Abstract
Background:
The objective of this review was to identify and synthesize the findings of the existing literature that highlighted the psychosocial and mental health issues of the migrants during the COVID-19 pandemic in India.
Materials and Methods:
An exploration of the PubMed, Google Scholar, Web of Science, ScienceDirect, Google search, and some other manual searches was undertaken so that no relevant study was missed. A search on Indian scientific literature and cross-references retrieved was also conducted to get further information. The period of the search has been one year from March 1, 2020, to March 31, 2021. The database was searched with the terms “migrants,” “migrant workers,” “COVID-19 pandemic,” “lockdown,” “migrant population,” “mental health issues,” “psychosocial issues” to retrieve the published literature.
Results:
Initially, 48 research articles were retrieved and 10 of them were excluded as they had no sufficient information about mental and psychosocial challenges faced by the migrants. In the remaining 38 articles, 9 articles were original research work (n = 9) published from India related to the impact of COVID-19 on migrants. The second category consisted of editorials or commentary or letters to the editor or policy paper on psychosocial and mental health aspects of migrants during the COVID-19 pandemic (n = 17). The third category was 11 articles on perspectives or opinions or viewpoints (n = 11) related to various psychosocial and mental health issues among migrants in India during the COVID-19 pandemic. Predominantly psychosocial issues found among migrants were living conditions, basic needs, family concerns, and joblessness. The mental health issues found among migrants during the COVID-19 pandemic included psychological distress, depressive disorders, anxiety disorders, substance use disorders.
Conclusion:
Existing literature from India has shown that the COVID-19 pandemic severely impacted the psychosocial and mental health status of the migrants in India. This review suggests the need for more research work from the affected states of India and the development of psychosocial and mental health intervention strategies to minimize the impact of the COVID-19 pandemic on migrants.
Keywords: COVID-19 pandemic, India, literature reviews, mental health issues, migrants, psychosocial issues
The COVID-19 pandemic has highlighted the vulnerability of the migrants in India as they were found at a higher risk than the local population for active disease. 1 Lockdown, announced in the country on the evening of March 24, 2020, struck a blow on their mental state, and they faced psychosocial and mental health crises during the pandemic. This pandemic has caused an increase in psychological stress, severe psychiatric disorders, substance dependence, and suicidal tendencies among the migrants. The pandemic has uncovered a mental health crisis for the migrants, which was described with a novel phrase, “pandemonium of the pandemic.” 2
Psychological support was provided to them in many states, as their mental health issues became prominent during the first wave of the pandemic. Subsequently, alleviating the harmful effects of COVID-19 on the mental health of migrants has become a priority for public health authorities in India. Lack of work, starvation, insanitary conditions, lack of housing and transport facilities, insecurity, unemployment, lack of social protection, and the uncertainty in life were the various crises they faced.3, 4 Literature has originated from some of the affected states of India, while their experiences living in other parts of India have remained an unresearched area.4, 5 Thus, there is a need for further research and understanding of this health problem in the affected states of India. The objective of the review was to determine the psychosocial and mental health issues among the migrants in India in the literature published during the COVID-19 pandemic.
Methods
Search Strategy
An exploration of PubMed, Google Scholar, Web of Science, ScienceDirect, and Google was done. Some other manual searches too were undertaken to cover maximum relevant studies. A search on Indian scientific literature and cross-references retrieved was also conducted to get further information. An initial search exercise revealed that the migrant research literature in India was too heterogeneous to permit a systematic review. The literature retrieved was sufficient only for conducting a narrative review. The database searches were conducted with the terms “migrants,” “migrant workers,” “COVID-19 pandemic,” “lockdown,” “migrant population,” “mental health issues,” and “psychosocial issues” to retrieve the research published literature. The period of the search was from March 1, 2020, to March 31, 2021. The review focused on this period because it was during this period that the migrants faced multiple health challenges during the first wave of the pandemic.
Study Selection and Data Extraction
Initially, 48 research articles were retrieved. Ten were excluded as they had no sufficient information about mental and psychosocial issues faced by the migrants. A careful review of the remaining 38 articles identified research literature relevant to the objective of this review. Most of the research work was conducted online or through telephone.
