Highlights
-
•
PCPs have disparate attitudes towards telemedicine primary care for adults >65.
-
•
Multilevel interventions are needed to optimize telemedicine care for older adults.
-
•
PCPs find telemedicine most effective for chronic disease management.
-
•
PCPs appreciate telemedicine’s convenience but worry about the lack of touch.
Keywords: Telemedicine, Older adults, Primary care, Implementation
Abstract
To learn how to improve telemedicine for adults >65, we asked primary care clinicians (“PCPs”) affiliated with one large Boston-area health system their views on using telemedicine (which included phone-only or video visits) with adults >65 during the COVID-19 pandemic. In open-ended questions, we asked PCPs to describe any challenges or useful experiences with telemedicine and suggestions for improving telemedicine as part of a larger web-based survey conducted between September 2020 and February 2021. Overall, 163/383 (42%) PCPs responded to the survey. Of these, 114 (70%) completed at least one open-ended question, 85% were non-Hispanic white, 59% were female, 75% were community-based, and 75% were in practice >20 years. We identified three major themes in participants’ comments including the need to optimize telemedicine; integrate telemedicine within primary care; and that PCPs had disparate attitudes towards telemedicine for older adults. To optimize telemedicine, PCPs recommended more effective digital platforms, increased utilization of home medical equipment (e.g., blood pressure cuffs), and better coordination with caregivers. For integration, PCPs recommended targeting telemedicine for certain types of visits (e.g., chronic disease management), enabling video access, and reducing administrative burdens on PCPs. As for PCP attitudes, some felt telemedicine enhanced the doctor-patient relationship, improved the patient experience, and improved show rates. Others felt that telemedicine visits were incomplete without a physical exam, were less rewarding, and could be frustrating. Overall, PCPs saw a role for telemedicine in older adults’ care but felt that more support is needed for these visits than currently offered.
1. Introduction
Adults >65 comprise 15.6% of the US population but account for 27% of US physician office visits annually; 45% of these visits are with a primary care physician (PCP) (Roberts et al., 2016, Rui and Okeyode, 2016). During the pandemic, many adults >65 years have received their primary care via telemedicine due to being at increased risk of poor outcomes from COVID-19 (Alexander et al., 2020, Vidal-Alaball et al., 2020, Wosik et al., 2020). In a May 2019 national survey of 2,256 adults aged 50–80 years, 4% reported a telemedicine visit in the previous year (Malani et al., 2019). As of June 2020, 30% of US adults aged 50–80 years reported a telemedicine visit (Malani et al., 2020).
Even before the pandemic, studies found telemedicine to be effective and acceptable to PCPs and patients, especially those in rural areas (Butzner and Cuffee, 2021, Hirko et al., 2020, Chu et al., 2021, Gomez et al., 2021, Vosburg and Robinson, 2021, Sinha et al., 2020, Powell et al., 2017, Polinski et al., 2016, Nguyen et al., 2020). However, there were many barriers to implementing telemedicine including costs, reimbursement, technological challenges, confidentiality concerns, resistance to change, and negative provider perceptions (Adler et al., 2014, LeRouge and Garfield, 2013, Molfenter et al., 2015, Rutledge et al., 2014). Coverage of virtual services was previously restricted to rural areas and communication technologies available for telemedicine were limited (Keesara et al., 2020). During the pandemic, restrictions to coverage of telemedicine were lifted and expansions included allowing the use of telemedicine services (including phone-only and video visits) for all fee-for-service Medicare beneficiaries and access to HIPAA-noncompliant private communication technologies (Keesara et al., 2020, 116th Congress, 2020).
For adults >65 years, there were known to be additional challenges to implementing telemedicine such as lower technological literacy, lack of desire, greater costs, and more sensory (e.g., visual acuity, hearing), cognitive (e.g., memory, attention) and functional (e.g., mobility, dexterity) limitations (Cajita et al., 2018, Evans et al., 2016, Joe et al., 2018, Ware et al., 2017). Yet, few studies have examined PCP perspectives on telemedicine for primary care of older adults since the pandemic. In a qualitative study, Goldberg et al. interviewed 33 U.S. PCPs who described the rapid uptake of telemedicine at the start of the pandemic and its value in protecting PCPs and patients from COVID-19 (Goldberg et al., 2021). However, as the threat of the virus waned, these PCPs also described a decline in telemedicine due to patient preference for in-person care and difficulties with telemedicine technology. Gomez et al. also used qualitative methods to learn about PCPs views on telemedicine (Gomez et al., 2021). They interviewed 11 Californian PCPs and 4 physicians-in-training and found that these physicians found telemedicine convenient and thought its use could improve care but were concerned about the lack of touch and reduced personal connection with telemedicine. Since PCPs in prior studies described the value of telemedicine but also its challenges, we aimed to use qualitative methods to continue to learn from PCPs how best to utilize and integrate telemedicine in the primary care of adults >65 years.
