Abstract
Antibiotic use (and misuse) accelerates antimicrobial resistance (AMR), and addressing this complex problem necessitates behaviour change related to infection prevention and management and to antibiotic prescribing and use. As most antibiotic courses are prescribed in primary care, a key focus of antimicrobial stewardship (AMS) is on changing behaviours outside of hospital. Behavioural science draws on behaviour change theories, techniques and methods developed in health psychology, and can be used to help understand and change behaviours related to AMR/AMS. Qualitative methodologies can be used together with a behavioural science approach to explore influences on behaviour and develop and evaluate behavioural interventions. This paper provides an overview of how the behavioural science approach, together with qualitative methods, can contribute and add value to AMS projects. First, it introduces and explains the relevance of the behavioural science approach to AMR/AMS. Second, it provides an overview of behaviour change ‘tools’: behaviour change theories/models, behavioural determinants and behaviour change techniques. Third, it explains how behavioural methods can be used to: (i) define a clinical problem in behavioural terms and identify behavioural influences; (ii) develop and implement behavioural AMS interventions; and (iii) evaluate them. These are illustrated with examples of using qualitative methods in AMS studies in primary care. Finally, the paper concludes by summarizing the main contributions of taking the behavioural science approach to qualitative AMS research in primary care and discussing the key implications and future directions for research and practice.
Introduction
Antimicrobial resistance (AMR) is a well-recognized urgent public health priority.1–3 The COVID-19 and earlier pandemics have shown us the challenges and dangers to individuals and societies globally when faced with a lack of effective treatments for infections. Worldwide, over 700 000 people die each year from drug-resistant infections and AMR is projected to cause 10 million deaths annually, becoming the leading cause of death by 2050, unless action is taken to avert it.4 While AMR is influenced by a variety of factors and requires multifaceted and multidisciplinary approaches, antibiotic over-prescribing and overuse are among the biggest modifiable contributors.3,4 Most antibiotics are prescribed in primary care,5 often inappropriately6 (i.e. not according to guidelines and for infections that do not usually benefit from antibiotics). Thus, optimizing antibiotic prescribing in primary care is a particularly important target for antimicrobial stewardship (AMS) programmes/interventions.
Human behaviours (actions) play an important role in both driving and mitigating AMR. As behaviours, they are influenced by factors and processes that shape all human behaviour. While multidisciplinary approaches are necessary due to the complexity of AMR and AMS, behavioural science can help with understanding and changing relevant behaviours of the public, patients, professionals and organizations. Understanding behaviour and promoting behaviour change related to AMR/AMS have been recommended in the global and national action plans to address AMR.2–4 The role and contribution of behavioural science and behaviour change in AMR/AMS have also been increasingly recognized in research.7–9 Growing evidence shows that behavioural interventions are effective in addressing AMR/AMS related behaviours (e.g. reducing clinically unnecessary antibiotic prescribing), thus supporting the use of behavioural science.10–13
Behavioural science stretches across multiple fields. In this paper, by a ‘behavioural science approach’ we specifically mean an approach to understanding and changing health-related behaviours that draws on the research on psychological and behaviour change developed in health psychology. It offers a wealth of health-related behaviour change ‘tools’ (e.g. behaviour change theories, techniques), methods (e.g. to develop behavioural interventions) and evidence (e.g. on behaviour change techniques and interventions). The behavioural science approach often involves using qualitative methodologies and methods because they are particularly suitable to identify influences on behaviour and help develop and evaluate interventions, and thus both can be used together in AMS research (M. Wanat, M. Santillo, A. J. Borek, C. C. Butler, S. Tonkin-Crine, ‘The value, challenges and practical considerations when conducting qualitative research on antimicrobial stewardship in primary care’, under review).14
In this paper we aim to outline how the behavioural science approach, together with use of qualitative methods, can contribute to AMS/AMR-related research in primary care, and thus enable more people to understand and use these approaches. First, we introduce the behavioural science approach and explain its relevance to qualitative AMS research. Second, we provide an overview of behaviour change ‘tools’ (theories, techniques). Next, we discuss how the behavioural science methods can be used. We illustrate it with examples of qualitative AMS studies in primary care, while also highlighting areas where this approach could be more utilized in the future. Finally, we summarize the main contributions of the behavioural approach to qualitative AMS research and discuss key implications and future directions for research and practice. The theories, methods and studies presented in this paper are not exhaustive; they have been selected to illustrate how behavioural science can be used and contribute to AMR/AMS research.
Introducing behavioural science and qualitative methodologies in AMS research
Overview of the behavioural science and behaviour change research
Behavioural science covers a range of disciplines and methodologies that focus on understanding human behaviour (i.e. an observable action), and then predicting, altering or promoting certain behaviours. With the growing burden of non-communicable diseases and evidence linking human behaviours to health, theories and research were developed in health psychology to understand and leverage behaviour change to improve health-related outcomes. The idea was to study behaviour change in a systematic and replicable way, and report behaviour change interventions precisely and comprehensively (using consistent terminology), similarly to scientific experiments, thus developing ‘a cumulative science of behaviour change’.15–17 Over decades many different behaviour change theories and models were developed that outline mechanisms/processes of psychological and behaviour change.18 This was enhanced by approaches to classify the content (‘active ingredients’) of behaviour change interventions and link them with change mechanisms.15,16,19–21 This, in turn, enabled accumulation of evidence from trials of behaviour change interventions on consistent and effective content/techniques to change behaviours.21–26 In parallel, methods and principles for developing and evaluating complex behaviour change interventions were developed and systematized.27–31 These approaches have been used to develop evidence on effective behaviour change interventions and techniques to prevent unhealthy (e.g. smoking32) and promote healthy (e.g. healthful diet and physical activity33,34) lifestyle behaviours. As tapering of effects and relapses to old behaviours are common following an initial behaviour change, lifestyle interventions increasingly focus on behaviour maintenance to ensure more sustainable impact.35
Relevance of the behavioural science approach to AMR/AMS
Behavioural science methods and tools, and behaviour change theories and strategies, were largely absent from the early interventions to address AMS/AMR and continue to be underutilized in AMS/AMR research.11,36–39 However, improvements in AMS/AMR depend on supporting the behaviour change of individuals, groups and organizations. These sets of behaviours (actions) relate to antibiotic prescribing and use, preventing and managing/treating infections, and implementing/using AMS interventions. The behavioural science approach can contribute to understanding and promoting change in these behaviours, and in developing and evaluating behavioural AMS/AMR-related interventions. Hence, to address this discrepancy between the absence of behavioural science and its potential, there have been calls to promote the use of behavioural science in AMS/AMR research to understand behavioural determinants and develop effective interventions in primary care9 and secondary care.7,8,40–42 For example, Lorencatto et al.41 outlined four areas where behavioural and social science can contribute to AMS/AMR research: (i) defining the problem in behavioural terms and understanding the current behaviour in a particular context; (ii) adopting a theory-driven, systematic approach to intervention design; (iii) investigating implementation and sustainability of interventions in practice; and (iv) maximizing learning through evidence synthesis and detailed intervention reporting. Donisi et al.40 proposed to incorporate a behavioural science approach into: (i) assessment of the specific context needs; (ii) intervention design; (iii) implementation, communication and education; and (iv) follow-up and audits. The behavioural science approach is well-positioned to contribute to AMS/AMR research as it offers: theories and frameworks to help us understand behaviour change processes and their determinants; techniques to change behaviours and evidence on what works in behaviour change; and principles and methods to systematically develop, refine, implement and evaluate behaviour change interventions. We discuss these aspects in the subsequent sections.
