Abstract
Background
Parents have faced substantial social and economic challenges during the COVID-19 pandemic. Preliminary cross-sectional research has demonstrated increases in mental health problems in mothers during the COVID-19 pandemic compared with pre-pandemic estimates. We aimed to study an existing longitudinal cohort of mothers to assess changes in the prevalence of maternal depression and anxiety symptoms as a result of the COVID-19 pandemic over time and at the individual level.
Methods
In this longitudinal observational study, women who took part in the All Our Families pregnancy cohort in Canada were invited to complete a COVID-19 impact survey between May 20 and July 15, 2020. Women who had not agreed to additional research, had discontinued, were lost to follow-up, or who were not contactable via email were excluded. Maternal depression and anxiety symptoms during the COVID-19 pandemic were compared with three previous estimates collected at 3, 5, and 8-year timepoints (between April, 2012, and October, 2019). Depression symptoms were assessed using the 10-item Center for Epidemiological Studies Depression scale and anxiety symptoms were assessed using the short form of the Spielberger State-Trait Anxiety Inventory. Repeated cross-sectional analyses were done to assess temporal trends and fixed-effects regression models were fitted to assess within-person change over time.
Findings
Of the 3387 women included in the All Our Families study, 2445 women were eligible and were invited to participate in the COVID-19 impact study, of whom 1333 consented to participate, and 1301 were included in the longitudinal analysis. At the COVID-19 impact survey timepoint, a higher proportion of mothers had clinically significant depression (35·21%, 95% CI 32·48–38·04) and anxiety symptoms (31·39%, 28·76–34·15) than at all previous data collection timepoints. The mean depression score (8·31, 95% CI 7·97–8·65) and anxiety score (11·90, 11·66–12·13) at the COVID-19 pandemic timepoint were higher than previous data collection waves at the 3-year timepoint (mean depression score 5·05, 4·85–5·25; mean anxiety score 9·51, 9·35–9·66), 5-year timepoint (mean depression score 5·43, 5·20–5·66; mean anxiety score 9·49, 9·33–9·65), and 8-year timepoint (mean depression score 5·79, 5·55–6·02; mean anxiety score 10·26, 10·10–10·42). For the within-person comparisons, depression scores were a mean of 2·30 points (95% CI 1·95–2·65) higher and anxiety scores were a mean of 1·04 points (0·65–1·43) higher at the COVID-19 pandemic timepoint, after controlling for time trends. Larger increases in depression and anxiety symptoms were observed for women who had income disruptions, difficulty balancing home schooling with work responsibilities, and those with difficulty obtaining childcare. White mothers had greater increases in anxiety scores than non-white mothers and health-care workers had smaller increases in depressive symptoms than non-health-care workers.
Interpretation
Compared with previous estimates, the prevalence of maternal depression and anxiety among mothers in a Canadian cohort increased during the COVID-19 pandemic. Financial support, childcare provision, and avoiding the closure of schools, might be key priorities for preventing future increases in maternal psychological distress.
Funding
Alberta Innovates Health Solutions Interdisciplinary Team, Canadian Institutes of Health Research, Alberta Innovates, and Alberta Children's Hospital Foundation.
Introduction
The COVID-19 pandemic has led to unprecedented social and economic disruptions worldwide. In addition to the negative impact of the pandemic on the physical health of millions of people, the public health measures employed to control the spread of the virus, including the closure of all non-essential services and schools, restrictions on social gatherings, work-from-home orders, and financial sequelae (eg, job and income loss) have caused psychological distress.1, 2, 3 A rapid review on the psychological effects of quarantine during public health crises found that depression, anxiety, and post-traumatic stress symptoms were common sequelae.4
It has been proposed that some members of the population might be more susceptible to mental distress during the COVID-19 pandemic than others.3 One group that has been particularly affected by the social and financial ramifications of the COVID-19 pandemic are parents,5 especially mothers.6 In addition to working to maintain a livelihood, some parents have adopted caregiving or home schooling roles. Cross-sectional studies of maternal mental health problems during the COVID-19 pandemic have found approximately 30% of mothers reporting clinically significant symptoms of depression or anxiety.6 However, all published studies of depression and anxiety symptoms in mothers to date have been limited by scarcity of data from the pre-pandemic period, and therefore, have been unable to assess within-person change over time.7, 8, 9, 10
Research in context.
Evidence before this study
We searched PubMed, Google Scholar, and PsyArXiv and medRxiv preprint archives from database inception to Jan 27, 2021, for studies published in English on the mental health of parents during the COVID-19 pandemic, using the search terms “mental health/distress”, “parent”, “mother”, and “COVID-19”. Although studies of changes in mental health problems in the general population from the pre-pandemic time period to that during the COVID-19 pandemic have demonstrated significant increases in mental distress, no peer-reviewed longitudinal research is available in which maternal depression and anxiety symptoms have been assessed specifically. All published studies on mothers have been cross-sectional and did not include baseline data for the pre-pandemic period. Two preprints assessed changes in the prevalence of mental health symptoms among parents before and during the COVID-19 pandemic; however, these studies did not control for expected time trends. One preprint described a longitudinal time trend analysis in the general population in which women and parents of young children were particularly susceptible to increases in psychological distress during the COVID-19 pandemic. No longitudinal studies have assessed the association between COVID-19-associated factors that affect parenting (ie, loss of childcare and home school educator responsibilities) and maternal depression and anxiety.
Added value of this study
In this first (to our knowledge) study to investigate depression and anxiety symptoms in mothers after controlling for expected time trends, which included predominantly white, well-educated mothers, we found that the prevalence of depression and anxiety symptoms was higher during the COVID-19 pandemic than would be expected on the basis of previous time trends. Mothers who had experienced disruptions in income or employment, faced challenges balancing home schooling with work responsibilities, or had difficulty obtaining childcare had greater increases in depression and anxiety symptoms. White mothers had larger increases in anxiety symptoms than non-white mothers, and mothers who were health-care workers had smaller increases in depression symptoms than mothers who were not health-care workers.
Implications of all the available evidence
The prevalence of depression and anxiety symptoms increased among mothers during the early months of the COVID-19 pandemic. Whether these elevations are maintained during and after the pandemic ends requires further investigation. In addition to implications for maternal physical health, maternal mental health problems are associated with poor child development. Support efforts from governments that help to stabilise family incomes and increase job opportunities are crucial. Recovery efforts following the COVID-19 pandemic should include prioritising stable childcare and schooling to enable mothers to resume full participation in employment and income earning, as well as access to mental health care services.
Pierce and colleagues3 found that the prevalence of clinically significant mental distress in the UK increased from 16·7% in the period before the pandemic to 27·3% during the COVID-19 pandemic. Importantly, Pierce and colleagues found that the mental health implications of the COVID-19 pandemic were not uniformly distributed across the population: the largest increases in mental distress were observed among women with young children in the home. Focused empirical attention on women with children is crucial considering the implications of poor maternal mental health on child development and wellbeing.11 To our knowledge, no longitudinal studies have assessed whether parent-specific factors during the COVID-19 pandemic, such as balancing home schooling with employment or difficulties obtaining childcare, might be associated with changes in maternal mental health, specifically, between the pre-pandemic and pandemic period.
