Abstract
Purpose:
Neighborhood factors such as crime, discrimination, and violence are increasingly recognized as correlates of poor glycemic control. However, pathways for these relationships are unclear. This study examined stress and self-efficacy as potential pathways for the relationship between neighborhood factors and glycemic control in adults with type 2 diabetes.
Design:
Cross-sectional study.
Setting:
Two primary care clinics in southeastern US.
Participants:
615 adults aged 18 years and older.
Measures:
Validated measures were used to capture neighborhood factors, stress, and self-efficacy, while hemoglobin A1c (HbA1c) was abstracted from the electronic health record.
Analysis:
Path analysis was used to investigate direct and indirect relationships between neighborhood factors, stress, self-efficacy, and glycemic control.
Results:
In the final model, violence (r = .17, P = .024), discrimination (r = .46, P < .001), and crime (r = .36, P = .046) were directly associated with higher perceived stress. Stress (r = −.5, P < .001) was directly associated with lower self-efficacy. Self-efficacy was directly associated with better general diet (r = .12, P < .001), better specific diet (r = .04, P < .001), more exercise (r = .08, P < .001), and lower HbA1c (r = −.11, P < .001). Stress (r = .05, P < .001), crime (r = .20, P < .001), and discrimination (r = .08, P < .001) were indirectly associated with higher HbA1c.
Conclusion:
Stress and self-efficacy are potential pathways for the relationship between neighborhood factors like violence, discrimination, and crime and glycemic control. Interventions aimed at mitigating stress and improving self-efficacy may improve self-care behaviors and glycemic control.
Keywords: neighborhood factors, crime, violence, discrimination, diabetes, glycemic control
In Briefs
Understanding diabetes care within the context of social determinants is necessary for secondary and tertiary prevention for adults with diabetes. This study used path analysis to investigate direct and indirect effects between neighborhood factors, stress, self-efficacy, and glycemic control among a sample adult population with type 2 diabetes.
The results of this study found significant direct effects between neighborhood factors (violence, discrimination, and crime) and increased perceived stress. Significant indirect effects were found between perceived stress and higher glycemic control, crime and higher glycemic control, and discrimination and higher glycemic control.
Leveraging the current findings within the context of the existing body of evidence from public health prevention programs offers a new way forward for conceptualizing prevention models for neighborhood factors and diabetes outcomes. Development of outward facing interventions to address multiple levels of influence on diabetes outcomes is an area where future work is needed.
Purpose
Diabetes is the seventh leading cause of death and a major public health concern.1 It affects more than 30.3 million people in the United States, and costs around $327 billion per year.2 Diabetes is also associated with significant morbidity, mortality, and increased disability.1 Glycemic control as measured by hemoglobin A1c (HbA1c) is a crucial clinical outcome for understanding the quality of a patient’s diabetes management over time.3 Self-care behaviors, such as dietary changes, regular checks of blood sugar, exercise, and foot care are essential for optimizing glycemic control and preventing diabetes complications.4,5 Social determinants of health, or the conditions in which people are born, age, work, and play, greatly impact patients’ long-term health and influence how and if patients can complete self-care behaviors.6 Therefore, understanding diabetes care within the context of social determinants is necessary for secondary and tertiary prevention for adults with diabetes.
Social determinants of health factors identified by the Center for Disease Control and Prevention as having an influence on immediate and long-term health include neighborhood factors.7,8 Within the context of diabetes, evidence shows that neighborhood factors such as discrimination, crime, and violence are associated with diabetes incidence as well as diabetes management.9–12 Discrimination, broadly defined as the biased treatment of members of a particular group by both individuals and social institutions, in particular has been strongly correlated with an increased incidence of diabetes and subsequent complications13–16 as well as increased blood pressure and continuous blood glucose levels.17 In addition, evidence shows walking or being physically active can be impeded due to do to high levels of crime and violence,18–20 increasing risk of obesity and diabetes.20 Finally, evidence suggests that across these 3 neighborhood factors of discrimination, crime, and violence, all 3 may also influence diabetes self-care behaviors and HbA1c through exposure to chronic stress.21
Stress is one of the major hypothesized mechanisms for why neighborhood factors affect health outcomes.22 Stress, both acute and chronic, are shown to have negative effects on overall health via physiological and psychosocial pathways22,23 and confers significant risk for developing diabetes.24–26 Acute and chronic stressors of everyday life interplay to affect the health of patients living with diabetes.27 For example, strong correlations have been demonstrated in the literature between perceived discrimination and stress,28 which can lead to poorer self-care behaviors and worse glycemic control as stress is shown to have direct and indirect influence, through these self-care behaviors, on glycemic control.29 Additionally, evidence shows that with increased stress, engagement in treatment recommendations decreases, negatively impacting glycemic levels,27 suggesting the integral role of stress in diabetes management.30
As stress plays a significant role in the development and management of diabetes, understanding the potential pathways between specific neighborhood factors and glycemic control is important. Self-efficacy, confidence in one’s ability to engage or perform specific behaviors, is a construct with theoretical foundations in the interaction across behavioral, personal, and environmental factors and has been directly linked to the performance of self-care behaviors across patients with diabetes.31–34 Specifically, higher self-efficacy has been shown to be related to higher engagement in specific diabetes self-care behaviors.34 However, little is known about the pathway between specific neighborhood factors, stress, self-efficacy, self-care behaviors, and glycemic control for patients with diabetes. Therefore, we developed a conceptual model to explain the potential pathways between neighborhood factors and glycemic control based on existing literature (see Figure 1). We hypothesized that stress and self-efficacy are potential pathways that explain the relationship between neighborhood factors and glycemic control.