2. Methods
2.1. Design and setting
Between September 2020 and February 2021, we emailed all PCPs affiliated with one large health system in Boston to complete a web-based questionnaire on their experiences providing primary care via telemedicine (which included phone-only and video visits) to adults >65 since the pandemic. The health system includes PCPs affiliated with three separate medical institutions, including one large academic medical center and two large community hospitals (see Appendix A1 for additional details). The questionnaire included both open-ended and closed-ended questions. For this study, we analyzed PCP responses to the five open-ended questions on PCP perspectives regarding telemedicine for older adults. Beth Israel Deaconess Medical Center’s Institutional Review Board approved this study as exempt human subjects’ research.
2.2. Recruitment
The health system provided the research team with affiliated PCPs’ emails. We then emailed PCPs a secure web-based REDCap questionnaire to complete about their experiences providing telemedicine to adults >65. The email informed participants that participation would be kept confidential, all analyses would be deidentified, and there was no harm or effect on employment for participation. Before seeing the survey questions, PCPs had to confirm that they provided primary care by telemedicine to adults >65 since the start of the pandemic and their consent. No financial incentive was offered for participation. We sent PCPs electronic reminders to complete the survey every 3–6 weeks during the study period, with a maximum of five contact attempts per PCP. The health system advertised the study in its monthly newsletter to community-based PCPs and the academic internal medicine practice’s medical director emailed their PCPs to encourage participation.
The survey asked participants to describe their thoughts on: 1) telemedicine for delivery of primary care for adults >65; 2) conducting a Medicare Annual Wellness visit via telemedicine; 3) the future use of telemedicine; and 4) how to improve telemedicine; and 5) to share any challenging and/or useful experiences with telemedicine. The survey was pilot tested by three PCPs not affiliated with the health center before use. No edits were made to these questions throughout the study.
2.3. Analysis
We analyzed all open-ended survey responses using NVivo 11 (QSR International) qualitative software. We conducted a thematic analysis to identify themes in participants’ comments. Four investigators (GMA, RB, LBD, MAS) read the text responses for the first 15 participants and coded phrases, sentences, or longer segments of text. All codes and themes were inductive (i.e., were new or emergent from the text). The research team met to organize codes to reflect major themes. We discussed disagreements in the meaning of codes or themes until consensus was achieved. Once a codebook was established (available in Appendix A2), the text was coded in detail by two (GMA, LBD) investigators. Differences in coding were reconciled until 100% agreement was achieved. Thematic saturation was reached after the 40th interview; however, we coded all open-ended responses. To learn if themes varied by PCPs based on their experience, in interpretive analyses, we examined the frequency a theme was expressed by years in practice (<20 vs. >20 years) to see if there were qualitative differences. We present direct quotes from the data to illustrate themes that emerged.
3. Results
Overall, 163/383 (42%) PCPs responded to the larger web-based survey. Respondents were similar to non-respondents based on sex and practice site, but were more likely to be >50 years old than non-respondents (69% vs. 46%, p = 0.04). Of the respondents, 114 (70%) completed open-ended questions of which 85% were non-Hispanic white, 59% were female, 75% were community-based, and 75% had been in practice >20 years (Table 1). We identified three major themes in PCPs’ comments related to telemedicine for older adults including: 1) the need to optimize telemedicine; 2) integrate telemedicine within primary care; and 3) that PCPs had disparate attitudes towards telemedicine for older adults.
Table 1.
Sample characteristics (n = 114).
| Characteristic | n (%) |
|---|---|
| Site | |
| Boston academic internal medicine practices | 22 (19.3) |
| Boston academic geriatrics practices | 6 (5.3) |
| Boston area community practices | 86 (75.4) |
| Affiliated Physicians’ Group (APG) | 36 (41.8) |
| Lahey Health | 35 (40.7) |
| Mount Auburn Health | 15 (17,4) |
| Female | 67 (58.8) |
| Age | |
| 30-39 years | 14 (12.2) |
| 40-49 years | 13 (11.4) |
| 50-59 years | 43 (37.7) |
| 60-69 years | 33 (28.9) |
| >70 years | 11 (9.6) |
| Race | |
| Non-Hispanic White | 97 (85.1) |
| Black/African American | 0 (0) |
| Other | 17 (14.9) |
| Specialty | |
| Internal Medicine | 76 (66.6) |
| Internal Medicine/Geriatrics | 8 (7.0) |
| Family Practice | 27 (23.7) |
| Family Practice/Geriatrics | 3 (2.7) |
| Role | |
| Physician | 111 (97.3) |
| Nurse Practitioner | 3 (2.6) |
| Years in practice | |
| <10 years | 13 (11.4) |
| 11-20 years | 17 (14.9) |
| >20 years | 86 (75.4) |
| Proportion of panel adults >65 (111 reported) | |
| <10% | 5 (4.5) |
| 10-20% | 18 (16.2) |
| 21-30% | 31 (27.9) |
| 31-40% | 22 (19.8) |
| 41-50% | 11 (9.9) |
| 50-74% | 18 (16.2) |
| >75% | 6 (5.4) |
3.1. Optimizing the telemedicine visit
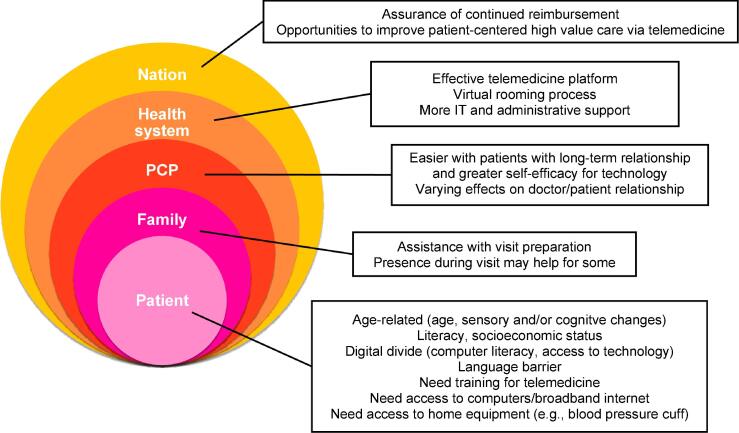
PCPs identified factors affecting optimization of telemedicine at the patient, family member, physician, health system, and national levels (Fig. 1).