We aimed to use an existing longitudinal cohort of mothers included in the All Our Families study to assess changes in the prevalence of maternal depression and anxiety symptoms over time and at the individual level. Specifically, we aimed to estimate the prevalence of depression and anxiety symptoms among mothers during the initial phase of the COVID-19 pandemic overall and by sociodemographic and COVID-19-associated factors; compare prevalence of depression and anxiety symptoms during the COVID-19 pandemic with three previous estimates from the pre-pandemic period; and to examine differences in the impact of the COVID-19 pandemic among sociodemographic groups and COVID-19-specific factors, controlling for within-person changes and time trends.
Methods
Study design and participants
The All Our Families study,12, 13 is an ongoing pregnancy cohort in Calgary, Alberta, Canada, which began in May, 2008. Using non-probability sampling, pregnant women were actively recruited from city-wide medical laboratory offices and primary care clinics and passively recruited through posters, allowing women to volunteer for the study. Study recruitment and cohort characteristics have been published previously.12, 13 Data collection was done in waves: twice during pregnancy, at 4 months, and at 1, 2, 3, 5, and 8 years after the birth of the target child.
Eligible mothers for this study were women who were recruited into the All Our Families study, agreed to additional research, had not discontinued, were not lost to follow-up, and had an email address available on file as of May 8, 2020. All eligible mothers were invited to participate in the COVID-19 impact survey.
The first identified positive COVID-19 case in Alberta was identified on March 5, 2020, and on March 15, 2020, all schools and childcare facilities were closed. At the time this study was done, all target children in the All Our Families cohort were of school age (9–11 years) and public schools did not re-open in Alberta until September, 2020.
Data collection for this study was approved by the University of Calgary institutional review board (REB13-0868). All participants provided informed consent through the online survey.
Procedures
The COVID-19 impact survey was emailed to 2445 mothers and was completed between May 20 and July 15, 2020, using the REDCap platform. Data from women who participated in data collection waves at 3 years, 5 years, and 8 years post partum were extracted and linked across waves. Data collection was done between April, 2012, and October, 2014 for the 3-year timepoint, between June, 2014, and October, 2016 for the 5-year timepoint, and between February, 2017, and October, 2019 for the 8-year timepoint. At each timepoint, mothers were contacted to complete the questionnaires on the basis of the birthdate of their child. All women who participated at the 3–8 year timepoints were included in the cross-sectional analyses; however, only women who had mental health data available at the COVID-19 pandemic timepoint were included in the fixed-effects analysis.
We collected data on symptoms of depression and anxiety at child ages 3, 5, and 8 years and as part of the COVID-19 impact survey. The 10-item Center for Epidemiological Studies Depression scale (CES-D-10) was used to measure self-reported symptoms of depression in the past week. The CES-D-10 has strong psychometric properties and is frequently used in primary care settings to screen for depressive symptoms.14, 15 The CES-D-10 captures symptoms consistent with diagnostic criteria for depression including depressed mood, hopelessness, and sleep disruption. The 6-item short form of the Spielberger State-Trait Anxiety Inventory (STAI-SF) was used to measure self-reported symptoms of state anxiety “right now, in this moment”.16 The STAI-SF has good internal consistency, highly correlates with the larger 20-item scale,17 and has been validated in mothers.18 The STAI-SF identifies symptoms of anxiety, including feeling worried, tense, and upset. Total scores for all scales were calculated and mean scores across women are reported as the primary outcome. Scores were weighted for non-response and 95% CIs are reported to facilitate comparisons across timepoints. Internal consistency across data collection waves, as determined by Cronbach's α, was 0·81–0·87 for the CESD-10 and 0·81–0·86 for the STAI-SF.
For depression, a cutoff score of 10 or higher on the CESD-10 was used to identify clinically significant levels of depressive symptoms, which is a well established cutoff score for being at-risk for a diagnosis of clinical depression.14 For anxiety, cutoff scores for the STAI-SF have not been consistently established but a cutoff of 1 SD above the mean for anxiety has been used in previous literature.19, 20 We therefore used a STAI-SF score 1 SD above the mean at the 8-year timepoint to define clinically significant anxiety at all timepoints (total anxiety score ≥14) because the mean calculated for the 8-year timepoint was most proximal to the COVID-19 impact survey timepoint and had the highest cutoff across data collection waves, providing the most conservative estimate.
Data on ethnicity were collected during pregnancy. Family income was measured in increments of CA$10 000 at each timepoint. At child ages 3, 5, and 8 years and in the COVID-19 impact survey, maternal age was calculated on the basis of the difference between the COVID-19 impact survey completion date and maternal date of birth obtained at the initial survey. During the period of pregnancy (2008–11), mothers reported whether they had a history of mental illness (ie, depression, generalised anxiety disorder, bipolar disorder, schizophrenia, or obsessive-compulsive disorder; scored as: 1, history of mental illness; 0, no history of mental illness). At the COVID-19 impact survey timepoint, mothers reported on the impact of the COVID-19 pandemic on their income or employment and the income or employment of their partner (scored as: 1, maternal or partner had permanent or temporary job loss or income reduction; 0, no job or income loss), partner status (scored as: 1, has a partner; 0, single parent), whether they were a health-care worker (scored as: 1, yes; 0, no), whether they had children younger than 5 years in the home (1=yes, 0=no), whether or not they or anyone in their family were infected with COVID-19 (1=yes, 0=no), whether they or their partner had difficulties obtaining daytime childcare during the COVID-19 pandemic so they could work (scored as: 1, yes; 0, no), and whether they had difficulties balancing home schooling with working from home and other household responsibilities during the COVID-19 pandemic (scored as: 1, somewhat or very difficult; 0, not difficult).
Statistical analysis
All analyses are exploratory and were done using SPSS (version 25.0) and STATA (version 16). Depression and anxiety scores of all participants who responded to the COVID-19 impact survey were presented as mean (95% CI) and results were categorised by all association variables included in the analyses. The mean scores and prevalence of depression and anxiety for all participants at the three timepoints before the COVID-19 impact survey (ie, child ages 3, 5, and 8 years) were calculated. These outcomes were also reported across age and income level at each specific timepoint. We used fixed-effect regression to assess the within-person effect of the COVID-19 pandemic on depression and anxiety scores, controlling for previous time trends. The result is an average estimate of the impact of the COVID-19 pandemic within individuals, whereby a positive coefficient was considered to indicate increased depression and anxiety symptoms during the COVID-19 pandemic, accounting for pre-existing trends in mental health problems.