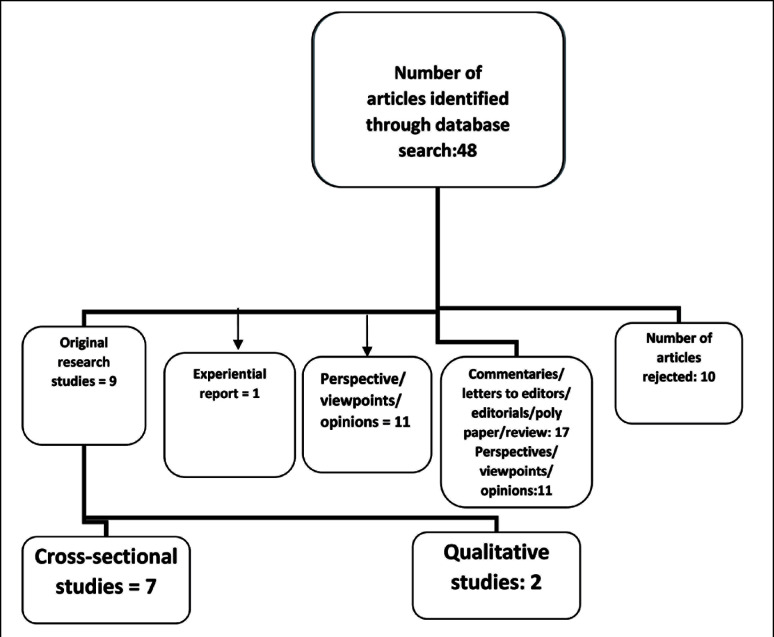
The literature from various resources were summarized and categorized into three subtypes. The first category was of nine articles that were original research work published from India. The second category consisted of editorials, reviews, commentaries, letters to the editors, and policy papers (n = 17). The remaining 11 articles were perspectives, opinions, or viewpoints (see Figure 1).
Figure 1. Flow-Diagram.
Results
Broadly, there were two themes (psychosocial and mental health issues) in the 38 selected articles. Only nine articles were original research work. They included seven cross-sectional studies6–11 and two qualitative studies,13, 14 and an experiential report. 15 Four studies were multicentric from various states and cities of India and were conducted with strong methodology and assessments.6–9 The findings pertaining to the migrants in the four multicentric studies have been highlighted in Table 1. The number of participants in various research studies ranged from 25 to 35,000.6–14
Table 1.
Multicentric Studies of Mental Health and Psychological Issues of Migrants Related to COVID-19 Pandemic from India5–9
| Authors | State/Cities | Participants | Methodology | Study Instruments | Results |
| Adhikari et al., 2020 5 | Bihar, Jharkhand, Uttar-Pradesh, Karnataka | 35,000 migrants | Helpline survey Qualitative |
Records of distress calls | 80% of the migrants of these four native states received no Government facilities. Poor mental health care was provided to the migrants of these four native states. |
| Rao et al., 2020 6 | Kerala, Gujarat, Uttar-Pradesh | 441 Migrants | Multistage, multicentric Qualitative |
Interstate Migrant policy index (IMPEX), social indicators | Kerala has the highest IMPEX score and provided social support measures to the migrants. |
| Chavan et al., 2021 7 | Chandigarh (UT), Panchkula (Haryana) Bhatinda (Punjab) Jaipur (Rajasthan) |
551 migrants | Cross-sectional, multicentric population-based study | Prime-MD-PHQ Drug Screening questionnaire |
Prevalence of one psychiatric diagnosis-19.3%; Ever use of substance-44% |
| Chavan et al., 2021 8 | Chandigarh, Bhatinda, Jaipur, Panchkula |
551 migrants | Cross-sectional, multicentric, Population based |
KAP, Migration and reverse migration questionnaire | Family concerns, unemployment, decreased self-esteem, multiple psychosocial issues. |
The large population-based observational study of a sample of 35,000 was reported from the states of Bihar, Jharkhand, Uttar Pradesh, and Karnataka. 6 The authors collected data from helpline records established to address the various psychosocial issues of the migrants.7, 8 Eighty percent of migrants from these four states received no government aid. Similarly, in an online survey, the authors examined the impact of joblessness following the pandemic on income and remittances of 451 migrants in the northeast region. 10 Some studies examined psychosocial and mental health issues of migrants staying in shelter homes established at various places by the Government of India.8, 9
Literature on Psychosocial Issues
Living conditions,6, 7, 11, 12, 16–18 basic needs,11, 12 housing,13, 14 transport facility,6, 7, 9 family concern,6, 9 risk of infection,8, 9 issues of children and women,5, 6, 7, 11, 12 poverty,10–12 unemployment,10–12 future insecurity,9, 13 and inadequate social support3, 6, 7 were the predominant psychosocial issues reported. The research work was from 13 states and one union territory, including state Bihar, Jharkhand, Uttar Pradesh, Kerala, Karnataka, Delhi, Chandigarh, Punjab, Haryana, Rajasthan, Odisha, West Bengal, and Gujarat, Assam.6–14 The native places of the migrants were Bihar, Jharkhand, Uttar Pradesh, Karnataka, and West Bengal.6, 7, 11 The psychosocial support and measures were better in Kerala than other states. 7 The interstate migrant policy index and social indicators were found to be the highest in Kerala. 7
In one cross-sectional study that highlighted joblessness issues, the migrants remained jobless for two months and failed to send remittances to their families. 10 The psychosocial impact of joblessness was observed more in elderly migrants. In a multicentric study, the authors administered migration questionnaire to 551 participants staying in shelter homes. They found that the participants feared contracting COVID-19 and were uncertain about return to their native places. 9 Twenty percent reported that they had no place to stay. 9 Thirty-eight percent went home due to family pressure. The financial issues revealed were the need to support the family during harvesting season and better job opportunities back home. Twelve percent of the participants reported termination of the job by the employer.9, 11
