Abstract
Background
Research on health across the life course consistently documents widening racial and socioeconomic disparities from childhood through adulthood, followed by stabilization or convergence in later life. This pattern appears to contradict expectations set by cumulative (dis)advantage (CAD) theory. Informed by the punctuated equilibrium perspective, we examine the relationship between midlife health and subsequent health change and mortality and consider the impact of earlier socioeconomic exposures on observed disparities.
Methods
Using the Health and Retirement Study, we characterize the functional impairment histories of a nationally representative sample of 8464 older adults between 1994 and 2016. We employ nonparametric and discrete outcome multinomial logistic regression to examine the competing risks of mortality, health change, and attrition.
Results
Exposures to disadvantages are associated with poorer functional health in midlife and mortality. However, a higher number of functional limitations in midlife is negatively associated with the accumulation of subsequent limitations for White men and women and for Black women. The impact of educational attainment, occupation, wealth, and marriage on later-life health differs across race and gender groups.
Conclusions
Observed stability or convergence in later-life functional health disparities is not a departure from the dynamics posited by CAD, but rather a result of the differential impact of racial and socioeconomic inequities on mortality and health at older ages. Higher exposure to disadvantages and a lower protective impact of advantageous exposures lead to higher mortality among Black Americans, a pattern which masks persistent health inequities later in life.
Keywords: Disablement process, Minority aging, Socioeconomic issues
Research on health and aging consistently documents widening racial and socioeconomic disparities from childhood through adulthood, followed by stabilization, convergence, or sometimes cross-overs in later life (1–4). Such findings have puzzled scholars of cumulative (dis)advantage (CAD) (5–7) who expect prolonged exposures to structural racism and discrimination on the basis of gender, socioecononmic status, and other characteristics may manifest in widening health inequities throughout the life course. Using nationally representative data tracking older adults for over 2 decades and an analytic approach informed by the recently developed Punctuated Equilibrium modeling framework (8), we offer a new perspective on this puzzle.
Specifically, we examine the relationship between midlife health and subsequent health changes and consider the impact of multiple early and midlife social and economic exposures on mortality and health change as 2 distinct yet interconnected—and sometimes competing—outcomes. We show that observed patterns of stable or diminished racial disparities are not a departure from the dynamics posited by CAD, but rather a result of the differential impact of racial and socioeconomic inequities on mortality relative to health at older ages. Our findings offer insight into the mechanisms through which multiple domains of disadvantage both shape and mask inequities in later-life health.
Cumulative (Dis)Advantage and Disappearing Disparities in Later Life
CAD theory provides a framework for understanding how advantages and disadvantages accumulate over the life course. This perspective—first developed in sociology (9–11) and increasingly used to inform gerontological research (6,12,13)—situates individual trajectories in the context of structural factors which may exacerbate or ameliorate previous (dis)advantages, with consequences for individual health and well-being in later life and population-level inequality.
A rich empirical literature has documented clear associations between exposures to social and economic (dis)advantages in early life and subsequent health disparities. It has demonstrated that education, occupations, income, and wealth, shape gradients in health both independently and jointly, with notable, persistent variation across groups defined by race/ethnicity and gender (14–17). It has also highlighted the role of social support and engagement (and their absence) as determinants of health (18) that operate upstream from proximate factors such as individual health behaviors (19).
Longitudinal studies inspired by CAD often consider demographic sub-populations defined by gender, race, ethnicity, nativity, or socioeconomic status (as well as intersections of these categories), and employ trajectory models to examine the extent to which they vary in baseline measures of health and in the rate of subsequent health declines (2,14,20–22). These studies have examined diverse health indicators including self-rated health (23), morbidity (20,24), functional status (21), and disability (25) and reached somewhat varied conclusions about the shape of the health trajectories, the magnitude of between-group differences, and the extent to which health trajectories respond to social and economic conditions. Still, a common finding across these studies is that exposures earlier in the life course are stronger predictors of health disparities at midlife than of the rate of subsequent health changes. Together, these studies suggest that social disparities in health either remain stable or narrow somewhat as populations age (14,21,22).
At first, these findings appear inconsistent with CAD theory, which posits the accumulation of advantage and disadvantage as continuous processes that sustain and increase inequality over time. Because the social determinants of health are thought to operate throughout the life course (26,27) finding stability or convergence of disparities in later life raises questions about the applicability of CAD to health at older ages.
Potential explanations for an “age-as-leveler-of-inequality” effect have drawn on biology, policy analysis, and demography. The biological argument posits that universal, biologically programmed health declines overtake social and economic factors as the most prominent determinants of health in later life, reducing observed disparities (28,29). Policy scholars have noted that at older ages Social Security and Medicare—programs that provide a steady income and health insurance coverage—may equalize access to health-promoting resources more than at younger ages (30). Finally, demographers have argued that an observed convergence in health and longevity may be a statistical artifact of selection: an outcome of differential mortality risks at younger ages (4,31,32). The demographic explanation points to a key distinction between the determinants of individual and population health at older ages: For individuals, death may follow but cannot precede a period of health declines. For cohorts, however, mortality at younger ages may influence patterns of health for those who survive into older ages. Building on this insight, our analysis aims to reconcile the expectations of CAD and the empirical literature on longitudinal health disparities and provide insight into the dynamic relationship between longevity and later-life health trajectories in the context of social and economic disparities.
The Current Study
Our analysis examines variation in the relationship between early and midlife social (dis)advantages and health in midlife, subsequent health change, and mortality. To capture health status most comprehensively, we examine a count of functional limitations, conceptually situated between chronic conditions and severe disability and encompassing a range of mild and severe impairments that individuals can develop or recover from over time (33). This measure is commonly used to test CAD hypotheses in trajectory studies examining how health disparities unfold in later life (21,22,34).
To capture social and economic (dis)advantage, we examine the role of education, occupation, and wealth. These factors together encompass multiple key attributes of socioeconomic status, including relatively early investment in human capital (itself a function of parental socioeconomic status), long-term exposure to particular working conditions and associated social and economic benefits, and the availability of economic resources in adulthood, including in postretirement years. These indicators are highly correlated with multiple health outcomes, yet their ability to predict changes in later-life health has been found to be somewhat limited (14,21,29).
We re-evaluate the salience of these factors for disparities in later-life health and mortality by moving away from the latent trajectory models most common in studies of health disparities toward a Punctuated Equilibrium modeling strategy (8,35). The latter explicitly incorporates both mortality and nonrandom attrition as competing risks for multidirectional health change via nonparametric methods and multinomial logistic regressions. A Punctuated Equilibrium orientation emphasizes that individual health change is neither as smooth, continuous, nor unidirectional as assumed by standard population trajectory models. Consequently, it highlights heterogeneity in individual health histories while also recognizing that they unfold in the context of structural racial, gendered, and socioeconomic stratification.
