Abstract
Background and Objectives
Residents of rural Appalachia tend to experience poorer health and greater economic distress than rural dwellers elsewhere in the United States. Although family is the first line of support for older adults needing care, it is unclear whether dementia caregivers in Appalachia assume these care responsibilities because of strong informal networks that support them in their caregiving role, underresourced formal services for persons with dementia, or culture-based reluctance to accept help from outsiders. This research examines how rural residents of Appalachia manage the care of relatives with dementia.
Research Design and Methods
The study was grounded in the Andersen Behavioral Model, supplemented with culturally relevant variables. Family caregivers from rural Appalachian counties in Virginia caring for community-dwelling relatives with dementia participated in a structured phone interview (N = 163). Generalized structural equation models were estimated, with predisposing, need, and enabling variables as predictors. Use of support services (e.g., meal delivery) and personal services (e.g., home health nurse) by family caregivers to care for the person with dementia were the dependent variables, and caregiver’s rural community identity and attitude toward services were moderators.
Results
Approximately half the sample utilized at least one support service and one personal service. Predisposing and need factors predicted the use of support services, whereas predisposing, need, and enabling factors predicted personal services. Caregivers who strongly identified with their cultural roots were less likely to use personal services unless they held a generally positive view of formal services.
Discussion and Implications
Although the extent of needs and the caregiver’s economic situation were essential influences on formal service utilization, the main drivers were the caregiver’s identification with rural Appalachian culture and attitude toward services. Findings point to within-group heterogeneity that requires differential approaches to delivery of community-based services accounting for varying attitudes, preferences, and family resources.
Keywords: Cultural identity, Home and community-based services, Service utilization
Translational Significance: The advancing age of residents in Appalachia and anticipated increase in the prevalence of dementia underscore the importance of understanding influences on formal service use by at-risk adults in this region who are caring for relatives with dementia. Our findings revealed an interaction between caregivers’ cultural identity and attitude toward formal services that led to variation in propensity to use services. Thus, researchers and journalists should attend to diversity within Appalachian communities, policymakers should supply funding for tailored services, and practitioners should develop approaches to delivery of community-based services that account for varying attitudes, preferences, and family resources.
An estimated 6.2 million Americans aged 65 and older are living with Alzheimer’s disease and related dementias (Alzheimer’s Disease Facts and Figures, 2021). In Virginia, an estimated 150,000 older adults are currently affected by dementia (Alzheimer’s Facts and Figures, 2021). Experts expect that the prevalence rate in rural areas is much higher as more than half of dementia cases go undiagnosed (Rahman et al., 2021). Given the progressive and debilitating nature of dementia, family caregivers play a critical role in managing the care of persons with dementia. They often assist with activities of daily living (e.g., personal care) and/or instrumental activities of daily living (e.g., finances, medication adherence), as well as arrange for other family members and paid workers to provide care (National Academies of Sciences, Engineering, and Medicine, 2016). Yet, information about family caregiving for persons with Alzheimer’s disease and other dementias (collectively referred to as dementia hereafter) in rural Appalachia has been slow to emerge.
Recent surveys have repeatedly shown that rural Appalachian residents suffer disparately poor health, including cognitive health, compared with the rest of the nation (Appalachian Regional Commission [ARC], 2017; Wing et al., 2020). The Appalachian region includes 420 counties in 13 states stretching 1,000 miles along the Appalachian Mountain Range from southern New York to northeast Mississippi. A network of thick forests and rugged terrain of mountains, deep gorges, and intermountain valleys has given this region its hardscrabble reputation. About 42% of the region’s population is rural, compared with 20% of the national population. An index that evaluates the Appalachian region compared to the rest of the nation on unemployment rates, per capita market income, and poverty rates classified 43% of the Appalachian counties as “distressed” or “at-risk” (ARC, 2021). Although progress has been made to narrow these disparities, significant divisions remain between Appalachia and the rest of the nation.
Many Appalachian residents live in rural, underresourced communities with disability rates significantly higher than in other parts of rural America (Pollard & Jacobsen, 2020). This place-based disparate population has also been influenced by the temperament of its primarily European-heritage inhabitants. Early Appalachian settlers often sought to avoid religious, social, economic, and political hierarchies of their homelands and were drawn to the isolation of the mountains (Jones, 1999). This geographic solitude encouraged the values of independence and individualism and contributed to reliance on strong kinship networks. These characteristics inherent in the Appalachian culture are often associated with responses to health issues and concerns, including a sense of filial obligation and strong family ties that are likely to influence how families approach the care for their relatives with dementia (Coyne et al., 2006).
People in Appalachia tend to be distrustful of outsiders, rarely seeking help from nonrelatives or formal service agencies to support them in their caregiving role (Bauer & Growick, 2003). Although family members usually are the primary source of care for persons with dementia (Friedman et al., 2015), it is unclear whether caregivers in Appalachia assume these care responsibilities because of strong, supportive informal networks, inadequate formal services for persons with dementia, dissatisfaction with available services, or culture-based reluctance to accept help from formal service providers. A systematic review of published research (1990–2010; Innes et al., 2011), focused on dementia family caregiving in rural and remote settings across the globe, identified 26 studies. Of the 15 studies that addressed service use by family caregivers to help them care for their relative with dementia, five were conducted in the United States. A more recent scoping review of published research (1997–2017; Bayly et al., 2020) focused on barriers to accessing dementia-related education and support services in rural areas worldwide. Ten of the 45 descriptive studies were conducted in the United States. Collectively, the findings from both these reviews confirmed conventional beliefs about family caregiving and service utilization in rural areas: use of formal support services has been low, gaps exist in service provision, and available services do not always meet families’ needs and expectations.
Previous examinations of cultural variations in caregiving experiences, care-related values and beliefs, care practices, and factors contributing to decisions about formal service use have focused primarily on racially and ethnically diverse family caregivers (Dilworth-Anderson et al., 2020). Rural–urban differences in family care patterns have also received some attention, with findings generally showing that rural caregivers and care recipients were more likely to use informal supports than those in more urban areas (Bédard et al., 2004; Henning-Smith et al., 2019; Innes et al., 2011). Independence coupled with a reluctance to ask for help, stigma associated with dementia, and concerns around confidentiality and privacy in a small community were commonly described cultural values that hindered service use among rural caregivers in the United States (Bayly et al., 2020; Wiese & Williams, 2018). However, little is known about formal service use by caregivers in rural Appalachia specifically. Based on their review of 18 years of rural caregiving literature, Goins et al. (2009) concluded that to discover how the rural environment influences the caregiving experience truly, greater attention must be given to macro-level influences of locations where families with older members reside, particularly how geography and culture intersect with each other, as most analyses have ignored these interfaces.
