Abstract
Objectives:
The Carers of Older People in Europe Index is a first-stage assessment tool to detect family caregivers in need of support. This instrument assesses caregivers’ subjective perceptions of their caregiving circumstances. The present study examines the psychometric properties of the Norwegian version of the Carers of Older People in Europe Index among family caregivers for older persons with dementia living at home.
Methods:
Cross-sectional survey data were collected from 430 dementia caregivers. The sample was randomly split as follows: the first half of the sample was used to identify the measurement model using an exploratory factor analysis, and the second half of the sample was used to cross-validate the model using a confirmatory factor analysis. The criterion validity and reliability (internal consistency and test–retest reliability) of the Carers of Older People in Europe Index were also examined.
Results:
Using an exploratory factor analysis, we extracted three factors that were consistent with previous findings: negative impact of caregiving, positive values of caregiving and quality of support. This model fit the data well using a confirmatory factor analysis. Moreover, a second-order model could replace the three-factor correlated model without sacrificing the model fit, supporting the use of a global impact of caregiving score. The three factors and the global factor correlated with the criteria measures in the expected directions. The internal consistency was assessed using Cronbach’s alpha and was good for the negative impact (α = 0.86) and the quality of support (α = 0.76) factors. The positive values factor was less consistent (α = 0.64). The test–retest reliability was examined using Spearman’s rank order correlation and was good for all three factors.
Conclusion:
The psychometric properties of the Norwegian version of the Carers of Older People in Europe Index are good. The instrument assesses dementia caregivers’ situations across three primary factors or alternatively validly summarizes the factors in a global impact of caregiving score.
Keywords: Dementia, dementia caregivers, factor analysis, questionnaire, validation
Background
The prevalence of dementia is increasing worldwide,1–3 and the disease is among the leading causes of disability, dependence3,4 and death 5 in old age. Hence, dementia is a key public health issue. 3 The recognition of the impact and challenges of this illness on healthcare systems, communities and affected families is growing worldwide,2,3,5 including in Norway. 6 International and national policies addressing dementia care challenges acknowledge the informal care provided by dementia caregivers as an important healthcare resource.3–6 The efforts of dementia caregivers are important for meeting health needs3,5 and improving the quality of life 7 of the recipients of care. Informal care constitutes a large proportion of the total care provided and contributes to reducing the societal cost associated with dementia care.2,5,8,9 Thus, studies investigating factors that support or reinforce dementia caregivers in their caregiving roles are important.
Considerable research has focused on the burden or negative consequences that can be inflicted by caring for a family member with dementia.10,11 Dementia caring may heighten the risks of stress 12 and depression 13 or may undermine the well-being of caregivers compared to non-caregivers. 12 In addition, the chronic caregiver burden may lead to physiological stress-related changes with diverse functional consequences, such as impaired cognitive functioning, risks of developing cardiovascular diseases or reduced sleep quality. 14 Thus, a dementia caregiver can be described as an “invisible second patient” with potentially unrecognized support and guidance needs.3,7
The extensive focus on negative health outcomes may have restricted innovation and development of support services for dementia caregivers10,15 because caregivers can derive a great deal of satisfaction from their role 16 and experience a strengthened relationship with the care recipient. 15 These positive experiences can enhance motivation and meaning and have an impact on the dementia caregiver’s well-being. 17 Moreover, providing care during the early phases of dementia encompasses expectations and needs other than those required as the dementia progresses.3,18 The advanced stages of dementia require more effort and time9,19 and involve more complex tasks3,20 and increased collaboration with formal caregivers.18,20 Hence, dementia caregivers should receive support that adjusts to their needs and the shifting demands over time to ensure their well-being. 18 Norms related to generation, gender and culture are contextual factors that may further moderate the dementia caregiver’s situation7,10 and, ultimately, the relationship between the caregiver and the care recipient.
Due to the multidimensional factors underpinning the dementia caregiver’s situation, formal healthcare professionals may benefit considerably from using systematic methods to obtain information. Such methods may also be favorable for dementia caregivers, as the information can be used to adapt targeted interventions based on individual needs. The Carers of Older People in Europe Index (COPE Index) is an instrument developed as a screening tool to detect family caregivers in need of support.21,22 The COPE Index is based on a theoretical model reflecting both the positive and negative aspects of caregiving, including the family caregivers’ subjective perceptions of the caregiver role, the quality of the relationship with the care recipient and support from the family, social network or health and care services.21–23 The COPE Index has been used in several studies, including studies assessing family caregivers of older care recipients living at home,24–28 caregivers of disabled people in different age groups, 29 caregivers of persons with bipolar disorders, 30 and dementia caregivers.20,31,32 Several studies have applied the subscales as outcome measures to evaluate caregiver support interventions27,30 or assess changes in the caregivers’ situations over time.20,25 The appropriateness of the instrument for longitudinal studies and intervention research has been discussed to some extent, although the instrument may not be sufficiently sensitive to evaluate changes. 20 Nevertheless, the instrument was designed to be a first-stage assessment tool, and more detailed assessments and dialogs with caregivers are warranted to adapt interventions to individual needs. 23
The psychometric properties of the original 2003 COPE Index 21 were sub-optimal; hence, a revised version was adopted in 2006 in a six-country European survey of family caregivers of older people (EUROFAMCARE study). 23 An exploratory factor analysis revealed that the following three components underpinned the 15 items: negative impact of caregiving, positive values of caregiving and quality of support. 23 Subsequent factor analysis studies have used similar exploratory methods to identify a similar three-factor structure.25,29 However, while exploratory factor analyses (EFA) are entirely empirically driven and most suitable for exploring the number and structure of the underlying dimensions of items, a confirmatory factor analysis (CFA) is more suitable for examining the replicability of a factor structure or how well an a priori defined model matches the collected data. 33 Thus, a good-fitting CFA model has better properties for generalizability than an EFA model.