Notably, while social, economic, and behavioral advantages are associated with advantageous health and longevity, both the ability to attain advantaged statuses and resources and the extent to which they translate into health advantages vary by race and gender. For the older cohort considered in this analysis, racial residential segregation and gendered and racial stratification in educational, employment, and family settings are particularly salient. For example, college degrees were more common for White men than for any other group among this birth cohort (36) and being married has been shown to be associated with greater health benefits for men than women (37,38). The disproportionate social and economic stressors (39) and higher burden of mortality and poor health faced by Black men (40), and Black women (41), are thus increasingly understood to reflect not only differential individual exposures, but also intersecting stratification systems that reinforce each other to influence population health and health disparities (42). To capture the heterogeneity in the association of social (dis)advantages with health, we stratify all analyses by race and gender.
Method
Data
Our analysis draws on the Health and Retirement Study (HRS), a nationally representative longitudinal panel study of older adults (43) that includes extensive repeated measures of health and a mortality record. Response rates to the survey are high, surpassing 80% at each wave (44). Because of these strengths, the survey is widely used to understand health change over time and test hypotheses derived from CAD theory. We use data from Waves 2–13 of the HRS collected biennially between 1994 and 2016. We exclude Wave 1 from our analysis because the response categories for questions on functional limitations, a key variable in our analysis, were not comparable with other waves in the study (45). Our sample comprises 8464 members of the HRS cohort (born between 1931 and 1941), which has the largest sample size and follow-up period. Our analysis focuses on 3662 White women, 3317 men, 887 Black women, and 598 Black men; respondents who identified as Hispanic or of some other race or ethnicity were not included due to small sample sizes.
Measures
To examine changes in functional health at older ages, we use the sum of 3 scales administered in the HRS:
(1) Mobility: Reported difficulty with walking several blocks, walking one block, walking across the room, climbing several flights of stairs, and climbing one flight of stairs.
(2) Large muscle functioning: Reported difficulty with sitting for 2 hr, getting up from a chair, stooping or kneeling or crouching, and pushing or pulling a large object.
(3) Fine motor skills: Reported difficulty with picking up a dime, eating, and dressing.
All items are scored so a value of 0 indicates no difficulty and 1 indicates difficulty. The functional limitations measure ranges from 0 (no limitations) to 12 (most limited). Given the range of possible functional limitations, this measure allows for varied starting points and considerable health change in both negative and positive directions.
Since the risk of death or attrition increases with both age and study duration, we consider loss to follow up and mortality as informative outcomes, consistent with the Punctuated Equilibrium approach (8). People are considered lost to follow up if they are not in sample for the last used round of the HRS (Wave 13) and do not have a date of death via the linked National Death Index. A description of sample loss across waves is included in Supplementary Figures A1 and A2.
Our predictors include multiple upstream social determinants of health and one proximate health behavior all measured at baseline. The socioeconomic status (SES) measures include highest level of education achieved by the respondent (less than high school, high school, some college, or 4-year college degree), household wealth quintile, and longest-held occupation (none reported, “office” occupation in professional, managerial, clerical or sales, or “non-office” occupation in production, operations, service or farming). In addition, our models include marital status as a measure of social support that has been shown to be particularly salient for members of this older American cohort (46). Smoking history (ever smoked) is included because of its role as a major proximate determinant of morbidity and mortality. It also serves as a useful comparison to the more distal determinants of health. Since associations between social (dis)advantages and health should be understood in the structural context where access to resources and exposure to discrimination may have varied by race and gender, we pay special attention to the potential of differential exposures and effects via analyses stratified by race and gender (See Supplementary Table 1 for characteristics by race and gender).
Analytic Strategy
We begin with a nonparametric descriptive analysis stratifying individuals by the number of functional limitations they reported at baseline (0, 1, 2, 3, 4, or 5+) and examining the distribution of demographic, social, and economic characteristics in each strata, as well as the outcome (same number of functional limitations as observed at baseline, more limitations than baseline, fewer limitations than baseline) at round 13. We also consider the percentages who ever experienced an improvement in functional status (fewer limitations) or a decline in functional status (more limitations). We classify 5+ limitations as the highest category because fewer than 10% of the sample have more than 5 functional limitations at baseline. To capture accumulated limitations among individuals lost to follow up (either due to death or survey-nonparticipation), we compared starting health and health change among individuals by their ultimate status in the survey (in sample with same or fewer limitations than baseline, in-sample with more limitations than baseline, lost to mortality, lost to follow up).
Next, we conducted a multinomial logistic regression to predict 4 possible health outcomes at Wave 13 of the survey: (i) in sample with the same (or fewer) number of functional limitations than baseline; (ii) in sample with a health decline as measured by an increase in functional limitations; (iii) lost to follow up; or (iv) lost to mortality. The models include functional status at baseline as well as education, occupation, marital status, smoking history, and household wealth quintile so as to examine the role of midlife health and prior socioeconomic (dis)advantages on subsequent outcomes.
We stratify all analyses by race and gender, which we consider as markers of differential life experiences due to structural inequality. In supplemental analyses, we pooled respondents across race and gender. Model fit statistics, specifically the Akaike Information Criterion, indicated that a model with multiple interactions by race and gender best fit the data, consistent with our understanding of how these variables operate to structure lived experiences. To streamline interpretation, we present results from the stratified models.
We present relative risk ratios (RRR) from these multinomial models with the category “no health change or a health improvement” as the reference. If poor health accumulated gradually across the life course, individuals who experienced disadvantages would be more likely to have a RRR greater than 1 for experiencing an increase in functional limitations or dying relative to remaining in the sample at the same or better health status.
However, the RRRs do not estimate the likelihood that each outcome will occur nor differences in likelihoods by social position and across race gender groups. To quantify the impact of midlife health and early conditions on subsequent health change and mortality, we also calculate the predicted probabilities of each outcome for our race-and-gender-stratified subpopulations under 3 scenarios:
Group average: assign each race-gender group its specific average level of baseline functional limitations, education, wealth, occupation, smoking history, and marital status.
Concentrated health and social advantage: assign each race-gender group zero functional limitations at baseline, college-level education, the highest wealth quintile, an office occupation, nonsmoker status, and married status at baseline.
Concentrated health and social disadvantage: assign each race–gender group 5 functional limitations at baseline, a less-than-high-school education, the lowest wealth quintile, a non-office occupation, smoker status, and not married status at baseline.
We first describe outcomes for the race–gender group mean to demonstrate group differences in health change and mortality risk and highlight systematic differences across groups in health and social opportunities. Next, we demonstrate how the concentration of advantages and disadvantages influences outcomes. To quantify uncertainty around estimates, we calculate standard errors for the predicted probabilities across 1000 bootstrapped samples (47).
Finally, we run a number of sensitivity checks to account for the impact of potentially selective survival and differential attrition. First, we examine the association between baseline health and health outcomes at Wave 6 of the HRS survey (approximately the midpoint of follow-up) to see if associations differ when cohort members have had less exposure to mortality and attrition. Second, for individuals observed at 2 or more survey rounds we run race–gender-stratified logistic regression models where the outcome is 1 if people have more limitations when last observed and 0 if people stay at the same or better functional status. Here, we focus on the association of midlife health and earlier life socioeconomic conditions with health change during the time respondents were in-sample.
