Abstract
Objectives:
GGreen pit vipers (GPV) envenomation causes consumptive coagulopathy mainly by thrombin-like enzymes. Fibrinogen levels are generally investigated to help evaluate systemic envenomation. However, tests of fibrinogen levels may not be available in every hospital. This study aimed to determine the sensitivity, specificity and accuracy for a range of various coagulation tests (20 minute whole blood clotting test (20WBCT), prothrombin time, international normalized ratio and thrombin time (TT)), comparing to the two gold standards performed in patients with GPV bite.
Methods:
This was the pilot study which we retrospectively reviewed fibrinogen level results including the hospital records of 24 GPV (Trimeresurus albolabris or macrops) bite patients visiting Ramathibodi Hospital, Thailand during 2013–2017 with 65 results of fibrinogen levels. The fibrinogen levels <164 and <100 mg/dL were used as the standard cut-off points or gold standards as the abnormal low and critical levels, respectively.
Results:
Most were male. All had local effects. For fibrinogen levels <164 and <100 mg/dL, prolonged TT had the highest sensitivity of 57.1% and 82.4%; the negative predictive value of 74.5% and 93.6%; the accuracy of 81.0% and 92.1%; and the area under a receiver operating characteristic curve of 0.762 and 0.873, respectively. For fibrinogen levels <164, unclotted 20WBCT and prolonged TT had the highest specificity and positive predictive value of 100% all. For fibrinogen levels <100, unclotted 20WBCT had the highest specificity and positive predictive value of 100% both, while prolonged TT had the specificity and positive predictive value of 95.7% and 87.5%, respectively. One patient developed isolated thrombocytopenia without hypofibrinogenemia and coagulopathy.
Conclusions:
Among four coagulation tests, TT was the most sensitive and accurate test to indicate hypofibrinogenemia in GPV bite patients. In case of unavailable fibrinogen levels thrombin time might be investigated to help evaluate patients’ fibrinogen status. Isolated thrombocytopenia could occur in GPV envenomation.
Keywords: Green pit vipers, Trimeresurus spp., thrombin time, fibrinogen, accuracy of tests
Introduction
Snakebites are an important public health problem worldwide. One of the most important effects of snake envenomation is hematologic abnormalities including coagulopathy, most commonly a venom-induced consumption coagulopathy (VICC). 1 Venom-induced activation of the coagulation pathway results in consumption of clotting factors and coagulopathy. The toxins in snake venom that produce VICC are commonly classified by where they act on the coagulation pathway such as prothrombin activators or thrombin-like enzymes (TLEs). VICC can be diagnosed based on a history of snakebite together with evidence of coagulopathy due to clotting factors consumption. 1 The VICC can be confirmed by an abnormal coagulation tests including abnormal prothrombin time (PT), or international normalized ratio (INR), low fibrinogen and an elevated D-dimer. 1
The TLEs naturally consume fibrinogen rather than activating the clotting pathway. Therefore, TLEs generally generate an isolated deficiency of fibrinogen and infrequently affect other clotting factors. 1 Fibrinogen plays an important role in maintaining hemostasis. It is a key factor for effective clot formation and without it, hemostasis is disrupted and bleeding occurs. 2
In Thailand, green pit vipers (GPV) (Trimeresurus spp. in subfamily Crotalinae, family Viperidae) are one of the most common three medically important venomous snakes which cause hematotoxic effects (Daboia siamensis or Russell’s vipers, Calloselasma rhodostoma or Malayan pit vipersand Trimeresurus spp. or GPV). 3 The GPV is distributed throughout the country and is commonly encountered by people. 3 GPV venom mainly activates pathways of blood coagulation by TLEs resulting in VICC which causes hypofibrinogenemia and defibrination syndrome. 4 Fibrinogen are low in some GPV envenomated patients with different severity.4,5