In summary, residents of Appalachia are not generally considered when discussing health disparities. Nevertheless, rural residents of Appalachia continue to experience economic distress, with concentrated areas of high poverty, unemployment, poor health, and low education (Thompson et al., 2021; Vanderpool & Huang, 2010). While some researchers have recognized the importance of examining health-related perceptions, beliefs, and behaviors within the cultural context of Appalachia (e.g., ARC, 2018; Behringer & Friedell, 2006; Della, 2011; Goins et al., 2011; Schoenberg et al., 2011), studies explicitly focused on caregiving for relatives with dementia in this region are scarce (Wiese & Williams, 2018). The advancing age of the residents in Appalachia and the anticipated increase in the number of persons with dementia underscore the importance of understanding how at-risk rural residents of Appalachia experience and manage the care of relatives with dementia.
Theoretical Framework and Research Questions
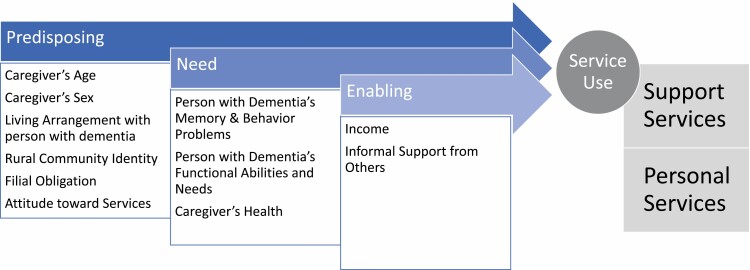
Andersen’s Behavioral Model (1995) identifies predisposing characteristics, the perceived need for services, and enabling resources that facilitate or impede service use. We extend Andersen’s model with additional constructs of help-seeking behavior, particularly cultural norms and values, to achieve a more comprehensive set of service use predictors pertinent to rural Appalachia (Figure 1). Specifically, we examine the interplay of the caregiver’s predisposing characteristics (caregiver’s age, sex, health, living arrangement relative to the person with dementia, rural culture identity, perceived filial obligations, attitude toward services), need for care (based on the person with dementia’s behaviors and functional abilities, as well as caregiver’s health), and enabling resources (income and availability of informal support) as antecedents of potential formal service use to care for the person with dementia. Grounded in this model, our main research aim was to identify what cultural beliefs, individual characteristics, and existing family support influence formal services caregivers use to meet the care needs of older relatives with dementia. Our research questions were as follows:
Figure 1.
Conceptual model based on Andersen’s behavioral model of service use.
What support services and personal services are used by family caregivers living in rural Appalachia to care for the person with dementia?
How do family caregivers’ cultural values of filial obligation, rural cultural identity, and attitude toward services influence service utilization?
Do enabling factors such as informal support from others and income predict services caregivers use for persons with dementia?
Do attitudes toward community services buffer the effects of cultural values on services used for persons with dementia?
Method
Study Design
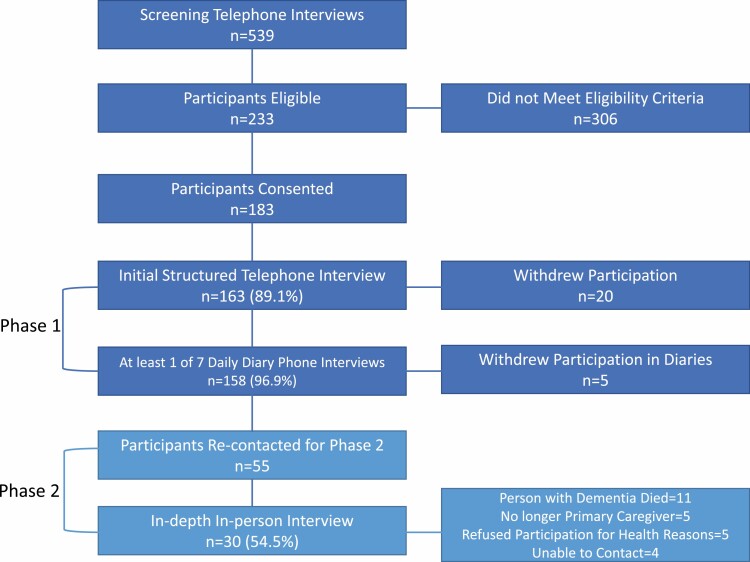
The data for the current article come from a multimethod, two-phased study that included 163 family caregivers of persons with dementia who lived in the rural Appalachia region of Virginia and who met all the eligibility criteria for the study. Following a telephone screening interview (Figure 2), in Phase 1 of the study, participants first completed a 60-min structured telephone interview. Next, they completed brief daily diary assessments on seven consecutive days about their everyday experiences of caring for a family member with dementia. In Phase 2, a subsample of family caregivers from Phase 1 participated in an in-person, in-depth interview to provide further insight into care decisions and experiences (see Roberto et al., 2021 for more details).
Figure 2.
Sampling flowchart of the two-phase, multimethod study (based on Strengthening the Reporting of Observational Studies in Epidemiology [STROBE] guidelines).
Study Participants
Family caregivers of persons with dementia were identified from a patient pool with a dementia diagnosis via Carilion Clinic, the largest health care provider in the study area, and five local Area Agencies on Aging that serve rural Appalachian counties in Virginia. Screening telephone interviews were conducted to verify eligibility criteria. Inclusion criteria for caregivers were as follows: currently resides in one of the 23 Appalachian counties in Virginia, has resided in the region for 10+ years, and is the primary caregiver for a person with dementia who either lives with the person with dementia or has contact with the community-living person with dementia at least 3 days/week. Other criteria included being 21 years of age or older, speaking English, and having no difficulty talking or hearing on the telephone.
This multimethod, two-phased study was first piloted on 39 family caregivers. Following the pilot study, the main study (called FACES-AD) collected data from 124 family caregivers. Data from the pilot study (AppCares) and FACES-AD were combined as there were no significant differences in the demographics of the two samples. All data were collected between 2017 and 2019. The current article uses data from Phase 1 structured telephone interviews only; therefore, the remainder of this article focuses on this phase of the study. Both Carilion Clinic’s and Virginia Tech’s Institutional Review Boards approved this study.