Analyses were conducted using Stata 16.1 (StataCorp LLC, College Station, TX) employing appropriate survey weights from Wave 2 of the HRS.
Results
Looking at respondent characteristics by first observed functional status (Table 1) reveals familiar disparities by race and gender. White and Black women (46.4% and 5.8% of the sample) are underrepresented in the no limitations category (39.5% and 3.7%) and over-represented in the high limitations category (52.5% and 12.5%). In contrast, White men (43.6% of the sample) are over-represented in the no limitations category (51.5%) and underrepresented in the high limitations category (29.8%). Black men (4.3% of the sample) are over-represented at both tails of the distribution: they are both more likely to have no limitations (5.3%) and a high number of limitations (5.3%).
Table 1.
Descriptive Statistics by Baseline Health
| No Limitations | One Limitation | Two Limitations | Three Limitations | Four Limitations | Five + Limitations | Total Sample | |
|---|---|---|---|---|---|---|---|
| N = 3456 | N = 1615 | N = 1035 | N = 677 | N = 513 | N = 1168 | N = 8464 | |
| White Female | 0.395 | 0.47 | 0.503 | 0.563 | 0.585 | 0.525 | 0.464 |
| White Male | 0.515 | 0.444 | 0.409 | 0.353 | 0.302 | 0.298 | 0.436 |
| Black Female | 0.037 | 0.058 | 0.056 | 0.058 | 0.074 | 0.125 | 0.058 |
| Black Male | 0.053 | 0.028 | 0.032 | 0.026 | 0.039 | 0.053 | 0.043 |
| Less than HS diploma | 0.194 | 0.224 | 0.272 | 0.321 | 0.39 | 0.506 | 0.27 |
| Completed HS | 0.317 | 0.378 | 0.36 | 0.398 | 0.366 | 0.303 | 0.341 |
| Some college | 0.232 | 0.212 | 0.203 | 0.163 | 0.165 | 0.129 | 0.202 |
| Completed college degree | 0.258 | 0.186 | 0.165 | 0.118 | 0.079 | 0.063 | 0.186 |
| Respondent married at Round 2 | 0.772 | 0.768 | 0.763 | 0.714 | 0.692 | 0.614 | 0.741 |
| Respondent ever smoked at Round 2 | 0.624 | 0.63 | 0.644 | 0.628 | 0.656 | 0.715 | 0.641 |
| First Wealth Quintile (Lowest Wealth) | 0.101 | 0.126 | 0.141 | 0.216 | 0.232 | 0.377 | 0.162 |
| Second Wealth Quintile | 0.147 | 0.166 | 0.160 | 0.209 | 0.200 | 0.237 | 0.171 |
| Third Wealth Quintile | 0.197 | 0.210 | 0.217 | 0.206 | 0.240 | 0.161 | 0.201 |
| Fourth Wealth Quintile | 0.258 | 0.231 | 0.226 | 0.171 | 0.189 | 0.128 | 0.221 |
| Fifth Wealth Quintile (Highest Wealth) | 0.298 | 0.267 | 0.256 | 0.197 | 0.139 | 0.098 | 0.244 |
| No occupation reported | 0.102 | 0.118 | 0.118 | 0.122 | 0.135 | 0.166 | 0.119 |
| Occupation professional, managerial, clerical or sales | 0.585 | 0.526 | 0.499 | 0.488 | 0.396 | 0.349 | 0.515 |
| Occupation production, service, operations or farming | 0.313 | 0.356 | 0.383 | 0.391 | 0.470 | 0.486 | 0.367 |
| Last observed with higher limitationsa | 0.628 | 0.657 | 0.605 | 0.635 | 0.602 | 0.501 | 0.614 |
| Functional limitations ever increased | 0.778 | 0.795 | 0.798 | 0.778 | 0.759 | 0.65 | 0.767 |
| Functional limitations ever decreased | 0 | 0.67 | 0.754 | 0.687 | 0.743 | 0.74 | 0.414 |
| Not observed for 2 or more survey rounds | 0.045 | 0.041 | 0.03 | 0.046 | 0.039 | 0.088 | 0.047 |
| Average last survey round observed | 10.359 | 10.008 | 10.32 | 9.629 | 9.47 | 8.744 | 9.974 |
| Died | 0.277 | 0.358 | 0.369 | 0.421 | 0.499 | 0.591 | 0.368 |
| Lost to follow up | 0.217 | 0.19 | 0.162 | 0.192 | 0.155 | 0.117 | 0.187 |
Note: aCalculated for those observed for 2 or more survey rounds.
As predicted by cumulative (dis)advantage theory, people with higher educational attainment and wealth are more likely to start the survey with few or no functional limitations and less likely to start with high impairment (5 or more limitations). However, the relation between starting health and subsequent health change is less intuitive. 77.8% of individuals who start out with no limitations experience some increase. In contrast, just 65.0% of those who start with 5 or more limitations ever experience increased impairment. Health improvement is not uncommon at midlife; 41.4% of respondents had some reduction in functional limitations, with the proportion even higher (71.3%) among those who started with limitations. While functional limitation appears inversely associated with added impairment, it is strongly and positively linked with mortality. 27.7% of those who start the survey without limitations die during follow-up; among those with high limitations at baseline, this share more than doubles (59.1%).
Classifying individuals by their final outcome (Table 2) reveals that remaining in sample for the duration of follow-up is associated with significant advantage across the life course. Differences in health and mortality are particularly salient at the intersection of race and gender. Relative to their share of the sample (46.4%) White women are more likely to remain in the survey at the same health (48.0%) or with more limitations (53.1%) than they are to be lost to mortality (39.4%). Meanwhile, White men, Black men, and Black women are all over-represented among those lost to mortality.
Table 2.
