Abstract
OBJECTIVES:
To describe relationships between compromised integrity (CI), burnout, and intent-to-leave (ITL) practice in critical care (CC) and noncritical care (non-CC) nurses and physicians.
DESIGN:
CC nurses (RNs) and physicians (MDs) from the American Medical Association Coping with COVID survey were matched by gender, race, years in practice, and role with non-CC clinicians to determine likelihood of ITL in relation to burnout and CI.
SETTING:
U.S. Healthcare organizations; July—December 2020.
SUBJECTS:
One hundred sixty-five CC RNs and 148 CC MDs (n = 313) matched with 165 non-CC RNs and 148 non-CC MDs from 83 healthcare organizations.
MEASUREMENTS AND MAIN RESULTS:
Burnout was measured with a single, validated question that mainly reflects emotional exhaustion (EE), and CI was determined by asking if respondents worried about doing things that compromised their integrity moderately or to a great extent. ITL included those moderately, likely, or definitely, intending to leave. Burnout correlated strongly with CI (tetrachoric r = 0.704 [0.606–0.803]; P < 0.001). Of 626 subjects, 59% experienced burnout, 24% CI, and 33% ITL. CC RNs experienced burnout more often (76%) than non-CC RNs (62%; P < 0.01) and CC MDs (51%; P < 0.001). CI was more frequent in CC RNs (44%) than non-CC RNs (23%) and CC MDs (16%; P < 0.001). In multivariate regressions, CC clinicians experiencing burnout had 50% greater odds of ITL than non-CC clinicians experiencing burnout; odds of ITL were substantially higher (odds ratio, 2.8–3.2) in those with CI regardless of location or burnout. In the ICU, those feeling valued by their organization had one-third the odds of ITL.
CONCLUSIONS:
Burnout (EE) is high (>50%) among CC RNs and MDs, which may result in losses of CC clinicians while demand rises. Preventing CI independent of burnout may reduce turnover in all settings and especially in ICUs. Feeling valued may promote staff retention.
Keywords: burnout, moral distress, retention, turnover
Burnout, composed of emotional exhaustion, depersonalization, and reduced personal accomplishment, has been a well-known driver of intention to reduce clinical time and to leave practice for nurses and physicians. Using the Maslach Burnout Inventory, burnout in U.S. critical care (CC) professionals ranges from 28% to 47% (1). Addressing burnout in the ICU has been identified as a major imperative by Critical Care Societies (2, 3). Burnout is associated with intent to leave (ITL) the job for nurses and physicians and is associated with two times the likelihood of leaving an organization (4–12). Another coping with COVID survey found that 50% of physicians, and 60% of nurses experienced burnout. Twenty-four percent of physicians and 40% of nurses intended to leave their position in the next 2 years (12). The CC setting has generally been associated with high levels of burnout, and risk factors such as workload and dealing with end-of-life issues are described (13). These issues have only become more frequent with COVID-19.
Moral distress occurs when a professional has an ethical construct of a correct action but is constrained from taking that action by external factors. Common examples of moral distress include providing nonbeneficial care to a patient because the family insists on full aggressive measures to a patient who is most likely to die regardless of this treatment, compromising patient care due to lack of resources, and lacking administrative action or support for a problem that compromises patient care and experiencing distress when no one will make the decision to withdraw support (14). These situations leave clinicians unable to follow their ethical judgment that leads to painful emotional disequilibrium. Moral distress, if repetitive and unaddressed, can progress to moral injury, which is a chronic sense of betrayal and loss of trust.
Measuring moral distress in healthcare workers is typically performed using the Measure of Moral Distress for Healthcare Professionals (14). There are other inventories such as the Moral Injury Events Scale (15). These inventories are lengthy assessments, and a short survey of moral distress has not been validated. Moral distress is more prevalent in nurses than physicians and in women than men (16–19). Longer years of service and being partnered at home are inversely associated with moral distress (19). In a 2017 Brazilian study of ICU and step-down clinicians, moral distress was associated with 2.4 higher odds of burnout (16). One type of moral distress, providing nonbeneficial care, has been associated with higher ITL the job (20). Fifteen percent of nurses have reported leaving a job due to moral distress (21). In a more recent, larger study of Canadian physicians, one-third of respondents had considered leaving or had left a position due to moral distress (22). In this study, burnout was associated with moral distress and ITL but no modifiable factors such as practice type and workload were identified. The COVID-19 pandemic has been associated with both high levels of burnout and moral distress. In a 3-month cohort study during the COVID-19 pandemic, moral distress was stable; having a supportive workplace was associated with less moral distress (21).