GPV bites are medical emergencies, with envenomation occasionally resulting in systemic bleeding.6,7 Systemic bleeding such as intracerebral hemorrhage from envenomation might affect or change the outcomes of patients. So, the treatment with antivenom aims to neutralize procoagulant toxins, allow the recovery of clotting factors and reverse the hematotoxic effect1,4 and then may contribute to prevent the major or systemic bleeding. Fibrinogen levels are routinely evaluated to help diagnose systemic envenomation and assess bleeding risk in vipers bite patients.6,7 A fibrinogen level 100 mg/dL was used as a critically low levels during major hemorrhage. 2 Some current treatment guidelines for massive bleeding recommend maintaining the fibrinogen level >100 mg/dL. 2 Some experts recommended this level as the standard cut-off point for initiation of treatment for GPV envenomation. 5
However, in some area, particularly rural hospitals, where laboratories are not fully equipped to analyze some special tests, fibrinogen assays might not be able to be investigated. Therefore, the other basic coagulation tests are required for patients’ evaluation and follow-up. These include 20 minute whole blood clotting test (20WBCT), conventional venous clotting time (VCT), PT with INR and the partial thromboplastin time (PTT);5,6,8 they were used to evaluate hematotoxic effect including hypofibrinogenemia in GPV bite patients. 5 Currently, the criteria for antivenom administration of snakebite’s management guideline of WHO in Southeast Asia includes unclotted 20WBCT, INR >1.2 or prolonged PT >4–5 s longer than laboratory control value, and platelet count <100,000/L. 9 The indications for antivenom treatment of venomous snakebite’s management guideline of Queen Saovabha Memorial Institute (QSMI), The Thai Red Cross Society (TRCS), Thailand are systemic bleeding, unclotted 20WBCT or prolonged PT, platelet count <50,000/L, severe pain and swelling suspected of compartment syndrome. 10
Thrombin time (TT) is a simple coagulation assay. It reflects the conversion of fibrinogen to fibrin after adding of thrombin reagent. TT is used as a screening test to detect of both qualitative and quantitative fibrinogen abnormalities and evaluation of fibrin formation disorders. 11 TT is reported to be more sensitive to hypofibrinogenemia than either PT or activated partial thromboplastin time (aPTT) in patients with GPV bite; nevertheless, the authors did not extensively evaluate the accuracy, sensitivity and specificity of TT to indicate low fibrinogen levels in GPV bite victims. 8 TT might be a useful test to help evaluate the fibrinogen levels of envenomated patients.
This clinical study was undertaken to evaluate the sensitivity, specificity, positive predictive value, negative predictive value, accuracy and the area under the receiver operating characteristic (ROC) curve (AUC) of unclotted 20WBCT, prolonged PT, prolonged INR and prolonged TT comparing to fibrinogen levels <164 mg/dL (abnormal low levels) and <100 mg/dL (critical levels) in GPV bite victim.
Materials and methods
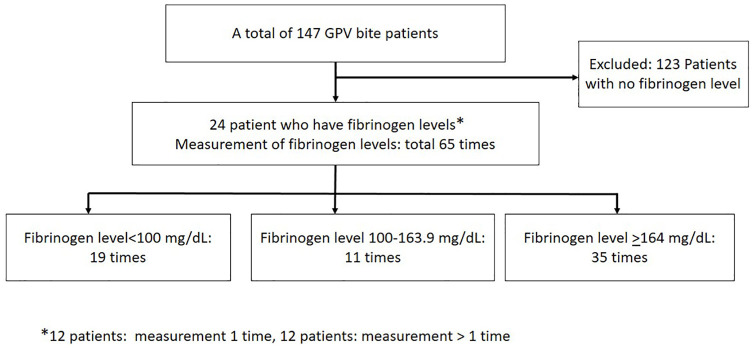
We performed the pilot study by retrospective review of medical records of patients with GPV bite who visited Ramathibodi Hospital (a tertiary teaching hospital), Bangkok, Thailand during 2013–2017. Patients with ICD-10 codeT63.00 (Snake venom, hematotoxin) were reviewed. We included all patients who were diagnosed of GPV bite with fibrinogen levels results and other hematologic laboratory investigations at the time of hospitalization for snakebite including complete blood count, 20WBCT, PT, INR and TT (Figure 1). We excluded patients with known underlying coagulopathy or thrombocytopenia. The results of complete blood count, fibrinogen levels, PT, INR and TT were analyzed and reported by our hospital laboratory. The PT, INR, PTT, TT and fibrinogen levels were determined by using the Sysmex CS 2500 Coagulation analyzer (HQ; Kobe, Japan). Fibrinogen levels were analyzed by using a clotting-based Clauss method (Siemens Healthineers, USA). During the study period, the normal range of fibrinogen levels, PT, INR and TT of our hospital’s laboratory were 164–400 mg/dL, 10.5–13.5 s, 0.91–1.17 and 10–13 s, respectively. The 20WBCT was performed following WHO snakebite guideline. 