Abstract
Background and aim:
Metallic screws are commonly used to fix tibial tubercle osteotomies (TTO). However, hardware removal late after osteotomy union is one of the most common causes of reoperation following TTOs. The use of bioabsorbable screws may eliminate secondary surgeries, but there is no study on their use in this indication. The purpose of this retrospective study was to evaluate the safety and efficacy of bioabsorbable magnesium (Alloy: MgYREZr) screws in tibial tubercle osteotomy (TTO) fixation.
Methods:
Ten consecutive patients with objective patellar instability who underwent distal realignment procedure using Fulkerson TTO were retrospectively reviewed. The osteotomy was secured with two parallel 4.8 mm magnesium screws in all patients. Kujala score and Lysholm knee score were used to assess the functional outcomes before and after the operation. During the follow-up, the union of the osteotomy, displacement, and other imaging findings were evaluated with serial knee radiographs.
Results:
There were five male and five female patients with a mean age of 23.4±9.2 years (range, 15–45). The mean follow-up duration was 11.5±3.2 months (range,6–17 months). The osteotomy united in all cases at an average of 3 months. No infection or wound healing problems were seen. A significant increase in Kujala (p:.005) and Lysholm knee scores (p:.005) were recorded in all patients.
Conclusion:
Despite a limited number of patients were reviewed, the findings support that bioabsorbable magnesium screws can be safely used as an alternative fixation technique in TTO. Furthermore, it provides the advantage of eliminating the need for implant removal. (www.actabiomedica.it)
Keywords: Tibial tubercle osteotomy, Fulkerson osteotomy, bioabsorbable, biodegradable, magnesium, screw, implant
Introduction
Tibial tubercle osteotomy (TTO) is an effective surgical procedure used for the treatment of various patellofemoral (PF) disorders such as recurrent PF instability, PF malalignment/maltracking, PF osteoarthritis, and focal osteochondral lesions (1). TTO can be performed in three different configurations; isolated anteriorization (Maquet osteotomy), isolated medialization (Elmslie-Trillat procedure), or antero-medialization (Fulkerson osteotomy) (2–5). Fulkerson osteotomy has become a popular distal realignment technique used in recurrent PF instability treatment due to its advantages, such as providing both medialization and anteriorization in the desired amount by changing the angle of the osteotomy. Furthermore, the patellar height can be adjusted (1). In general, satisfactory clinical outcomes have been reported in several previous studies (6–8). Fulkerson osteotomy is a useful osteotomy, but it is not without complications. Tibial fracture, loss of knee range of knee motion, superficial and deep infection, delayed or nonunion of the osteotomy, failure of fixation, and sensorial loss have all been reported (9).
In general, two or three metallic screws are used to secure the TTO (10, 11). Because the soft tissue envelope is thin around the tibial tubercle, irritation due to protruding implants (head of screws) is one of the most common complaints, which makes kneeling uncomfortable. Thus, hardware removal late after osteotomy union is one of the most common causes of reoperation following TTOs. In a recent systematic review, Saltzman et al. reported a 19% overall incidence of implant removal in 1055 tibial TTO procedures (7). In another systematic review, almost half of the cases (49%) required hardware removal after Fulkerson osteotomy (8). Moreover, some authors reported routine implant removal in all patients (100%) regardless of symptoms (12, 13).
Hardware removal operations increase the cumulative cost of the treatment and constitute an economic burden on the limited healthcare sources (14–16). Besides, the second operation produces psychological distress for the patients and may cause undesirable complications (17). Theoretically, hardware removal might be abandoned with the use of bioabsorbable screws in TTO. Recently, magnesium screws have been used in fracture and osteotomy fixations, and successful results have been obtained in several previous studies (18–19). However, no previous clinical study demonstrates that the use of bioabsorbable Mg screws is safe and effective in TTO. The reason behind that might be the relative biomechanical weakness of bioabsorbable screws compared to conventional metallic implants (20).TTO requires a rigid fixation that should resist high shearing forces and allow union and early mobilization. The purpose of this preliminary study was to report the radiological and clinical outcomes and complications in patients who underwent Fulkerson osteotomy fixed with bioabsorbable Mg screws.
