Abstract
Objectives
This study summarizes the introduction of a novel telescopic pathway, which streamlines 2‐week‐wait suspected head and neck cancer referrals to our unit, describes the logistics of the pathway, and analyzes referral numbers and outcomes. We also discuss wider issues surrounding remote assessment in head and neck cancer.
Methods
Data were collected prospectively between January and May 2021, capturing all 2‐week‐wait referrals to our unit following the introduction of a telescopic pathway which utilized a nurse‐led clinic for nasendoscopic examination of selected patients and consultant‐led remote assessment using store and forward technology. Information on referral numbers, waiting times and outcomes was recorded.
Results
Three hundred and forty (185 high risk, 155 low risk) patients entered the telescopic pathway with the remaining 74 patients seen on the conventional standard of care pathway. Cancer conversion rates were 17%, <1%, and 5.4% for the high‐risk telescopic, low‐risk telescopic and standard of care pathways respectively. No patients discharged from the telescopic pathway were re‐referred within 3 months. Review capacity for endoscopic examination was higher per consultant on the telescopic pathway versus the standard of care (p = .01).
Conclusion
A combination of risk stratification and asynchronous telescopic assessment shows promise for the management of suspected head and neck cancer referrals. Potential benefits include consultant‐led care for all patients and enhanced documentation. Digital communication with patients may also assist with adherence to the new NHS 28‐day diagnostic standard for cancer referrals. Ongoing data collection is required to assess how the pathway functions over a longer period.
Level of Evidence
2c
Keywords: COVID19, head and neck cancer, technology, telemedicine
This article summarizes the introduction of a novel telescopic pathway for assessing suspected head and neck cancer patients.

1. INTRODUCTION
The novel coronavirus 19 disease (COVID19) pandemic has had a profound impact on the way we practice medicine in the United Kingdom, and this has been notable in the referral, assessment and management of suspected Head and Neck Cancer (HNC) patients. A nationwide lockdown implemented in March 2020 formed part of a strategy which aimed to reduce the potential impact of the pandemic on the National Health Service (NHS) and, as part of this, there was a reduction in our capacity to deliver timely and comprehensive elective services, including head and neck cancer care. The British Association of Head and Neck Oncologists (BAHNO) issued a position statement on delivering HNC care during the pandemic. 1 With regards to suspected HNC referrals, their focus was on the identification and prioritization of “high‐risk” patients likely to have a malignancy and minimizing hospital exposure in patients who are frail or those with significant comorbidities. BAHNO also advocated the use of a validated head and neck cancer risk calculator to assist with patient stratification. 2 While many centers saw a reduction in the number of 2‐week‐wait head and neck referrals during the early stages of the pandemic, 3 referral numbers have now increased and are at pre‐pandemic levels in our unit. These unprecedented pressures on the HNC pathway have served as a stimulus for the development of new methods of service delivery, such as the use of telephone triage, 4 , 5 to optimize patient care.
The COVID19 pandemic has also coincided with an evolution in NHS cancer targets, via the introduction of a new Faster Diagnosis Standard, introduced in April 2020, to ensure that all patients who are referred for the investigation of suspected cancer find out, within 28 days, if they do or do not have a cancer diagnosis. 6 Currently, cancer referrals in the United Kingdom are held against the standard outlined in the Cancer Reform Strategy. 7 This means all suspected cancer patients should be seen by a specialist within 14 days of referral, patients should wait no longer than 31 days between diagnosis or decision to treat and commencement of treatment and patients should wait no longer than 62 days between the initial referral and commencement of treatment. The new Faster Diagnosis Standard should lead to a reduction in the time between referral and diagnosis with a subsequent improvement in clinical outcomes for those with cancer and a reduction in anxiety for those patients waiting for an “all clear.”