Descriptive Statistics by Outcome
| In Sample All Rounds Limitations at Last Round Same or Lower than First Round | In Sample All Rounds Limitations at Last Round Higher than First Round | Died During Follow-up Period | Lost to Follow up | Total | |
|---|---|---|---|---|---|
| N = 1338 | N = 2376 | N = 3227 | N = 1523 | N = 8464 | |
| White Female | 0.48 | 0.531 | 0.394 | 0.484 | 0.464 |
| White Male | 0.432 | 0.376 | 0.479 | 0.443 | 0.436 |
| Black Female | 0.052 | 0.063 | 0.064 | 0.045 | 0.058 |
| Black Male | 0.036 | 0.029 | 0.063 | 0.029 | 0.043 |
| Less than HS diploma | 0.203 | 0.222 | 0.346 | 0.251 | 0.27 |
| Completed HS | 0.328 | 0.355 | 0.325 | 0.366 | 0.341 |
| Some college | 0.205 | 0.217 | 0.19 | 0.203 | 0.202 |
| Completed college degree | 0.264 | 0.207 | 0.139 | 0.181 | 0.186 |
| Respondent married at Round 2 | 0.793 | 0.763 | 0.689 | 0.766 | 0.741 |
| Respondent ever smoked at Round 2 | 0.545 | 0.577 | 0.76 | 0.59 | 0.641 |
| First Wealth Quintile (Lowest Wealth) | 0.110 | 0.135 | 0.230 | 0.115 | 0.162 |
| Second Wealth Quintile | 0.146 | 0.159 | 0.201 | 0.154 | 0.171 |
| Third Wealth Quintile | 0.187 | 0.204 | 0.199 | 0.212 | 0.201 |
| Fourth Wealth Quintile | 0.242 | 0.227 | 0.197 | 0.242 | 0.221 |
| Fifth Wealth Quintile (Highest Wealth) | 0.315 | 0.275 | 0.173 | 0.277 | 0.244 |
| No longest occupation reported | 0.097 | 0.106 | 0.137 | 0.120 | 0.119 |
| Longest occupation professional, managerial, clerical or sales | 0.591 | 0.574 | 0.435 | 0.515 | 0.515 |
| Longest occupation production, service, operations or farming | 0.311 | 0.321 | 0.428 | 0.364 | 0.367 |
| Last observed with higher limitationsa | 0 | 1 | 0.673 | 0.441 | 0.614 |
| Functional limitations ever increased | 0.643 | 1 | 0.759 | 0.54 | 0.767 |
| Functional limitations ever decreased | 0.543 | 0.375 | 0.429 | 0.328 | 0.414 |
| Not observed for 2 or more survey rounds | 0 | 0 | 0.06 | 0.136 | 0.047 |
| No functional limitations Round 2 | 0.442 | 0.497 | 0.317 | 0.488 | 0.42 |
| One functional limitation Round 2 | 0.177 | 0.209 | 0.189 | 0.197 | 0.194 |
| Two functional limitations Round 2 | 0.142 | 0.123 | 0.124 | 0.107 | 0.123 |
| Three functional limitations Round 2 | 0.079 | 0.062 | 0.09 | 0.08 | 0.078 |
| Four functional limitations Round 2 | 0.046 | 0.046 | 0.08 | 0.049 | 0.059 |
| Five + functional limitations Round 2 | 0.115 | 0.063 | 0.201 | 0.078 | 0.125 |
Note: aCalculated for those observed for 2 or more survey rounds.
Social advantage is also related to survey retention, suggesting that our understanding of health declines in later life may be disproportionately informed by the experiences of relatively advantaged adults. Respondents with a college education, those in “office” occupations, married persons, and the wealthiest households are disproportionately represented among those who stay in the sample at the same or worse health and underrepresented among those lost to mortality.
A key counter-intuitive finding is that advantaged health status in midlife appears to increase the risk of subsequent health declines. Tables 3 and 4 present results from race- and gender-stratified multinomial logistic regression models highlighting the differential exposure to and impact of social (dis)advantage across demographic groups. For all groups except Black men, the number of functional limitations at baseline is negatively associated with the likelihood of having more impairments at the last observation (RR = 0.854; 95% CI: 0.812–0.897 for White women; RR = 0.823 95% CI: 0.765–0.886 for White men; RR = 0.822; 95% CI: 0.749–0.902 for Black women). For Black men, there is no statistically significant association between starting limitations and health change (RR = 0.917; 95% CI: 0.792–1.062). For White women, White men, and Black men, starting limitations are positively associated with mortality risk (RR = 1.062 95% CI: 1.014–1.113 for White women; RR = 1.076 95% CI: 1.011–1.145 for White men; RR = 1.128 95% CI: 1.015–1.254 for Black men). For Black women, the relative risk ratio is similar to other groups (RR = 1.078 95% CI: 0.992–1.172) but only marginally significant (p < .10). In other words, for most groups, starting with a health advantage increases an individual’s risk of acquiring more impairment but decreases the chances of mortality.
Table 3.
Multinomial Logistic Regression Results From Models Predicting Health Outcomes for White Men and Women at Wave 13 of the HRS
| White Women | White Men | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Limitations Higher than First Observed | Died | Lost to Follow up | Limitations Higher than First Observed | Died | Lost to Follow up | |||||||
| Functional limitations Round 2 | 0.854*** | (0.812–0.897) | 1.062* | (1.014–1.113) | 0.884*** | (0.835–0.937) | 0.823*** | (0.765–0.886) | 1.076* | (1.011–1.145) | 0.916* | (0.846–0.991) |
| Birth Year | 0.927*** | (0.897–0.959) | 0.855*** | (0.825–0.886) | 0.959* | (0.924–0.995) | 0.904*** | (0.869–0.939) | 0.827*** | (0.797–0.857) | 0.930*** | (0.892–0.969) |
| Less than HS diploma | 1.460 | (0.997–2.137) | 1.762** | (1.170–2.652) | 2.049*** | (1.338–3.139) | 1.243 | (0.818–1.890) | 1.649* | (1.106–2.458) | 1.576* | (1.021–2.432) |
| Completed HS | 1.387* | (1.018–1.890) | 1.651** | (1.163–2.343) | 1.907*** | (1.341–2.713) | 1.440* | (1.029–2.014) | 1.410* | (1.016–1.956) | 1.403 | (0.977–2.016) |
| Some college | 1.526* | (1.094–2.128) | 1.368 | (0.934–2.003) | 1.444 | (0.976–2.136) | 1.148 | (0.804–1.639) | 1.756** | (1.255–2.457) | 1.556* | (1.072–2.258) |
| Ever smoked at Round 2 | 1.176 | (0.951–1.455) | 2.692*** | (2.155–3.364) | 1.169 | (0.925–1.478) | 1.203 | (0.930–1.555) | 2.052*** | (1.590–2.650) | 1.183 | (0.899–1.557) |
| Married at Round 2 | 0.767* | (0.590–0.998) | 0.752* | (0.577–0.982) | 0.769 | (0.578–1.025) | 1.229 | (0.858–1.760) | 0.690* | (0.501–0.951) | 0.803 | (0.560–1.150) |
| First Wealth Quintile (Lowest Wealth) | 1.796** | (1.179–2.736) | 2.857*** | (1.867–4.374) | 1.441 | (0.911–2.278) | 1.719* | (1.059–2.791) | 2.594*** | (1.660–4.053) | 0.960 | (0.569–1.620) |
| Second Wealth Quintile | 1.438* | (1.012–2.042) | 2.217*** | (1.536–3.198) | 1.023 | (0.689–1.518) | 1.352 | (0.905–2.019) | 2.191*** | (1.505–3.188) | 1.234 | (0.814–1.872) |
| Third Wealth Quintile | 1.242 | (0.907–1.699) | 1.911*** | (1.368–2.668) | 1.376 | (0.974–1.944) | 1.405 | (0.988–1.996) | 1.624** | (1.157–2.279) | 1.102 | (0.761–1.598) |
| Fourth Wealth Quintile | 1.062 | (0.795–1.419) | 1.460* | (1.059–2.011) | 1.157 | (0.842–1.589) | 1.129 | (0.821–1.553) | 1.452* | (1.065–1.978) | 1.079 | (0.770–1.513) |
| No longest occupation | 1.295 | (0.895–1.874) | 1.509* | (1.052–2.164) | 1.428 | (0.963–2.117) | 0.969 | (0.605–1.552) | 1.165 | (0.755–1.797) | 0.885 | (0.537–1.459) |
| Longest occupation professional, managerial, clerical or sales | 1.232 | (0.935–1.624) | 0.920 | (0.695–1.218) | 1.003 | (0.743–1.354) | 0.858 | (0.638–1.155) | 0.835 | (0.632–1.105) | 0.731* | (0.539–0.993) |
| 3662 | 3317 | |||||||||||
Notes: Relative Risk Ratios; Confidence interval in parentheses.
