Abstract
Usually, bee sting systemic envenomation is self-limited mild allergic reaction rarely associated with systemic manifestations such as anaphylaxis, myocardial injury, encephalitis, acute kidney injury and serum sickness. Kounis syndrome also known as allergic myocardial infarction is uncommon clinical feature and reported cases are scarce in literature. Herein, we described a hypothetical case of Kounis syndrome diagnosed in a 74-year-old man initially presenting for anaphylactic reaction.
Keywords: Kounis syndrome, myocardial infarction, bee stings
Introduction
Bee sting systemic envenomation is common in Northern Sri Lanka. 1 The natural course of reaction may variable, 95% of time mild local or no reaction and occasionally develop severe systemic reaction. The clinical manifestation varies from localized severe allergic reaction to severe systemic manifestations such as acute kidney injury, rhabdomyolysis, disseminated intravascular coagulation, anaphylactic shock, myocardial infarction and hepatitis which are mediated by IgE-related mechanism.2–4 Acute myocardial injury is first reported as syndrome of allergic angina by Kounis and Zavas 3 in 1991 which is associated with mast cell activation involving allergic or hypersensitivity and anaphylactic or anaphylactoid reactions. The three type of Kounis syndrome were described as myocardial ischaemia following toxin effect of bee sting in normal coronary artery, pre-existing coronary atherovascular disease and coincidence of hypersensitivity reaction following implantation of drug-eluting stent, respectively, in literature. Here, we described a patient with multiple bee stings causing anaphylaxis and myocardial injury who had mild ST depression and T inversion in V1–V4 in 12 lead electrocardiography. Our case showed the rare presentation of acute myocardial injury following multiple bee sting envenomation. Therefore, clinicians should be aware of myocardial infarction among patients complaining chest pain following bee sting.
Case history
A 74-year-old man was admitted to an emergency unit with a history of shortness of breath and lip swelling following multiple bee stings after 1 h of the incident. He had a past history of diabetes mellitus, hypertension, dyslipidaemia, chronic kidney disease stage III B, and ischaemic heart disease. On admission, more than 50 bee sting marks were noted all over his body. On further evaluation, he was conscious and alert. His pulse rate was 80 beats/min and his blood pressure was 100/70 mmHg. His respiratory rate was 16 per minute with saturation of 98% on room air. He had lip swelling and mild swelling at bite marks. His lungs were clear on examination. His full blood count showed white cell count of 17,500 mm−3 (4,000–11,000 mm−3) with predominant eosinophilia of 10% (0%–5%), haemoglobin of 13.1 g/dL (11.5–14.5 g/dL) and platelets of 262,000 mm−3 (150,000–450,000 mm−3). His aspartate aminotransferase (AST) was 42 IU/L (10–25 IU/L) and alanine aminotransferase (ALT) was 62 IU/L (15–35 IU/L). His serum electrolytes showed sodium of 146 mmol/L (1,350,145 mmol/L) and potassium of 4.9 mmol/L (3.5–5.5 mmol/L). His blood urea was 88 mg/dL (<30 mg/dL) and serum creatinine was 2.5 mg/dL (<1.1 mg/dL). His prothrombin time (PT)/international normalized ratio (INR) was 1.0 (<1.4) and activated partial thromboplastin time (APTT) was 32 (30–45). He was initially managed with intravenous hydrocortisone 100 mg and thereafter 6-hourly along with intravenous chlorpheniramine 10 mg. His previous ultrasound scan of abdomen showed bilateral renal parenchymal disease. His previous two-dimensional (2D) echocardiography was compatible with ischemic heart disease with ejection fraction of 45% and previous coronary angiography showed minor coronary artery disease.
