Abstract
Background:
Crisis pregnancy centers (CPCs) seeking to dissuade women from abortion often appear in internet searches for abortion clinics. We aimed to assess whether women can use screenshots from real websites to differentiate between CPCs and abortion clinics.
Methods:
We conducted a cross-sectional, nationally representative online study of English- and Spanish-speaking women aged 18–49 in the United States. We presented participants with screenshots from five CPCs and five abortion clinic websites and asked if they thought an abortion could be obtained at that center. We scored correct answers based on clinic type. Outcomes included ability to correctly identify CPCs and abortion clinics as well as risk factors for misidentification. The survey also included five questions about common abortion myths and a validated health literacy assessment.
Results:
We contacted 2223 women, of whom 1057 (48%) completed the survey and 1044 (47%) were included in the analysis. The median score for correctly identifying CPCs as facilities not performing abortion was 2 out of 5 (Q:1 0, Q:3 4). The median score for correctly identifying abortion clinics as facilities performing abortion was 5 out of 5 (Q:1 3, Q:3 5). Those less likely to endorse abortion myths had higher odds of correctly identifying CPCs (aOR 2.43, CI 1.78— 3.32). A low health literacy score was associated with decreased odds of correct identification of CPCs (aOR 0.39, CI 0.25—0.59).
Conclusions:
Websites of CPCs were more difficult for women to correctly identify than those of abortion clinics. Women with limited knowledge about abortion and low health literacy may be particularly susceptible to misidentification of CPC websites.
Keywords: Crisis pregnancy centers, website identification, abortion misinformation, health literacy
Introduction
Crisis pregnancy centers (CPCs) are counseling facilities that aim to prevent abortion by intercepting women who are actively looking for a health center that provides abortion (Rosen, 2012). Websites of CPCs frequently contain inaccurate information about abortion and may not alert prospective clients, including those self-referring for abortion, that they do not provide abortion services (Dodge et al., 2018). Some women, mostly those who plan to continue their pregnancies, do seek services at CPCs (Kimport, 2020; Kimport et al., 2018). However, reproductive rights advocates remain concerned that women may not realize they are not going to an abortion clinic when they arrive at a CPC (Bryant & Levi, 2012; Bryant & Swartz, 2018).
Little is known about what might make a woman seeking abortion susceptible to diversion to a CPC. In other areas of reproductive health, health literacy has been shown to be important to both improved knowledge and outcomes, so low health literacy may make women especially susceptible to mistaking these sites (“Committee Opinion No. 676,” 2016; Kilfoyle et al., 2016). Those with low knowledge about sexual and reproductive health also often hold misperceptions about the safety of abortion (Kavanaugh et al., 2013). This could make misinformation about abortion at CPCs seem more convincing and exacerbate existing health disparities in abortion care (Dehlendorf et al., 2013). In particular, individuals who have low incomes, are young, and have low educational attainment undergo abortion at disproportionately high rates (Jones & Jerman, 2017). This population might be more likely to believe false claims by CPCs that abortion causes breast cancer, is associated with poor mental health outcomes, or is unsafe (Bryant & Swartz, 2018).
Our objective was to test whether reproductive-aged women were able to reliably differentiate between websites for CPCs and abortion clinics. We also sought to identify risk factors associated with misidentification. We hypothesized that participants would have more difficulty correctly identifying CPCs as facilities that do not provide abortions than they would identifying abortion clinics as facilities that do provide abortion. We further hypothesized that poor health literacy, low socioeconomic status, limited educational attainment, poor knowledge of state abortion laws, and frequent endorsement of abortion myths would be risk factors for misidentification of CPCs and abortion clinics.
Materials and Methods
We conducted a cross-sectional survey study of a nationally representative sample of women aged 18–49 who spoke English or Spanish and were members of the GfK KnowledgePanel. This study received approval from the University of North Carolina Institutional Review Board (#18–2140).
KnowledgePanel is a nationally representative, probability-based Internet panel developed by GfK and has been used for multiple prior studies on abortion and reproductive health (Finer et al., 2014; Grossman et al., 2015; Nelson et al., 2018). KnowledgePanel provides a statistically valid sampling method with a published sample frame of residential addresses that covers approximately 97% of households in the United States. GfK uses geodemographic benchmarks from the U.S. Census Bureau’s Current Population Survey to weight active pool members. GfK provides modest incentives to encourage continued participation.
Women who spoke English or Spanish, were aged 18–49, and were members of the GfK KnowledgePanel were eligible to participate. We did not include responses from those with incomplete surveys, those who completed the survey but excluded or skipped >50% of the questions in the whole survey, those who completed the entire survey in ≤2 minutes, or those who skipped all 10 of the questions assessing website identification.
GfK administered the survey to KnowledgePanel members March 1–8, 2019, a field period of eight days. Non-responders received an email reminder to complete the survey on days three and six of the field period. Participation overall and each survey item was voluntary.
Given a diverse sample of reproductive-aged women in the US population through GfK, we planned our target sample size to achieve accurate estimates and allow subgroup analyses. This target sample size was 1000 women to complete the survey, which would yield a margin of error of 3.1% with a 95% confidence level around estimates. KnowledgePanel’s survey completion rate is approximately 60%, though generally lower in younger populations.