* p < .05” **p < .01 ***p < .0001.
Table 4.
Multinomial Logistic Regression Results From Models Predicting Health Outcomes for Black Men and Women at Wave 13 of the HRS
| Black Women | Black Men | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Limitations Higher than First Observed | Died | Lost to Follow up | Limitations Higher than First Observed | Died | Lost to Follow up | |||||||
| Functional Limitations Round 2 | 0.822*** | (0.749–0.902) | 1.078 | (0.992–1.172) | 0.921 | (0.833–1.018) | 0.917 | (0.792–1.062) | 1.128* | (1.015–1.254) | 0.998 | (0.842–1.182) |
| Birth year | 0.889** | (0.829–0.954) | 0.807*** | (0.753–0.865) | 0.862*** | (0.795–0.935) | 0.854** | (0.774–0.942) | 0.788*** | (0.722–0.860) | 0.868* | (0.775–0.972) |
| Less than HS diploma | 0.567 | (0.216–1.488) | 0.725 | (0.274–1.921) | 0.732 | (0.246–2.173) | 1.293 | (0.313–5.333) | 0.733 | (0.193–2.785) | 0.719 | (0.157–3.294) |
| Completed HS | 0.511 | (0.203–1.286) | 0.556 | (0.220–1.406) | 0.729 | (0.264–2.013) | 0.945 | (0.229–3.893) | 0.725 | (0.190–2.766) | 0.525 | (0.118–2.337) |
| Some college | 0.701 | (0.278–1.765) | 0.704 | (0.271–1.832) | 0.655 | (0.230–1.865) | 0.843 | (0.190–3.739) | 0.685 | (0.174–2.704) | 0.658 | (0.146–2.967) |
| Ever smoked at Round 2 | 1.448 | (0.908–2.308) | 2.143*** | (1.362–3.373) | 1.352 | (0.799–2.289) | 1.159 | (0.605–2.222) | 2.387** | (1.327–4.295) | 1.382 | (0.671–2.849) |
| Married at Round 2 | 1.273 | (0.774–2.096) | 1.388 | (0.846–2.277) | 1.314 | (0.745–2.319) | 1.245 | (0.570–2.723) | 0.654 | (0.339–1.261) | 0.977 | (0.424–2.248) |
| First Wealth Quintile (Lowest Wealth) | 1.122 | (0.347–3.629) | 1.424 | (0.447–4.539) | 0.785 | (0.219–2.817) | 1.506 | (0.384–5.900) | 2.399 | (0.614–9.369) | 0.257 | (0.057–1.151) |
| Second Wealth Quintile | 0.954 | (0.301–3.022) | 1.165 | (0.369–3.673) | 0.917 | (0.262–3.203) | 1.071 | (0.287–3.988) | 1.634 | (0.438–6.098) | 0.821 | (0.222–3.035) |
| Third Wealth Quintile | 1.271 | (0.392–4.120) | 1.104 | (0.336–3.631) | 1.089 | (0.296–4.000) | 0.945 | (0.241–3.704) | 1.651 | (0.433–6.301) | 0.279 | (0.070–1.117) |
| Fourth Wealth Quintile | 0.868 | (0.255–2.954) | 0.474 | (0.133–1.681) | 0.344 | (0.083–1.436) | 0.846 | (0.218–3.285) | 0.957 | (0.251–3.653) | 0.519 | (0.138–1.952) |
| No longest occupation | 0.978 | (0.414–2.310) | 2.150 | (0.990–4.672) | 1.743 | (0.718–4.235) | 1.419 | (0.489–4.118) | 0.722 | (0.290–1.797) | 0.690 | (0.188–2.530) |
| Longest occupation professional, managerial, clerical or sales | 0.540* | (0.298–0.976) | 0.661 | (0.367–1.190) | 0.767 | (0.392–1.500) | 1.225 | (0.535–2.804) | 0.823 | (0.394–1.722) | 0.956 | (0.378–2.417) |
| 887 | 598 | |||||||||||
Notes: Relative Risk Ratios; Confidence intervals in parentheses.
* p < .05” **p < .01 ***p < .0001.
The association of social (dis)advantage and health change differs systematically by race and gender, suggesting that the findings above go beyond simple floor and ceiling effects. White women and men with less than a college education and those not in the highest wealth quintile are more likely to experience health declines or be lost to mortality relative to remaining in the sample at the same or better health. However, no such education–health or wealth–health gradient is observed for Black men and women. Relative to working in a “non-office” occupation, reporting no longest held occupation is associated with an elevated risk of mortality for White women (RR = 1.509; 95% CI: 1.052–2.164). For Black women, being in an “office” occupation is associated with a lower risk of subsequent health declines (RR = 0.540; 95% CI: 0.298–0.976). For White men and Black men, there are no statistically significant associations between occupation and morbidity or mortality. Being married is another factor that seems to operate differently by race and gender. For White women, being married reduces the risk of health declines (RR = 0.767; 95% CI: 0.590–0.998) and mortality (RR = 0.752; 95% CI: 0.577–0.982) relative to staying at the same or better health. For White men, being married is not associated with the likelihood of health change but does reduce the risk of being lost to mortality (RR = 0.690; 95% CI: 0.501–0.951). Finally, for Black men and women, there are no associations between marital status and subsequent health change or mortality risk. Smoking is the only behavioral factor that appears to operate similarly across race gender groups—for all respondents, having ever smoked is not associated with functional health but does substantially increase risk of mortality.
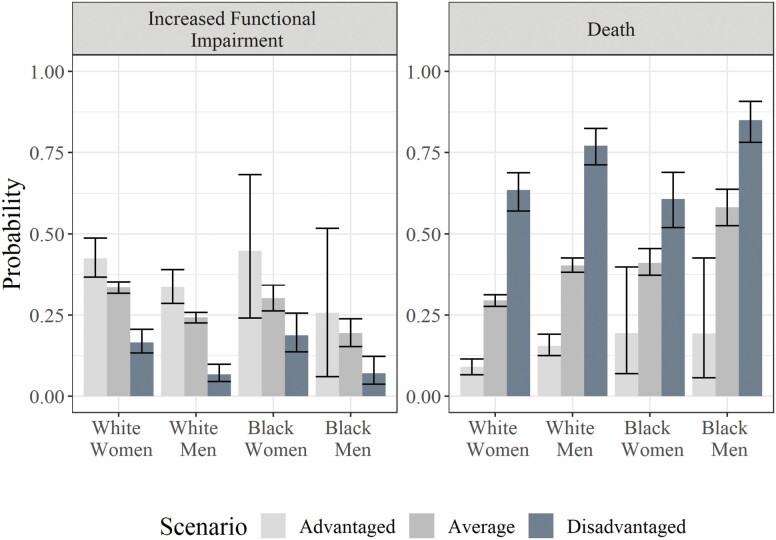
Relative associations may obscure systematic differences in outcomes across health statuses, social positions, race, and gender. To address this concern, we use coefficients from the multinomial logistic regression models to calculate predicted probabilities of outcomes for the race-gender group average and for profiles of concentrated health and social (dis)advantage (See Supplementary Table A2 for a full listing of calculated probabilities). Figure 1 provides further evidence of an impairment paradox: The groups and scenarios with the most advantages often show the highest probabilities of experiencing an increase in functional limitation but the lowest probability of mortality.