9 The diagnosis of GPV bite was made via identifying the snake’s carcass or patient’s clear identification of snakes or the diagnosis of snakebite together with hematologic abnormalities, in conjunction with occurrence of bites in Bangkok, the capital city. By epidemiologic data, among three most common hematotoxic venomous snakes in Thailand, only GPV inhabits in Bangkok, with the two most common species as Trimeresurus albolabris and Trimeresurus macrops.3,9 Therefore, we concluded that all of our patients were bitten by GPV (T. albolabris or T. macrops). Demographic data, medical history and laboratory results analyzed by Ramathibodi Hospital’s laboratory were collected. Some patients were investigated with these laboratory results more than one time. The fibrinogen level <164 mg/dL (levels with lower than normal levels) and <100 mg/dL were used as the gold standards or cut-off fibrinogen levels for the abnormal fibrinogen level and critical level, respectively. The 20WBCT, PT, INR and TT, which were measured at the same time with each of fibrinogen levels, were compared to these two cut-off fibrinogen levels. Then the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), accuracy and the AUC of the abnormal laboratory results (unclotted 20WBCT, INR > 1.2, TT and PT > upper normal levels of our laboratory during the study period) were determined and used as our primary outcomes. These were aimed to assess their abilities to indicate hypofibrinogenemia in GPV bite patients over the course of the patients’ hospitalization.
Figure 1.
Patients’ flow diagram.
For statistical analyses, we used PASW Statistics for Windows, Version 18 (SPSS Inc., USA) to collect and analyze the data. The mean and standard deviation were used for continuous data with normal distribution; otherwise, the median with minimum and maximum were used. The frequency and percentage were used for categorical data analysis.
Results
During 5 years, there were a total of 147 GPV bite patents. Only 24 patients who had the investigations that were required for analysis were included in our study. All were bitten in Bangkok. Six patients brought snakes to the hospital. Most (58.3%) were male with the median age of 57 years. Feet were the most common bite site (70.8%). All had local effects as wound swelling. Demographic data including abnormal laboratories findings were described in Table 1. Following the venomous snakebite’s management guideline of QSMI, TRCS, Thailand, 10 seven patients received Thai Red Cross antivenoms (Table 1). One had bleeding per gum. No severe systemic bleeding and death occurred. Twelve patients were measured for fibrinogen levels and the other laboratory results more than 1 time (median, 2 times; range, 2–7 times).
Table 1.
Demographic data and laboratories findings of patients.
| Characteristics | Number of patients (%) |
|---|---|
| Gender | |
| Male | 14 (58.3) |
| Female | 10 (41.7) |
| Age in years, median (min-max) | 57 (10–84 years) |
| Bite site | |
| Feet | 70.8% |
| Hands | 29.2% |
| The time to the hospital, median (min-max) | 1.25 h (30 min–16 h) |
| Fang marks | |
| Identified (obviously visible) | 24 (100) |
| Local effects | 24 (100) |
| Abnormal Laboratories findings | |
| Fibrinogen level <100 mg/dL | 19 (29.2) |
| Fibrinogen level 101–163 mg/dL | 11 (16.9) |
| Unclotted 20WBCT | 3 (12.5) |
| Prolonged PT (>13.5 s) (normal PT 10.5–13.5 s) | 6 (25.0) a |
| Prolonged INR (>1.2) (normal INR 0.91–1.17) | 5 (20.8) |
| Prolonged TT (>13 s) (normal TT 10–13 s) | 6 (25.0) |
| Platelet < 100,000/mm3 (normal platelet 140–450 × 103 mm3) | 5 (20.8) |
| Thai Red Cross Antivenom treatment b | 7 (29.2) |
| Prolonged INR (>1.2) | 3 |
| Platelet <100,000/mm3 | 2 |
| Unclotted 20WBCT | 1 |
| Prolonged INR (>1.2) and unclotted 20WBCT | 1 |
20WBCT: 20 minute whole blood clotting test; PT: prothrombin time; INR: international normalized ratio; TT: thrombin time.