Criterion validity tests among family caregivers of older people21,23 and caregivers of older persons with dementia 31 have shown that overall the subscales correlate satisfactorily with the chosen criteria. The test score reliability in terms of internal consistency (Cronbach’s alpha) has previously been examined in populations of family caregivers of older people 23 , caregivers of older homecare clients (not including clients with cancer, dementia or psychiatric disorders) 25 and caregivers of disabled people. 29 In these studies, the internal consistency was satisfactory for the negative impact subscale (0.79–0.87) but questionable for the positive values (0.54–0.66) and quality of support (0.56–0.78) subscales. To date, the test–retest reliability has not been examined, although this measure is recommended for reliability analyses.33,34
Objectives
The aim of the present study is to examine the psychometric properties of the translated Norwegian version of the COPE Index among family caregivers of older people with dementia living at home. The construct validity was examined using a cross-validation approach by first conducting an EFA in an exploration sample, followed by a CFA in a second cross-validation sample. We assessed the criterion validity by examining whether the bivariate correlations of the criterion variables were in the expected directions. This study is the first to examine the test–retest reliability of the COPE Index.
Methods
This study is a part of a research project titled “Public dementia care in terms of equal services—family, local and multiethnic perspectives.” The overarching project aims to provide new knowledge concerning access, use, quality and content of municipal healthcare services available to dementia caregivers in Northern Norway and investigate dementia caregivers’ experiences and perceptions of their caregiver roles. The project consists of two separate sub-studies that focus on different aspects of dementia care. The first sub-study involves qualitative interviews with senior volunteers and healthcare professionals.35,36 The second sub-study is a quantitative cross-sectional study involving a self-administered questionnaire measuring different aspects of the situation of dementia caregivers. The current study is the first paper from the quantitative part of the project.
Sample and setting
Dementia caregivers in 32 municipalities in Northern Norway were invited to participate in the study. The municipalities were selected based on size, geographical dispersion, urban/rural areas, and location inside (n = 5), partially inside (n = 17), or outside (n = 10) the area under the Sami Parliament subsidy scheme for cultural and economic development (STN area). Sami people are indigenous people and the majority live in Norway. 37
Because no registry of persons with dementia diagnoses and their relatives was available, we collaborated with research assistants in each of the 32 municipalities. Initially, the municipal healthcare managers approved the study and appointed research assistants who were registered nurses or licensed practical nurses. All research assistants worked with dementia care within community homecare services or respite care services, and several assistants had special education in geriatric and dementia care. The research team carried out individual training sessions with the research assistants prior to the recruitment of the participants. The training included a detailed examination of the inclusion criteria, how to safely storage the study materials, and how to secure the anonymity and confidentiality of the participants.
The research assistants identified dementia caregivers of persons who received home-based services and/or respite care services and met the inclusion criteria. The inclusion criteria were as follows: provided unpaid help and support at least once a week to people aged ⩾65 years with dementia living at home; were over 18 years of age; were a spouse, son/daughter, friend or a more distant relative; and provided most informal support and help. Support and help were broadly defined as personal care, emotional and psychological support, regular visits and phone calls, financial help and organization of care provided by formal caregivers. 24
The initial contact with the research assistants disclosed that several care recipients did not have a dementia diagnosis due to insufficient diagnostic procedures. In these cases, the condition was described as cognitive impairment or memory loss. Hence, dementia was defined as a dementia diagnosis or cognitive impairment with symptoms consistent with dementia. These symptoms included progressive memory loss and difficulties with cognitive skills (e.g. language and problem-solving) that affected the care recipients’ ability to perform everyday activities. 5 If cognitive impairment was caused by other conditions (e.g. brain injury, brain tumor or delirium), the caregiver was not included in the study. If the research assistants were unsure whether the cognitive impairment was caused by conditions other than dementia, they were instructed to not include the caregiver in the study.
The research assistants identified 788 dementia caregivers who met the inclusion criteria. To obtain the general characteristics and carry out a selective reminder procedure, the research assistants recorded information pertaining to gender, the dementia caregivers’ relationship with the care recipient, and the contact information of the potential participants. Individual information was not shared with the research team. The research assistant distributed the questionnaire by mail between April and November 2016, followed by a reminder after 4 weeks. In total, 436 responders agreed to participate in the study. After the data cleaning, 430 dementia caregivers were included in the final sample, yielding a response rate of 54.6%. Among the responders, 31.1% were men and 68.9% were women. The relationships between the responders and the care recipients included spouses (28.8%), daughters (42.4%), sons (18.3%) and other (10.5%). The responders ranged in age between 29 and 95 years (mean age = 61.8 years, standard deviation (SD) = 11.7 years, median age = 60 years), and approximately 81% of the responders were married, 11% of the responders were single, 7% of the responders were divorced and 1% of the responders were widows or widowers. In total, 7% of the dementia caregivers were Sami. De-identified summarized data from the inclusion records regarding the gender and kinship relationships of all invited dementia caregivers were used to compare the responders and non-responders. The non-responders differed from the responders as follows: 33.2% were men, 19.7% were spouses, 44.9% were daughters, 25.5% were sons, and 9.8% were other. To examine the test–retest reliability, a heterogeneous group of 40 participants was invited to complete the questionnaire a second time 4 weeks later.
Instruments
The demographic data included age, gender, ethnicity, marital status, and kinship relationship. The COPE Index consists of 15 items (see Table 1) that assess the family caregiver’s situation across the following three dimensions: negative impact of caregiving (NI, seven items), positive values of caregiving (PV, four items) and quality of social support (QS, four items). 23 The responses were recorded using a 4-point Likert-type scale response format (1 = never, 2 = sometimes, 3 = often and 4 = always). A “not applicable” response option was added to five items regarding how caregiving influenced relationships with friends (item 3), relationships with family (item 5), support from friends/neighbors (item 8), support from family (item 10) and support from health and social services (item 12). 21 These items had a large proportion of missing data (ranging between 7.2% and 23.5%) due to the “not applicable” option. Student’s t-tests and chi-square tests were used to compare age, gender, ethnicity, marital status and relationship and revealed small differences between those who selected and those who did not select this option.
