Abstract
Surgical treatment of primary and recurrent volar radial wrist–forearm ganglia has yielded higher recurrence rates of ganglia when compared to surgical treatment of dorsal wrist ganglia. The published surgical literature hypothesizes that the variability in etiology of volar radial wrist–forearm ganglia may account for the higher surgical recurrence rates of these ganglia. Currently, the literature states that volar radial wrist–forearm ganglia may be secondary to arthritic intercarpal joints, carpal interosseous ganglia, or by mechanical stress within tendon sheaths, joint capsules, and ligaments. The literature has not reported pathology isolated to the flexor carpi radialis tendon and its tendon sheath at the volar trapezial fibro-osseous synovial sheath tunnel as a cause of volar radial wrist–forearm ganglia. This case series reports findings of pathology isolated to the flexor carpi radialis tendon at the trapezial fibro-osseous synovial sheath tunnel that caused primary and recurrent volar radial wrist–forearm ganglia. The pathology identified in this case series hypothesizes an additional etiologic factor in development of volar radial wrist–forearm ganglia. Surgeon awareness of potential pathology of the flexor carpi radialis tendon at the trapezial fibro-osseous synovial sheath tunnel may reduce recurrence rates of volar radial wrist–forearm ganglia treated by surgical intervention.
Keywords: Ganglion, volar, radial, wrist–forearm, tendon, sheath, surgery, sports medicine
Introduction
Ganglions are the most common tumor of the hand and wrist, and when they are symptomatic, surgical treatment may be necessary.1–4 The surgical treatment of volar radial wrist–forearm ganglion may result in higher recurrence rates than surgical treatment of dorsal wrist ganglia. This may be attributed to variable origins of volar radial wrist–forearm ganglia and to flexor carpi radialis (FCR) tendinopathy.1–10 Nonetheless, the proven etiology of hand, wrist, and forearm ganglia remains unknown. The literature has not specifically identified pathology isolated to the FCR tendon and sheath at the trapezial fibro-osseous synovial sheath tunnel (TFOSST) that may cause volar radial wrist–forearm ganglia. The ganglia of the FCR tendon and sheath may clinically manifest at various locations from the trapezium distally to the radial volar forearm proximally. This surgical case series, over a duration of 8.5 years, by a single hand surgeon includes nine patients with pathology identified and isolated to the FCR tendon and sheath at the TFOSST that resulted in either primary or recurrent volar radial wrist–forearm ganglion.
Case series
All patients or their authorized representative assented and submitted signed written informed consents for their anonymized information to be used in this research of nine cases of symptomatic primary and recurrent volar radial wrist–forearm ganglions that were evaluated, treated, and followed by a single hand surgeon. One case in this series was followed over 9 years, one case over 6 years, one case over 5 years, one case over 4 years, three cases over 3 years, and two cases over 2 years. The mean follow-up of the nine cases was 4.8 years. The unique intra-operative findings of these cases prompted a MEDLINE literature search from 1968 to 2020 using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) tool to better understand the anatomy and etiology of FCR tendon and sheath ganglia. This case series included seven females of ages 19, 32, 39, 43, 44, 53, and 71 years, and two males of ages 20 and 51 years, respectively. All patients were evaluated by physical examination and X-rays, and all patients were without radiographic evidence of arthritis. All but one of the cases had visible ganglia in the volar radial wrist or distal forearm with one occult ganglion diagnosed by magnetic resonance imaging (MRI) in the region of the volar radial palm at the TFOSST (Figure 1). Two of the nine cases of ganglions treated by surgical excision were recurrent. One in a female patient and one in a male patient, and the remaining seven cases were primary ganglions. Of the recurrent ganglion cases, one was a female aged 71 years who had two previous excisions of the same volar radial wrist–forearm ganglion with each ganglion reoccurring within 2 months after surgery prompting referral to a hand surgeon. This patient’s initial ganglion and its recurrent ganglion remained in the same location as the original primary ganglion, and both were located along the FCR tendon from the distal volar wrist crease proximal to the carpus of the hand extending into the proximal forearm (Figure 2). There was no physical evidence of the ganglion being present in the carpus of the hand; however, on physical examination, there was pain localized to the volar trapezium on physical palpation with a normal X-ray of the wrist. Prior to a third surgical intervention, a pre-operative non-contrast MRI of the patient revealed that the physically visible forearm ganglion extended along the FCR tendon into the volar trapezium of the hand (Figure 3). Intra-operative inspection in all patients of this series did not reveal arthritic intercarpal joints, carpal interosseous ganglia, mucinous fistula, or joint capsular disruptions as reported in the surgical literature. The ganglions were dissected from the FCR tendon and traced to the trapezial TFOSST. The excised soft tissues were sent to pathology confirming ganglion material.