Figure 1.
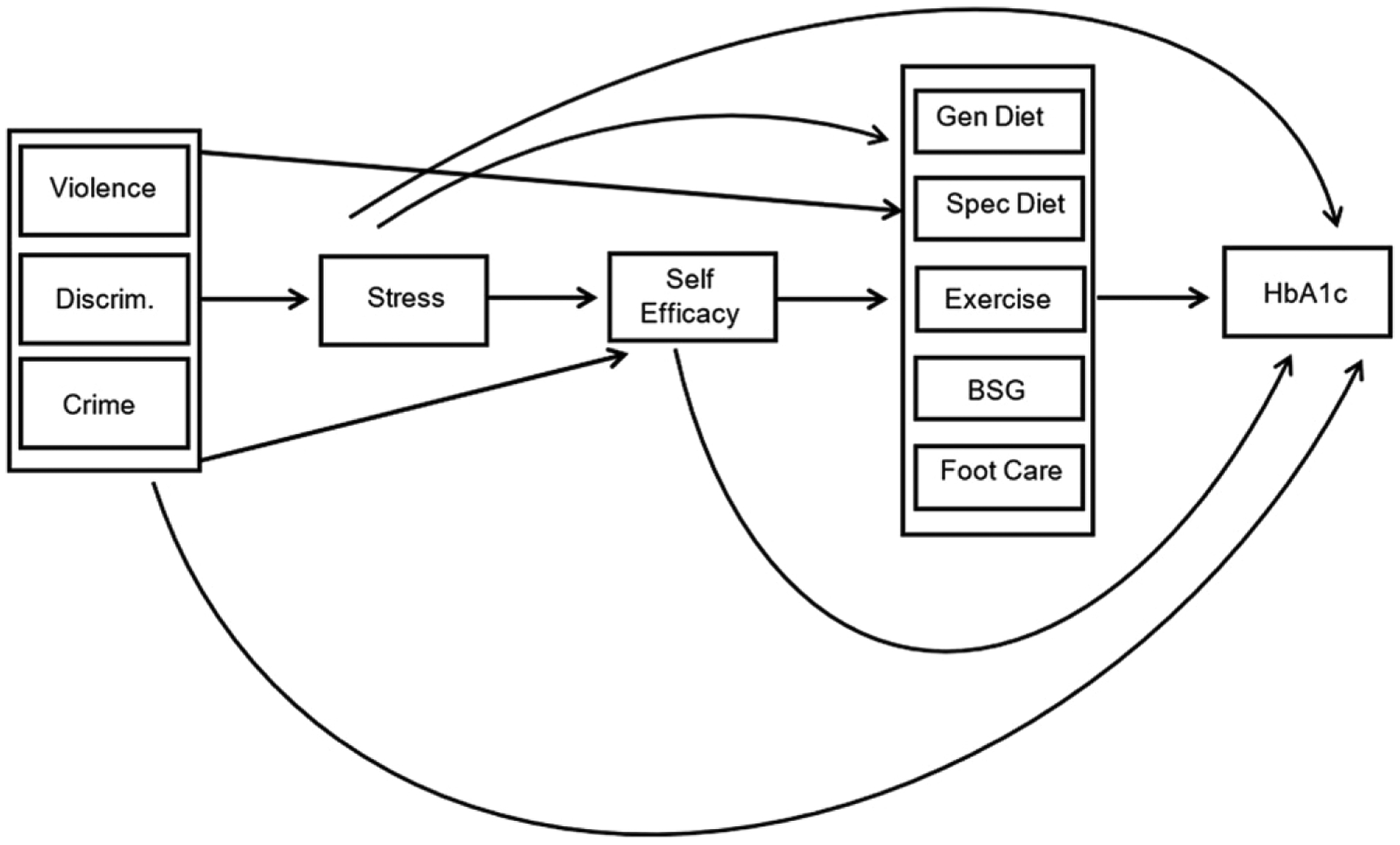
Initial model indicating hypothesized pathways between neighborhood factors and glycemic control.
Methods
Design and Sample
This cross-sectional study included 615 adult participants with type 2 diabetes recruited from 2 primary care clinics in the southeastern United States. Inclusion criteria for this study included being 18 years or older, having a clinical diagnosis of type 2 diabetes within their medical record, and ability to complete a paper-based survey in English. Recruitment strategies included in person and targeted mailings. Approximately 90% of the study sample was recruited in person, while 10% was recruited using targeted mailings. The survey took on average 1 hour to complete. Ninety-five percent of eligible individuals agreed to participate. No patients were excluded from this study. In person recruitment took place within the clinic waiting room where study announcements were made and interested participants were screened for eligibility in a private location provided by the clinic director. Those interested and eligible were scheduled for a visit to complete a one-time paper-based survey with a research assistant. For those willing, the survey was completed at the time of recruitment following informed consent procedures. Mailed recruitment including mailing out letters of invitation to eligible participants detailing the study goals, procedures, and eligibility criteria. Those interested contacted the research team to schedule an appointment for screening, enrollment, and survey completion. All study procedures were approved by the Medical University of South Carolina (PRO17676).
Measures
Outcome - HbA1c.
HbA1c was the primary outcome of interest and was abstracted from each participant’s electronic health record. HbA1c values within 6 months of survey completion were used for the analysis.