Table 1.
Exploratory and confirmatory factor analyses of the COPE Index in the exploration (n1 = 215) and cross-validation (n2 = 215) samples, respectively.
| Item | Latent factors |
|||||
|---|---|---|---|---|---|---|
| 1 (NI) |
2 (QS) |
3 (PV) |
||||
| EFA | CFA | EFA | CFA | EFA | CFA | |
| 7. Feeling trapped in the caregiver role (n = 210) | 0.80 | 0.71 | ||||
| 14. Caregiving has a negative impact on emotional well-being (n = 208) | 0.73 | 0.71 | ||||
| 3. Caregiving causes difficulties with friend relationships (n = 192) | 0.72 | 0.70 | ||||
| 4. Caregiving has a negative impact on physical health (n = 207) | 0.68 | 0.69 | ||||
| 2. Caregiving is too demanding (n = 219) | 0.66 | 0.76 | ||||
| 5. Caregiving causes difficulties with family relationships (n = 190) | 0.60 | 0.64 | ||||
| 15. Overall support in caregiver role (n = 203) | 0.89 | 0.87 | ||||
| 12. Feeling supported by health and social services (n = 182) | 0.61 | 0.68 | ||||
| 13. Feeling appreciated as a caregiver (n = 205) | 0.55 | 0.61 | ||||
| 10. Feeling supported by family (n = 200) | 0.53 | 0.61 | ||||
| 8. Feeling supported by friends and neighbors (n = 162) | 0.50 | 0.53 | ||||
| 9. Feeling that caregiving is worthwhile (n = 207) | 0.76 | 0.70 | ||||
| 11. Relationship with the person cared for (n = 210) | 0.51 | 0.52 | ||||
| 1. Coping well as a caregiver (n = 208) | 0.48 | 0.60 | ||||
| 6. Caregiving causes financial implications a | 0.16 | 0.23 | −0.13 | |||
| Eigenvalues (unrotated) | 5.20 | 1.86 | 1.07 | |||
| Cronbach’s alpha | 0.86 | 0.76 | 0.64 | |||
COPE: Carers of Older People in Europe; EFA: factor loadings based on an exploratory factor analysis; CFA: factor loadings based on a confirmatory factor analysis specifying a correlated three-factor model; NI: negative impact; QS: quality of support; PV: positive values.
The item measuring the financial implications of caregiving was excluded from the EFA and CFA due to low factor loadings. The reported factor loadings were obtained from the initial analysis.
The World Health Organization-5 Well-being Index (WHO-5), general health status, the Social Restriction Scale and a single item assessing demand associated with caregiving were used to evaluate the criterion validity. Three of the criteria (WHO-5, general health status and the Social Restriction Scale) were used in a previous comprehensive validation study of the COPE Index. 23 The rationale for using several of the same criteria was to allow for a comparison of the results.
The WHO-5 is a five-item generic scale that assesses the subjective perception of well-being over the previous 2 weeks. The scores range from 0 to 25, and higher scores indicate better well-being. 38 The WHO-5 has demonstrated good validity 39 and reliability. 23 In the present study, the scale demonstrated high internal consistency (Cronbach’s alpha = 0.92).
The general health status was assessed using the following single item drawn from the Tromsø Study: 40 “How would you rate your health overall?.” The responses were recorded using a 5-point scale ranging from 1 (very good) to 5 (very poor).
We assessed caregiver role inflexibility with two items drawn from the Common Assessment Tool (CAT) used in the EUROFAMCARE survey study 23 that were originally adapted from the Social Restriction Scale. 41 The responses were recorded using a 3-point scale, and higher scores indicate more social restriction. 23 In the present study, the internal consistency of the two items was satisfactory (Cronbach’s alpha = 0.84).
The single item assessing the demands associated with providing care was drawn from a Norwegian project that evaluated school programs for dementia caregivers. 42 The responses were recorded using a 4-point scale ranging from 1 (very demanding) to 4 (not demanding). This item has not been previously used as a criterion, and in this study, we assumed that dementia caregivers who consider caregiving demanding also experienced a high negative impact due to caregiving.
The Norwegian translations of the COPE Index and the Social Restriction Scale conformed with the principles of the International Society for Pharmacoeconomics and Outcomes Research (ISPOR). 43 The forward translations were performed by using two translators, followed by back translation by two independent translators. Any discrepancies were resolved through a consensus discussion. The entire questionnaire, including the COPE Index, was pilot tested on five adult dementia caregivers. These dementia caregivers should represent the target population and differed in gender, age, educational level and kinship relationship to the care recipient. The pilot test included an interview regarding how the respondents interpreted the meaning of the items. The feedback of the respondents resulted in minor revisions and refinements that did not significantly alter the items.
Statistical analyses
We used IBM SPSS Statistics for Windows version 23.0 for all analyses, except for the CFA, which was conducted using Mplus 7.4. 44
Construct validity
The construct validity investigation followed a cross-validation approach. The sample was randomly split (n1 = 215 and n2 = 215) using the first and second half to conduct the EFA and the CFA, respectively. The two samples did not differ in demographics, such as age, gender, ethnicity, educational level and kinship relationship to the care recipient. The preferred EFA model from sample 1 was retested using CFA methodology on sample 2 (n = 215). The EFA used the principal axis factoring method. Because the correlations between the factors were expected, the solution was promax rotated (k = 5). Factors exceeding initial eigenvalues >1 (cf. Kaiser’s criterion) were extracted, and factor loadings <0.4 were suppressed. In addition, a scree-plot of the eigenvalues was examined. The missing data were mainly due to the response option “not applicable” on five of the items. The Little’s Missing Completely at Random (MCAR) Test was statistically significant for these items, indicating that the data not were missing completely at random. Moreover, imputation was not considered entirely feasible as the imputation model would differ from the analysis model (i.e. regression vs factor model). Thus, the missing variables were excluded pairwise as this option included all available data in the factor analysis, basing the correlations on all available pairs. In the initial analysis, one item measuring the financial implications of caregiving (originally in the negative impact dimension) appeared to be uncorrelated to any of the factors and was, therefore, excluded from further analysis (Table 1).