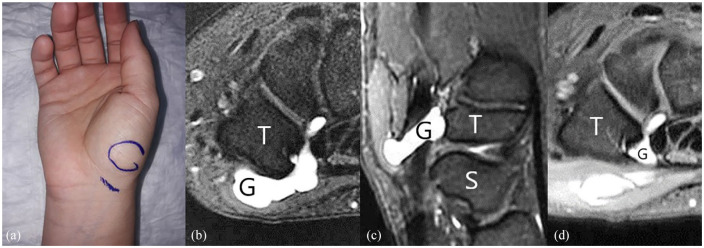
Figure 1.
(a) A 19-year-old female with occult symptomatic ganglion at drawn circle. (b, c, and d) Diagnosed by non-contrast T1 STIR MRI images—ganglion (G), scaphoid (S), and trapezium (T).
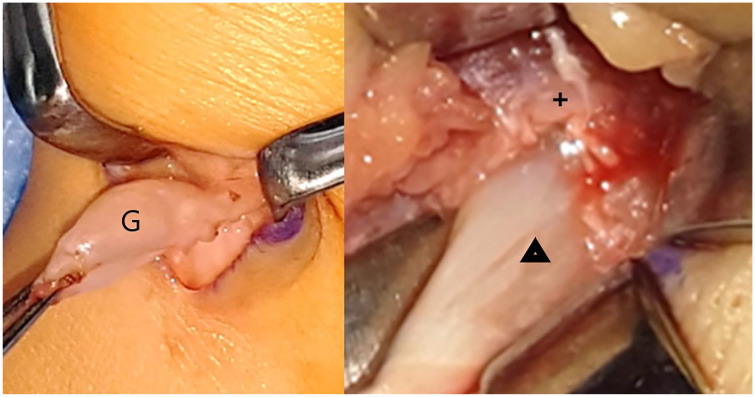
Figure 2.
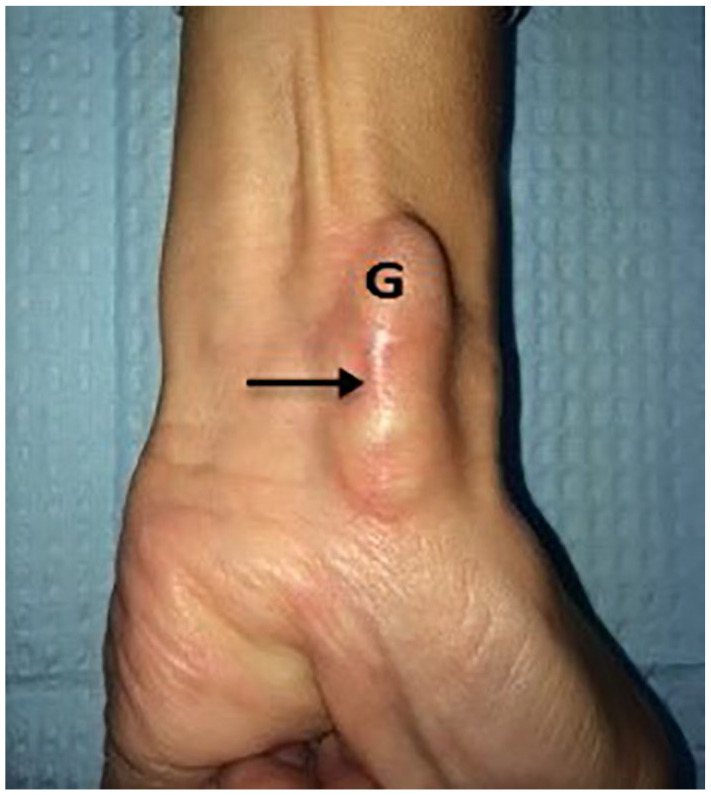
A 71-year-old female with recurrent ganglion (G). Note the surgical scar at arrow in distal forearm to distal wrist crease.