Measures
We designed a 10-item assessment to test whether participants could determine if a health center provided abortion by looking at its website. First, we collected images of actual websites of abortion clinics and crisis pregnancy centers in January 2019. To gather a diverse sample, we used a random city generator to create a list of 25 cities (Random US City Generator—Populated Areas of the US, n.d.). We cleared the search history and used Firefox browser to search using Google. We used the phrase “abortion [city, state].” We selected an abortion clinic and CPC from the first page of results. If an abortion clinic and a CPC were not featured on the first page of results, we moved to the next city. For each facility, we created a set of two screenshots including the homepage and what the searcher would see if they clicked “services” or “pregnancy services.” We repeated this process until we had images from abortion clinics and CPCs from ten different cities.
In the administered survey, we introduced the activity by indicating that participants would see pictures of health center websites. Participants were then shown a randomized series of 10 images that included five screenshots of abortion clinic websites (including one Planned Parenthood) and five screenshots of CPC websites. Above the images, we asked the question: “If a pregnant woman was trying to obtain an abortion, do you think she could have one at this health center?”. Participants could answer, “yes,” “no,” or “not sure.”
Questions were scored as to whether the participant correctly determined if a facility provided abortion. For CPC websites, a “no” was considered correct identification that the center did not perform abortion and was scored one point. Both “yes” and “not sure” were scored zero points. For abortion clinics, a “yes” was considered correct identification that the facility did perform abortion and was scored one point. Both “no” and “not sure” were scored zero points. Missing or skipped questions were also scored zero points. Two sum scores were calculated for each participant, one for CPCs and one for abortion clinics, that indicate the number of each type of clinic participants could correctly categorize. These were our primary and secondary outcomes, respectively.
In addition to our primary assessment, the survey included a total of 41 additional items. We included items about state abortion laws (12), common abortion myths (5), personal views on abortion (1), self-reported pregnancy and abortion history (3), health literacy (6), and prior knowledge of the existence of CPCs (1). We adapted previously published survey tools when available (Berglas et al., 2017; Bessett et al., 2015; Dodge et al., 2013; White et al., 2016).
For assessment of health literacy, we used the Newest Vital Sign, a rapid health literacy measure validated in English and Spanish that we adapted for online administration (The Newest Vital Sign | Pfizer: One of the World’s Premier Biopharmaceutical Companies, n.d.). Toolspecific scoring stratified respondents into three categories: “Low health literacy,” “Possible low health literacy,” and “Adequate health literacy” (The Newest Vital Sign | Pfizer: One of the World’s Premier Biopharmaceutical Companies, n.d.).
We received demographic data on each participant from GfK. We used data on number of family members living in the household and income to stratify participants using the 2019 Federal Poverty Level (FPL). We condensed religious affiliation to six categories. We also condensed political affiliation to three categories from seven.
Analysis
Participant characteristics were summarized using frequency with sampling weights provided by GfK. We calculated summary statistics for the number of CPCs participants correctly identified as facilities not performing abortion and the number of abortion clinics participants correctly identified as facilities performing abortion.
In the regression analysis, we defined the primary outcome as a binary outcome with 0 denoting incorrect identification and 1 being correct identification for each website that was shown to a participant. This yielded 10 measures per participant. To investigate the association between each participant characteristic and the outcome, we fit a generalized estimating equations (GEE) model with a logit link and independent working correlation structure. The model included the indicator for facility type (time-dependent covariate), participant characteristics, and a facility type and participant characteristic product term. Contrast statements were used to obtain comparisons of interest and multiple comparisons adjustment was made using Bonferroni.
Next, the data were stratified by facility type (CPC or abortion clinic) for the purpose of identifying factors associated with correctly identified CPCs or abortion clinics separately. An initial multivariable GEE model which included age, race, household income, marital status, metropolitan statistical area status, census region, language proficiency, political affiliation, whether participants had heard of CPCs, pregnancy history, having accompanied someone for an abortion, personal views on abortion, health literacy score, state abortion knowledge score, and abortion myths score was fit. We did not include participant personal history of abortion because the question was only asked of women who reported they had been pregnant in the past. Variables with p-values < 0.05 were retained and refit in the final model. This procedure was performed separately for CPCs and abortion clinics. All analyses were performed with SAS 9.4 (SAS Institute Inc., Cary, NC).
Sensitivity analyses
Planned Parenthood is a highly recognizable brand associated with abortion care and we included it in our assessment to intentionally provide a named clinic that might be more familiar. Each participant had exactly one Planned Parenthood website included among the 10 websites in the assessment. As a sensitivity analysis, we calculated summary statistics for the number of correctly identified abortion clinics not including Planned Parenthood. Furthermore, we recoded skipped questions or “unsure” as missing and reran the regression analyses on this cohort of participants (N=975) as a sensitivity analysis. (Appendix A)
Results
As we reported previously in a related study (Swartz et al., 2020), among 1,057 participants who completed the survey, we excluded 7 participants who completed the questionnaire in ≤ 2 minutes and 4 participants who answered “Refused” to more than 50% of the questionnaire. This yielded a slightly larger sample size than in our prior study (Swartz et al., 2020). The analysis dataset consisted of 1,046 participants, which yielded a weighted sample size of 1,044 (Figure 1).
Figure 1: Participant flowchart.
As was reported previously (Swartz et al., 2020), one thousand one hundred sixty-six women declined to participate after the initial invitation from GfK. A small minority, 81 women (4% of those invited), opened the survey and did not complete it. Non-participants were more likely have low incomes and lower levels of education but were otherwise demographically similar to participants.
