Gemini brand, 3M).
Materials and Methods:
One hundred consecutive patients were randomized to treatment with either SL or CE brackets. The participants were treated by one of three specialists in orthodontics and with continuous instructions alternately by five orthodontic assistants according to our normal treatment routine (ie, modified 0.022″ MBT preadjusted edgewise technique). The treatments were evaluated in terms of overall treatment time, number of visits, and treatment outcome using the Index of Complexity, Outcome and Need (ICON). The number of emergency appointments, number of archwires, overjet, relative space, and extractions at treatment start were noted.
Results:
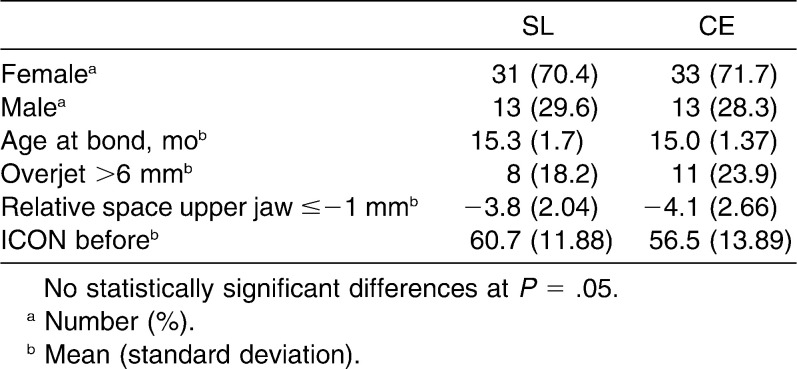
After dropouts, the analyzed material consisted of 44 patients treated with SL (mean age 15.3 years, mean ICON 60.7, 70.4% female) and 46 patients treated with CE (mean age 15.0 years, mean ICON 56.5, 71.7% female). There were no statistically significant differences between the SL and CE groups in terms of mean treatment time in months (20.4 vs 18.2), mean number of visits (15.5 vs 14.1), mean ICON scores after treatment (13.2 vs 11.9), or mean ICON improvement grade (7.9 vs 9.1).
Conclusion:
Orthodontic treatment with SL brackets does not reduce treatment time or number of appointments and does not affect posttreatment ICON scores or ICON improvement grade compared with CE brackets.
Keywords: Orthodontic, Treatment efficiency, Conventional, Self-ligating
INTRODUCTION
The concept of self-ligating brackets was presented in 1935.1 Over the past years, the use of self-ligating brackets has increased. In 2002, 8.7% of American orthodontists used at least one self-ligating system; in 2008, the number had increased to 42%.2
When compared with conventional brackets, several advantages of self-ligating brackets have been claimed, including faster ligation, reduced friction, and faster treatment time with reduced number of visits and less pain.3–6 In laboratory setups, self-ligating brackets have demonstrated reduced friction compared with conventional brackets tied with modules.7,8 In other studies, however, reduced frictional resistance with self-ligating brackets compared with conventional brackets was found only in combination with certain wires.9–11 In a recent review concerning frictional resistance, it was concluded that there is evidence that self-ligating brackets produce lower friction only when coupled with small round wires in an aligned arch with absence of tipping and malalignment. Sufficient evidence is lacking to claim that self-ligating brackets produce lower friction with larger wires or tipped and misaligned teeth.12
Prospective studies have shown equal efficiency of initial alignment when comparing self-ligating brackets to conventional ones.13–16 Retrospective research has shown a reduction in overall treatment time of 4 to 7 months and fewer appointments needed to reach a similar treatment outcome with self-ligating brackets as compared with conventional brackets.17,18
There is still controversy and limited knowledge regarding the evidence for reduced overall treatment time with self-ligating brackets, and the need for prospective randomized studies is obvious.3–5 Recent prospective randomized studies have shown that self-ligating brackets do not reduce overall treatment time, neither in terms of number of visits nor treatment outcome.19,20 The need for further evaluation of the overall efficiency of self-ligating brackets in daily orthodontic clinical work is thus important.