Neighborhood Factors
Previously validated measures35,36 of neighborhood factors were used to examine 3 neighborhood factors for this study from the patient’s perspective: (1) Violence; (2) Discrimination; (3) Crime.35,36 Four items were used to measure violence (Cronbach’s alpha [.83]) including questions such as “During the past 6 months, how often was there a fight in this neighborhood in which a weapon was used?” and if gang fights occurred, sexual assaults occurred, or robberies and muggings. Response options ranged from “Often” to “Never.” Four items were used to measure perceived discrimination (Cronbach’s alpha [.74]), including questions such as in the past 12 months, how often have you felt that people treated you poorly or made you feel inferior because of your race or ethnicity?” Response options included “Never” to “Often.” A single item was used to measure neighborhood crime. Participants were asked “how safe from crime do you consider your neighborhood to be?” and responses ranged from not at all safe to extremely safe. All neighborhood variables were treated as continuous.
Stress and Self-Efficacy
Stress and self-efficacy were measured using validated measures including the Perceived Stress Scale (PSS)37 and the Perceived Diabetes Self-Management Scale (PDSMS).38 The 4-item PSS assesses perceived stress and is a well validated measure of stress (Cronbach’s alpha [.69]).39 Scores for the PSS are created by summing responses and range from 0 to 16 with higher scores indicating higher stress. The PDSMS is a widely used and validated measure (Cronbach’s alpha [.83]) of self-efficacy and includes 8-items that measure diabetes specific self-efficacy.38 Example questions include “It is difficult for me to find effective solutions for problems that occur with managing my diabetes.” Participants rate their agreement on a scale from “1 Strongly Agree” to “5 Strongly Disagree.” A summary score is created ranging from 8 to 40 with higher scores indicating more confidence in self-management.38
Self-Care Behaviors
The Summary of Diabetes Self-Care Activities Scale (SDSCA) was used to measure self-care behaviors.40 The SDSCA assesses 6 self-care behaviors across 11 items that includes general and specific diet, exercise, blood glucose monitoring, foot care, and smoking. Example questions include asking participants “How many of the last 7 days have you followed a healthful eating plan?” and “On how many of the last 7 days did you test your blood sugar?” Scores are calculated for each individual item (diet, exercise, blood glucose test, foot care, and smoking). Higher scores indicate higher performance of self-care behaviors. This scale has been validated and demonstrated inter-item correlations (M = .47) and moderate test-retest correlations (M = .40).40
Statistical Analysis
Descriptive statistics were used to describe the data, followed by investigation into normality for each measure included in the path analysis. Demographics for the sample were summarized using percentages for categorical and means and standard deviations for continuous variables. Measures included in the path analyses were each treated as continuous variables based on scoring specific to the validated scales and were summarized in a separate table using means and standard deviation.
We found that the sample met all path analysis assumptions of normally distributed, linearly related and at least interval scale measured variables for the analysis.41,42 Normality was examined using histograms and outlier analysis. Missing data was evaluated to ensure we could assume missing at random. Variables were found to be normally distributed and no variable had more than 2% missing data. Linearity and strength of relationship between variables included in the path analysis was then investigated using Pearson’s correlation with pairwise comparisons for all variables and reported. The sample size of 615 allowed for the best practice of 20:1 (subject to variable) ratio that ensured we could maintain 80% power while providing stability of parameter estimates.42,43
Path analysis was used to investigate direct and indirect effects for the relationship between neighborhood factors, stress, self-efficacy, self-care, and glycemic control. Path analysis allows testing of a hypothesized model incorporating multiple independent and dependent variables.41–43 We used the sem command in Stata version 16 to estimate a path analysis based on the hypothesized model (see Figure 1) following testing procedures as outlined by Kline.41
Second, direct, indirect, and total effects were estimated using the maximum likelihood estimation procedure and standardized coefficients. The mlmv option in Stata was used to retain as many variables as possible by allowing full-information maximum likelihood estimation rather than using listwise deletion. Standardized coefficients were used to allow comparison between paths regarding strength of the relationship and can be interpreted as the change in standard deviation of the outcome resulting from 1 SD increase in the predictor variable.
Third, a number of model fit statistics were investigated to determine the fit of the model, following best practices of structured equation modeling as outlined by Kline and Hooper et al.41,44 As noted by best practice guidelines, indication of good fit by 3 different fit statistics, rather than significance of chi-square for the overall model is recommended.41,44 Cut points were based on published recommendations for structured equation modeling41,44 and included root square mean error of approximation less than .05, comparative fit index (CFI) greater than .9, and non-significant pclose value. Modification of the model was constrained to allowing covariance between self-care variables.
Finally, hypotheses regarding relationships between variables in the model were evaluated using the direction and strength of path coefficients. Standardized coefficients that were statistically significant based on P < .05 we reported in the final model. The magnitude of the coefficient was used to investigate the strength of individual relationships within the model, with direct, indirect, and total effects reported along with P-value. All analyses were performed using Stata version 16.
Results
Figure 1 shows the hypothesized pathways between specific neighborhood factors, stress, self-efficacy, self-care behaviors, and glycemic control for patients with diabetes (Figure 1), with paths shown using arrows and measured variables shown using boxes. Neighborhood factors (violence, discrimination, and crime) were hypothesized as being directly and indirectly related to stress, self-efficacy, self-care, and glycemic control. Stress and self-efficacy were also hypothesized as being directly and indirectly associated with glycemic control. Self-care was hypothesized as being directly related to glycemic control, with each self-care behavior treated as a separate measured variable.