We estimated fixed-effects models according to the methods of Gunasekara and colleagues21 to assess within-person differences in depression and anxiety symptoms associated with the COVID-19 timepoint. Continuous depression and anxiety symptom scores were used to maximise variability in the outcome variable. Fixed-effects models are preferred over mixed-effects models in situations where there might be unmeasured time-invariant confounding, as determined by a significant Hausman test,21 which was the case in this study for both depression (p=0·03) and anxiety (p=0·047). The time trend variable included in the fixed-effects model was calculated as the difference in months between when the participant completed the 3, 5, and 8-year surveys and the completion of the COVID-19 impact survey, with an indicator variable for the COVID-19 timepoint to allow additional variation at that time. The monthly time trends in depression and anxiety scores before the COVID-19 pandemic were assessed using both linear and quadradic terms. For depression, a linear monthly increase in depression scores was observed and included in the model. For anxiety, the anxiety scores first increased and then levelled off over time and therefore both linear and quadratic terms were included in the model. Unadjusted bivariate models and adjusted multivariable models are reported. Factors that were significant (p<0·05) in the unadjusted analyses were included in the adjusted model. Thus, the impact of COVID-19 on income or employment, health-care worker status, difficulty balancing home schooling and employment, and difficulty obtaining childcare were included as variables in the adjusted depression model. Ethnicity, impact of COVID-19 on income on employment, health-care worker status, difficulty balancing home schooling and employment, and difficulty obtaining childcare were included as variables in the adjusted anxiety model.
Only participants who responded to the COVID-19 impact survey and had data available for at least one pre-pandemic timepoint were included in the fixed-effects analyses. Since less than 10% of data were missing across outcome variables and associated factors at each timepoint, we did complete case analysis. At the COVID-19 impact survey timepoint, we did analyses to compare individuals with and without missing data (appendix p 1); no differences were identified on associated variables based on missing outcome data. We did independent sample t-tests to assess demographic differences between women who were initially enrolled in the All Our Families study at baseline and those who participated in the COVID-19 impact survey.
Inverse probability weights were calculated and used to account for non-response in both the cross-sectional and fixed-effects analyses.22 Inverse probability weights for each separate timepoint (3-year, 5-year, 8-year, and COVID impact survey timepoint) were used for the cross-sectional analyses and the weights for the COVID-19 impact survey timepoint were used in the fixed-effects analyses (appendix pp 3–4). For continous variables, Pearson correlation was used to estimate the association between depression and anxiety scores at the COVID-19 timepoint.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
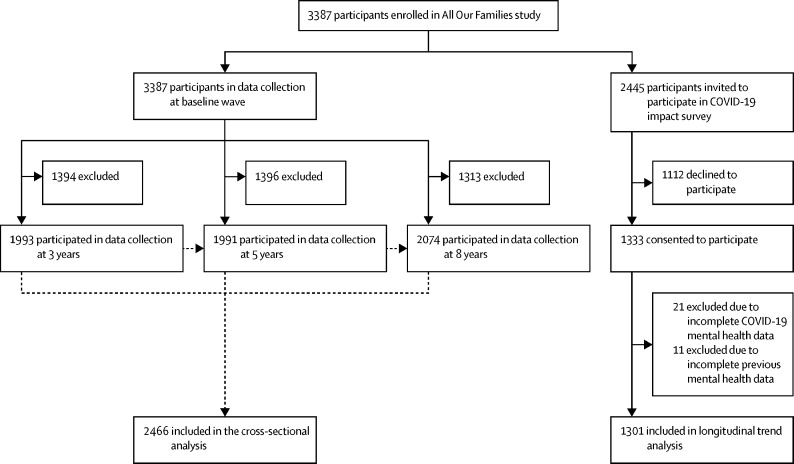
2446 women provided data for at least one of the 3, 5, or 8-year timepoints, and thus were included in the cross-sectional analyses. Of the 3387 women included in the original study, 2445 (72%) were eligible to participate in this study (figure ). Between May 20, and July 15, 2020, these 2445 women were invited to participate in the COVID-19 impact survey, of whom 1333 consented to participate (table 1 ). 1301 completed the COVID-19 impact survey and had completed at least one previous questionnaire about their mental health and thus were included in the longitudinal trend analysis (figure). Compared with women who were initially enrolled in the All Our Families survey at baseline (n=3387), women who participated in the COVID-19 impact survey had higher income (t=–6·53, p<0·0001), were older (t=–4·44, p<0·0001), and had higher education levels (t=–5·82, p<0·0001). A comparison of baseline demographic characteristics for women who responded to the COVID-19 impact survey and women who did not respond is included in the appendix (p 2).
Figure.
Study flowchart
Table 1.
Demographics of women who completed the COVID-19 impact survey and their depression and anxiety scores
| Women, n | Unweighted sample, % | Weighted sample, % | Mean depression score (95% CI) | Mean anxiety score (95% CI) | Proportion of women with clinically significant depression (95% CI) | Proportion of women with clinically significant anxiety (95% CI) | ||
|---|---|---|---|---|---|---|---|---|
| Total sample | 1333 | 100·00% | .. | 8·31 (7·97–8·65)* | 11·90 (11·66–12·13)† | 35·21% (32·48–38·04)* | 31·39% (28·76–34·15)† | |
| Women with missing data, n (%) | 113 | 8·5% | .. | .. | .. | .. | .. | |
| Age, years | ||||||||
| 25–34 | 63 | 4·93% | 6·99% | 9·32 (7·76–10·87) | 12·84 (11·76–13·91) | 44·15% (31·19–57·97) | 40·52% (27·97–54·44) | |
| 35–44 | 887 | 69·35% | 69·07% | 8·23 (7·82–8·64) | 11·79 (11·50–12·07) | 33·78% (30·60–37·12) | 30·08% (27·00–33·35) | |
| 45–54 | 329 | 25·72% | 23·94% | 8·18 (7·57–8·80) | 11·83 (11·37–12·29) | 36·13% (30·90–41·70) | 31·15% (26·22–36·55) | |
| Ethnicity | ||||||||
| Asian | 148 | 11·16% | 12·59% | 8·08 (7·05–9·11) | 11·52 (10·81–12·23) | 35·27% (27·30–44·15) | 27·05% (19·75–35·83) | |