Phase 1 Procedure
Potential participants were family caregivers of persons with dementia living in rural Appalachia counties of Virginia. To identify them, a designated staff member (nurse, medical resident, or care manager) scanned case records for individuals who had been diagnosed with a form of dementia and had visited a Carilion Clinic ambulatory facility or contacted one of the five area agency on aging located in the study area in the last 2 years. Contact information for the person with dementia and their responsible party was released to the Principal Investigators. No other medical information of either the person with dementia or their responsible party was requested. Once the contact information was released, the Principal Investigators assigned a random ID number to the person with dementia and their responsible party and passed this information to the Project Coordinator. The Project Coordinator then mailed an information letter describing the study and providing the option to decline participation. A detailed consent form and visual aids for the telephone interview were also included in the package. Two weeks after the letter was mailed, either the Project Coordinator or a project interviewer contacted the potential study participant (i.e., family caregiver) via telephone for a screening interview. After confirming eligibility, the interviewer provided detailed information about the study and confirmed interest in participating.
When a family caregiver agreed to participate, the Project Coordinator or interviewer confirmed that the participant received the information package, a copy of the consent letter, and visual aids for reference during the telephone interviews. They also arranged the days and time for the telephone interviews. We used telephone interviews because they are more efficient than in-home face-to-face interviews, particularly with this geographically dispersed sample. Compared to field interviewing or postal surveys, telephone interviews include additional advantages, such as asking follow-up questions, limiting missing data, and affording quicker and more economical data collection.
Nine advanced student research assistants conducted all interviews with the caregivers. The interviewers participated in mandatory training sessions. During training, project goals were explained, and interview procedures were described and rehearsed. Research instruments were reviewed item-by-item to ensure consistency in the interpretation of questions and recording of responses. Interviewers participated in weekly debriefing meetings with the Study Investigators to foster accuracy and ensure proper interviewing protocol. Data collection records were checked by an independent data verifier to assure data consistency, adequacy, and quality. Ongoing feedback was provided so the interviewers could make needed adjustments or receive additional training. The telephone surveys were administered and recorded using Research Electronic Data Capture (Harris et al., 2009), a secure web-based data acquisition and tracking system.
Phase 1 Interviews
The Phase 1 interview included a structured telephone survey and open-ended items to obtain an in-depth assessment from the perspective of the caregivers of their and the person with dementia’s health status, their perceptions of and attitudes about informal and formal care, and the types of services they were using for the care of the person with dementia. The initial interview took approximately 60 min; caregivers received a $15 gift card for their participation. Following this interview, caregivers were called every evening for seven consecutive days. The daily diary assessments collected information about caregivers’ everyday stressors, the support they received, and the services they used to provide care for the person with dementia. Caregivers received a $5 gift card for each of the daily assessments they completed. We informed caregivers participating in Phase 1 that some individuals would be invited to participate in a more extensive interview about themselves and their relative’s current and future care needs and asked for consent to contact them later if selected.
Study Variables
Guided by our conceptual framework and input from the Community Partners, we used validated measures from the literature or constructed others as needed to ensure cultural sensitivity and community relevance. Caregivers answered using Likert-type scale response sets or briefly described the nature of their situation in their own words. Open-ended questions elicited experiences of caring for a person with dementia and interacting with health and service professionals in Appalachia regions.
Predisposing Factors
Demographic characteristics of the caregivers included age and sex. Age was a continuous variable with a range of 26–89 years. Sex was dummy-coded as 0 (male) and 1 (female). Coresidential living status was measured using a binary variable (1 = Caregiver and Person with dementia live together; 0 = Person with dementia does not live with the Caregiver). Two measures captured cultural values. The Appalachian rural community identity scale (Krok-Schoen et al., 2015) is an 11-item measure (e.g., “I identify a lot with people who live in rural communities,” “I feel a sense of loyalty to my community”) that assesses one’s sense of belonging to the land and identification with the rural Appalachian community, culture, and values. Responses to each item are rated on a 4-point Likert-type scale, with higher summed scores indicating a stronger rural community identity (Cronbach’s α = 0.91). Filial obligation was measured using the 10-item Cultural Justifications for Caregiving Scale (Powers & Whitlatch, 2016). Example items were “I was raised to believe care should be provided in the family” and “My family expects me to provide care.” Participants indicated the extent of agreement with these items on a 4-point Likert-type scale, with higher average scores indicating stronger feelings of filial obligation (Cronbach’s α = 0.81). Caregivers’ attitudes about community services were measured by 16 items adapted from the Community Service Attitude Scale (Collins et al., 1991). Example items included “Community service providers do not provide good care” and “Community services take too long to get lined up.” Participants were asked if they agreed (0) or disagreed (1) with each of these items, with a higher average score indicating a more positive attitude toward community services.
Need Factors
The degree of the person with dementia’s needs was measured using two constructs. First, memory and behavior problems were captured by 33 items adapted from the Revised Memory and Behavior Problems Checklist (Teri et al., 1992). Caregivers were asked if a certain behavior problem had occurred in the last week (0 = not occurred; 1 = occurred). Higher summed scores indicated more problematic behaviors. Functional limitations were measured at two levels: difficulties with instrumental activities of daily living (IADL) and difficulties with personal activities of daily living (ADL). The IADL questions addressed the person with dementia’s need for assistance in eight categories: cooking, driving or going places, grocery shopping, house cleaning, doing laundry, managing money and paying bills, performing minor household repairs, and taking/managing medications. The ADL questions addressed assistance needed for eating, dressing, grooming, bathing, using the toilet, and getting in and out of bed. Caregivers rated the person with dementia’s abilities on a 4-point scale (1 = does not need help at all; 4 = cannot do on their own) with higher summed values indicating worse functioning (Cronbach’s α for IADL = 0.90; for ADL = 0.93). Caregivers provided a self-rating of their overall health at present on a 4-point Likert-type scale (1 = very good to 4 = poor).
Enabling Factors
Caregivers reported how well they could get along on their income on a 4-point scale (1 = can’t make ends meet; 2 = have just enough, never any leftover; 3 = have enough with a little leftover sometimes; 4 = always have money leftover). Informal support from family and friends for ADL and IADL tasks was coded as a binary variable (1 = informal support; 0 = no informal support).
Dependent Variables
Caregivers reported whether they had used each of the five support services (meal delivery, in-home respite, transportation, adult day care, homemaker) and two personal services (home health nurse, assistance for ADL) for their relative since the dementia diagnosis. The total number of support services and the total number of personal services were used as dependent variables.
