Abstract
Background
Early initiation of breast cancer screening is recommended for high-risk women, including survivors of childhood cancer treated with chest radiation. Recent studies suggest that female survivors of childhood leukemia or sarcoma treated without chest radiation are also at elevated early onset breast cancer risk. However, the potential clinical benefits and cost-effectiveness of early breast cancer screening among these women are uncertain.
Methods
Using data from the Childhood Cancer Survivor Study, we adapted 2 Cancer Intervention and Surveillance Modeling Network simulation models to reflect the elevated risks of breast cancer and competing mortality among leukemia and sarcoma survivors. Costs and utility weights were based on published studies and databases. Outcomes included breast cancer deaths averted, false-positive screening results, benign biopsies, and incremental cost-effectiveness ratios.
Results
In the absence of screening, the lifetime risk of dying from breast cancer among survivors was 6.8% to 7.0% across models. Early initiation of annual mammography with breast magnetic resonance imaging screening between ages 25 and 40 years would avert 52.6% to 64.3% of breast cancer deaths. When costs and quality-of-life impacts were considered, screening starting at age 40 years was the only strategy with an incremental cost-effectiveness ratio below the $100 000 per quality-adjusted life-year (QALY) gained cost-effectiveness threshold ($27 680 to $44 380 per QALY gained across models).
Conclusions
Among survivors of childhood leukemia or sarcoma, early initiation of breast cancer screening at age 40 years may reduce breast cancer deaths by half and is cost-effective. These findings could help inform screening guidelines for survivors treated without chest radiation.
Female survivors of childhood and adolescent cancer previously treated with chest radiation are at elevated risk for early onset breast cancer (1), and guidelines recommend initiation of breast cancer screening with mammography and breast magnetic resonance imaging (MRI) starting at age 25 years (2-6). Recent data suggest that in addition, female childhood cancer survivors who did not receive chest radiation are also at high risk for developing breast cancer (7–11). Factors contributing to this increased risk include a primary diagnosis of leukemia or sarcoma, as well as exposure to specific chemotherapy agents. For example, survivors of leukemia and sarcoma, representing the majority of nonirradiated breast cancer cases in a recent study (7), have a four- to sixfold higher risk of developing breast cancer compared with the general population. Use of anthracyclines is associated with an increased risk in a dose-dependent manner (7–11). Early initiation of screening with mammography and adjunct breast MRI could reduce breast cancer deaths in these survivors. However, the health benefits of breast cancer screening and treatment may be lower among survivors given their greater burden of comorbidities and higher risk for mortality (12,13). Currently, there are no specific screening recommendations tailored for childhood cancer survivors treated without radiation (6).
Building on prior work (14), we estimated the benefits, harms, and cost-effectiveness of early initiation of breast cancer screening among childhood cancer survivors treated without chest radiation, focusing on leukemia and sarcoma survivors.
Methods
Overview
We used data from the Childhood Cancer Survivor Study (CCSS) to adapt 2 simulation models from the National Cancer Institute’s Cancer Intervention and Surveillance Modeling Network (CISNET) to estimate long-term outcomes for various breast cancer screening strategies among childhood leukemia and sarcoma survivors. The CCSS is a multi-institutional cohort study with longitudinal follow-up of North American 5-year survivors of childhood and adolescent cancers diagnosed before 21 years of age between 1970 and 1999 (15). CISNET breast cancer models have previously informed cancer screening guidelines for average-risk women in the United States (16,17) and evaluated screening strategies for childhood cancer survivors with a history of chest radiation (14). Using CCSS data to reflect the elevated risks of breast cancer and competing mortality among leukemia and sarcoma survivors treated without chest radiation (7,18), we estimated the long-term outcomes for various screening strategies, including breast cancer deaths, quality-adjusted life-years (QALY), false-positive exams, benign biopsies, and costs using the Georgetown-Einstein (model G-E) and Wisconsin (model W) breast cancer models. The models share common inputs, such as screening test performance and competing mortality risks, but vary in their approaches to modeling unobservable aspects of disease natural history, such as tumor onset and progression (19–21). Use of 2 models provides a range of results and, thereby, allows examination of results across models and assessment of the robustness of study conclusions due to structural uncertainty and different approaches to modeling breast cancer natural history (see Figure 1).
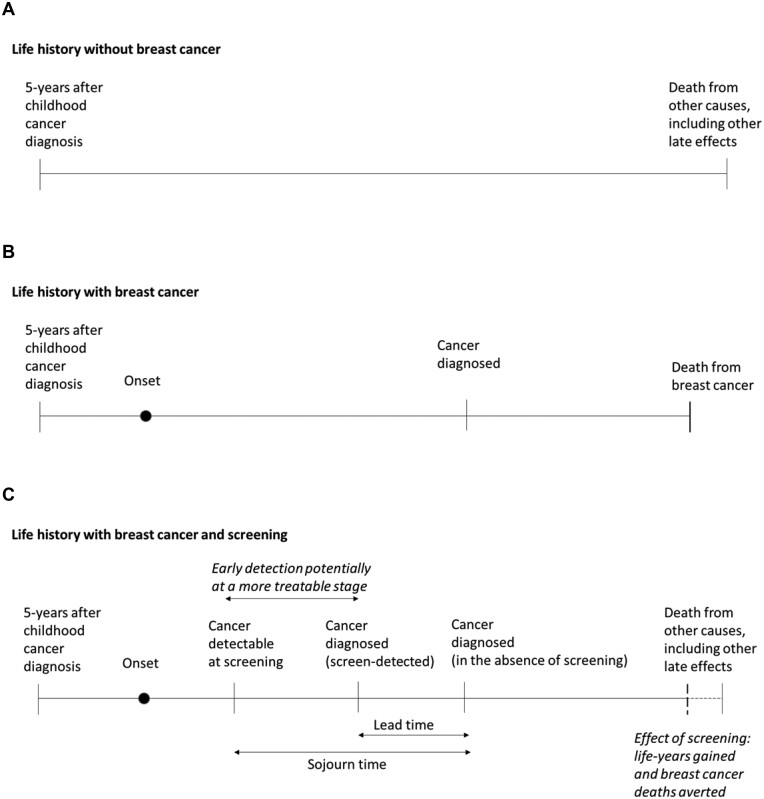
Figure 1.