The persistent COVID-19 pandemic offers more unique issues in compromised integrity (CI) for healthcare workers. Record numbers of deaths combined with protracted ICU stays are a major stressor for the entire healthcare team. This stress is amplified by the fact that vaccine hesitancy has continued to drive these largely preventable deaths. The COVID-19 virus itself has become politicized, and interactions with patients and families are navigating the space of science versus politics. Patients and their families often request medications or treatments that are not indicated for COVID treatment, and this can lead to conflict between the clinicians and patients. Resources are extremely short; ICU beds for time sensitive care such as trauma, myocardial infarction, sepsis, and stroke are delayed by long periods of boarding in the emergency department or at ready access hospitals due to lack of available ICU beds in referral centers. This is especially harmful to the care team when there are ICU patients on full support, and the team knows their care is nonbeneficial, but there is no expeditious way forward to reallocate care to those who may benefit most.
What is less well known is how moral injury or having a sense of compromising one’s integrity may relate to stress, burnout, and ITL the practice, especially in high-intensity settings such as CC units during the COVID era. Furthermore, there is little knowledge of what contributes to moral injury or integrity compromise or what factors might mitigate or reduce it. We sought to determine prevalence of CI in CC settings during the COVID-19 pandemic, which role type (physicians or nurses) seems to experience the most CI, what factors contribute to, and which aspects of organizational structure or culture might reduce the sense of CI. To answer these questions, we used data from the Coping with COVID national survey through the American Medical Association (AMA) (23).
MATERIALS AND METHODS
The Coping with COVID study has been described in detail elsewhere in previous studies (23). A brief, U.S. national survey was administered by multiple healthcare organizations beginning in April 2020–December 2020. Healthcare workers from nearly 100 organizations were surveyed. Many of these institutions were invited after having worked with the AMA on work-life projects, other institutions learned of the study by word of mouth, and participated. Enrollment was on a rolling basis, and there was a second survey after the first 10,000 respondents. This study includes responses from 20,974 respondents collected between July 2020 and December 2020. Responses were compiled at a databank at Forward Health Group, a healthcare data management group in Madison, WI. The Hennepin Healthcare Institutional Review Board (IRB) deemed this study a quality improvement/program evaluation project that did not need IRB review as it did not fall under human subjects research. The brief Coping with COVID survey included demographics (race/ethnicity, gender, years in practice, outpatient versus inpatient practice, and work role), as well as questions about overall stress, fear of infection and transmission, anxiety or depressive symptoms, work overload, sense of meaning and purpose, feeling valued by the organization, and burnout. Burnout was assessed by the Mini Z single-item burnout measure, which has been validated predominantly against the emotional exhaustion subscale of the Maslach Burnout Inventory (24–27). Workers were also asked about their “likelihood of leaving your practice in the next 2 years.” Responses of “none,” “slight,” “moderately,” “likely,” and “definitely” were options. Responses of “moderately, likely, and definitely” were counted in ITL. Finally, although we did not directly measure moral injury, there was a question about the respondent’s perception of having “worry that I have had to do things at work that compromise (my) integrity.” Response options were “not at all,” “somewhat,” “moderately,” and “to a great extent.” If respondents chose “moderately” or “to a great extent,” they were considered to have CI at work.
Descriptive statistics were run on all variables, and missing data were analyzed for being missing at random and missing completely at random. Odds ratios (ORs) determined if respondents suffering burnout or CI were likely to leave. Tetrachoric correlations were calculated between burnout and CI as binary variables (burned out vs not burned out and compromised vs not compromised). Structural logit multivariable modeling was performed to describe both direct and indirect effects for burnout and CI on ITL and to determine contributors to and mitigators of burnout, integrity compromise, and ITL. These models, in this cross-sectional study, did assess the role of mediating variables. Although the cross-sectional design poses some restrictions on drawing causal conclusion (28), the use of cross-sectional data based on well-founded theoretical foundations for the causal direction, as well as prior findings, allows cross-sectional mediation models to reveal potential causal mechanisms (29, 30).