A combination of pandemic recovery and the need to adhere to the new 28‐day diagnostic standard has provided impetus to optimize and refine suspected HNC referrals to our unit. Evidence already exists to suggest that remote assessment using telemedicine may be a feasible option in ENT. 8 , 9 , 10 , 11 Indeed, a visual examination of the upper aerodigestive tract, usually in the form of flexible nasendoscopy and oral examination with a headlight, is essential for the assessment of suspected HNC patients. Both the acquisition of high‐quality images and the development of technology, which allows secure storage and forwarding of such images facilitates an environment in which senior clinicians can provided a comprehensive clinical assessment entirely remotely. This paper summarizes the introduction of a novel telescopic pathway which streamlines 2‐week‐wait suspected HNC referrals to our unit, describes the logistics and equipment used on the pathway and analyzes referral numbers, waiting times, clinical outcomes, and cancer conversion rate. The novel pathway is compared with our current standard of care. We also discuss wider issues surrounding the use of remote assessment, the advantages and disadvantages of such a pathway and areas in which further research are required.
2. MATERIALS AND METHODS
2.1. Description of new telescopic pathway
All 2‐week‐wait (TWW) referrals allocated to two consultant head and neck surgeons at our center between January 2021 and May 2021 were reviewed by those consultants. Unexplained neck lump referrals were diverted directly for imaging prior to review and remaining referrals were triaged into high‐ and low‐risk based on a validated head and neck cancer risk calculator (http://www.orlhealth.com/risk-calculator-2.html). 2 Triage was carried out based on the written referral. This calculator has been validated on over 10,000 patients and was endorsed by ENT UK for referral triage during the COVID19 pandemic. 4 High‐risk patients were seen face‐to‐face by one of two head and neck consultants (teleconsultants 1 and 2). Low‐risk patients were diverted to a telescopic clinic led by a trained advanced nurse practitioner (ANP) and reviewed as soon as possible. During this consultation, a flexible nasendoscopy and an oral examination was performed and recorded using store and forward technology (see below for equipment details). This information was then reviewed by either teleconsultant 1 or 2 and a summary sheet, which included history, endoscopic images and outcome, was generated within 48 h. This summary was automatically uploaded onto the digital patient records system and forwarded to both the patient (via text message, if mobile number provided) and the general practitioner (GP). A summary of the telescopic pathway is shown in Figure 1.
FIGURE 1.
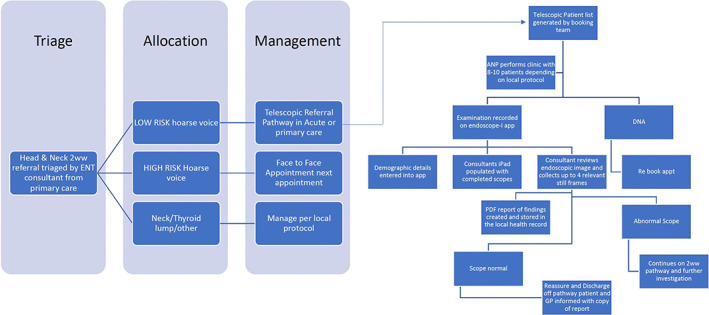
Summary of telescopic pathway
2.2. Conventional pathway (standard of care)
All TWW referrals to a third consultant head and neck surgeon between January 2021 and May 2021 were reviewed by a single senior head and neck surgeon. Unexplained neck lump referrals were diverted directly for imaging prior to review and remaining referrals were booked into the next available face‐to‐face clinic for review, either by that consultant or a supporting registrar. Where possible, these were all seen within 2 weeks as per the conventional cancer pathway.
2.3. Equipment
All images were acquired using a standard fiberoptic flexible nasendoscope (DP Medical) attached to an iPhone SE2 (Apple Inc.) using an endoscope‐smartphone adapter (endoscope‐i Ltd). This iPhone was a managed device which was secured by endoscope‐i and therefore could only be used for image capture and storage using the secure hospital network. Images were viewed, recorded and stored using the e‐i Pro application (endoscope‐i Ltd) in accordance with trust protocol. Videos stored on this device were then accessible by the reviewing consultant using a corresponding iPad (8th generation, Apple Inc.) equipped with a bespoke software that allows the user to view captured images at 60 frames‐per‐second (FPS), choose and store stills from the video and generate a summary document which includes four stills alongside a diagnosis and outcome. The equipment used on the telescopic pathway is demonstrated in Figure 2.
