Abstract
Background and aim:
The Kinesio Taping (KT) is being increasingly applied in physical therapy and rehabilitation. The aim of this study was to evaluate the effect of KT on an early rehabilitation program, in combination with the standard protocol after ACL reconstruction (ACLR).
Methods:
This study enrolled 52 male patients, aged 18 to 45 years, who underwent ACLR with doubled gracilis and semitendinosus tendon (DGST) autograft. The patients were randomized into 2 groups: Group A (the control group) which received a standard rehabilitation protocol, and Group B (the experimental group), which had the same rehabilitation protocol plus the KT application. Pain intensity, range of motion, edema, thigh circumference, Tegner-Lysholm Scale and KOOS scale were measured at the second and fourth week follow-ups.
Results:
Patients in the experimental group showed significant results during the second week for both pain and edema reduction compared to the control group (p< 0.05). After 4 weeks of rehabilitation, pain intensity in the two groups was similar (n.s.), while edema reduction in the experimental group showed a significant result compared to the control group (p< 0.05). Nevertheless, the other outcomes did not show significant differences.
Conclusions:
The application of KT after ACLR contributed to relieve pain and reduce edema in the early postoperative rehabilitation period. Other potential benefits of KT on muscle activation and strength should be investigated through a longer follow-up and a targeted test. (www.actabiomedica.it)
Keywords: Kinesio Tape, ACL, Anterior cruciate ligament reconstruction, Pain
Introduction
Anterior cruciate ligament (ACL) tear is one of the most common orthopaedic sports injuries(1-4). A successful ACL reconstruction (ACLR) requires proper physical rehabilitation to help patients return to their prior active lifestyle.
The rehabilitation process is essential and targets the reduction of pain and swelling, improvement of neuromuscular control, range of motion (ROM), proprioception, and muscular strength. In the early phase of ACLR-patient rehabilitation, different protocols such as cryotherapy, knee brace, leg elevation, compression socks, continuous passive motion therapy, ankle pumping exercises, isometric exercises, and electrical stimulation are applied(5).
In this regard, the Kinesio Taping® (KT) method, developed by Dr. Kenzo Kase in 1979, has gained increasing interest in both sporting and clinical settings. It is hypothesized that the application of kinesiology taping helps to reduce inflammation, swelling, and pain, increase proprioception, muscular strength, and ROM in lower extremities(6-11). However, few studies exist reporting beneficial effects of KT in patients with ACLR (7-9). In this regard, whether there is some evidence documenting the efficacy of KT for the treatment of postoperative edema (6), the same level of evidence is not available to support its role in pain and ROM recovery. Thus, the present study not only aims to analyze the positive outcomes on reducing postoperative knee edema but also to further investigate the role of KT, in addition to a standard rehabilitation program, in the treatment of knee pain, ROM, and muscle mass recovery. We postulate that KT application alleviates early postoperative pain and knee edema after ACLR.
Materials and methods
The study protocol was approved by the local Ethical Review Board, and it was conducted under the principles of the Declaration of Helsinki and its amendments. Informed consent was obtained from all participants. We performed a prospective, randomized control study with a 4-week follow-up after ACLR. From January 2018 to June 2019 we enrolled 85 patients who had undergone ACLR with doubled gracilis and semitendinosus tendon (DGST) autograft. The following inclusion criteria were adopted: male gender, no previous history of knee surgery, ACLR with DGST autograft within 2 weeks from injury.
Exclusion criteria were the following: age less than 18 years or more than 45 years, history of lower limb surgery, history of allergic contact dermatitis, and disabilities in understanding and speech. After inclusion and exclusion criteria were applied, 52 male patients (mean age of 28.9 years) were available for the study (Fig. 1).
Figure 1.