RESULTS
Table 1 contains data from 313 ICU clinicians (148 physicians and 165 nurses) and a group of 313 non-ICU clinicians (148 physicians and 165 nurses) matched for gender, race, years in practice, and proportional roles. In the portrayal of findings, burnout refers predominantly to emotional exhaustion. The correlation of burnout and integrity compromise treated as binary variables with normal distributions was 0.704 (0.606–0.803); P < 0.001. Table 1 includes demographics of ICU versus non-ICU clinicians by gender (female vs male), race/persons of color (such as Black, Latinx, Asian, Native American vs other), and years in practice by role. It also shows prevalence of burnout, CI, and ITL by role and practice location.
TABLE 1.
Demographics and Outcomes of Coping With COVID ICU Physicians and Nurses Versus Matched Non-ICU Sample
| Variables | Noncritical Care | Critical Care | Totals | ||
|---|---|---|---|---|---|
| Physicians (n = 148) | Nurses (n = 165) | Physicians (n = 148) | Nurse (n = 165) | ||
| Intent to leave | 20.95% | 33.33% | 23.65% | 52.73% | 33.23% |
| Burned out | 43.24% | 62.42% | 51.35% | 75.76% | 58.79% |
| Integrity | 12.16% | 20.03% | 16.22% | 43.64% | 24.28% |
| Stress | 34.46% | 36.36% | 43.24% | 47.88% | 40.58% |
| Fear | 58.11% | 66.67% | 68.24% | 76.36% | 67.57% |
| Anxiety | 22.30% | 39.39% | 31.08% | 61.21% | 39.14% |
| Workload | 30.41% | 53.33% | 52.70% | 72.12% | 52.72% |
| Purpose | 35.14% | 33.33% | 50.68% | 29.09% | 36.74% |
| Valued | 54.73% | 30.91% | 43.92% | 18.79% | 36.42% |
| Matched variables | |||||
| Years in clinic | |||||
| 1–5 yr | 30.41% | 25.45% | 23.65% | 33.74% | |
| 6–10 yr | 27.03% | 31.52% | 22.30% | 29.45% | |
| 11–15 yr | 18.92% | 24.85% | 24.32% | 13.50% | |
| 16–20 yr | 3.38% | 6.06% | 14.19% | 9.20% | |
| More than 20 yr | 20.27% | 12.12% | 15.54% | 14.11% | |
| People of color/race | 22.97% | 1.21% | 30.25% | 1.40% | |
| Gender (female) | 23.65% | 92.12% | 31.78% | 90.41% | |
Overall, 59% of all clinicians were burned out, 24% described frequently compromising their integrity, and 33% intended to leave within 2 years. High stress was found in 41%, fear of exposure or transmission in 68%, anxiety or depressive symptoms in 39%, and work overload in 53%. Only 36% of clinicians felt valued by their organization; feeling valued was particularly infrequent in CC RNs (18.8%).
Burnout/Emotional Exhaustion and Integrity Compromise
Of CC clinicians, 76% of nurses and 51% of physicians were experiencing burnout/emotional exhaustion; 44% of CC nurses and 16% of CC physicians often compromised their integrity (Table 2). Of CC nurses, 53% intended to leave in 2 years, as did 24% of CC physicians. These values were somewhat lower in noncritical care (non-CC) clinicians.
TABLE 2.