Compatibility of the behavioural science approach and qualitative methodologies
The behavioural science approach fits well with, and often relies on, qualitative methodologies. First, qualitative methods allow an exploratory approach that can help to identify relevant behaviours and to understand influences on behaviours and how best to support behaviour change. Second, qualitative content coding can be used to identify behaviour change techniques in intervention reports and accumulate evidence on effective strategies to change behaviours. Third, qualitative methods are particularly well-suited and recommended for developing, implementing and evaluating behaviour change interventions. Thus, combining behavioural and qualitative methods can contribute to better understanding and improving AMS-related behaviours in primary care and the community. In this paper we draw on examples of studies that combined these approaches. More details on how qualitative methodologies can be used in, and contribute to, the AMS/AMR research can be found elsewhere (M. Wanat, M. Santillo, A. J. Borek, C. C. Butler, S. Tonkin-Crine, ‘The value, challenges and practical considerations when conducting qualitative research on antimicrobial stewardship in primary care’, under review).14,43
Overview of behaviour change tools
Theories and models of behaviour change
A good behaviour change theory provides ‘a parsimonious, coherent explanation of phenomena and general predictions that can be compared against observation’ (Michie et al.,18 p. 23). A model is often considered a schematic representation (e.g. of a theory or phenomenon) but a distinction between theories and models is often blurred and the terms are sometimes used synonymously.44 Theories and models are important because they offer testable, falsifiable predictions, provide a common language to describe the phenomena, and help formulate and address questions and accumulate knowledge systematically.18 Therefore, they can inform development and evaluation of behaviour change interventions in systematic ways, and expand evidence on what works, when and how.
Over 83 behaviour change theories/models have been identified to date,18 and 100 behaviour change maintenance theories.35 Some theories are specific to particular behaviours (e.g. smoking, communication), populations (e.g. adolescents) and types of change (e.g. individual, social, technological). Table 1 briefly summarizes examples of theories of individual health-related behaviour, which have been used in interventions to change AMS/AMR-related behaviours. While behaviour change theories mostly focus on individual, intrapersonal change, there are also theories that relate to group-level behaviours (e.g. group dynamics45), interpersonal behaviour change processes46,47 (e.g. social comparisons,48 social influence49), and social change (e.g. social change theory50 on social norms influencing community and individual change, social action theory51 for population-level behaviour change). It is important and prudent to draw on this wealth of behaviour change theories in AMS/AMR research.
Table 1.
Selected examples of behaviour change theories/models and their use in AMS interventions
| Example behaviour change theories | Summary of proposed psychological and behaviour change mechanisms | Examples of potential and actual use in AMS interventions in primary care and the community |
|---|---|---|
| Health belief model (by Rosenstock)102 | Health-related behaviour (change) is influenced by the perceived susceptibility to the health risk, perceived seriousness of the health risk and belief that perceived benefits of taking action outweigh the barriers to taking action. Other modifying factors include cues to action (internal, external), demographic variables, sociopsychological variables, structural variables (e.g. knowledge about the disease) and self-efficacy (i.e. belief about capability to take action; added later to the model). | To understand and promote behaviours of:
|
| Social learning theory (by Miller and Dollard104 and Bandura)105 | Learning is influenced by drives (motivation for action), cues (stimuli that determines whether, when and where action is taken), responses and rewards. Learning occurs when a response to certain drives and cues is performed and rewarded (internally/externally). It also occurs through imitation of others. Bandura’s theory proposed that learning occurs through observing, modelling, imitating, and reactions of others, and is also influenced by interacting environmental and cognitive factors. | To understand and influence why, how and when:
|
| Theory of planned behaviour (by Ajzen)106 | Behaviour (change) is influenced by attitudes (positive/negative beliefs about the behaviour), subjective norms (perceptions of others’ beliefs about and approval of the behaviour), perceived behavioural control (belief of whether one is able to perform the behaviour, and of barriers/facilitators to its performance); these factors influence behavioural intentions (motivation or willingness to perform the behaviour), which then influences the behaviour. | To understand and influence intentions of:
|
| Self-efficacy theory107 and social cognitive theory108 (by Bandura) | Behaviour (change) is influenced by people’s beliefs about being capable of that change (i.e. self-efficacy), which are influenced by information from: performance accomplishment (e.g. personal experience of success/failure), vicarious experience (of the behaviour or its observation), verbal persuasion and emotional arousal (e.g. stress). Social cognitive theory proposes that the behaviour, the environment and the personal and cognitive factors (including perceived self-efficacy) all interact and determine each other. | To understand and influence:
|
| COM-B system (by Michie et al.)53,111 | Behaviour (change) is influenced by three interacting elements: capability (physical, psychological); opportunity (physical, social); and motivation (automatic, reflective). Behaviour occurs when the motivation to engage with it is greater than motivation for alternative behaviours. | To understand and influence COM-B elements for:
|
Behavioural determinants
Behavioural determinants are the types of factors that influence (facilitate or impede) behaviour and behaviour change. Behavioural determinants identified in behaviour change theories have been synthesized, organized and defined in the theoretical domains framework (TDF).52 The TDF is a list of 14 domains (types) of health-related determinants of individual behaviours (Table 2), which comprise 83 more specific constructs. It is an important and helpful ‘tool’ in the behavioural science approach because it integrates, simplifies and makes more accessible the many different constructs included across behaviour change theories. It provides common vocabulary that can be used to describe behavioural determinants in more abstract, general, and thus comparable terms. The TDF, as a framework, does not explain how these concepts may influence or lead to behaviour change, and which are or are not relevant and important for the targeted behaviour change. However, as these constructs were derived from theories, they can be reverse-linked with change mechanisms. After identifying important behavioural determinants in a target population and for a target behaviour, we can select the most appropriate intervention functions and behaviour change techniques (BCTs) to address them. The behaviour change wheel guide53 provides matrices that link the TDF domains with theoretically congruent COM-B elements, intervention functions (Table 2) and BCTs.54 For example, the TDF domain ‘knowledge’ can be addressed by intervention function ‘education’, ‘skills’ by ‘training’, whereas ‘beliefs about consequences’ can be addressed by interventions involving ‘education’, ‘persuasion’ and/or ‘modelling’.
Table 2.
Behavioural determinants and intervention functions
| Domains of behavioural determinants in the TDF52 | Intervention functions from the behaviour change wheel53 |
|---|---|
|
|
Behaviour change techniques (BCTs)
BCTs are also a key element in the behaviour change ‘toolkit’. A BCT is ‘an observable, replicable, and irreducible component of an intervention designed to alter or redirect causal processes that regulate behaviour; that is, a technique is proposed to be an “active ingredient” of an intervention.55 Taxonomies of BCTs were derived from earlier classifications and descriptions of interventions, mostly targeting lifestyle behaviours.21,55 The most comprehensive BCT Taxonomy v1 comprises 93 types of BCTs, organized into 16 categories.55 Other taxonomies were developed specific to different health behaviours/outcomes, such as smoking cessation,26 sexual health22 or weight loss.56,57 Although to our knowledge there is currently no taxonomy of BCTs specific to AMS/AMR-related behaviours, the BCT Taxonomy v1 is a useful source of generic and commonly used BCTs.