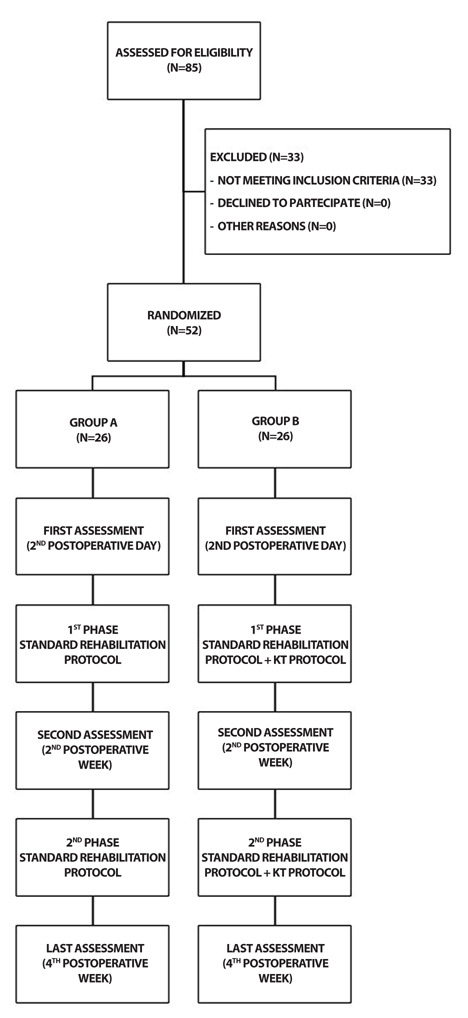
Flow diagram of study participants.
Patients were blinded randomized into two groups, group A (n=26; mean age, 29.2; SD, 4.6) and group B (n=26; mean age, 28.5; SD 5.3), by one of the study investigators using an online randomizer tool. After randomization, another study investigator assigned group A to the control group and group B to the experimental group. The control group received a standard rehabilitation protocol with isometric and isotonic muscular exercises, articular range of motion, and ice for 4 weeks; and the experimental group received the same standard rehabilitation protocol plus the KT application every 5 days for 4 weeks. All patients completed the study and were available for final follow-up.
Outcomes
The assessments were performed by the study investigators, in the absence of the physiotherapist, at the end of the 2nd and the 4th postoperative weeks. Study outcomes included the Visual Analogue Scale (VAS) for pain assessment, the knee girth (measured at the mid patella) to evaluate edema and thigh circumference (measured 10 cm above the upper edge of the patella) for muscle mass estimate after ACLR(12), the passive ROM of the knee and the submission of clinical scales: Tegner-Lysholm Knee Scale(13) and Knee Injury and Osteoarthritis Outcome Score (KOOS)(14).
Statistical Analysis
The data were analyzed by using IBM SPSS Statistics for Windows, version 23.0 (IBM Corp., Armonk, N.Y., USA). All the data were first analyzed for normality of distribution using the Kolmogorov–Smirnov test. Continuous variables were expressed as mean ± standard deviation (SD), categorical variables displayed as frequencies, and the appropriate parametric (Student’s Test t) or non-parametric test (Mann–Whitney U test or X2 test) was used to assess the significance of the differences between groups. All of the intergroup comparisons were two-sided and statistical significance was set at p<0.05.
Intervention
The rehabilitation and kinesiology taping protocols were performed by the same physiotherapist with advanced musculoskeletal physiotherapy qualifications and formal training in the application of kinesiology taping.
Rehabilitation protocol
The rehabilitation protocol common to the two groups had two phases. The first phase started on the first postoperative day and ended on the day of discharge, on the second postoperative day. The objectives of this phase were: control of pain and swelling with ice and painkillers; quadriceps recruitment through isometric and isotonic exercises performed with orthopedic knee brace locked in extension, standing and walking re-education with crutches. The second phase started from the patient's discharge and ended at the fourth postoperative week. The objectives of this phase were: control of pain and swelling with ice, recovery of complete knee ROM, recovery of the quadriceps tropism through isometric and isotonic exercises performed with orthopedic knee brace locked in extension until the 2nd postoperative week. At the 2nd postoperative week patients underwent the first clinical check, stitches were removed and outcome measures were collected. The orthopedic brace was unlocked between 0o and 90o degrees. The exercises for the muscular tropism recovery were carried out without the help of the orthopedic knee brace. At 4-week follow-up the patients underwent the second clinical evaluation, outcome measures were collected and indications were given to abandon the use of the orthopedic brace. The rehabilitation protocol was summarised in Table 1.
Table 1.