Schematic overview of simulated life histories and effect of screening among 5-year survivors of childhood cancer. These panels depict examples of life histories simulated in models G-E and W for (A) survivors who do not develop breast cancer during their lifetime, (B) survivors who develop breast cancer, and (C) survivors who develop breast cancer and undergo screening. Model G-E is an event-driven, continuous time-state transition model in which the preclinical, screen-detectable phase of the tumor (sojourn time) is sampled from a distribution. Model W is a discrete-event, stochastic tumor growth simulation model, where the detectability of a tumor via screening is based on tumor size. In both models, the benefit of screening is modeled via early detection at more treatable stages. In model G-E, the stage of detection is based on distributions. In model W, the likelihood of detection is a function of a survivor’s age and tumor size. G-E = Georgetown-Einstein; W = Wisconsin .
Simulation Models
Models G-E and W are discrete-event system microsimulation models of the natural history of breast cancer among US women. Models G-E and W reproduce US temporal trends in incidence and mortality for average-risk women (22) and also demonstrate predictive validity by replicating the UK Age Trial results (23,24). Model G-E is a state-transition model that simulates the development of breast cancer without explicitly modeling tumor growth (21). For each breast cancer, a time period during which the cancer can be detected prior to clinical symptoms is assigned. Screening benefit is a function of cancer detection at younger ages and earlier stage (ie, stage-shift). Treatment benefits are modeled as a hazard reduction (ie, because of lower stage of disease from detection at younger age). Model W uses a continuous tumor growth model to simulate breast cancer natural history (19). Screening benefit is based on detection at smaller tumor sizes and earlier stages. For treatment benefit, a proportion of those women diagnosed have lifelong cure (ie, no possibility of dying from breast cancer), and the remaining women have no cure and progress according to the natural history until death. Additional details on the models are available in Supplementary Table 1 (available online) and at https://cisnet.cancer.gov/ and have been previously published (19–21).
Breast Cancer Risk
In a CCSS study of 2343 survivors of leukemia or sarcoma diagnosed between 1970 and 1986 and treated without radiation at median age of 5 years (range = 0 to 20 years), the cumulative risk of breast cancer by age 50 years was 7.5% (95% confidence interval [CI] = 5.0% to 10.6%) (Supplementary Figure 1, available online) (7). Compared with Surveillance, Epidemiology and End Results (SEER) estimates for average-risk women, this represented an increased relative risk of 4.1 (95% CI = 2.4 to 6.9) for leukemia survivors and 5.3 (95% CI = 3.6 to 7.8) for sarcoma survivors (7). To reflect this higher risk of breast cancer, we applied age-specific standardized incidence ratios estimated among the leukemia and sarcoma survivors (relative to age- and calendar year–specific SEER rates) to adjust breast cancer incidence rates in models G-E and W (25). As described in Table 1, we assumed that breast cancer natural history was similar among survivors and average-risk women, including stage distribution and joint distribution of estrogen receptor (ER) and human epidermal growth factor 2 (HER2) status, and breast cancer mortality rates (26).
Table 1.
Model input parameters
| Parameter | Description | Data source |
|---|---|---|
| Natural history of breast cancer | ||
| Incidence in the absence of screening | Age-period-cohort model calibrated to observed SEER program rates. Adjusted to reflect the elevated risk among childhood cancer survivors without a history of chest radiation using age-specific standardized incidence ratios: 6.6 (95% CI = 2.7 to 15.8) for ages 20-29 years, 4.1 (95% CI = 2.5 to 6.8) for 30-39 years, and 5.9 (95% CI = 3.8 to 9.2) for 40-49 years. As estimates for survivors ages 50 years and older were unavailable, we assumed that the elevated risk observed between ages 40 and 49 years persisted beyond age 50 years. | (7,25) |
| Stage distributiona | Stage distribution among women with clinically, interval-, and screen-detected cancer by age group (younger than 50 years, 50-64 years, 65 years and older). Assumed stage distribution in survivors similar to those in average-risk women (26). | BCSC |
| ER/HER2 joint distribution | Probability of ER/HER2 status conditional on age and stage and tumor size at diagnosis. Assumed tumor characteristics in survivors similar to those in average-risk women (26). | BCSC |
| Sojourn time | Period of time preclinical disease is detectable by screening but asymptomatic, by joint ER/HER2 status and age. | (27) |
| Mean stage dwell time/tumor progress rates | Dwell time, defined as the time spent within a stage, varies by age and ER/HER2 status and by model. Assumed tumor characteristics in survivors similar to those in average-risk women. | (19,21,28) |
| Breast cancer screening | ||
| Sensitivity/detection rates | Sensitivity by age group for digital mammography with MRI (younger than 50 years: 0.932, 95% CI = 0.793 to 0.980; 50 years and older: 0.941, 95% CI = 0.777 to 0.987) and MRI (without mammography: younger than 50 years: 0.857, 95% CI = 0.694 to 0.941; 50 years and older: 0.844, 95% CI = 0.618 to 0.948). | (29) |
| Specificity | Specificity by age group for mammography with MRI (younger than 50 years: 0.787, 95% CI = 0.706 to 0.850; 50 years and older: 0.853, 95% CI = 0.785 to 0.902) and MRI (younger than 50 years: 0.835, 95% CI = 0.776 to 0.881; 50 years and older: 0.885, 95% CI = 0.835 to 0.922). Assuming 75% of false-positive screens for mammography with MRI were due to MRI, the proportion of women screened undergoing additional imaging without biopsy (6.7% vs 6.1%) or having a benign biopsy (14.4% vs 9.4%) was higher for mammography with MRI vs MRI only. | |
| Breast cancer treatment | ||
