Transgender individuals often take exogenous hormones to align their appearance more strongly with their gender identity (1,2). These treatments may change their kidney health and disease prevalence. Kidney disease is largely unexamined in the transgender population (3–5). This cross-sectional study was performed to fill this gap. This study was approved by the institutional review board of the University of Alabama at Birmingham (UAB).
Using the Informatics for Integrating Biology and the Bedside research tool to query the electronic medical record (EMR) database of the UAB health system for 2009–2019, diagnostic codes (e.g., ICD10: F64, ICD10: Z87.890, and SNOMED: 12271241000119109) were used to define the initial adult cohort. Preferred pronouns and gender identity in conjunction with recorded sex were used to refine the cohort. Narrative text within EMRs that indicated gender identity and sex, including assigned sex at birth, defined the cohorts. Intersex individuals and individuals whose assigned sex at birth could not be determined were excluded. The final cohort was divided into four groups on the basis of gender identity and gender-affirming hormone therapy (GAHT). Estradiol treatment was used to identify transfeminine individuals receiving gender-affirming hormone therapy (TFH); testosterone treatment was used to identify transmasculine individuals receiving gender-affirming hormone therapy (TMH). The final cohort included 274 individuals (transfeminine [TF]=74, TFH=82, transmasculine [TM]=96, and TMH=22).
Serum creatinine values and eGFRs were graphed with R; patients with one or fewer serum creatinine measurements were excluded (n=86). Manual review of patient data, including eGFR, presence of proteinuria, hematuria, and abnormal imaging data (Kidney Disease Improving Global Outcomes criteria), was used to determine AKI or CKD diagnosis and verified by a nephrologist (A.A.). A history of AKI and CKD was defined by any AKI event or CKD condition, respectively, over the 10-year span. Prevalence was defined as the number of affected individuals in the entire number of individuals.
Statistical analyses were performed using the Fisher exact test (https://www.langsrud.com/fisher.htm); a P=0.05 was considered significant. Patients who indicated Asian, Latino/Hispanic, or multiple, as well as those who declined to answer self-reported race and ethnicity, had small numbers. To reduce the risk of reidentification, those groups were combined into “non-White/non-Black.”
The mean ages of each total cohort were TFTOTAL=43 years (±1.2) and TMTOTAL=48 years (±1.7). The ages for each individual cohort were TF=45±2.1 years; TFH=40±1.3 years; TM=51±1.9 years; and TMH=35±2.8 years. TMH were significantly younger than TM (P<0.001) and significantly younger than TF (P=0.03). TFH were significantly younger than TM (P<0.001). All other comparisons were not significantly different. The racial demographic of the entire transgender cohort was 47% White patients, 46% Black patients, and 6% non-White/non-Black patients. The racial makeups (percentage White patients, percentage Black patients, percentage non-White/non-Black patients) of each individual cohort were as follows: TF (42%, 49%, 9%, respectively), TFH (32%, 59%, 10%, respectively), TM (59%, 39%, 2%, respectively), and TMH (73%, 27%, 0%, respectively). A comparison of the distribution of percentage White patients and percentage Black patients between cohorts indicated significant differences in TF and TMH (P=0.05), TFH and TM (P=0.001), and TFH and TMH (P=0.003); no significant differences were observed in TF and TM (P=0.08), TF and TFH (P=0.23), and TM and TMH (P=0.34). Because of low numbers, we did not compare non-White/non-Black patient distributions between cohorts.
Prevalence within the entire transgender cohort was 32% for AKI and 36% for CKD. In comparisons of prevalence of AKI between groups (Figure 1A), statistically significant differences were seen in TF and TM (P=0.005), TF and TMH (P=0.03), and TF and TFH (P=0.001). In comparisons of prevalence of CKD (Figure 1B), significant differences included TFH and TM (P=0.001); significance was not reached in the differences between TF and TFH (P=0.06) and between TM and TMH (P=0.05). No differences in stages of AKI and CKD were found. Predisposing conditions, including hypertension and diabetes, were examined independently. No differences in hypertension prevalence were found; TF=41%, TFH=33%, TM=52%, and TMH=45%. Diabetes prevalence was lower in TFH (9%) than in TM (26%; P=0.006), but no other differences were found (TF=18% and TMH=5%).
Figure 1.