The purpose of this prospective randomized study was to compare the efficiency of orthodontic treatment with self-ligating edgewise brackets (here abbreviated as SL) and conventional edgewise preadjusted brackets (here abbreviated as CE) in terms of overall treatment time, number of visits, and treatment outcome by using the Index of Complexity, Outcome and Need (ICON).21
MATERIALS AND METHODS
This prospective randomized clinical trial was performed at the Specialist Clinic of Orthodontics in Östersund, Sweden. Subjects were recruited consecutively after recall from our waiting list of patients in preparation for treatment with fixed appliance from January 2007 to August 2007.
A total of 100 patients were planned to participate in the study. Based on a retrospective power analysis, 100 patients with a 10% noncompletion rate would demonstrate a difference in treatment time of 3.76 months with a power of 80% and a significance level of .05. A list for randomization according to rectangularly distributed random numbers generated in SAS (Statistical Analysis System) was set up with two groups each consisting of 50 patients. Fifty subjects were randomized to treatment with SL brackets (Time2 brand, American Orthodontics, Sheboygan, Wis) and 50 to treatment with CE brackets (Gemini brand, 3M Unitek, Monrovia, Calif). All patients were treated in accordance with the Swedish system of free child and youth dental care. The age at treatment start ranged from 11.7 to 18.2 years.
Inclusion criteria were planned treatment with fixed orthodontic appliance in at least one jaw. Patients who previously had received interceptive treatment or extractions were included. Exclusion criteria were impacted teeth, multiple agenesis, or need for orthognathic surgery. If a patient declined treatment before treatment start, the patient was replaced by the next consecutive patient from the waiting list who met the inclusion criteria.
The participants were diagnosed and treatment was planned by three specialists in orthodontics, and the treatments were performed by the same specialists and with continuous instructions alternately by five orthodontic assistants. All participants were treated with our normal treatment routine (ie, modified 0.022″ MBT technique),22 with a general arch wire sequence of 0.014-in. nickel-titanium, 0.020 × 0.020-in. heat-activated nickel-titanium, and 0.019 × 0.025-in. stainless steel, with individual variations and appointment intervals of 6 to 10 weeks. Eight patients in each group were treated only in the upper jaw according to the individual treatment plan. The operators were experienced with the two bracket systems, and they were not blinded to bracket type during treatment.
Study casts to assess ICON scores, overjet, and relative space were taken before and after treatment. ICON scores were assessed blindly and randomly by one author as the study casts were coded and mixed with other pretreatment and posttreatment study casts. To assess the intraexaminer reliability for ICON, 20 study casts (10 before and 10 after treatment) were selected by random-number table and remeasured more than 1 month after the first measurement. Continuous calibration of ICON is made at the weekly therapy conferences at the Specialist Clinic of Orthodontics in Östersund. Treatment duration was measured in months from initial bonding to removal of the fixed appliance. The number of planned and emergency appointments, the number of archwires, extractions at treatment start, and the allocation of the three specialists in each group were also noted.
Statistical Analysis
SPSS software version 19 (Chicago, Ill) was used for descriptive and analytical statistical analysis. The differences in baseline characteristics were tested. Analysis of covariance was used to compare the treatment effects of the bracket systems while accounting for baseline differences and confounding variables. These included overjet >6 mm, ICON scores, total number of visits, extractions, and treatment time. The level of significance was set at P < .05. The Mann Whitney U-test was used for group differences regarding number of emergency visits and number of archwires. To test differences between the groups regarding extracted teeth, the chi-squared test was used. Testing mean differences of treatment time, number of visits, ICON after, and ICON improvement grade was made by t-test. To validate the intraexaminer reliability of the ICON assessments, the Spearman Rho coefficient was used.
RESULTS
One hundred patients were recruited for the study, with 50 allocated for treatment with SL brackets and 50 for CE brackets. For different reasons, the analyzed sample consisted of 44 patients treated with SL and 46 patients treated with CE (Figure 1).
Figure 1.