Table 1 provides sample demographics. The mean age was 61.3 years, with majority of participants being non-Hispanic black (64.9%), men (61.6%), and insured (90.7%). Mean duration of diabetes was 12.3 years. Table 2 provides descriptive statistics for all variables included into the path analysis model, and Table 3 provides Pearson’s correlations between all variables. Table 4 presents the standardized direct, indirect, and total effects for the relationship between neighborhood factors psychosocial factors, self-care behaviors, and glycemic control.
Table 1.
Sample Demographics (n = 615).
| Variables | Mean ± SD or % |
|---|---|
| Age | 61.3 ± 10.9 |
| Diabetes duration | 12.3 ± 9.1 |
| Education (years of school) | 13.4 ± 2.8 |
| Employment | |
| Employed | 28.6 |
| Disabled | 27.1 |
| Unemployed | 10.3 |
| Retired | 34.0 |
| Race | |
| White | 33.0 |
| Black | 64.9 |
| Other | 2.1 |
| Gender | |
| Women | 38.4 |
| Men | 61.6 |
| Marital status | |
| Never married | 11.2 |
| Married | 49.7 |
| Separated/Divorced/Widow | 39.1 |
| Income | |
| <$19,000 | 41.6 |
| $20,000–$34,999 | 25.1 |
| $35,000–$49,999 | 13.8 |
| $50,000 or more | 19.5 |
| Insurance | |
| None | 9.3 |
| Private | 20.2 |
| Medicare/Medicaid | 34.9 |
| VA | 23.9 |
| Other | 11.7 |
| Health status | |
| Excellent/Very good | 13.3 |
| Good | 38.2 |
| Fair/Poor | 48.5 |
Table 2.
Descriptive Statistics for Measures Included in the Path Model.
| Variables | Mean Values ± SD |
|---|---|
| Glycemic control (HbA1c) | 7.9 ± 1.8 (4.1–14) |
| Violence | 5.1 ± 1.9 (4–16) |
| Crime | 2.1 ± .8 (1–4) |
| Discrimination | 4.7 ± 1.7 (4–15) |
| Self-efficacy | 28.2 ± 5.4 (10–40) |
| Perceived stress | 5.3 ± 3.3 (0–15) |
| Self-care | |
| General diet | 4.7 ± 2.0 (0–7) |
| Special diet | 4.0 ± 1.6 (0–7) |
| Exercise | 2.6 ± 2.2 (0–7) |
| Blood sugar testing | 4.6 ± 2.5 (0–7) |
| Foot care | 4.3 ± 2.5 (0–7) |
Range of values are in parenthesis.
Table 3.
Pearson’s Correlation (Pairwise) for All Measures Included in Path Model.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Glycemic control | – | – | – | – | – | – | – | – | – | – |
| 2. General diet | −.12 * | – | – | – | – | – | – | – | – | – |
| 3. Specific diet | −.07 | .36 * | – | – | – | – | – | – | – | – |
| 4. Exercise | −.10 * | .29 * | .15 * | – | – | – | – | – | – | – |
| 5. Blood sugar testing | .09 * | .21 * | .19 * | .11 * | – | – | – | – | – | – |
| 6. Foot care | .03 | .22 * | .22* | .12 * | .28 * | – | – | – | – | – |
| 7. Self-efficacy | −.34 * | .37 * | .22 * | .21 * | .09 * | .08 | – | – | – | – |
| 8. Stress | .12 * | −.22* | −.22 * | −.13 * | −.11 * | −.07 | −.35 * | – | – | – |
| 9. Violence | .12 * | −.09 * | −.08 | .02 | −.04 | .03 | −.15 * | .19 * | – | – |
| 10. Crime | .13 * | −.12 * | −.10 * | −.05 | −.02 | .02 | −.23* | .18 * | .46 * | – |
| 11. Discrimination | .06 | −.10 * | −.13 * | .01 | −.002 | −.01 | −.17 * | .27 * | .25 * | .20 * |
P < .05.
Table 4.
Standardized Direct, Indirect, and Total Effects for the Relationship between Neighborhood Factors, Stress, Self-Efficacy, Self-care Behaviors, and Glycemic Control.