Analytical Plan
We hypothesized that predisposing, need, and enabling variables would have unique direct effects on current service use. A generalized linear structural equation model (GSEM) was estimated with predisposing, need, and enabling variables as predictors and use of support and personal services as dependent variables. Because participants who use personal services are more likely to use support services (Spearman’s ρ = 0.27, p < .005), instead of estimating two separate GSEMs, we simultaneously estimated the caregiver’s likelihood of using support services and personal services. The paths in the GSEM were estimated with Poisson regression, as the number of support services and personal services were count outcomes. In a second model, we tested the hypothesis that a combination of predisposing, need, and enabling variables would predict service use. Specifically, to assess whether caregivers’ cultural beliefs and attitudes toward services contribute to the likelihood of using services, we considered the moderating role of cultural values and attitude toward services to evaluate one’s propensity to use services. Predisposing and demographic characteristics served as control variables in this model.
Coefficients from the GSEM, robust standard errors, and incident rate ratios (IRRs; Exp(coefficient)), which is the estimated rate ratio of the dependent variable for a one-unit increase in the independent variable, given other variables are held constant, were computed. To aid in interpreting significant moderation effects, GSEM with a logistic link using a binary dependent variable (e.g., 0 = no personal services used; 1 = one to two personal services used) was computed, and effects were graphically produced using the margins function in STATA. All analyses were conducted in STATA 16.1.
Results
Table 1 presents demographic characteristics of participants in AppCares, FACES-AD, and the combined study sample. Mirroring the study region in which 84%–94% of residents are White (Pollard & Jacobsen, 2020), all of the AppCares participants were White; however, approximately 85% of the FACES-AD participants were White. Although FACES-AD participants were caring for persons with dementia who were relatively older (Mage = 80.07, SD = 9.68) compared to AppCares participants (Mage = 76.38, SD = 9.87), and needed more help with IADL tasks, a significantly larger number of caregivers from AppCares coresided with the person with dementia (n = 36, 92.31%) compared to FACES-AD (n = 89, 71.77%). There were no other significant differences between the AppCares and FACES-AD sample on any of the demographic characteristics.
Table 1.
Demographic Characteristics of AppCares and FACES-AD Participants
| Variables | AppCares (N = 39) | FACES-AD (N = 124) | Combined sample (N = 163) |
|---|---|---|---|
| M ± SD or n (%) | M ± SD or n (%) | M ± SD or n (%) | |
| Caregiver characteristics | |||
| Race (White) | 39 (100) | 106 (85.48) | 145 (88.96) |
| Sex (female) | 28 (71.79) | 92 (74.19) | 120 (73.62) |
| Age (range: 26–89) | 66.03 ± 10.65 | 64.99 ± 12.16 | 65.23 ± 11.80 |
| Self-rated health (range: 1–4) | 2.23 ± 0.90 | 2.14 ± 0.81 | 2.16 ± 0.83 |
| Income | |||
| Cannot make ends meet | 3 (7.69) | 6 (4.84) | 9 (5.52) |
| Have just enough; never leftover | 13 (33.33) | 24 (19.35) | 37 (22.70) |
| Have enough with a little leftover | 16 (41.03) | 57 (45.97) | 73 (44.79) |
| Always have money leftover | 7 (17.95) | 37 (29.84) | 44 (26.99) |
| Relationship to person with dementia | |||
| Husband | 9 (23.08) | 20 (16.13) | 29 (17.79) |
| Wife | 14 (35.90) | 31 (25.00) | 45 (27.61) |
| Son | 1 (2.56) | 10 (8.06) | 11 (6.75) |
| Daughter | 11 (28.21) | 44 (35.48) | 55 (33.74) |
| Son-in-law | 0 (0) | 1 (0.81) | 1 (0.61) |
| Daughter-in-law | 1 (2.56) | 4 (3.23) | 5 (3.07) |
| Sister | 0 (0) | 4 (3.23) | 4 (2.45) |
| Grandson | 0 (0) | 1 (0.81) | 1 (0.61) |
| Granddaughter | 0 (0) | 1 (0.81) | 1 (0.61) |
| Other | 3 (7.69) | 8 (6.45) | 11 (6.75) |
| Person with dementia’s characteristics | |||
| Sex (female) | 20 (51.28) | 82 (66.13) | 102 (62.58) |
| Age (range: 46–98) | 76.38 ± 9.87 | 80.07 ± 9.68 | 79.19 ± 9.82 |
| Memory behavior problems (range: 1–22) | 10.05 ± 4.73 | 11.08 ± 4.56 | 10.83 ± 4.61 |
| Years since diagnosis (range: 0.5–25) | 4.91 ± 4.63 | 4.15 ± 3.63 | 4.33 ± 3.89 |
| Limitations in ADLs (range: 3–24) | 11.36 ± 5.33 | 12.71 ± 6.08 | 12.39 ± 5.92 |
| Limitations in IADLs (range: 0–32) | 23.21 ± 8.35 | 27.08 ± 6.55 | 26.15 ± 7.19 |
| Coresiding with caregiver | 36 (92.31) | 89 (71.77) | 125 (76.69) |
Notes: ADLs = activities of daily living; IADLs = instrumental activities of daily living. Significant differences between AppCares and FACES-AD participants occurred for caregiver race, person with dementia’s age age, IADLs, and coresidence status of person with dementia.
Collectively, 89% of the caregivers were White and 74% were women, with the majority being daughters or wives. The caregivers, on average, were 65 years old (SD = 11.80), with 67% of caregivers rating their health as good or very good. Approximately 6% of the sample noted that they could not make ends meet with their income; 23% said that they had just enough, never any leftover. The rest of the sample (72%) said they had enough money, with some leftover. The person with dementia was, on average, 79 years old (SD = 9.82); 63% of them were women. They had been diagnosed with dementia about 4 years prior to the start of the study (SD = 3.89). Persons with dementia generally displayed 10–11 memory and behavior problems (SD = 4.61); 45% of them needed help with two or more ADL activities (M = 2.07, SD = 2.28), and 74% of them needed help with six or more IADL activities (M = 6.30, SD = 2.45). Three fourths of persons with dementia lived with caregivers (77%).