Materials and methods
Patients and study design
Ten prospectively followed consecutive patients with objective patellofemoral instability who underwent distal realignment procedure using Fulkerson TTO were retrospectively reviewed. The fixation of TTO was performed with two bioabsorbable magnesium screws (4.8 mm Ø, MAGNEZIX® CSc, Syntellix AG, Hanover, Germany) in all patients without additional fixation materials. Patients with missing clinical and radiological data and patients who were followed less than six months were excluded from the study. The imaging data stored in the picture archiving and communication system (PACS) and medical records obtained from the institutional clinical database were used to extract the demographic information, clinical findings, and imaging findings. This study was conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The institutional review board approved the study protocol, and all patients provided written informed consent for participation.
Indications for surgical treatment
There were ten patients (5 male and 5 female) with a mean age of 23.4±9.2 years (range, 15–45). Five patients presented with first-time patellar dislocation and the remaining five patients had recurrent patellar dislocation at least once previously (avarage:4, range, 2–7). The patellar apprehension test and J-sign were positive on physical examination in all patients. Preoperative clinical and radiographic characteristics of patients are summarized in Table 1. Because the tibial tubercle-trochlear groove (TT-TG) distance was abnormal and all patients were carrying several risk factors for recurrent patellar dislocation, including MPFL rupture, trochlear dysplasia, increased patellar tilt, surgical treatment (MPFL reconstruction and distal realignment) was planned. Two patients had a large osteochondral patellar fracture at the time of presentation.
Table 1.
Demographic, clinical and imaging characteristics of patients. Abbreviations, M: Male, F: Female, L: Left, R: Right, TT-TG: Tibial Tubercle-Trochlear Groove. PFI: Patellofemoral Instability
| Case # | Age, Sex, Side | Diagnosis | Number of Dislocations | Patellar Height Caton-Deschamps index | TT-TG Distance (mm) | Patellar Tilt (°) | Sulcus Angle (°) | Trochlear Dysplasia | Limb Alignment |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 17, M, L | Recurrent PFI | 2 | 0.84 | 21.3 | 30.5 | 147.4 | Type A | Normal |
| 2 | 15, F, L | Recurrent PFI | 4 | 1.18 | 18.9 | 20.5 | 148.6 | Type A | Normal |
| 3 | 17, M, R | Acute dislocation | 1 | 1.20 | 26.5 | 29.3 | 146.1 | Type B | Varus |
| 4 | 45, F, L | Recurrent PFI | 5 | 0.95 | 21.7 | 25.5 | 142 | Type B | Varus |
| 5 | 33, F, L | Acute dislocation | 1 | 1.07 | 20.3 | 26.9 | 141.9 | Type A | Valgus |
| 6 | 18, M, L | Acute dislocation | 1 | 0.87 | 22.9 | 31.2 | 161.8 | Type B | Normal |
| 7 | 22, F, R | Recurrent PFI | 7 | 0.93 | 21.0 | 47.6 | 144.9 | Type B | Normal |
| 8 | 26, M, R | Acute dislocation | 1 | 1.1 | 17.3 | 15.4 | 133.2 | Type A | Valgus |
| 9 | 23, M, L | Recurrent PFI | 2 | 1.06 | 17.8 | 31.4 | 150.3 | Type A | Normal |
| 10 | 18, F, L | Acute dislocation | 1 | 1.05 | 20.5 | 21.2 | 139.8 | Type B | Normal |
Surgical technique, implants, and postoperative rehabilitation
Under spinal anesthesia and proximal thigh tourniquet control, a longitudinal incision just lateral to the tibial tubercle was used for the surgical approach in the supine position, starting from 1cm proximal to the tibial tubercle and finishing at 6–7 cm distally. After identification of patellar tendon insertion, a 6–8 cm bone block was marked (Figure 1.a). The anterior muscular compartment was dissected, and the anterolateral cortex of the tibia was exposed with the help of posteriorly placed retractors. Two or three parallel guide-wires were placed medial to the lateral direction at the planned angle of the osteotomy (Figure 1.b). The osteotomy was performed with the help of an oscillating saw using the K-wires as a guide (Figure 1.c). Care was taken to leave an intact periosteal attachment at the distal end of the osteotomy. The proximal part of the osteotomy was carried out with thin osteotomes. After completion of osteotomy, the fragment was carefully elevated and shifted medially at the desired distance. Temporary K-wires were used to keep the osteotomy in the desired position (Figure 1.d). Two 4.8 mm bioabsorbable magnesium compression screw was used for the definitive fixation (Figure 1.e). The screws were inserted perpendicular to the osteotomy plane towards the posteromedial cortex of the tibia. Because the screws were headless, they were countersunk to the level of the cortical bone surface without leaving a prominence (Figure 1.f and g). No bone healing augmentation was used in any of the cases. The subcutaneous tissue and the skin were closed properly. In nine patients, MPFL reconstruction using semitendinosus tendon graft was also performed. Fluoroscopy was used to identify the femoral and patellar footprints of the MPFL and the proper length and position of the screws used in the TTO fixation.