The CFA-estimated factor scores and loadings were extracted using the robust maximum likelihood method as several items had negatively (Z ranging from −3.99 to −11.01) or positively (Z ranging from 2.02 to 2.95) skewed distributions. Kurtosis was also higher for several of these items (Z ranging from −3.99 to 2.7). This robust method adjusts the standard errors appropriately. The measurement model fit was evaluated using the comparative fit index (CFI), Tucker–Lewis Index (Tucker–Lewis Index (TLI)), root mean square residual (root mean square error approximation (RMSEA)), and chi-square test. The RMSEA, CFI and TFI values range from 0 to 1, where a CFI/TLI close to 0.95 and RMSEA close to 0.06 indicate a good model fit. 45 The preferred EFA model should fit better than a null model (fixing all item-factor correlations to zero) or a one-factor model. In addition, we examined whether replacing the correlated three-factor EFA model with a general second-order factor could fit the data equally well. If supported, a single sum score may be used if brevity is needed.
Criterion validity
The bivariate associations of the criterion measures were examined using Spearman’s rank order correlations and associated p-values.
Reliability
Cronbach’s alpha was used to assess the internal consistency of each of the COPE Index subscale scores. The test–retest reliability was assessed using Spearman’s rank order correlation. The statistical power analysis indicated that at least 35 participants should be included considering a Spearman test–retest correlation of 0.8 representative of an acceptably high stability and a coefficient below 0.5 unacceptably low (power = 0.80).
Ethics approval and consent to participate
The Regional Committee for Medical and Health Research Ethics for Northern Norway evaluated the study and concluded that their approval was unnecessary, as no data regarding the health and functional status of the dementia patients were gathered (Ref. No. 2015/1107/REK North). This study, including the research assistants’ use of local records to identify potential participants, data collection procedure, obtaining of informed consent, data handling procedure ensuring the anonymity and confidentiality of the participants, and use of de-identified numbers, was approved by the Norwegian Center for Research Data (NSD) (Ref. No. 2015/43778/3/KS). Written consent was not obtained from the participants before the distribution of the questionnaire. Along with the questionnaire, all invited persons received written information about the purpose of the study and that participation was voluntary. Confidentiality and anonymity were guaranteed. In the information letter, the invited persons were informed that their informed consents were given by completing and returning the questionnaire anonymously to the research team. The participants received a gift of two lottery tickets worth approximately US$6.
Results
Construct validity
The EFA revealed three factors with eigenvalues >1 that explained 58.0% of the variance. The numbers of extracted factors were supported by examining the point of inflection in the scree-plot (Figure 1). Factor one accounted for six items (R2 = 37.1%) and was labeled “negative impact” (Table 1). The second factor accounted for five items (R2 = 13.3%) and was labeled “quality of support.” The third factor accounted for three items (R2 = 7.6%) and was labeled “positive values.”
Figure 1.
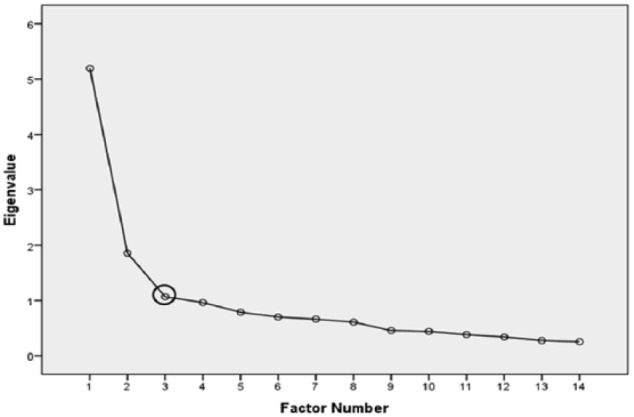
Scree-plot of the eigenvalues of the COPE Index. The point of inflection is marked.
In the CFA, the three-factor EFA model was compared with several other factor models. Expectedly, the null model fit poorly (Table 2). The one-factor model was clearly better than the null model, but also fit poorly. The correlated three-factor EFA model had a good model fit in terms of both model misspecification (RMSEA) and relative fit (CFI and TLI). A more parsimonious model specifying a second-order factor fit the data equal well as the correlated three-factor model. An even more parsimonious model constraining all second-order factor loadings as equal did not yield a significantly worse fit, supporting the use of a global score.
Table 2.
Comparisons of the measurement model fit of the COPE Index.
| Model | χ 2 | df | RMSEA | 95% CI | CFI | TLI |
|---|---|---|---|---|---|---|
| Null model | 883.3 | 91 | 0.202 | 0.190–0.214 | 0.000 | 0.000 |
| One factor | 314.1 | 77 | 0.120 | 0.106–0.134 | 0.701 | 0.646 |
| Three factors | 113.1 | 74 | 0.050 | 0.030–0.067 | 0.951 | 0.939 |
| 2nd order | 113.1 | 74 | 0.050 | 0.030–0.067 | 0.951 | 0.939 |
| 2nd-order EQ | 113.8 | 76 | 0.048 | 0.028–0.066 | 0.952 | 0.943 |
COPE: Carers of Older People in Europe; χ2: chi-square; df: degree of freedom; RMSEA: root mean square error of approximation; 95% CI: RMSEA confidence interval; CFI: comparative fit index; TLI: Tucker–Lewis index; 2nd order: a second-order factor accounting for all three factors; 2nd-order EQ: same as second order but with equal second-order loadings.