Demographic characteristics were also reported in our prior study though as noted results from the current study reflect the slightly larger sample (Swartz et al., 2020). Mean age was 34 (SD 8.7) and study participants reflected racial and ethnic diversity representative of the US population (Table 1). Women from all states and the District of Columbia responded, with the exception of Hawaii. Overall, women were well educated (36% with a bachelor’s degree or higher) and had greater health literacy than the general population (Cutilli & Bennett, 2009), and few came from households living below 100% federal poverty level (12%). The majority of women believed the government should not make abortion illegal (771/1018; 76%) and identified with the Democratic party (616/1044; 59%). While the majority of women reported having been pregnant in the past (619/1033; 60%), a minority of those who had been pregnant reported a personal history of abortion (107/618; 17%) or having accompanied someone else to obtain an abortion (79/1031; 8%). Women had limited knowledge of their state’s abortion regulations and limited ability to differentiate common abortion myths from facts about abortion (Swartz et al., 2020).
Table 1:
Sociodemographic and reproductive characteristics of women aged 18–49 participating in a US-based assessment of website identification
| Characteristics | Total with weight (N=1,043.8) |
|---|---|
|
| |
| Age | |
| Mean (SD) | 33.8 (8.7) |
| Median [Q1, Q3] | 34 [27, 41] |
| Range | (18–49) |
| Race / Ethnicity | |
| White, Non-Hispanic | 584.5 (56%) |
| Black, Non-Hispanic | 141 (13.5%) |
| Other, Non-Hispanic | 87.1 (8.3%) |
| Hispanic | 212.2 (20.3%) |
| 2+ races, Non-Hispanic | 19 (1.8%) |
| Education | |
| Less than high school | 95.8 (9.2%) |
| High school | 239.1 (22.9%) |
| Some college | 330.2 (31.6%) |
| Bachelor's degree or higher | 378.7 (36.3%) |
| Household income as % of federal poverty level | |
| <100% of FPL | 123.7 (11.8%) |
| 100–199% of FPL | 138.7 (13.3%) |
| 200%+ of FPL | 781.5 (74.9%) |
| Marital status | |
| Married | 543.1 (52%) |
| Widowed/divorced/separated | 82.6 (7.9%) |
| Never married | 309.2 (29.6%) |
| Living with partner | 108.9 (10.4%) |
| MSA Status | |
| Non-metro | 124.8 (12%) |
| Metro | 919 (88%) |
| Census regions - based on state of residence | |
| Northeast | 176.2 (16.9%) |
| Midwest | 212.4 (20.4%) |
| South | 402 (38.5%) |
| West | 253.3 (24.3%) |
| Language proficiency | |
| Spanish speaking | 93.8 (9%) |
| Bilingual | 118.4 (11.3%) |
| English speaking | 831.6 (79.7%) |
| Religion | |
| Missing | 4.9 (0.5%) |
| Catholic | 236.6 (22.8%) |
| Evangelical, Protestant, and other Christian | 442.8 (42.6%) |
| Jewish | 25.7 (2.5%) |
| Islam/Muslim | 10.7 (1%) |
| Other non-Christian religion | 36.4 (3.5%) |
| No religion | 286.7 (27.6%) |
| Political affiliation | |
| Republican | 364.3 (34.9%) |
| Independent | 61 (5.8%) |
| Democrat | 618.5 (59.3%) |
| Heard of CPCs | 615.5 (59.4%) |
| Missing | 7.3 (0.7%) |
| Personal views on abortion | |
| Missing | 25.8 (2.5%) |
| Abortion is morally acceptable and should be legal | 318.5 (31.3%) |
| Personally against abortion, but government should not prevent a | 452.3 (44.4%) |
| woman from making that decision | |
| Abortion is morally wrong and should be illegal | 247.3 (24.3%) |
| Have been pregnant | 619.4 (60%) |
| Missing | 10.6 (1%) |
| Have had an abortion | 107.2 (17.4%) |
| Missing | 1.4 (0.2%) |
| Have accompanied someone else to obtain an abortion | 78.8 (7.6%) |
| Missing | 12.5 (1.2%) |
|
| |
| Health literacy score | |
| High likelihood of limited literacy | 75.8 (7.3%) |
| Possibly limited literacy | 150.8 (14.4%) |
| Adequate literacy | 817.2 (78.3%) |
|
| |
| State abortion knowledge score (categorized) | |
| ≤ 25th percentile (score = 0) | 383.3 (36.7%) |
| 26th - 75th percentiles (score = 1–3) | 395.2 (37.9%) |
| > 75th percentile (score = 4–12) | 265.3 (25.4%) |
|
| |
| Score on abortion myth questions (categorized) | |
| ≤ 25th percentile (score = 0) | 472.3 (45.2%) |
| 26th - 75th percentiles (score = 1–2) | 396.9 (38%) |
| > 75th percentile (score = 3–5) | 174.6 (16.7%) |
On the website assessment, the median number of correctly identified CPCs was 2 (Q:1 0, Q:3 4) compared to the median number of correctly identified abortion clinics of 5 (Q:1 3, Q:3 5) (Table 2). Four respondents answered all 10 questions with “Unsure” or “Refused” and their responses were excluded. In our sensitivity analysis, the median number of correctly identified abortion clinics excluding Planned Parenthood was 4 (Q:1 3, Q:3 4). This suggested inclusion of Planned Parenthood did not bias our results. Eighty percent of participants correctly identified Planned Parenthood as an abortion clinic.
