ABSTRACT
Background
There is no consensus on how to define “junk food.” In 2016, Chile implemented the most comprehensive set of obesity-preventive regulations in the world, including criteria to define unhealthy foods.
Objectives
The objective of this study was to examine the amount of energy, sodium, sugar, and saturated fat consumed by US adults defined as junk food using the Chilean criteria.
Methods
We used 2 nationally representative surveys of food intake in 10,001 US adults: NHANES 2015–2016 and NHANES 2017–2018. The main outcome measures were the contributions of energy, total sugars, saturated fat, and sodium deriving from junk food sources. Mean intake and proportion of energy, sugar, saturated fat, and sodium for junk food overall and each food category were calculated.
Results
Overall, 47% of energy, 75% of total sugar, 46% of sodium, and 48% of saturated fat consumed by US adults derived from junk food sources. Sugar-sweetened beverages (SSBs) were responsible for more than 40% of total sugar intake deriving from junk foods. Non-Hispanic black adults had the highest mean energy, total sugar, and sodium intake deriving from junk foods, with non-Hispanic white adults having the highest saturated fat intake. Non-Hispanic black adults had the highest intake of total sugar deriving from junk food sources of SSBs (26.7 g/d), with SSBs representing >40% of total sugar intake deriving from junk food sources for all race/ethnic groups.
Conclusions
Foods that meet the Chilean criteria for junk food provide approximately half or more daily energy and food components to limit in the diet of US adults, with important differences observed between race/ethnic groups. Policy efforts to reduce junk food intake, particularly the intake of SSBs, must be expanded to improve the cardiometabolic health equitably in the United States.
Keywords: junk food, dietary intake, sugar-sweetened beverages, NHANES, food policy
Introduction
Large disparities have been documented in nutrition-related noncommunicable diseases (NCDs) such as obesity, diabetes, and hypertension across racial/ethnic and socioeconomic groups in the United States (1–3). Overweight and obesity as well as nutrition-related NCDs remain the top health problems and causes of death and disability in the country (4). Hispanic and non-Hispanic black adults have significantly higher prevalence of obesity and nutrition-related NCDs (1, 5), and recent research has demonstrated that overweight and obese patients are at a higher risk of mortality from COVID-19 infection (6, 7).
Diet quality can heavily influence health outcomes, particularly nutrition-related NCDs (8–11). A recent landmark crossover randomized controlled trial showed that subjects had an average weight loss of ∼1 kg when switching from an ultraprocessed to minimally processed diet (12), which supports prior research linking ultraprocessed foods with lower dietary quality; increased weight gain; and risks of obesity, diabetes, hypertension, and all-cause mortality (13–18).
The US food supply is dominated by packaged food and beverages, contributing ∼75% of daily calorie intake in the US population (19). In the United States, studies have shown that a large proportion of daily energy derives from foods commonly viewed as “junk foods,” such as salty snacks, desserts, and sweets, and that disparities in diet quality exist in demographic subgroups (20–22). For example, a recent US study found that >70% of daily calorie intake and >90% of total sugar intake in children and adolescents derived from junk foods, with differences seen between demographic subgroups (23).
In the academic literature, there is no consistent definition for junk foods, and most studies assume that only products within categories such as salty snacks, desserts, and sweets are considered junk foods. Consequently, products containing excessive amounts of saturated fat, energy, added sugar, or salt but that are not in these junk food categories (e.g., sandwiches with less healthy ingredients, juice drinks, and bakery products) have been excluded from such a definition. In recognizing these gaps, studies have started using alternative methods such as degree of food processing to define unhealthy foods and operationalize these definitions in available data. In 2016, Chile implemented the Chilean law of food labeling and advertising, including the most comprehensive set of obesity-preventive regulations in the world (24, 25). The law applies marketing and sales restrictions to foods and beverages with high levels of energy density and added saturated fats, sodium, and sugar ingredients. Thresholds to be considered high in these nutrients and food components have become more restrictive according to 3 phases of implementation of the law. Since Chile's groundbreaking regulations, similar approaches have been adopted in Israel (26), Peru (27), Mexico (28), and Brazil (29).
In this study, we aimed to determine the proportion of energy, nutrients, and food components consumed by US adults by race/ethnic, age, and income groups that would be considered junk food using the Chilean regulation criteria. In particular, we examined heterogeneity in the prevalence of junk food consumption for key subgroups.