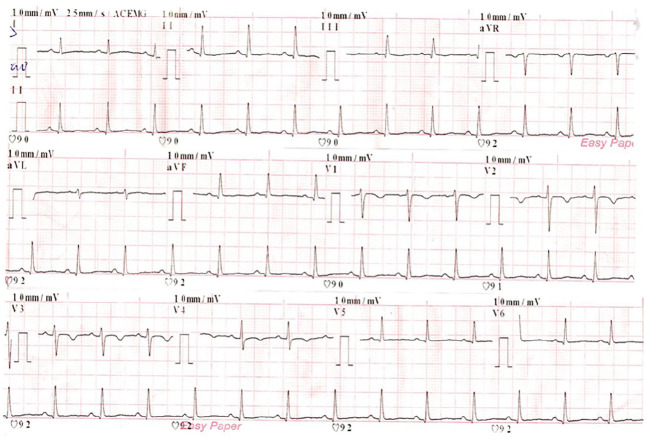
Two hours after admission, he developed an ischeamic chest pain. He was found to have sweating and anxious. His 12-lead electrocardiogram (ECG) showed mild ST depression and T inversions in V1 to V4 shown in Figure 1. His high sensitivity troponin I was positive (1439 ng/L). He was managed with loading doses of aspirin 300 mg, clopidogrel 300 mg and atorvastatin 40 mg followed by enoxaparin 1 mg/kg twice daily for 3 days. His 2D echocardiography showed left ventricular dysfunction with ejection fraction of 35% and his ultrasound (USS) abdomen showed acute chronic kidney disease. His repeat 2D echocardiography showed improved left ventricular function with ejection fraction of 45% and repeat USS scan showed chronic renal parenchymal disease. A coronary angiography was not performed due to high serum creatinine level following expert cardiologist opinion at the time of admission. One month later, the coronary angiography was performed after adequate hydration and N-Acetyl cysteine infusion and showed minor coronary artery disease. The cardiac magnetic resonance imaging (MRI) was not performed for financial issues and unavailability at our medical centre. The anti-anginal drugs were continued after expert opinion considering his multiple risk factors for coronary artery disease.
Figure 1.
The 12-lead ECG showed mild ST depression and T inversions in V1 to V4 in a patient with multiple bee sting bites.
Discussion
Bee stings are related hymenoptera order of insects and its envenomation ranges from mild self-limiting allergic reactions to severe anaphylaxis. The venom consists a mixture of peptides and enzymes which causes allergic local reaction or systemic toxic reactions. 2 It can rarely cause systemic manifestations such as anaphylaxis, myocardial injury, encephalitis, acute kidney injury and serum sickness which are rarely reported in literature.2,3 Acute myocardial injury is first reported as syndrome of allergic angina by Kounis and Zavas 3 in 1991 which is associated with mast cell activation involving allergic or hypersensitivity and anaphylactic or anaphylactoid reactions. There are few cases of acute myocardial injury reported in literature.1–10 It results in vasculitic event, platelet aggregation and thrombosis following release of vasoactive inflammatory mediators of anaphylactic reaction which cause myocardial ischaemia and infarction (Kounis syndrome). 5 Direct toxic myocardial necrotizing effect also reported as causative for acute coronary syndrome.5–7
The Kounis syndrome is describes as a syndrome of an allergic angina by Kounis et al. which is due to immune mediated injury triggered by mast cell activation and degranulation induced by IgE-related mechanism. The release of vasoactive inflammatory mediators such as histamine, serotonin, proteases, and various cytokines cause vasospasm, platelet, and clotting factor activation, which results in coronary vasospasm and thrombosis leading to myocardial ischaemia and infarction.3,5
The three type of Kounis syndrome were described as myocardial ischaemia following toxin effect of bee sting in normal coronary artery, pre-existing coronary atherovascular disease and coincidence of hypersensitivity reaction following implantation of drug-eluting stent, respectively, in literature. Type I Kounis syndrome is manifested as acute ST-elevation myocardial infarction (STEMI) which can occur among normal patients without predisposing factors for coronary artery disease.5,8 Type II Kounis syndrome is manifested as acute non-ST segment elevation MI (NSTEMI) which can occur among pre-existing atheromatous disease in whom allergic reaction can induce plaque erosion or rupture manifesting as MI.5,8 Our patient has developed likely Type II Kounis syndrome based on pre-existing risk factors for atheromatous disease which was diagnosed by ischemic chest pain, elevated cardiac troponin level and ECG changes related to specific coronary artery territory with history of bee sting. Type III, coincidence of hypersensitivity reaction following implantation of drug-eluting stent, causes stent thrombosis.9,10 The clinical presentation of myocardial infarction may be quite which varies from silent to delayed presentation several hours following bee sting.9,10
An acute myocardial injury is manifested by elevated cardiac markers and ECG changes. The ECG changes include ST elevation, ST depression, and pathological Q waves or T wave changes. The common rhythms of abnormalities are supra-ventricular arrhythmia, ventricular ectopic, junctional rhythm and right bundle branch block.2,6,8 Serial ECG is mandatory to identify high-risk patients who complain chest pain following bee sting irrespective of severity of patient’s reaction to the bee sting. 9 The physicians should be aware of diagnosis of acute myocardial infarction to prevent complications at the earliest suspicion following bee sting.