Table 2:
Number of times N=1044 women could correctly identify crisis pregnancy centers as facilities not performing abortions based on their websites and number of times women could correctly identify abortion clinics as facilities that perform abortions based on their websites
| Main analysis including Planned Parenthood among abortion clinic screenshot pool | ||
|---|---|---|
| Number of screenshots correctly identified | Respondents correctly identified... | |
| Crisis pregnancy centers as facilities not performing abortion (out of 5 screenshots) N(%) | Abortion clinics as facilities performing abortion (out of 5 screenshots) N(%) | |
| 0 | 299 (29) | 136 (13) |
| 1 | 170 (16) | 28 (3) |
| 2 | 174 (17) | 29 (3) |
| 3 | 135 (13) | 68 (7) |
| 4 | 127 (12) | 181(17) |
| 5 | 140 (13) | 602 (58) |
| Median* [Q1, Q3] | 2 [0, 4] | 5 [3, 5] |
| Sensitivity analysis excluding Planned Parenthood from abortion clinic screenshot pool | ||
| Number of screenshots correctly identified | Respondents correctly identified. | |
| Abortion clinics as facilities performing abortion (out of 4 screenshots) N (%) | Planned Parenthood as a facility providing abortion (out of 1 screenshot) | |
| Median* [Q1, Q3] | 4 [3, 4] | |
| 0 | 148 (14) | 207 (20%) |
| 1 | 35.8 (3) | 837 (80) |
| 2 | 57 (6) | n/a |
| 3 | 177 (17) | n/a |
| 4 | 3 (1) | n/a |
Data represented as N (%).
Median [Q1, Q3] presented because the data were not normally distributed.
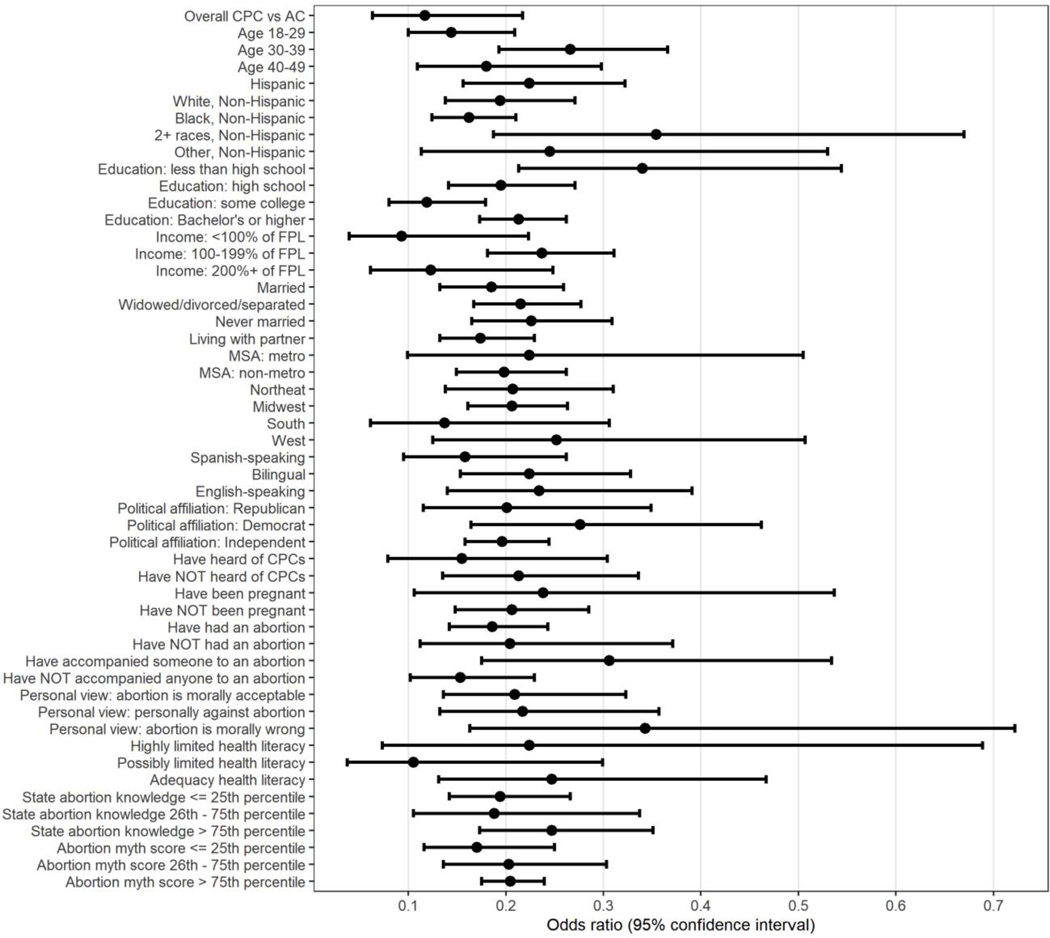
We were interested in sociodemographic characteristics associated with the ability to determine whether facilities perform abortion. Separate regression models were fit for each characteristic (Figure 2). Overall, we observe that participants had significantly lower odds of correctly identifying CPCs as compared to abortion clinics. This was evident in all the characteristics that we analyzed (Figure 2).
Figure 2. Odds of correct identification of crisis pregnancy centers versus correct identification of abortion clinics by patient characteristics.