| Black | 10 | 0·75% | 1·18% | 5·64 (3·15–8·12) | 11·29 (9·62–12·95) | 25·14% (6·39–62·30) | 19·43% (4·81–53·48) | |
| First Nations, Inuit, or Metis | 7 | 0·53% | 0·90% | 18·35 (10·95–25·75) | 15·23 (10·44–20·03) | 72·06% (31·88–93·43) | 72·06% (31·88–93·43) | |
| Latin | 20 | 1·51% | 2·09% | 7·42 (5·41–9·43) | 11·99 (10·48–13·50) | 23·89% (10·17–46·52) | 44·21% (24·53–65·90) | |
| Other or mixed race | 39 | 2·94% | 3·55% | 7·65 (6·02–9·27) | 10·56 (9·33–11·78) | 26·46% (14·45–43·40) | 24·09% (12·15–42·12) | |
| White | 1102 | 83·11% | 79·69% | 8·34 (7·98–8·71) | 11·98 (11·72–12·23) | 35·78% (32·79–38·87) | 31·72% (28·87–34·71) | |
| Annual household income before COVID-19, CA$ | ||||||||
| ≤79 999 | 193 | 15·13% | 17·78% | 9·27 (8·38–10·16) | 12·52 (11·89–13·16) | 41·88% (34·44–49·72) | 35·09% (28·04–42·85) | |
| ≥80 000 | 1083 | 84·87% | 82·22% | 8·10 (7·73–8·47) | 11·73 (11·48–11·99) | 33·68% (30·78–36·71) | 30·10% (27·29–33·06) | |
| Impact of COVID-19 on employment | ||||||||
| No | 492 | 40·36% | 39·12% | 7·52 (7·02–8·02) | 11·35 (11·00–11·71) | 30·53% (26·41–34·99) | 26·63% (22·66–31·01) | |
| Yes | 727 | 59·64% | 60·88% | 8·59 (8·12–9·06) | 12·17 (11·84–12·50) | 36·74% (33·00–40·64) | 33·25% (29·66–37·04) | |
| Single parent | ||||||||
| No | 1204 | 92·97% | 92·44% | 8·19 (7·84–8·54) | 11·86 (11·61–12·10) | 34·47% (31·64–37·41) | 30·88% (28·15–33·74) | |
| Yes | 91 | 7·03% | 7·56% | 9·66 (8·33–11·00) | 12·09 (11·14–13·04) | 42·78% (32·50–53·72) | 33·65% (24·16–44·67) | |
| Health-care worker | ||||||||
| No | 990 | 75·86% | 76·32% | 8·52 (8·13–8·90) | 11·94 (11·67–12·21) | 37·07% (33·89–40·37) | 32·34% (29·30–35·54) | |
| Yes | 315 | 24·14% | 23·68% | 7·75 (7·02–8·48) | 11·81 (11·30–12·32) | 30·22% (24·99–36·02) | 29·01% (23·88–34·74) | |
| Children aged <5 years | ||||||||
| No | 1134 | 87·64% | 86·66% | 8·24 (7·87–8·61) | 11·86 (11·61–12·11) | 34·19% (31·32–37·18) | 30·73% (27·94–33·66) | |
| Yes | 160 | 12·36% | 13·34% | 8·62 (7·72–9·52) | 11·93 (11·25–12·62) | 40·75% (32·53–49·53) | 33·10% (25·51–41·69) | |
| Difficulty balancing home schooling with work and other responsibilities | ||||||||
| No | 279 | 21·53% | 21·64% | 5·89 (5·30–6·49) | 10·15 (9·71–10·58) | 19·12% (14·56–24·70) | 15·95% (11·67–21·41) | |
| Yes | 1017 | 78·47% | 78·36% | 8·96 (8·57–9·35) | 12·35 (12·08–12·62) | 39·44% (36·28–42·69) | 35·24% (32·18–38·43) | |
| Difficulty obtaining childcare | ||||||||
| No | 964 | 74·61% | 73·71% | 7·79 (7·40–8·19) | 11·47 (11·19–11·75) | 30·65% (27·62–33·85) | 28·06% (25·10–31·23) | |
| Yes | 328 | 25·39% | 26·29% | 9·65 (8·98–10·31) | 13·04 (12·58–13·50) | 46·56% (40·84–52·38) | 39·86% (34·37–45·61) | |
| Family exposure to COVID-19 | ||||||||
| No | 1210 | 91·25% | 90·69% | 8·24 (7·89–8·60) | 11·88 (11·63–12·13) | 34·67% (31·83–37·63) | 31·32% (28·57–34·20) | |
| Yes | 116 | 8·75% | 9·31% | 8·91 (7·71–10·12) | 12·08 (11·35–12·82) | 40·33% (31·15–50·24) | 32·14% (23·66–41·98) | |
| History of mental illness | ||||||||
| No | 874 | 65·91% | 64·99% | 7·41 (7·02–7·80) | 11·47 (11·19–11·75) | 28·37% (25·19–31·77) | 26·54% (23·49–29·83) | |
| Yes | 452 | 34·09% | 35·01% | 9·99 (9·38–10·59) | 12·70 (12·27–13·12) | 47·94% (43·07–52·84) | 40·44% (35·73–45·34) | |
Sample size values are true (unweighted). All analyses were weighted, adjusting for non-response.
Data missing for 49·00 (3·7%) women.
Data missing for 43·00 (3·2%) women.
At the time of the COVID-19 impact survey, the mean depression score was 8·31 (95% CI 7·97–8·65), and 35·21% (95% CI 32·48–38·04) of women had clinically significant depression symptoms. The mean score for anxiety was 11·90 (11·66–12·13) and 31·39% (28·76–34·15) of women had clinically significant anxiety symptoms. At the COVID-19 pandemic timepoint, a positive association was identified between total depression and anxiety scores (r=0·72, p<0·0001) and 21·83% of mothers reported both clinically significant depressive and anxiety symptoms. Mean depression scores were higher among mothers for whom family income or employment was disrupted (8·59, 8·12–9·06) than mothers for whom family income or employment was not disrupted (7·52, 7·02–8·02). First Nations, Inuit, and Metis mothers had higher mean depression scores (18·35, 10·95–25·75) at the COVID-19 impact survey timepoint than all other mothers. Mothers who had difficulty balancing home schooling with work and other responsibilities had higher mean depression scores (8·96, 95% CI 8·57–9·35) than those who did not (5·89, 5·30–6·49). Mothers who had difficulty obtaining childcare had higher mean depression scores (9·65, 8·98–10·31) than mothers who did not (7·79, 7·40–8·19).
Mothers for whom family income or employment was disrupted had higher mean anxiety scores (12·17, 95% CI 11·84–12·50) than mothers who had no income or employment disruption in the family (11·35, 11·00–11·71). Mean anxiety scores were also higher among mothers who had difficulty balancing home schooling and working (12·35, 12·08–12·62) and difficulty obtaining childcare (13·04, 12·58–13·50). Mothers who had a history of mental illness had higher depressive symptoms scores at the COVID-19 impact survey timepoint (9·99, 9·38–10·59) than mothers who did not have a reported history of mental illness (7·41, 7·02–7·80). Similarly, mothers who reported a history of mental illness had higher anxiety symptoms at the COVID-19 impact survey timepoint (12·70, 12·27–13·12) than mothers without a history of mental illness (11·47, 11·19–11·75). No differences were identified in mental health problems for the remaining sociodemographic variables.