Rehabilitation protocol
| Timing | Group A (Non-Taping) n=26 | Group B (Taping) n=26 |
|---|---|---|
| 2nd postoperative day | Discharge | Discharge |
| 1st phase (1st and 2nd week) | ROM recovery; muscle strengthening; knee brace in extension; lymph drainage. |
ROM recovery; muscle strengthening; knee brace in extension; lymph drainage; KT. |
| First assessment | Clinical evaluation | Clinical evaluation |
| 2nd phase (3rd and 4th week) | ROM recovery; muscle strengthening; lymph drainage; knee brace 0-90°. |
ROM recovery; muscle strengthening; lymph drainage; knee brace 0-90°; KT. |
| Final assessment | Clinical evaluation; knee brace removal |
Clinical evaluation; knee brace removal |
Kinesiology Taping protocol
Subjects in the experimental group received the knee rehabilitation protocol plus the KT application. Taping was applied in accordance with the general taping direction of Dr. Kenzo Kase (15). In all applications, the edges of the strips were rounded to prevent them from coming unstuck. The first phase started on the second postoperative day and ended on the 2nd postoperative week. A 5-cm-wide Kinesio Tex® Tape Gold™ (Kinesio USA, Albuquerque, NM, USA) was used for the treatment. The leg was shaved before surgery. Two-strip Y-shaped tapes were applied (with 40% tension) in the origin-insertion direction in correspondence with the muscular bellies of vastus medialis and vastus lateralis of the quadriceps to facilitate the muscles. Another two strips were cut into 5 bands and applied to the popliteal fossa without tension to facilitate the hematoma resorption (Fig. 2). The second phase started from the 2nd postoperative week and ended at the 4th week. The leg was shaved again, to allow better adhesion of the tape. The same KT application was maintained for the vastus medialis and the vastus lateralis. Nevertheless, the draining application pattern changed, two KT strips were cut into 5 bands and applied without tension across the knee at 90° of flexion (Fig. 3).
Figure 2.

Application pattern of the Kinesio Tape during the first 2 weeks. The objectives were to drain the popliteal fossa and to stimulate the medial and lateral vastus.
Figure 3.

Application pattern of the Kinesio Tape from week 2 to week 4. The objectives were to drain the anterior aspect of the knee and to stimulate the medial and lateral vastus.
Results
The study sample consisted of fifty-two male patients randomly allocated into two groups: Group A (control group; n=26) and Group B (experimental group; n=26). The groups were homogeneous in terms of demographic characteristics (p>0.05). Eight patients in group A and 7 in group B underwent concomitant partial meniscectomy due to meniscal lesion (p=0.214; t=1.275). In particular, in group A the lateral meniscus (LM) was involved in 5 cases, and the medial meniscus (MM) in 3 cases; in group B the LM was involved in 6 cases and the MM in 2 cases. (Tab. 2).
Table 2.
Demographic data
| Variable | Group A (Non-Taping) n=26 |
Group B (Taping) n=26 |
pb |
|---|---|---|---|
| Average age ± SD | 29.2 ± 4.60 | 28.5 ± 5.30 | 0.531 |
| Gender (Male/Female) | 26/0 | 26/0 | 1.000 |
| BMI ± SD | 23.6 ± 1.8 | 23.7 ± 2.1 | 0.187 |
| Dominant side (Right/Left) | 18/8 | 16/10 | 0.128 |
| Affected side (Right/Left) | 15/11 | 14/12 | 0.620 |
| Meniscus surgery | 8 | 7 | 0.214 |
| Wound healing complications | 0 | 0 | 1.000 |
SD, Standard Deviation; BMI, Body Mass Index; bboldface indicates statistical significance (p<0.05)
Clinical data for intergroup comparison at the second and fourth week are reported in Table 3.
Table 3.
Clinical outcomes average intergroup comparison
| 2nd week | Group A (Non-Taping) n=26 (± SD) |
Group B (Taping) n=26 (± SD) |
pb |
|---|---|---|---|
| Pain VAS | 4.7 ± 1.9 | 3.2 ± 1.6 | 0.029 |
| ROM (°) | 80.3 ± 6.3 | 83.5 ± 5.7 | 0.351 |
| Knee edema (%) | -0.75 ± 0.5 | -6.0 ± 2.2 | 0.007 |
| Thigh circumference (%) | -3.5 ± 2.1 | -3.1 ± 2.0 | 0.805 |
| Tegner-Lysholm Scale | 65 ± 10.8 | 75 ± 8.7 | 0.707 |
| KOOS | 54.8 ± 4.8 | 58.3 ± 5.2 | 0.611 |
| 4th week | Group A (Non-Taping) n=26 (± SD) | Group B (Taping) n=26 (± SD) | pb |
| Pain VAS | 2.2 ± 1.3 | 1.9 ± 0.9 | 0.135 |
| ROM (°) | 91.5 ± 4.5 | 101.0 ± 9.6 | 0.213 |
| Knee edema(%) | -2.75 ± 1.4 | -7.6 ± 2.9 | 0.006 |
| Thigh circumference (%) | -4.6 ± 2.5 | -3.8 ± 2.2 | 0.798 |
| Tegner-Lysholm Scale | 76 ± 5.5 | 85 ± 9.3 | 0.866 |
| KOOS | 61.9 ± 5.3 | 67.3 ± 5.9 | 0.609 |
SD, Standard Deviation; ROM, Range of Motion; KOOS, Knee Injury and Osteoarthritis Outcome Score; bboldface indicates statistical significance (p<0.05)
The KT group showed lower pain intensity scores at the second week in comparison to the control group (p=0.029; t=2.316), while at the fourth week, the VAS score did not significantly differ between the two cohorts (p=0.135; t=1.544). In comparison to the control group, the KT group showed significant knee edema reduction in the early postoperative period both at the second (p=0.007; t=2.938) and the fourth (p=0.006; t=3.002) postoperative weeks.