Fig. 1.
Multi-level factors affecting optimization of telemedicine for older adults.
3.1.1. Patient factors
At the patient level, PCPs noted that age-related difficulties, such as sensory limitations (e.g., loss of hearing or vision), cognitive and functional decline, lower health literacy and computer literacy, language barriers, and differing access to technology affected visit quality: “This [telemedicine] can be challenging for patients with hearing impairment or language barriers” (PCP139). PCPs also noted that patients needed training in how to prepare for these visits: “Every patient needs to be coached to bring 1–3 chief complaints. They need to discard their outer clothing and wear loose [shirts] to allow visual examination, they need to wear their dentures and hearing aids, they need to be seated with the phone propped up, [and] bring their medicine bottles to the visit for viewing” (PCP52). PCPs also recommended that patients become familiar with telemedicine software and utilize home medical equipment (e.g., blood pressure cuffs) in advance of a visit. (Table 2).
Table 2.
Multi-level factors affecting optimization of the telemedicine visit and ideas for implementation and integration of telemedicine into primary care*
| Visit optimization | Example quotes |
|---|---|
| Pre-visit preparation (telemedicine instructions) | |
| Technology training | “Pre-visit preparation to determine optimal mode for [telemedicine appointment] – telephone/video.” (PCP2) |
| Coordination with caregiver | “If [patient] >65 is not as technology savvy it helps for them to have a family member set things up, particularly if a video visit is going to be done well.” (PCP51) |
| Medical assistant check-in/virtual rooming process | “Separate appointments with medical assistant to ensure subspeciality notes, labs, imaging, screenings are up to date.” (PCP13) |
| Operationalizing equipment at home | “Making sure everybody has a [blood pressure] cuff and can check their sugars.” (PCP16) |
| During visit | |
| Live virtual support (MA, technicians, operations, IT) | “Virtual support that is live with the MD/NP.” (PCP62) |
| Functional caregiver presence | “It helps to have a family member present, which is what most of my patients over 65 (and especially if older than 70) have been doing.” (PCP134) |
| Need for objective data (e.g., vital signs, labs) | “Devise a way to obtain vital signs, labs, etc.” (PCP6) |
| Support to transition visit | “Telemedicine is great for “routine” follow up of less complex patients and for initial triaging of new problems. However, there should also be an easy “exit ramp” to quickly get people into the clinic for in person [evaluation] if it is determined that telemedicine will not suffice.” (PCP71) |
| Post-visit support | |
| System for check-out management | “Need to develop more efficient effective systems for management of check out. Provider is left doing visit plus a great deal of the care coordination.” (PCP61) |
| Implementation/integration of telemedicine | Example quotes |
| Better for chronic disease management than acute care | “This is a useful modality for maintenance and surveillance of chronic conditions, however without in-person care, new diagnoses are difficult to assess fully.” (PCP83) |
| Needs to be made more efficient | “Implementation needs to be simple, single click sign on with minimal technology knowledge required.” (PCP51) |
| Video is essential compared to phone | “Video essential for all [telemedicine] visits- enhances understanding and trust and collaborative care to make eye contact, note body language, also [assessing] home [background is] helpful.” (PCP4) |
| Opportunities to make care more patient-centered | “This [has] been an incredible convenience for patients who can't travel to the practice or are fearful of coronavirus. This has also created a larger geographic footprint for patients who can come to my practice.” (PCP3) |
| Advance preparation is needed for Medicare Annual Wellness visit | “Can be quite hard going through all the necessary paperwork.” (PCP95) |
| Need for continued reimbursement | “It will have to be appropriately reimbursed and supported by office staff.” (PCP73) |
*Abbreviations: IT = information technology; MD = medical doctor; NP = nurse practitioner.
3.1.2. Family member factors
PCPs commented that it would be helpful to have family member assistance with preparation, such as setting up the technology or using home medical equipment, as well as family member presence during visits to offer support with any technological challenges or communication difficulties: “It helps to have a family member present, which is what most of my patients over 65 have been doing. They help to hold the camera, or to reiterate questions, and to set up the video call” (PCP134).
3.1.3. PCP factors
Some PCPs expressed discomfort with telemedicine technology and several expressed fear of missing something on physical exam. PCPs felt that telemedicine could support care, but that in-person visits are sometimes necessary: “It complements and helps to provide better care of the patient if we assure in-person access when medically necessary” (PCP26).