Criterion validity
The zero-order correlations between the three COPE factors, the second-order factor and the criterion variables are presented in Table 3. The NI factor was strongly correlated in the expected directions with variables measuring the demands of the caregiving role and the caregivers’ subjective perceptions of well-being (WHO-5). Moreover, the associations between the NI factor, the general health status item and the two items measuring social restriction were moderate. The QS and PV factors demonstrated statistically significant correlations in the expected directions using the criterion measures, although the absolute level of the associations ranged from weak to moderate. The second-order factor was generally moderately to strongly correlated with the criterion variables. In addition, the inter-correlations between the NI, QS and PV factors were moderate.
Table 3.
Bivariate correlations between the COPE Index factors and the criterion validity measures (N = 430).
| Negative impact | Quality of support | Positive values | COPE global | |
|---|---|---|---|---|
| COPE: negative impact | ||||
| COPE: quality of support | 0.39** | |||
| COPE: positive values | 0.42** | 0.43** | ||
| General health status item | −0.42** | −0.26** | −0.23** | −0.37** |
| WHO-5 | 0.63** | 0.39** | 0.37** | 0.62** |
| Demands of caregiving item | 0.61** | 0.19* | 0.31** | 0.49** |
| Social restriction scale 2 items | −0.32** | −0.27** | −0.20** | −0.33** |
COPE: Carers of Older People in Europe; COPE global: a second-order factor accounting for all three factors; WHO-5: World Health Organization-5 Well-Being Index.
p < 0.01 (two-tailed).
p < 0.001 (two-tailed).
Reliability
The internal consistency, which was evaluated using Cronbach’s alpha (α), was 0.86 for the factors reflecting a negative impact, 0.76 for the five items reflecting the quality of support and 0.64 for the positive values subscale (Table 1). To examine the test–retest reliability, a heterogeneous group of 32 dementia caregivers completed a second questionnaire. The mean values of the test–retest scores and Spearman’s rho are presented in Table 4. The mean scores of all three factors were slightly lower after the second measurement. The NI and PV factors had high test–retest correlations (r = 0.91 and 0.92, respectively), whereas the QS factor had a relatively lower correlation (r = 0.76).
Table 4.
Test–retest reliability of the COPE Index (n = 32).
| Factors | Test | Retest | Spearman’s rho* | ||
|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | ||
| Factor 1: negative impact | 29 | 18.86 (3.78) | 28 | 18.25 (3.65) | 0.91 |
| Factor 2: quality of support | 23 | 14.22 (3.10) | 28 | 13.29 (3.74) | 0.76 |
| Factor 3: positive values | 32 | 9.38 (1.62) | 32 | 9.25 (1.57) | 0.92 |
COPE: Carers of Older People in Europe; Spearman’s rho: Spearman’s rank order correlation; SD: standard deviation.
p < 0.001 (two-tailed).
Discussion
Construct validity
This study is the first to evaluate the construct validity of the COPE Index using CFA methodology, which is recommended to ensure the replicability of a factor structure or model. 33 The large sample size allowed for the creation of two subsamples; the first subsample was used to identify the most suitable measurement model using EFA, and the second subsample was used to cross-validate the model using CFA. Our EFA model revealed the following three factors: negative impact, quality of support and positive values. The good fit of the three-factor measurement model supported the assumption of a multidimensional theoretical construct. This model was verified in a subsequent CFA and was comparable to previously published models,23,25,29 strengthening the generalizability of the COPE Index. As shown in previous psychometric studies, the dimensional structure included both negative and positive appraisals of the caregiving role; hence, these factors are independent contributors to the overall caregiving index.21,23
We also extended the CFA by including a second-order factor that accounted for the correlations between the three primary factors. A second-order factor analysis represents a second (and new) factor analysis based on the latent factor scores (rather than the item scores per se), thus examining whether the factor scores may be further reduced to a fewer set of “super factors.” If the reduction in fit is minor compared to the model from the primary factor analysis, the second-order model is favored as it is more parsimonious. Since the fit of this model was comparable to the more “complex” three-factor model, a total COPE Index score can be safely used as a general indicator of family caregivers’ appraisal of the caregiving role.
We noted a few disparate psychometric findings. In the EFA, the item concerning the financial implications of caregiving did not correlate with any of the three factors and was therefore excluded from further analysis. This item had an extreme negative skew, which normally weakens the association with other items. 46 In this study, this item may not have been associated with the other items because more than 80% of the participants did not experience financial difficulties due to caregiving (results not shown). The Scandinavian welfare system, which ensures equal health, care and socio-economic services for all, may be an important contributing factor. 47 Furthermore, only seven dementia caregivers (1.6%) reported working less due to increased caregiving demands, and none of the caregivers had to quit working or work part-time to manage their caregiving responsibilities.
The item “Do you feel that anyone appreciates you as a caregiver?” (item 13) did not correlate with the positive values factor as expected and instead correlated with the quality of support factor. Similar results emerged in the Swedish and Italian datasets in the EUROFAMCARE study 23 and two Finnish validation studies.25,29 These loading patterns may be due to cross-cultural differences, which cannot be disregarded. 29 We chose to retain this item due to its theoretical relevance because it can be associated with support. Sherbourne and Stewart 48 described five dimensions of social support, including emotional support, informational support and affectionate support. Support from family, friends or formal caregivers may cause feelings of being appreciated as a caregiver and vice versa.
Criterion validity
The criterion validity of the COPE Index was good. As expected, the NI factor correlated particularly well with the WHO-5 well-being scale. 38 The WHO-5 is widely used to measure quality of life 49 and may even be used to screen for depression. 39 The negative impact of caregiving has been suggested to have a stronger relationship with mental health and quality of life than with the other dimensions, 23 and the results of the current study support this assumption. Furthermore, the relatively strong association between the second-order factor, which measures the common underlying construct, and the WHO-5 is interesting. A previous study found that higher psychological well-being is related to reduced caregiver burden and a higher quality of life among caregivers of persons with dementia living at home. 50 Thus, the underlying construct of the COPE Index may be related to the dementia caregivers’ perception of caregiver burden. As none of the criteria used were burden-specific instruments, this assumption should be addressed in detail in future studies.