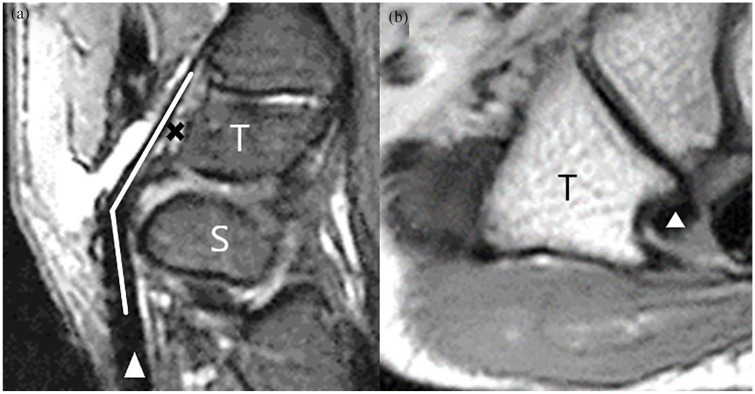
Figure 3.
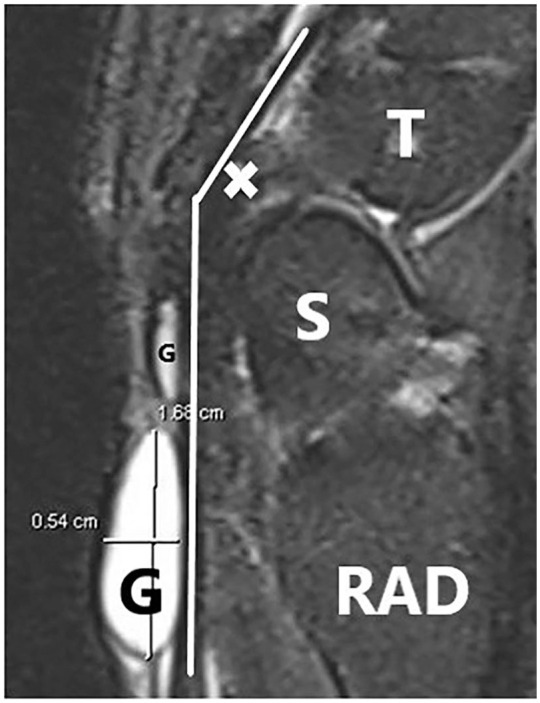
A 71-year-old female T1 STIR MRI lateral images with (x) identifying intra-operative origin of ganglion at TFOSST crest—ganglion (G), radius (RAD), scaphoid (S), trapezium (T), and white line is route of flexor carpi radialis tendon to metacarpal insertion.
In all cases, there were no slips of FCR tendon inserting into the trapezium or the scaphoid, and the posterior dorsal trapezial sulci appeared normal and exhibited white glistening surface typical of true synovial sheaths. 5 Intra-operatively, it was not possible to introduce or advance a 1.0 mm tip of a probe in between the anterior surface of the FCR tendon and the proximal internal surface of the TFOSST in any one of the nine cases. The TFOSST was measured after complete division using a probe that revealed an average length of approximately 2.1 cm from the volar proximal margin to the volar distal margin of the trapezium consistent with the published literature. 11 In all cases, the TFOSST proximal width corresponded with the width of the FCR tendon and measured approximately 0.8 cm from the proximal base of the radial trapezial crest to the proximal volar ulnar edge of the sheath. After complete division of the anterior volar ulnar TFOSST, the FCR tendon displaced from a posterior restrained position to about 3.0 mm anterior position and slightly ulnar toward the carpal tunnel with the wrist in neutral position consistent with the literature.12,13 There were prominent volar radial trapezial bone crests abutting against the FCR tendons in three cases with two in the recurrent ganglia and one in a primary ganglion causing deformity and attrition of the FCR tendon at the TFOSST (Figures 4–6). In these three cases, the prominent trapezial bone crests were excised, which also resulted in the complete division of the volar anterior portion of the TFOSST. Excision of these trapezial bone crests was accomplished using a rongeur extending deep into the trapezial cancellous bone body and deep to the posterior trapezial fibro-osseous synovial sheath and periosteal soft tissues. The defects caused by excision of the prominent trapezial crests were not covered with soft tissue as the defects were deep to the TFOSST posterior sheath soft tissue surfaces and did not create abutting sharp margins to cause attrition of the FCR tendons. All cases were done using local anesthetic surgical field block of 1% lidocaine with epinephrine mixed 1:1 with 0.5% Marcaine with epinephrine and sedation with tourniquet times averaging 30″. The surgical skin wounds were approximated with intradermal absorbable suture followed by the application of biocclussive dressings and removable volar-based wrist splints that were continued for 2 weeks if no bone excision was performed and continued for 6 weeks if trapezial bone crest excision was performed. No patient complained of pain in the immediate post-operative period. The patients were instructed to not remove or change biocclussive dressings for 7 days and were allowed to remove splints for personal hygiene to shower and wash hands in clean water with soap daily and as necessary.