| Variables | Direct Effects | Indirect Effects | Total Effects |
|---|---|---|---|
| Glycemic Control | |||
| →Self-efficacy | −.11*** | −.001 | −.11*** |
| →Perceived stress | −.004 | .05*** | .05* |
| →Violence | .05 | .002 | .06 |
| →Crime | .08 | .20*** | .29** |
| →Discrimination | −.02 | .08*** | .06 |
| →General diet | −.004 | - | −.004 |
| →Specific diet | −.01 | - | −.01 |
| →Exercise | −.03 | - | −.03 |
| →Blood sugar testing | .09** | - | .09** |
| →Foot care | .02 | - | .02 |
| General diet | |||
| →Self-efficacy | .12*** | - | .12*** |
| →Perceived stress | −.05* | −.06*** | .12*** |
| →Violence | −.02 | −.02 | −.04 |
| →Crime | −.04 | −.21** | −.25* |
| →Discrimination | −.02 | −.11*** | −.13* |
| Specific diet | |||
| →Self-efficacy | 04*** | - | .04*** |
| →Perceived stress | −.07** | −.02** | −.09*** |
| →Violence | −.002 | −.01 | −.02 |
| →Crime | −.04 | −.10* | −.14 |
| →Discrimination | −.05 | −.06*** | .12** |
| Exercise | |||
| →Self-efficacy | .08*** | - | .08*** |
| →Perceived stress | −.06* | −.04*** | −.10** |
| →Violence | .07 | −.02 | .06 |
| →Crime | −.10 | −.06 | −.16 |
| →Discrimination | .09 | −.06** | .02 |
| Blood sugar testing | |||
| →Self-efficacy | .03 | - | .03 |
| →Perceived stress | −.07* | −.01 | −.08* |
| →Violence | −.04 | −.01 | −.05 |
| →Crime | .06 | −.11 | −.05 |
| →Discrimination | .04 | −.06* | −.01 |
| Foot care | |||
| →Self-efficacy | .03 | - | .03 |
| →Perceived stress | −.05 | −.02 | −.06 |
| →Violence | .06 | −.01 | .05 |
| →Crime | .07 | −.01 | .06 |
| →Discrimination | −.004 | −.02 | −.02 |
| Self-efficacy | |||
| →Perceived stress | −.50*** | - | −.50*** |
| →Violence | .005 | −.09* | −.08 |
| →Crime | −1.06*** | −.26 | −.1.32*** |
| →Discrimination | −.18 | −.38*** | −.55*** |
| Perceived stress | |||
| →Violence | .17* | - | .17* |
| →Crime | .36* | .17* | .53** |
| →Discrimination | .46*** | .08** | .54*** |
| Violence | |||
| →Crime | 1.02*** | - | 1.02*** |
| →Discrimination | .19*** | .10*** | .29*** |
| Crime | |||
| →Discrimination | .10*** | - | .10*** |
Significant direct effects indicate direct association between variables. For example, higher levels of self-efficacy are associated with higher glycemic control. Significant indirect effects indicate pathways through which variables influence outcomes. For example, increased levels of crime are associated with glycemic control through psychosocial factors and self-care behaviors.
P < .05,
P < .01,
P < .001.
Figure 2 shows the final model of hypothesized pathways between specific neighborhood factors, stress, self-efficacy, self-care behaviors, and glycemic control for patients with diabetes with only significant direct paths indicated.
Figure 2.
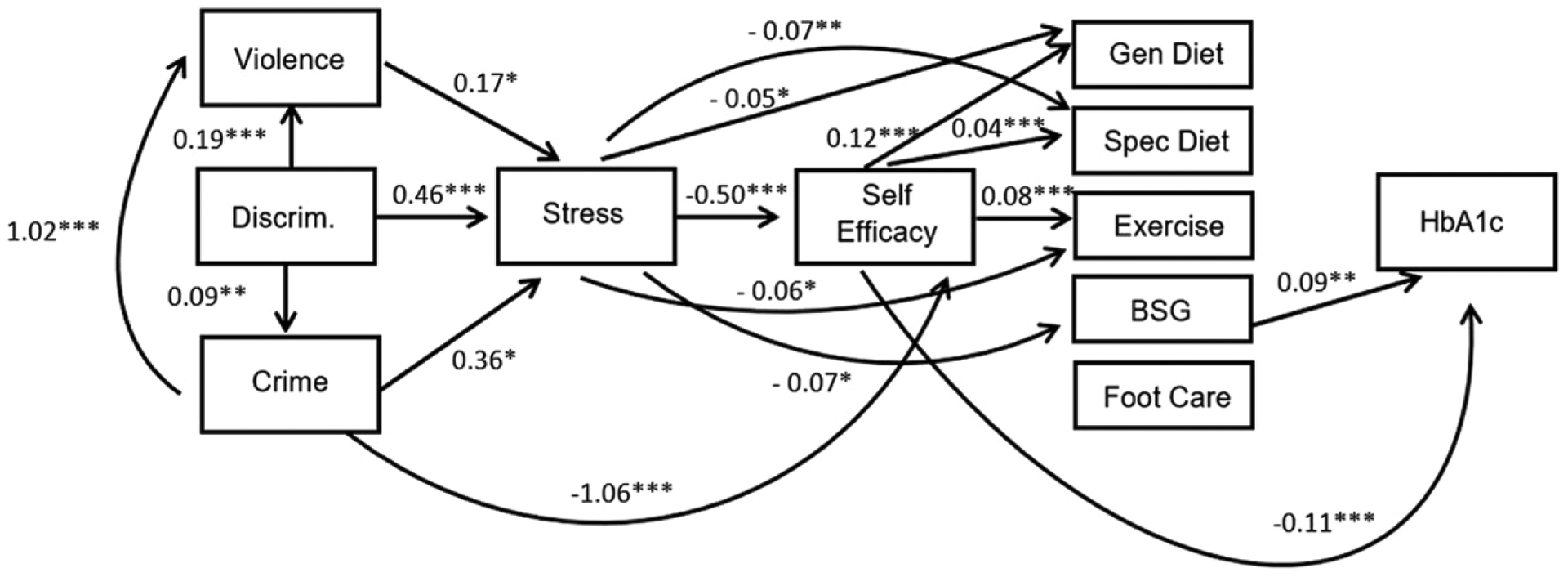
Final model showing significant pathways between neighborhood factors and glycemic control.