Figure 1.
Predicted probability of having an increase in limitations or dying as calculated from multinomial logistic regression models stratified by race and gender. The predicted probability is on the y axis and the race gender group is on the x axis. Probabilities from the advantaged scenario are shaded in light gray; probabilities from the averaged scenario are shaded in gray; the probabilities from the disadvantaged scenario are shaded in dark gray. The error bars reflect 95% confidence intervals calculated via bootstrapping.
At the group averages, White women have the highest probability of experiencing an increase in functional impairment (0.335; 95% CI: 0.317–0.352) but the lowest risk of mortality (0.295; 95% CI: 0.276–0.312). Conversely, Black men have the lowest risk of experiencing an increase in limitation (0.194; 95% CI: 0.153–0.238) but the highest risk of mortality (0.582; 95% CI: 0.525–0.638). In comparison, under a scenario of concentrated socioeconomic and health advantage, all race-gender groups experience increased limitations and lower mortality. Differences in probabilities between the average and advantaged scenarios are larger for Black men and women, reflecting greater levels of health and social disadvantage on average. When social and health advantages are applied consistently, inequality by race and gender persists—with the lowest risk of death (0.090; 0.066–0.115) for White women and the highest risk among Black women and men (0.194; 95% CI: 0.070–0.399 for Black women; 0.193; 95% CI: 0.057–0.426). The confidence intervals surrounding these predicted probabilities are quite wide for Black respondents, reflecting the small sample for whom such advantages are observed.
Conversely, when exposed to concentrated disadvantage, the probability of experiencing a health decline is lower than average for all race and gender groups. Strikingly, for all race and gender groups with disadvantaged health and social positions, the probability of death is higher than that of survival in poorer functional health. Furthermore, race differences persist, with a high probability of death for White and Black women (0.635; 95% CI: 0.571–0.688 for White women; 0.607; 95% CI: 0.520–0.689 for Black women), and an even higher one for Black men (0.850; 95% CI: 0.782–0.907).
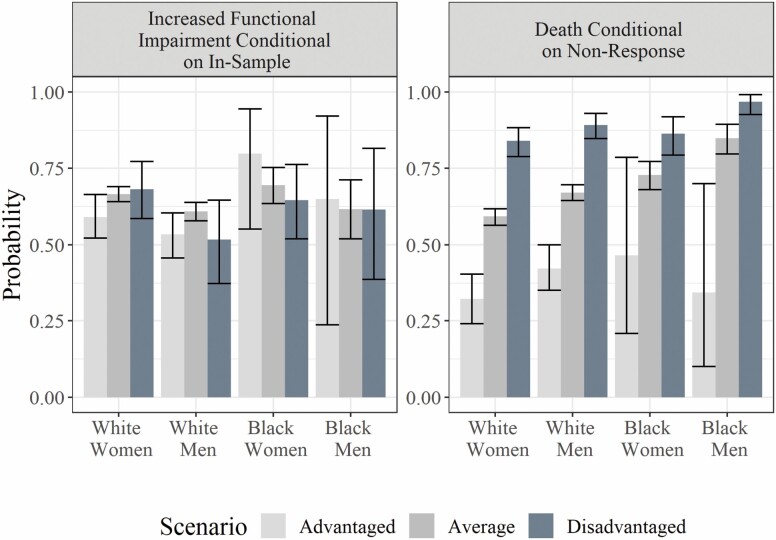
While social and health advantages protect against mortality, they do not necessarily decrease the probability of experiencing an increase in limitations for those who remain in the study. As shown in Figure 2, there is significant heterogeneity across groups in the association of concentrated (dis)advantage and subsequent increases in functional limitations. Changes in the conditional probabilities of observed health declines are much smaller and more ambiguous than the changes in mortality in response to the same conditions.
Figure 2.
Predicted probability of having an increase in limitations conditional on remaining in-sample or dying conditional on non-response as calculated from multinomial logistic regression models stratified by race and gender. The predicted probability is on the y axis and the race gender group is on the x axis. Probabilities from the advantaged scenario are shaded in light gray; probabilities from the averaged scenario are shaded in gray; the probabilities from the disadvantaged scenario are shaded in dark gray. The error bars reflect 95% confidence intervals calculated via bootstrapping.
Finally, the predicted probabilities point to inequalities in follow-up, and underscore the need to understand respondent outcomes—and variation by race and gender—following attrition. Conditional on attrition, the average White woman has the lowest probability (0.593; 95% CI: 0.564–0.618) and the average Black man has the highest probability (0.849; 95% CI: 0.797–0.894) of dying during the follow-up period. For the most advantaged, mortality decreases substantially although significant variation by race and gender remain. Among disadvantaged respondents lost to follow up, the probability of mortality converges across groups yet Black men still have the highest risk (0.968; 95% CI: 0.926–0.991).
To examine the sensitivity of our findings to the selectivity associated with respondents who are in the first and last survey rounds, we conducted 2 robustness checks. First, we reran the multinomial logistic models using outcomes halfway through the survey (Wave 6 instead of at Wave 13). Consistent with prior results, we find that having more functional limitations at baseline is associated with a lower risk of added impairment relative to remaining in sample with the same or better health for all groups but Black men and that socioeconomic gradients in health change and mortality operate only for White men and women (Supplementary Table A3). Second, we use a logistic regression to examine functional limitation change between the first and last observed round for the subgroup who remain in the HRS for 2 or more survey rounds. The results (Supplementary Table A4) are also consistent with prior findings from the multinomial logistic models; here we find that starting with more limitations is negatively associated with the likelihood of being last observed with more impairment for all groups including Black men.
Discussion
Our analysis shows that an observed increase in functional impairment in later life is, paradoxically, a marker of prior advantage. While previous studies informed by CAD theory and employing trajectory models are predicated on an expectation that baseline disparities in functional health will persist or widen, we consider functional health change, mortality, and loss to follow up as competing risks for individuals. We explore the implications of this “Punctuated Equilibrium” (8) in individual health histories for observed population health disparities at older ages. We find that those who enter midlife in poorer health are less likely to acquire additional impairments over time, but are more vulnerable to mortality. At the same time, a health advantage in midlife reduces mortality risk but increases the likelihood of subsequently experiencing a health decline.