Forest plot shows bivariate association between sociodemographic and reproductive characteristics with performance on a web-based survey in which participants were shown a website screenshot of a crisis pregnancy center or abortion clinic and asked, “If a woman were seeking an abortion, could she have one at this center?” The plot compares the odds of correctly identifying a crisis pregnancy center as a non-abortion providing facility versus correctly identifying an abortion clinic as providing abortion. State abortion law knowledge was scored on the basis of a 12-item assessment and abortion myth score was on the basis of a 5-item assessment.(Swartz et al., 2020) In both assessments, higher percentiles represent more correct 431 answers.
FPL, federal poverty level; MSA, metropolitan statistical area.
In multivariable analysis, several factors were found to be associated with correct identification of CPCs as facilities that did not perform abortion (Table 3). Having prior knowledge of CPCs was associated with increased odds of correctly identifying CPCs (aOR 1.48, CI 1.20—1.82). Those with personal moral opposition to abortion also had increased odds of correctly identifying CPCs (aOR 1.58, CI 1.19—2.10) as did those who were less likely to endorse common myths about abortion (aOR 2.43, CI 1.78—3.32). In contrast, a low health literacy score was associated with decreased odds of correct identification of CPCs (aOR 0.39, CI 0.25—0.59) (Table 3).
Table 3:
Participant characteristics associated with correctly determining that a crisis pregnancy center did not provide abortion
| Variables | OR (95% CI) | P-value |
|---|---|---|
|
| ||
| Heard of CPC | 1.48 (1.20, 1.82) | <0.001 |
| Personal views on abortion | 0.006 | |
| Abortion is morally acceptable and should be legal | Reference | |
| Personally against abortion, but the government should not prevent a woman from making that decision | 1.16 (0.91, 1.48) | 0.221 |
| Abortion is morally wrong and should be illegal | 1.58 (1.19, 2.10) | 0.002 |
| Health literacy score | <0.001 | |
| Adequate literacy | Reference | |
| Possibly limited literacy | 0.81 (0.59, 1.13) | 0.219 |
| High likelihood of limited literacy | 0.39 (0.25, 0.59) | <0.001 |
| Abortion myths score | <0.001 | |
| ≤ 25th percentile | Reference | |
| 26th - 75th percentiles | 1.22 (0.99, 1.52) | 0.066 |
| > 75th percentile | 2.43 (1.78, 3.32) | <0.001 |
Health literacy scale from the Newest Vital Sign (The Newest Vital Sign | Pfizer: One of the World’s Premier Biopharmaceutical Companies, n.d.). Abortion myth score based on five questions asking whether participants thought a common abortion myth or a fact was closer to the truth.
Factors associated with correct identification of abortion clinics as facilities performing abortion largely mirrored those associated with correct identification of CPCs (Table 4). Those who had heard of CPCs (aOR 1.62, CI 1.22—2.15) and were less likely to endorse myths about abortion (aOR 2.53, CI 1.63—3.92) had increased odds of correct identification of abortion clinics, while those with low health literacy had decreased odds (aOR 0.26, CI 0.16—0.42). In contrast to correct identification of CPCs, those who had moral opposition to abortion (aOR 0.52, CI 0.35—0.76) and were personally against abortion but oppose government prohibition of abortion (aOR 0.71, CI 0.51—0.98) had decreased odds of correct identification of abortion clinics compared to those who thought abortion was morally acceptable.
Table 4:
Participant characteristics associated with correctly determining that an abortion clinic did provide abortion
| Variables | OR (95% CI) | P-value |
|---|---|---|
|
| ||
| Language proficiency | 0.042 | |
| English speaking | Reference | |
| Spanish speaking | 0.60 (0.39, 0.92) | 0.019 |
| Bilingual | 1.29 (0.77, 2.15) | 0.332 |
| Heard of CPC | 1.62 (1.22, 2.15) | 0.001 |
| Personal views on abortion | 0.004 | |
| Abortion is morally acceptable and should be legal | Reference | |
| Abortion is morally wrong and should be illegal | 0.52 (0.35, 0.76) | 0.001 |
| Personally against abortion, but the government should not prevent a woman from making that decision | 0.71 (0.51, 0.98) | 0.037 |
| Have accompanied someone else to an abortion | 1.91 (1.03, 3.55) | 0.019 |
| Health literacy score | <0.001 | |
| Adequate literacy | Reference | |
| Possibly limited literacy | 0.41 (0.28, 0.61) | <0.001 |
| High likelihood of limited literacy | 0.26 (0.16, 0.42) | <0.001 |
| Abortion myths score | <0.001 | |
| ≤ 25th percentile | Reference | |
| 26th - 75th percentiles | 1.71 (1.27, 2.31) | <0.001 |
| > 75th percentile | 2.53 (1.63, 3.92) | <0.001 |
Caption: Health literacy scale from the Newest Vital Sign (The Newest Vital Sign | Pfizer: One of the World’s Premier Biopharmaceutical Companies, n.d.). Abortion myth score based on five questions asking whether participants thought a common abortion myth or a fact was closer to the truth.
In the sensitivity analysis, factors associated with CPC identification were unchanged. Factors associated with correct identification of abortion clinics did change and race/ethnicity was significant while language proficiency, prior knowledge of CPCs, and abortion myth knowledge were no longer significant (Appendix A).
Discussion
In a nationally representative assessment of reproductive-aged women, we found that women had more difficulty identifying CPCs as non-abortion providing facilities from screenshots of their websites than they did identifying abortion clinics from screenshots of their websites. This misidentification of facility type was consistent across all sociodemographic characteristics we evaluated. We found several notable risk factors for misidentification of CPCs, including low health literacy, lack of prior knowledge of CPCs, and lesser ability to differentiate abortion myths from facts about abortion.