Figure 4.
Left volar radial wrist ganglion (G) originating from trapezial fibro-osseous synovial sheath tunnel with deformed FCR tendon (Δ) with a prominent trapezial crest (+). Proximal at bottom of pictures and radial at left of pictures.
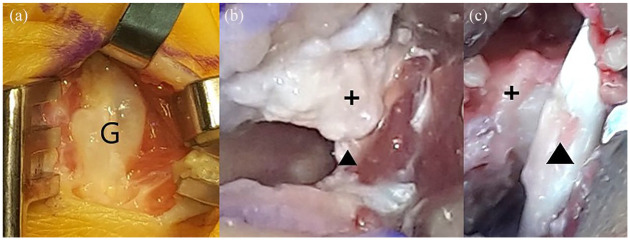
Figure 5.
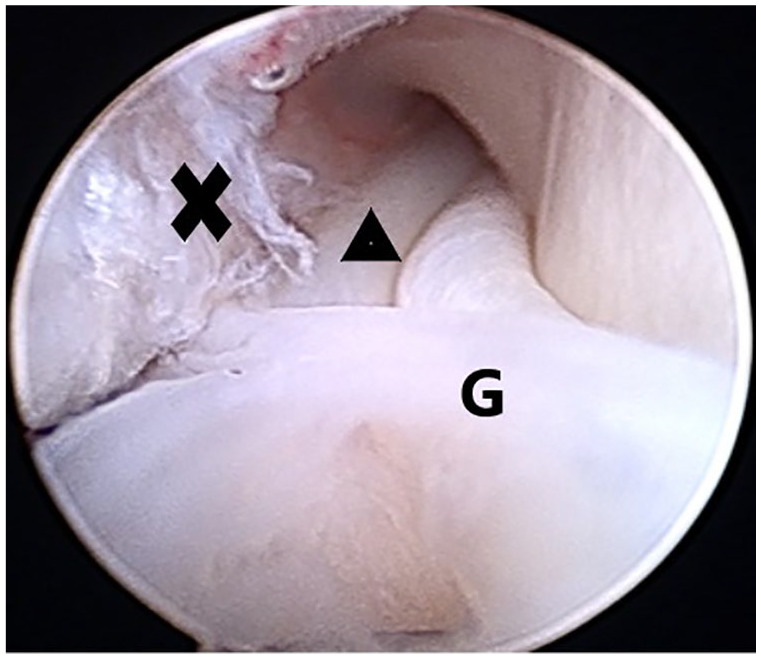
Arthroscopic view of proximal fraying of interior anterior ulnar fibro-osseous synovial sheath (x); FCR tendon (Δ); and ganglion (G). Proximal at bottom of picture.
Figure 6.
(a) Volar radial ganglion (G) superficial to TFOSST. (b) FCR tendon (Δ) entering proximal TFOSST ulnar to radial trapezial crest (+). (c) Anterior ulnar displacement of FCR tendon (Δ) from floor of TFOSST and from radial trapezial crest (+) after TFOSST complete division. Proximal at bottom of pictures and radial at left of pictures.
All patients were instructed and requested to initiate home exercises after 2 weeks of immobilization and were released to unrestricted activities of daily living if they were pain-free 6 weeks post-operatively. Only one patient, a military active duty member attended therapy post-operatively because it was available at no cost to the patient. In all patients, there were no complications, and pre-operative symptoms of pain resolved after surgical intervention. There was intermittent mild post-surgical pain with wrist motion that resolved after 2 weeks and controlled by nonsteroidal anti-inflammatory drug (NSAID) or and acetaminophen. All patients achieved normal wrist and hand active range of motion an average of 8 weeks after surgical intervention. There has been no recurrence of ganglia or pain symptoms in any patient over the duration of this study.