We also find that, consistent with CAD theory, deleterious social and economic exposures earlier in the life course are strongly associated with poorer functional health in midlife and with higher mortality. However, exposures to and consequences of social (dis)advantage play out differently across groups defined by race and gender. In particular, higher educational attainment and wealth appeared protective for the health and mortality risk of White men and women but a similar educational and wealth gradient was not visible for Black men and women. One possible explanation is that for Black adults, the potential advantages of higher education or greater wealth are countered by other lifetime experiences of disadvantage rooted in racism. It is also possible that while economic advantage did matter for Black women and men’s health at earlier ages, the excess burden of premature mortality created a selected sample of survivors for whom the socioeconomic advantages were less significant
Taken together, our findings suggest that the leveling of racial and socioeconomic inequalities in later-life health is in fact a product of (rather than a departure from) ongoing processes of cumulative (dis)advantage. Differential exposure to (dis)advantage shapes later-life health inequities by impacting the composition of cohort members who survive into midlife and older ages. Differential impacts of earlier socioeconomic advantages by race and gender in turn create an unexpected dynamic: More advantaged individuals have a longer survival time during which to develop functional limitation.
Scholars of health disparities increasingly call for research that goes beyond documenting gaps by race, gender, and class to illuminating how structural forces such as racism, concentrated poverty and constrained economic opportunities, and experiences of discrimination and marginalization related to gender, race, class, disability status, and other characteristics create differential health and longevity outcomes across populations (1,48,49). A limitation of our study is that because the HRS only enrolls respondents starting in their 50s, we were unable to account for a complete set of lifetime exposures or account for mortality and health disparities that occurred prior to midlife. However, by adopting a punctuated equilibrium perspective (8) and recognizing continued survival (albeit with accumulated limitation) as a marker of advantage relative to earlier mortality our analysis provides an avenue for more clearly linking together stratification by race, gender, and class with later-life inequities in health.
Our findings suggest a need for equity-enhancing policies and programs to consider interventions on both survival and health change, as improvements on both fronts are needed. The greater variability in the impact of upstream factors relative to the impact of smoking suggest that social determinants are likely more powerful levers for influencing population health relative to health behaviors. Addressing later-life functional health without considering differential survival will not be sufficient for eliminating racial disparities, and may even contribute to widening them. Furthermore, interventions that reduce premature mortality may increase the survivorship of persons in relatively poorer functional health, creating the appearance of greater health disparities across groups even if such policies in fact increase equity in survival. Finally, the differential relationship of socioeconomic factors with health change and mortality by race and gender points to a need for health equity policies to encompass broader, multifaceted interventions that address systemic racism jointly with socioeconomic disadvantage. To truly achieve health equity in later life, such interventions must begin at younger ages and be sustained throughout in the life course.
Supplementary Material
Funding
This research was supported by the Steven H. Sandell Grant Program for Junior Scholars in Retirement Research, the Network on Life Course Health Dynamics and Disparities in 21st Century America (NIA R24AG045061), the Center for Demography of Health and Aging (NIA P30 AG17266) at the University of Wisconsin–Madison, and the Eunice Kennedy Shriver National Center for Child Health and Human Development grant (P2C-HD041041). The funders had no role in the design of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Conflict of Interest
None declared.
References
- 1. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 2. Brown TH. Racial stratification, immigration, and health inequality: a life course-intersectional approach. Soc Forces. 2018;96:1507–1540. doi: 10.1093/sf/soy013 [DOI] [Google Scholar]
- 3. Kim J, Miech R. The Black–White difference in age trajectories of functional health over the life course. Soc Sci Med. 2009;68:717–725. doi: 10.1016/j.socscimed.2008.12.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lynch SM, Brown JS, Harmsen KG. Black-white differences in mortality compression and deceleration and the mortality crossover reconsidered. Res Aging. 2003;25:456–483. doi: 10.1177/0164027503254675 [DOI] [Google Scholar]
- 5. DiPrete TA, Eirich GM. Cumulative advantage as a mechanism for inequality: A review of theoretical and empirical developments. Annu Rev Sociol. 2006;32:271–297. doi: 10.1146/annurev.soc.32.061604.123127 [DOI] [Google Scholar]
- 6. Ferraro KF, Shippee TP. Aging and cumulative inequality: how does inequality get under the skin? Gerontologist. 2009;49:333–343. doi: 10.1093/geront/gnp034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(1_suppl2):19–31. doi: 10.1177/00333549141291S206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Engelman M, Jackson H. Gradual change, homeostasis, and punctuated equilibrium: reconsidering patterns of health in later life. Demography. 2019;56:2323–2347. doi: 10.1007/s13524-019-00826-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. O’Rand AM. The precious and the precocious: understanding cumulative disadvantage and cumulative advantage over the life course. Gerontologist. 1996;36:230–238. doi: 10.1093/geront/36.2.230 [DOI] [PubMed] [Google Scholar]
- 10. Crystal S, Shea D. Cumulative advantage, cumulative disadvantage, and inequality among elderly people. Gerontologist. 1990;30:437–443. doi: 10.1093/geront/30.4.437 [DOI] [PubMed] [Google Scholar]
- 11. Dannefer D. Cumulative advantage/disadvantage and the life course: cross-fertilizing age and social science theory. J Gerontol B Psychol Sci Soc Sci. 2003;58:S327–S337. doi: 10.1093/geronb/58.6.S327 [DOI] [PubMed] [Google Scholar]
- 12. Kemp BR, Ferraro KF. Are biological consequences of childhood exposures detectable in telomere length decades later? J Gerontol A Biol Sci Med Sci 2021;76:7–14. doi: 10.1093/gerona/glaa019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Taylor MG, Min SN, Reid KM. Cumulative inequality at the end of life?: racial disparities in impairment in the time before death. J Gerontol B Psychol Sci Soc Sci. 2020;75:1292–1301. doi: 10.1093/geronb/gby129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gueorguieva R, Sindelar JL, Falba TA, et al. The impact of occupation on self-rated health: cross-sectional and longitudinal evidence from the health and retirement survey. J Gerontol B Psychol Sci Soc Sci. 2009;64:118–124. doi: 10.1093/geronb/gbn006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980–2015. Lancet. 2017;389:1475–1490. doi: 10.1016/S0140-6736(17)30571-8 [DOI] [PubMed] [Google Scholar]