FIGURE 2.

Demonstration of the equipment being used on the low‐risk telescopic pathway
2.4. Data collection
Data were collected prospectively between January 2021 and May 2021, capturing all TWW referrals to our unit. Information on referral numbers, patient demographics, waiting times, radiological investigation, diagnostic surgery and cancer diagnosis rates were recorded, for both the telescopic and standard of care pathway.
2.5. Data analysis
Data were entered into Microsoft Excel and a descriptive analysis was undertaken reporting referral numbers, investigations, theater conversion rate and cancer conversion rate for each part of the telescopic pathway and the standard of care. IBM SPSS Statistics (version 27) was used to conduct tests of normality and one‐way ANOVA to compare the number of patients reviewed on the standard of care pathway and the two teleconsultant groups.
2.6. Institutional approval/clinical governance
The new pathway was set up as a quality improvement project to help manage pressures on the head and neck cancer pathway, and therefore this project was registered with and approved by the clinical governance department at our unit. As this work was evaluating a trust‐approved service, ethical approval was not required.
3. RESULTS
There were 661 TWW referrals to our unit between January 2021 and May 2021. Two hundred and forty seven (37.4%) of these were for unexplained neck lumps and were diverted for imaging prior to review. The remaining 414 (62.6%) patients required examination with flexible nasendoscopy. Of these, 340 (82%) patients entered the telescopic pathway with the remaining 74 (18%) patients kept on the standard of care in which they were offered an appointment within 2 weeks. Overall, there were a mean of 15 face to face endoscopies per month performed by a consultant on the standard of care pathway and a mean of 34 endoscopies per month examined by a consultant on the telescopic pathway (Table 1). Overall cancer conversion rate was 11% with 21% of patients requiring a diagnostic procedure in theater.
TABLE 1.
Review capacity for the telescopic pathway versus standard of care
| Month | Number of endoscopies reviewed | |||
|---|---|---|---|---|
| SOC | Teleconsultant 1 | Teleconsultant 2 | Total | |
| January | 25 | 33 | 38 | 96 |
| February | 12 | 50 | 44 | 106 |
| March | 46 | 46 | 51 | 143 |
| April | 24 | 71 | 70 | 165 |
| May | 22 | 67 | 62 | 151 |
| 661 | ||||
Note: The number of endoscopies seen by each of teleconsultants 1 and 2 include both their high‐risk face‐to‐face reviews and remote telescopic assessments. One‐way ANOVA showed a statistically significant difference in review capacity between groups (p = .01).
3.1. High‐risk telescopic pathway
Of the 340 patients on the telescopic pathway, 185 (54.4%) were deemed to be high‐risk, based on the risk calculator. These patients were seen by a consultant in a face‐to‐face clinic for nasendoscopy within 5 days. Within this cohort, there were 31 positive cancer diagnoses, giving a conversion rate of 17%. Fifty five patients were listed for a diagnostic procedure, giving a theater conversion rate of 30%. Outcomes for the triaged high‐risk patients are summarized in Table 2. No patients were re‐referred into the system, due to progressive symptoms, within 3 months.
TABLE 2.