BCT taxonomies are helpful because they provide ‘menus’ of BCTs that could be selected and used to facilitate behaviour change processes. However, they do not provide guidance on which BCTs may be helpful or effective at changing a particular determinant or behaviour, so they should be used with consideration of change mechanisms, i.e. which BCTs are theoretically congruent with different TDF domains and/or intervention functions.53,54 BCT taxonomies also help specify the content of interventions during intervention design and reporting, thus improving clarity and transparency of the ‘active ingredients’ in behaviour change interventions. Finally, they can be used to code the content (descriptions) of existing interventions and compare them in systematic reviews and meta-analyses, thus helping develop evidence on which techniques increase intervention effectiveness.23,24,26,58
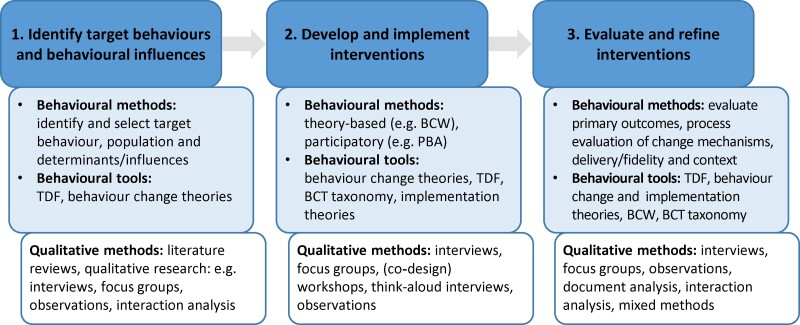
Using behavioural science and qualitative methods in AMS research in primary care
In this section we describe how the behavioural science methods and behaviour change tools can be used together with qualitative methods to target AMS-related behaviour change in primary care. We illustrate it with examples from our and others’ studies, and highlight areas for future contributions.
1. Identifying target behaviours and behavioural influences
Before we can address a health-related problem, the behavioural science approach stipulates that we first conduct a ‘behavioural diagnosis’ to develop a good understanding of what the problem is and identify behaviour(s) contributing to it and influences on these behaviours.41,53
When identifying target behaviours, it helps to do so precisely—that is, by specifying the target behaviour and type of change, how to perform it correctly, who needs to perform it, and when or in what context. Many AMS behaviours are actually complex sets of multiple behaviours (actions, steps) performed by different people and in different contexts. For example, infection prevention is a vague category that could include many potential behaviours (e.g. handwashing, covering a cough, avoiding contact); whereas washing hands is a specific behaviour but involves several steps to do it correctly (e.g. taking soap, hand movements, drying), at the right time, in the right context, and by the right person. It also helps to consider and specify what kind of behaviour change we aim for, for example, performance/discontinuation, increase/decrease or a change in an aspect of a behaviour (e.g. prescribing a different type of antibiotic). Moreover, we need to decide whether our intervention will target one behaviour (e.g. an automatic reminder of prescribing guidelines to prompt a change in the type of antibiotic prescribed), or if it will target multiple behaviours with multifaceted components (e.g. a training programme to increase the use of specific communication strategies and patient leaflets). Finally, it is important to specify the target population (i.e. whose behaviour needs to change, e.g. patients, doctors, administrative staff), and when or in what context (e.g. during or outside a consultation).
Facilitating change in modifiable, observable and specific behaviours that contribute to the identified issue is the main aim of behavioural interventions; whereas facilitating change in psychological/behavioural determinants is how that change can be achieved. Psychological concepts, such as intentions or motivation, are behavioural determinants and may not always correspond with actual behaviour; this is commonly referred to as the ‘intention-behaviour gap’.59 For example, one can be aware of the importance of a behaviour (e.g. handwashing) and motivated to perform it, but may still not perform it due to different types of barriers (e.g. environmental: lack of soap/space; social: observing others not washing their hands in a similar context; psychological/cognitive: forgetting/lack of habit).
After defining target behaviours, it is important to identify relevant behavioural determinants and influences. Influences are sometimes referred to as ‘barriers and facilitators’ to mean the factors that impede/prevent or facilitate/enhance the behaviour (change). It can also help to be mindful of a difference between influences on the behaviour versus influences on the behaviour change. For example, knowledge of prescribing guidelines influences antibiotic prescribing but alone will not necessarily influence a change in prescribing behaviour, whereas knowledge of a discrepancy between one’s prescribing and guidelines might. Behavioural determinants/influences can be also expressed in general, abstract terms using the TDF.52 For example, a belief that most acute infections resolve without antibiotics can be expressed using a TDF domain ‘beliefs about health consequences’.
Qualitative research can help identify target behaviours and behavioural influences. If relevant empirical research already exists, a review of qualitative studies can help identify these. For example, reviews of qualitative studies have synthesized influences on antibiotic prescribing for acute respiratory infections in primary care,60–63 and on parental views related to antibiotic prescribing for children in primary care.64 If sufficient or relevant research is lacking, conducting a qualitative study may help. For example, interviews and focus groups allow identification of participants’ perceptions and experiences of specific behaviours and behavioural influences.65–69 Other approaches, such as ethnographic43,70 and interaction analyses,71,72 can help identify patterns of behaviours and influences, rather than depending only on perceptions or recollections. Moreover, consulting with stakeholders and patient and public involvement (PPI) groups (e.g. comprising public and patient representatives) can help in multiple ways: to identify and select key target behaviours that are important and feasible to change and their determinants, to inform reviews and/or to design ethical and acceptable qualitative studies to explore the behaviours and determinants.
Qualitative methods to identify behavioural influences can be informed and/or supported by the use the TDF52 or COM-B elements.53 For example, they can be used to inform semi-structured interview topic guides;73,74 this can be beneficial by ensuring that interviewers explore all the potential ways behaviours may be influenced. They can also be used to inform data analysis or interpretation in qualitative studies and syntheses of qualitative studies, including deductive75 and inductive (Figure 1)62 approaches; this can be beneficial by making specific types of influences more generalizable and comparable, and allowing linking them with behavioural mechanisms.
Figure 1.
Example behavioural analysis of AMS-related influences and interventions in primary care.