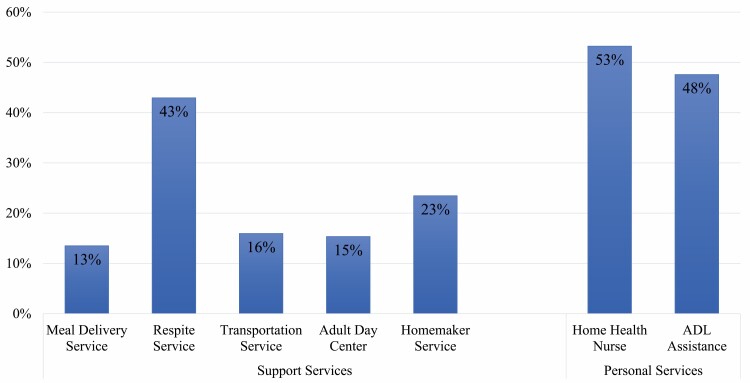
Of the 163 participants, 39 caregivers (23.93%) did not use any services in caring for their relative with dementia. Among those who used services, more than half used approximately two support services (M = 1.72, Mdn = 2, SD = 0.88, range = 1–5) and two personal services (M = 1.56, Mdn = 2, SD = 0.50, range = 1–2). Figure 3 shows the distribution of the types of services caregivers used. Among the support services, most caregivers (43%) used respite care, followed by homemaker services (23%). Similar proportions of caregivers used adult daycare (15%), transportation (16%), and meal delivery services (13%). Among the personal services, 53% of caregivers received help from home health nurses and 48% received help from personal care providers for assistance with ADL activities.
Figure 3.
Home and community-based services used by caregivers for persons with dementia. Note: ADL = activities of daily living.
Table 2 presents the direct effects of predisposing, need, and enabling factors on the utilization of support services and personal services by caregivers. Person with dementia’s predisposing factors and needs predicted more significant use of support services. Specifically, the severity of dementia as measured by the number of memory and behavioral problems was a significant predictor of the number of support services used (IRR = 1.02, p < .05). Also, caregivers of persons with dementia with more significant limitations of daily activities were more likely to use more support services (IRR = 1.04, p < .01). A more positive attitude toward community services enabled the use of more support services (IRR = 2.19, p < .05).
Table 2.
Generalized Structural Equation Model Predicting Use of Support Services and Personal Services
| Variables | Support services | Personal services | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| IRR | Coeff | RSE | 95% CI | IRR | Coeff | RSE | 95% CI | |||
| Lower | Upper | Lower | Upper | |||||||
| Predisposing factors | ||||||||||
| Caregiver age | 1.00 | 0.00 | 0.01 | −0.01 | 0.02 | 0.99 | −0.01 | 0.01 | −0.03 | 0.00 |
| Sex (Ref: Woman) | 1.08 | 0.08 | 0.15 | −0.23 | 0.38 | 0.92 | −0.09 | 0.16 | −0.40 | 0.22 |
| Coresidential status (Ref. Caregiver and person with dementia live together) | 0.87 | −0.14 | 0.18 | −0.49 | 0.21 | 0.89 | −0.12 | 0.17 | −0.44 | 0.21 |
| Rural community identity | 0.98 | −0.02 | 0.02 | −0.07 | 0.03 | 0.89 | −0.12** | 0.03 | −0.17 | −0.06 |
| Filial obligation | 0.88 | −0.13 | 0.17 | −0.46 | 0.20 | 1.72 | 0.54* | 0.27 | 0.02 | 1.07 |
| Attitude toward community services | 2.19 | 0.78* | 0.36 | 0.08 | 1.48 | 1.92 | 0.65 | 0.40 | −0.14 | 1.44 |
| Need factors | ||||||||||
| Memory and behavior problems | 1.02 | 0.02* | 0.01 | 0.00 | 0.05 | 1.01 | 0.01 | 0.01 | −0.01 | 0.04 |
| Limitations in ADLs | 1.04 | 0.04** | 0.01 | 0.01 | 0.06 | 1.04 | 0.04** | 0.02 | 0.01 | 0.07 |
| Limitations in IADLs | 1.02 | 0.02 | 0.02 | −0.01 | 0.05 | 1.06 | 0.06** | 0.02 | 0.01 | 0.11 |
| Caregiver health | 1.16 | 0.15 | 0.10 | −0.04 | 0.34 | 1.09 | 0.08 | 0.10 | −0.12 | 0.28 |
| Enabling factors | ||||||||||
| Income | ||||||||||
| Have just enough, never leftover | 1.17 | 0.16 | 0.48 | −0.79 | 1.11 | 2.29 | 0.83 | 0.60 | −0.35 | 2.01 |
| Have enough, a little leftover | 1.84 | 0.61 | 0.48 | −0.33 | 1.54 | 4.40 | 1.48* | 0.59 | 0.32 | 2.65 |
| Always have money leftover | 1.78 | 0.58 | 0.51 | −0.42 | 1.58 | 3.81 | 1.34* | 0.63 | 0.11 | 2.56 |
| Informal support from others | 1.10 | 0.09 | 0.26 | −0.41 | 0.60 | 1.38 | 0.32 | 0.25 | −0.16 | 0.80 |
| Constant | 0.11 | −2.25 | 0.88 | −3.96 | −0.53 | 0.01 | −4.21 | 0.97 | −6.12 | −2.29 |
| Interaction effect | ||||||||||
| Rural identity × Service attitude | 0.86 | −0.16 | 0.11 | −0.37 | 0.06 | 1.36 | 0.30** | 0.11 | 0.10 | 0.51 |
Note: IRR = incidence rate ratio; Coeff = beta coefficients; RSE = robust standard error; CI = confidence interval; Ref = reference group ADLs = activities of daily living; IADLs = instrumental activities of daily living.
*p < .05, **p < .01.
Predisposing, need, and enabling factors also predicted the use of personal services. Specifically, caregivers who reported stronger rural community identity were less likely to utilize personal services (IRR = 0.89, p < .01). Conversely, caregivers who expressed higher filial obligation were more likely to utilize personal services (IRR = 1.72, p < .05). Caregivers were more likely to use personal services when their person with dementia had more difficulties with ADL (IRR = 1.04, p < .01) and IADL (IRR = 1.06, p < .01) needs. Caregivers who had enough income, with a little leftover (IRR = 4.40, p < .05) or always had money leftover (IRR = 3.81, p < .05), were significantly more likely to use more personal care services.
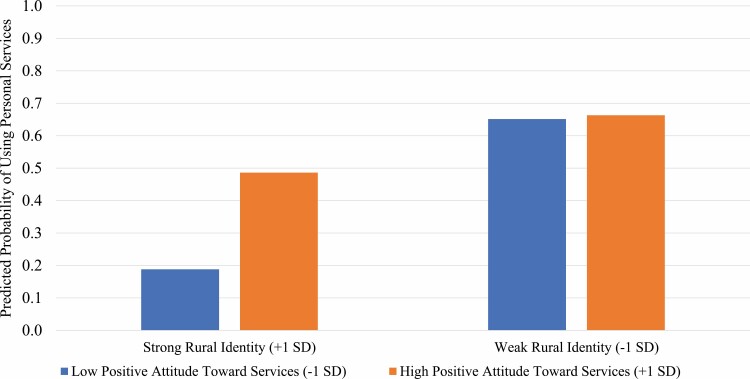
Finally, the interaction effect between rural community identity and attitude toward community services was positively associated with greater use of personal services (IRR = 1.36, p < .01), suggesting that caregivers who had a more positive attitude toward services were more likely to use personal services, despite strongly identifying with rural communities. Figure 4 shows that caregivers who strongly identified with their rural community and had a less positive attitude toward formal services had a 19% chance of using personal services. In comparison, caregivers who identified strongly with their rural community but had a more positive attitude toward services had a 49% chance of using personal services. Likewise, the figure shows that caregivers who had a weaker rural community identity, regardless of their attitude toward formal assistance, had a 65% chance of using personal services.