From WHO guideline’s criteria 9 (PT > 4–5 s longer than laboratory control value): only two patients had prolonged PT >4–5 s longer than laboratory control value.
Treatments following the indications for antivenom treatment of venomous snakebite’s management guideline of QSMI, The TRCS, Thailand. 10
A total of 65 fibrinogen levels which were measured at the median interval between each test of 8 h (range, 4–35 h) during hospitalization were reported and used as the gold standard to compare to other tests results from envenomed patients. Twenty-three out of 65 fibrinogen levels were measured after antivenom treatment. For all patients who were treated with the antivenom, their abnormal coagulation tests results were improved and finally resolved after the antivenom administration. Table 2 showed sensitivity, specificity, PPV, NPV, accuracy and AUC of unclotted WBCT, INR > 1.2, TT and PT > upper normal levels of our laboratory during the study period compared to the two fibrinogen level gold standards. All patients had normal PTT. Two patients in our study developed isolated thrombocytopenia. Both had improvement of thrombocytopenia after antivenom therapy. However, one patient’s platelet count increased significantly (from 3000 to 75,000/mm3 after antivenom treatment), but it did not reach to the normal level of platelet count. He had normal PT, INR and fibrinogen levels. Then he was investigated and finally diagnosed as myelodysplastic syndromes (a group of diverse bone marrow disorders) during the outpatient follow-up. Another female patient had isolated thrombocytopenia with normal coagulation test and fibrinogen levels. She had normal PT, INR and all fibrinogen levels which were measured for 5 times during hospital admission. The lowest platelet count was 25,000/mm3. She received one dose of GPV monovalent antivenom and completely recovered with normal platelet count.
Table 2.
The sensitivity, specificity, positive predictive value, negative predictive value, accuracy and area under the ROC curve of 20WBCT, prolonged PT, prolonged INR and prolonged TT compared to fibrinogen levels <100 and <164 mg/dL.
| Fibrinogen levels (number of laboratory results) | Variable | Unclotted 20WBCT (N = 38) | PT > 13.5 s (10.5–13.5) (N = 64) | INR > 1.2 (0.91–1.17) (N = 65) | TT > 13 s (10–13) (N = 63) |
|---|---|---|---|---|---|
| Number of laboratory abnormal results (%) | 4 (10.5) | 8 (12.5) | 7 (10.8) | 16 (25.4) | |
| <164 mg/dL (N = 30) | Sensitivity (%) | 20.0 | 20.7 | 20.0 | 57.1 |
| Specificity (%) | 100 | 94.3 | 97.1 | 100 | |
| Positive predictive value (%) | 100 | 75.0 | 85.7 | 100 | |
| Negative predictive value (%) | 52.9 | 58.9 | 58.6 | 74.5 | |
| Accuracy (%) | 57.9 | 60.9 | 61.5 | 81.0 | |
| Area under the curve | 0.600 (0.419–0.481) | 0.566 (0.405–0.727) | 0.557 (0.396–0.718) | 0.762 (0.617–0.907) | |
| <100 mg/dL (N = 19) | Sensitivity (%) | 33.3 | 33.3 | 26.3 | 82.4 |
| Specificity (%) | 100 | 95.7 | 95.7 | 95.7 | |
| Positive predictive value (%) | 100 | 75.0 | 71.4 | 87.5 | |
| Negative predictive value (%) | 76.5 | 78.6 | 75.9 | 93.6 | |
| Accuracy (%) | 78.9 | 78.1 | 75.4 | 92.1 | |
| Area under the curve | 0.667 (0.462–0.871) | 0.630 (0.439–0.821) | 0.603 (0.412–0.795) | 0.873 (0.732–1.000) |
ROC: receiver operating characteristic; 20WBCT: 20 minute whole blood clotting test; PT: prothrombin time; INR: international normalized ratio; TT: thrombin time.
Discussion
GPV envenomation mostly causes only local symptoms; however, hematologic abnormalities and systemic bleeding including deaths could occur.6,7,12 Prompt antivenom administration to snakebite patients who develop and show the systemic effects is necessary to help prevent systemic or major bleeding. The range of different coagulation tests were used to help identify the patients who were envenomated and developed systemic effects.