Differences Between Burnout, Compromised Integrity, and Intent-to-Leave Practice in Critical Care and Noncritical Care Samples
| Physicians | Critical Care (n = 148) | Noncritical Care (n = 148) | P |
|---|---|---|---|
| Burnout | 51% (n = 76) | 43% (n = 64) | 0.16 |
| Compromised integrity | 16% (n = 24) | 12% (n = 18) | 0.32 |
| Intent-to-leave practice | 24% (n = 35) | 21% (n = 31) | 0.57 |
| Nurses | Critical Care (n = 165) | Noncritical Care (n = 165) | P |
| Burnout | 76% (n = 125) | 62% (n = 103) | 0.009 |
| Compromised integrity | 44% (n = 72) | 23% (n = 38) | < 0.001 |
| Intent-to-leave practice | 53% (n = 87) | 33% (n = 55) | < 0.001 |
| Outcomes | Contrast | Contrast | |
| Burnout (MD vs nurse) | Nurse > MD; P < 0.001 | Nurse > MD; P = <0.001 | |
| Compromised integrity (MD vs nurse) | Nurse > MD; P < 0.001 | Nurse > MD; P = 0.012 | |
| Intent-to-leave practice (MD vs nurse) | Nurse > MD; P < 0.001 | Nurse > MD; P = 0.014 |
Associations With Intent to Leave (Direct Effects)
Supplement 1 (http://links.lww.com/CCX/A903) demonstrates that burnout/emotional exhaustion and CI were both associated with ITL the job. In particular, burned out non-CC clinicians had 2.00 times the odds of intending to leave versus those not burned out (95% CI, 1.00–4.00; P < 0.05). Odds of intending to leave were higher in burned out CC MDs and RNs versus those without burnout (OR, 4.11; CI, 1.96–8.65; P < 0.001). Odds of intending to leave if burned out were 50% higher in CC versus non-CC clinicians. Likewise, non-CC clinicians who had compromised their integrity had higher odds of intending to leave (OR, 3.20) versus non-CC clinicians who had not compromised their integrity (CI, 1.63–6.28; P = 0.001). These figures were comparable in the ICUs, where clinicians who had compromised their integrity had 2.88 times the odds of intending to leave (CI, 1.60–5.19; P < 0.001), with a slightly lower relative odds of intending to leave versus non-ICU clinicians with integrity compromise (11%). ITL was less in those CC clinicians feeling valued by their organization (OR, 0.33; CI, 0.16–0.66; P < 0.01).
Work Conditions Associated With Burnout/Emotional Exhaustion and Integrity Compromise
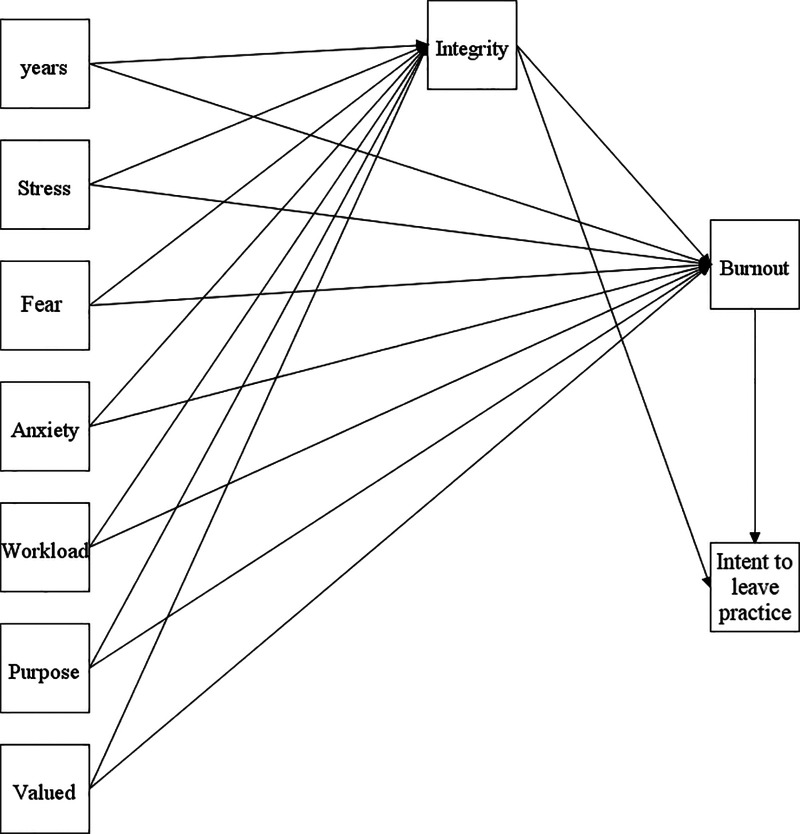
Supplement 1 (http://links.lww.com/CCX/A903) illustrates that burnout inside and outside the ICU was related to several work condition variables, including a single-item stress measure, anxiety/depression, and workload (ORs ranging from 2.67–6.01; P < 0.01). Integrity compromise was related to anxiety/depression and workload in CC clinicians (ORs ranging from 2.37–3.63; P < 0.01). Burnout was lower in those feeling valued by their organization, mainly in non-CC clinicians (OR, 0.30; P ≤ 0.001). Non-ICU clinicians who felt valued were significantly less likely to endorse having compromised their integrity (OR, 0.29; P = 0.002). Feeling valued was protective of burnout and CI predominantly in non-CC clinicians (ORs, 0.30 and 0.29, respectively; P < 0.01). Figure 1 illustrates these relationships in CC clinicians.