| Treatment use | Assume receipt of and adherence to the most effective available treatment specific to age, stage, and ER/HER2 status. | (31) |
| Treatment effects | Meta-analysis of clinical trial results. Modeled as a reduction in breast cancer-specific mortality risk or increase in proportion cured in the absence of adjuvant treatment. | (32) |
| Survival | ||
| Breast cancer survival | Long-term breast cancer survival before adjuvant treatment by joint ER/HER2 status, age group, and stage or tumor size. | (27) |
| Nonbreast cancer mortality | Age- and cohort-specific all-cause mortality rates by year, modified to include survivor-specific late mortality risks based on female CCSS participants diagnosed between 1970 and 1999 treated with chemotherapy alone. | (18,33) |
| Costs, US 2018 dollarsb | ||
| Screening mammography | $141 | CMS |
| Screening MRI | $550 | CMS |
| Work-up after false-positive screen result | Imaging costs: $157 (all ages). Biopsy costs by age for mammography: $1040 for ages 20-49 years, $1508 for ages 50-64 years, $1516 for ages 65-74 years, and $1606 for ages 75 years and older. Assumed biopsy costs for MRI were 30% higher than for mammography. | (34) |
| Work-up after true-positive screen result | By age: $2556 for ages 20-49 years, $2400 for ages 50-64 years, $2412 for ages 65-74 years, and $2034 for ages 75 years and older. | (34) |
| Breast cancer treatment | By stage during initial treatment: $14 440 for DCIS, $23 573 for local stage, $40 215 for regional stage, and $54 446 for distant stage. During the last year of life among women with cancer that was not cured and progressed , depending on stage at diagnosis: $55 428 for DCIS, $57 912 for local stage, $62 741 for regional stage, and $79 411 for distant stage. | (35–37) |
| Utilities | ||
| Survivors | Age- and sex-specific quality-of-life utilities among female survivors of childhood cancer: 0.761 for ages 18-29 years, 0.748 for ages 30-39 years, 0.735 for ages 40-49 years. For ages 50 years and older, we extrapolated the relative difference among survivors and the general population between ages 18 and 49 years (0.736 for ages 50-59 years, 0.742 for ages 60-69 years, 0.708 for ages 70-79 years, and 0.663 for ages 80 years and older). | (38) |
| Screening mammography | Decrement of 0.006 for 1 week. | (39) |
| Screening MRI | Assumed MRI, including potential side effects from gadolinium, was associated with a twofold higher decrement than mammography (ie, 0.012 decrement for 1 week). | (39) |
| Diagnostics after positive screen | Decrement of 0.185 for 5 weeks for mammography with MRI (assuming that a greater proportion of women will require biopsies with multimodality screening compared with mammography). | (39) |
| Cancer treatment | By stage: decrement of 0.1 for 2 years for DCIS and local stage, 0.25 for 2 years for regional stage, and 0.4 for initial 2 years and final year of life for distant stage. | (40) |
Stage based on American Joint Committee on Cancer (version 6) for model G-E and Surveillance, Epidemiology, and End Results (SEER) historical staging for model W. BCSC = Breast Cancer Surveillance Consortium; CCSS = Childhood Cancer Survivor Study; CMS = Centers for Medicaid and Medicare Services; DCIS = ductal carcinoma in situ; ER = estrogen receptor; HER2 = human epidermal growth factor 2; MRI = magnetic resonance imaging.
Costs were adjusted to 2018 dollars using the medical care component of the Consumer Price Index.
Screening Strategies
We evaluated the following strategies: 1) no screening and 2) joint digital mammography and MRI screening starting at ages 25, 30, 35, or 40 years (and continuing to age 74 years). Because of the limited available data on screening performance specific to childhood cancer survivors, we based screening test performance estimates on a meta-analysis from 6 high-risk screening studies in BRCA1 and 2 mutation carriers (29).
Costs and Quality of Life
We based the costs associated with screening and diagnostic evaluation of a positive screen on US 2018 Medicare reimbursement rates and published estimates (see Table 1) (34). Cancer treatment costs were based on SEER-Medicare data and varied by cancer stage and treatment phase (35–37).
To reflect quality of life among survivors living with late effects from childhood cancer treatment, we used age- and sex-specific utility weights (38). We also incorporated further utility reductions for undergoing screening, having false-positive screen results, and undergoing breast cancer treatment (by stage) (39,40).
Statistical Analysis
Models G-E and W simulated a cohort of 20-year-old female survivors of childhood leukemia or sarcoma treated without chest radiation undergoing screening for breast cancer. Model outcomes included lifetime clinical benefits (reduction in breast cancer deaths, gains in life-years and QALYs), potential harms (number of screening exams, false-positive screen results, and benign biopsies), and costs. To illustrate tradeoffs, we calculated harm-benefit ratios per death averted for screening tests, false-positive screens, and benign biopsies. We compared results with published estimates for average-risk women and used the ratios of harms to benefits observed for biennial screening from ages 50 to 74 years (17,24) as a proxy for an accepted benchmark.
We also estimated incremental cost-effectiveness ratios (ICERs), defined as the additional cost of a strategy divided by the additional clinical benefit, compared with the next least expensive strategy, and expressed as cost per QALY gained. Costs and QALYs were discounted at 3%, and analyses were conducted from a payer perspective with a lifetime horizon following established recommendations (41,42).
To reflect uncertainty in key model parameters on results, we conducted sensitivity analyses on the elevated breast cancer risk observed among survivors, screening performance, screening and diagnostic disutility weights, and cancer treatment costs. Plausible ranges were based on 95% confidence intervals for data used in the base case and expert opinion. For all outcomes, we report estimates as a range across models to reflect the impact of structural uncertainty on modeled outcomes.