The prolonged PT mainly reflects a coagulation factor deficiency state of extrinsic and final common pathways. 13 The unclotted 20WBCT is found to be reliable as an indicator of low plasma fibrinogen concentration in patients envenomed by Bothrops snakes. 14 However, in one study, the 20WBCT shows low sensitivity for detecting coagulopathy in Russell’s viper envenoming. 15 For GPV bite, one study demonstrates that 20WBCT and INR have the high sensitivity to indicate severe hypofibrinogenemia but TT was not included in that study. 5
Of 24 GPV envenomed patients where data was available, prolonged TT had the highest sensitivity, NPV, accuracy and AUC among four tests to indicate these two low fibrinogen levels, especially in patients with the fibrinogen level <100 mg/dL.
Since different coagulation tests are designed toward the detection of different coagulation factors and cellular components of clotting. TT is used to detect fibrinogen abnormalities and evaluate fibrin formation disorder, 11 so this supported our findings that prolonged TT had the highest sensitivity, NPV, accuracy and AUC and also had high specificity.
Therefore, in case of unavailable fibrinogen levels such as no laboratory analysis, TT might be considered to be the screening test for hypofibrinogenemia in GPV envenomation and the abnormal TT might indicate the requirement for antivenom to prevent major bleeding. In the situations of shortages of antivenoms, TT might play some role to facilitate the proper selection priority of the patients for antivenom treatment. From our finding, TT should be studied further especially in the larger studies which include more patients with GPV bite or in patients with other hematotoxic snake envenomation such as Malayan pit vipers.
Interestingly, one patient developed isolated severe thrombocytopenia without hypofibrinogenemia and coagulopathy. The proposed pathophysiology for thrombocytopenia is aggregation of platelets in vivo which causes accelerated clearance by phagocytic system. 4 Our finding was consistent with one study’s finding that some patients had severe thrombocytopenia but normal VCT. However, that study did not evaluate other coagulation tests including PT and TT. 6 This finding emphasizes that patients with GPV bite should be followed not only the coagulation tests but also the platelet count together to detect thrombocytopenia.
Our study had some limitations. First, it was a retrospective study and might contain incomplete data. Second, a small number of patients’ data were included. Third, to our knowledge, currently, there is no previous publications which studied the sensitivity, specificity, positive predictive value, negative predictive value, accuracy and area under the ROC curve of TT, comparing to fibrinogen levels. Thus, we did not calculate the sample size before the beginning of this study. Finally, there was no venom confirmation for the definite diagnosis of GPV bite.
Conclusion
TT was the most sensitive and accurate test among four coagulation tests to indicate hypofibrinogenemia in patients with GPV bite. In case of unavailable fibrinogen levels, TT might be considered as the screening test and be investigated to help evaluate patients’ fibrinogen status after GPV bite. Isolated thrombocytopenia without hypofibrinogenemia and coagulopathy could occur in GPV envenomation.
Acknowledgments
The authors express sincere thanks to Mrs Umaporn Udomsubpayakul, section for Clinical Epidemiology and Biostatistics, Research Center, Faculty of Medicine Ramathibodi Hospital, Mahidol University for her help with statistical analysis and Mr Wendell Joseph Dujsik for his help with the English editing.
Footnotes
Author contributions: AT and ST conceived and designed the study; AT and CS conducted the data extraction; AT, PN and ST analyzed/interpreted the data; WW and ST supervised data analysis and AT and ST drafted the manuscript. All authors read and approved the final manuscript as submitted and agree to be accountable for all aspects of the work. The corresponding author attests that all listed authors meet authorship criteria.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: This study was approved by the Institutional Ethics Committee Board of Ramathibodi Hospital Faculty of Medicine, Mahidol University (ID 07-61-24). Due to the retrospective nature of the study design and because we used the preexisting, confidential patient’s medical record, patient consent was not required by our hospital’s Ethics Committee Board. Ethical approval for this study was obtained from the Institutional Ethics Committee Board of Ramathibodi Hospital Faculty of Medicine, Mahidol University (Approval Number/ID 07-61-24).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The author(s) received the article processing charge (APC) support from Ramathibodi Hospital Faculty of Medicine, Mahidol University.
Informed consent to participate: Informed consent was not sought for the present study. Because of the retrospective nature of the study design and we used the preexisting, confidential patient’s medical record, patient consent was not required by our hospital’s Ethics Committee Board.