Figure 1.
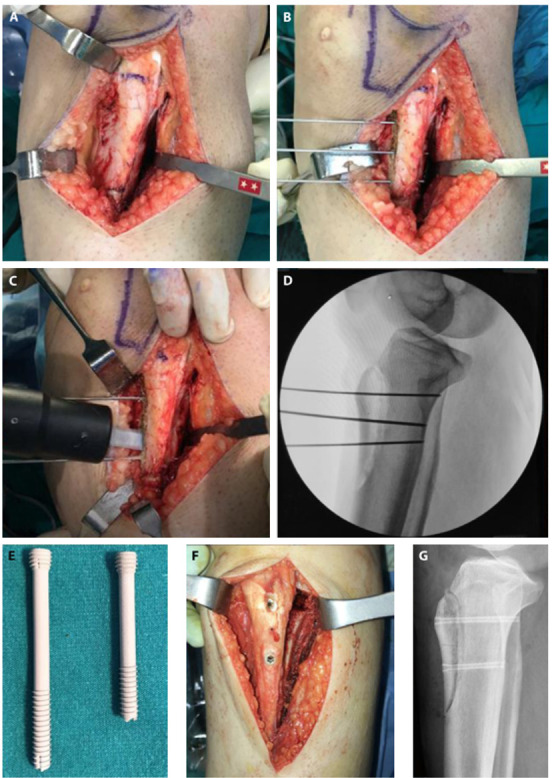
(a) Identification and marking of tibial tubercle (b) Insertion of K wires. (c) Creation of osteotomy (d) Fluoroscopic control (e) Appearance of 4.8 mm bioabsorbable magnesium compression screws (f) Fixation of the TTO and postoperative lateral radiograph (g).
Patients were not allowed weight-bearing for two weeks, but they were mobilized with crutches. The controlled knee range of motion exercises between 0–90° knee flexion and quadriceps muscle strengthening exercises were started with a hinged knee brace. In the following next two weeks, patients were encouraged full weight bearing with a locked knee brace in full extension, and patellofemoral mobility exercises (including superior, inferior, and medial but not lateral) were started. The range of motion exercises increased gradually up to 120–140° knee flexion. At the end of the 4th week, patients were allowed full weight-bearing and full knee ROM without using a knee brace. Low-intensity non-contact sport participation such as swimming, jogging was allowed after the 4th month if the instability symptoms disappeared and knee strength and motion recovered completely.
Functional evaluations
Functional outcomes were evaluated using the Kujala and Lysholm knee score before the operation and at the final follow-up. The knee range of motion was measured and compared to the contralateral side. Patellar mobility and apprehension tests were performed.
Radiographic evaluations
Patients were examined with preoperative knee radiographs, computerized tomography and/or magnetic resonance imaging. The measurements on the imaging studies included TT-TG distance, trochlear dysplasia according to Dejour classification, patellar tilt, sulcus angle, patellar height using Caton-Deschamps index, and limb alignment.
Postoperative radiographic follow-up was made with direct knee radiographs. Fracture union, any displacement, failure of fixation was monitored. Lack of tenderness with palpation and disappearance of osteotomy line on lateral radiographs were accepted as fracture union. Patients who had postoperative CT examination were also evaluated, if available.
During the course of treatment, all complications, including wound healing problems, infection, and all secondary interventions were recorded.
Statistical analysis
Statistical analysis was performed using SPSS Statistics Base v.23 for Windows. Descriptive statistics were presented using as mean ± standard deviation (SD), median, range, percentages, and frequency distribution. The Kolmogorov-Smirnov test was used to determine whether the data were distributed normally. A comparative analysis of independent variables was performed using the Wilcoxon Signed-Rank test. A value of p < 0.05 was accepted as statistically significant.