There was no statistically significant decrease in thigh circumference between the two groups. No statistical significance was found concerning to the ROM recovery at the second (p=0.351; t=0.950) and the fourth (p=0.213; t=1.277) week. In the control group, the mean ROM was 80.3° at the second week and 91.5° at the fourth week; while in the KT group the mean ROM was respectively 83.5° and 101.0°.
We reported no statistical difference between the two groups at intergroup comparison for Tegner-Lysholm Knee Scale. In the second week, the control group mean score was 65 versus 75 for the experimental group (p=0.707; t=0.380). At the four week follow-up, subjects in Group A performed a mean score of 76, while the mean score in Group B was 85 (p=0.866; t=0.170). There were no statistically significant differences between the control and the experimental groups for KOOS at the second and fourth postoperative week. In the second week, mean score was 54.8 in Group A and 58.3 in Group B (p=0.611; t=0.515). At the final evaluation, group A’s mean score was 61.9, and Group B’s mean score was 67.3 (p=0.609; t=0.518).
Discussion
The most important findings of the present study were that the use of KT contributed to the reduction of early postoperative pain and edema following ACL reconstruction. The ROM did not show a statistically significant difference, but there was an appreciable difference between the 2 groups at 4 weeks (101.0 vs 91.5). This could be explained by the small sample, but there is a correlation with the reduction of edema and pain.
About the functioning of the KT, it has been theorized that the application of the KT pulls the skin upwards and increases the lymphatic drainage through an increase in interstitial space beneath the underlying skin, alleviating the interstitial pressures and therefore reducing edema and pain(6).
Previous literature examining KT efficacy in conjunction with conventional physical therapy is conflicting and confusing(6,16-18). To date, some studies show limited evidence that KT is more effective than conventional physical therapy alone in reducing pain and swelling in the short term(7,8). On the other hand, Balki et al.(9) reported that the KT method, applied in addition to the acute rehabilitation program of ACL reconstruction, was beneficial in reducing pain, swelling and improving knee flexion and hamstring muscle strength. These findings are in keeping with Boguszewski et al.(19), who reported that KT contributed to a faster improvement of ROM and a reduction in edema. However, as in several previous studies, the strength of evidence was limited by sample size (n=26).
Some authors have not found KT to be effective in improving knee rehabilitation(6,18). For instance, Laborie et al.(18) in a prospective, non-randomized comparative study, reported that KT was not effective for early postoperative pain following ACL reconstruction; while Chan et al.(8) demonstrated in a randomized controlled study the reduction of pain intensity, but no improvement in swelling, ROM or knee function. In these studies, the KT was maintained respectively for just 3 and 5 days; which is subject to considerable bias, since all studies included in the systematic review of Hörmann et al.(6) suggested that effects were visible after 7 days.
The treatment of pain and edema remains an important phase of the postoperative therapeutic regimen, especially since edema can negatively impact ROM, pain, function, and muscular strength. Traditionally, decongestive measures, including manual lymphatic drainage and compression treatment using compression hosiery, as well as exercises to promote lymph drainage, have been established for the treatment of edema(20,21).