At the COVID-19 impact survey timepoint, mean depression scores (8·31, 95% CI 7·97–8·65) were higher than those at the 3-year timepoint (5·05, 4·85–5·25), 5-year timepoint (5·43, 5·20–5·66), and 8-year timepoint (5·79, 5·55–6·02; table 2 ; appendix p 9). Mean anxiety scores at the COVID-19 impact survey timepoint were substantially higher (11·90, 11·66–12·13) than scores at the 3-year timepoint (9·51, 9·35–9·66), 5-year timepoint (9·49, 9·33–9·65), and 8-year timepoint (10·26, 10·10–10·42). The proportion of individuals who had clinically significant depression and anxiety scores at the COVID-19 survey timepoint was substantially higher than that at all pre-pandemic timepoints (table 3 ; appendix p 10). Compared with the three pre-pandemic timepoints (proportion of women with clinically significant depressive symptoms 14·08–19·01% [95% CI 12·52–20·4]), 35·21% (32·48–38·04) of women had clinically significant symptoms of depression at the COVID-19 timepoint. Similarly, for anxiety, a higher proportion of mothers reported clinically significant anxiety symptoms at the COVID-19 impact survey timepoint (31·39%, 28·76–34·15) than the three pre-pandemic timepoints (proportion of women with clinically significant anxiety symptoms 12·01–18·28% [10·53–20·15). The findings for depression and anxiety symptoms remained the same across timepoints when only women who participated in the COVID-19 impact survey were included (appendix pp 5–6). Having more than one child versus an only child was not associated with differences in depressive or anxiety symptoms (appendix p 8). Sensitivity analyses based on when mothers responded to the survey and associations with balancing multiple roles and difficulties with childcare are presented in the appendix (p 11).
Table 2.
Mean depression and anxiety scores for mothers at study timepoints
| 3-year timepoint*(n=1993) | 5-year timepoint†(n=1991) | 8-year timepoint‡(n=2074) | COVID-19 impact survey timepoint§(n=1333) | |
|---|---|---|---|---|
| Depression score | ||||
| Overall | 5·05 (4·85–5·25) | 5·43 (5·20–5·66) | 5·79 (5·55–6·02) | 8·31 (7·97–8·65) |
| Women with missing data, n (%) | 7·00 (0·4%) | 71·00 (3·6%) | 177·00 (8·5%) | 49·00 (3·7%) |
| Age, years | ||||
| <25 | 6·80 (4·95–8·65) | 8·68 (6·58–10·77) | .. | .. |
| 25–34 | 5·04 (4·77–5·32) | 5·49 (5·07–5·91) | 7·01 (6·25–7·77) | 9·32 (7·76–10·87) |
| 35–44 | 5·01 (4·72–5·31) | 5·34 (5·06–5·61) | 5·57 (5·31–5·82) | 8·23 (7·82–8·64) |
| 45–54 | 4·17 (2·77–5·57) | 5·98 (4·64–7·33) | 5·76 (5·11–6·41) | 8·18 (7·57–8·80) |
| Annual household income before COVID-19, CA$ | ||||
| ≤79 999 | 6·14 (5·68–6·60) | 6·99 (6·35–7·63) | 7·47 (6·83–8·12) | 9·27 (8·38–10·16) |
| ≥80 000 | 4·68 (4·47–4·89) | 5·05 (4·81–5·28) | 5·36 (5·12–5·59) | 8·10 (7·73–8·47) |
| Anxiety score | ||||
| Overall | 9·51 (9·35–9·66) | 9·49 (9·33–9·65) | 10·26 (10·10–10·42) | 11·90 (11·66–12·13) |
| Women with missing data, n (%) | 9·00 (0·5%) | 64·00 (3·2%) | 145·00 (7·0%) | 43·00 (3·2%) |
| Age, years | ||||
| <25 | 9·90 (8·48–11·31) | 11·95 (10·07–13·83) | .. | .. |
| 25–34 | 9·42 (9·21–9·63) | 9·41 (9·12–9·69) | 10·20 (9·71–10·69) | 12·84 (11·76–13·91) |
| 35–44 | 9·63 (9·40–9·86) | 9·49 (9·30–9·69) | 10·30 (10·11–10·49) | 11·79 (11·50–12·07) |
| 45–54 | 8·44 (7·47–9·40) | 9·86 (8·87–10·84) | 10·08 (9·66–10·49) | 11·83 (11·37–12·29) |
| Annual household income before COVID-19, CA$ | ||||
| ≤79 999 | 10·17 (9·83–10·52) | 10·14 (9·74–10·53) | 11·04 (10·61–11·47) | 12·52 (11·89–13·16) |
| ≥80 000 | 9·28 (9·11–9·45) | 9·33 (9·16–9·50) | 10·06 (9·89–10·24) | 11·73 (11·48–11·99) |
Data are mean (95% CI), unless otherwise stated. All analyses were weighted, adjusting for non-response.
Data collected between April, 2012, and October, 2014.
Data collected between April, 2014, and October, 2016.
Data collected between February 2017, and October, 2019.
Data collected between May 20, and July 15, 2020.
Table 3.
Proportion of mothers with clinically significant depression and anxiety symptoms at study timepoints
| 3-year timepoint*(n=1993) | 5-year timepoint†(n=1991) | 8-year timepoint‡(n=2074) | COVID-19 impact survey timepoint§(n=1333) | |
|---|---|---|---|---|
| Depression | ||||
| Overall | 14·08% (12·52–15·81) | 16·58% (14·84–18·47) | 19·01% (17·21–20·94) | 35·21% (32·48–38·04) |
| Women with missing data, n (%) | 7·00 (0·4%) | 71·00 (3·6%) | 177·00 (8·5%) | 49·00 (3·7%) |
| Age, years | ||||
| <25 | 30·52% (14·59–53·03) | 39·19% (9·49–79·84) | .. | .. |
| 25–34 | 14·72% (12·53–17·22) | 17·49% (14·36–21·13) | 27·88% (22·07–34·54) | 44·15% (31·19–57·97) |
| 35–44 | 12·66% (10·56–15·10) | 15·59% (13·56–17·85) | 17·06% (15·10–19·23) | 33·78% (30·60–37·12) |
| 45–54 | 15·52% (5·91–34·95) | 21·78% (13·13–33·91) | 20·65% (16·04–26·17) | 36·13% (30·90–41·70) |
| Annual household income before COVID-19, CA$ | ||||
| ≤79 999 | 21·73% (17·76–26·32) | 26·53% (21·67–32·02) | 28·85% (23·93–34·34) | 41·88% (34·44–49·72) |
| ≥80 000 | 11·48% (9·92–13·24) | 14·19% (12·44–16·13) | 16·47% (14·64–18·47) | 33·68% (30·78–36·71) |
| Anxiety | ||||
| Overall | 12·01% (10·58–13·62) | 12·01% (10·53–13·68) | 18·28% (16·54–20·15) | 31·39% (28·76–34·15) |
| Women with missing data, n (%) | 9·00 (0·5%) | 64·00 (3·2%) | 145·00 (7·0%) | 43·00·00 (3·2%) |
| Age (years) | ||||
| <25 | 15·13% (4·80–38·64) | 19·14% (2·54–68·22) | .. | .. |
| 25–34 | 11·48% (9·58–13·72) | 11·40% (8·85–14·58) | 16·59% (11·93–22·62) | 40·52% (27·97–54·44) |
| 35–44 | 12·71% (10·60–15·17) | 12·19% (10·40–14·24) | 19·06% (17·03–21·27) | 30·08% (27·00–33·35) |
| 45–54 | 4·12% (0·58–24·13) | 13·95% (7·39–24·76) | 15·52% (11·54–20·56) | 31·15% (26·22–36·55) |
| Annual household income before COVID-19, CA$ | ||||
| ≤79 999 | 16·47% (13·06–20·56) | 14·43% (10·78–19·06) | 25·46% (20·81–30·75) | 35·09 (28·04–42·85) |
| ≥80 000 | 10·41% (8·92–12·11) | 11·42% (9·85–13·21) | 16·39% (14·60–18·36) | 30·10 (27·29–33·06) |
Data are proportion of women (95% CI), unless otherwise stated. All analyses were weighted, adjusting for non-response. For depression, a cutoff score of 10 or higher on the 10-item Center for Epidemiological Studies of Depression scale was used to identify clinically significant levels of depressive symptoms; for anxiety, a 6-item short form of the Spielberger State-Trait Anxiety Inventory score 1 SD above the mean at the 8-year timepoint to define clinically significant anxiety at all timepoints (total anxiety score ≥14).