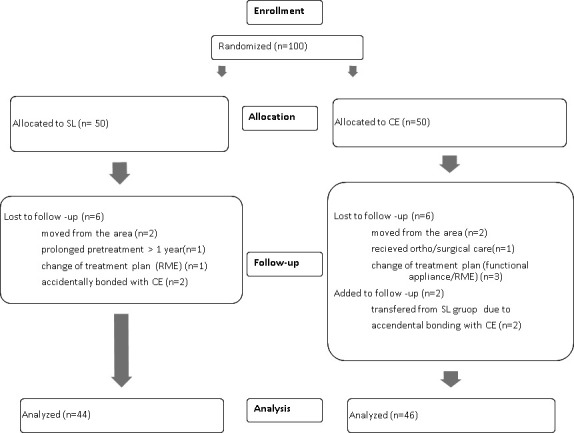
Flow diagram for subjects through the study.
In the baseline data, there were no statistically significant differences between the groups in the analyzed sample (Table 1).
Table 1.
Baseline Data
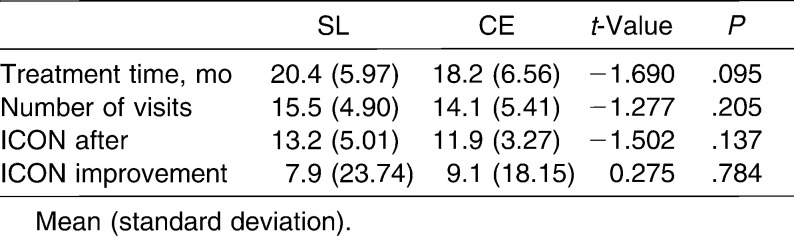
There were no statistically significant differences between the SL group and CE group in terms of mean (±SD) treatment time in months, 20.4 ± 5.97 vs 18.2 ± 6.56, P = .095; mean (±SD) number of visits, 15.5 ± 4.90 vs 14.1 ± 5.41, P = .205; mean (±SD) ICON scores after treatment, 13.2 ± 5.01 vs 11.9 ± 3.27, P = .137; or mean (±SD) ICON improvement grade, 7.9 ± 23.74 vs 9.1 ± 18.15, P = .784 (Table 2).
Table 2.
Results
When the influence of treatment time was adjusted for, there was no statistically significant difference between the SL group and the CE group regarding ICON posttreatment scores and ICON improvement grade.
The median number of archwires used was four in the upper jaw in both groups (P = .230). In the lower jaw, the number was four for SL and three for CE (P = .070), which means that there was no statistically significant difference in number of archwires between the groups.
In both groups, the median number of emergency visits was 1; there was no statistically significant difference between the groups (P = .709).
There was a positive correlation of higher ICON pretreatment scores and prolonged treatment time in the CE group (P = .034) but not in the SL group (P = .209).
An overjet >6 mm prolonged the treatment time statistically significantly in the CE bracket group (mean +5.0 months, P = .012), unlike the SL bracket group (mean +1.1 months, P = .625). The mean treatment time in months in patients with overjet ≤6 mm was 20.2 (SL) vs 17.0 (CE), and in patients with overjet >6 mm, the figures were 21.4 (SL) vs 22.0 (CE).
When testing for group differences regarding treatment time adjusted for ICON before and overjet >6 mm, there was no statistically significant difference regarding treatment time between the groups (P = .181).
There was no statistically significant difference between the SL and CE groups regarding number of extracted teeth at treatment start (1.52 vs 1.93, P = .184), but there was a statistically significant difference between the SL and CE groups regarding the percentage of individuals having extracted teeth at treatment start (38.5% vs 61.5%, P = .021).
When adjusting for extractions, the treatment time was shorter with CE brackets compared with SL brackets (P = .016).
SL and CE patients were evenly distributed between the three specialists; at the most, the distribution was 45% vs 55% (n = 17 vs 21).
The Spearman Rho coefficient for validation of the assessment of ICON scores was .55 for the pretreatment study casts and .87 for the posttreatment study casts.