Informed consent for publication: Informed consent was not sought for the present study. Because of the retrospective nature of the study design and we used the preexisting, confidential patient’s medical record, patient consent was not required by our hospital’s Ethics Committee Board.
Data availability: The data is not available for public access because of patient privacy concerns, but is available from the corresponding author on reasonable request.
ORCID iD: Satariya Trakulsrichai  https://orcid.org/0000-0002-8313-026X
https://orcid.org/0000-0002-8313-026X
References
- 1. Berling I, Isbister GK. Hematologic effects and complications of snake envenoming. Transfus Med Rev 2015; 29(2): 82–89. [DOI] [PubMed] [Google Scholar]
- 2. Levy JH, Welsby I, Goodnough LT. Fibrinogen as a therapeutic target for bleeding: a review of critical levels and replacement therapy: fibrinogen: a therapeutic target for bleeding. Transfusion 2014; 54(5): 1389–1405. [DOI] [PubMed] [Google Scholar]
- 3. Viravan C, Looareesuwan S, Kosakarn W, et al. A national hospital-based survey of snakes responsible for bites in Thailand. Trans R Soc Trop Med Hyg 1992; 86(1): 100–106. [DOI] [PubMed] [Google Scholar]
- 4. Rojnuckarin P. Snakebite-induced coagulopathy and bleeding disorders. In: Kini RM, Clemetson KJ, Markland FS, et al. (eds) Toxins and hemostasis: from bench to bedside. Dordrecht, Netherlands: Springer, 2010, pp. 699–710. [Google Scholar]
- 5. Pongpit J, Limpawittayakul P, Juntiang J, et al. The role of prothrombin time (PT) in evaluating green pit viper (Cryptelytrops sp) bitten patients. Trans R Soc Trop Med Hyg 2012; 106(7): 415–418. [DOI] [PubMed] [Google Scholar]
- 6. Rojnuckarin P, Mahasandana S, Intragumtornchai T, et al. Moderate to severe cases of green pit viper bites in Chulalongkorn hospital. Thai J Hematol Transfus Med 1996; 6(3): 199–205. [Google Scholar]
- 7. Rojnuckarin P, Mahasandana S, Intragumthornchai T, et al. Prognostic factors of green pit viper bites. Am J Trop Med Hyg 1998; 58(1): 22–25. [DOI] [PubMed] [Google Scholar]
- 8. Rojnuckarin P, Intragumtornchai T, Sattapiboon R, et al. The effects of green pit viper (Trimeresurus albolabris and Trimeresurus macrops) venom on the fibrinolytic system in human. Toxicon 1999; 37(5): 743–755. [DOI] [PubMed] [Google Scholar]
- 9. World Health Organization Regional Office for South-East Asia. Guidelines for the management of snakebites. 2nd ed. New Delhi, India: World Health Organization, 2016. [Google Scholar]
- 10. Sibunruang SVSS. Manual of practical management of snake-bites and animal toxin injury. Bangkok, Thailand: Queen Saovabha Memorial Institute, the Thai Red Cross Society, 2013. [Google Scholar]
- 11. Undas A. Determination of fibrinogen and thrombin time (TT). Methods Mol Biol 2017; 1646: 105–110. [DOI] [PubMed] [Google Scholar]
- 12. Cockram CS, Chan JC, Chow KY. Bites by the white-lipped pit viper (Trimeresurus albolabris) and other species in Hong Kong. J Trop Med Hyg 1990; 93(2): 79–86. [PubMed] [Google Scholar]
- 13. Kamal AH, Tefferi A, Pruthi RK. How to interpret and pursue an abnormal prothrombin time, activated partial thromboplastin time, and bleeding time in adults. Mayo Clin Proc 2007; 82(7): 864–873. [DOI] [PubMed] [Google Scholar]
- 14. Sano-Martins IS, Fan HW, Castro SC, et al. Reliability of the simple 20 minute whole blood clotting test (WBCT20) as an indicator of low plasma fibrinogen concentration in patients envenomed by Bothrops snakes. Toxicon 1994; 32(9): 1045–1050. [DOI] [PubMed] [Google Scholar]
- 15. Isbister GK, Maduwage K, Shahmy S, et al. Diagnostic 20-min whole blood clotting test in Russell’s viper envenoming delays antivenom administration. QJM 2013; 106(10): 925–932. [DOI] [PubMed] [Google Scholar]