Results
Functional outcomes
Patients were followed at least six months with a mean of 11.5±3.2 months (range,6-17 months). At the final follow-up, knee range of motion was normal in seven cases, but 10-degree knee flexion was lost in 3 cases compared to the contralateral side. The patellar apprehension test was negative in all cases, but the J-sign was still positive in one case. Patellar mobility was restricted (lateral stiffness) in one case compared to the contra-lateral side. No recurrent dislocation was seen during the follow-up. A significant increase in Kujala and Lysholm knee scores was recorded in all patients (Table 2).
Table 2.
Comparison of functional outcomes before and after surgery. Abbreviations, SD: Standard Deviation. * Wilcoxon Signed Rank test.
| Variable | Preoperative Score | Final follow-up Score | p value* |
|---|---|---|---|
| Kujala Score | .005 | ||
| Mean ± SD | 47.9±18.9 | 91.6±7.9 | |
| Median | 48.5 | 91.5 | |
| Range | 13-72 | 73-100 | |
| Lysholm Knee Score | .005 | ||
| Mean ± SD | 55.9±22.5 | 93.0±8.6 | |
| Median | 58.0 | 97.0 | |
| Range | 16-87 | 72-100 | |
Radiographic results and findings
The osteotomy was united in all cases without any complications such as failure of fixation or displacement (Figure 2). In early knee radiographs, various amount of gas formation (radiolucent zone) was seen within the soft tissue and around the screws. The amount of the radiolucent zones was gradually decreased and almost disappeared in the first year of follow-up. Focal absorption of the screws was observed after the six to twelve months of follow-up (Figure 3). Postoperative CT examination was available in four cases. The gas formation was also visible clearly in CT imaging.
Figure 2.
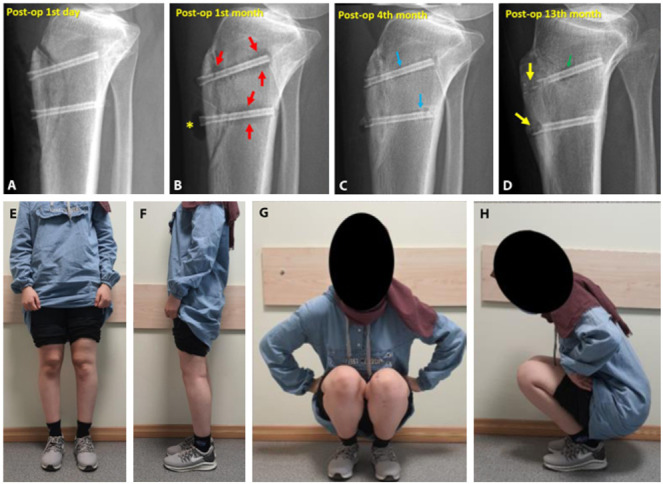
(a) Immediate postoperative radiograph. (b) First month follow-up showing radiolucent zone around the screws (red arrows) and gas accumulation within the subcutaneous tissue (yellow asterix). (c) Fourth month follow-up. Decreased radiolucency (blue arrows) and union of the osteotomy was seen. (d) Final follow-up demonstrated consolidation of the osteotomy, absorption of the screw heads and radiolucent zone around the screw (green arrow). (e-h) Final clinical appearance of the patient.
Figure 3.