3.1.4. Health system factors
PCPs felt more numerous telemedicine platforms were needed: “I think having several options for how to reach [patients] are helpful. Sometimes you have to try three different things before you figure out a way to connect. Having hospital systems facilitate different ways will allow us to connect more successfully with older people” (PCP106). Most PCPs felt that telemedicine platforms could be simplified and better integrated into the electronic health record: “More streamlined, consistently operational, and integrated video platform would make this easier” (PCP61). PCPs also felt that more support was needed from both information technology (IT) and administrative services: “Many [patients are] unable to do the [videoconference] through Epic devised by our IT staff and IT [is] slow to absorb what the difficulties are” (PCP114).
3.1.5. National policy factors
PCPs also reported needing the assurance of continued reimbursement for telemedicine: “We are happy to continue using telemedicine as long as it continues to be reimbursed the same as an office visit” (PCP105). PCPs felt that telemedicine could allow opportunities for optimizing care (e.g., reduction of low-value care): “Excellent improvement for chronic care management and improved access for urgent care. [An] experienced [PCP] on televideo can eliminate a lot of unnecessary lab and imaging at urgent care/emergency rooms” (PCP24).
3.2. Integrating telemedicine into primary care
3.2.1. Targeting specific visit or problem types
Many PCPs felt that telemedicine, particularly when using video, was useful for some acute problems, for triage, for managing less complex chronic problems, and for counseling visits for mental health disorders: “I’d prefer in person visits for most issues, with perhaps the exception for certain conditions that can be monitored at home (e.g., blood pressure and diabetes) in patients who are able and for certain concerns like anxiety/depression” (PCP53). However, they felt that telemedicine was deficient in providing care for new problems, unstable chronic and/or complex problems, and for problems requiring objective data (e.g., labs, physical exam, etc.): “Diagnosing [a] new problem is difficult and I worry about missing [something]” (PCP79).
3.2.2. Telemedicine for Medicare annual wellness visits (AWV)
Some PCPs described some advantages of using telemedicine for AWVs because AWVs do not require a physical exam: “Why not do it this way always, especially if one has video and can see inside the home better and it allows you to address social issues better?” (PCP85). However, others felt that telemedicine made preventive visits more difficult: “What is most difficult is to try to fit all the Medicare requirements into the visit along with a review of all their current concerns and chronic medical conditions. At an in-person visit, the [medical assistant] is able to assist with the Medicare questions, background history, etc., which helps but at a telemedicine visit it’s hard to fit all that in by myself with no support” (PCP20). They also described how telemedicine AWVs could be less efficient if the patient still needed to come in for vaccinations or for an electrocardiogram and that it was: “difficult to assess gait” (PCP157). PCPs noted that “we need to make completing an HRA (health risk assessment) via telemedicine easier” (PCP155).
3.2.3. Advantages and disadvantages of telemedicine
PCPs felt telemedicine allowed for improved show rates, timeliness of visits, increased flexibility for both clinicians and patients, decreased exposures to both COVID-19 and other transmissible infections, and reduced transportation challenges for patients: “I notice improved show rates with visits, [and] more timely visits for same day/acute problems” (PCP49). However, PCPs also noted some disadvantages to telemedicine including that the visits could be more time-consuming, could increase their workload, add administrative challenges, and were not always efficient since many patients still needed to come in-person for bloodwork, imaging, screenings, and vaccines: “With coming into the office, it eliminates two visits (one telemedicine and one in-person) as they usually want to discuss health concerns in-person.” (PCP50).
3.3. Disparate attitudes towards telemedicine
3.3.1. Effects on the doctor-patient relationship
Some PCPs felt that telemedicine enhanced the doctor-patient relationship and improved the patient experience (Table 3): “I was able to assess the home environment, living conditions, home safety, and socioeconomic status. A patient stated that this was the most meaningful visit I've had“ (PCP26). Others felt that telemedicine visits were less rewarding and could be frustrating: “I find it far less useful or satisfying” (PCP130). Many PCPs, including those who had positive attitudes toward telemedicine, felt in-person care was more preferable to telemedicine, and that telemedicine could serve as an adjunct to but not a replacement for in-person care: “telemedicine has a role but is not a complete substitute for all care” (PCP75).
Table 3.
PCP attitudes vary towards telemedicine.
| PCP attitudes | Example quotes | |
|---|---|---|
| Effects on doctor-patient relationship | Strengthens: “I have enjoyed seeing people through video when we were closed. The visits are more likely to start on time so I find them less stressful than in person visits. More relaxed. Also, I love to see patients in their homes.” (PCP92) | Weakens: “It is not good medicine. You can't take care of the whole patient without laying hands on them and listening to their heart etc.” (PCP102) |
| Impacts on quality | Improves: “It creates immediate access and sudden intimacy with our patients who cannot come into the office. By improving access, we improve health. It’s that simple.” (PCP127) | Reduces: “It cannot replace the in-office care in terms of quality and safety.” (PCP132) |
| Intentions on future use | Will continue: “Will continue to use, good for some types of visits and for the folks who have trouble getting to the office.” (PCP98) | Will not continue: “I hope to significantly reduce my telemedicine visits to everyone after the pandemic.” (PCP38) |
3.3.2. Future use
Some PCPs plan to regularly incorporate telemedicine into their practices: “I plan to switch to telehealth completely in the next 1–2 years” (PCP52). However, others will not use it, will use it sparingly for specific problem or visit types, or will use it depending on practice norms: “I will do what I am allowed to do by the organization” (PCP85).