Note: Standardized estimates indicated. Overall model fit: chi2(2)=9.48, p<0.009, RMSEA=0.078, CFI=0.99, pclose=nonsignificant *=p<0.05, **=p<0.01, ***=p<0.001
As shown in Figure 2, the overall model fit was good using accepted standards (chi2 [2] = 9.48, P < .009, RMSEA = .078, pclose .134, CFI = .99) indicating our hypothesized relationships was supported by the data. Standardized estimates shown in Figure 2 can be compared to understand the strength of each relationship compared to others in the model with coefficients of a larger magnitude indicating greater strength. Based on direct effects in the final model, violence (r = .17, P = .024), discrimination (r = .46, P < .001), and crime (r = .36, P = .046) were directly associated with higher perceived stress, with discrimination being the strongest of those 3 relationships. Crime (r = −1.06, P < .001) and perceived stress (r = −.5, P < .001) were directly associated with lower self-efficacy, with crime being the stronger of the relationships. Stress was directly associated with poorer general diet (r = −.05, P = .031), poorer specific diet (r = −.07, P = .001), less exercise (r = −.06, P = .044), and less blood sugar testing (r = −.07, P = .046) with similar strength across self-care variables. Self-efficacy was directly associated with better general diet (r = .12, P < .001), better specific diet (r = .04, P < .001) and more exercise (r = .08, P < .001). Self-efficacy was associated with lower HbA1c (r = −.11, P < .001), while blood sugar testing was directly associated with higher HbA1c (r = .09, P = .003). Significant indirect effects included perceived stress indirectly associated with higher HbA1c (r = .05, P < .001), crime indirectly associated with higher HbA1c (r = .20, P < .001), and discrimination indirectly associated with higher HbA1c (r = .08, P < .001).
Discussion
In a sample of adults with diabetes, we found significant direct relationships between neighborhood factors (violence, discrimination, and crime) and increased stress. In addition, we found significant direct relationships between crime and poor self-efficacy. Both stress and self-efficacy were directly associated with multiple self-care variables, and self-efficacy was directly associated with better glycemic control. Blood glucose monitoring was also directly associated with better glycemic control. Based on significant direct and indirect effects, this study suggests that neighborhood factors (particularly crime and discrimination) are indirectly associated with poorer glycemic control through higher levels of perceived stress, lower levels of self-efficacy, and completion of diabetes self-care behaviors.
While existing evidence shows the relationship across various neighborhood factors and diabetes incidence and outcomes,15,17,18,45 these results provide novel insights into the stress pathway through which specific neighborhood factors (specifically discrimination and crime) appear to negatively influence diabetes outcomes, namely, glycemic control. Prior work shows perceived discrimination impacts glycemic control directly through stress and indirectly through stress via self-care behaviors29 among patients with diabetes. The current path model highlights the role of crime, violence, and discrimination play on stress and the indirect relationships of discrimination and crime on glycemic control through stress and self-efficacy, providing important insight on possible targets for programs aimed to improve outcomes for individuals with diabetes.
Specifically, programs aimed at addressing the potential impact of social determinants on health factors such as neighborhood factors on glycemic control need to account for stress and self-efficacy. These findings underscore the need to address diabetes from a more holistic standpoint that accounts for the daily lived experiences of individuals with diabetes. For example, awareness of the influence of stress resulting from where individuals live as having a role in whether patients can effectively complete self-management behaviors is needed. Although clinicians cannot directly change neighborhood factors, awareness of the role of chronic stress and poor self-efficacy that results may guide recommendations for care. For example, stress reduction interventions, empowerment strategies and social support are potential solutions that can mitigate the impact of neighborhood factors on health outcomes.
Frameworks such as the chronic care model clearly indicate that health care does not occur in a vacuum and recent work has shown that individual, community and health systems factors are important drivers of diabetes outcomes.46 Therefore, as diabetes care moves away from traditional models of care, outward facing interventions using public health approaches are greatly needed to address the role that neighborhood factors are playing on diabetes management and outcomes. For example, a number of public sector and community-based efforts have demonstrated that violence and crime can be reduced in communities by improving connectivity,47,48 developing and expanding green space across communities and surrounding vacant lots,47,48 and safe ride programs.48,49 However, due to fragmentation and isolation of interventions to address population wide disease burden such as diabetes, very little has been done to effectively integrate community level efforts into diabetes intervention development and to examine the feasibility and effect it may have on specific health outcomes, namely diabetes.50 Leveraging the current findings within the context of the existing body of evidence from public health prevention programs offers a new way forward for conceptualizing prevention models for neighborhood factors and diabetes outcomes. Development of outward facing interventions to address multiple levels of influence on diabetes outcomes is an area where future work is needed. Given the complex pathways that impact clinical outcomes and the intersection of individual, community, and health system factors, multidisciplinary efforts that leverage expertise from clinical medicine, public health and the social sciences are needed.
Though this study used novel methodology that allows investigation of direct and indirect effects, there are limitations worth noting. First, though path analysis is appropriate to investigate potential relationships and pathways, the data is cross-sectional and cannot speak to causality. Reverse causation for some elements of the model is possible and future investigation should further this work by using longitudinal data. Secondly, the time frame for study variables varied based on the look-back period for the validated scales as well as the timeframe for the A1c variable. Again, this limits our ability to evaluate for causal relationships. Longitudinal studies with measures at set intervals would be needed to address this limitation. Third, our discrimination measure was assessed at the individual level, but treated as a neighborhood factor. This is appropriate because structural racism and resulting residential segregation, which exert their influence at both the individual and neighborhood levels are underlying drivers of discrimination. Fourth, path analysis can only estimate pathways hypothesized in the model. As a result, variables not incorporated into the hypothetical model, such as frequency of diabetes care and socioecological status may have additional influence. Investigation of variables using latent structures is another possible next step in understanding pathways for factors that measured variables may not completely capture, such as self-management as a construct. Finally, this sample was collected from 2 primary care centers in the southeastern US and may not be generalizable to the entire US population. Additional work is warranted to test similar relationships across multiple regions and populations.
So What?
What is already known on this topic?
Social determinants of health such as neighborhood factors impact diabetes self-care behaviors and outcomes.
What does this article add?