Data collected between April, 2012, and October, 2014.
Data collected between April, 2014, and October, 2016.
Data collected between February 2017, and October, 2019.
Data collected between May 20, and July 15, 2020.
Within-person depression scores increased by a mean of 2·30 points (95% CI 1·95–2·65) and anxiety scores by a mean of 1·04 points (0·65–1·43; table 4 ). In the depression model, after controlling for time trends, significant differences in mean score increases were observed across sociodemographic subgroups. Health-care workers had lower increases in depressive symptoms than non-healthcare workers. Mothers who experienced income disruption during the COVID-19 pandemic had higher increases in depressive symptoms (2·67, 95% CI 2·24–3·10) than those who did not (1·79, 1·34–2·24). Mothers who had difficulty balancing home schooling and working from home had larger increases in depressive symptoms (2·68, 2·31–3·06) than those who did not (0·91, 0·33–1·49). Mothers who had difficulty obtaining childcare during the COVID-19 pandemic had higher increases in depressive symptoms (3·06, 2·50–3·63) than those who did not (1·97, 1·59 to 2·35).
Table 4.
Fixed-effects regression analysis of mean within-person change in depression and anxiety scores associated with the COVID-19 timepoint, by sociodemographic and COVID-19 related variables
|
Unadjusted |
Adjusted* |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean increase in depression score (95% CI) | p value | Mean increase in anxiety score (95% CI) | p value | Mean increase in depression score (95% CI) | p value | Mean increase in anxiety score (95% CI) | p value | ||
| Overall change at COVID-19 timepoint | 2·30 (1·95 to 2·65) | <0·0001 | 1·04 (0·65 to 1·43) | <0·0001 | .. | .. | .. | ||
| Household income before COVID-19 pandemic, CA$ | |||||||||
| >80 000 | 2·38 (2·01 to 2·74) | 0·563 | 1·05 (0·65 to 1·46) | 0·836 | .. | .. | .. | .. | |
| ≤79 999 | 2·15 (1·39 to 2·90) | .. | 1·11 (0·49 to 1·73) | .. | .. | .. | .. | .. | |
| Single parent | |||||||||
| No | 2·40 (1·27 to 3·53) | 0·873 | 0·76 (−0·14 to 1·66) | 0·498 | |||||
| Yes | 2·30 (1·95 to 2·66) | .. | 1·06 (0·67 to 1·46) | .. | .. | .. | .. | .. | |
| Children aged <5 years | |||||||||
| No | 2·26 (1·89 to 2·62) | 0·462 | 1·05 (0·65 to 1·45) | 0·868 | .. | .. | .. | .. | |
| Yes | 2·57 (1·75 to 3·38) | .. | 1·00 (0·32 to 1·68) | .. | .. | .. | .. | .. | |
| Ethnicity | |||||||||
| White | 2·39 (2·03 to 2·76) | 0·145 | 1·19 (0·79 to 1·59) | 0·005 | .. | .. | 2·06 (1·51 to 2·62) | 0·027 | |
| Non-white | 1·89 (1·22 to 2·55) | .. | 0·41 (−0·19 to 1·00) | .. | .. | .. | 1·42 (0·69 to 2·15) | .. | |
| Impact of COVID-19 on income or employment | |||||||||
| No | 1·79 (1·34 to 2·24) | 0·001 | 0·58 (0·12 to 1·04) | <0·0001 | 2·14 (1·39 to 2·89) | <0·0001 | 0·65 (−0·09 to 1·39) | <0·0001 | |
| Yes | 2·67 (2·24 to 3·10) | .. | 1·36 (0·92 to 1·79) | .. | 3·00 (2·29 to 3·71) | .. | 1·42 (0·69 to 2·15) | .. | |
| Health-care worker | |||||||||
| No | 2·49 (2·11 to 2·87) | 0·017 | 1·05 (0·64 to 1·46) | 0·999 | 3·82 (3·15 to 4·48) | 0·005 | .. | .. | |
| Yes | 1·76 (1·19 to 2·33) | .. | 1·05 (0·51 to 1·58) | .. | 3·00 (2·29 to 3·71) | .. | .. | .. | |
| Difficulty balancing home schooling with work and other responsibilities | |||||||||
| No | 0·91 (0·33 to 1·49) | <0·0001 | 0·07 (−0·44 to 0·59) | <0·0001 | 1·43 (0·48 to 2·39) | <0·0001 | 0·30 (−0·61 to 1·21) | 0·052 | |
| Yes | 2·68 (2·31 to 3·06) | .. | 1·30 (0·89 to 1·71) | .. | 3·00 (2·29 to 3·71) | .. | 1·39 (0·61 to 2·18) | .. | |
| Difficulty obtaining childcare | |||||||||
| No | 1·97 (1·59 to 2·35) | <0·0001 | 0·84 (0·43 to 1·25) | 0·001 | 2·09 (1·38 to 2·81) | <0·0001 | 0·94 (0·26 to 1·62) | <0·0001 | |
| Yes | 3·06 (2·50 to 3·63) | .. | 1·62 (1·11 to 2·14) | .. | 3·00 (2·29 to 3·71) | .. | 1·42 (0·69 to 2·15) | .. | |
| History of mental illness† | |||||||||
| No | 2·28 (1·89 to 2·68) | 0·847 | 1·05 (0·64 to 1·46) | 0·922 | .. | .. | .. | .. | |
| Yes | 2·34 (1·83 to 2·84) | .. | 1·03 (0·53 to 1·53) | .. | .. | .. | .. | .. | |
Data are weighted within-person change, unless stated otherwise. Fixed-effect analyses show changes associated with the COVID-19 pandemic timepoint, compared with previous trends over time.
Adjusted for all variables that had p<0·05 level in the unadjusted analysis. The adjusted depression model included the following factors: impact of COVID-19 on income or employment, healthcare worker, difficulty balancing home schooling and work, and difficulty obtaining childcare. The p value for the COVID change coefficient indicates that it is statistically different from zero. The p value for the subgroup analyses indicate if subgroups are statistically different from one another.