Results
Reduction in Breast Cancer Deaths
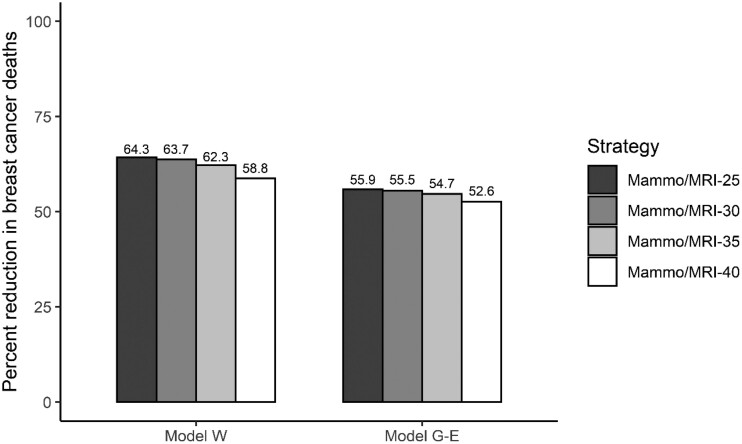
The models project that 36.3%-43.4% (range across models) of survivors would develop breast cancer in their lifetimes and, in the absence of screening, 6.8%-7.0% would die from breast cancer (Table 2). Screening with mammography and MRI starting between ages 25 and 40 years would avert 52.6% to 64.3% of these breast cancer deaths (Table 2; Figure 2). For all strategies, estimates of breast cancer deaths averted were greater in model W compared with model G-E, reflecting differences in how screening benefits occur in the models (ie, detection of smaller vs earlier-stage tumors).
Table 2.
Lifetime benefits and harms of screening strategies varying by start age among female childhood cancer survivors of leukemia and sarcoma treated without chest radiation
| Strategya | Breast cancer deaths per 1000 women, No. |
Reduction in breast cancer deaths, %b |
Life-years gained per 1000 women, No.b,c |
QALYs gained per 1000 women, No.b,d |
Screening tests per 1000 women, No.b |
False-positive screens per 1000 women, No.b |
Benign biopsies per 1000 women, No.b |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model G-E | Model W | Model G-E | Model W | Model G-E | Model W | Model G-E | Model W | Model G-E | Model W | Model G-E | Model W | Model G-E | Model W | |
| No screening | 70.1 | 67.6 | — | — | — | — | — | — | — | — | — | — | — | — |
| Mammo/MRI-40 | 33.2 | 27.8 | 52.6 | 58.8 | 341 | 660 | 201 | 422 | 48 079 | 42 396 | 3872 | 3565 | 1239 | 1141 |
| Mammo/MRI-35 | 31.8 | 25.5 | 54.7 | 62.3 | 396 | 769 | 228 | 487 | 57 354 | 51 174 | 4846 | 4502 | 1551 | 1441 |
| Mammo/MRI-30 | 31.2 | 24.6 | 55.5 | 63.7 | 421 | 817 | 232 | 507 | 66 901 | 60 481 | 5851 | 5494 | 1872 | 1758 |
| Mammo/MRI-25 | 30.9 | 24.1 | 55.9 | 64.3 | 433 | 840 | 227 | 509 | 76 641 | 70 084 | 6876 | 6517 | 2200 | 2085 |
Strategies rank ordered by increasing reduction in breast cancer deaths. G-E = Georgetown-Einstein; mammo = mammography; MRI = magnetic resonance imaging; W = Wisconsin.
Compared with no screening.
Life-years per 1000 women for no screening was 56 965 in model G-E and 56 185 in model W.
Quality-adjusted life-years per 1000 women for no screening was 41 609 in model G-E and 41 066 in model W.
Figure 2.
Reduction in breast cancer deaths for screening strategies varying by start age among female survivors of childhood leukemia and sarcoma treated without chest radiation. Reductions in breast cancer deaths were estimated for each screening strategy, by starting age (25, 30, 35 or 40 years), compared with no screening. G-E = Georgetown-Einstein; Mammo = mammography; MRI = magnetic resonance imaging; W = Wisconsin.
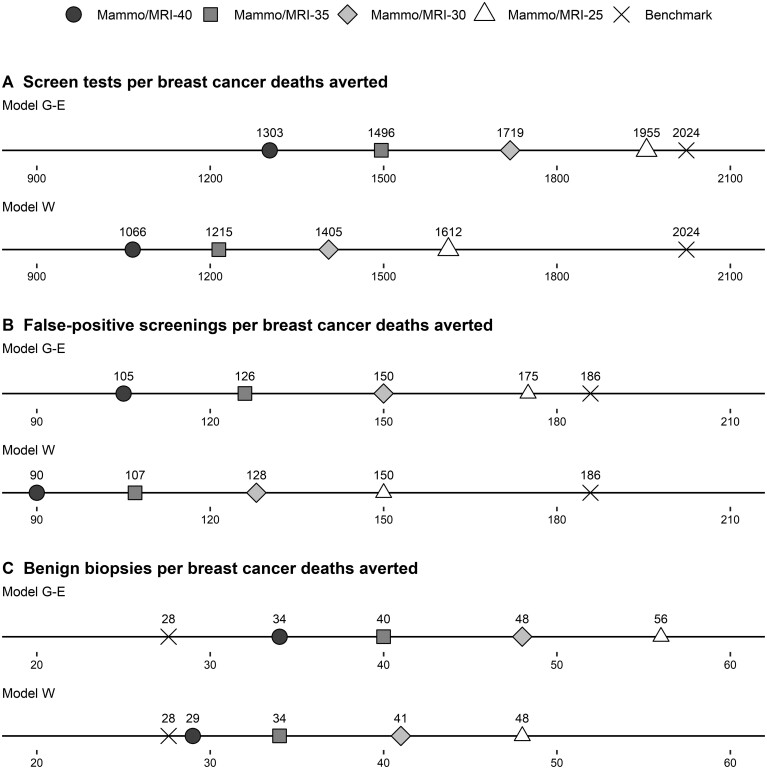
Harm-Benefit Tradeoffs
The number of screening tests, false-positive screens, and benign biopsies associated with each screening strategy is shown in Table 2. For all strategies, the number of screening tests per breast cancer death averted ranged from 1066 to 1955 per 1000 women, the number of false-positive screening results per death averted was 90 to 175 per 1000 women, and the number of benign biopsies per death averted was 29 to 56 per 1000 women across models (Supplementary Table 2, available online). For all screening strategies, the number of screening tests per death averted was more favorable in both models than accepted benchmarks (Figure 3). This was also the case for false-positive screen results but not benign biopsies (although the estimate for screening starting at age 40 years was close to the benchmark in model W).