Figure 1.
Pathways to burnout/emotional exhaustion, integrity compromise, and intent to leave in critical care clinicians (structural models and indirect effects).
Indirect effects associated with ITL in CC clinicians are presented in Table 3. The effects of stress (OR, 1.47; P < 0.05) and anxiety/depression (OR, 2.00; P < 0.01) on ITL were mediated by burnout; thus, the pathway from stress and anxiety/depression to ITL appears to go through burnout. The relationship of workload (OR, 1.54; P < 0.05) to ITL was explained in part by increases in integrity compromise. No double mediation was discovered, that is, there were no variables that were explained by both burnout and integrity compromise.
TABLE 3.
Intent to Leave Indirect Effects for Critical Care Clinicians
| Indirect Effects | OR (95% CI) | P |
|---|---|---|
| Single mediation | ||
| Stress → burnout → intent to leave practice | 1.47 (1.01–2.14) | 0.041 |
| Fear → burnout → intent to leave practice | 1.30 (0.94–1.81) | 0.109 |
| Anxiety → burnout → intent to leave practice | 2.00 (1.24–3.22) | 0.004 |
| Work load → burnout → intent to leave practice | 1.41 (0.96–2.08) | 0.074 |
| Purpose → burnout → intent to leave practice | 0.79 (0.59–1.07) | 0.133 |
| Valued → burnout → intent to leave practice | 0.83 (0.59–1.16) | 0.295 |
| Stress → integrity → intent to leave practice | 1.04 (0.84–1.28) | 0.665 |
| Fear → integrity → intent to leave practice | 1.12 (0.862–1.44) | 0.382 |
| Anxiety → integrity → intent to leave practice | 1.34 (0.99–1.81) | 0.051 |
| Work load → integrity → intent to leave practice | 1.54 (1.04–2.29) | 0.031 |
| Purpose → integrity → intent to leave practice | 0.93 (0.74–1.16) | 0.530 |
| Valued → integrity → intent to leave practice | 0.80 (0.60–1.08) | 0.156 |
| Double mediation | ||
| Stress → integrity → burnout → intent to leave practice | 1.01 (0.94–1.09) | 0.669 |
| Fear → integrity → burnout → intent to leave practice | 1.04 (0.94–1.14) | 0.401 |
| Anxiety → integrity → burnout → intent to leave practice | 1.11 (0.97–1.27) | 0.109 |
| Work load → integrity → burnout → intent to leave practice | 1.16 (0.98–1.38) | 0.070 |
| Purpose → integrity → burnout → intent to leave practice | 0.97 (0.89–1.05) | 0.542 |
| Valued → integrity → burnout → intent to leave practice | 0.92 (0.82–1.03) | 0.191 |
OR = odds ratio.