Outcome summary for telescopic pathway patients in the high‐risk group
| Outcome from clinic review | Number of patients (number with positive cancer diagnosis) |
|---|---|
| Listed for theater | 55 (21) |
| Sent for imaging | 42 (7) |
| Followed up | 18 (0) |
| Discharged | 57 (0) |
| Referred to another clinician | 4 (2) |
| Did not attend appointment | 9 (1) |
| Cancer conversion rate | 17% |
| Theater conversion rate | 30% |
3.2. Low‐risk telescopic pathway
Of the 340 patients on the telescopic pathway, 155 (45.6%) were seen in a nurse‐led nasendoscopy clinic, including 80 (23.5%) new primary care referrals who were in the low‐risk category as per the calculator, 45 (13.2%) patients who required nasendoscopy following imaging, 14 (4.1%) follow‐up scopes for high‐risk patients, 13 (3.8%) patients referred internally by another department and 3 (0.88%) reviews following scans. The 80 new primary care referrals waited for a mean of 15.3 days (range 2–48) for a review. Of these, five required a diagnostic procedure in theater, giving a theater conversion rate of 6%. 21 (26.3%) required imaging. There was one positive cancer diagnosis giving a cancer conversion rate of <1%. None of the patients with a negative cancer diagnosis were re‐referred into the system within 3 months of discharge. Due to progressive symptoms, and all but three of them received an outcome within 28 days. Of the three that did not, one patient did not attend their initial appointment, one patient was missed due to an administrative error and one patient breeched. Outcomes for the low‐risk patients on the telescopic pathway are summarized in Table 3.
TABLE 3.
Outcome summary for telescopic pathway patients in the low‐risk group
| Outcome from clinic review | Number of patients (number with positive cancer diagnosis) |
|---|---|
| Listed for theater | 5 (1) |
| Sent for imaging | 21 (0) |
| Followed up | 0 (0) |
| Discharged | 41 (0) |
| Referred to another clinician | 0 (0) |
| Did not attend appointment | 0 (0) |
| Cancer conversion rate | <1% |
| Theater conversion rate | 6% |
3.3. Standard of care
There were 74 patients on the standard of care pathway who were seen at the next available face‐to‐face appointment once neck lump referrals had been diverted for imaging. Patients were seen in a face‐to‐face clinic within a mean of 14.0 days (range 2–56). Ten patients required a diagnostic procedure in theater, giving a theater conversion rate of 13.5%, and 18 patients (24.3%) required cross‐sectional imaging. There were four positive cancer diagnoses giving a cancer conversion rate of 5.4%. Outcomes for the standard of care pathway are summarized in Table 4.
TABLE 4.
Outcome summary for patients on the standard of care pathway
| Outcome from clinic review | Number of patients (number with positive cancer diagnosis) |
|---|---|
| Listed for theater | 10 (2) |
| Sent for imaging | 18 (2) |
| Cancer conversion rate | 5.4% |
| Theater conversion rate | 13.5% |
4. DISCUSSION
This paper describes the introduction of a novel telescopic pathway for the assessment of TWW suspected head and neck cancer referrals to our unit. As far as the authors are aware, this type of pathway is not currently being used elsewhere within the NHS and therefore the presented data provides information on the feasibility of such a service and the likely impact on the patient journey. It also gives some indication of the potential benefits of such a service while providing an opportunity to explore equipment requirements, the logistics of transferring to a telescopic service and wider issues raised by the introduction of a remote assessment pathway.