Adequate hydration and prompt anaphylaxis management are pivotal in the management of bee sting envenomation. The myocardial infarction should be treated as standard clinical therapy as well. Kounis syndrome is a rare aetiology of acute coronary syndrome with atypical presentation. This may lead to delayed diagnosis and appropriate treatment. Our case highlights the importance of early suspicion and recognition of this rare presentation. In the presence of coronary syndrome, clinicians should treat promptly with appropriate therapy.
Conclusion
This case illustrates the rare presentation of an acute myocardial injury following multiple bee sting envenomation. The physicians should be aware of myocardial infarction in a patient who complain chest pain following bee sting even though rare presentation.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient for their anonymised information to be published in this article.
ORCID iD: Selladurai Pirasath  https://orcid.org/0000-0002-4274-4919
https://orcid.org/0000-0002-4274-4919
References
- 1. Nisahan B, Selvaratnam G, Kumanan T. Myocardial injury following multiple bee stings. Trop Doct 2014; 44(4): 233–234. [DOI] [PubMed] [Google Scholar]
- 2. Mathew A, Chrispal A, David T. Acute myocardial injury and rhabdomyolysis caused by multiple bees stings. J Assoc Physicians India 2011; 59: 518–520. [PubMed] [Google Scholar]
- 3. Kounis NG, Zavas GM. Histamine induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract 1991; 45(2): 121–128. [PubMed] [Google Scholar]
- 4. Freeman TM. Hypersensitivity to hymenoptera stings. N Engl J Med 2004; 351: 1978–1984. [DOI] [PubMed] [Google Scholar]
- 5. Kounis NG. Kounis syndrome (allergic angina and allergic myocardial infarction): a natural paradigm? Int J Cardiol 2006; 110: 7–14. [DOI] [PubMed] [Google Scholar]
- 6. Ceyhan C, Ercan E, Tekten T, et al. Myocardial infarction following a bee sting. Int J Cardiol 2001; 80: 251–253. [DOI] [PubMed] [Google Scholar]
- 7. Nittner-Marszalska M, Kopeć A, Biegus M. Non-ST elevation myocardial infarction after multiple bee stings. A case of ‘Delayed’ Kounis Syndrome? Int J Cardiol 2013; 166: e62–e65. [DOI] [PubMed] [Google Scholar]
- 8. Vang HP, Chen FC, Chen CC, et al. Manifestation mimicking AMI after honeybee sting. Acta Cardiolog Sin 2009; 25: 31–35. [Google Scholar]
- 9. Lombardi A, Vandelli R, Cerè E, et al. Silent acute myocardial infarction following a wasp sting. Ital Heart J 2003; 4(9): 638–641. [PubMed] [Google Scholar]
- 10. Erbilen E, Gulcan E, Albayrak S, et al. Acute myocardial infarction due to a bee sting manifested with ST wave elevation after hospital admission. South Med J 2008; 101(4): 448. [DOI] [PubMed] [Google Scholar]