DISCUSSION
In this study of 313 CC nurses and physicians during the first year of COVID, compared with a matched sample of non-CC clinicians, we found burnout/emotional exhaustion was high in both groups but higher in the ICU sample, and particularly high in CC nurses (76%). Likewise, a sense of CI was prevalent and higher in ICU clinicians (e.g. % in CC nurses compared with 23% of non-CC nurses; P < 0.001). Clinicians experiencing burnout had a two- to four-fold higher odds of intending to leave their jobs. Those working in ICUs were 50% more likely to intend to leave on account of burnout compared with those working in non-ICU settings. Those sensing they had compromised their integrity were approximately three times more likely to intend to leave versus those not having compromised their integrity. This was comparable in CC and non-CC samples. A sense of integrity compromise was an independent predictor of ITL in the ICU (OR, 2.88; P < 0.001). A critical factor in the ICU that appeared to protect against intending to leave was feeling-valued by the organization (OR, 0.33 of ITL if feeling valued; P < 0.01). Risk factors for intending to leave practice in CC clinicians included stress, anxiety/depression, and workload, as well as burnout and a sense of having compromised one’s integrity. These findings suggest that an ICU environment is not only stressful but is also home to many who feel they must compromise their integrity in their work. Both burnout and CI interact with potentially remediable workplace factors, such as mental health symptoms and workload, to promote leaving the practice. Better understanding of what leads to CI and how to reduce it may be beneficial to the improvement of work life and reduction of turnover in CC staff.
There is strong theoretical support for these findings. A meta-analysis of 91 studies (87 cross-sectional) of nurses suggests that job characteristics such as workload, low work control, and high psychologic demands are related to burnout (31). Several studies support relationships between burnout and ITL; ORs vary from 2 to 5 (4–8). In terms of the relationship between ITL and number who actually turnover, this can vary from 25% to 40% (4, 5, 7). There are ongoing studies aimed at understanding which other factors drive both ITL and actually leaving a job.
The direct relationship we found between integrity compromise and ITL is novel and bears further exploration as a potential mediator of actual turnover. Our work also adds new variables, such as work-related anxiety/depression symptoms as a potential component of burnout and leaving, confirms the contribution of workload, and reinforces new mitigators such as a sense of feeling valued. Our structural models provide a new conceptual framework to explore in future studies.
Dodek et al (22) recently identified moderate scores of burnout and moral distress in a large survey of Canadian CC physicians. They also showed moderately high scores for satisfaction and resilience, but no modifiable factors associated with their wellness measures. They concluded that further studies are needed to identify effective interventions to reduce moral distress and burnout (22). Our work expands the findings of that study into ICU nurses, the group with the highest burnout of our studied groups. Our study also updates Dodek et al’s (22) data with the current status during the pandemic and offers insight into potentially modifiable workplace factors, including workload, mental health support, and feeling valued by one’s organization. Intervention trials with these variables would be valuable and indeed can be seen as urgently needed.
The data we provide raise troubling compromises that may be perceived as necessary for clinicians, especially in ICUs, such as duty to care for patients versus attending to one’s own wellbeing. Prior literature resonates with these findings, showing high prevalence of challenges to maintaining well-being during the pandemic, especially in ICU clinicians (32, 33). The current study raises hope for improvement: several variables that could be addressed by workflow redesign, and workload monitoring may be able to reduce ITL and burnout. In addition, addressing the potential antecedents of CI (such as by maintaining manageable workloads, ensuring sufficient resources, and providing support for clinicians faced with ethical dilemmas) may reduce burnout and intention to leave one’s current job and possibly also intentions to leave one’s profession. Finally, efforts that convey a sense of being valued by one’s organization can be expected to reduce burnout, decrease experiences of CI, and improve retention among nurses and physicians. Developing practice efficiencies, addressing childcare concerns, and supporting personal resilience are imperative for building trust and a feeling of being valued in an organization. Organizational culture should include wellness; this can be improved with leadership development (including values alignment, and succession planning), supporting collegiality, normalizing diversity, and promoting control, autonomy, and teamwork (34). We suggest activities such as transparent communication about the current state of emergency, assuring sufficient staffing and soliciting input through listening sessions as mechanisms that may increase a sense of being valued by the organization when coupled with action.
Ethical climate is another factor in addressing integrity compromise. The nature of ICU care will raise ethical issues; what is appropriate is to set a climate expectation for ethical review and support that prevents moral injury due to compromising one’s integrity. Moral injury occurs when one is not able to do what one believes is morally right in a challenging circumstance (35). Providing time to reflect and providing ethical counseling at critical moments can serve to reduce integrity compromise, allow an enhanced sense of purpose, and show value by an organization. We believe these factors can be used to address the worrisome findings of high numbers of ICU clinicians intending to leave in part due to integrity compromise and burnout from the pandemic.