A number of studies have demonstrated that CPC websites provide inaccurate information about contraception and abortion (Borrero et al., 2019; Bryant & Levi, 2012; Swartzendruber et al., 2018). Further, CPCs are abundant, outnumbering abortion clinics nationally by a factor of 3:2 (Swartzendruber & Lambert, 2020). They are often located close to abortion clinics, have similar names to abortion clinics, and appear in Internet searches for clinics (Bryant & Levi, 2012; Bryant & Swartz, 2018; Dodge et al., 2018; Swartzendruber & Lambert, 2020). Support services at CPCs are often limited to the provision of clothes and diapers, and may come with information about Christianity and pressure to pray with CPC workers. CPCs do not provide comprehensive longitudinal services or even Medicaid enrollment to help women with pregnancy. The combination of biased pregnancy options counseling and physical locations that could intercept women seeking abortion clinics decreases reproductive autonomy (Borrero et al., 2019). This is especially true for women who go to a CPC expecting to receive education about all pregnancy options, including reliable information about abortion, adoption, and parenting (Borrero et al., 2019; Bryant & Swartz, 2018; Kimport et al., 2018; Rosen, 2012).
Despite concerns about the unethical practices of CPCs, research demonstrating the effect of CPCs on pregnancy-related decision-making is limited (Bryant & Swartz, 2018). A minority of women recruited from abortion and prenatal clinics in Louisiana visited CPCs (6% from abortion clinics and 5% of prenatal patients) (Kimport et al., 2018). Among those who entered prenatal care, most reported they planned to continue their pregnancies when they decided to visit the CPC (Kimport et al., 2018). Those recruited from abortion clinics were not interviewed (Kimport et al., 2018). Among the women recruited from prenatal clinics in Louisiana and Maryland, many of those who reported visiting CPCs said they viewed them as an opportunity to obtain free resources such as pregnancy tests, ultrasound, clothes, and diapers (Kimport, 2020). Some women reported they sought support when others, including physicians, might have discouraged them from becoming pregnant or continuing a pregnancy (Kimport, 2020). This research demonstrates CPCs may have a limited role in pregnancy decision-making, though it cannot be generalized to women who are seeking abortion and accidentally present to a CPC (Kimport, 2020; Kimport et al., 2018).
Results suggesting that those who had moral opposition to abortion had greater odds of correctly identifying CPCs and lesser odds of correctly identifying abortion clinics seem paradoxical. However, prior research indicates that on politicized topics, participants interpret data to conform with their preexisting outlook (Kahan et al., 2013). In other words, subjective beliefs may influence objective information in cognitive tasks like our request that they interpret facility type using a website.
Strengths and Limitations
Strengths of this study include a nationally representative and diverse sample of reproductive-aged women. Further, our assessment included images of actual CPC and abortion clinic websites that appeared in search results for abortion clinics. Finally, the inclusion of a measure of health literacy highlights a key factor associated with accurate interpretation of health information in other domains (Berkman, Sheridan, Donahue, Halpern, Viera, et al., 2011; Kilfoyle et al., 2016; Lorini et al., 2018). One limitation of this assessment is that we were not able to assess whether participants would in fact choose a CPC over an abortion clinic if they had a list of clinics to choose from. Instead, we have information only on how easily individual sites were distinguished. Moreover, those seeking abortion might be drawn to a known clinic or brand (e.g., Planned Parenthood), which could be protective against diversion to a non-abortion providing facility. Additionally, the low proportion (Jones & Jerman, 2017) of women in our study reporting a personal history of abortion may be evidence of a non-representative sample or social-desirability bias in responses. This study may underestimate susceptibility to diversion to CPCs as the majority of respondents were older than the median age of abortion seekers nationally, had incomes >200% above the FPL, and had higher levels of health literacy than the general population.
Our study demonstrates reproductive-aged women commonly misinterpret CPC websites. CPCs freedom to offer misleading information was recently protected in the NIFLA v. Becerra decision by the US Supreme Court (Raymond-Sidel, 2019). In that case, the National Institute of Family Life Advocates challenged a California law requiring that CPCs disclose if they were unlicensed and that California provides free or low-cost access to abortion services. In the majority opinion, the Supreme Court held that such a requirement violated CPCs’ First Amendment rights (Raymond-Sidel, 2019). While NIFLA v. Becerra made regulation of CPCs even more difficult for states inclined toward evidence-based health information, private industry may be able to help.
Google has recently renewed efforts to make its abortion search results more transparent. Under pressure from NARAL Pro-Choice America, Google added a new feature to ads appearing in search results in 2019 (Hsu, 2019). Organizations advertising in searches for abortion must now verify their abortion-providing status, and a banner under the ad states, “Does not provide abortions” or “Provides abortions” (Hsu, 2019). While this is a remarkable step, it also conveys that CPCs could not be relied upon to offer this basic information of their own volition. Moreover, CPCs are still allowed by Google to select keywords for services they do not offer.
Implications for policy and practice
Reproductive rights advocates may need to engage other creative solutions to help decrease the negative impact of misinformation about abortion. One additional opportunity for advocacy would be further regulation by private companies like Google so that CPCs are unable to purchase ads related to services they do not offer, such as abortion.
More research is needed to better understand how people use Internet search results to select a clinic to attend. As noted above, it seems likely that our sample underestimates the risk of misidentification of CPCs and abortion clinic websites as it included a higher proportion of higher-income, higher-educated, older women with greater health literacy than would be found in the general population, and particularly the abortion-seeking population. However, this young population is conceivably also more Internet-savvy, which might protect abortion seekers from diversion to a non-abortion clinic. Further research could also inform clinics that wish to design websites with the goal of clear communication.