The COVID19 pandemic had a profound impact on Head and Neck Cancer service delivery 12 , 13 and has driven a shift toward triaging and risk stratification to help with referral prioritization. Data have already emerged in the wake of the initial COVID19 wave to suggest telephone triage via a validated risk calculator 2 is safe and effective way of identifying patients who are high‐risk for HNC, while minimizing harm to patients who are identified as low risk on the calculator. Indeed, Hardman et al demonstrated that the negative predictive value of a “low risk” outcome from the calculator was 99.1% in data from over 4500 patients triaged during the initial COVID19 surge. 14 Our results were in keeping with this finding, with cancer conversion rates of 17% and <1%, respectively, for the high‐ and low‐risk pathways. The patients at our center identified as high‐risk were essentially managed as they would have been prior to the pandemic; that is they are reviewed in a face to face clinic for clinical examination including fiberoptic nasendoscopy. However, the introduction of a nurse‐led clinic for the low‐risk patients means that this subgroup can still undergo a thorough clinical examination, including fiberoptic nasendoscopy, with a consultant‐led outcome, in a timely fashion. This has the additional benefit of shifting the burden away from an often overbooked consultant TWW clinic, allowing high‐risk patients to be seen in person by a head and neck consultant within 5 days of receipt of referral. It may offer a collateral benefit of increased capacity whereby other patient groups, such as follow‐ups, can also be reviewed. It should be noted that despite this theoretical advantage, our standard HNC pathway performed well in the five‐month study period, with the majority of patients seen within 2 weeks. The diagnostic sensitivity of a HNC pathway, or it is ability to rule out cancer, is paramount and the performance of the telescopic pathway was encouraging with no missed cancers noted, however these results should be interpreted with caution given that patients were only followed up for 3 months post discharge, and therefore missed cancers cannot be completely excluded. Nonetheless, these findings suggest that asynchronous remote assessment of endoscopic images by a HNC consultant is adequate for either detecting cancer or triggering the need for further investigation in low‐risk patients. Despite this, there are obvious advantages to an in‐person outpatient review in the traditional manner, when compared to remote telescopic assessment. For example, the tactile feedback of palpation is not possible and this holds particular relevance in the assessment of oropharyngeal tumors. Likewise, while our acquired images were felt to be adequate, the reviewing consultant does not have the ability to direct the scope and this may prevent them from viewing an anatomical area of specific interest in greater detail. Of note, the quality of image acquisition was not formally measured in this study.
Clearly, the acquisition of high‐quality images underpins the ability of an assessor to make an accurate diagnosis remotely, and a key component of the software described in our pathway is its capability to slow down recorded videos to 60FPS. This facilitates thorough assessment of recorded videos and also allows the reviewing consultant to select the most appropriate still image for storage in the patient records. The bespoke software also compresses video files to a size which is small enough to facilitate storing and forwarding on the specified devices. Furthermore, the use of videos, rather than still images, allows assessment of more dynamic pathology, such as vocal cord paralysis. Additionally, inclusion of these images in the patient record acts as a useful form of documentation not traditionally used in HNC clinics and may optimize communication within the HNC team. For example, these images will be accessible at the multidisciplinary team (MDT) meeting, at future follow‐up appointments and by allied members of the HNC team, for example, speech and language therapists. If the patient requires a diagnostic procedure in theater, these images can serve as an aide memoire for the surgeon on the day of surgery to refamiliarize themselves with the patient's pathology and may also help the anesthetist with planning of airway management. Utilizing these images in the patient records also ensures accountability for the outcome generated post assessment. Furthermore, these images also make up part of the correspondence between the HNC team and the patient's GP, alongside a summary of the presenting complaint and a clinic outcome. The purpose of this document is to provide a succinct and informative summary of the outpatient review for the GP so their records can be updated appropriately and any action required is easily identifiable. Looking forward, widespread implementation of image storage would likely produce a vast library of data on which automated diagnostic technologies and the use of artificial intelligence (AI) could be based. Indeed, a recent literature review by Mahmood et al. 15 summarized this emerging field in HNC and, while the majority of studies into AI focus on either radiological or histological data, one study 16 highlighted the promise of machine‐learning algorithms for the detection of early‐stage laryngeal cancer, based on endoscopically acquired images. The use of other diagnostic adjuncts, such as narrow band imaging (NBI), may also enhance a remote assessment pathway as their use becomes more widespread.