There are limitations to our study. A convenience sample was used due to the rapid emergence and spread of the pandemic. This sample was limited to a single time point in the pandemic from July to December 2020. The matching sample was not necessarily similar in all demographic manners nor in the climate of the ICUs and other clinical environments sampled. The ITL to the job question does not fully explain what factors actually would be associated with ITL, for example, financial decisions versus family or social reasons to leave the current job or leaving the profession altogether, and we do not know what percent of persons intending to leave will actually leave. Finally, the CI question is new and requires further study comparing it with other more standardized questions of moral distress and injury.
CONCLUSIONS
In conclusion, we found high rates of burnout and integrity compromise among all clinicians during the pandemic, especially among those working in ICUs. Nurses are at particularly high risk. Work-life factors of anxiety, depression, and workload make ITL higher, whereas feeling valued by one’s organization can potentially reduce adverse outcomes including burnout, integrity compromise, and ITL. We propose further studies of the critically important variable, integrity compromise, as we seek to determine best means to support ICU and non-ICU staff during this latest phase of this devastating pandemic.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Dr. Sinsky is employed by the American Medical Association. The remaining authors have disclosed that they do not have any potential conflicts of interest.
The opinions expressed in this article are those of the author(s) and should not be interpreted as American Medical Association policy.
REFERENCES
- 1.Chuang CH, Tseng PC, Lin CY, et al. : Burnout in the intensive care unit professionals: a systematic review. Medicine (Baltimore) 2016; 95:e5629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kleinpell R, Moss M, Good VS, et al. : The critical nature of addressing burnout prevention: results from the critical care societies collaborative’s national summit and survey on prevention and management of burnout in the ICU. Crit Care Med 2020; 48:249–253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moss M, Good VS, Gozal D, et al. : An official critical care societies collaborative statement: burnout syndrome in critical care healthcare professionals: a call for action. Crit Care Med 2016; 44:1414–1421 [DOI] [PubMed] [Google Scholar]
- 4.Buchbinder SB, Wilson M, Melick CF, et al. : Primary care physician job satisfaction and turnover. Am J Manag Care 2001; 7:701–713 [PubMed] [Google Scholar]
- 5.Rittenhouse DR, Mertz E, Keane D, et al. : No exit: an evaluation of measures of physician attrition. Health Serv Res 2004; 39:1571–1588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hann M, Reeves D, Sibbald B: Relationships between job satisfaction, intentions to leave family practice and actually leaving among family physicians in England. Eur J Public Health 2011; 21:499–503 [DOI] [PubMed] [Google Scholar]
- 7.Sinsky CA, Dyrbye LN, West CP, et al. : Professional satisfaction and the career plans of US physicians. Mayo Clin Proc 2017; 92:1625–1635 [DOI] [PubMed] [Google Scholar]
- 8.Hamidi MS, Bohman B, Sandborg C, et al. : Estimating institutional physician turnover attributable to self-reported burnout and associated financial burden: a case study. BMC Health Serv Res 2018; 18:851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Windover AK, Martinez K, Mercer MB, et al. Correlates and outcomes of physician burnout in a large academic medical center. JAMA Int Med 2018; 176:856–858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shanafelt TD, Mungo M, Schmitgen J, et al. : Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc 2016; 91:422–431 [DOI] [PubMed] [Google Scholar]
- 11.Willard- Grace R, Knox M, Huang B. Burnout and health care workforce turnover. Ann Fam Med 2019; 19:784–790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sinsky CA, Brown R, Linzer M, et al. COVID-related stress, burnout, and work intentions of U.S. Healthcare workers. Mayo Clin Proc 2021; 5;127–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pastores SM, Kvetan V, Coopersmith CM, et al. ; Academic Leaders in Critical Care Medicine (ALCCM) Task Force of the Society of the Critical Care Medicine: Workforce, workload, and burnout among intensivists and advanced practice providers: a narrative review. Crit Care Med 2019; 47:550–557 [DOI] [PubMed] [Google Scholar]