Figure 4.
Moderating effect of rural identity and attitude toward services on use of personal services. Note: This plot shows the predicted probability of using personal services by caregivers with strong (1 SD above the mean) and weak (1 SD below the mean) rural community identity (M = 9.37, SD = 3.19; range = 1–16.5) and low positive attitude (1 SD below the mean) and high positive attitude (1 SD above the mean) toward community services (M = 0.63, SD = 0.20; range = 0.13–1).
Discussion
The study findings confirmed that although the person with dementia’s needs and the caregiver’s economic situation were essential influences on formal service utilization, the caregiver’s rural identity and attitude toward services were the main drivers of formal service use. Different factors swayed the use of support services versus personal services. Specifically, caregivers of persons with dementia with significant disabilities and dementia-related behavior problems were more likely to use support services if they had a more positive attitude toward community services. However, caregivers who strongly identified with their cultural roots were less likely to use personal services unless they held a generally positive view of formal services. This finding recognizes within-group differences in rural communities and spotlights a critical element of the rural homecare experience. Although all the caregivers in this study were longstanding residents of their communities, we speculate that one group of caregivers may have had a history of social engagement with their community and therefore have a more positive attitude toward community services because they know the care providers as community members. The second group of caregivers, despite having lived in the community for years, may be more socially isolated, with fewer links to others outside their household. It is also possible that these caregivers are worried about confidentiality or privacy, particularly in their small rural communities where everyone knows everyone. Thus, they may have feared negative judgments from care workers regarding the condition of their house or their caregiving practices, therefore resisting the use of services (Arai et al., 2000; Glueckauf et al., 2005; Nomura et al., 2009). This latter group of caregivers reinforces the perception of rural Appalachians as people who have a strong cultural identity, prefer to provide care to their own, and are reluctant to use services.
Contrary to previous studies of rural populations that found caregivers’ values and beliefs inhibited reliance on formal services (Weaver et al., 2018), when the person with dementia’s need for care was significant, the caregivers in our study were highly likely to utilize formal assistance. Approximately half of the sample utilized at least one personal service and one support service; however, the distribution of service use varied. For example, meal delivery, transportation, and adult day services were utilized by less than one fifth of the sample. The limited use of these services may be because they are not readily available. A recent study of food pantries in rural Appalachia found that the hilly terrain and distances between homes and towns in the Appalachian regions make it difficult for meal delivery services and transportation services to be viable and economical (Grier-Welch et al., 2021). Moreover, our preliminary mapping of adult day services (data available upon request) showed only three adult day centers in the 23 counties we studied. To make rural Appalachian counties more age-friendly requires a concerted effort by policymakers, community care providers, and local residents (Menec et al., 2015) to address the lack of adequate services for family caregivers that facilitate home-based care for persons with dementia.
A widely held belief is that rural communities contain a convoy of family members, friends, and relatives who will support or care for older adults as they age (Huxhold & Fiori, 2019). Earlier studies have also noted that residents of Appalachia believe in caring for themselves and their family members. Formal support was not pursued because caregivers rely on their informal support network (Savla et al., 2019). We found weak evidence of this pattern in the present study, perhaps because of smaller family sizes (Pollard & Jacobsen, 2020) which offer fewer relatives available to help with the extensive care needed by persons with dementia. Outmigration related to education and employment opportunities elsewhere may also leave care responsibilities to a remaining family member. Indeed, most of the counties included in this study had higher than average outmigration rates than the rest of the United States (Pollard & Jacobsen, 2018).
Like previous studies (Bouldin et al., 2018), we found that affordability is a substantial predictor of service use. Although it was not a significant predictor of support services, those who were financially better off could afford more personal services. Older adults who have Medicare may receive coverage for short-term support services; however, it will not cover long-term personal care services. Older adults eligible for skilled nursing care can receive in-home and community-based services through the Programs of All-Inclusive Care for the Elderly (PACE); however, our entire study area has only one PACE program, which serves three counties and one independent city. It is possible that persons with dementia who had significant care needs and also required ongoing supervision, but whose families could not afford in-home care services, were already living in a long-term care facility and were not included in our study sample. Regardless of the circumstances, the effects of economic disparity on personal service use in rural areas require further exploration.
Numerous studies have shown that caregivers who supplement their care work with support from formal services benefit physically and mentally (Wagner & Brandt, 2018; Zarit et al., 2014). Our study found that attitude toward community services is a significant driver of the uptake of services in the rural Appalachian counties we studied. Thus, to increase the use of services to supplement the care provided by families, comprehensive caregiver intervention programs that promote utilization of services should include and evaluate the effectiveness of behavior change techniques that target psychological determinants of service use such as personal attitudes and self-efficacy. Future studies also are needed to further understand other deep-rooted reasons for reluctance to use formal services, such as mismatch of services and needs, the stigma of dementia, and privacy concerns.
One limitation of this study is potential selection bias in our sample. Although we recruited from the region’s largest health care system and the local area agencies on aging as well as advertising locally, we may have missed caregivers who live in isolation and keep to themselves. Other strategies are needed to recruit from these invisible populations in future studies. A second limitation of our study is that we chose to collapse support services (homemaker, meal delivery, etc.) and personal services into two categories to avoid multiple comparisons and prevent the inflation of false positives (i.e., Type 1 error). We acknowledge a reasonable expectation that certain factors would influence the use of specific services more than others. In addition, our study captured caregivers’ need for help from others by using caregiver’s self-assessment of their own health. Future studies should include other variables that can capture the multidimensional aspects of caregiver’s need (e.g., caregiving self-efficacy) and competing demands (e.g., availability). Another limitation is the cross-sectional design, which captures service utilization at a single time point in the dementia caregiving trajectory. Longitudinal studies that assess service utilization over time as dementia progresses would provide insight into whether attitudes toward service use change as home-based caregiving becomes more challenging to manage.