A population-based large-scale study of 25,371 migrants reported that 40% of them faced food scarcity. 12 Similar finding was also revealed in another study: 40% experienced psychosocial issues related to the lack of access to food, housing, and living conditions. 11
Some studies discussed the mode of transport used by the migrants in reaching their native places.6, 7, 11 They reported that 51%–83% of the participants made the journey by bus and train and 6%–10% made the journey on foot.6, 7, 11 The majority of the migrants were psychologically distressed and showed a lack of resilience to the pandemic crisis.4, 6 Another article explained that an understanding of migration and livelihood would be helpful in designing a mitigating strategy for the psychosocial impact of COVID-19. The authors emphasized that the migrants suffer from the dual burden of being poor and migrants. 19 The migrants in informal sectors faced significant psychosocial issues and had to bear the difficulties of survival.14, 10 India’s maximum migrants work in the informal sectors. During the COVID-19 pandemic, many lost their jobs overnight and did not get any compensation. In one report, there was a significant association between human development index indicators in state’s informalization processes. 14
Besides these original research, other published literature comprised commentaries, viewpoints, editorials, letters to editors, opinions, and reviews. Largely, these articles discussed the experiences and factors of reverse migration.16, 17, 20–30, 38 The psychosocial issues discussed also included sources and destination points of vast migration,30–32, 33 history of migrants’ sufferings,31–33 the trend of migration and historical trajectories,6, 34, 22, 24–26, 35 informal sectors’ concern, 30 and socioeconomic challenges.20, 21, 24–26, 35
Some articles discussed the psychosocial interventions and approach of primary care physicians for minimizing the mental health and psychosocial issues of the migrants.27–29 Brief psychosocial interventions and community outreach services program were found to be useful in resolving mental and psychosocial issues of the migrants.27–29
Literature on Mental Health Issues
A small number of studies found some migrants to have mental health issues.6–9, 15 In a North Indian study, the prevalence of substance use was found to be higher among migrants than the general population. 8 The prevalence of ever use for all the substances was 44%, ever use of alcohol was 16%, and the current use of alcohol was 11% among migrants. The authors reported the prevalence of ever use of cannabis was 4% and tobacco use were 36% in their study. 8 Another study revealed that the migrants had decreased self-esteem, poor socialization, and were facing multiple mental health issues. They were feeling helpless, suffering from anxiety, and fearing death. Fear of getting infection was reported by 16% of migrants. Twenty percent (20%) reported that they had felt low and gloomy, and 19% reported restlessness. 9 Marked psychological distress, insomnia, deliberate self-harm, severe depressive symptoms were reported. At least one psychiatric diagnosis (depressive disorder) was found to be significantly higher among the migrants than the general population. 9 Another study from North India, published as letter to the editor, reported that 73% of the migrants screened positive for depression. 18 There have been some reports of severe anxiety, panic disorder, increased susceptibility to major depressive disorder with psychotic symptoms, and suicidal risk.21, 24, 27
A population-based study of 353 migrants found mental stress and anxiety in 31% of the participants. 11 In an experiential report from Karnataka, 15 13 migrants were found to have a pre-existing psychiatric disorder, five were diagnosed with new-onset psychiatric disorders, and five were referred for further psychiatric care. The authors reported that the mental health team made available supported in the migrants’ camps and shelter homes, and brief psychosocial interventions helped in decreasing the distress of the migrants. 15