The HNC referral pathway is safeguarded by several standards which are there to ensure that patients with suspected cancer are seen, investigated and treated in a timely fashion. The definitions associated with these standards are important when assessing the performance of a HNC pathway as the 2‐week‐wait endpoint is only reached when a patient is either seen by a consultant (or one of their team) or the patient is seen in a diagnostic clinic as part of a consultant‐led service. 17 The telescopic pathway described would fall under this remit. A patient cannot be removed from this pathway with a telephone consultation or remote triage alone, highlighting the fact that, while telephone appointments and triaging have an important part to play, they alone are not sufficient for managing such patients. The cancer pathway focus has evolved since April 2020 with the introduction of a new 28‐day diagnostic standard within the NHS to ensure that all patients who are referred for the investigation of suspected cancer find out, within 28 days, if they do or do not have a cancer diagnosis. 6 To help achieve this, the telescopic pathway utilizes text messaging as the primary method of outcome communication for the majority of patients undergoing remote assessment. The same outcome summary that is sent to the GP immediately following consultant review of images, is simultaneously sent, in pdf format via text message, to any patients who register a mobile phone number with the department. All consultant reviews took place within 48 h of remote image acquisition and therefore patients can receive an outcome within 48 h of their assessment. Time spent awaiting transcription of dictated letters is minimized, as is the time it takes for posted letters to reach the patient, which should assist in adherence to the 28‐day standard. However, it should be noted that the National Cancer Waiting Times Monitoring Dataset Guidance states that the 28‐day pathway end date should be recorded as the date that the “all clear” letter or digital communication is sent, rather than when the patient actually receives it. 17 With regards to postal communication, this negates any delays with patients receiving their letters, however we would suggest that timely communication with patients should be prioritized. A digital method of communication is also more easily auditable, as opposed to posted letters in which it is difficult to prove definitively whether the patient has received their outcome, however the above guidance also encourages the use of audit to ensure that patients receive and understand their letters. Sending clinic outcomes in pdf format via text message is obviously limited to smartphone users and at this time it is likely that many patients will still prefer traditional communications via post, however it is likely that this will also be expanded to email communication in the near future. The real value of this digital communication is following the assessment of the “worried well”; low‐risk patients who require reassurance that their symptoms are not cancer related. Clearly, in a patient whereby an unexpected cancer is picked up during a remote assessment, it is at the clinician's discretion how to communicate this to the patient. We would usually advocate that this patient is brought to the next available face to face clinic for a formal discussion in an appropriate environment, and this is supported by NHS guidance surrounding the new diagnostic standard. 17 The environmental impact of any new pathway should also be considered, as evidenced by the introduction of a Greener NHS Programme, 18 which aims to reach net zero for all carbon emissions, controlled directly by the NHS, by the year 2040. A transition toward digital communication with both patient and GP and a move away from traditional postage of letters is likely to reduce the carbon footprint at this stage of the patient journey and the use of digital messaging is specifically cited in the NHS report. Likewise, the concept of remote assessment and moving care closer to patient homes is also mentioned in this document, and it is envisaged that a community diagnostic hub would be a suitable setting for the low‐risk patients on our pathway to undergo an assessment, with an entirely remote consultant‐led outcome.
Utilization of consultant time is another issue that has been highlighted by the introduction of a telescopic pathway and this is highlighted by the greater theater conversion rate and cancer conversion rate observed in the high‐risk telescopic group versus the standard of care. Due to referral triaging and the capacity to examine low‐risk patients via a remote assessment, the patients seen by a consultant in the high‐risk clinic have much higher rates of significant pathology. As a result, a higher proportion of consultant time is spent with patients in need of consultant care; for example, explaining diagnoses and consenting for theater, while most patients with benign pathology can be reassured remotely. While no formal data was collected on duration of consultation, we postulate that a telescopic pathway could eventually be more time efficient. Anecdotally, consultant reviews of endoscopic videos and generation of outcome documents were taking around 6 min, which may facilitate a higher number of patients getting a consultant opinion within a given clinical session. Of course, this is currently speculation and further work is required which investigates this under controlled conditions. Remote assessment of patients may also increase the scope for cross‐cover if a consultant is absent, for example, during times of leave or illness. However, this is limited to the assessment of low‐risk patients.