The findings presented in this article add to this knowledge base by specifying violence, discrimination, and crime as key factors that influence diabetes self-care and outcomes directly and indirectly via stress and self-efficacy pathway.
What are the implications for health promotion practice or research?
Interventions aimed at mitigating stress and improving self-efficacy may improve self-care behaviors and glycemic control. In addition, as diabetes care moves away from traditional models of care, outward facing interventions using public health approaches are greatly needed to address the role that neighborhood factors are playing on diabetes management and outcomes.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article: Efforts for this study were partially supported by: National Institute of Diabetes and Digestive Kidney Disease (K24DK093699, R01DK118038, R01DK120861, PI: Egede); National Institute for Minority Health and Health Disparities (R01MD013826, PI: Egede/Walker); and American Diabetes Association (1-19-JDF-075, PI: Walker). Funding organizations had no role in the analysis, interpretation of data, or writing of the manuscript.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All study procedures were approved by the Medical University of South Carolina (PRO17676)
References
- 1.Centers for Disease Control and Prevention. National Diabetes Statistics Report. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2017. [Google Scholar]
- 2.American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Little RR, Sacks DB. HbA1c: How do we measure it and what does it mean?. Curr Opin Endocrinol Diabetes Obes. 2009; 16(2):113–118. [DOI] [PubMed] [Google Scholar]
- 4.Norris SL, Engelgau MM, Venkat Narayan KM. Effectiveness of self-management training in type 2 diabetes: A systematic review of randomized controlled trials. Diabetes Care. 2001; 24(3):561–587. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Physical activity/exercise and diabetes. Diabetes Care. 2004;27(suppl 1):s58–s62. [DOI] [PubMed] [Google Scholar]
- 6.Marmot M Social determinants of health inequalities. Lancet. 2005;365(9464):1099–1104. [DOI] [PubMed] [Google Scholar]
- 7.Cubbin C, Egerter S, Braveman P, and Pedregon V. Where We Live Matters for Our Health: Neighborhoods and Health. Robert Wood Johnson Foundation. Accessed from: http://www.commissiononhealth.org/PDF/888f4a18-eb90-45be-a2f8-159e84a55a4c/Issue%20Brief%203%20Sept%2008%20-%20Neighborhoods%20and%20Health.pdf. Accessed June 4, 2020
- 8.Healthy People 2020, Social Determinants of Health. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-healthAccessed June 4, 2020
- 9.Gebreab SY, Hickson DA, Sims M, Wyatt SB, Davis SK, Correa A, et al. Neighborhood social and physical environments and type 2 diabetes mellitus in African Americans: The Jackson Heart Study. Health Place. 2017;43:128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smalls BL, Gregory CM, Zoller JS, Egede LE. Assessing the relationship between neighborhood factors and diabetes related health outcomes and self-care behaviors. BMC Health Services Research. 2015. Jun;15(1):445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christine PJ, Auchincloss AH, Bertoni AG, Carnethon MR, Sánchez BN, Moore K, et al. Longitudinal associations between neighborhood physical and social environments and incident type 2 diabetes mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA). JAMA Int Med. 2015;175(8): 1311–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walker RJ, Smalls BL, Campbell JA, Strom Williams JL, Egede LE. Impact of social determinants of health on outcomes for type 2 diabetes: A systematic review. Endocrine. 2014; 47(1):29–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. J Behav Med. 2009;32(1):20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bacon KL, Stuver SO, Cozier YC, Palmer JR, Rosenberg L, Ruiz-Narváez EA. Perceived racism and incident diabetes in the Black Women’s Health Study. Diabetologia. 2017;60(11):2221–2225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peek ME, Wagner J, Tang H, Baker DC, Chin MH. Self-reported racial/ethnic discrimination in healthcare and diabetes outcomes. Med Care. 2011. Jul;49(7):618, 625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whitaker KM, Everson-Rose SA, Pankow JS, Rodriguez CJ, Lewis TT, Kershaw KN, et al. Experiences of discrimination and incident type 2 diabetes mellitus: The Multi-Ethnic Study of Atherosclerosis (MESA). AJE (Am J Epidemiol). 2017;186(4): 445–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dawson AZ, Walker RJ, Campbell JA, Egede LE. Effect of perceived racial discrimination on self-care behaviors, glycemic control, and quality of life in adults with type 2 diabetes. Endocrine. 2015;49(2):422–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McDonald NC. The effect of objectively measured crime on walking in minority adults. Am J Health Promot. 2008. Jul;22(6): 433–435. [DOI] [PubMed] [Google Scholar]
- 19.Tamayo A, Karter AJ, Mujahid MS, Warton EM, Moffet HH, Adler N, et al. Associations of perceived neighborhood safety and crime with cardiometabolic risk factors among a population with type 2 diabetes. Health Place. 2016;39:116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Piccolo RS, Duncan DT, Pearce N, McKinlay JB. The role of neighborhood characteristics in racial/ethnic disparities in type 2 diabetes: Results from the Boston Area Community Health (BACH) Survey. Soc Sci Med. 2015;130:79–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bermudez-Millan A, Schumann KP, Feinn R, Tennen H, Wagner J. Behavioral reactivity to acute stress among Black and White women with type 2 diabetes: The roles of income and racial discrimination. J Health Psychol. 2016. Sep;21(9): 2085–2097. [DOI] [PubMed] [Google Scholar]