Conclusions
In their mission to prevent abortion, CPCs need to attract patients who might otherwise attend abortion clinics. Our findings demonstrate that websites of these facilities do not clearly communicate whether they provide abortion, with over 85% of participants failing to correctly identify at least one CPC. Unfortunately, the burden of deception is likely to fall on those with low health literacy who are already more likely to have worse health outcomes. Abortion clinics might also take a lesson from this study. Forty percent of participants failed to correctly identify at least one abortion clinic. To best serve patients, clinics should prioritize clear communication and presentation of services they provide.
Supplementary Material
Acknowledgments
Role of the funding source: This work was supported by the Society of Family Planning Research fund (SFPRF19-04) who reviewed the protocol but had no other role in study design, data collection, analysis, interpretation of data, writing of the report or decision to submit for publication. The Duke Biostatistics, Epidemiology, and Research Design Methods Core’s support of this project was made possible in part by CTSA Grant (UL1TR002553) from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH), and the NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCATS or NIH. Jonas Swartz is a Women’s Reproductive Health Research Scholar (K12HD103083-01).
Presentation: An abstract of this work was presented at the North American Forum on Family Planning held October 2019.
Author biographical information
Jonas J. Swartz, MD, MPH, is Assistant Professor, Division of Women’s Community and Population Health, Department of Obstetrics and Gynecology, Duke University, Durham, North Carolina.
Carly Rowe, MSW, is Program Manager, Institute of Translational Health Sciences, University of Washington, Seattle, Washington.
Tracy Truong, MS, is Biostatistician, Department of Biostatistics & Bioinformatics, Duke University, Durham, North Carolina.
Amy Bryant, MD, MSCR, is Associate Professor, Division of Complex Family Planning, Department of Obstetrics and Gynecology, University of North Carolina, Chapel Hill, North Carolina.
Jessica Morse, MD, MPH, is Associate Professor, Division of Complex Family Planning, Department of Obstetrics and Gynecology, University of North Carolina, Chapel Hill, North Carolina.
Gretchen Stuart, MD, MPHTM is Professor, Division of Complex Family Planning, Department of Obstetrics and Gynecology, University of North Carolina, Chapel Hill, North Carolina.
Footnotes
Disclosure: The authors report no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- Berglas NF, Gould H, Turok DK, Sanders JN, Perrucci AC, & Roberts SCM (2017). State-Mandated (Mis)Information and Women’s Endorsement of Common Abortion Myths. Women’s Health Issues, 27(2), 129–135. 10.1016/j.whi.2016.12.014 [DOI] [PubMed] [Google Scholar]
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Viera A, Crotty K, Holland A, Brasure M, Lohr KN, Harden E, Tant E, Wallace I, & Viswanathan M. (2011). Health literacy interventions and outcomes: An updated systematic review. Evidence Report/Technology Assessment, 199, 1–941. [PMC free article] [PubMed] [Google Scholar]
- Bessett D, Gerdts C, Littman LL, Kavanaugh ML, & Norris A. (2015). Does state-level context matter for individuals’ knowledge about abortion, legality and health? Challenging the ‘red states v. blue states’ hypothesis. Culture, Health & Sexuality, 17(6), 733–746. 10.1080/13691058.2014.994230 [DOI] [PubMed] [Google Scholar]
- Borrero S, Frietsche S, & Dehlendorf C. (2019). Crisis Pregnancy Centers: Faith Centers Operating in Bad Faith. Journal of General Internal Medicine, 34(1), 144–145. 10.1007/s11606-018-4703-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant AG, & Levi EE (2012). Abortion misinformation from crisis pregnancy centers in North Carolina. Contraception, 86(6), 752–756. 10.1016/j.contraception.2012.06.001 [DOI] [PubMed] [Google Scholar]
- Bryant AG, & Swartz JJ (2018). Why Crisis Pregnancy Centers Are Legal but Unethical. AMA Journal of Ethics, 20(1), 269–277. 10.1001/journalofethics.2018.20.3.pfor1-1803 [DOI] [PubMed] [Google Scholar]
- Committee Opinion No. 676: Health Literacy to Promote Quality of Care. (2016). Obstetrics & Gynecology, 128(4), e183–e186. 10.1097/AOG.0000000000001714 [DOI] [PubMed] [Google Scholar]
- Cutilli CC, & Bennett IM (2009). Understanding the Health Literacy of America Results of the National Assessment of Adult Literacy. Orthopaedic Nursing / National Association of Orthopaedic Nurses, 28(1), 27–34. 10.1097/01.NOR.0000345852.22122.d6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehlendorf C, Harris LH, & Weitz TA (2013). Disparities in Abortion Rates: A Public Health Approach. American Journal of Public Health, 103(10), 1772–1779. 10.2105/AJPH.2013.301339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge LE, Haider S, & Hacker MR (2013). Knowledge of state-level abortion laws and regulations among reproductive health care providers. Women’s Health Issues: Official Publication of the Jacobs Institute of Women’s Health, 23(5), e281–286. 10.1016/j.whi.2013.06.003 [DOI] [PubMed] [Google Scholar]