History of mental illness was collected in pregnancy from 2008 to 2011.
In the anxiety model, white women had higher increases in anxiety symptoms (1·19, 95% CI 0·79 to 1·59) than non-white women (0·41, −0·19 to 1·00; table 4). Mothers who experienced income disruption during the COVID-19 pandemic had larger increases in anxiety symptom scores (1·36, 0·92 to 1·79) than those who did not (0·58, 0·12 to 1·04). Mothers who had difficulty balancing child schoolwork and working from home had larger increases in anxiety symptom scores (1·30, 0·89 to 1·71) than those who did not (0·07, −0·44 to 0·59). Mothers who had difficulty obtaining childcare during the COVID-19 pandemic had larger increases in anxiety symptoms (1·62, 1·11 to 2·14) than those who did not (0·84, 0·43 to 1·25). The pattern of results and differences between groups largely remained the same in the adjusted multivariable models controlling for significant factors (table 4). Regression estimates are presented in the appendix (p 7).
Discussion
This study builds on existing cross-sectional evidence by demonstrating an increase in maternal depressive and anxiety symptoms in the early months of the COVID-19 pandemic (May–July, 2020), when compared with data from three pre-pandemic timepoints collected in the previous 10 years. Mean depression scores were 2·30 points (95% CI 1·95–2·65) higher and mean anxiety scores were 1·04 points (0·65–1·43) higher than that expected considering previous time trends. Individuals who had disruptions in employment or income had a mean increase in depression score of 2·67 points compared with a mean increase of 1·79 points for those without employment or income disruption, and individuals with income or employment disruption had a mean increase in anxiety score of 1·36 points compared with a mean increase of 0·58 points for those without. White women had a larger increase in mean anxiety scores than non-white mothers. Additionally, balancing home schooling with working from home and other responsibilities, and difficulty obtaining childcare were associated with increases in depression and anxiety. Larger point increases in depression scores than anxiety scores, which have also been found in a previous study,23 might be associated with the types of symptoms that manifest from prolonged stress (ie, sleep disruption, decreased mood, decreased physical activity) rather than acute anxiety symptoms.
We found that mothers who reported family loss of income or employment as a consequence of the economic shift at the start of the COVID-19 pandemic had greater increases in mental health symptoms than those who did not. In this study, more than 50% of families experienced some form of disruption to their income or employment status due to the COVID-19 pandemic. Such an observation is important because it indicates that families are likely to be experiencing financial strain, which is associated with psychological distress,24 and provides a targeted opportunity for government intervention (eg, workplace protection or financial support).
A unique finding from this cohort of mothers is that parenting-specific factors associated with the pandemic, including difficulty balancing multiple parental roles and obtaining childcare during the COVID-19 pandemic, emerged as important modifiers of increases in depressive and anxiety symptoms. The burden of caring for children in addition to balancing other responsibilities during the COVID-19 pandemic has been strongly associated with depressive and anxious symptoms in cross-sectional studies.25 In the early stages of the pandemic, mothers in dual-income households worked 5 hours less per week on average than their male counterparts,26 and mothers reported they were nearly five times more likely to devote their time to home schooling than their partners.27 Although some research has suggested that the gap in gender-based household roles has narrowed during the COVID-19 pandemic,28 other research suggests that mothers continue to be disproportionately affected by inequalities in perceived job performance and hours of sleep achieved.29
At the COVID-19 impact survey timepoint, a history of mental illness was associated with higher depression and anxiety symptoms during the COVID-19 pandemic. However, no differences regarding within-person change in depressive or anxiety symptoms during the COVID-19 pandemic were identified for mothers with a reported history of mental illness versus mothers without a history of mental illness. This finding suggests that after controlling for individual differences in this sample, increases in depression and anxiety symptoms during the COVID-19 pandemic occurred universally, regardless of previous mental health history.
At the COVID-19 impact survey timepoint, we found that being a health-care worker was protective against increases in depressive symptoms, but not anxiety symptoms. This finding is contrary to findings from a meta-analysis, which suggested high levels of depressive symptoms in health-care workers during the COVID-19 pandemic, highlighting the importance of assessing these constructs in samples with pre-pandemic baseline estimates, and across specific populations of health-care workers.30 Individuals who were health-care workers in our sample might have engaged in work outside the home and had more in-person social interactions with colleagues that might have mitigated decreases in mood. Sampling bias could also have contributed to this finding, whereby health-care workers who were coping well might have been more likely to respond to the survey than those who were not.
Our study had some limitations. First, women who participated in the COVID-19 impact survey were generally older, had a higher level of educational attainment, and higher income than women recruited to the longitudinal All Our Families study, decreasing the generalisability of our findings to less advantaged populations. Women included in the current study also had a target biological child aged 9–11 years, reducing the generalisability of findings to parents of younger children or adoptive parents. Second, the study was underpowered to examine differences among specific ethnic groups. Third, the measurement tools in the current study are common screening tools used in primary care that assess symptomatology not diagnoses of depression or anxiety disorders. Studies that include clinical interviews are needed to demonstrate increases in diagnostic classification. Additionally, no established standardised cutoff score exists for the STAI-SF, which was used to measure anxiety in the current study. Thus, additional caution should be taken when interpreting the anxiety findings. Fourth, most associated variables in the fixed-effects analysis were collected at the time of the COVID impact survey, raising the issue of shared-method variance, and thus we cannot examine directional associations or infer causal associations from the data. The examination of income and job loss in the current study was based on single-item questions. Future research would benefit from obtaining more detailed information on the financial impact of the pandemic on families, and understanding how working full-time versus part-time might be associated with challenges with balancing multiple roles and childcare.
An important topic for future research is to identify the mechanisms, specifically how and for whom, by which mental health problems increased during the COVID-19 pandemic, and to determine the persistence of increased mental distress. Some research has suggested a narrowing of gender-based parenting roles during the COVID-19 pandemic, highlighting the need to re-examine the mental distress of mothers as the COVID-19 pandemic progresses.28 Future work should also examine social support as a protective factor, and paternal mental health during the COVID-19 pandemic separately, and in comparison with maternal mental health.
Mothers in this study reported increases in depressive and anxiety symptoms during the COVID-19 pandemic when compared with pre-pandemic estimates. These changes were primarily driven by the financial impact of the pandemic and challenges balancing child schoolwork and working from home and lack of childcare. Support efforts from governments that help to stabilise financial security, increased job opportunities, and availability of childcare will be crucial to support maternal mental health, and its sequelae, child wellbeing.