2. Developing and implementing AMS interventions
One of the main contributions of the behavioural science approach is in promoting and offering systematic, rigorous methods to develop behaviour change interventions. Many different approaches to intervention development exist; for example, a systematic methods overview and taxonomy identified eight types of approaches to developing health interventions (each with multiple specific methodologies).29 Some approaches are centred on behaviour change theory and evidence, e.g. the behaviour change wheel53 and intervention mapping;76 others focus on partnerships, co-production77 and target population (e.g. the person-based approach78,79). Behavioural theories and qualitative methods can contribute to most intervention development approaches, and can increase acceptability, feasibility and relevance of the interventions. For example, one of the barriers to clinicians changing their antibiotic prescribing is a perception that their actions have little role to play; theory-based interventions aimed to address these by providing reasons for change (the ‘why’) and feasible and time-efficient strategies (the ‘how’).80 The ‘Stemming the Tide of Antimicrobial Resistance’ (STAR) intervention was developed based on social learning theory and qualitative research as it aimed to address clinicians’ reasons for changing, increase their perceived importance of change, and their ability and perceived efficacy to change.12,81 The ‘Internet Training for Reducing antibiOtic use’ (GRACE-INTRO) intervention drew on the theory of planned behaviour as it aimed to influence clinicians’ attitudes, confidence and intentions to reduce antibiotic prescribing, and on qualitative research on influences and views of potential interventions.60,82–84
The person-based approach (PBA) is an example of an intervention development methodology that integrates the theory- and evidence-based approaches with qualitative methods with the target population and stakeholders.78,79,85 This helps ensure that interventions have clear intended mechanisms of change; are feasible to implement; and are acceptable, correctly understood and used by the target population. The PBA highlights the importance of identifying target behaviours and influences through (synthesizing or conducting empirical) qualitative research with the target population and stakeholder consultations. The influences are mapped to relevant theories and frameworks (e.g. COM-B53 or TDF52) to identify the behavioural determinants and theoretically congruent intervention functions. Relevant BCTs are selected to facilitate specific psychological and behaviour changes.55 The PBA (and other approaches) involves developing a programme theory that outlines how exactly the intervention is intended to work: its objectives, components/features and delivery methods, and how they are linked together into a mechanism of action. The programme theory may draw on an established behaviour change theory (or theories) or be unique to the intervention and target behaviours and population. A logic model is usually developed to diagrammatically summarize the programme theory.
The initial intervention (materials) can be then developed through (e.g. co-design) workshops and refined with ‘think-aloud’ interviews with the target users—these involve participants from the target population using the prototype/initial intervention while ‘thinking aloud’ and answering questions about design and content. They help identify ways to improve the intervention to make it more acceptable, easier to use and correctly understood, and thus more likely to be effective. During the different stages of intervention development research activities are accompanied by consultations with collaborators and stakeholders, and members of the PPI group. Using the PBA and qualitative methods is illustrated in developing AMS interventions in secondary86 and primary care (Figure 2).87
Figure 2.
Example of developing an AMS intervention in primary care. aM. Wanat, M. Santillo, U. Galal, M. Davoudianfar, E. Bongard, S. Savic, L. Savic, C. E. Porter, J. Fielding, C. Butler, S. H. Pavitt, J. A. T. Sandoe, S. Tonkin-Crine; ‘Mixed-methods evaluation of a behavioural intervention package to identify and amend incorrect penicillin allergy records in UK general practice’, under review.
A similar behavioural science approach can be also used to support and improve the implementation of existing AMS interventions in primary care. Implementation involves a complex set of behaviours; for example, it may require developing new practice protocols, introducing new practices, using new equipment or communicating a change in practice to the team. Implementation may require the change in individual, team or organizational behaviours and practices (e.g. ways of working together). Behaviour change tools can help facilitate change in implementation-related behaviours. For example, a guide outlines how the TDF can be applied to assess and address implementation issues.88 Moreover, there are theories and frameworks that are specific to outlining and facilitating implementation89,90and de-implementation processes.91 Interventions to address implementation issues can be developed using behavioural and qualitative methods and by drawing on behavioural and implementation theories/frameworks. For example, the PBA was used to develop an intervention to promote the implementation of evidence-based AMS interventions underused in English primary care (Figure 3).92
Figure 3.
Example of developing an intervention to improve implementation of AMS interventions in primary care. aS. Tonkin-Crine, M. Mcleod, A. J. Borek, A. Campbell, P. Anyanwu, C. Costelloe, M. Moore, A. Holmes, C. C. Butler, A. S. Walker and the STEP-UP team; ‘Supporting the use of three antibiotic stewardship strategies in high antibiotic prescribing general practices: an implementation study’, unpublished results.
3. Evaluating behavioural AMS interventions
Evaluation and refinement of behaviour change interventions are important steps for achieving effective, feasible, acceptable and sustainable interventions and, in general, for accumulating evidence. The importance of evaluation and process evaluation, and of addressing a wide range of questions beyond only effectiveness, is highlighted in the Medical Research Council guidance on complex health interventions.27,30,31 These wider questions relate to the mechanisms of impact/action (i.e. how interventions facilitate change); delivery and implementation (i.e. what is delivered and how); and the wider context and system (i.e. what contextual/system factors influence the intervention delivery, implementation, mechanisms and outcomes). Qualitative methods are suitable for these different questions, can be integrated with social science and theory-based approaches,93 and, alongside quantitative research, allow triangulation of methods and findings.94
Behavioural and qualitative approaches to process evaluations allow exploring and understanding the mechanisms of impact, whether the intervention worked in the intended way (i.e. compared with the programme theory), why it did not work or what unintended consequences it led to. The programme theory and logic model provide concepts and processes that should be explored in process evaluation. These usually include psychological change (e.g. in motivation, self-efficacy), cognitive change (e.g. in knowledge) and/or change in capabilities/skills related to performing the target behaviour. We can use qualitative methods to explore participants’ perceptions and experiences related to different types of change, whether and how interventions worked (or not), and which BCTs were seen as helpful (or not). For example, the mixed-methods process evaluation of the GRACE-INTRO intervention helped explore and confirm the change mechanisms (Figure 4).95,96
Figure 4.
Example of using mixed methods to evaluate an AMS intervention in primary care.
Behavioural and qualitative approaches can also contribute to exploring issues related to delivery, implementation and receipt of interventions, which may help explain outcomes and/or identify future refinements. Fidelity of delivery is the extent to which the core components of interventions are delivered as intended; good fidelity is critical for study validity.97,98 There are many aspects of fidelity, including intervention components, interventionist behaviours, participant comprehension and adherence.98 As delivery may involve intentional or unintentional changes to the intervention components delivered, fidelity of delivery should be assessed against the intervention theory/logic model that specifies the core intervention components and delivery methods. This is particularly important for interventions delivered by people (e.g. trainers, providers) who may need to be trained and provided with delivery manuals/protocols. Other important aspects include reach (i.e. the proportion of the target population who receive or are affected by the intervention),99 and receipt (i.e. the extent to which participants received the intervention, their engagement, comprehension and/or use of the intervention).98 These components are particularly important for digital or self-delivered interventions. Different methods can be used to ensure and assess intervention delivery and receipt.97 Qualitative methods may help to understand these issues through observations or analyses of recordings of the intervention being delivered, interviews or focus groups with participants and those delivering the intervention, or delivery checklists (with open questions about delivery issues or adaptations). For example, an intervention comprising a commitment poster for clinicians (pledging a commitment to prudent antibiotic prescribing) showed no significant effect on prescribing behaviour.100 Interviews with clinicians, as part of the process evaluation, showed suboptimal implementation and receipt of the intervention, which might partly explain the lack of effect; for example, some clinicians did not realize that they were making a pledge (e.g. their signatures were added to posters without clinicians reading them), and some thought the posters were supposed to influence patients’ not clinicians’ behaviours (S. Tonkin-Crine, A. Schneider, N. Herd, S. Michie, C. C. Butler, T. Chadborn, A. Sallis, ‘Implementing practice-level nudge interventions to encourage prudent antibiotic prescribing in general practice: a mixed-methods process evaluation’, under review).