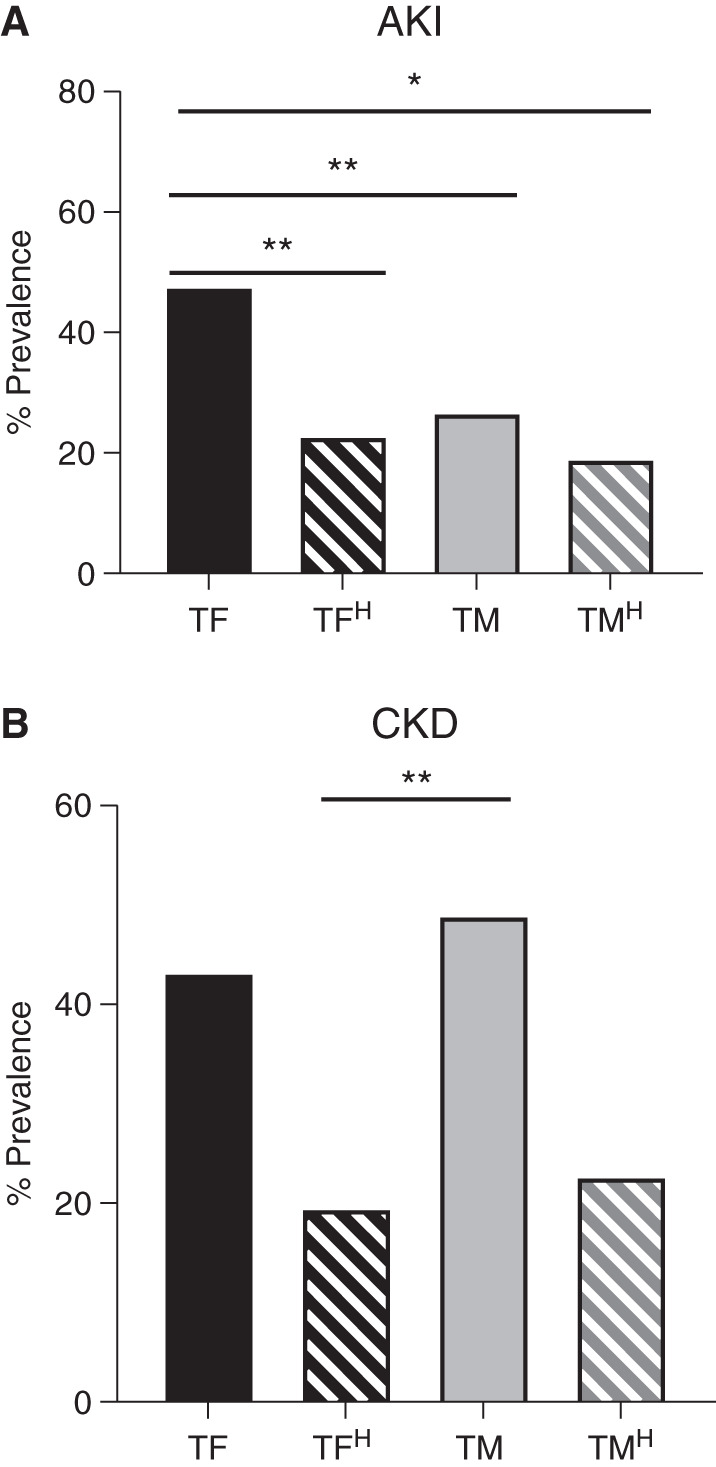
AKI and CKD prevalence rates in the transgender population differ. Prevalence within a population was examined for biologically relevant comparisons. These included (1) a comparison of transfeminine (TF) and transmasculine (TM) to establish a baseline comparison relative to cisgender individuals, (2) a comparison of transfeminine individuals receiving gender-affirming hormone therapy (TFH) and TF to understand the role of exogenous estrogen in modifying prevalence, (3) a comparison of transmasculine individuals receiving gender-affirming hormone therapy (TMH) and TM to explore the role of exogenous testosterone in modifying prevalence, (4) a comparison of TFH with TM to compare exogenous to native testosterone effects on prevalence, (5) a comparison of TMH with TF to compare exogenous and native estrogen effects on prevalence, and (6) a comparison of TFH with TMH to establish sex differences after gender-affirming hormone therapy. (A) AKI had statistically significant differences (P=0.05) between TF (47%) and TM (27%; P=0.005), between TF and TFH (P=0.002), and between TF and TMH (P=0.03). (B) CKD had significant differences between TFH (20%) and TM (49%; P=0.001). Decreases in TFH versus TF and in TMH versus TM did not reach significance (P=0.06 and P=0.05, respectively). *P≤0.05; **P≤0.01
In this study, we did not examine possible dose or duration effects of GAHT. Intersex and nonbinary individuals, who may have atypical GAHT routines, were excluded. This study used data collected from a single center; thus, these findings may not be reflective of a more heterogeneous population. Our cohort-defining methods rely on identifiable documentation. A provider may not document or may ambiguously document the transgender identity of a patient in the EMR to prevent the disclosure or due to a cisgender-facing EMR. The prevalence rates of AKI and CKD were substantially higher than expected relative to cisgender data. This result may be due to the high rate of hypertension (43%) or the high HIV positivity rate in the transgender cohort (21%), or it could potentially be indicative of high early-life stress, which may lead to greater kidney damage in adulthood.