Discussion
The intra-operative findings and the result of surgical treatment for primary and recurrent volar radial wrist–forearm ganglia in this series highlight the potential pathology of the FCR tendon at the TFOSST that may cause ganglia. In this case series, there was intra-operative evidence of attrition of the FCR tendon isolated to within the TFOSST, and there was attrition of the anterior internal proximal visceral synovial surface of the TFOSST at the origins of the resected primary and recurrent ganglia. Anatomic descriptions of the trapezium has documented that the volar trapezium has both a sulcus and a trapezial crest to constrain the FCR tendon within the TFOSST.5,6,10–13 Yet, stenosis of the TFOSST resulting in FCR tendon attrition is not defined in the literature, and with stenosis, there is a potential of frictional forces that can lead to soft tissue degeneration and formation of ganglia as hypothesized.1,2 One case of recurrent volar radial wrist ganglion originating from the FCR tendon at the TFOSST revealed significant attrition of the FCR tendon at the TFOSST. The FCR tendon was debrided back to grossly normal appearing tendon and sent to pathology. Pathology revealed an eroded FCR tendon with degeneration and interstitial calcifications in the submitted FCR tendon from the TFOSST zone of the trapezium. This circumstantially does correspond to tendinopathy that may or may not result in ganglia that originate from the TFOSST. Like other flexor pulley systems, the FCR tendon TFOSST construct is tightly constrained with the FCR tendon occupying the greatest volume within the TFOSST and nowhere else throughout the entire FCR tendon domain. 5
This tight FCR tendon TFOSST construct was observed in all cases in this case series by the inability to introduce a 1.0 mm tip of a probe in between the anterior surface of the FCR tendon and the internal proximal surface of the TFOSST. It was observed in this case series that complete division of the TFOSST resulted in the FCR tendon displacing anteriorly. This highlights the constraint placed on the FCR tendon at the TFOSST. This displacement was due to intra-operative loss of posterior constraint by the TFOSST of the FCR tendon and the anterior moment exerted on the FCR tendon as it passed over the volar scaphoid tubercle as the FCR tendon transitioned to the volar trapezium.5,6 This anterior displacement of the FCR tendon in this case series is consistent with the studies that describe the FCR tendon transitioning from an anterior neutral position at the scaphoid tubercle and then acutely angulating posteriorly by about 35°–60° to a constrained position at the volar trapezial TFOSST (Figure 7).5,6 The acute angulation of the FCR tendon from the scaphoid to the volar trapezium requires an intact TFOSST with a tight tolerance as the FCR tendon transitions to the metacarpal insertion(s) meeting the criteria of a pulley. Because of this unique constrained construct of the FCR tendon at the TFOSST, it is hypothesized that repetitive mechanical frictional forces likely caused mucoid degeneration within the TFOSST that led to ganglia formation in these patients, and this finding is consistent with the surgical literature.1–3,5,8–12,14,15 In addition, the surgical literature describes symptomatic FCR tendinopathy or tendinitis at the TFOSST that can be treated by tenolysis of the TFOSST. 12 However, the surgical literature only mentioned that a ganglion sometimes may be identified in the TFOSST by MRI resulting in symptomatic FCR tendinopathy or tendinitis requiring surgical tenolysis of the TFOSST for symptomatic FCR tendinopathy or tendinitis. 12 In contrast, the literature does not specifically identify or state that a volar radial wrist–forearm ganglion may be caused by pathology isolated to the FCR tendon and the TFOSST as stated in this study.1–10,12,14 Future studies are needed to focus on pathologic changes of the FCR tendon at the TFOSST that may cause volar radial wrist–forearm ganglia to validate the findings and conclusions of this case study.
Figure 7.
(a) MRI T2 image showing anterior to ≈35° posterior transition (long white arrow) of the FCR tendon (Δ) over the scaphoid tubercle as it enters trapezial TFOSST. (b) MRI T1 image showing FCR tendon (Δ) within TFOSST sulcus with volar (anterior) and dorsal (posterior) margins (x); trapezium (T); and scaphoid (S).
Conclusion
Surgical treatment of primary and recurrent volar radial wrist–forearm ganglia has yielded higher recurrence rates of ganglia when compared to surgical treatment of dorsal wrist ganglia. The published literature does not describe, or attribute, the pathology isolated to the FCR tendon at the TFOSST that may cause primary and recurrent volar radial wrist–forearm ganglia. In contrast, this case series observed pathology isolated to the FCR tendon at the TFOSST as the most likely etiologic factor resulting in primary and recurrent volar radial wrist–forearm ganglia. In addition to previously reported and hypothesized causes of radial volar wrist–forearm ganglia, recognizing and treating an additional site of potential pathology of the FCR tendon at the TFOSST may mitigate recurrence rates of surgically treated volar radial wrist–forearm ganglia.