The behavioural science approach and guidance for complex interventions also recognize the importance of exploring the role and influence of context in which the intervention takes place, and how it might affect the mechanisms, delivery/implementation and outcomes. Context may involve place, setting, team, organization or community, as well as the wider social, cultural, economic, regulatory, policy or political influences. For example, the behaviour change wheel model outlines seven categories constituting a wider policy and regulatory context (i.e. regulation, legislation, fiscal measures, guidelines, environmental/social planning and communication/marketing).53 Qualitative research can help us understand contextual factors. For example, interviews with professionals from general practices and clinical commissioning groups that explored the implementation and mechanisms of the Quality Premium (an intervention to improve antibiotic prescribing in English general practice) allowed us to identify contextual factors on the practice, local and national level that were perceived to influence antibiotic prescribing and engagement with AMS interventions.69 Another example involves interviews with professionals in general practices participating in the implementation study of the intervention described in Figure 3; the interviews helped to identify how the differences in the practice-level context (e.g. practice communication, leadership) influenced engagement with the intervention (S. Tonkin-Crine, M. Mcleod, A. J. Borek, A. Campbell, P. Anyanwu, C. Costelloe, M. Moore, A. Holmes, C. C. Butler, A. S. Walker and the STEP-UP team; ‘Supporting the use of three antibiotic stewardship strategies in high antibiotic prescribing general practices: an implementation study’, unpublished results).
Contributions and implications of using the behavioural science in AMS research
Behavioural science and qualitative methods have contributed to AMS/AMR research and have the potential to improve existing and future AMS interventions: their capacity to affect relevant, important determinants; their acceptability, feasibility, reach and capacity to engage the target population; and their effectiveness and implementation outside research contexts. Figure 5 offers a summary of the described ways in which the behavioural science tools and methods, together with qualitative methods, can contribute to enhancing our knowledge of AMS/AMR issues and developing, improving, adapting and implementing AMS interventions.
Figure 5.
Contributions of the behavioural and qualitative methods to AMS/AMR research. BCW, behaviour change wheel; BCT, behaviour change techniques; PBA, person-based approach; TDF, theoretical domains framework.
The ambition for advancing health-related behaviour change research was to improve the scientific rigour, evidence and replicability of behaviour change interventions. Using behavioural theories and methodologies will help develop evidence of what works and how in AMS research. With the increasing threat of AMR consequences, it is critical to build on and improve existing knowledge and evidence.
Using the behavioural science approach with qualitative methods has implications for planning and conducting research and practice-based quality improvement projects. It means that those involved in such projects need to understand, or be trained in, the behavioural and qualitative methods. Projects can benefit from multidisciplinary teams including behavioural and qualitative researchers. Using the behavioural and qualitative methods has also methodological implications. It is important to consider carefully, and reflect on, how behavioural and qualitative methods are used together and what impact that might have on the process, data and findings. For example, consideration may be given to the potential impact of decisions about how theory is selected and used; who is involved in intervention development; which qualitative methodology is used (e.g. interviews allow identification of self-reported perceptions and experiences, whereas observations allow identification of actual behaviour); or whether deductive or inductive approaches to data analysis are used.
Behaviour change theories were mostly developed based on, and aimed at, health-related lifestyle behaviours. Some theories may be more or less relevant to AMS/AMR-related behaviours. Similarly, some BCTs may be not applicable to clinical and/or AMS/AMR behaviours, whereas other potential BCTs may have not been included in the existing taxonomies. Future research could develop or identify theories and BCTs specific to changing clinical and AMS/AMR-related behaviours. Moreover, it is important to develop theories, techniques and evidence on maintenance of promoted AMS-related behaviours (not only behaviour change), thus helping to improve sustainability of intervention effects.
The importance of transparent and comprehensive reporting of the content, mechanisms and active ingredients of behaviour change interventions seems now indisputable.15–17 Guidelines, such as TIDieR,101 promote better reporting of interventions (including e.g. theory, mechanisms, components, delivery, adaptations/modifications). Behavioural tools provide consistent, common vocabulary for behaviour change interventions. These tools and guidelines should be used when reporting AMS interventions too. Publishing reports of development and content of AMS interventions would also be helpful.
Finally, the behavioural science approach offers a perspective and a set of tools, out of many that might be relevant and helpful. Slowing down and mitigating AMR, a complex problem with different types of contributing/influencing factors, requires a multidisciplinary approach. Behavioural and social scientists can make important and helpful contributions as part of multidisciplinary teams, and may help develop relevant, effective/impactful, feasible, acceptable and implementable interventions.
In summary, our key recommendations for utilizing the behavioural science approach more fully in AMS/AMR research and practice include: ensuring a thorough understanding of behaviours and determinants/influences that contribute to the identified AMS/AMR-related problem before trying to change them; using more diverse qualitative methods to identify and understand behaviours and (behavioural and contextual) influences, especially through observations and interaction analyses; using and reporting behaviour change theories, frameworks and techniques more consistently in AMS interventions, and ensuring that each intervention has a programme theory and a logic model outlining the change mechanisms; involving target populations/users, stakeholders and PPI groups to guide/inform all stages of intervention development and evaluation; and including qualitative and mixed-methods process evaluations in studies piloting and evaluating behavioural AMS interventions. For behavioural scientists working on AMS/AMR, the next steps may need to involve developing behaviour change theories and techniques specific to AMS/AMR-related behaviours and contexts; further developing evidence on what works, how and in what contexts, when using different behaviour change strategies and types of interventions to address AMS/AMR-related problems; and promoting the implementation of effective behavioural AMS interventions.
Conclusions
The behavioural science approach and qualitative methods fit well together and can contribute to AMS/AMR research. The behavioural science approach offers theories, frameworks and techniques related to changing human behaviours, and methods for developing behaviour change interventions. The qualitative approaches offer methodologies and methods for collecting, analysing and interpreting data from relevant target populations and stakeholders, and thus can help understand the behaviours and influences, develop acceptable, engaging and effective interventions, and evaluate them. These approaches were mostly absent from early AMS/AMR interventions,11,36–38 however their role in AMS has been increasingly recognized and promoted in secondary care.7,8,40–42 They now also have an important role to promote AMS and optimize antibiotic prescribing in primary care.9 We hope that this paper will enable more researchers and healthcare professionals to understand and use these approaches.
Funding
The work was supported by the Economic and Social Research Council through the Antimicrobial Resistance Cross Council Initiative supported by the seven research councils in partnership with other funders (ES/P008232/1 to A.J.B. and S.T.-C.) and by the National Institute for Health Research (NIHR) Health Protection Research Unit in Healthcare Associated Infections and Antimicrobial Resistance (NIHR200915) at the University of Oxford in partnership with the UK Health Security Agency (UKHSA) (S.T.-C. and C.C.B.).
Transparency declarations
None to declare.
Disclaimer
The views expressed in this publication are those of the authors and not necessarily those of the NIHR, UKHSA or the Department of Health and Social Care.
For the purpose of open access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising.
References
- 1. Department of Health . UK 5 Year Antimicrobial Resistance Strategy 2013 to 2018. 2013. https://www.gov.uk/government/publications/uk-5-year-antimicrobial-resistance-strategy-2013-to-2018.