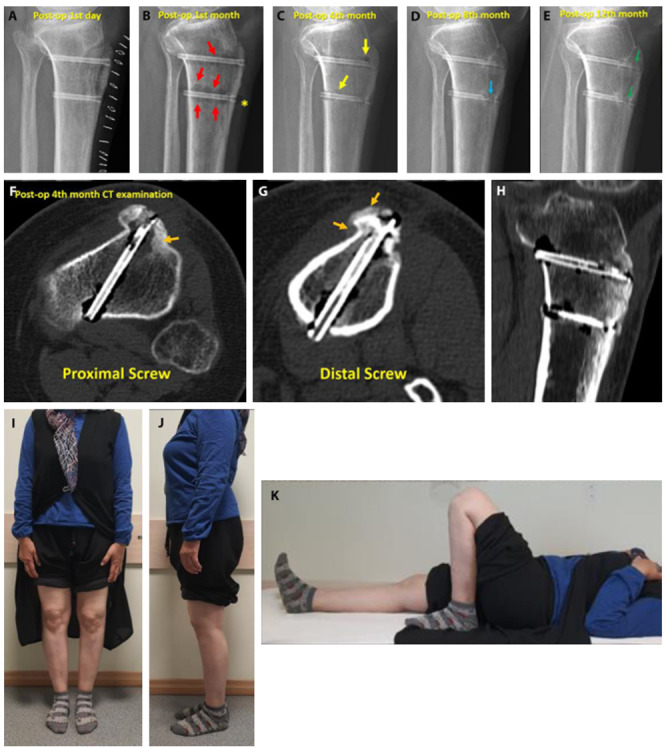
(a) Knee radiograph at the first postoperative day. (b) Red arrows show the radiolucent zones (gas formation) around the screws and subcutaneous gas at the tip of inferior screw (yellow asterix). (c) At the 4th month, note the reduced gas formation around screws (yellow arrows) and union of osteotomy. (d) At the 8th month, the absorption of the head of the inferior screw was observed (blue arrow). (e) At the final follow-up, the absorption of the screw heads was more prominent (green arrows). CT examination taken at the 4th month (f, g, h) demonstrated union of the osteotomy and ongoing new bone formation (orange arrows). (i, j, k) Clinical appearance of the patient at final follow-up.
Complications
We have observed skin crepitation over the head of the screw at the 6th week of follow-up in two patients. The patient complained of crepitation and distention feeling. A small gas bubble was observed just beneath the skin within the soft tissue on knee radiographs. There was no sign of hyperemia or wound discharge. We followed this patient without any intervention, and the gas absorption was seen in follow-up radiographs (Figure 4). None of the patients had wound healing problems or infections.
Figure 4.
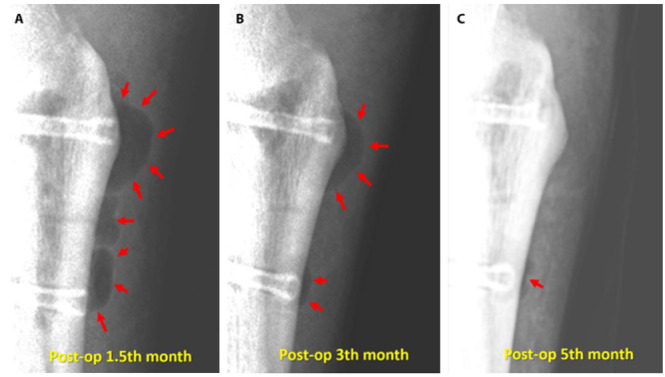
23-year-old-man with recurrent patellar dislocation. Serial lateral knee radiographs (a, b, c) with soft-tissue contrast to visualize the gas within the subcutaneous tissue (red arrows). Please note the absorption of gas through 1.5th month to 5th month follow-up.
Discussion
This preliminary study investigated the use of bioabsorbable magnesium screw fixation in a small group of patients who underwent Fulkerson TTO. The findings in this study support that bioabsorbable Mg screws are safe and effective in obtaining union without significant complications. None of the patients required a secondary implant removal operation, which was the most crucial advantage of these implants.
The knee is the largest synovial joint of the skeleton, and the quadriceps is the strongest muscle in the human body. The average maximum quadriceps force subjected to the tibial tubercle is estimated to be approximately 400 N during walking with knee extension (10, 11, 21). Thus, any implant should resist these loads and hold the fixation securely until the end of the bony union. TTO fixation can be performed either with screws or cerclage wiring. However, it has been shown that screw fixation is biomechanically superior to cerclage wiring. Davis et al. compared TTO fixation with two 4.5 mm screws and three 18-gauge cerclage wiring in 36 cadaver knees and reported that two bi-cortical screws provide the greater static fixation strength in both bevel-cut and step-cut TTO (10). In another cadaveric study, Warner et al. compared three 3.5mm screws versus two 4.5mm screws fixation for Fulkerson TTO and could not show a significant difference between these constructs regarding both the amount of displacement and load to failure (22). In a finite element analysis, Chang et al. tested different TTO shapes (step-cut, bevel-cut, and straight-cut) with different screw configurations (horizontal, trapezoid, and downwards). They suggested two horizontally inserted parallel 4.5mm screws for step-cut osteotomy fixation due to the least fragment opening between the fragments with horizontal fixation (23). These previous studies suggest that two parallel and horizontal 4.5mm fixation is sufficient for TTO fixation; however, all these studies were conducted with conventional metallic implants.