Some other articles published as editorials, commentaries, viewpoints, opinions, perspectives, or letters to the editor focused on the development of fear; anxiety, depressive, and other common mental disorders (CMDs); and related issues among the migrants.18, 21, 22, 36, 37 In an editorial, the mental health implications and suicide-related issues among the migrants from various states of India was highlighted. 21 The author reported that migrants faced multiple concerns related to starvation, fear of getting infected, job loss, family issues, and CMDs. 21 Similar reports documented that the painful experiences of migrants were precipitated with the lockdown during the COVID-19 pandemic and they faced severe mental stress, starvation, suicide, and roadside accidents. 38 The mental health status of the migrants was reported as poor in Odisha and they were facing uncertainty for future living prospects. 36 The large number of published articles highlighted the need for psychosocial and mental health care for migrants.6–9, 13, 18, 36, 21, 37, 22
Discussion
The present review represents literature about the psychosocial and mental health issues of the migrants during contemporary pandemic times. At the time of COVID-19 pandemic outbreak in India, the migrants constituted the most vulnerable group for developing psychosocial and mental health issues, given their economic and stressful environmental situations. The research findings have been synthesized from different parts of India. A systematic review was not feasible due to the small number and heterogeneous nature of studies, variability in the number of participants, and variable living conditions of migrants in different states of India. Thus, a narrative review was undertaken
The majority of studies elucidated multiple psychosocial issues and some authors reported about usefulness of brief psychosocial support.6, 9, 15, 28, 37 Living conditions, basic needs, housing, transport facility, family concern, risk of infection, issues of children and women, poverty, unemployment, and insecurity about future were predominant psychosocial issues reported. The social support indicators were found to have a positive impact on the mental status of migrants.6, 14 The joblessness issues were also looked at in a cross-sectional study. 10 The psychosocial impact of joblessness was observed more in elderly migrants. Some studies reported poor mental health care in states like Odisha, Bihar, and Uttar Pradesh.6, 17, 36 The migrants received optimal social security measures in Kerala.6, 21
The prevalence of substance use was found to be higher among migrants than the general population. 8 The prevalence of (at least) one psychiatric diagnosis was 19% among reverse migrants. The prevalence of ever use for all the substances was 44%, ever use of alcohol was 16%, and the current use of alcohol was 11% among the migrants. In a study from North India, 73% of the migrants screened positive for at least one psychiatric disorder. Fifty-one percent of the migrants screened positive for both depression and anxiety. 18 The majority of findings revealed severe mental stress, starvation, suicide, and roadside accidents among migrants.8, 9, 10, 15, 27 Basic psychosocial measures in the form of a multidisciplinary approach for minimizing various crisis situations were attempted, with positive outcomes.15, 18, 37 The mental health team support and brief psychosocial support helped in decreasing the distress of the migrants and their fear of threat to survival.15, 34, 37 The psychosocial services were provided to migrants by district mental health team at Chandigarh and Bengaluru. Regular assessment and early intervention of mental disorders were undertaken. Telepsychiatry services with a helpline for mental health issues was utilized by migrants.
In a large-scale international survey, 33 migrant’s mental health issues were assessed in the context of COVID-19. The findings of this survey revealed that daily stressors of basic needs, medical needs, and social needs were found to have a significant association with the mental health issues of the migrants. The other findings of this global survey were that the perceived discrimination among migrants had a significant effect on their anxiety and depression. In the present review, many Indian researchers reported similar findings of the significance of basic needs, living conditions, and mental health issues among migrants. Similar to the present review, in a systematic review of mental health among migrants before COVID-19, Mucci et al. 39 reported that migrants showed an increase in the incidence of psychiatric disorders due to loss of social status and separation from the families. The important emerging disorders were depressive disorders, anxiety disorders, alcohol or substance abuse, and poor sleep quality. Similar findings of psychiatric morbidity among migrants were found in the present review during COVID-19 even though the number of studies was small. Mucci et al. 39 emphasized the role of promotion in the well-being of migrants.