The introduction of a telescopic 2‐week‐wait pathway is likely to have an impact on training opportunities as it fundamentally changes the way clinics have traditionally functioned. All patients on both the high‐ and low‐risk side of the telescopic pathway are getting consultant‐led care, which is beneficial for patients, however there is a potential cost to surgical trainees who will likely see a reduction in the number of TWW clinic patients they see. Conversely, a telescopic pathway may provide a platform for more direct trainee supervision by consultants with enhanced training opportunities and safeguarding of patient care. 19 For example, remote assessment clinics may involve a trainee interpreting the video‐endoscopic findings with the opportunity for direct feedback and discussion from a supervising consultant. This may also provide a good opportunity for the completion of work‐based assessments currently required by UK surgical trainees. There are also training issues surrounding the setup of such a pathway. In the above model, an advanced nurse practitioner (ANP) was trained directly by a consultant to perform the required examination. A period of performing the examination under direct supervision followed, before the ANP was permitted to conduct clinics independently. Currently, there is no formal training pathway for this and these logistics would need to be addressed locally if a unit was looking to instigate a similar service. Likewise, utilizing other allied health care professionals, such as physicians associates, may also be an option.
While early results from the implementation of our telescopic HNC pathway are encouraging, there are a number of areas in which further work is required. Firstly, ongoing data collection is needed as our pathway develops to provide greater numbers for analysis. Additionally, COVID19 recovery, health care demand and the potential for further disruptions from COVID19 variants means the NHS is in a volatile state, and therefore more data are required on how the pathway will cope with increased referral numbers and the potential for staff absences, among other things. There may also be a reluctance for NHS consultants to pick up extra clinics, due to the unresolved issues with potential pensions tax implications, and this may affect how the telescopic pathway is utilized. It is also imperative to seek feedback, in the form of qualitative studies, from key stakeholders, including patients and health care professionals in the wider head and neck community to better inform the development of a telescopic service. Health economic analysis would also provide more information on the long‐term sustainability of this service within the current NHS model.
5. CONCLUSION
A combination of risk stratification and asynchronous telescopic assessment shows promise as a novel pathway for the management of 2‐week‐wait suspected HNC referrals. Potential benefits include consultant‐led care for all patients, optimized utilization of consultant time and focused learning opportunities for trainees. Digital communication with patients may also assist with adherence to the new NHS 28‐day diagnostic standard for cancer referrals and storage of digital images as part of patient records may optimize communication across the multidisciplinary team. Ongoing data collection is required to provide larger numbers for analysis and to assess how the pathway functions over a longer period. Further research is required in the form of qualitative assessments which seek the feedback of key stakeholders, including patients, to better inform the development of a telescopic service.
CONFLICT OF INTERESTS
Mr. Ajith George is the Medical Director of endoscope‐i Ltd, a developer of physical adaptors and smartphone applications for mobile endoscopic imaging.
ACKNOWLEDGMENTS
Thank to you the staff at University Hospitals North Midlands for their assistance with the introduction of the new pathway.
Metcalfe C, Dogan M, Glazzard N, Ross E, George A. Introduction of a novel telescopic pathway to streamline 2‐week‐wait suspected head and neck cancer referrals and improve efficiency: A prospective service evaluation. Laryngoscope Investigative Otolaryngology. 2022;7(1):117‐124. doi: 10.1002/lio2.721
Funding information West Midlands Cancer Alliance, Grant/Award Number: N/A
REFERENCES
- 1. BAHNO . Statement on Covid‐19 . Accessed July 20, 2021. https://bahno.org.uk/bahno_statement_on_covid-19.aspx.
- 2. Head and neck cancer risk calculator (HaNC‐RC)‐V.2 . Adjustments and addition of symptoms and social history factors—PubMed. Accessed July 4, 2021. https://pubmed.ncbi.nlm.nih.gov/31985180/. [DOI] [PMC free article] [PubMed]
- 3. Taylor R, Omakobia E, Sood S, Glore RJ. The impact of coronavirus disease 2019 on head and neck cancer services: a UK tertiary centre study. J Laryngol Otol. 2020;134:1‐4. doi: 10.1017/S0022215120001735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. ENT UK . Remote triaging of urgent suspected head and neck cancer referrals during Covid‐19 pandemic . https://www.entuk.org/sites/default/files/files/ENTUK_2WW_Telephone_Triage_Letter.pdf. [DOI] [PMC free article] [PubMed]
- 5. Banerjee S, Voliotidis D, Parvin L, Rama SPK. Telephone triage of suspected head and neck cancer patients during the coronavirus disease 2019 pandemic using the head and neck cancer risk calculator version 2. J Laryngol Otol. 2021;135(3):241‐245. doi: 10.1017/S0022215121000657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. NHS England Faster diagnosis . Accessed October 18, 2021. https://www.england.nhs.uk/cancer/faster-diagnosis/.