Figure 3.
Harm-benefit ratios for screening strategies varying by start age among female survivors of childhood leukemia and sarcoma treated without chest radiation. For each screening strategy, harm-benefit ratios are estimated per death averted for (A) screening tests, (B) false-positive screens, and (C) benign biopsies. Ratios are compared with benchmarks based on published estimates for average-risk women in the general population undergoing US Preventive Services Task Force screening recommendations (biennial mammography between ages 50 and 74 years) (17,24). G-E = Georgetown-Einstein; mammo = mammography; MRI = magnetic resonance imaging; W = Wisconsin.
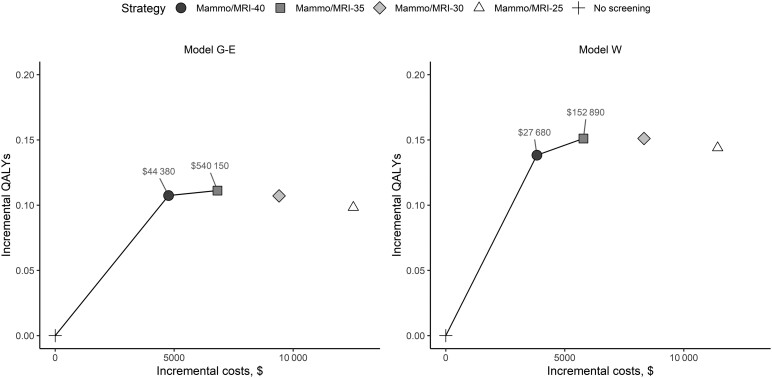
Cost-Effectiveness
When costs and quality-of-life impacts were considered, compared with no screening, the ICER for screening starting at age 40 years was $27 680 per QALY gained in model W and $44 380 per QALY gained in model G-E (Table 3). The ICER for screening starting at age 35 years vs age 40 years was $152 890 per QALY gained in model W and $540 150 per QALY gained in model G-E. ICERs were lower in model W compared with model G-E because of the estimated greater reductions in breast cancer deaths associated with each strategy. Moreover, those strategies that begin screening at ages 30 or 25 years were more expensive and resulted in fewer QALYs gained in both models (Figure 4; Supplementary Table 3, available online).
Table 3.
Cost-effectiveness of breast cancer screening among female childhood cancer survivors of leukemia and sarcoma treated without chest radiation: base case and sensitivity analyses on elevated breast cancer riska
| Strategy | Cost per QALY gainedb |
|||||||
|---|---|---|---|---|---|---|---|---|
| Base case |
Lower bound of 95% confidence intervals used in the base case |
Upper bound of 95% confidence intervals used in the base case |
Base case, except for 50% reduction in elevated risk starting at age 50 years |
|||||
| Model G-E | Model W | Model G-E | Model W | Model G-E | Model W | Model G-E | Model W | |
| No screening | — | — | — | — | — | — | — | — |
| Mammo/MRI-40 | $44 380 | $27 680 | 90 510 | $89 880 | $19 820 | $16 180 | $58 750 | $71 600 |
| Mammo/MRI-35 | $540 150 | $152 890 | c | $1 640 160 | $162 380 | $103 930 | $155 620 | $360 960 |
| Mammo/MRI-30 | c | c | c | c | c | c | c | c |
| Mammo/MRI-25 | c | c | c | c | c | c | c | c |
Standardized incidence ratios used to reflect the elevated risk of breast cancer among survivors (base case and 95% confidence intervals) were based on CCSS participants compared to Surveillance, Epidemiology, and End Results estimates (7). G-E = Georgetown-Einstein; LY = life-year; mammo = mammography; MRI = magnetic resonance imaging; QALY = quality-adjusted life-year; W = Wisconsin.
Costs and benefits discounted 3% annually.
Dominated (more costly, less effective).
Figure 4.
Cost-effectiveness efficiency frontier for screening strategies varying by start age among female survivors of childhood leukemia and sarcoma treated without chest radiation. Incremental discounted costs per gain in discounted QALYS compared with the baseline strategy in model G-E and model W. Strategies on the efficiency frontier (solid line) offer both higher effectiveness and lower cost than those strategies below it. Incremental cost-effectiveness ratios (ICERs), expressed as cost per QALY gained, are shown for these strategies. Both costs and benefits were discounted 3% annually. G-E = Georgetown-Einstein; mammo = mammography; MRI = magnetic resonance imaging; QALY = quality-adjusted life-year; W = Wisconsin.
Sensitivity Analyses
Using the upper bounds of the 95% confidence intervals of elevated breast cancer risk in leukemia and sarcoma survivors, the lifetime risk of developing breast cancer increased to 49.1%-52.7% (data not shown). All harm-benefit ratios were more favorable than average-risk benchmarks (Supplementary Figure 2, available online), and the ICER for screening starting at age 35 years declined to $103 930-$162 380 per QALY gained (Table 3; Supplementary Figure 3, available online). In contrast, using the lower bounds of breast cancer risk, the lifetime risk of developing breast cancer was 25.7%-29.0%, and screening starting at age 40 years was the only strategy meeting any of the average-risk harm-benefit benchmarks (Supplementary Figure 4, available online); the ICER for this strategy was $89 880 to $90 510 per QALY gained across models (Table 3; Supplementary Figure 5, available online). To evaluate the uncertainty in risk at older ages, if we assumed that the elevated risk for breast cancer was 50% lower than base case estimates on reaching age 50 years, both the harm-benefit ratios for screening starting at age 40 years remained lower than average-risk benchmarks (Supplementary Figure 6, available online), and the ICERs below the $100 000 per QALY gained threshold in both models ($71 600 per QALY gained in model G-E and $58 750 per QALY gained in model W) (Table 3; Supplementary Figure 7, available online).