More specifically, manual lymphatic drainage is widely accepted and used for the treatment of postoperative edema in lower extremities surgery (22,23). KT may be a valid alternative for promoting blood flow and lymphatic drainage. For this reason, KT application every 5 days can be considered as a low-cost alternative performing lymph drainage versus a patient-dedicated therapist in terms of money and time savings, and professional resources. A line of studies have focused on different potential benefits of KT application such as muscle excitability, strength, and neuromuscular control; speculating that KT may send continuous mechanical/elastic stimuli to skin receptors(24,25). However, the present study did not find that muscle atrophy could be prevented through the application of KT in the early rehabilitation period. This finding is in line with a recent meta-analysis investigating the effects of KT on muscle strength, demonstrating that KT does not promote strength gains in healthy individuals(26). Limitations of this study may include the absence of baseline values, and a control group with a sham tape. Second, neither the participant nor the investigator was blinded because the tape was clearly visible. Third, the small sample size of only 26 patients for each group and the absence of female subjects. Finally, in order to produce full observation of the changes in muscle strength, a longer follow-up period could have been required.
Conclusions
Conclusively, the application of KT in the early postoperative period after ACLR can safely relieve knee pain and reduce edema. Potential beneficial effects of KT in improving muscle activation and strength should be investigated with a longer follow-up. KT treatment may be recommended during rehabilitation after ACLR.
Acknowledgements:
The authors are grateful to L. J. Mesh for careful reading of the manuscript and language assistance. We would also like to show our gratitude to D. Frosoni, physiotherapist, for his useful suggestions.
Conflict of Interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement, etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810–817. doi: 10.4085/1062-6050-48.6.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agel J, Rockwood T, Klossner D. Collegiate ACL Injury Rates Across 15 Sports: National Collegiate Athletic Association Injury Surveillance System Data Update (2004-2005 Through 2012-2013) Clin J Sport Med. 2016;26(6):518–523. doi: 10.1097/JSM.0000000000000290. [DOI] [PubMed] [Google Scholar]
- Ferretti A, Monaco E, Fabbri M, Maestri B, De Carli A. Prevalence and Classification of Injuries of Anterolateral Complex in Acute Anterior Cruciate Ligament Tears. Arthroscopy. 2017;33(1):147–154. doi: 10.1016/j.arthro.2016.05.010. [DOI] [PubMed] [Google Scholar]
- Noyes FR, Barber Westin SD. Anterior cruciate ligament injury prevention training in female athletes: a systematic review of injury reduction and results of athletic performance tests. Sports Health. 2012;4(1):36–46. doi: 10.1177/1941738111430203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Grinsven S, van Cingel RE, Holla CJ, van Loon CJ. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18(8):1128–1144. doi: 10.1007/s00167-009-1027-2. [DOI] [PubMed] [Google Scholar]
- Hörmann J, Vach W, Jakob M, Seghers S, Saxer F. Kinesiotaping for postoperative oedema - what is the evidence? A systematic review. BMC Sports Sci Med Rehabil. 2020;12:14. doi: 10.1186/s13102-020-00162-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balki S, Göktas HE. Short-Term Effects of the Kinesio Taping® on Early Postoperative Hip Muscle Weakness in Male Patients With Hamstring Autograft or Allograft Anterior Cruciate Ligament Reconstruction. J Sport Rehabil. 2019;28(4):311–317. doi: 10.1123/jsr.2017-0219. [DOI] [PubMed] [Google Scholar]
- Chan MC, Wee JW, Lim MH. Does Kinesiology Taping Improve the Early Postoperative Outcomes in Anterior Cruciate Ligament Reconstruction? A Randomized Controlled Study. Clin J Sport Med. 2017;27(3):260–265. doi: 10.1097/JSM.0000000000000345. [DOI] [PubMed] [Google Scholar]