3.3.3. Variation by years in practice
PCPs in practice >20 years tended to be less likely to plan to use telemedicine after the pandemic: “I prefer in office and have for 41 years” (PCP93). They also tended to be more likely to describe negative features of telemedicine such as patient difficulty using videoconferencing software: “A large percentage of my visits are in patients >70 which drives my telephone only visits up” (PCP145).
4. Discussion
One hundred and fourteen PCPs affiliated with one large Boston-area health system described some of the benefits of telemedicine for older adults including its convenience for patients and clinicians, the ability to have a window into patients’ home lives, the opportunity to reduce transportation hurdles for older adults, and the potential efficiency for chronic disease management. However, most PCPs described favoring in-person visits because of the ability to complete a physical examination and to obtain blood work and other tests during the visit, and because of the challenges of completing a telemedicine visit with an older adult due to a multitude of factors such as low computer literacy and/or sensory limitations. Our findings suggest a need for continued innovation to improve telemedicine, that telemedicine should continue to be supported, and that its effectiveness be tested for chronic disease management in older adults.
Prior to the pandemic, there were recognized benefits to using telemedicine in some settings, however limited coverage through the Centers for Medicare and Medicaid Services (CMS) and through other insurances prevented its widespread use or development (Nguyen et al., 2020, Vosburg and Robinson, 2021, Sinha et al., 2020). During the pandemic, a rapid expansion of telemedicine occurred in both practice and policy (North, 2020, Kaplan, 2021, Centers for Medicare & Medicaid Services, 2020). While these changes were initially restricted to the public health emergency period, longer-term plans have begun to be made at both the state and federal levels; currently, 14 states specifically require payment parity between telemedicine and office visits, up from 10 in 2019 (Kaplan, 2021). Federally, telemedicine benefits for Medicare beneficiaries were modestly, but permanently, expanded at the end of 2020 (Centers for Medicare & Medicaid Services, 2020, 117th Congress, n.d..). Private insurers will likely be guided by public policy and public opinion (Kaplan, 2021, Jin et al., 2020, Volk et al., 2021). Since funding for telemedicine is likely to continue in some capacity, understanding how best to optimize and integrate telemedicine into primary care is essential.
Based on our findings, successfully integrating telemedicine in the primary care of older adults will require multiple steps at multiple levels (Cheng et al., 2021). First, there needs to be an effective and reliable telemedicine platform that is straightforward to access and for which patients and clinicians may be easily trained to use. Second, virtual support from IT, administrative staff, and caregivers are often needed. Given the dramatic increase in the demand for telemedicine at the start of the pandemic, IT was not ready (Bird, 2021, Brodwin and Ross, 2020). To keep up with the rapid demand for telemedicine, some health systems have developed automated logic flows, or bots, to act as triage/referral systems (Hollander and Carr, 2020), whereas others implemented the use of “technological liaisons” to provide set-up instructions and to perform test runs before the visit as well as to help troubleshoot the visit in real time (Calton et al., 2020). Almost all PCPs in this and other studies have described challenges associated with IT, such as difficulties navigating telemedicine platforms and having patients unable to handle the technology without support (Gomez et al., 2021, Goldberg et al., 2021). It may not be feasible to have administrative support or live IT support for these types of visits, but future platforms that allow for more digital support could be beneficial, particularly for older patients.
Similar to physicians in other studies, PCPs in our study described missing the physical exam when engaged in telemedicine and worried about missed diagnoses as a result (Gomez et al., 2021). PCPs also described the importance of video rather than phone-only for the efficiency of these visits. Prior to the pandemic, CMS provided reimbursement for telemedicine only if it included audio and visual means of communication. (Mehrotra et al., 2020, Weigel et al., 2020). However, during the pandemic telemedicine was expanded to include audio only. Despite the limitations of phone-only visits, should CMS revert to its prior requirements of both audio and visual communication regardless of patient age and/or access to technology, this may exacerbate healthcare disparities since older patients are less likely to have access to the technology or the computer literacy needed for an effective telemedicine visit (Eberly et al., 2020). To facilitate video visits with older adults, PCPs in our study noted the value of family assistance or caregivers who could troubleshoot technological difficulties, hold the camera and angle it appropriately, reiterate questions, and help with the use of home medical equipment. While older adults may need more support and care coordination to successfully use video visits, the effort to enable video visits for these patients is much needed. PCPs in our study and in others found it helpful to see patients’ homes and living conditions and transportation to medical visits can be difficult for older adults and their families (Goldberg et al., 2021). To further support these visits, home nurses and/or personal care assistants may need to be trained to support older adults with video technology.