- 14.Epstein EG, Whitehead PB, Prompahakul C, et al. : Enhancing understanding of moral distress: the measure of moral distress for health care professionals. AJOB Empir Bioeth 2019; 10:113–124 [DOI] [PubMed] [Google Scholar]
- 15.Nash WP, Marino Carper TL, Mills MA, et al. : Psychometric evaluation of the moral injury events scale. Mil Med 2013; 178:646–652 [DOI] [PubMed] [Google Scholar]
- 16.Fumis RRL, Junqueira Amarante GA, de Fátima Nascimento A, et al. : Moral distress and its contribution to the development of burnout syndrome among critical care providers. Ann Intensive Care 2017; 7:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson-Coyle L, Opgenorth D, Bellows M, et al. : Moral distress and burnout among cardiovascular surgery intensive care unit healthcare professionals: a prospective cross-sectional survey. Can J Crit Care Nurs 2016; 27:27–36 [PubMed] [Google Scholar]
- 18.Whitehead PB, Herbertson RK, Hamric AB, et al. : Moral distress among healthcare professionals: report of an institution-wide survey. J Nurs Scholarsh 2015; 47:117–125 [DOI] [PubMed] [Google Scholar]
- 19.Dodek PM, Wong H, Norena M, et al. : Moral distress in intensive care unit professionals is associated with profession, age, and years of experience. J Crit Care 2016; 31:178–182 [DOI] [PubMed] [Google Scholar]
- 20.Schwarzkopf D, Rüddel H, Thomas-Rüddel DO, et al. : Perceived nonbeneficial treatment of patients, burnout, and intention to leave the job among ICU nurses and junior and senior physicians. Crit Care Med 2017; 45:e265–e273 [DOI] [PubMed] [Google Scholar]
- 21.Hines SE, Chin KH, Glick DR, et al. : Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the COVID-19 pandemic. Int J Environ Res Public Health 2021; 18:E488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dodek PM, Cheung EO, Burns KEA, et al. : Moral distress and other wellness measures in Canadian critical care physicians. Ann Am Thorac Soc 2021; 18:1343–1351 [DOI] [PubMed] [Google Scholar]
- 23.Prasad K, McLoughlin C, Stillman M, et al. : Prevalence and correlates of stress and burnout among US healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. EClinicalMedicine 2021; 16:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dolan R, Mohr D, Lempa M, et al. Using a single item to measure burnout in a primary care staff: a psychometric evaluation. J Gen Intern Med 2014; 30:582– 597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brady K, Pengsheng N, Carlasare L, et al. Establishing crosswalks between common measures of burnout in US physicians. J Gen Intern Med 2021. Mar 31. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.West CP, Dyrbye LN, Sloan JA, et al. Single item measures of emotional exhaustion and depersonalization. J Gen Intern Med 2009; 24:318–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rohland BM, Kruse GR, Rohrer JE: Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health 2004; 20:75–79 [Google Scholar]
- 28.Maxwell SE, Cole D. Can we test mediation with cross-sectional data? Psych Methods 2007; 12:23–44 [DOI] [PubMed] [Google Scholar]
- 29.MacKinnon DP, Fairchild AJ, Fritz MS: Mediation analysis. Annu Rev Psychol 2007; 58:593–614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shrout PE: Commentary: mediation analysis, causal process, and cross-sectional data. Multivariate Behav Res 2011; 46:852–860 [DOI] [PubMed] [Google Scholar]
- 31.Dall’Ora C, Ball J, Reinius M, et al. : Burnout in nursing: a theoretical review. Hum Resour Health 2020; 18:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Linzer M, Stillman M, Brown R, et al. : Preliminary report: US physician stress during the early days of the COVID 19 pandemic. Mayo Clin Proc Innov Qual Outcomes 2021: 5:127–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shanafelt T, Ripp J, Trockel M: Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA 2020; 323:2133–2134 [DOI] [PubMed] [Google Scholar]
- 34.Olson K, Marchalik M, Farley H, et al. Organizational strategies to reduce physician burnout and improve professional fulfillment. Currr Probl Pediatr Adolesc Health Care 2019; 49:1–15 [DOI] [PubMed] [Google Scholar]
- 35.Dean W, Talbot S, Dean A: Reframing clinician distress: moral injury not burnout. Fed Pract 2019; 36:400–402 [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.