DISCUSSION
In this prospective randomized trial, there were no statistically significant differences in treatment time, number of visits, ICON posttreatment scores, or improvement grade between self-ligating edgewise brackets (SL; Time2) and conventional edgewise brackets (CE; Gemini).
The treatment protocol was an individualized, modified 0.022 MBT technique,22 and the patients were treated alternatively by specialists in orthodontics and orthodontic assistants. Deviations from the treatment protocol were accepted if judged necessary by an orthodontist to meet individual needs.
At bonding, two patients allocated for the SL group were incorrectly bonded with CE brackets. After dropouts, the two groups were still comparative despite this bonding error.
Patients who had received interceptive treatment were included. There were no statistically significant differences in baseline data between the groups regarding the number of patients with overjet more than 6 mm, mean relative space in patients with crowding >1 mm in the upper jaw, or ICON pretreatment scores, indicating that interceptive measures had similar effects in both groups.
The mean treatment time in months was 20.4 for the SL group and 18.2 for the CE group, which is comparable to previous studies.19,20
In the SL group, the treatment time was not statistically significantly influenced by increased overjet (>6 mm) or higher ICON pretreatment scores. This finding was in contrast to the GE group, which had a positive correlation of higher ICON pretreatment scores and increased overjet with prolonged treatment time. When separating patients with overjet >6 mm and patients with overjet ≤6 mm, we found that the treatment time was similar in the SL and CE groups for the patients with overjet >6 mm. On the other hand, it was shorter for CE patients with overjet ≤6 mm, indicating that treatment of patients without excessive overjet was faster in the CE than the SL group.
According to the individual treatment plan, the number of extracted teeth at treatment start was higher in the CE group than in the SL group, although not statistically significant, and the percentage of patients having extractions was statistically significantly higher in the CE group. In the literature, extraction therapy is considered to lengthen orthodontic treatment.23–25 In this study, there was still no statistically significant difference in treatment time between SL and CE brackets, but when adjusting for extractions, the treatment time was shorter in the CE group. Treatment time in months for SL and CE, respectively, was for patients with extracted teeth 22.0 ± 6.32 vs 19.9 ± 5.91 and for patients treated without extractions 19.2 ± 5.46 vs 14.4 ± 6.58.
Before conducting this study, we believed that the number of emergency visits might be higher in the SL group because of problems with the clip. However, the number of emergency visits was similar in the two groups. It should be noted that no registration of breakages was made when found during regular visits. A recent study presented a similar nonsignificant difference in breakages when comparing SL brackets (Damon3) and CE brackets (Synthesis).20
Since the ICON index21 is used in the everyday work at the Specialist Clinic of Orthodontics in Östersund, it was used in this study to assess the treatment need, outcome, and improvement grade. In other studies comparing self-ligating and conventional brackets, the Peer Assessment Review Index (PAR index) has been used. ICON is, however, validated to assess treatment need26 and to be used in place of PAR and the American Board of Orthodontics Objective Grading System (ABO-OGS) for assessing treatment outcome.27
The ICON scores were assessed blindly and randomly, and intraexaminer reliability was verified by reassessment of 20 study casts, which ensures accurate assessments.
Acceptable treatment results (ICON post treatment <31)21 were obtained in 89 of 90 patients (98.9%), compared with 71 of 100 patients (71%) in a Swedish study concerning treatment outcome measured by ICON28 and an international study showing a range of acceptable cases measured by ICON of 70%–100%,29 indicating good treatment results in this study.
Two recently published randomized prospective studies of other brackets have reported no significant difference in the efficiency of orthodontic treatment with self-ligating brackets compared with conventional brackets.19,20 On the contrary, they showed, in accordance with our findings, a minor, not statistically significant prolonged treatment time with self-ligating brackets.
The self-ligating bracket used in our study (Time2) is initially passive and with heavier wires active. It has been showed that neither the use of Smart Clip “active on demand” nor the passive Damon 3 significantly affected treatment efficiency.19 It thus seems that the type of self-ligating bracket we used in this study presents relevant findings regarding treatment efficiency comparing SL and CE brackets.