Results were robust across assumptions on disutility associated with screening and diagnostic procedures and cancer treatment costs. As quality of life among survivors was mainly driven by declining general health (Supplementary Figure 8, available online), ICERs were largely unchanged when the disutility weights associated with screening or diagnostic procedures were 50% lower ($40 050 per QALY gained in model G-E and $25 570 per QALY gained in model W). Even if treatment costs for distant stage cancers were 25% higher, mammography with MRI screening starting at age 40 years remained attractive with ICERs below $100 000 per QALY gained ($80 660 per QALY gained in model G-E and $48 760 per QALY gained in model W).
Discussion
In our study, we found that early initiation of annual breast cancer screening with mammography and MRI starting at age 40 could avert half of breast cancer deaths among female survivors of childhood leukemia or sarcoma without a history of chest radiation. Compared with benchmarks for average-risk women, the estimated balance between false-positive screening results and breast cancer deaths averted was acceptable for all screening starting ages. However, this was not the case for benign biopsies, where screening starting at age 40 years was the only strategy with a harm-benefit tradeoff close to the average-risk benchmark. Further, mammography with MRI screening starting at age 40 years was the only strategy that was cost-effective given commonly cited thresholds (43).
Together, our findings suggest that based on the currently available evidence, survivors of childhood leukemia or sarcoma may benefit from early initiation of breast cancer screening with mammography and MRI starting at age 40 years. This later onset of surveillance for survivors of leukemia and sarcoma compared with that recommended for survivors treated with chest radiation is consistent with the lower breast cancer risk observed before age 40 years (2% vs 12%) among CCSS participants (Supplementary Figure 1, available online) (1,7). In a previous study conducted with the same simulations models and comparable CCSS data, we found that early initiation of breast cancer screening among survivors with a history of chest radiation starting at ages 25-30 years could also avert more than half of breast cancer deaths and would be cost-effective using the same cost-effectiveness threshold as our current study (14).
Our study is the first to our knowledge to evaluate breast cancer screening among survivors without a history of chest radiation. However, our findings should be interpreted within the context of the uncertainty in the underlying mechanism for the elevated risk observed among leukemia and sarcoma survivors. The elevated risk could be due to cancer predisposition, explaining both the primary cancer and the secondary cancer in Li-Fraumeni syndrome and other conditions. Yet the prevalence among CCSS participants of TP53 pathogenic variants, the most likely gene mutation associated with sarcoma and breast cancer, is low (0.2%; 11 out of 5105), suggesting that this co-occurrence is not explained by Li-Fraumeni syndrome for most of these individuals (44). A dose-dependent effect for anthracyclines on breast cancer risk has been shown in several studies (7–11). A recent CCSS study found that the combination of anthracyclines and radiotherapy markedly increased breast cancer risk among survivors, with the combined risk being greater than the individual effects (9). As new studies inform risk stratification and better delineate the underlying etiology of breast cancer, including the roles of anthracycline exposure, cancer predisposition syndromes, gene-chemotherapy interactions, and other factors, our models can be refined to reflect these data and provide updated estimates.
Our findings could help inform screening guidelines for survivors of leukemia or sarcoma not previously treated with radiation. Currently, guidelines by the Children’s Oncology Group and the International Late Effects Guidelines Harmonization Group do not include recommendations for these survivors (2,6). Our findings suggest that screening with mammography and MRI starting at age 40 years warrants careful consideration. We note that a screening start age of 40 years for leukemia and sarcoma survivors is similar to some recommendations for average-risk women (45) and also distinctly later than recommendations for childhood cancer survivors with a history of chest radiation (who are currently recommended screening at age 25 years) (2–6). As the understanding of breast cancer risk and cancer screening recommendations continues to evolve, ensuring survivors have a summary of their cancer treatment is crucial so that clinicians can monitor and care for these women.
Limitations to our study include using data on survivors diagnosed with cancer between 1970 and 1986 to adapt the simulation models and may not reflect newer therapies. Our conclusions remained consistent however when using the lower bounds of breast cancer risk at all ages and/or at only older ages where data are limited. Because many patients diagnosed with leukemia or sarcoma were also treated with anthracyclines, we could not disentangle the effects of risk due to genetic predisposition to breast cancer vs treatment-related cancers. We also assumed that breast cancer natural history among survivors was similar to average-risk women as data are currently lacking. Because of the large number of model inputs and the computing resources needed, we were unable to conduct probabilistic sensitivity analyses to capture all parameter uncertainty simultaneously. However, despite differences in model structures and assumptions about breast cancer natural history, our findings were consistent across models. Further, in sensitivity analyses, we consistently found ICERs for screening starting at age 40 years were below the $100 000 per QALY gained threshold (and above this threshold for all other strategies evaluated) across models, which provides some additional assurance of the robustness of our conclusions.
In summary, our findings suggest that early initiation of annual breast cancer screening with mammography and MRI starting at age 40 years may reduce half of breast cancer deaths among survivors of childhood leukemia and sarcoma without a history of radiation and would be cost-effective. These findings could help inform screening guidelines for these high-risk survivors. At this time, our findings are most relevant to women with a sporadic (nonfamilial) primary leukemia or sarcoma and can aid efforts to improve secondary breast cancer prevention among survivors of childhood cancer.
Funding
This work was supported by the American Cancer Society (Research Scholar Grant, RSG-16-018-01—CPHPS, JM Yeh, Principal Investigator) and the National Cancer Institute at the National Institutes of Health (U01CA199218, J Mandelblatt, C Schechter, and A Trentham-Dietz, Principal Investigators; U24CA55727, GT Armstrong, Principal Investigator; R01CA134722, K Oeffinger and J Ford, Principal Investigators). Support to St. Jude Children’s Research Hospital was also provided by the Cancer Center Support (CORE) grant (CA21765, C Roberts, Principal Investigator) and the American Lebanese-Syrian Associated Charities (ALSAC).