In summary, rural identity and love for the land intertwined with familial ties to the community translate into a strong sense of self-reliance and an equally strong desire to age in place for older adults. Adequate use of home- and community-based services enables many people to remain in their homes and communities as they grow old. Nevertheless, the uptake of services in rural Appalachian communities continues to be a concern for health care providers and policymakers seeking to sustain the highest possible quality of life for their citizens. This study identified critical elements and drivers of service use and sheds light on the importance of reframing caregiver’s attitudes toward services. Future research that examines other ecologically valid issues, such as concerns for privacy, autonomy, and the disconnect between the types of services available and the needs of family caregivers and persons with dementia, is warranted.
Acknowledgments
The authors would like to thank Anna Harris, Kevin Lancki, and Harper Lovegrove for their role as Project Coordinators. We would also like to thank Andrew Vipperman, Emily Hoyt, Shelby Borowski, Deneisha Poe, Emma Potter, and Marlene Strege for their assistance with recruitment and interviews, and Derek Burns and Muchin Ruiz for their help with data cleaning, archiving, and analyses. We also gratefully acknowledge the assistance of Virginia Tech Carilion School of Medicine, and Virginia Tech’s Institute for Society, Culture and Environment for their technical and infrastructure support, as well as the Mountain Empire Older Citizens, Inc., the Appalachian Agency for Senior Citizens, District Three Senior Services, the New River Valley Area Agency on Aging, and the Southern Area Agency on Aging for their guidance regarding recruitment and retention of participants, and finalizing research instruments and developing outreach materials.
Funding
This research was supported by Award No. 17-2 from the Commonwealth of Virginia’s Alzheimer’s and Related Diseases Research Award Fund and the National Institute on Aging at the National Institutes of Health (R21AG054682).
Conflict of Interest
Authors have no conflicts of interest.
References
- Alzheimer’s disease facts and figures . (2021). Alzheimer’s & dementia: The Journal of the Alzheimer’s Association, 17(3), 327–406. doi: 10.1002/alz.12328 [DOI] [PubMed] [Google Scholar]
- Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36(1), 1–10. doi: 10.2307/2137284 [DOI] [PubMed] [Google Scholar]
- Appalachian Regional Commission . (2017). Creating a culture of health in Appalachia: Disparities and bright spots.https://www.arc.gov/wp-content/uploads/2020/06/Health_Disparities_in_Appalachia_August_2017.pdf
- Appalachian Regional Commission . (2021, May 1). County economic status and distressed areas by state, FY 2021. https://www.arc.gov/county-economic-status-and-distressed-areas-by-state-fy-2021/
- Arai, Y., Sugiura, M., Miura, H., Washio, M., & Kudo, K. (2000). Undue concern for others’ opinions deters caregivers of impaired elderly from using public services in rural Japan. International Journal of Geriatric Psychiatry, 15(10), 961–968. doi: [DOI] [PubMed] [Google Scholar]
- Bauer, W. M., & Growick, B. (2003). Rehabilitation counseling in Appalachian America. Journal of Rehabilitation, 69(3), 18–24. [Google Scholar]
- Bayly, M., Morgan, D., Froehlich Chow, A., Kosteniuk, J., & Elliot, V. (2020). Dementia-related education and support service availability, accessibility, and use in rural areas: Barriers and solutions. Canadian Journal on Aging, 39(4), 545–585. doi: 10.1017/S0714980819000564 [DOI] [PubMed] [Google Scholar]
- Bédard, M., Koivuranta, A., & Stuckey, A. (2004). Health impact on caregivers of providing informal care to a cognitively impaired older adult: Rural versus urban settings. Canadian Journal of Rural Medicine, 9(1), 15–23. [PubMed] [Google Scholar]
- Behringer, B., & Friedell, G. H. (2006). Appalachia: Where place matters in health. Preventing Chronic Disease, 3(4), A113. www.cdc.gov/pcd/issues/2006/oct/06_0067.htm [PMC free article] [PubMed] [Google Scholar]
- Bouldin, E. D., Shaull, L., Andresen, E. M., Edwards, V. J., & McGuire, L. C. (2018). Financial and health barriers and caregiving-related difficulties among rural and urban caregivers. The Journal of Rural Health, 34(3), 263–274. doi: 10.1111/jrh.12273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins, C., Stommel, M., King, S., & Given, C. W. (1991). Assessment of the attitudes of family caregivers toward community services. The Gerontologist, 31(6), 756–761. doi: 10.1093/geront/31.6.756 [DOI] [PubMed] [Google Scholar]
- Coyne, C. A., Demian-Popescu, C., & Friend, D. (2006). Social and cultural factors influencing health in southern West Virginia: A qualitative study. Preventing Chronic Disease, 3(4), A124. http://www.cdc.gov/pcd/issues/2006/oct/06_0030.htm [PMC free article] [PubMed] [Google Scholar]
- Della, L. J. (2011). Exploring diabetes beliefs in at-risk Appalachia. The Journal of Rural Health, 27(1), 3–12. doi: 10.1111/j.1748-0361.2010.00311.x [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson, P., Moon, H., & Aranda, M. P. (2020). Dementia caregiving research: Expanding and reframing the lens of diversity, inclusivity, and intersectionality. The Gerontologist, 60(5), 797–805. doi: 10.1093/geront/gnaa050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman, E. M., Shih, R. A., Langa, K. M., & Hurd, M. D. (2015). US prevalence and predictors of informal caregiving for dementia. Health Affairs (Project Hope), 34(10), 1637–1641. doi: 10.1377/hlthaff.2015.0510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glueckauf, R. L., Stine, C., Bourgeois, M., Pomidor, A., Rom, P., Young, M. E., Massey, A., & Ashley, P. (2005). Alzheimer’s Rural Care Healthline: Linking rural caregivers to cognitive-behavioral intervention for depression. Rehabilitation Psychology, 50(4), 346–354. doi: 10.1037/0090-5550.50.4.346 [DOI] [Google Scholar]
- Goins, R. T., Spencer, S. M., & Byrd, J. C. (2009). Research on rural caregiving: A literature review. Journal of Applied Gerontology, 28(2), 139–170. doi: 10.1177/0733464808326294 [DOI] [Google Scholar]
- Goins, R. T., Spencer, S. M., & Williams, K. (2011). Lay meanings of health among rural older adults in Appalachia. The Journal of Rural Health, 27(1), 13–20. doi: 10.1111/j.1748-0361.2010.00315.x [DOI] [PubMed] [Google Scholar]