Expectedly, the general health status item was moderately correlated with the NI factor and the second-order factor. In this study, the magnitude of these correlations was greater than previously reported. 23 The single item concerning demands associated with caregiving 42 has not been previously used as a criterion variable. We assumed that dementia caregivers who perceived caregiving as demanding would also report a higher negative impact of caregiving. The magnitude of the correlations between the item, the NI factor and the second-order factor was as expected and indicated the appropriateness of the item as a criterion in the current analysis. The Modified Social Restriction Scale measured the ease of obtaining substitute help if the caregiver became ill or needed a break from caregiving. 23 The magnitude of the associations between the QS and NI factors was relatively weaker than that expected and previously reported 23 but considered acceptable.
Reliability
The overall reliability of the COPE Index is considered good. The stability correlations (test–retest) were high for the NI and PV factors, whereas the correlation of the QS factor was somewhat lower. The sample size (32 participants) was slightly lower than that calculated prior to the analysis as the statistical power analysis indicated that at least 35 subjects should be included considering a Spearman test–retest correlation of 0.8. However, since two of the three stability estimates were above 0.90, we considered the current sample size sufficient.
The NI and QS factors had good internal consistency, and the Cronbach’s alpha values were greater than the recommended value of 0.7. 51 The lower value of the PV factor is consistent with outcomes reported in previous studies.23,25,29 Cronbach’s alpha depends on the number of items included in the analysis, 52 and the PV factor consists of only three items. An easy future solution could be to reformulate the existing questions 29 or add items.23,29 A counter-argument is that one of the strengths of the index is its brevity;21,23 therefore, adding items or dimensions may affect its properties as a first-stage assessment tool. 23 However, the developers emphasized the importance of providing a measurement reflecting both the positive and negative aspects of caregiving,21,22 and a refinement of the PV scale should be accomplished to improve the reliability of the instrument.
Strengths and limitations of the study
The response rate of 54.6% may be considered high for a mail survey. 53 The analysis of gender and kinship relationships with the care recipient showed no great differences between the responders and non-responders. There was a larger proportion of sons among the non-responders and more spouses among the responders. This finding is consistent with outcomes reported in previous studies in which men and younger people exhibited a lower willingness to participate in health research surveys. 54 Moreover, the questionnaire is based on items and scales that have been evaluated as appropriate and used to assess caregivers’ situations in previous studies. Thus, our results are comparable to results from other studies.
The current analysis was somewhat limited by the large proportion of missing data for several items mainly due to the inclusion of a fifth response option (“not applicable”) on three items measuring support and two items measuring the extent to which caregiving causes relationship difficulties with families and friends. The rationale is that social circumstances may vary, and the response option provides the opportunity to score the item as not relevant to the individual. This response option may cause a substantial loss of data that may bias the statistical analysis, 55 and we recommend omitting this response option in the future. However, due to the sufficient number of participants with complete data, we consider the bias related to non-responsiveness and missing data minor. Furthermore, the factor structure was consistent with existing EFA analyses,23,25,29 confirming the validity of the current analysis.
The evaluation of criterion validity is based on brief instruments and single items; thus, questions may emerge regarding their properties as criteria measurements. In addition, we used several of the same criteria used by Balducci et al. 23 in their comprehensive validation study of the revised COPE Index. The assessment of criterion validity is recommended as a part of the cross-cultural validation process when an instrument is translated and/or used in a new population, 33 and these results are considered a supplement to previous research. Moreover, the association between the second-order factor and the criterion variables generates valuable information about the validity of this factor that measures a common underlying construct. The exact meaning of the second-order factor is difficult to define due to the limited number of selected criterion variables. Future studies should address this issue in detail.
Conclusion
The cross-validation approach used in this study enabled us to perform EFA and CFA in two separate samples, and the factor solution of the COPE Index was replicated in both samples. The three-factor solution had a good model fit, supporting theoretical assumptions that dementia caregivers’ perception of caregiving is a multidimensional construct. Moreover, the good model fit of the second-order factors indicates that a common underlying construct exists, supporting the use of a general score to assess the overall impact of caregiving.
Overall, the psychometric properties of the Norwegian version of the COPE Index tested among dementia caregivers are good. The instrument includes important aspects of the dementia caregivers’ situation and can be used by healthcare professionals (e.g. medical practitioners and nurses) as a first-stage assessment tool to identify dementia caregivers in need of help and support. This instrument may be used to assess the caregivers’ situation at the general level and across each of the three factors and, thus, may serve as a tool to adapt healthcare services and interventions to the individual needs of caregivers. Future research may examine the creation of a usable cut-off criterion for the three dimensions or global score to screen for caregivers who need additional attention from healthcare professionals.
Acknowledgments
The authors would like to thank the management and healthcare providers for their assistance with the data collection. The publication charges for this article have been funded by a grant from the publication fund of UiT The Arctic University of Norway.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The Regional Committee for Medical and Health Research Ethics for Northern Norway evaluated the study and concluded that their approval was unnecessary, as no data regarding the health and functional status of the dementia patients were gathered (Ref. No. 2015/1107/REK North). This study, including the research assistants’ use of local records to identify potential participants, data collection procedure, obtaining of informed consent, data handling procedure ensuring the anonymity and confidentiality of the participants, and use of de-identified numbers, was approved by the Norwegian Center for Research Data (NSD) (Ref. No. 2015/43778/3/KS).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Research Council of Norway (grant no. 238146). The funding body played no role in the study design, data collection, analysis, data interpretation or manuscript preparation.