Data sharing
The All Our Families meta-data are available online. Investigators can submit a proposal that has been approved by an independent ethics and scientific review committee to obtain de-identified individual participant data. Data requestors will need to sign confidentiality and access agreements. The study protocol for the current study is available upon request to stough@ucalgary.ca. Data are also available from the principal investigator of the All Our Families study, Suzanne Tough, through University of Calgary processes.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
The All Our Families study is funded by an Alberta Innovates Health Solutions Interdisciplinary Team (grant 200700595) and the Alberta Children's Hospital Foundation. Funding for the COVID-19 impact survey data collection was provided by the Canadian Institutes of Health Research and Alberta Innovates, through the COVID-19 Rapid Research Response Operating Grant. We thank the All Our Families research team and the women who participated in our study.
Contributors
NR, SM, and ER accessed and verified the underlying data and take responsibility for the integrity of the data and accuracy of data analysis. NR and SM conceptualised the study. SMc and ST maintained data over time and linked data across data collection waves over time. NR and EH did the formal analyses. EH, SMc, SE, and ST acquired the funding for this study. EH, SMc, and ST led the survey methodology. ST and SMc are the project administrators. SM provided supervision. NR, EH, and SM wrote the original manuscript draft. All authors contributed to reviewing and editing the manuscript. All authors had full access to all the data and had final responsibility for the decision to submit for publication.
Supplementary Material
References
- 1.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daly M, Sutin AR, Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol Med. 2020 doi: 10.1017/S0033291720004432. published online Nov 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pierce M, Abel KM, Muwonge J, Jr, et al. Prevalence of parental mental illness and association with socioeconomic adversity among children in Sweden between 2006 and 2016: a population-based cohort study. Lancet Public Health. 2020;5:e583–e591. doi: 10.1016/S2468-2667(20)30202-4. [DOI] [PubMed] [Google Scholar]
- 6.Cameron EE, Joyce KM, Delaquis CP, Reynolds K, Protudjer JLP, Roos LE. Maternal psychological distress & mental health service use during the COVID-19 pandemic. J Affect Disord. 2020;276:765–774. doi: 10.1016/j.jad.2020.07.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Racine N, Korczak DJ, Madigan S. Evidence suggests children are being left behind in COVID-19 mental health research. Eur Child Adolesc Psychiatry. 2020 doi: 10.1007/s00787-020-01672-8. published online Nov 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amsalem D, Dixon L, Neria Y. The coronavirus disease 2020 (COVID-19) outbreak and mental health. JAMA Psychiatry. 2021;78:9–10. doi: 10.1001/jamapsychiatry.2020.1730. [DOI] [PubMed] [Google Scholar]
- 9.Pierce M, McManus S, Jessop C, et al. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020;7:567–568. doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rogers A, Obst S, Teague SJ, et al. Association between maternal perinatal depression and anxiety and child and adolescent development: a meta-analysis. JAMA Pediatr. 2020;174:1082–1092. doi: 10.1001/jamapediatrics.2020.2910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tough SC, McDonald SW, Collisson BA, et al. Cohort profile: the All Our Babies pregnancy cohort (AOB) Int J Epidemiol. 2017;46:1389–1390k. doi: 10.1093/ije/dyw363. [DOI] [PubMed] [Google Scholar]
- 13.McDonald SW, Lyon A, Benzies K, et al. The All Our Babies pregnancy cohort: design, methods, and participant characteristics. BMC Pregnancy Childbirth. 2015;13:1–12. doi: 10.1186/1471-2393-13-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 15.Björgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20:429–436. doi: 10.1177/1073191113481998. [DOI] [PubMed] [Google Scholar]
- 16.Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI) Br J Clin Psychol. 1992;31:301–306. doi: 10.1111/j.2044-8260.1992.tb00997.x. [DOI] [PubMed] [Google Scholar]
- 17.Tluczek A, Henriques JB, Brown RL. Support for the reliability and validity of a six-item state anxiety scale derived from the State-Trait Anxiety Inventory. J Nurs Meas. 2009;17:19–28. doi: 10.1891/1061-3749.17.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bayrampour H, McDonald S, Fung T, Tough S. Reliability and validity of three shortened versions of the State Anxiety Inventory scale during the perinatal period. J Psychosom Obstet Gynaecol. 2014;35:101–107. doi: 10.3109/0167482X.2014.950218. [DOI] [PubMed] [Google Scholar]
- 19.Hetherington E, McDonald S, Wu M, Tough S. Risk and protective factors for mental health and community cohesion after the 2013 Calgary flood. Disaster Med Public Health Prep. 2018;12:470–477. doi: 10.1017/dmp.2017.91. [DOI] [PubMed] [Google Scholar]
- 20.Hetherington E, Racine N, Madigan S, McDonald S, Tough S. Relative contribution of maternal adverse childhood experiences to understanding children's externalizing and internalizing behaviours at age 5: findings from the All Our Families cohort. CMAJ Open. 2020;8:e352–e359. doi: 10.9778/cmajo.20190149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gunasekara FI, Richardson K, Carter K, Blakely T. Fixed effects analysis of repeated measures data. Int J Epidemiol. 2014;43:264–269. doi: 10.1093/ije/dyt221. [DOI] [PubMed] [Google Scholar]
- 22.Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2013;22:278–295. doi: 10.1177/0962280210395740. [DOI] [PubMed] [Google Scholar]
- 23.Hawes MT, Szenczy AK, Klein DN, Hajcak G, Nelson BD. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med. 2021 doi: 10.1017/S0033291720005358. published online Jan 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olesen SC, Butterworth P, Leach LS, Kelaher M, Pirkis J. Mental health affects future employment as job loss affects mental health: findings from a longitudinal population study. BMC Psychiatry. 2013;13:144. doi: 10.1186/1471-244X-13-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Russell BS, Hutchison M, Tambling R, Tomkunas AJ, Horton AL. Initial challenges of caregiving during COVID-19: caregiver burden, mental health, and the parent-child relationship. Child Psychiatry Hum Dev. 2020;51:671–682. doi: 10.1007/s10578-020-01037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Collins C, Landivar LC, Ruppanner L, Scarborough WJ. COVID-19 and the gender gap in work hours. Gend Work Organ. 2021;28:101–112. doi: 10.1111/gwao.12506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anders J, Macmillan L, Sturgis P, Wyness G. Homeschooling during lockdown deepens inequality. June 5, 2020. https://blogs.lse.ac.uk/covid19/2020/06/05/homeschooling-during-lockdown-will-deepen-inequality/
- 28.Craig L, Churchill B. Dual-earner parent couples' work and care during COVID-19. Gend Work Organ. 2020;28:66–79. doi: 10.1111/gwao.12497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shockley KM, Clark MA, Dodd H, King EB. Work-family strategies during COVID-19: examining gender dynamics among dual-earner couples with young children. J Appl Psychol. 2021;106:15–28. doi: 10.1037/apl0000857. [DOI] [PubMed] [Google Scholar]
- 30.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The All Our Families meta-data are available online. Investigators can submit a proposal that has been approved by an independent ethics and scientific review committee to obtain de-identified individual participant data. Data requestors will need to sign confidentiality and access agreements. The study protocol for the current study is available upon request to stough@ucalgary.ca. Data are also available from the principal investigator of the All Our Families study, Suzanne Tough, through University of Calgary processes.