- Grier-Welch, A., Marquis, J., Spence, M., Kavanagh, K., & Anderson Steeves, E. T. (2021). Food acquisition behaviors and perceptions of food pantry use among food pantry clients in rural Appalachia. Ecology of Food and Nutrition, 60(1), 70–88. doi: 10.1080/03670244.2020.1793138 [DOI] [PubMed] [Google Scholar]
- Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henning-Smith, C., Lahr, M., & Casey, M. (2019). A national examination of caregiver use of and preferences for support services: Does rurality matter? Journal of Aging and Health, 31(9), 1652–1670. doi: 10.1177/0898264318786569 [DOI] [PubMed] [Google Scholar]
- Huxhold, O., & Fiori, K. L. (2019). Do demographic changes jeopardize social integration among aging adults living in rural regions? The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 74(6), 954–963. doi: 10.1093/geronb/gby008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Innes, A., Morgan, D., Kosteniuk, J., & Kostineuk, J. (2011). Dementia care in rural and remote settings: A systematic review of informal/family caregiving. Maturitas, 68(1), 34–46. doi: 10.1016/j.maturitas.2010.10.002 [DOI] [PubMed] [Google Scholar]
- Jones, L. (1999). Faith and meaning in the Southern Uplands. University of Illinois Press. doi: 10.1353/aph.1999.0083 [DOI] [Google Scholar]
- Krok-Schoen, J. L., Palmer-Wackerly, A. L., Dailey, P. M., & Krieger, J. L. (2015). The conceptualization of self-identity among residents of Appalachia Ohio. Journal of Appalachian Studies, 21(2), 229–246. doi: 10.5406/jappastud.21.2.0229 [DOI] [Google Scholar]
- Menec, V., Bell, S., Novek, S., Minnigaleeva, G. A., Morales, E., Ouma, T., Parodi, J. F., & Winterton, R. (2015). Making rural and remote communities more age-friendly: Experts’ perspectives on issues, challenges, and priorities. Journal of Aging & Social Policy, 27(2), 173–191. doi: 10.1080/08959420.2014.995044 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine . (2016). Family caring for an aging America. The National Academies Press. doi: 10.17226/23606 [DOI] [PubMed] [Google Scholar]
- Nomura, M., Makimoto, K., Kato, M., Shiba, T., Matsuura, C., Shigenobu, K., Ishikawa, T., Matsumoto, N., & Ikeda, M. (2009). Empowering older people with early dementia and family caregivers: A participatory action research study. International Journal of Nursing Studies, 46(4), 431–441. doi: 10.1016/j.ijnurstu.2007.09.009 [DOI] [PubMed] [Google Scholar]
- Pollard, K., & Jacobsen, L. A. (2020). The Appalachian region: A data overview from the 2014–2018 American Community Survey Chartbook. Population Reference Bureau. https://www.arc.gov/report/the-appalachian-region-a-data-overview-from-the-2014-2018-american-community-survey/ [Google Scholar]
- Powers, S. M., & Whitlatch, C. J. (2016). Measuring cultural justifications for caregiving in African American and White caregivers. Dementia (London, England), 15(4), 629–645. doi: 10.1177/1471301214532112 [DOI] [PubMed] [Google Scholar]
- Rahman, M., White, E. M., Mills, C., Thomas, K. S., & Jutkowitz, E. (2021). Rural–urban differences in diagnostic incidence and prevalence of Alzheimer’s disease and related dementias. Alzheimer’s & Dementia, 17(7), 1213–1230. doi: 10.1002/alz.12285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberto, K. A., Savla, J., McCann, B. R., Blieszner, R., & Knight, A. L. (2021). Dementia family caregiving in rural Appalachia: A sociocultural model of service use [Manuscript submitted for publication]. Center for Gerontology, Virginia Tech. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savla, J., Bivens, L. R., Roberto, K. A., & Blieszner, R. (2019). Where you age matters: Individual- and county-level predictors of formal and informal care in rural Appalachia. Journal of Aging and Health, 31(5), 837–860. doi: 10.1177/0898264318761907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenberg, N. E., Bardach, S. H., Manchikanti, K. N., & Goodenow, A. C. (2011). Appalachian residents’ experiences with and management of multiple morbidity. Qualitative Health Research, 21(5), 601–611. doi: 10.1177/1049732310395779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teri, L., Truax, P., Logsdon, R., Uomoto, J., Zarit, S., & Vitaliano, P. P. (1992). Assessment of behavioral problems in dementia: The revised memory and behavior problems checklist. Psychology and Aging, 7(4), 622–631. doi: 10.1037//0882-7974.7.4.622 [DOI] [PubMed] [Google Scholar]
- Thompson, J. R., Risser, L. R., Dunfee, M. N., Schoenberg, N. E., & Burke, J. G. (2021). Place, power, and premature mortality: A rapid scoping review on the health of women in Appalachia. American Journal of Health Promotion, 35(7), 1015–1027. doi: 10.1177/08901171211011388 [DOI] [PubMed] [Google Scholar]
- Vanderpool, R. C., & Huang, B. (2010). Cancer risk perceptions, beliefs, and physician avoidance in Appalachia: Results from the 2008 HINTS Survey. Journal of Health Communication, 15(Suppl. 3), 78–91. doi: 10.1080/10810730.2010.522696 [DOI] [PubMed] [Google Scholar]
- Wagner, M., & Brandt, M. (2018). Long-term care provision and the well-being of spousal caregivers: An analysis of 138 European regions. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73(4), 24–34. doi: 10.1093/geronb/gbx133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver, R. H., Roberto, K. A., & Blieszner, R. (2018). Older adults in rural Appalachia: Preference and expectations for future care. International Journal of Aging & Human Development, 86(4), 364–381. doi: 10.1177/0091415017720891 [DOI] [PubMed] [Google Scholar]
- Wiese, L. K., & Williams, C. L. (2018). An Appalachian perspective of Alzheimer’s disease: A rural health nurse opportunity. Online Journal of Rural Nursing and Health Care, 18(1), 180–208. doi: 10.14574/ojrnhc.v17i1.469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing, J. J., Levine, D. A., Ramamurthy, A., & Reider, C. (2020). Alzheimer’s disease and related disorders prevalence differs by Appalachian residence in Ohio. Journal of Alzheimer’s Disease, 76(4), 1309–1316. doi: 10.3233/JAD-200491 [DOI] [PubMed] [Google Scholar]
- Zarit, S. H., Kim, K., Femia, E. E., Almeida, D. M., & Klein, L. C. (2014). The effects of adult day services on family caregivers’ daily stress, affect, and health: Outcomes from the Daily Stress and Health (DaSH) study. The Gerontologist, 54(4), 570–579. doi: 10.1093/geront/gnt045 [DOI] [PMC free article] [PubMed] [Google Scholar]