Notes
Role of the funders: The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosures: The authors have no conflicts of interest to report.
Author contributions: JMY: Conceptualization, Formal Analysis, Funding acquisition, Investigation, Methodology, Supervision, Validation, Visualization, Writing—original draft, Writing—review & editing. KPL: Conceptualization, Investigation, Validation, Writing—review & editing. CBS: Conceptualization, Investigation, Methodology, Software, Writing—review & editing. LRD: Conceptualization, Investigation, Validation, Writing—original draft, Writing—review & editing. GO: Data curation, Formal Analysis, Visualization, Writing—review & editing. OA: Conceptualization, Investigation, Methodology, Writing—review & editing. GTA: Funding acquisition, Investigation, Resources, Writing—review & editing. JMH: Data curation, Formal Analysis, Software, Visualization, Writing—review & editing. MMH: Conceptualization, Investigation, Writing—review & editing. WL: Data curation, Investigation, Methodology, Resources, Writing—review & editing. QL: Formal Analysis, Writing—review & editing. JSM: Conceptualization, Funding acquisition, Investigation, Resources, Writing—review & editing. DLM: Conceptualization, Investigation, Writing—review & editing. CSM: Formal Analysis, Investigation, Writing—review & editing. PCN: Investigation, Writing—review & editing. JPN: Investigation, Writing—review & editing. KCO: Conceptualization, Investigation, Writing—review & editing. ATD: Conceptualization, Investigation, Supervision, Writing—review & editing. NKS: Conceptualization, Formal Analysis, Funding acquisition, Investigation, Methodology, Supervision, Validation, Writing—review & editing.
Data Availability
Additional details about the CISNET simulations models is available at https://cisnet.cancer.gov/breast/profiles.html and in references (19) and (21). Output data from the models is available from the corresponding author.
Supplementary Material
References
- 1. Moskowitz CS, Chou JF, Wolden SL, et al. Breast cancer after chest radiation therapy for childhood cancer. J Clin Oncol. 2014;32(21):2217–2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Children’s Oncology Group. Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers Version 5.0. Children’s Oncology Group; October 2018. www.survivorshipguidelines.org. Accessed May 8, 2020.
- 3. Saslow D, Boetes C, Burke W, et al. ; for the American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89. [DOI] [PubMed] [Google Scholar]
- 4.National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. Breast Cancer Screening and Diagnosis Version 1. National Comprehensive Cancer Network; 2019. [DOI] [PubMed]
- 5. Monticciolo DL, Newell MS, Moy L, Niell B, Monsees B, Sickles EA.. Breast cancer screening in women at higher-than-average risk: recommendations from the ACR. J Am Coll Radiol. 2018;15(3, pt A):408–414. [DOI] [PubMed] [Google Scholar]
- 6. Mulder RL, Hudson MM, Bhatia S, et al. Updated breast cancer surveillance recommendations for female survivors of childhood, adolescent, and young adult cancer from the International Guideline Harmonization Group. J Clin Oncol. 2020;38(35):4194–4207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Henderson TO, Moskowitz CS, Chou JF, et al. Breast cancer risk in childhood cancer survivors without a history of chest radiotherapy: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2016;34(9):910–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Turcotte LM, Liu Q, Yasui Y, et al. Chemotherapy and risk of subsequent malignant neoplasms in the Childhood Cancer Survivor Study cohort. J Clin Oncol. 2019;37(34):3310–3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Veiga LH, Curtis RE, Morton LM, et al. Association of breast cancer risk after childhood cancer with radiation dose to the breast and anthracycline use: a report from the Childhood Cancer Survivor Study. JAMA Pediatr. 2019;173(12):1171–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Teepen JC, van Leeuwen FE, Tissing WJ, et al. ; for the DCOG LATER Study Group. Long-term risk of subsequent malignant neoplasms after treatment of childhood cancer in the DCOG LATER study cohort: role of chemotherapy. J Clin Oncol. 2017;35(20):2288–2298. [DOI] [PubMed] [Google Scholar]
- 11. Ehrhardt MJ, Howell CR, Hale K, et al. Subsequent breast cancer in female childhood cancer survivors in the St Jude Lifetime Cohort Study (SJLIFE). J Clin Oncol. 2019;37(19):1647–1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moskowitz CS, Chou JF, Neglia JP, et al. Mortality after breast cancer among survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2019;37(24):2120–2130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Milano MT, Li H, Gail MH, Constine LS, Travis LB.. Long-term survival among patients with Hodgkin’s lymphoma who developed breast cancer: a population-based study. J Clin Oncol. 2010;28(34):5088–5096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yeh JM, Lowry KP, Schechter CB, et al. Clinical benefits, harms, and cost-effectiveness of breast cancer screening for survivors of childhood cancer treated with chest radiation: a comparative modeling study. Ann Intern Med. 2020;173(5):331–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Robison LL, Armstrong GT, Boice JD, et al. The Childhood Cancer Survivor Study: a National Cancer Institute-supported resource for outcome and intervention research. J Clin Oncol. 2009;27(14):2308–2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mandelblatt JS, Cronin KA, Bailey S, et al. ; for the Breast Cancer Working Group of the Cancer Intervention and Surveillance Modeling Network. Effects of mammography screening under different screening schedules: Model estimates of potential benefits and harms. Ann Intern Med. 2009;151(10):738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mandelblatt JS, Stout NK, Schechter CB, et al. Collaborative modeling of the benefits and harms associated with different U.S. breast cancer screening strategies. Ann Intern Med. 2016;164(4):215–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yeh JM, Ward ZJ, Chaudhry A, et al. Life expectancy of adult survivors of childhood cancer over 3 decades. JAMA Oncol. 2020;6(3):350–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Alagoz O, Ergun MA, Cevik M, et al. The University of Wisconsin breast cancer epidemiology simulation model: an update. Med Decis Making. 2018;38(suppl 1):99S–111S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mandelblatt JS, Near AM, Miglioretti DL, et al. Common model inputs used in CISNET collaborative breast cancer modeling. Med Decis Making. 2018;38(suppl 1):9S–23S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schechter CB, Near AM, Jayasekera J, Chandler Y, Mandelblatt JS.. Structure, function, and applications of the Georgetown-Einstein (GE) breast cancer simulation model. Med Decis Making. 2018;38(suppl 1):66S–77S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Plevritis SK, Munoz D, Kurian AW, et al. Association of screening and treatment with breast cancer mortality by molecular subtype in US Women, 2000-2012. JAMA. 2018;319(2):154–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. van den Broek JJ, van Ravesteyn NT, Mandelblatt JS, et al. Comparing CISNET breast cancer incidence and mortality predictions to observed clinical trial results of mammography screening from ages 40 to 49. Med Decis Making. 2018;38(suppl 1):140S–150S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mandelblatt JS, Cronin K, de Koning H, Miglioretti DL, Schechter CS, Stout N, Modeling Technical Report. Collaborative modeling of U.S. breast cancer screening strategies. AHRQ Publication No. 14-05201-EF-4. April 2015. 2015. Contract No.: Accessed May 2015.