- 22.Epel ES, Crosswell AD, Mayer SE, Prather AA, Slavich GM, Puterman E, et al. More than a feeling: A unified view of stress measurement for population science. Front Neuroendocrinol. 2018;49:146–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hilliard ME, Yi-Frazier JP, Hessler D, Butler AM, Anderson BJ, Jaser S. Stress and A1c among people with diabetes across the lifespan. Curr Diabetes Rep. 2016;16(8):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marcovecchio ML, Chiarelli F. The effects of acute and chronic stress on diabetes control. Sci Signal. 2012;5(247):pt10. [DOI] [PubMed] [Google Scholar]
- 25.Kawakami N, Takatsuka N, Shimizu H, Ishibashi H. Depressive symptoms and occurrence of type 2 diabetes among Japanese men. Diabetes Care. 1999;22(7):1071–1076. [DOI] [PubMed] [Google Scholar]
- 26.Knol MJ, Twisk JWR, Beekman ATF, Heine RJ, Snoek FJ, Pouwer F. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006;49(5): 837, 845. [DOI] [PubMed] [Google Scholar]
- 27.Vasanth R, Ganesh A, Shanker R. Impact of stress on type 2 diabetes mellitus management. Psychiatr Danub. 2017. Sep; 29(3):416–421. [PubMed] [Google Scholar]
- 28.Achuko O, Walker RJ, Campbell JA, Dawson AZ, Egede LE. Pathways between discrimination and quality of life in patients with type 2 diabetes. Diabetes Technol Therapeut. 2016;18(3): 151–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dawson AZ, Walker RJ, Campbell JA, Egede LE. Validation of theoretical pathway between discrimination, diabetes self-care and glycemic control. J Diabetes Complicat. 2016;30(5): 858–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glover CM, Wang Y, Fogelfeld L, Lynch EB. Stress and other determinants of diabetes-specific quality of life in low-income African Americans with uncontrolled type 2 diabetes mellitus. J Health Care Poor Underserved. 2016;27(3): 1345–1356. [DOI] [PubMed] [Google Scholar]
- 31.Salim U, Bandura A. Self Efficacy the Exercise of Control. New York: WH Freeman and Company; 1997. [Google Scholar]
- 32.Lorig KR, Holman HR. Self-management education: History, definition, outcomes, and mechanisms. Ann Behav Med. 2003; 26(1):1–7. [DOI] [PubMed] [Google Scholar]
- 33.Bandura A Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191, 215. [DOI] [PubMed] [Google Scholar]
- 34.Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy?. Diabetes Care. 2006;29(4):823–829. [DOI] [PubMed] [Google Scholar]
- 35.Echeverria SE, Dietz-Roux AV, Link BG. Reliability of self-reported neighborhood characteristics. J Urban Health: Bull N Y Acad Med. 2004;81(4):682–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moffet HH, Adler N, Schillinger D, Ahmed AT, Laraia B, Selby JV, et al. Cohort Profile: The Diabetes Study of Northern California (DISTANCE)—objectives and design of a survey follow-up study of social health disparities in a managed care population. Int J Epidemiol. 2009;38(1):38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cohen S, Williamson G. Perceived Stress in a Probability Sample of the United States. In: Spacapan S, Oskamp S, eds. The Social Psychology of Health. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 38.Wallston KA, Rothman RL, Cherrington A. Psychometric Properties of the Perceived Diabetes Self-Management Scale (PDSMS). J Behav Med. 2007;30:395–401. [DOI] [PubMed] [Google Scholar]
- 39.Andreou E, Alexopoulos EC, Lionis C, Varvogli L, Gnardellis C, Chrousos GP, et al. Percieved stress scale: Reliability and validity study in Greece. Int J Environ Res Publ Health. 2011;8: 3287–3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950. [DOI] [PubMed] [Google Scholar]
- 41.Kline RB. Principles and Practice of Structural Equation Modeling. 4th Ed. New York: Guilford Press; 2016. [Google Scholar]
- 42.Schumacker RE, Lomax RG. A Beginner’s Guide to Structural Equation Modeling. 3rd ed. New York: Taylor and Francis Group; 2010. [Google Scholar]
- 43.Schreiber JB. Core reporting practices in structural equation modeling. Res Soc Adm Pharm. 2008;4:83–97. [DOI] [PubMed] [Google Scholar]
- 44.Hooper D, Caughlan J, Mullen MR. Structural equation modeling: Guidelines for determining model fit. Electron J Bus Res Methods. 2008;6:53–60. [Google Scholar]
- 45.Kowitt SD, Donahue KE, Fisher EB, Mitchell M, Young LA. How is neighborhood social disorganization associated with diabetes outcomes? A multilevel investigation of glycemic control and self-reported use of acute or emergency health care services. Clinical Diabetes Endocrinol. 2018;4(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Campbell JA, Egede LE. Individual-, community-, and health system-level barriers to optimal type 2 diabetes care for inner-city african americans: An integrative review and model development. Diabetes Educat. 2020;46(1):11–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zavoski RW, Lapidus GD, Lerer TJ, Burke G, Banco LI. Evaluating the impact of a street barrier on urban crime. Inj Prev. 1999;5(1):65–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kondo MC, Andreyeva E, South EC, MacDonald JM, Branas CC. Neighborhood interventions to reduce violence. Annu Rev Publ Health. 2018;39:253–271. [DOI] [PubMed] [Google Scholar]
- 49.Weber B Can safe ride programs reduce urban crime?. Reg Sci Urban Econ. 2014;48:1–11. [Google Scholar]
- 50.Horowitz C, Lawlor EF. Community approaches to addressing health disparities. Report for the Institute of Medicine. Washington, DC: National Academies Press; 2008. [Google Scholar]