- 7.NHS England. Cancer Reform Strategy (2007). https://www.nhs.uk/NHSEngland/NSF/Documents/Cancer%20Reform%20Strategy.pdf. Accessed on December 24, 2021.
- 8. Dorrian C, Ferguson J, Ah‐See K, et al. Head and neck cancer assessment by flexible endoscopy and telemedicine. J Telemed Telecare. 2009;15(3):118‐121. doi: 10.1258/jtt.2009.003004 [DOI] [PubMed] [Google Scholar]
- 9. Gupta N, Chawla N, Gupta D, Dhawan N, Janaki VR. Community triage of otology patients using a store‐and‐forward telemedicine device: a feasibility study. Ear Nose Throat J. 2017;96(7):246‐249. [PubMed] [Google Scholar]
- 10. Gupta T, Gkiousias V, Bhutta MF. A systematic review of outcomes of remote consultation in ENT. Clin Otolaryngol. 2021;46(4):699‐719. doi: 10.1111/coa.13768 [DOI] [PubMed] [Google Scholar]
- 11. Metcalfe C, Muzaffar J, Orr L, Coulson C. A systematic review of remote otological assessment using video‐otoscopy over the past 10 years: reliability and applications. Eur Arch Otorhinolaryngol. 2021;278:4733‐4741. doi: 10.1007/s00405-020-06596-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Day AT, Sher DJ, Lee RC, et al. Head and neck oncology during the COVID‐19 pandemic: reconsidering traditional treatment paradigms in light of new surgical and other multilevel risks. Oral Oncol. 2020;105:104684. doi: 10.1016/j.oraloncology.2020.104684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Collaborative COVIDS. Head and neck cancer surgery during the COVID‐19 pandemic: an international, multicenter, observational cohort study. Cancer. 2021;127(14):2476‐2488. doi: 10.1002/cncr.33320 [DOI] [PubMed] [Google Scholar]
- 14. Hardman JC, Tikka T, Paleri V, ENT UK , BAHNO , INTEGRATE (the UKENT trainee research network) . Remote triage incorporating symptom‐based risk stratification for suspected head and neck cancer referrals: a prospective population‐based study. Cancer. 2021;127(22):4177‐4189. doi: 10.1002/cncr.33800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mahmood H, Shaban M, Rajpoot N, Khurram SA. Artificial intelligence‐based methods in head and neck cancer diagnosis: an overview. Br J Cancer. 2021;124(12):1934‐1940. doi: 10.1038/s41416-021-01386-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moccia S, De Momi E, Guarnaschelli M, et al. Confident texture‐based laryngeal tissue classification for early stage diagnosis support. J Med Imaging. 2017;4(3):034502. doi: 10.1117/1.JMI.4.3.034502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. NHS England . National Cancer Waiting Times Monitoring Dataset Guidance—Version 11.0. Published online September 2020.
- 18. NHS England . Greener NHS . Delivering a net zero NHS. Accessed October 18, 2021. https://www.england.nhs.uk/greenernhs/a-net-zero-nhs/.
- 19. Liu YF, Kim CH, Bailey TW, et al. A prospective assessment of nasopharyngolaryngoscope recording adaptor use in residency training. Otolaryngol—Head Neck Surg Off J Am Acad Otolaryngol‐Head Neck Surg. 2016;155(4):710‐713. doi: 10.1177/0194599816656169 [DOI] [PubMed] [Google Scholar]