While PCPs in the Gomez et al. study noted that telemedicine visits tended to be shorter than in-person visits, PCPs in our study did not describe this (Gomez et al., 2021). However, PCPs in both studies reported that telemedicine improved show rates (Morris, 2020) and was convenient, particularly for chronic management of hypertension, diabetes, and/or depression. Broader access and reimbursement of home medical equipment that is accurate and easy to use would further facilitate telemedicine. PCPs also appreciated the ability to call patients who were scheduled for an in-person visit and were seemingly a “no show” to conduct the visit by telemedicine instead; thereby reducing inefficiency.
While PCPs described challenges in conducting a Medicare AWV via telemedicine, they also felt that there was opportunity for innovation. Ideally, self-health assessments could be easily obtained online and transmitted to PCPs. Existing tests for auditory function, such as the digits-in-noise test (designed to test hearing acuity), have been found to be feasible and valid when done via telephone (Watson et al., 2012, Williams-Sanchez et al., 2014), and video gait and mobility assessments have been performed successfully (Venkataraman et al., 2020). Many existing questionnaires for assessing function, cognition, and mood could be optimized for implementation via telehealth. Tools to support shared decision-making around cancer screening are available on the ePrognosis website and could be used via a shared screen. To ensure such innovation occurs, there needs to be the assurance of continued reimbursement for telemedicine annual wellness visits.
A few PCPs in our study, particularly those in practice >20 years, reported that they planned to stop using telemedicine after the pandemic. Lack of data on optimal use of telemedicine, when it is most cost-effective and safe, and lack of training for PCPs may contribute to this waning enthusiasm for telemedicine. Experts have called for curricula and faculty development on telemedicine and research on the comparable safety and effectiveness of telemedicine versus traditional care (Herzer and Pronovost, 2021, Henschen et al., 2021). Our findings suggest that training PCPs on the use of telemedicine in the care of older adults may be particularly useful and that data on the outcomes of Medicare AWVs provided by telemedicine are needed.
Our study has limitations. First, our findings are limited to one geographic area and one health system. Second, respondents were older than non-respondents in the overall survey and older PCPs tended to be more likely to respond to the survey’s open-ended questions which may limit generalizability. Further limiting generalizability, 85% of participants were non-Hispanic white while 68% of internal medicine physicians are non-Hispanic white nationally (Careers, 2021). Lastly, we surveyed PCPs at one point in time and perceptions of telemedicine may be changing quickly.
Based on our findings, there are multiple levels (e.g., patient, family, PCP, health system, and national policy) where improvements to telemedicine for the provision of primary care for adults >65 are needed. Importantly, most PCPs felt that telemedicine was useful and would continue to use it in the future, particularly as a supplement to in-person care. Future work should aim to continue to improve telemedicine and test its utility in areas where it is most likely to be beneficial such as in chronic disease management.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Funding
This research was supported by Dr. Schonberg’s NIA K24 AG071906. The Investigators retained full independence in the conduct of this research. The sponsor had no role in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
Prior presentations
This manuscript was presented in part as an oral presentation at the virtual 2021 annual meeting of the Society of General Internal Medicine.
Data Availability
Data were entered into NVivo 11 (QSR international) qualitative software. The data are not publicly available to maintain participant confidentiality but are available from the corresponding author on reasonable request.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2022.101729.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Roberts T.W., Ogunwole S.U., Blakeslee L., Rabe M.A. The Population 65 Years and Older in the United States. American Community Survey ReportsPublished online. 2016;2018:25. [Google Scholar]
- Rui P, Okeyode T. National Ambulatory Medical Care Survey: 2016 National Summary Tables. Published online 2016. https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2016_namcs_ web_tables.pdf.
- Alexander G.C., Tajanlangit M., Heyward J., Mansour O., Qato D.M., Stafford R.S. Use and Content of Primary Care Office-Based vs Telemedicine Care Visits During the COVID-19 Pandemic in the US. JAMA Netw Open. 2020;3(10):e2021476. doi: 10.1001/jamanetworkopen.2020.21476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidal-Alaball J., Acosta-Roja R., Pastor Hernández N., Sanchez Luque U., Morrison D., Narejos Pérez S., Perez-Llano J., Salvador Vèrges A., López Seguí F. Telemedicine in the face of the COVID-19 pandemic. Atención Primaria. 2020;52(6):418–422. doi: 10.1016/j.aprim.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. Journal of the American Medical Informatics Association. 2020;27(6):957-962. 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed]
- Malani P, Kullgren J, Solway E. National Poll on Healthy Aging (NPHA), [United States], May 2019. Inter-university Consortium for Political and Social Research. Published online June 11, 2021. https://doi.org/10.3886/E142661V2.
- Malani P, Kullgren J, Solway E, Buis L, Singer D, Kirch M. National Poll on Healthy Aging: Telehealth Use Among Older Adults Before and During COVID-19. Published online 2020:4.