- 16. Pollack CE, Chideya S, Cubbin C, Williams B, Dekker M, Braveman P. Should health studies measure wealth?: a systematic review. Am J Prev Med. 2007;33:250–264. doi: 10.1016/j.amepre.2007.04.033 [DOI] [PubMed] [Google Scholar]
- 17. Brown TH, Richardson LJ, Hargrove TW, Thomas CS. Using multiple-hierarchy stratification and life course approaches to understand health inequalities: the intersecting consequences of race, gender, SES, and age. J Health Soc Behav. 2016;57:200–222. doi: 10.1177/0022146516645165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hakulinen C, Pulkki-R\aaback L, Jokela M, et al. Structural and functional aspects of social support as predictors of mental and physical health trajectories: Whitehall II cohort study. J Epidemiol Community Health. 2016;70:710–715. doi: 10.1136/jech-2015-206165 [DOI] [PubMed] [Google Scholar]
- 19. Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–398. doi: 10.1016/0277-9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- 20. Quiñones AR, Liang J, Bennett JM, Xu X, Ye W. How does the trajectory of multimorbidity vary across Black, White, and Mexican Americans in middle and old age? J Gerontol B Psychol Sci Soc Sci. 2011;66:739–749. doi: 10.1093/geronb/gbr106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liang J, Xu X, Bennett JM, Ye W, Quiñones AR. Ethnicity and changing functional health in middle and late life: a person-centered approach. J Gerontol B Psychol Sci Soc Sci. 2010;65:470–481. doi: 10.1093/geronb/gbp114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brown TH, O’Rand AM, Adkins DE. race-ethnicity and health trajectories tests of three hypotheses across multiple groups and health outcomes. J Health Soc Behav. 2012;53:359–377. doi: 10.1177/0022146512455333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cullati S, Rousseaux E, Gabadinho A, Courvoisier DS, Burton-Jeangros C. Factors of change and cumulative factors in self-rated health trajectories: a systematic review. Adv Life Course Res. 2014;19:14–27. doi: 10.1016/j.alcr.2013.11.002 [DOI] [PubMed] [Google Scholar]
- 24. Ferraro KF, Schafer MH, Wilkinson LR. Childhood disadvantage and health problems in middle and later life: early imprints on physical health? Am Sociol Rev. 2016;81:107–133. doi: 10.1177/0003122415619617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gill TM, Gahbauer EA, Han L, Allore HG. Trajectories of disability in the last year of life. N Engl J Med. 2010;362:1173–1180. doi: 10.1056/NEJMoa0909087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. O’Rand AM, Henretta JC.. Age and Inequality: Diverse Pathways through Later Life. Westview Press; 1999. [Google Scholar]
- 27. Dannefer D. Systemic and reflexive: foundations of cumulative dis/advantage and life-course processes. J Gerontol B Psychol Sci Soc Sci. 2020;75:1249–1263. doi: 10.1093/geronb/gby118 [DOI] [PubMed] [Google Scholar]
- 28. Hoffmann R. Illness, not age, is the leveler of social mortality differences in old age. J Gerontol B Psychol Sci Soc Sci. 2011;66:374–379. doi: 10.1093/geronb/gbr014 [DOI] [PubMed] [Google Scholar]
- 29. Taylor MG. Capturing transitions and trajectories: The role of socioeconomic status in later life disability. J Gerontol B Psychol Sci Soc Sci. 2010;65:733–743. doi: 10.1093/geronb/gbq018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Herd P. Do functional health inequalities decrease in old age? Educational status and functional decline among the 1931–1941 birth cohort. Res Aging. 2006;28:375–392. doi: 10.1177/0164027505285845 [DOI] [Google Scholar]
- 31. Vaupel JW, Yashin AI. Heterogeneity’s ruses: some surprising effects of selection on population dynamics. Am Stat. 1985;39:176–185. doi: 10.2307/2683925 [DOI] [PubMed] [Google Scholar]
- 32. Zheng H. Unobserved population heterogeneity and dynamics of health disparities. Demogr Res. 2020;43:1009–1048. doi: 10.4054/DemRes.2020.43.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- 34. Haas S, Rohlfsen L. Life course determinants of racial and ethnic disparities in functional health trajectories. Soc Sci Med. 2010;70:240–250. doi: 10.1016/j.socscimed.2009.10.003 [DOI] [PubMed] [Google Scholar]
- 35. Jackson H, Engelman M, Bandeen-Roche K. Robust respondents and lost limitations: the implications of nonrandom missingness for the estimation of health trajectories. J Aging Health. 2019;31:685–708. doi: 10.1177/0898264317747079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. DiPrete TA, Buchmann C. Gender-specific trends in the value of education and the emerging gender gap in college completion. Demography. 2006;43:1–24. doi: 10.1353/dem.2006.0003 [DOI] [PubMed] [Google Scholar]
- 37. Lillard LA, Waite LJ. ‘Til death do us part: marital disruption and mortality. Am J Sociol. 1995;100:1131–1156. doi: 10.1086/230634# [DOI] [Google Scholar]
- 38. Rogers RG. Marriage, sex, and mortality. J Marriage Fam. 1995;57:515–526. doi: 10.2307/353703 [DOI] [Google Scholar]
- 39. Brown LL, Mitchell UA, Ailshire JA. Disentangling the stress process: race/ethnic differences in the exposure and appraisal of chronic stressors among older adults. J Gerontol B Psychol Sci Soc Sci. 2020;75:650–660. doi: 10.1093/geronb/gby072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pathak EB. Mortality among black men in the USA. J Racial Ethn Health Disparities. 2018;5:50–61. doi: 10.1007/s40615-017-0341-5 [DOI] [PubMed] [Google Scholar]
- 41. Erving CL, Satcher LA, Chen Y. Psychologically resilient, but physically vulnerable? Exploring the psychosocial determinants of African American women’s mental and physical health. Sociol Race Ethn. 2021;7:116–133. doi: 10.1177/2332649219900284 [DOI] [Google Scholar]
- 42. Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. 2014;110:10–17. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 43. Juster FT, Suzman R. An overview of the Health and Retirement Study. J Hum Resour. 1995;30:S7–S56. doi: 10.2307/146277 [DOI] [Google Scholar]
- 44.HRS Staff. https://hrs.isr.umich.edu/sites/default/files/biblio/ResponseRates_2017.pdf Sample Sizes and Response Rates.
- 45. Bugliari D, Campbell N, Chan C, et al. RAND HRS longitudinal file 2016 (V1) documentation. St Monica CA RAND Cent Study Aging. Published online 2019. https://www.rand.org/content/dam/rand/www/external/labor/aging/dataprod/randhrs1992_2018v1.pdf [Google Scholar]
- 46. Waite LJ. Marital history and well-being in later life. In: Uhlenberg P, ed. International Handbook of Population Aging. Springer; 2009:691–704. doi: 10.1007/978-1-4020-8356-3_31 [DOI] [Google Scholar]
- 47. Efron B, Tibshirani R. Bootstrap methods for standard errors, confidence intervals, and other measures of statistical accuracy. Stat Sci. 1986;1:54–75. doi: 10.1214/ss/1177013815 [DOI] [Google Scholar]
- 48. Health WC on SD of, Organization WH. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health: Commission on Social Determinants of Health Final Report. Commission on Social Determinants of Health. World Health Organization; 2008. https://www.who.int/publications/i/item/WHO-IER-CSDH-08.1 [Google Scholar]
- 49. Grollman EA. Multiple disadvantaged statuses and health: the role of multiple forms of discrimination. J Health Soc Behav. 2014;55:3–19. doi: 10.1177/0022146514521215 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.