In summary, we found lower prevalence of AKI and CKD in transgender individuals receiving GAHT compared with those not receiving GAHT, particularly in TFH. This novel study is the first to investigate AKI and CKD prevalence in transgender individuals. Given the high prevalence of AKI and CKD in this entire transgender cohort as well as differences observed with or without GAHT, further investigation is needed to ensure that transgender patients receive robust and equitable care.
We have attempted to use language that is as inclusive as possible but understand that our experiences may differ from those of the transgender community, and the language may not be as inclusive as intended. We welcome critique regarding the language used, especially from the members of the transgender, nonbinary, and gender-nonconforming community.
Disclosures
A. Agarwal reports consultancy agreements with Dynamed (reviewed content related to AKI for Dynamed and reviewed updated materials prepared by the Dynamed editorial team for AKI topics), Akebia Therapeutics (has been invited to serve on an expert panel to review new therapeutics on the basis of the hypoxia inducible factor pathway for AKI), and Reata Pharmaceuticals. A. Agarwal also reports ownership interest in Goldilocks Therapeutics, Inc.; receiving research funding from the Genzyme/Sanofi Fabry Fellowship Award; receiving honoraria from Akebia Therapeutics, Emory, the University of Southern California, and Vanderbilt; serving on the editorial boards of American Journal of Physiology–Renal Physiology, Kidney International, and Laboratory Investigation; being invited to serve on the advisory board of Goldilocks Therapeutics, Inc., a New York–based company investigating delivery of drugs in the kidney using nanotechnology for acute kidney disease and CKD; serving on the External Evaluation Panel for the Kidney Precision Medicine Program; and being invited to serve on the advisory boards of Alpha Young, LLC and Angion. L.M. Curtis is President for Women in Nephrology (2021–2022). L.M. Curtis reports receiving honoraria from the National Institutes of Health and serving on the Women in Nephrology Executive Board. O.M. Gutierrez reports consultancy agreements with QED; receiving research funding from Akebia, Amgen, and GlaxoSmithKline; receiving honoraria from Akebia, Amgen, Ardelyx, AstraZeneca, and Reata; and serving as an associate editor of CJASN. All remaining authors have nothing to disclose.
Funding
The authors acknowledge support from the UAB-University of California San Diego O’Brien Center through National Institute of Diabetes and Digestive and Kidney Diseases grant DK079337, including a Sex Differences Supplement. Research reported in this publication was supported by National Center for Advancing Translational Sciences award UL1TR003096.
Acknowledgments
The authors thank Dr. Gary Cutter, Director, Biostatistical Resource of the UAB-University of California San Diego O’Brien Center, for his help in the analysis of the data and Mr. R. Dale Johnson for his help obtaining the raw data.
This work was presented as an eposter at the 2021 American Society of Nephrology Kidney Week annual meeting (PO2241).
The authors acknowledge the use of the Informatics for Integrating Biology and the Bedside resource (i2b2).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Because Dr. Orlando M. Gutiérrez is an associate editor of CJASN, he was not involved in the peer review process for this manuscript. Another editor oversaw the peer review and decision-making process for this manuscript.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Tangpricha V: Transgender medicine: Best practices and clinical care for the future. Endocrinol Metab Clin North Am 48: xv–xvii, 2019 [DOI] [PubMed] [Google Scholar]
- 2.Lapinski J, Covas T, Perkins JM, Russell K, Adkins D, Coffigny MC, Hull S: Best practices in transgender health: A clinician’s guide. Prim Care 45: 687–703, 2018 [DOI] [PubMed] [Google Scholar]
- 3.Ocon A, Peredo-Wende R, Kremer JM, Bhatt BD: Significant symptomatic improvement of subacute cutaneous lupus after testosterone therapy in a female-to-male transgender subject. Lupus 27: 347–348, 2018 [DOI] [PubMed] [Google Scholar]
- 4.Ramadan OA-O, Naji AA-O, Levine MA-O, Porrett PA-O, Dunn TA-O, Nazarian SA-O, Weinrieb RM, Kaminski M, Johnson D, Trofe-Clark JA-O, Lorincz IA-O, Blumberg EA-O, Weikert BC, Bleicher M, Abt PL: Kidney transplantation and donation in the transgender population: A single-institution case series. Am J Transplant 20: 2899–2904, 2020 [DOI] [PubMed] [Google Scholar]
- 5.Whitley CT, Greene DN: Transgender man being evaluated for a kidney transplant. Clin Chem 63: 1680–1683, 2017 [DOI] [PubMed] [Google Scholar]