Fernandes et al. 40 reported specific somatic and psychiatric conditions among migrants, particularly women, as a result of deterioration of their mental health and psychosocial status. The specific conditions were backache, shoulder pain, headache, various psychiatric disorders, and suicide. In the present review, somatic-specific conditions and sex-specific reports were lacking. The previous international studies of mental health issues among migrants were more focused on first-generation migrants coming from low-income countries and previous researchers studied cross-cultural issues. Zhong et al. 41 found that psychological distress was more prevalent in the newer rather than older generation migrants (36.2% vs. 28.2%). In the present review conducted in the period of COVID-19, the cross-cultural issues and psychiatric morbidity among first or second-generation migrants were not separately reported, though it would have given a better understanding of the psychosocial status of migrants.
Implications for Practice
In the literature, there is an association of social parameters such as joblessness, income, housing, and living conditions with common mental disorders (CMDs) in general population. 29 The etiology of psychiatric disorders is multifactorial and include biological and psychosocial factors. The COVID-19 pandemic acted as a precipitant in exacerbating the mental health crisis in the migrants in India. The anxiety and stress were not only due to the fear of contracting COVID-19 infection but also related to their family concerns, joblessness, poverty, lack of housing, and uncertainty about future. The Government of India also realized this mental health crisis and issued guidelines for psychosocial support and telepsychiatry services to them in community outreach programmes. 42
The periodic screening for CMD and psychological stress among migrants was a component of successful intervention. This approach helped in managing migrants’ psychosocial issues. This strategy was based on the fact that an integrated mental health service with trained manpower was the need of the hour to handle such a critical situation in India. Basic mental health care services and telepsychiatry services need to be prioritized at the district and primary health care levels.11, 15, 37, 28
Implications for Policy and Research
There was no uniform national policy or strategy to handle the migrant crisis in India during the COVID-19 pandemic.19, 35 The state health authorities adopted the psychosocial support measures, which were initially sluggish in some states, with a lack of concern related to migrant distress during the pandemic crisis. 6 The COVID-19 pandemic crisis raised several lessons for social scientists, policy planners, and mental health experts. This review will help them in better understanding of various psychosocial and mental issues of migrants during this crisis. 19
To reach the unreached migrant population, policy planners should think and plan of regular registration facilities and mobile apps for migrants. An integrated mental health awareness drive among them also helped them in utilizing various psychosocial and mental health services and social welfare schemes by the Government of India.15, 42 The migrant population should be incorporated into the mainstream of general population by providing them social, legal, health, and occupational security.35, 42 It was found that the destination state’s social protective policy played an important role in resolving the psychosocial issues of the migrants. 14 Poverty measurements serve as justification for state social protection measures. It is better to identify the poor migrants and deliver social welfare schemes to them.. The long-term mental health implication of this migrant crisis needs to be further studied so that proper policy decision could be taken in future pandemic conditions. Government schemes of One Nation One Ration Card should be implemented on a priority basis. 35 In a future eventuality, migrant population’s social measures must be kept in mind in disaster planning so that their sufferings could be minimized. Decentralization is an important strategy to provide services to the migrants.11, 12, 15, 19 Health insurance scheme needs to be initiated, better coordination needs to be ensured between government agencies and migrants population, and housing conditions need to be addressed so that migrants are able to live in dignity, peace, security, and safety.11, 12, 15, 19, 44 The present review suggests the need for more research in this area and the adoption of mental health and psychosocial intervention for migrants in clinical practice at various levels.
Limitations
This review has some methodological limitations, which include small sample sizes, weak statistical analyses, and limited scope of some studies. Only nine studies were original research. The published literature mostly comprised commentaries, viewpoints, editorials, opinions, and letters to the editor. The studies were less in number. Further long-term multicenter studies with standardized assessments and large sample size are warranted to replicate the findings of this review.