- 2. Department of Health and Social Care . UK 5-year Action Plan for Antimicrobial Resistance 2019 to 2024. 2019. https://www.gov.uk/government/publications/uk-5-year-action-plan-for-antimicrobial-resistance-2019-to-2024.
- 3. WHO . Global Action Plan on AMR. 2015. https://www.who.int/publications/i/item/9789241509763.
- 4. O’Neill J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. The Review on Antimicrobial Resistance. 2016. https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf.
- 5. Public Health England . English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2019 to 2020. 2020. https://www.gov.uk/government/publications/english-surveillance-programme-antimicrobial-utilisation-and-resistance-espaur-report.
- 6. Smieszek T, Pouwels KB, Dolk FCKet al. Potential for reducing inappropriate antibiotic prescribing in English primary care. J Antimicrob Chemother 2018; 73Suppl 2: ii36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Charani E, Castro-Sánchez E, Holmes A. The role of behavior change in antimicrobial stewardship. Infect Dis Clin 2014; 28: 169–75. [DOI] [PubMed] [Google Scholar]
- 8. Bassetti M, Giacobbe DR, Vena Aet al. Challenges and research priorities to progress the impact of antimicrobial stewardship. Drugs Context 2019; 8: 212600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tonkin-Crine S, Walker AS, Butler CC. Contribution of behavioural science to antibiotic stewardship. BMJ 2015; 350: h3413. [DOI] [PubMed] [Google Scholar]
- 10. Cuevas C, Batura N, Wulandari LPLet al. Improving antibiotic use through behaviour change: a systematic review of interventions evaluated in low- and middle-income countries. Health Policy Plan 2021; 36: 754–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Davey P, Marwick CA, Scott CLet al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev 2017; issue 2: CD003543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Butler CC, Simpson SA, Dunstan Fet al. Effectiveness of multifaceted educational programme to reduce antibiotic dispensing in primary care: practice based randomised controlled trial. BMJ 2012; 344: d8173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Little P, Stuart B, Francis Net al. Effects of internet-based training on antibiotic prescribing rates for acute respiratory-tract infections: a multinational, cluster, randomised, factorial, controlled trial. Lancet 2013; 382: 1175–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. van den Bergh D, Brink A. A commitment and call to strengthen and expand qualitative research efforts to improve the impact of antimicrobial stewardship. JAC Antimicrob Resist 2021; 3: dlab151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Michie S, Abraham C. Advancing the science of behaviour change: a plea for scientific reporting. Addiction 2008; 103: 1409–10. [DOI] [PubMed] [Google Scholar]
- 16. Michie S, Fixsen D, Grimshaw JMet al. Specifying and reporting complex behaviour change interventions: the need for a scientific method. Implementat Sci 2009; 4: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Michie S, Johnston M. Theories and techniques of behaviour change: developing a cumulative science of behaviour change. Health Psychol Rev 2012; 6: 1–6. [Google Scholar]
- 18. Michie S, West R, Campbell Ret al. ABC of Behaviour Change Theories: An Essential Resource for Researchers, Policy Makers and Practitioners. Silverback Publishing, 2014. [Google Scholar]
- 19. Stavri Z, Michie S. Classification systems in behavioural science: current systems and lessons from the natural, medical and social sciences. Health Psychol Rev 2012; 6: 113–40. [Google Scholar]
- 20. Michie S, Abraham C. Interventions to change health behaviours: evidence-based or evidence-inspired? Psychol Health 2004; 19: 29–49. [Google Scholar]
- 21. Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008; 27: 379–87. [DOI] [PubMed] [Google Scholar]
- 22. Albarracín D, Gillette JC, Earl ANet al. A test of major assumptions about behavior change: a comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull 2005; 131: 856–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gardner B, Whittington C, McAteer Jet al. Using theory to synthesise evidence from behaviour change interventions: the example of audit and feedback. Soc Sci Med 2010; 70: 1618–25. [DOI] [PubMed] [Google Scholar]
- 24. Dusseldorp E, van Genugten L, van Buuren Set al. Combinations of techniques that effectively change health behavior: evidence from Meta-CART analysis. Health Psychol 2014; 33: 1530. [DOI] [PubMed] [Google Scholar]
- 25. Peters G-JY, de Bruin M, Crutzen R. Everything should be as simple as possible, but no simpler: towards a protocol for accumulating evidence regarding the active content of health behaviour change interventions. Health Psychol Rev 2015; 9: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. West R, Walia A, Hyder Net al. Behavior change techniques used by the English Stop Smoking Services and their associations with short-term quit outcomes. Nicotine Tob Res 2010; 12: 742–7. [DOI] [PubMed] [Google Scholar]
- 27. Craig P, Dieppe P, Macintyre Set al. Developing and evaluating complex interventions: the new guidance. BMJ 2008; 337: a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. O’Cathain A, Croot L, Duncan EASet al. Guidance on how to develop complex interventions to improve health and health care. BMJ Open 2019; 9: e029954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. O’Cathain A, Croot L, Sworn Ket al. Taxonomy of approaches to developing interventions to improve health: a systematic methods overview. Pilot Feasibility Stud 2019; 5: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Skivington K, Matthews L, Simpson SAet al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021; 374: n2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Moore GF, Audrey S, Barker Met al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015; 350: h1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Black N, Johnston M, Michie Set al. Behaviour change techniques associated with smoking cessation in intervention and comparator groups of randomized controlled trials: a systematic review and meta-regression. Addiction 2020; 115: 2008–20. [DOI] [PubMed] [Google Scholar]
- 33. Cradock KA, ÓLaighin G, Finucane FMet al. Behaviour change techniques targeting both diet and physical activity in type 2 diabetes: a systematic review and meta-analysis. Int J Behav Nutr Phys Act 2017; 14: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Samdal GB, Eide GE, Barth Tet al. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int J Behav Nutr Phys Act 2017; 14: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kwasnicka D, Dombrowski SU, White Met al. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychol Rev 2016; 10: 277–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Charani E, Edwards R, Sevdalis Net al. Behavior change strategies to influence antimicrobial prescribing in acute care: a systematic review. Clin Infect Dis 2011; 53: 651–62. [DOI] [PubMed] [Google Scholar]
- 37. Davey P, Peden C, Charani Eet al. Time for action—Improving the design and reporting of behaviour change interventions for antimicrobial stewardship in hospitals: early findings from a systematic review. Int J Antimicrob Agents 2015; 45: 203–12. [DOI] [PubMed] [Google Scholar]
- 38. Pinder R, Sallis A, Berry Det al. Antibiotic Prescribing and Behaviour Change in Healthcare Settings: Literature Review and Behavioural Analysis. Public Health England, 2015. https://www.gov.uk/government/publications/antibiotic-prescribing-and-behaviour-change-in-healthcare-settings.