There is no clinical study on the use of bioabsorbable screws in TTO fixation, but only one biomechanical study has been conducted so far. Nurmi et al. compared standard self-tapping fully threaded cortical 4.5-mm stainless steel screw with a bioabsorbable fully threaded 4.5-mm self-reinforced polylactide (SR-PLLA) screw in 22 pairs of cadaveric knees. Based on their findings, the authors concluded that metallic screws provided better fixation strength; however, both constructs were capable of withstanding physiological loads (400N) during the knee extension (21). Magnesium alloys have been shown better mechanical strength compared to polymer materials because their tensile strength is three times that of PLLA (24). In the current study, 4.8 mm bioabsorbable Mg screws provided sufficient fixation without leading displacement or failure until the bony union. In addition, a standard rehabilitation program has been applied to these patients, similar to those who underwent metallic screw fixation. It can be concluded that bioabsorbable Mg screws are clinically satisfactory and biomechanically sufficient for TTO fixation.
Apart from the mechanical strength of magnesium screws, the reactions that occur after implantation in the human body and their radiological imaging are another issue that should be discussed. Typical radiological properties exhibited by Magnesium biomaterials were also observed in this study. Mg alloys undergo a corrosion process during bioabsorption in vivo. They react with body fluids, particularly the water, and turn into magnesium hydroxide and hydrogen gas (Mg + 2 H2O → Mg (OH) 2 + H2) (19). This gas-releasing reaction can be observed as a radiolucent zone around the screws and also within the soft tissue in direct radiographs. This phenomenon is an expected and desired reaction, and it corresponds to the corrosion process (18-19). In CT examination, the simultaneous presence of gas and the new bone formation shows that corrosion products do not interfere with bone healing. In some cases, we have observed screw breakage, which may endanger the strength of the fixation and lead to failure. However, screw breakage occurred after the bone healing process had already begun; thus, it did not cause any displacement or complication in our patients. The corrosion process is not homogenous throughout the screw, and some focal areas of the screw might react faster than the rest of the screw. This is partly related to the intensity of the exposure to the body fluids. The head of the screws could not be observed, which was compatible with the complete absorption, whereas the screw embedded within the bone was still observed during our short follow-up. The amount of gas formation is directly related to the size of the biomaterial. Since we have used relatively large 4.8mm screws, the gas formation within the soft tissue was felt by the patients as subcutaneous crepitation in two patients. On radiographic examination, we have seen relatively large gas accumulation in a focal area, which is typically seen in diffuse pattern. Both the radiologist and physicians should understand the corrosion process and its radiological consequences to avoid inaccurate interpretations and even unnecessary surgical interventions.
One of the critical issues that should be noted about Mg screws is their cost. Mg screws are more expensive than conventional implants; thus, the initial cost of the treatment is comparatively higher. However, considering the high implant removal rates in this indication (19%-100%), the cumulative costs may be reduced. Although there is no previous cost-benefit analysis study on magnesium screws, bioabsorbable screws made of polymers have been shown to be cost-effective in several different indications (25–26). Bostman et al. estimated that a bioabsorbable implant could provide economic benefit when the implant removal requirements rise above 31% after ankle fractures (25). Each surgical procedure has specific conditions such as length of hospital stay, implant costs, and the average time to return time. Although we cannot generalize these previous findings for magnesium screws used in TTO fixation, it can be proposed that a method that completely eliminates implant removal will reduce costs and, more importantly, increase patient satisfaction.
The current study has several apparent limitations, including short follow-up duration, the limited number of patients, and the lack of a comparative group. However, this preliminary study reports the initial experience of Mg screws in this specific indication in current literature. All patients were closely followed at least the union of osteotomy and relatively sufficient duration of time to observe the short-term clinical results.