- Butzner M., Cuffee Y. Telehealth Interventions and Outcomes Across Rural Communities in the United States: Narrative Review. J Med Internet Res. 2021;23(8) doi: 10.2196/29575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirko KA, Kerver JM, Ford S, et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. Journal of the American Medical Informatics Association. 2020;27(11):1816-1818. doi:10.1093/jamia/ocaa156. [DOI] [PMC free article] [PubMed]
- Chu C., Cram P., Pang A., Stamenova V., Tadrous M., Bhatia R.S. Rural Telemedicine Use Before and During the COVID-19 Pandemic: Repeated Cross-sectional Study. Journal of Medical Internet Research. 2021;23(4) doi: 10.2196/26960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez T., Anaya Y.B., Shih K.J., Tarn D.M. A Qualitative Study of Primary Care Physicians’ Experiences With Telemedicine During COVID-19. J Am Board Fam Med. 2021;34(Supplement):S61–S70. doi: 10.3122/jabfm.2021.S1.200517. [DOI] [PubMed] [Google Scholar]
- Vosburg RW, Robinson KA. Telemedicine in Primary Care During the COVID-19 Pandemic: Provider and Patient Satisfaction Examined. Telemed J E Health. Published online May 17, 2021. 10.1089/tmj.2021.0174. [DOI] [PubMed]
- Sinha S., Kern L.M., Gingras L.F., Reshetnyak E., Tung J., Pelzman F., McGrath T.A., Sterling M.R. Implementation of Video Visits During COVID-19: Lessons Learned From a Primary Care Practice in New York City. Front Public Health. 2020;8 doi: 10.3389/fpubh.2020.0051410.3389/fpubh.2020.00514.s001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell R.E., Henstenburg J.M., Cooper G., Hollander J.E., Rising K.L. Patient Perceptions of Telehealth Primary Care Video Visits. Ann Fam Med. 2017;15(3):225–229. doi: 10.1370/afm.2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polinski J.M., Barker T., Gagliano N., Sussman A., Brennan T.A., Shrank W.H. Patients’ Satisfaction with and Preference for Telehealth Visits. J GEN INTERN MED. 2016;31(3):269–275. doi: 10.1007/s11606-015-3489-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen M., Waller M., Pandya A., Portnoy J. A Review of Patient and Provider Satisfaction with Telemedicine. Curr Allergy Asthma Rep. 2020;20(11):72. doi: 10.1007/s11882-020-00969-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler G., Pritchett L.R., Kauth M.R., Nadorff D. A Pilot Project to Improve Access to Telepsychotherapy at Rural Clinics. Telemedicine and e-Health. 2014;20(1):83–85. doi: 10.1089/tmj.2013.0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeRouge C., Garfield M. Crossing the Telemedicine Chasm: Have the U.S. Barriers to Widespread Adoption of Telemedicine Been Significantly Reduced? IJERPH. 2013;10(12):6472–6484. doi: 10.3390/ijerph10126472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molfenter T., Boyle M., Holloway D., Zwick J. Trends in telemedicine use in addiction treatment. Addict Sci Clin Pract. 2015;10(1):14. doi: 10.1186/s13722-015-0035-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutledge C.M., Haney T., Bordelon M., Renaud M., Fowler C. Telehealth: Preparing Advanced Practice Nurses to Address Healthcare Needs in Rural and Underserved Populations. International Journal of Nursing Education Scholarship. 2014;11(1):1–9. doi: 10.1515/ijnes-2013-0061. [DOI] [PubMed] [Google Scholar]
- Keesara S., Jonas A., Schulman K. Covid-19 and Health Care’s Digital Revolution. N Engl J Med. 2020;382(23):e82. doi: 10.1056/NEJMp2005835. [DOI] [PubMed] [Google Scholar]
- 116th Congress. Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020.; 2020.
- Cajita M.I., Hodgson N.A., Lam K.W., Yoo S., Han H.R. Facilitators of and Barriers to mHealth Adoption in Older Adults With Heart Failure. CIN. Computers, Informatics, Nursing. 2018;36(8):376–382. doi: 10.1097/CIN.0000000000000442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans J., Papadopoulos A., Silvers C.T., Charness N., Boot W.R., Schlachta-Fairchild L., Crump C., Martinez M., Ent C.B. Remote Health Monitoring for Older Adults and Those with Heart Failure: Adherence and System Usability. Telemedicine and e-Health. 2016;22(6):480–488. doi: 10.1089/tmj.2015.0140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joe J., Hall A., Chi N.C., Thompson H., Demiris G. IT-based wellness tools for older adults: Design concepts and feedback. Inform Health Soc Care. 2018;43(2):142–158. doi: 10.1080/17538157.2017.1290637. [DOI] [PubMed] [Google Scholar]
- Ware P., Bartlett S.J., Paré G., Symeonidis I., Tannenbaum C., Bartlett G., Poissant L., Ahmed S. Using eHealth Technologies: Interests, Preferences, and Concerns of Older Adults. Interact J Med Res. 2017;6(1):e3. doi: 10.2196/ijmr.4447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg EM, Jiménez FN, Chen K, et al. Telehealth was beneficial during COVID-19 for older Americans: A qualitative study with physicians. J Am Geriatr Soc. Published online July 20, 2021:jgs.17370. 10.1111/jgs.17370. [DOI] [PMC free article] [PubMed]
- North S. Telemedicine in the Time of COVID and Beyond. J Adolesc Health. 2020;67(2):145–146. doi: 10.1016/j.jadohealth.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan DA. Telehealth Is Poised for a Post–COVID-19 Future. OncologyLive. 2021. 22(07). 58.