- Balki S, Göktaş HE, Öztemur Z. Kinesio taping as a treatment method in the acute phase of ACL reconstruction: A double-blind, placebo-controlled study. Acta Orthop Traumatol Turc. 2016;50(6):628–634. doi: 10.1016/j.aott.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yam ML, Yang Z, Zee BC, Chong KC. Effects of Kinesio tape on lower limb muscle strength, hop test, and vertical jump performances: a meta-analysis. BMC Musculoskelet Disord. 2019;20(1):212. doi: 10.1186/s12891-019-2564-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limroongreungrat W, Boonkerd C. Immediate effect of ACL kinesio taping technique on knee joint biomechanics during a drop vertical jump: a randomized crossover controlled trial. BMC Sports Sci Med Rehabil. 2019;11:32. doi: 10.1186/s13102-019-0144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soderberg GL, Ballantyne BT, Kestel LL. Reliability of lower extremity girth measurements after anterior cruciate ligament reconstruction. Physiother Res Int. 1996;1(1):7–16. doi: 10.1002/pri.43. [DOI] [PubMed] [Google Scholar]
- Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- Salavati M, Akhbari B, Mohammadi F, Mazaheri M, Khorrami M. Knee injury and Osteoarthritis Outcome Score (KOOS); reliability and validity in competitive athletes after anterior cruciate ligament reconstruction. Osteoarthritis Cartilage. 2011;19(4):406–410. doi: 10.1016/j.joca.2011.01.010. [DOI] [PubMed] [Google Scholar]
- Kase K, Wallis J, Kase T. 3rd ed. Tokyo: Kení-kai Co Ltd; 2003. Clinical Therapeutic Applications of the Kinesio Taping™ Method. [Google Scholar]
- Liu K, Qian J, Gao Q, Ruan B. Effects of Kinesio taping of the knee on proprioception, balance, and functional performance in patients with anterior cruciate ligament rupture: A retrospective case series. Medicine (Baltimore) 2019;98(48):e17956. doi: 10.1097/MD.0000000000017956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gülenç B, Kuyucu E, Biçer H, Genç SG, Yalçin S, Erdil M. Kinesiotaping Reduces Knee Diameter but Has No Effect on Differences Pain and Edema Following Knee Artroscopy. Acta Chir Orthop Traumatol Cech. 2018;85(4):285–290. [PubMed] [Google Scholar]
- Laborie M, Klouche S, Herman S, Gerometta A, Lefevre N, Bohu Y. Inefficacy of Kinesio-Taping(®) on early postoperative pain after ACL reconstruction: Prospective comparative study. Orthop Traumatol Surg Res. 2015;101(8):963–967. doi: 10.1016/j.otsr.2015.09.025. [DOI] [PubMed] [Google Scholar]
- Boguszewski D, Tomaszewska I, Adamczyk JG, Białoszewski D. Evaluation of effectiveness of kinesiology taping as an adjunct to rehabilitation following anterior cruciate ligament reconstruction. Preliminary report. Ortop Traumatol Rehabil. 2013;15(5):469–478. doi: 10.5604/15093492.1084361. [DOI] [PubMed] [Google Scholar]
- Badger C, Preston N, Seers K, Mortimer P. Physical therapies for reducing and controlling lymphoedema of the limbs. Cochrane Database Syst Rev. 2004;4:CD003141. doi: 10.1002/14651858.CD003141.pub2. [DOI] [PubMed] [Google Scholar]
- Hopkins JT, Ingersoll CD. Arthrogenic muscle inhibition: a limiting factor in joint rehabilitation. J Sport Rehabil. 2000;9(2):135–159. [Google Scholar]
- Ebert JR, Joss B, Jardine B, Wood DJ. Randomized trial investigating the efficacy of manual lymphatic drainage to improve early outcome after total knee arthroplasty. Arch Phys Med Rehabil. 2013;94(11):2103–2111. doi: 10.1016/j.apmr.2013.06.009. [DOI] [PubMed] [Google Scholar]
- Vairo GL, Miller SJ, McBrier NM, Buckley WE. Systematic review of efficacy for manual lymphatic drainage techniques in sports medicine and rehabilitation: an evidence-based practice approach. J Man Manip Ther. 2009;17(3):e80–e89. doi: 10.1179/jmt.2009.17.3.80E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serra MV, Vieira ER, Brunt D, Goethel MF, Gonçalves M, Quemelo PR. Kinesio Taping effects on knee extension force among soccer players. Braz J Phys Ther. 2015;19(2):152–158. doi: 10.1590/bjpt-rbf.2014.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira AK, Borges DT, Lins CA, Cavalcanti RL, Macedo LB, Brasileiro JS. Immediate effects of Kinesio Taping(®) on neuromuscular performance of quadriceps and balance in individuals submitted to anterior cruciate ligament reconstruction: A randomized clinical trial. J Sci Med Sport. 2016;19(1):2–6. doi: 10.1016/j.jsams.2014.12.002. [DOI] [PubMed] [Google Scholar]
- Csapo R, Alegre LM. Effects of Kinesio(®) taping on skeletal muscle strength-A meta-analysis of current evidence. J Sci Med Sport. 2015;18(4):450–456. doi: 10.1016/j.jsams.2014.06.014. [DOI] [PubMed] [Google Scholar]