Conclusion
Majority of research articles highlighted the need for psychosocial and mental health care for migrants. Predominant psychosocial issues found among migrants were living conditions, basic needs, risk of infection, issues of children and women, family concerns, joblessness, transport and housing facilities, and future insecurity. The mental health issues found included psychological distress, depressive disorders, anxiety disorders, and substance use disorders. Brief psychosocial interventions and integrated comprehensive mental health care approach for migrants were found useful in resolving their mental and psychosocial issues.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Guttmann AF, Gandhi S, Wanigaratne S, et al. COVID-19 in immigrants, Refugees and other newcomers in Ontario: Characteristics of those tested and those confirmed positive. http://www.ices.on.Ca. (2020, accessed on August 20, 2021)
- 2.Banerjee D and Bhattacharya P. “Pandemonium of the pandemic”: Impact of COVID-19 in India, focus on mental health. Psychol Trauma, 2020; 12 588–592. [DOI] [PubMed] [Google Scholar]
- 3.Sengupta S and Jha MK. Social policy, COVID-19 and impoverished migrants: Challenges and prospects in locked down India. The Int J Community Soc Dev, 2020; 2 152–172. [Google Scholar]
- 4.Kumar S and Choudhury S. Migrant workers and human rights: A critical study on India’s COVID-19 lockdown policy. Soc Sci Humanit Open, 2021; 3: 100130. [Google Scholar]
- 5.Choudhari R. COVID-19 pandemic: Mental health challenges of internal migrant workers of India. Asian J Psychiatr, 2020; 54: 102254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adhikari A, Goregaonkar N, Narayanan R, et al. Manufactured Maladies: Lives and livelihoods of migrant workers during COVID-19 lockdown in India. Indian J Labour Econ, 2020; 63 969–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rao N, Narain N, Chakraborty S, et al. Destinations matter: Social policy and migrant workers in the times of COVID. Eur J Dev Res, 2020: 32: 1639–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chavan BS, Sidana A, Arun P, et al. Psychiatric morbidity and substance use in migrant workers: A population-based study. Int J Soc Psychiatry, 2021: 20764020988881. [DOI] [PubMed] [Google Scholar]
- 9.Chavan BS, Sidana A, Arun P, et al. Factors leading to reverse migration among migrant workers during the COVID-19 pandemic: A multicenter study from Northwest India. Prim Care Companion CNS Disord, 2021; 23: 20m02810. [DOI] [PubMed] [Google Scholar]
- 10.Guha P, Islam B, and Hussain M. COVID-19 lockdown and penalty of joblessness on income and remittances: A study of inter-state migrant labourers from Assam, India. J Public Affairs, 2020: e2470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaudhary S. In search of home: A study on migrant workers’ access to housing and land. Housing and Land Rights Network, 2020. [Google Scholar]
- 12.Gaon Connection. Gaon Connection Survey: COVID-19 lockdown and reverse migration. Gaon Connection, https://en.gaonconnection.com/gaon-connection-survey-decoding-reverse-migration-the-COVID-19-lockdown-led-to/ (2020, assessed on July 10, 2021). [Google Scholar]
- 13.Gupta P and Sengupta A. A qualitative analysis of social scientists’ opinions on socioeconomic and demographic implications of the lockdown during COVID-19 in India. J Public Aff, 2020: e2531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Das D. Regional disparities of growth and internal migrant workers in informal sectors in the age of COVID-19. J Public Aff, 2020: e2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chander R, Murugesan M, Ritish D, et al. Addressing the mental health concerns of migrant workers during the COVID-19 pandemic: An experiential account. Int J of Soc Psychiatry, 2020: 20764020937736. [DOI] [PubMed] [Google Scholar]
- 16.Mukherjee S. Disparities, desperation, and divisiveness: Coping with COVID-19 in India. Psychol Trauma, 2020; 12 582–584. [DOI] [PubMed] [Google Scholar]
- 17.Jha SS and Lahiri A. Domestic migrant workers in India returning to their homes: emerging socioeconomic and health challenges during the COVID-19 pandemic. Rural Remote Health, 2020; 20: 6186. [DOI] [PubMed] [Google Scholar]
- 18.Kumar K, Mehra A, Sahoo S, et al. The psychological impact of COVID-19 pandemic and lockdown on the migrant workers: A cross-sectional survey. Asian J Psychiatr, 2020; 53: 102252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhagat RB, Reshmi RS, Sahoo H, et al. The COVID-19, migration and livelihood in India. A Background Paper for Policy Makers, IIPS Analytical Series on COVID-19; No. 13054, https://iipsindia.ac.in/sites/default/files/iips_covid19_mlli.pdf (2020, accessed September 3, 2021).