- Centers for Medicare & Medicaid Services. Trump Administration Finalizes Permanent Expansion of Medicare Telehealth Services and Improved Payment for Time Doctors Spend with Patients. Published online December 1, 2020. https://www.cms.gov/newsroom/press-releases/trump-administration-finalizes-permanent-expansion-medicare-telehealth-services-and-improved-payment.
- 117th Congress. Telehealth Modernization Act. https://www.congress.gov/bill/117th-congress/senate-bill/368.
- Jin M.X., Kim S.Y., Miller L.J., Behari G., Correa R. Telemedicine: Current Impact on the Future. Cureus. 2020;12(8) doi: 10.7759/cureus.9891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volk J, Palanker D, O’Brien M, Goe CL. States’ Actions to Expand Telemedicine Access During COVID-19 | Commonwealth Fund. Commonwealth Fund. Published online June 2021. 10.26099/r95z-bs17.
- Cheng M.K.W., Allison T.A., McSteen B.W., Cattle C.J., Lo D.T. The Adoption of Video Visits During the COVID-19 Pandemic by Home Based Primary Care. J Am Geriatr Soc. 2021;69(2):318–320. doi: 10.1111/jgs.16982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird H. A now-or-never moment for telehealth? Demand will remain strong as long as technology and the healthcare industry can meet it. Healthcare Financial Management Association. Published online May 1, 2021. https://www.hfma.org/topics/hfm/2021/may/now-or-never-moment-telehealth-demand-remains-strong-technology-healthcare-industry.html.
- Brodwin E, Ross C. Surge in patients overwhelms telehealth services amid coronavirus pandemic. STAT News. Published online March 17, 2020.
- Hollander J.E., Carr B.G. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- Calton B., Abedini N., Fratkin M. Telemedicine in the Time of Coronavirus. Journal of Pain and Symptom Management. 2020;60(1):e12–e14. doi: 10.1016/j.jpainsymman.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehrotra A, Wang B, Snyder G. Telemedicine: What Should the Post-Pandemic Regulatory and Payment Landscape Look Like? Published online 2020:10.
- Weigel G, Ramaswamy A, Sobel L, Salganicoff A, Cubanski J, Freed M. Opportunities and barriers for telemedicine in the US during the COVID-19 emergency and beyond. Women’s Health Policy. Published online May 11, 2020. https://www.kff.org/womens-health-policy/issue-brief/opportunities-and-barriers-for-telemedicine-in-the-u-s-during-the-covid-19-emergency-and-beyond/.
- Eberly L.A., Khatana S.A.M., Nathan A.S., Snider C., Julien H.M., Deleener M.E., Adusumalli S. Telemedicine Outpatient Cardiovascular Care During the COVID-19 Pandemic: Bridging or Opening the Digital Divide? Circulation. 2020;142(5):510–512. doi: 10.1161/CIRCULATIONAHA.120.048185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris N.P. Virtual Visits and the Future of No-Shows. J GEN INTERN MED. 2020;35(8):2449–2450. doi: 10.1007/s11606-020-05948-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson C.S., Kidd G.R., Miller J.D., Smits C., Humes L.E. Telephone Screening Tests for Functionally Impaired Hearing: Current Use in Seven Countries and Development of a US Version. J Am Acad Audiol. 2012;23(10):757–767. doi: 10.3766/jaaa.23.10.2. [DOI] [PubMed] [Google Scholar]
- Williams-Sanchez V., McArdle R.A., Wilson R.H., Kidd G.R., Watson C.S., Bourne A.L. Validation of a Screening Test of Auditory Function Using the Telephone. J Am Acad Audiol. 2014;25(10):937–951. doi: 10.3766/jaaa.25.10.3. [DOI] [PubMed] [Google Scholar]
- Venkataraman K., Amis K., Landerman L.R., Caves K., Koh G.C., Hoenig H. Teleassessment of Gait and Gait Aids: Validity and Interrater Reliability. Physical Therapy. 2020;100(4):708–717. doi: 10.1093/ptj/pzaa005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzer K.R., Pronovost P.J. Ensuring Quality in the Era of Virtual Care. JAMA. 2021;325(5):429–430. doi: 10.1001/jama.2020.24955. [DOI] [PubMed] [Google Scholar]
- Henschen B.L., Jasti H., Kisielewski M., Pincavage A.T., Levine D. Teaching Telemedicine in the COVID-19 Era: a National Survey of Internal Medicine Clerkship Directors. J Gen Intern Med. 2021;36(11):3497–3502. doi: 10.1007/s11606-021-07061-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zippia Careers. Internal Medicine Doctor Demographics and Statistics [2021]: Internal Medicine Doctor Statistics By Race. Published January 29, 2021. Accessed December 6, 2021. https://www.zippia.com/internal-medicine-doctor-jobs/demographics/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data were entered into NVivo 11 (QSR international) qualitative software. The data are not publicly available to maintain participant confidentiality but are available from the corresponding author on reasonable request.