CONCLUSION
Evidence is strengthened that self-ligating brackets do not improve orthodontic efficiency in terms of overall treatment time, number of visits, or treatment outcome.
Acknowledgment
This study has been supported by the County Council of Jämtland, Sweden.
REFERENCES
- 1.Stolzenberg J. The Russell attachment and its improved advantages. Int J Orthodont Dent Child. 1935;21:837–840. [Google Scholar]
- 2.Keim R. G, Gottlieb E. L, Nelson A. H, Vogels D. S., III JCO study of orthodontic diagnosis and treatment procedures. Part 1: results and trends. J Clin Orthod. 2008;42:625–640. [PubMed] [Google Scholar]
- 3.Harradine N. The history and development of self-ligating brackets. Semin Orthod. 2008;14:5–18. [Google Scholar]
- 4.Fleming P. S, Johal A. Self-ligating brackets in orthodontics: a systematic review. Angle Orthod. 2010;80:575–584. doi: 10.2319/081009-454.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miles P. G. Self-ligating brackets in orthodontics: do they deliver what they claim. Aust Dent J. 2009;54:9–11. doi: 10.1111/j.1834-7819.2008.01081.x. [DOI] [PubMed] [Google Scholar]
- 6.Damon D. H. The rationale, evolution and clinical application of the self-ligating bracket. Clin Orthod Res. 1998;1:52–61. doi: 10.1111/ocr.1998.1.1.52. [DOI] [PubMed] [Google Scholar]
- 7.Pizzoni L, Ravnholt G, Melsen B. Frictional forces related to self-ligating brackets. Eur J Orthod. 1998;20:283–291. doi: 10.1093/ejo/20.3.283. [DOI] [PubMed] [Google Scholar]
- 8.Sims A. P, Waters N. E, Birnie D. J, Pethybridge R. J. A comparison of the forces required to produce tooth movement in vitro using two self-ligating brackets and a pre-adjusted bracket employing two types of ligation. Eur J Orthod. 1993;15:377–385. doi: 10.1093/ejo/15.5.377. [DOI] [PubMed] [Google Scholar]
- 9.Read-Ward G. E, Jones S. P, Davies E. H. A comparison of self-ligating and conventional orthodontic bracket systems. Br J Orthod. 1997;24:309–317. doi: 10.1093/ortho/24.4.309. [DOI] [PubMed] [Google Scholar]
- 10.Redlich M, Mayer Y, Harari D, Lewinstein I. In vitro study of frictional forces during sliding mechanics of “reduced-friction” brackets. Am J Orthod Dentofacial Orthop. 2003;124:69–73. doi: 10.1016/s0889-5406(03)00238-5. [DOI] [PubMed] [Google Scholar]
- 11.Reicheneder C. A, Gedrange T, Berrisch S, Proff P, Baumert U, Faltermeier A, Muessig D. Conventionally ligated versus self-ligating metal brackets—a comparative study. Eur J Orthod. 2008;30:654–660. doi: 10.1093/ejo/cjn053. [DOI] [PubMed] [Google Scholar]
- 12.Ehsani S, Mandich M. A, El-Bialy T. H, Flores-Mir C. Frictional resistance in self-ligating orthodontic brackets and conventionally ligated brackets: a systematic review. Angle Orthod. 2009;79:592–601. doi: 10.2319/060208-288.1. [DOI] [PubMed] [Google Scholar]
- 13.Miles P. G, Weyant R. J, Rustveld L. A clinical trial of Damon2 vs conventional twin brackets during initial alignment. Angle Orthod. 2006;76:480–485. doi: 10.1043/0003-3219(2006)076[0480:ACTODV]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Scott P, DiBiase A. T, Sherriff M, Cobourne M. T. Alignment efficiency of Damon3 self-ligating and conventional orthodontic bracket systems: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2008;134:470.e1–470.e8. doi: 10.1016/j.ajodo.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 15.Pandis N, Polychronopoulou A, Eliades T. Active or passive self-ligating brackets? A randomized controlled trial of comparative efficiency in resolving maxillary anterior crowding in adolescents. Am J Orthod Dentofacial Orthop. 