Informed consent: Because no registry of persons with dementia diagnoses and their relatives was available, research assistants (registered nurses or licensed practical nurses) in each of the 32 community healthcare services identified family caregivers who fulfilled the inclusion criteria and distributed the invitations to participate along with the questionnaire. Written consent from the participants was not obtained before distribution of the questionnaire. Along with the questionnaire, all invited persons received written information about the purpose of the study and that participation was voluntary. Confidentiality and anonymity were guaranteed. In the information letter, the invited persons were informed that their informed consent was given by completing and returning the questionnaire anonymously to the research team. This procedure was approved by the Norwegian Center for Research Data (NSD).
ORCID iD: Jill-Marit Moholt  https://orcid.org/0000-0002-8660-1522
https://orcid.org/0000-0002-8660-1522
References
- 1. Prince M, Bryce R, Albanese E, et al. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement 2013; 9: 63–75. [DOI] [PubMed] [Google Scholar]
- 2. Alzheimer’s Disease International. World Alzheimer report 2010: the global economic impact of dementia. London: Alzheimer’s Disease International, 2010. [Google Scholar]
- 3. World Health Organization. Dementia: a public health priority. Geneva: World Health Organization, 2012. [Google Scholar]
- 4. Alzheimer’s Disease International. World Alzheimer report 2013. Journey of Caring: an analysis of long-term care for dementia. London: Alzheimer’s Disease International, 2013. [Google Scholar]
- 5. Alzheimer’s Association. Alzheimer’s association report. 2017 Alzheimer’s disease facts and figures. Alzheimers Dement 2017; 13: 325–373. [Google Scholar]
- 6. Norwegian Ministry of Health and Care Services. Demensplan 2020. Et Mer Demensvennlig Samfunn [Dementia plan 2020. A more dementia-friendly society]. Oslo: Norwegian Ministry of Health and Care Services, 2015. [Google Scholar]
- 7. Brodaty H, Donkin M. Family caregivers of people with dementia. Dialogues Clin Neurosci 2009; 11: 217–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wimo A, Jönsson L, Bond J, et al. The worldwide economic impact of dementia 2010. Alzheimers Dement 2013; 9: 1–11. [DOI] [PubMed] [Google Scholar]
- 9. Nordberg G, von Strauss E, Kåreholt I, et al. The amount of informal and formal care among non-demented and demented elderly persons—results from a Swedish population-based study. Int J Geriatr Psychiatry 2005; 20: 862–871. [DOI] [PubMed] [Google Scholar]
- 10. Montgomery RJV, Williams KN. Implications of differential impacts of care-giving for future research on Alzheimer care. Aging Ment Health 2001; 5: S23–S34. [DOI] [PubMed] [Google Scholar]
- 11. Schulz R, Martire LM. Family caregiving of persons with dementia: prevalence, health effects, and support strategies. Am J Geriatr Psychiatry 2004; 12: 240–249. [PubMed] [Google Scholar]
- 12. Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging 2003; 18: 250–267. [DOI] [PubMed] [Google Scholar]
- 13. Mausbach BT, Chattillion EA, Roepke SK, et al. A comparison of psychosocial outcomes in elderly Alzheimer caregivers and noncaregivers. Am J Geriatr Psychiatry 2013; 21: 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fonareva I, Oken BS. Physiological and functional consequences of caregiving for relatives with dementia. Int Psychogeriatr 2014; 26: 725–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Peacock S, Forbes D, Markle-Reid M, et al. The positive aspects of the caregiving journey with dementia: Using a strengths-based perspective to reveal opportunities. J Appl Gerontol 2010; 29: 640–659. [Google Scholar]
- 16. Andrén S, Elmståhl S. Family caregivers’ subjective experiences of satisfaction in dementia care: aspects of burden, subjective health and sense of coherence. Scand J Caring Sci 2005; 19: 157–168. [DOI] [PubMed] [Google Scholar]
- 17. Quinn C, Clare L, Woods RT. The impact of motivations and meanings on the wellbeing of caregivers of people with dementia: a systematic review. Int Psychogeriatr 2010; 22: 43–55. [DOI] [PubMed] [Google Scholar]
- 18. Lethin C, Hallberg IR, Karlsson S, et al. Family caregivers experiences of formal care when caring for persons with dementia through the process of the disease. Scand J Caring Sci 2016; 30: 526–534. [DOI] [PubMed] [Google Scholar]
- 19. Vossius C, Selbæk G, Ydstebø AE, et al. Ressursbruk Og Sykdomsforløp Ved Demens (REDIC) [Resource use and disease course in dementia (REDIC)]. Ottestad: Alderspsykiatrisk forskningssenter Sykehuset Innlandet HF, 2015. [Google Scholar]
- 20. Holst G, Edberg AK. Wellbeing among people with dementia and their next of kin over a period of 3 years. Scandi J Caring Sci 2011; 25: 549–557. [DOI] [PubMed] [Google Scholar]
- 21. McKee KJ, Philp I, Lamura G, et al. The COPE index—a first stage assessment of negative impact, positive value and quality of support of caregiving in informal carers of older people. Aging Ment Health 2003; 7: 39–52. [DOI] [PubMed] [Google Scholar]
- 22. Nolan M, Philp I. COPE: towards a comprehensive assessment of caregiver need. Br J Nurs 1999; 8: 1364–1372. [DOI] [PubMed] [Google Scholar]
- 23. Balducci C, Mnich E, McKee KJ, et al. Negative impact and positive value in caregiving: validation of the COPE index in a six-country sample of carers. Gerontologist 2008; 48: 276–286. [DOI] [PubMed] [Google Scholar]
- 24. Lamura G, Mnich E, Nolan M, et al. Family carers’ experiences using support services in Europe: empirical evidence from the EUROFAMCARE study. Gerontologist 2008; 48: 752–771. [DOI] [PubMed] [Google Scholar]
- 25. Toljamo M, Perälä ML, Laukkala H. Impact of caregiving on Finnish family caregivers. Scand J Caring Sci 2012; 26: 211–218. [DOI] [PubMed] [Google Scholar]