- 20.Joob B and Wiwanitkit V. COVID-19 and migrant workers: Lack of data and need for specific management. Public Health, 2020; 183: 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh O. Mental health of migrant laborers in COVID-19 pandemic and lockdown: Challenges ahead. Indian J Psychiatry, 2020; 62 233–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suresh R, James J, and Balraju RSJ. Migrant workers at crossroads-the COVID-19 pandemic and the migrant experience in India. Soc Work Public Health, 2020; 35 633–643. [DOI] [PubMed] [Google Scholar]
- 23.Dalal PK, Roy D, Choudhary P, et al. Emerging mental health issues during the COVID-19 pandemic: An Indian perspective. Indian J Psychiatry, 2020; 62: S354–S64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mohan M and Mishra S. India’s response to the COVID-19 pandemic: A frontal assault on the “Historically Dispossessed.” Int J Health Serv, 2020; 51 107–114. [DOI] [PubMed] [Google Scholar]
- 25.Agoramoorthy G and Hsu MJ. How the Coronavirus lockdown impacts the impoverished in India. J Racial Ethn Health Disparities, 2021; 8 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jayaram N and Varma D. Examining the “Labour” in labour migration: Migrant workers’ informal work arrangements and access to labour rights in urban sectors. Indian J Labour Econ, 2020: 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nelson VM. Suicide Prevention India Foundation, http://www.rfi.fr/en/international/20200514-mental-illness-suicides-on-the-rise-in-india-during-COVID-19-lockdown (2020, August 20, 2021).
- 28.Manjunatha N, Naveen Kumar C, Math SB, and Jagadisha T. Clinical schedules for primary care psychiatry: 2.3 (COVID Version). National Institute of Mental Health and Neurosciences, http://nimhans.co.in/wpcontent/uploads/2020/05/CSP-2.3-COVID-19-May-2020.pdf. (2020, August 20, 2021). [Google Scholar]
- 29.Weich S and Lewis G. Poverty, unemployment, and common mental disorders: Population based cohort study. BMJ Clinical Res, 1998, 317 115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yadav S and Priya KR. Migrant workers and COVID-19: Listening to the unheard voice of invisible India. J Anthropological Sur India 2020. (December 1), 10.1177//2277436X20968984. [DOI] [Google Scholar]
- 31.Dandekar A and Ghai R. Migration and reverse migration in the age of COVID-19. Econ Pol Wkly, 2020; 4 28–31. [Google Scholar]
- 32.Patel JA, Nielsen F, Badiani AA, et al. Poverty, inequality and COVID-19: The forgotten vulnerable. Public Health, 2020; 183 110–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Beerden ES, Verelst A, Devlieger I, et al. Mental health of refugees and migrants during the COVID-19 pandemic: The role of experienced discrimination and daily stressors. Int J Environ Res Public Health, 2021; 18: 6354, 10.3390/ijerph18126354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kumar R. Migrant in my own country: The long march of migrant workers in India during the COVID-19 pandemic 2020-Failure of postcolonial governments to decolonize Bihar and rebuild Indian civilization after 1947. J Family Med Prim Care, 2020; 9 5087–5091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krishnamurty J. An employment guarantee for the urban worker. Indian J Labour Econ, 2020: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mohapatra RK, Das PK, and Kandi V. Challenges in controlling COVID-19 in migrants in Odisha, India. Diabetes Metab Syndr, 2020; 14 1593–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lakhan R, Kosgi S, Agrawal A, et al. Letter to editor: Re: “Primary care physician’s approach for mental health impact of COVID-19”: Case of migrant workers mental health. J Family Med Prim Care, 2020; 9 5394–5396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mukhra R, Krishan K, and Kanchan T. COVID-19 sets off mass migration in India. Arch Med Res, 2020; 51 736–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mucci N, Traversini V, Giorgi G, et al. Migrant workers and psychological health: An umbrella review. Sustainability, 2019; 11: 232. [Google Scholar]
- 40.Fernandes C and Pereira A. Exposure to psychosocial risk factors in the context of work: A systematic review. Rev Saude Publica, 2016; 50: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhong BL, Chan SSM, Liu TB, et al. Mental health of the old- and new-generation migrant workers in China: Who are at greater risk for psychological distress? Oncotarget, 2017; 8 59791–59799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Government of India. Psychological issues among migrants during COVID-19, https://www.mohfw.gov.in/pdf/RevisedPsychosocialissuesofmigrantsCOVID19.pdf (2020, accessed on July 5, 2021).
- 43.Singh SK, Patel V, Chaudhary A, and Mishra N. Reverse migration of labourers amidst COVID-19. Econd Pol Wkly, 2020; 55 28–31. [Google Scholar]
- 44.Rajan I, Sivakumar P, and Srinivasan A. The COVID-19 pandemic and internal labour migration in India: A “Crisis of Mobility” S. Indian J Labour Econ, 2020; 63 1021–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]