2010;137:12.e1–12.e6. doi: 10.1016/j.ajodo.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 16.Fleming P. S, DiBiase A. T, Sarri G, Lee R. T. Efficiency of mandibular arch alignment with 2 preadjusted edgewise appliances. Am J Orthod Dentofacial Orthop. 2009;135:597–602. doi: 10.1016/j.ajodo.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 17.Eberting J. J, Straja S. R, Tuncay O. C. Treatment time, outcome, and patient satisfaction comparisons of Damon and conventional brackets. Clin Orthod Res. 2001;4:228–234. doi: 10.1034/j.1600-0544.2001.40407.x. [DOI] [PubMed] [Google Scholar]
- 18.Harradine N. W. Self-ligating brackets and treatment efficiency. Clin Orthod Res. 2001;4:220–227. doi: 10.1034/j.1600-0544.2001.40406.x. [DOI] [PubMed] [Google Scholar]
- 19.Fleming P, DiBiase A. T, Lee R. T. Randomized clinical trial of orthodontic treatment efficiency with self-ligating and conventional fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2010;137:738–742. doi: 10.1016/j.ajodo.2009.06.023. [DOI] [PubMed] [Google Scholar]
- 20.Di Biase A. T, Nasr I. H, Scott P, Cobourne M. T. Duration of treatment and occlusal outcome using Damon3 self-ligated and conventional orthodontic bracket systems in extraction patients: a prospective randomized clinical trial. Am J Orthod Dentofacial Orthop. 2011;139:e111–e116. doi: 10.1016/j.ajodo.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 21.Daniels C, Richmond S. The development of the Index of Complexity, Outcome and Need (ICON) J Orthod. 2000;27:149–162. doi: 10.1093/ortho/27.2.149. [DOI] [PubMed] [Google Scholar]
- 22.McLaughlin R. P, Bennett J. C, Trevisi H. J. Systemized Orthodontic Treatment Mechanics. Mosby; Edinburgh, UK: 2001. [Google Scholar]
- 23.Turbill E. A, Richmond S, Wright J. L. The time-factor in orthodontics: what influences the duration of treatments in National Health Service practices. Community Dent Oral Epidemiol. 2001;29:62–72. [PubMed] [Google Scholar]
- 24.Vig P. S, Weintraub J. A, Brown C, Kowalski C. J. The duration of orthodontic treatment with and without extractions: a pilot study of five selected practices. Am J Orthod Dentofacial Orthoped. 1990;97:45–51. doi: 10.1016/S0889-5406(05)81708-1. [DOI] [PubMed] [Google Scholar]
- 25.Fink D. F, Smith R. J. The duration of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1992;102:45–54. doi: 10.1016/0889-5406(92)70013-Z. [DOI] [PubMed] [Google Scholar]
- 26.Firestone A. R, Beck F. M, Beglin F. M, Vig K. W. Validity of the Index of Complexity, Outcome, and Need (ICON) in determining orthodontic treatment need. Angle Orthod. 2002;72:15–20. doi: 10.1043/0003-3219(2002)072<0015:VOTIOC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 27.Onyeaso C. O, Begole E. A. Relationship between index of complexity, outcome and need, dental aesthetic index, peer assessment rating index, and American Board of Orthodontics objective grading system. Am J Orthod Dentofacial Orthop. 2007;131:248–252. doi: 10.1016/j.ajodo.2005.04.045. [DOI] [PubMed] [Google Scholar]
- 28.Richmond S, Ikonomou C, Williams B, Ramel S, Rolfe B, Kurol J. Orthodontic treatment standards in a public group practice in Sweden. Swedish Dent J. 2001;25:137–144. [PubMed] [Google Scholar]
- 29.Deans J, Playle R, Durning P, Richmond S. An exploratory study of the cost-effectiveness of orthodontic care in seven European countries. Eur J Orthod. 2009;31:90–94. doi: 10.1093/ejo/cjn040. [DOI] [PMC free article] [PubMed] [Google Scholar]