Conclusion
In conclusion, this preliminary study has shown that 4.8 mm bioabsorbable Mg screws are safe and effective fixation technique for Fulkerson TTO without creating any major complication. No nonunion or malunion was seen in this series. However, it should be kept in mind that these results were obtained on a limited number of patients. Typical radiographic findings specific to the corrosion of magnesium implants were observed. The corrosion of the implant and its products did not have any undesirable effect both on the stability of the osteotomy and bone healing. Further prospective clinical trials on a higher number of patients with long-term follow-up are needed, particularly focusing on cost-effectiveness.
Ethical approval:
Institutional Review Board approved the study protocol (IRB approval date and issue: 2020.17/12)
Conflicts of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Grimm NL, Lazarides AL, Amendola A. TibialTubercle Osteotomies: a Review of a Treatment for Recurrent Patellar Instability. Curr Rev Musculoskelet Med. 2018;11(2):266–271. doi: 10.1007/s12178-018-9482-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maquet P. Advancement of the tibial tuberosity. Clin Orthop Relat Res. 1976;115:225–230. [PubMed] [Google Scholar]
- Trillat A, Dejour H, Couette A. Diagnosis and treatment of recurrent dislocations of the patella. Rev Chir Orthop Reparatrice Appar Mot. 1964;50:813–824. [PubMed] [Google Scholar]
- Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA. Anteromedial tibial tubercle transfer without bone-graft. Am J Sport Med. 1990;18(5):490–497. doi: 10.1177/036354659001800508. [DOI] [PubMed] [Google Scholar]
- Dejour D, Le Coultre B. Osteotomies in Patello-Femoral Instabilities. Sports Med Arthrosc Rev. 2018;26(1):8–15. doi: 10.1097/JSA.0000000000000183. [DOI] [PubMed] [Google Scholar]
- Longo UG, Rizzello G, Ciuffreda M, et al. Elmslie-Trillat, Maquet, Fulkerson, Roux Goldthwait, and Other Distal Realignment Procedures for the Management of Patellar Dislocation: Systematic Review and Quantitative Synthesis of the Literature. Arthroscopy. 2016;32(5):929–43. doi: 10.1016/j.arthro.2015.10.019. [DOI] [PubMed] [Google Scholar]
- Saltzman BM, Rao A, Erickson BJ, et al. A Systematic Review of 21 Tibial Tubercle Osteotomy Studies and More Than 1000 Knees: Indications, Clinical Outcomes, Complications, and Reoperations. Am J Orthop (Belle Mead NJ) 2017;46(6):E396–E407. [PubMed] [Google Scholar]
- Payne J, Rimmke N, Schmitt LC, Flanigan DC, Magnussen RA. The Incidence of Complications of Tibial Tubercle Osteotomy: A Systematic Review. Arthroscopy. 2015;31(9):1819–25. doi: 10.1016/j.arthro.2015.03.028. [DOI] [PubMed] [Google Scholar]
- Johnson AA, Wolfe EL, Mintz DN, Demehri S, Shubin Stein BE, Cosgarea AJ. Complications After Tibial Tuberosity Osteotomy: Association With Screw Size and Concomitant Distalization. Orthop J Sports Med. 2018;6(10):2325967118803614. doi: 10.1177/2325967118803614. doi: 10.1177/2325967118803614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis K, Caldwell P, Wayne J, Jiranek WA. Mechanical comparison of fixation techniques for the tibial tubercle osteotomy. Clin Orthop Relat Res. 2000;380:241–9. doi: 10.1097/00003086-200011000-00033. [DOI] [PubMed] [Google Scholar]
- Caldwell PE, Bohlen BA, Owen JR, et al. Dynamic confirmation of fixation techniques of the tibial tubercle osteotomy. Clin Orthop Relat Res. 2004;424:173–9. doi: 10.1097/01.blo.0000130205.57095.a2. [DOI] [PubMed] [Google Scholar]
- Tecklenburg K, Feller JA, Whitehead TS, Webster KE, Elzarka A. Outcome of surgery for recurrent patellar dislocation based on the distance of the tibial tuberosity to the trochlear Groove. J Bone Joint Surg Br. 2010;92(10):1376–80. doi: 10.1302/0301-620X.92B10.24439. [DOI] [PubMed] [Google Scholar]