- 26. Lüdecke D, Mnich E, Kofahl C. The impact of sociodemographic factors on the utilisation of support services for family caregivers of elderly dependents—results from the German sample of the EUROFAMCARE study. Psychosoc Med. Epub ahead of print 25 October 2012. DOI: 10.3205/psm000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Barbabella F, Poli A, Andréasson F, et al. A web-based psychosocial intervention for family caregivers of older people: results from a mixed-methods study in three European countries. JMIR Res Protoc 2016; 5: e196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Vellone E, Fida R, Cocchieri A, et al. Positive and negative impact of caregiving to older adults: A structural equation model. Prof Inferm 2011; 64: 237–248. [PubMed] [Google Scholar]
- 29. Juntunen K, Nikander R, Törmäkangas T, et al. Reliability and validity of the COPE Index among caregivers of disabled people. Appl Nurs Res 2017; 33: 102–107. [DOI] [PubMed] [Google Scholar]
- 30. Jönsson PD, Wijk H, Danielson E, et al. Outcomes of an educational intervention for the family of a person with bipolar disorder: a 2-year follow-up study. J Psychiatr Ment Health Nurs 2011; 18: 333–341. [DOI] [PubMed] [Google Scholar]
- 31. Roud H, Keeling S, Sainsbury R. Using the COPE assessment tool with informal carers of people with dementia in New Zealand. N Z Med J 2006; 119: U2053. [PubMed] [Google Scholar]
- 32. Alwin J, Öberg B, Krevers B. Support/services among family caregivers of persons with dementia–perceived importance and services received. Int J Geriatr Psychiatry 2010; 25: 240–248. [DOI] [PubMed] [Google Scholar]
- 33. de Vet HCW, Terwee CB, Mokkink LB, et al. Measurement in medicine: a practical guide. New York: Cambridge University Press, 2011. [Google Scholar]
- 34. Paiva CE, Barroso EM, Carneseca EC, et al. A critical analysis of test-retest reliability in instrument validation studies of cancer patients under palliative care: a systematic review. BMC Med Res Methodol 2014; 14: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Blix BH, Hamran T. “When the saints go marching in”: constructions of senior volunteering in Norwegian government white papers, and in Norwegian senior volunteers’ and health-care professionals’ stories. Ageing Soc 2018; 38: 1399–1428. [Google Scholar]
- 36. Blix BH, Hamran T. “They take care of their own”: healthcare professionals’ constructions of Sami persons with dementia and their families’ reluctance to seek and accept help through attributions to multiple contexts. Int J Circumpolar Health 2017; 76: 1328962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Statistics Norway. Samisk Statistikk 2018 Sámi Statistihkka 2018 [Sami statistics 2018]. Oslo; Kongsvinger: Statistisk sentralbyrå, 2018. [Google Scholar]
- 38. World Health Organization. WHO info package: mastering depression in primary care, version 2.2. Copenhagen: WHO, 1998. [Google Scholar]
- 39. Topp CW, Østergaard SD, Søndergaard S, et al. The WHO-5 well-being index: a systematic review of the literature. Psychother Psychosom 2015; 84: 167–176. [DOI] [PubMed] [Google Scholar]
- 40. Fylkesnes K, Førde OH. The Tromsø study: predictors of self—evaluated health—has society adopted the expanded health concept? Soc Sci Med 1991; 32: 141–146. [DOI] [PubMed] [Google Scholar]
- 41. McKee KJ, Philp I, Ballinger B, et al. Carer and care-receiver perceptions of dependency for activities of daily living in informal care of older people: negative impact of disagreement on outcomes of care. Gerontology 2001; 47: 159. [Google Scholar]
- 42. Norwegian National Advisory Unit on Ageing and Health (Ageing and Health). Evalueringsskjema for Pårørende Etter Siste Samling [Appraisal form for school program]. Tønsberg: Norwegian National Advisory Unit on Ageing and Health; (Ageing and Health), 2011. [Google Scholar]
- 43. Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for Patient-Reported Outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health 2005; 8: 94–104. [DOI] [PubMed] [Google Scholar]
- 44. Muthén LK, Muthén BO. Mplus user`s guide. 7th ed. Los Angeles, CA: Muthén & Muthén, 1998. –2015. [Google Scholar]
- 45. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Eq Model 1999; 6: 1–55. [Google Scholar]
- 46. Clark LA, Watson D. Constructing validity: basic issues in objective scale development. Psychol Assess 1995; 7: 309–319. [Google Scholar]
- 47. Ministry of Health and Care Services. Lov om pasient- og brukerrettigheter (pasient-og brukerretighetsloven) [Act relating to patient’s rights (Patient’s Rights Act)], https://lovdata.no/dokument/NL/lov/1999-07-02-63 (1999, accessed 15 March 2018).
- 48. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991; 32: 705–714. [DOI] [PubMed] [Google Scholar]
- 49. McDowell I. Measures of self-perceived well-being. J Psychosom Res 2010; 69: 69–79. [DOI] [PubMed] [Google Scholar]
- 50. Lethin C, Renom-Guiteras A, Zwakhalen S, et al. Psychological well-being over time among informal caregivers caring for persons with dementia living at home. Aging Ment Health 2017; 21: 1138–1146. [DOI] [PubMed] [Google Scholar]
- 51. Nunnally JC. Psychometric theory. New York: McGraw-Hill Education, 1967. [Google Scholar]
- 52. Cortina JM. What is coefficient alpha? An examination of theory and applications. J Appl Psychol 1993; 78: 98–104. [Google Scholar]
- 53. Kelley K, Clark B, Brown V, et al. Good practice in the conduct and reporting of survey research. Int J Qual Health Care 2003; 15: 261–266. [DOI] [PubMed] [Google Scholar]
- 54. Glass DC, Kelsall HL, Slegers C, et al. A telephone survey of factors affecting willingness to participate in health research surveys. BMC Public Health 2015; 15: 1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Field A. Discovering statistics using IBM SPSS statistics. 4th ed. Los Angeles, CA: SAGE, 2013. [Google Scholar]


