Abstract
Unilateral pulmonary edema after minimally invasive cardiac surgery is a rare, but potentially life-threatening condition. However, the exact causes of unilateral pulmonary edema remain unclear. We experienced aggressive unilateral pulmonary edema followed by redo-resection of recurrent left atrial myxoma through a right mini-thoracotomy. Intraoperative veno-venous extracorporeal membrane oxygenation was applied after the termination of cardiopulmonary bypass, and separate mechanical ventilation using a double-lumen endotracheal tube was applied after surgery. The patient was successfully treated and discharged uneventfully.
Keywords: Surgical operation, Minimally invasive surgery, Case report
Case report
A 46-year-old woman with a history of hypertension, diabetes mellitus, and atrial flutter was referred for reoperation due to recurrent left atrial myxoma. She had undergone myxoma resection via median sternotomy at Yeungnam University Medical Center 4 years earlier. The laboratory findings were within the normal ranges. Echocardiography demonstrated a recurrence of left atrial myxoma. A visible, round, mobile echogenic mass (1.65×1.53 cm) was attached at the left side of the interatrial septum with preserved left ventricular function.
After anesthetic induction with a double-lumen endotracheal tube (DLT), the surgical procedure was performed through the right fourth anterolateral intercostal space with a 6-cm skin incision. At the time of entrance into the right pleural cavity, single-lung ventilation was initiated, and multiple pericardial tagging sutures were fixed to the skin incision site after opening the pericardium. Cardiopulmonary bypass (CPB) was established via the right femoral artery and vein. The additional cannula for the superior vena cava was inserted percutaneously via the right internal jugular vein. After the full establishment of CPB, lung ventilation was stopped. Cardiac arrest was obtained by administering an antegrade cardioplegic solution through a catheter inserted into the aortic root after direct aortic cross-clamping (ACC), and the thoracic cavity was filled with carbon dioxide. The myxoma was surgically removed from the interatrial septum, and the septal defect was repaired with bovine pericardium after a Cox maze IV procedure with cryoablation. The intraoperative course was uneventful. Ventilation was restarted during weaning from CPB. The CPB time was 321 minutes, and the ACC time was 166 minutes. Some time was necessary before ACC to release the periaortic adhesions cautiously and after ACC to manage hypoxia.
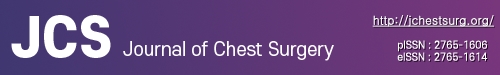
During weaning from CPB, hypoxia abruptly developed, and the patient’s vital signs became unstable. When checked with a fiber-optic bronchoscope, a continuous serous discharge from the right bronchus was observed (no discharge was observed on the left side) (Fig. 1). We maintained the DLT to prevent secretions from flooding from the right side to the left side, and veno-venous extracorporeal membrane oxygenation (ECMO) was applied to maintain oxygen saturation. After ECMO application, the patient’s vital signs rapidly stabilized, and she was transferred to the intensive care unit with the DLT and veno-venous ECMO. Unilateral pulmonary edema (UPE) was identified on a postoperative chest X-ray examination (Fig. 2A). After massive diuresis, serous discharge from the right side of the DLT gradually decreased and the tidal volume progressively increased. Veno-venous ECMO was removed after 63 hours. The total intubation time was 108 hours. DLT ventilation was used for 46 hours and then changed to a single lumen. The patient was transferred to the general ward on postoperative day 7 and was discharged on postoperative day 19 (Fig. 2B). The patient provided written informed consent for the publication of the clinical details and images.
Fig. 1.
Intraoperative bronchoscopic image shows massive fluid collection filling up and puddling in the right side of the double-lumen endotracheal tube, like “water in the well.” Written informed consent for publication of this image was obtained from the patient.
Fig. 2.
These images show immediate (A) postoperative and (B) pre-discharge chest X-rays. (A) The immediate postoperative chest X-ray shows a totally hazy right lung field, corresponding to the approached side, but the left side was relatively normal. (B) A pre-discharge chest X-ray shows the disappearance of lung haziness.
R, right; L, left; AP, anterior-posterior.
Discussion
UPE after minimally invasive cardiac surgery (MICS) is a rare but potentially catastrophic complication unless proper management is applied. The incidence varies from study to study. The reported incidence of radiographically evident UPE after MICS was 5.0%–7.9%, and that of symptomatic UPE after MICS was reported to be 1.5% or “rare” [1,2]. As the number of MICS procedures has increased, reports related to UPE after MICS have increased as well.
The pathogenesis and risk factors for UPE after MICS are not clear. The possible suggested risk factors of UPE after MICS include long CPB time, diabetes, chronic obstructive pulmonary disease, right ventricular dysfunction, high pulmonary artery pressure, intraoperative fresh frozen plasma transfusion, and a high perioperative C-reactive protein level [3,4].
UPE after MICS may occur mainly by pulmonary ischemia-reperfusion injury and an inflammatory response to CPB. Ischemia-reperfusion injury damages the microvasculature with the release of multiple proinflammatory cytokines, released oxygen free radicals, and upregulation of cell surface adhesion molecules on the lung endothelium [5]. These can increase pulmonary vascular resistance, microvascular permeability, and pulmonary edema, making alveolar gas exchange worse.
In our case, massive serous secretions were aspirated through the endotracheal tube, which led to unstable hemodynamics with hypoxia. Based on our experience, ECMO should be considered immediately after UPE is confirmed intraoperatively or if the patient is unstable hemodynamically. DLT should be maintained to prevent contralateral aspiration. While maintaining ECMO and using separate ventilation with a DLT, massive diuresis may also be helpful. We believe that using separate ventilation with a DLT could be the cornerstone for preserving the contralateral lung from aspiration and shortening the hospital stay. Finally, we suggest maintaining positive end-expiratory pressure to prevent the total collapse of the right lung during CPB to minimize the possibility of re-expansion pulmonary edema.
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Yamashiro S, Arakaki R, Kise Y, Kuniyoshi Y. Prevention of pulmonary edema after minimally invasive cardiac surgery with mini-thoracotomy using neutrophil elastase inhibitor. Ann Thorac Cardiovasc Surg. 2018;24:32–9. doi: 10.5761/atcs.oa.17-00102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keyl C, Staier K, Pingpoh C, et al. Unilateral pulmonary oedema after minimally invasive cardiac surgery via right anterolateral minithoracotomy. Eur J Cardiothorac Surg. 2015;47:1097–102. doi: 10.1093/ejcts/ezu312. [DOI] [PubMed] [Google Scholar]
- 3.Moss E, Halkos ME, Binongo JN, Murphy DA. Prevention of unilateral pulmonary edema complicating robotic mitral valve operations. Ann Thorac Surg. 2017;103:98–104. doi: 10.1016/j.athoracsur.2016.05.100. [DOI] [PubMed] [Google Scholar]
- 4.Renner J, Lorenzen U, Borzikowsky C, et al. Unilateral pulmonary oedema after minimally invasive mitral valve surgery: a single-centre experience. Eur J Cardiothorac Surg. 2018;53:764–70. doi: 10.1093/ejcts/ezx399. [DOI] [PubMed] [Google Scholar]
- 5.den Hengst WA, Gielis JF, Lin JY, Van Schil PE, De Windt LJ, Moens AL. Lung ischemia-reperfusion injury: a molecular and clinical view on a complex pathophysiological process. Am J Physiol Heart Circ Physiol. 2010;299:H1283–99. doi: 10.1152/ajpheart.00251.2010. [DOI] [PubMed] [Google Scholar]