- 39. Rawson TM, Moore LSP, Tivey AMet al. Behaviour change interventions to influence antimicrobial prescribing: a cross-sectional analysis of reports from UK state-of-the-art scientific conferences. Antimicrob Resist Infect Control 2017; 6: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Donisi V, Sibani M, Carrara Eet al. Emotional, cognitive and social factors of antimicrobial prescribing: can antimicrobial stewardship intervention be effective without addressing psycho-social factors? J Antimicrob Chemother 2019; 74: 2844–7. [DOI] [PubMed] [Google Scholar]
- 41. Lorencatto F, Charani E, Sevdalis Net al. Driving sustainable change in antimicrobial prescribing practice: how can social and behavioural sciences help? J Antimicrob Chemother 2018; 73: 2613–24. [DOI] [PubMed] [Google Scholar]
- 42. Rzewuska M, Charani E, Clarkson JEet al. Prioritizing research areas for antibiotic stewardship programmes in hospitals: a behavioural perspective consensus paper. Clin Microbiol Infect 2019; 25: 163–8. [DOI] [PubMed] [Google Scholar]
- 43. Tompson AC, Manderson L, Chandler CIR. Understanding antibiotic use: practices, structures and networks. JAC Antimicrob Resist 2021; 3: dlab150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wunsch G. Theories, models, and data. Demografie 1994; 36: 20. [PubMed] [Google Scholar]
- 45. Cartwright D, Zander AF. Group Dynamics: Research and Theory, 3rd edn. Tavistock, 1968. [Google Scholar]
- 46. Borek AJ, Abraham C. How do small groups promote behaviour change? An integrative conceptual review of explanatory mechanisms. Appl Psychol Health Well-Being 2018; 10: 30–61. [DOI] [PubMed] [Google Scholar]
- 47. Borek AJ, Abraham C, Greaves CJet al. Identifying change processes in group-based health behaviour-change interventions: development of the mechanisms of action in group-based interventions (MAGI) framework. Health Psychol Rev 2019; 13: 227–47. [DOI] [PubMed] [Google Scholar]
- 48. Festinger L. A theory of social comparison processes. Hum Relat 1954; 7: 117–40. [Google Scholar]
- 49. Turner JC. Social Influence, 1st edn. Cengage Learning, 1991. [Google Scholar]
- 50. Thompson B, Kinne S. Social change theory: applications to community health. In: Bracht N, ed. Health Promotion at the Community Level 2: New Advances. Sage, 1999; 29–46. [Google Scholar]
- 51. Ewart CK. Social action theory for a public health psychology. Am Psychol 1991; 46: 931–46. [DOI] [PubMed] [Google Scholar]
- 52. Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012; 7: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Michie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. Silverback Publishing, 2014. [Google Scholar]
- 54. Michie S, Johnston M, Rothman Aet al. Behaviour Change Techniques and Theory. https://www.ucl.ac.uk/pals/research/clinical-educational-and-health-psychology/research-groups/behaviour-change-techniques-and.
- 55. Michie S, Richardson M, Johnston Met al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013; 46: 81–95. [DOI] [PubMed] [Google Scholar]
- 56. Michie S, Ashford S, Sniehotta FFet al. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011; 26: 1479–98. [DOI] [PubMed] [Google Scholar]
- 57. Hartmann-Boyce J, Aveyard P, Koshiaris Cet al. Development of tools to study personal weight control strategies: OxFAB taxonomy. Obesity 2016; 24: 314–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Hankonen N, Sutton S, Prevost ATet al. Which behavior change techniques are associated with changes in physical activity, diet and body mass index in people with recently diagnosed diabetes? Ann Behav Med 2015; 49: 7–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sheeran P. Intention—behavior relations: a conceptual and empirical review. Eur Rev Soc Psychol 2002; 12: 1–36. [Google Scholar]
- 60. Tonkin-Crine S, Yardley L, Little P. Antibiotic prescribing for acute respiratory tract infections in primary care: a systematic review and meta-ethnography. J Antimicrob Chemother 2011; 66: 2215–23. [DOI] [PubMed] [Google Scholar]
- 61. Germeni E, Frost J, Garside Ret al. Antibiotic prescribing for acute respiratory tract infections in primary care: an updated and expanded meta-ethnography. Br J Gen Pract 2018; 68: e633–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Borek AJ, Wanat M, Atkins Let al. Optimising antimicrobial stewardship interventions in English primary care: a behavioural analysis of qualitative and intervention studies. BMJ Open 2020; 10: e039284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. O’Connor R, O’Doherty J, O’Regan Aet al. Antibiotic use for acute respiratory tract infections (ARTI) in primary care; what factors affect prescribing and why is it important? A narrative review. Ir J Med Sci 2018; 187: 969–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Lucas PJ, Cabral C, Hay ADet al. A systematic review of parent and clinician views and perceptions that influence prescribing decisions in relation to acute childhood infections in primary care. Scand J Prim Health Care 2015; 33: 11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. van der Zande MM, Dembinsky M, Aresi Get al. General practitioners’ accounts of negotiating antibiotic prescribing decisions with patients: a qualitative study on what influences antibiotic prescribing in low, medium and high prescribing practices. BMC Fam Pract 2019; 20: 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wood F, Simpson S, Butler CC. Socially responsible antibiotic choices in primary care: a qualitative study of GPs’ decisions to prescribe broad-spectrum and fluroquinolone antibiotics. Fam Pract 2007; 24: 427–34. [DOI] [PubMed] [Google Scholar]
- 67. Kumar S, Little P, Britten N. Why do general practitioners prescribe antibiotics for sore throat? Grounded theory interview study. BMJ 2003; 326: 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Borek AJ, Campbell A, Dent Eet al. Implementing interventions to reduce antibiotic use: a qualitative study in high-prescribing practices. BMC Fam Pract 2021; 22: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Borek AJ, Anthierens S, Allison Ret al. Social and contextual influences on antibiotic prescribing and antimicrobial stewardship: a qualitative study with clinical commissioning group and general practice professionals. Antibiotics 2020; 9: 859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Charani E, Smith I, Skodvin Bet al. Investigating the cultural and contextual determinants of antimicrobial stewardship programmes across low-, middle- and high-income countries—a qualitative study. PLoS One 2019; 14: e0209847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Cabral C, Horwood J, Hay ADet al. How communication affects prescription decisions in consultations for acute illness in children: a systematic review and meta-ethnography. BMC Fam Pract 2014; 15: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Stivers T. Managing patient pressure to prescribe antibiotics in the clinic. Pediatr Drugs 2021; 23: 437–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Eley CV, Sharma A, Lecky DMet al. Qualitative study to explore the views of general practice staff on the use of point-of-care C reactive protein testing for the management of lower respiratory tract infections in routine general practice in England. BMJ Open 2018; 8: e023925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lecky DM, Howdle J, Butler CCet al. Optimising management of UTIs in primary care: a qualitative study of patient and GP perspectives to inform the development of an evidence-based, shared decision-making resource. Br J Gen Pract 2020; 70: e330–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Atkins L, Sallis A, Chadborn Tet al. Reducing catheter-associated urinary tract infections: a systematic review of barriers and facilitators and strategic behavioural analysis of interventions. Implement Sci 2020; 15: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Bartholomew LK, Parcel GS, Kok Get al. Planning Health Promotion Programs: An Intervention Mapping Approach. 4th edn. Jossey-Bass, 2016. [Google Scholar]
- 77. Voorberg WH, Bekkers VJJM, Tummers LG. A systematic review of co-creation and co-production: embarking on the social innovation journey. Public Manag Rev 2015; 17: 1333–57. [Google Scholar]