- 25. Gangnon RE, Sprague BL, Stout NK, et al. The contribution of mammography screening to breast cancer incidence trends in the United States: an updated age-period-cohort model. Cancer Epidemiol Biomarkers Prev. 2015;24(6):905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Elkin EB, Klem ML, Gonzales AM, et al. Characteristics and outcomes of breast cancer in women with and without a history of radiation for Hodgkin’s lymphoma: a multi-institutional, matched cohort study. J Clin Oncol. 2011;29(18):2466–2473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Munoz D, Near AM, van Ravesteyn NT, et al. Effects of screening and systemic adjuvant therapy on ER-specific US breast cancer mortality. J Natl Cancer Inst. 2014;106(11):dju289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. van den Broek JJ, van Ravesteyn NT, Mandelblatt JS, et al. Comparing CISNET breast cancer models using the maximum clinical incidence reduction methodology. Med Decis Making. 2018;38(suppl 1):112S–125S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Phi XA, Houssami N, Obdeijn IM, et al. Magnetic resonance imaging improves breast screening sensitivity in BRCA mutation carriers age >/= 50 years: evidence from an individual patient data meta-analysis. J Clin Oncol. 2015;33(4):349–356. [DOI] [PubMed] [Google Scholar]
- 30. Lee JM, Ichikawa L, Valencia E, et al. Performance benchmarks for screening breast MR imaging in community practice. Radiology. 2017;285(1):44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: breast cancer; 2015. www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed August 1, 2016.
- 32. Peto R, Davies C, Godwin J, et al. ; for the Early Breast Cancer Trialists’ Collaborative Group. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet. 2012;379(9814):432–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gangnon RE, Stout NK, Alagoz O, Hampton JM, Sprague BL, Trentham-Dietz A.. Contribution of breast cancer to overall mortality for US women. Med Decis Making. 2018;38(suppl 1):24S–31S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Stout NK, Lee SJ, Schechter CB, et al. Benefits, harms, and costs for breast cancer screening after US implementation of digital mammography. J Natl Cancer Inst. 2014;106(6):dju092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lowry KP, Trentham-Dietz A, Schechter CB, et al. Long-term outcomes and cost-effectiveness of breast cancer screening with digital breast tomosynthesis in the United States. J Natl Cancer Inst. 2020;112(6):582–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mariotto AB, Warren JL, Zeruto C, et al. Cancer-attributable medical costs for colorectal cancer patients by phases of care: what is the effect of a prior cancer history? J Natl Cancer Inst Monogr. 2020;2020(55):22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR.. Medical care costs associated with cancer survivorship in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29(7):1304–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Yeh JM, Hanmer J, Ward ZJ, et al. Chronic conditions and utility-based health-related quality of life in adult childhood cancer survivors. J Natl Cancer Inst. 2016;108(9):djw046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. de Haes JC, de Koning HJ, van Oortmarssen GJ, van Agt HM, de Bruyn AE, van Der Maas PJ.. The impact of a breast cancer screening programme on quality-adjusted life-years. Int J Cancer. 1991;49(4):538–544. [DOI] [PubMed] [Google Scholar]
- 40. Stout NK, Rosenberg MA, Trentham-Dietz A, Smith MA, Robinson SM, Fryback DG.. Retrospective cost-effectiveness analysis of screening mammography. J Natl Cancer Inst. 2006;98(11):774–782. [DOI] [PubMed] [Google Scholar]
- 41. Neumann PJ, Sanders GD, Russell LB, Siegel JE, Ganiats TG.. Cost-Effectiveness in Health and Medicine 2nd ed. New York, NY: Oxford University Press; 2017. [Google Scholar]
- 42. Caro JJ, Briggs AH, Siebert U, Kuntz KM; for the ISPOR-SMDM Modeling Good Research Practices Task Force. Modeling good research practices–overview: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force–1. Value Health. 2012;15(6):796–803. [DOI] [PubMed] [Google Scholar]
- 43. Neumann PJ, Cohen JT, Weinstein MC.. Updating cost-effectiveness–the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–797. [DOI] [PubMed] [Google Scholar]
- 44. Morton LM, Karyadi DM, Hartley SW, et al. Subsequent neoplasm risk associated with rare variants in DNA damage response and clinical radiation sensitivity syndrome genes in the Childhood Cancer Survivor Study. J Clin Oncol Precis Oncol. 2020;4: 926–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Oeffinger KC, Fontham ET, Etzioni R, et al. ; for the American Cancer Society. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Additional details about the CISNET simulations models is available at https://cisnet.cancer.gov/breast/profiles.html and in references (19) and (21). Output data from the models is available from the corresponding author.