Footnotes
Ethical approval: Our institution, Guam SurgiCenter, does not require ethical approval for reporting individual cases or case series.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study and manuscript development were self-funded.
Informed consent: There is no case identifying information, including names, initials, or hospital numbers in the submission. Legally authorized written informed consent was obtained from all patients or their authorized representatives assenting for their anonymized information to be used in this manuscript. All patients or their authorized representative have assented and submitted signed written informed consents for their anonymized information to be used in research and or in scientific studies. The informed signed and assented consents meet all patient confidentiality regulations.
Statement of human rights: This submitted study is in accordance with the Helsinki Declaration of 2013 and there is no violation of Human Rights in this scientific study.
Statement of publication: This submitted manuscript has not been previously published and this manuscript is not under consideration for publication elsewhere, and if accepted, it will not be published elsewhere.
ORCID iD: Jerone T Landstrӧm  https://orcid.org/0000-0002-7618-9896
https://orcid.org/0000-0002-7618-9896
References
- 1. Nahra ME, Bucchieri JS. Ganglion cysts and other tumor related conditions of the hand and wrist. Hand Clin 2004; 20(3): 249–260v. [DOI] [PubMed] [Google Scholar]
- 2. Gude W, Morelli V. Ganglion cysts of the wrist: pathophysiology, clinical picture, and management. Curr Rev Musculoskelet Med 2008; 1(3–4): 205–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wright TW, Cooney WP, Ilstrup DM. Anterior wrist ganglion. J Hand Surg 1994; 6: 954–958. [DOI] [PubMed] [Google Scholar]
- 4. Lidder S, Ranawat V, Ahrens P. Surgical excision of wrist ganglia; literature review and nine-year retrospective study of recurrence and patient satisfaction. Orthop Rev 2009; 1: 17–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bishop AT, Gabel G, Carmichael SW. Flexor carpi radialis tendinitis: part I. Operative Anatomy. J Bone Joint Surg Am 1994; 76: 1009–1014. [DOI] [PubMed] [Google Scholar]
- 6. Greendyke SD, Wilson M, Shepler TR. Anterior wrist ganglia from the scaphotrapezial joint. J Hand Surg Am 1992; 17(3): 487–490. [DOI] [PubMed] [Google Scholar]
- 7. Osagie L, Gallivan S, Wickham N, et al. Intraosseous ganglion cysts of the carpus: current practice. Hand (N Y) 2015; 10(4): 598–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McAuliffe JA. Tendon disorders of the hand and wrist. J Hand Surg 2010; 35: 846–853. [DOI] [PubMed] [Google Scholar]
- 9. Watson HK, Weinzweig J. The wrist. Philadelphia, PA: Lippincott Williams & Wilkins, 2001, pp. 99, 688. [Google Scholar]
- 10. Fitton JM, Shea FW, Goldie W. Lesions of the flexor carpi radialis tendon and sheath causing pain at the wrist. J Bone Joint Surg Br 1968; 50(2): 359–363. [PubMed] [Google Scholar]
- 11. Loisel F, Chapuy S, Rey P, et al. Dimensions of the trapezium bone: a cadaver and CT study. Surg Radiol Anat 2015; 37(7): 787–792. [DOI] [PubMed] [Google Scholar]
- 12. Brink PRG, Franssen Disseldorp DJ. A simple blind tenolysis for flexor carpi radialis tendinopathy. Hand (N Y) 2015; 10(2): 323–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nigro RO. Anatomy of the flexor retinaculum of the wrist and the flexor carpi radialis tunnel. Hand Clin 2001; 17(1): 61–64vi. [PubMed] [Google Scholar]
- 14. Vuillemin V, Guerini H, Bard H, et al. Stenosing tenosynovitis. J Ultrasound 2012; 15: 20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Senda H, Mizutani J, Okamoto H. Intratendinous ganglion of the hand: two case reports occurring in the extensor digitorum communis and the flexor digitorum superficialis tendon. Case Reports Plast Surg Hand Surg 2017; 4(1): 9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]