- 78. Yardley L, Ainsworth B, Arden-Close Eet al. The person-based approach to enhancing the acceptability and feasibility of interventions. Pilot Feasibility Stud 2015; 1: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Yardley L, Morrison L, Bradbury Ket al. The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res 2015; 17: e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. McNulty CAM, Francis NA. Optimizing antibiotic prescribing in primary care settings in the UK: findings of a BSAC multi-disciplinary workshop 2009. J Antimicrob Chemother 2010; 65: 2278–84. [DOI] [PubMed] [Google Scholar]
- 81. Butler CC, Rollnick S, Kinnersley Pet al. Reducing antibiotics for respiratory tract symptoms in primary care: consolidating ‘why’ and considering ‘how’. Br J Gen Pract 1998; 48: 1865–70. [PMC free article] [PubMed] [Google Scholar]
- 82. Anthierens S, Tonkin-Crine S, Douglas Eet al. General practitioners’ views on the acceptability and applicability of a web-based intervention to reduce antibiotic prescribing for acute cough in multiple European countries: a qualitative study prior to a randomised trial. BMC Fam Pract 2012; 13: 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Tonkin-Crine S, Yardley L, Coenen Set al. GPs’ views in five European countries of interventions to promote prudent antibiotic use. Br J Gen Pract 2011; 61: e252–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Tonkin-Crine S, Yardley L, Coenen Set al. Strategies to promote prudent antibiotic use: exploring the views of professionals who develop and implement guidelines and interventions. Fam Pract 2013; 30: 88–95. [DOI] [PubMed] [Google Scholar]
- 85. Morrison L, Muller I, Yardley Let al. The person-based approach to planning, optimising, evaluating and implementing behavioural health interventions. Eur Health Psychol 2018; 20: 464–9. [Google Scholar]
- 86. Santillo M, Sivyer K, Krusche Aet al. Intervention planning for Antibiotic Review Kit (ARK): a digital and behavioural intervention to safely review and reduce antibiotic prescriptions in acute and general medicine. J Antimicrob Chemother 2019; 74: 3362–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Santillo M, Wanat M, Davoudianfar Met al. Developing a behavioural intervention package to identify and amend incorrect penicillin allergy records in UK general practice and subsequently change antibiotic use. BMJ Open 2020; 10: e035793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Atkins L, Francis J, Islam Ret al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci 2017; 12: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci 2015; 10: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Esmail R, Hanson HM, Holroyd-Leduc Jet al. A scoping review of full-spectrum knowledge translation theories, models, and frameworks. Implement Sci 2020; 15: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Nilsen P, Ingvarsson S, Hasson Het al. Theories, models, and frameworks for de-implementation of low-value care: a scoping review of the literature. Implement Res Pract 2020; 1. 10.1177/2633489520953762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Borek AJ, Campbell A, Dent Eet al. Development of an intervention to support the implementation of evidence-based strategies for optimising antibiotic prescribing in general practice. Implement Sci Commun 2021; 2: 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Morgan-Trimmer S. Improving process evaluations of health behavior interventions: learning from the social sciences. Eval Health Prof 2015; 38: 295–314. [DOI] [PubMed] [Google Scholar]
- 94. Tonkin-Crine S, Anthierens S, Hood Ket al. Discrepancies between qualitative and quantitative evaluation of randomised controlled trial results: achieving clarity through mixed methods triangulation. Implement Sci 2016; 11: 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Yardley L, Douglas E, Anthierens Set al. Evaluation of a web-based intervention to reduce antibiotic prescribing for LRTI in six European countries: quantitative process analysis of the GRACE/INTRO randomised controlled trial. Implement Sci 2013; 8: 134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Anthierens S, Tonkin-Crine S, Cals JWet al. Clinicians’ views and experiences of interventions to enhance the quality of antibiotic prescribing for acute respiratory tract infections. J Gen Intern Med 2015; 30: 408–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J Public Health Dent 2011; 71: S52–63. [PubMed] [Google Scholar]
- 98. Gearing RE, El-Bassel N, Ghesquiere Aet al. Major ingredients of fidelity: a review and scientific guide to improving quality of intervention research implementation. Clin Psychol Rev 2011; 31: 79–88. [DOI] [PubMed] [Google Scholar]
- 99. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999; 89: 1322–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Sallis A, Bondaronek P, Sanders JGet al. Prescriber commitment posters to increase prudent antibiotic prescribing in English general practice: a cluster randomized controlled trial. Antibiotics 2020; 9: 490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Hoffmann TC, Glasziou PP, Boutron Iet al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014; 348: g1687. [DOI] [PubMed] [Google Scholar]
- 102. Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr 1974; 2: 328–35. [DOI] [PubMed] [Google Scholar]
- 103. McNulty CAM, Lecky DM, Farrell Det al. Overview of e-Bug: an antibiotic and hygiene educational resource for schools. J Antimicrob Chemother 2011; 66 Suppl 5: v3–12. [DOI] [PubMed] [Google Scholar]
- 104. Miller NE, Dollard J. Social Learning and Imitation. Yale University Press, 1941. [Google Scholar]
- 105. Bandura A. Social Learning Theory. General Learning Press, 1977. [Google Scholar]
- 106. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991; 50: 179–211. [Google Scholar]
- 107. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977; 84: 191–215. [DOI] [PubMed] [Google Scholar]
- 108. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall, 1986. [Google Scholar]
- 109. McDermott L, Yardley L, Little Pet al. Developing a computer delivered, theory based intervention for guideline implementation in general practice. BMC Fam Pract 2010; 11: 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Gulliford MC, Prevost AT, Charlton Jet al. Effectiveness and safety of electronically delivered prescribing feedback and decision support on antibiotic use for respiratory illness in primary care: REDUCE cluster randomised trial. BMJ 2019; 364: l236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Michie S, van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci 2011; 6: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Hayes CV, Eley CV, Ashiru-Oredope Det al. Development and pilot evaluation of an educational programme on infection prevention and antibiotics with English and Scottish youth groups, informed by COM-B. J Infect Prev 2021; 22: 212–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Borek AJ, Wanat M, Roberts Net al. Exploring the Implementation of Interventions to Reduce Antibiotic Use (ENACT) Study: Report. Public Health England; 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1014323/ENACT_AMS_Report.pdf.
- 114. Reddy V, Baman NS, Whitener Cet al. Drug resistant infections with methicillin-resistant Staphylococcus aureus, Clostridium difficile, and vancomycin resistant Enterococcus are associated with a higher prevalence of penicillin allergy. J Allergy Clin Immunol 2013; 131: AB170. [Google Scholar]
- 115. West RM, Smith CJ, Pavitt SHet al. ‘Warning: allergic to penicillin’: association between penicillin allergy status in 2.3 million NHS general practice electronic health records, antibiotic prescribing and health outcomes. J Antimicrob Chemother 2019; 74: 2075–82. [DOI] [PubMed] [Google Scholar]
- 116. Wanat M, Anthierens S, Butler CCet al. Patient and prescriber views of penicillin allergy testing and subsequent antibiotic use: a rapid review. Antibiotics 2018; 7: 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Little P, Stuart B, Francis Net al. Antibiotic prescribing for acute respiratory tract infections 12 months after communication and CRP training: a randomized trial. Ann Fam Med 2019; 17: 125–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Tonkin-Crine S, Anthierens S, Francis NAet al. Exploring patients’ views of primary care consultations with contrasting interventions for acute cough: a six-country European qualitative study. NPJ Prim Care Respir Med 2014; 24: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]