- Shelbourne KD, Porter DA, Rozzi W. Use of a modified Elmslie-Trillat procedure to improve abnormal patellar congruence angle. Am J Sports Med. 1994;122:318–323. doi: 10.1177/036354659402200304. [DOI] [PubMed] [Google Scholar]
- Juutilainen T, Pätiälä H, Ruuskanen M, Rokkanen P. Comparison of costs in ankle fractures treated with absorbable or metallic fixation devices. Arch Orthop Trauma Surg. 1997;116(4):204–8. doi: 10.1007/BF00393710. [DOI] [PubMed] [Google Scholar]
- Böstman OM. Metallic or absorbable fracture fixation devices. A cost minimization analysis. Clin Orthop Relat Res. 1996;329:233–9. [PubMed] [Google Scholar]
- Böstman O, Hirvensalo E, Partio E, Törmälä P, Rokkanen P. Impact of the use of absorbable fracture fixation implants on consumption of hospital resources and economic costs. J Trauma. 1991;31(10):1400–3. doi: 10.1097/00005373-199110000-00016. [DOI] [PubMed] [Google Scholar]
- Onche II, Osagie OE, INuhu S. Removal of orthopaedic implants: indications, outcome and economic implications. J West Afr Coll Surg. 2011;1(1):101–12. [PMC free article] [PubMed] [Google Scholar]
- Acar B, Kose O, Unal M, Turan A, Kati YA, Guler F. Comparison of magnesium versus titanium screw fixation for biplane chevron medial malleolar osteotomy in the treatment of osteochondral lesions of the talus. Eur. J. Orthop. Surg. Traumatol. 2020;30(1):163–173. doi: 10.1007/s00590-019-02524-1. [DOI] [PubMed] [Google Scholar]
- Kose O, Turan A, Unal M, Acar B, Guler F. Fixation of medial malleolar fractures with magnesium bioabsorbable headless compression screws: short-term clinical and radiological outcomes in eleven patients. Arch Orthop Trauma Surg. 2018;138(8):1069–1075. doi: 10.1007/s00402-018-2941-x. [DOI] [PubMed] [Google Scholar]
- Kozakiewicz M. Are Magnesium Screws Proper for Mandibular Condyle Head Osteosynthesis? Materials (Basel) 2020;13(11):2641. doi: 10.3390/ma13112641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurmi JT, Itälä A, Sihvonen R, et al. Bioabsorbable Versus Metal Screw in the Fixation of Tibial Tubercle Transfer: A Cadaveric Biomechanical Study. Orthop J Sports Med. 2017;5(7):2325967117714433. doi: 10.1177/2325967117714433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner BT, Kamath GV, Spang JT, Weinhold PS, Creighton RA. Comparison of fixation methods after anteromedialization osteotomy of the tibial tubercle for patellar instability. Arthroscopy. 2013;29(10):1628–34. doi: 10.1016/j.arthro.2013.06.020. [DOI] [PubMed] [Google Scholar]
- Chang CW, Chen YN, Li CT, Chung CR, Chang CH, Peng YT. Finite element study of the effects of fragment shape and screw configuration on the mechanical behavior of tibial tubercle osteotomy. J Orthop Surg (Hong Kong) 2019;27(3):2309499019861145. doi: 10.1177/2309499019861145. [DOI] [PubMed] [Google Scholar]
- Marukawa E, Tamai M, Takahashi Y, et al. Comparison of magnesium alloys and poly-l-lactide screws as degradable implants in a canine fracture model. J Biomed Mater Res B Appl Biomater. 2016;104(7):1282–9. doi: 10.1002/jbm.b.33470. [DOI] [PubMed] [Google Scholar]
- Böstman O, Hirvensalo E, Partio E, Törmälä P, Rokkanen P. Impact of the use of absorbable fracture fixation implants on consumption of hospital resources and economic costs. J Trauma. 1991;31(10):1400–3. doi: 10.1097/00005373-199110000-00016. [DOI] [PubMed] [Google Scholar]
- Juutilainen T, Pätiälä H, Ruuskanen M, Rokkanen P. Comparison of costs in ankle fractures treated with absorbable or metallic fixation devices. Arch Orthop Trauma Surg. 1997;116(4):204–208. doi: 10.1007/BF00393710. [DOI] [PubMed] [Google Scholar]