- Dodge LE, Phillips SJ, Neo DT, Nippita S, Paul ME, & Hacker MR (2018). Quality of Information Available Online for Abortion Self-Referral. Obstetrics & Gynecology, 132(6), 1443. 10.1097/AOG.0000000000002950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, Sonfield A, & Jones RK (2014). Changes in out-of-pocket payments for contraception by privately insured women during implementation of the federal contraceptive coverage requirement. Contraception, 89(2), 97–102. 10.1016/j.contraception.2013.11.015 [DOI] [PubMed] [Google Scholar]
- Grossman D, Hendrick E, Fuentes L, White K, Hopkins K, Stevenson A, Lopez CH, Yeatman S, & Potter JE (2015). Knowledge, opinion and experience related to abortion self-induction in Texas. Contraception, 92(4), 360–361. 10.1016/j.contraception.2015.06.036 [DOI] [Google Scholar]
- Hsu T. (2019, May 21). Google Changes Abortion Ad Policy (2228046060). New York Times: (Online); New York Times Company; ProQuest Central. https://login.proxy.lib.duke.edu/login?url=https://www.proquest.com/docview/2228046060?accountid=10598 [Google Scholar]
- Jones RK, & Jerman J. (2017). Population Group Abortion Rates and Lifetime Incidence of Abortion: United States, 2008–2014. American Journal of Public Health, 107(12), 1904–1909. 10.2105/AJPH.2017.304042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahan DM, Peters E, Dawson E, & Slovic P. (2013). Motivated Numeracy and Enlightened Self-Government (SSRN Scholarly Paper ID 2319992). Social Science Research Network. 10.2139/ssrn.2319992 [DOI] [Google Scholar]
- Kavanaugh ML, Bessett D, Littman LL, & Norris A. (2013). Connecting Knowledge about Abortion and Sexual and Reproductive Health to Belief about Abortion Restrictions: Findings from an Online Survey. Women’s Health Issues, 23(4), e239–e247. 10.1016/j.whi.2013.04.003 [DOI] [PubMed] [Google Scholar]
- Kilfoyle KA, Vitko M, O’Conor R, & Bailey SC (2016). Health Literacy and Women’s Reproductive Health: A Systematic Review. Journal of Women’s Health, 25(12), 1237–1255. 10.1089/jwh.2016.5810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimport K. (2020). Pregnant Women’s Reasons for and Experiences of Visiting Antiabortion Pregnancy Resource Centers. Perspectives on Sexual and Reproductive Health, 52(1), 49–56. 10.1363/psrh.12131 [DOI] [PubMed] [Google Scholar]
- Kimport K, Kriz R, & Roberts SCM (2018). The prevalence and impacts of crisis pregnancy center visits among a population of pregnant women. Contraception, 98(1), 69–73. 10.1016/j.contraception.2018.02.016 [DOI] [PubMed] [Google Scholar]
- Lorini C, Santomauro F, Donzellini M, Capecchi L, Bechini A, Boccalini S, Bonanni P, & Bonaccorsi G. (2018). Health literacy and vaccination: A systematic review. Human Vaccines & Immunotherapeutics, 14(2), 478–488. 10.1080/21645515.2017.1392423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson AL, Cohen S, Galitsky A, Hathaway M, Kappus D, Kerolous M, Patel K, & Dominguez L. (2018). Women’s perceptions and treatment patterns related to contraception: Results of a survey of US women. Contraception, 97(3), 256–273. 10.1016/j.contraception.2017.09.010 [DOI] [PubMed] [Google Scholar]
- Random US City Generator—Populated areas of the US. (n.d.). Random Lists. Retrieved October 23, 2020, from https://www.randomlists.com/random-us-cities
- Raymond-Sidel T. (2019). I SAW THE SIGN: NIFLA V. BECERRA AND INFORMED CONSENT TO ABORTION. Columbia Law Review, 119(8), 2279–2318. JSTOR. 10.2307/26844591 [DOI] [Google Scholar]
- Rosen JD (2012). The public health risks of crisis pregnancy centers. Perspectives on Sexual and Reproductive Health, 44(3), 201–205. 10.1363/4420112 [DOI] [PubMed] [Google Scholar]
- Swartz JJ, Rowe C, Morse JE, Bryant AG, & Stuart GS (2020). Women’s knowledge of their state’s abortion regulations. A national survey. Contraception. 10.1016/j.contraception.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartzendruber A, & Lambert DN (2020). A Web-Based Geolocated Directory of Crisis Pregnancy Centers (CPCs) in the United States: Description of CPC Map Methods and Design Features and Analysis of Baseline Data. JMIR Public Health and Surveillance, 6(1), e16726. 10.2196/16726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartzendruber A, Newton-Levinson A, Feuchs AE, Phillips AL, Hickey J, & Steiner RJ (2018). Sexual and Reproductive Health Services and Related Health Information on Pregnancy Resource Center Websites: A Statewide Content Analysis. Women’s Health Issues, 28(1), 14–20. 10.1016/j.whi.2017.10.007 [DOI] [PubMed] [Google Scholar]
- The Newest Vital Sign | Pfizer: One of the world’s premier biopharmaceutical companies. (n.d.). Retrieved April 27, 2018, from https://www.pfizer.com/health/literacy/public-policyresearchers/nvs-toolkit
- White K, Potter JE, Stevenson AJ, Fuentes L, Hopkins K, & Grossman D. (2016). Women’s Knowledge of and Support for Abortion Restrictions in Texas: Findings from a Statewide Representative Survey. Perspectives on Sexual and Reproductive Health, 48(4), 189–197. 10.1363/48e8716 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.