Methods
Survey population
Data were obtained from 2 nationally representative surveys of food intake in 10,001 US adults (defined as age >18 y): NHANES 2015–2016 and NHANES 2017–2018 (NHANES 15–18) (Table 1). NHANES is based on a multistage, stratified area probability sample of noninstitutionalized US households. Detailed information about each survey and its sampling design has been published previously (30). By utilizing secondary deidentified NHANES data, we were exempted from institutional review board concerns.
TABLE 1.
Sociodemographic characteristics for US adults aged >18 y, NHANES 2015–2018
| Characteristic | 2015–2018 |
|---|---|
| Participants, n | 10,001 |
| % men | 48.5 |
| Age group, % | |
| 19–29 y | 17.7 |
| 30–59 y | 47.4 |
| ≥60 y | 35.0 |
| BMI,1 % | |
| Underweight | 1.5 |
| Normal weight | 25.2 |
| Overweight | 31.9 |
| Obese | 41.4 |
| Race/ethnicity, % | |
| Mexican American | 15.5 |
| Other Hispanic | 11.3 |
| Non-Hispanic white | 34.7 |
| Non-Hispanic black | 22.4 |
| Other race | 16.1 |
| Household income, % | |
| <185% federal poverty level | 45.5 |
| 185–350% federal poverty level | 25.4 |
| >350% federal poverty level | 29.1 |
| Head of household education, % | |
| Less than high school diploma | 20.9 |
| High school diploma | 23.7 |
| More than high school diploma | 55.4 |
BMI categories were defined as underweight (<18.5), normal weight (18.5 to <25.0), overweight (25.0 to <30.0), and obese (≥30.0).
Junk food definition
Typically, food groups are used rather than added nutrients and food components to identify junk foods. The Chilean nutrient profile model is one approach that uses nutrients and food components to define junk foods, but there are many other definitions in the literature (31, 32), most of which identify food groups of concern. Although the Chilean regulation was implemented in 2016, the nutrient thresholds were set to become increasingly stringent over a series of 3 implementation dates. The phase 2 criteria were utilized for this analysis on the basis that these criteria are most widely used in the literature and were adopted by Israel and Peru as their first of 2 phases (26, 33, 34). The nutritional content of each food consumed in NHANES was compared to the phase 2 thresholds from the Chilean regulation for energy, saturated fat, total sugars, and sodium per 100 g (25) (Supplemental Table 1). Products that exceeded the nutrient thresholds were considered junk foods in this analysis. The Chilean regulation also includes an ingredient criterion, with products containing added sugars, saturated fat, or sodium ingredients as well as exceeding the nutrient and/or food component criteria considered junk foods (Supplemental Figure 1). Steele et al. (22, 35, 36), along with collaborators at the CDC, provided data for this study identifying products from NHANES 2015–2018 that have added sugar, saturated fat, and/or sodium ingredients.
Dietary data
The first day's data (a single, interviewer-administered 24-h dietary recall) collected from each individual was used (as recommended by the USDA). Appropriate weights and adjustments were used for the sample design (37).
Food groupings
All foods reported in NHANES surveys were assigned to 1 of 10 food categories (Supplemental Table 2). Food categories were those used in a previous similar analysis examining changes in junk food consumption in US children and adolescents (23). In brief, to focus on food categories of interest, analysis was limited to categories with >50% of products exceeding the Chilean phase 2 nutrient criteria. All remaining food categories were grouped together.
Statistical analysis
Junk food intake was examined using 3 age groups (19–29 y, 30–59 y, and ≥60 y), 5 race/ethnic groups (Mexican American, other Hispanic, non-Hispanic white, non-Hispanic black, and other race), 2 genders (male and female), and 3 income groups (<185%, 185–350%, and >350% of the federal poverty level). Mean intake and proportion of energy, sugars, saturated fat, and sodium deriving from junk food overall and within each food category were calculated. Analyses were done overall and by demographic subgroup. The number of junk food items per day was calculated by dividing the number of items consumed that were classified as junk food items using the Chilean criteria by the total number of food items consumed.
Survey methods were used within Stata to account for the clustering that is inherent in the NHANES sampling methodology. Linear regression models were also used to examine differences within subgroups, with adjustment for gender, age, race/ethnicity, income, head of household educational level, BMI, and activity level. A P value <0.01 was considered significant. Stata version 16 (StataCorp) was used for all analyses.
Results
Overall intake of junk foods
Overall in 2015–2018, US adults consumed an average of 4.8 junk food items daily. Mean intake of energy deriving from junk food sources was 1043 kcal/d (47.1% of total energy intake). Total sugar intake deriving from junk foods was 54.4 g/d (75.0% of total sugar intake), saturated fat was 14.4 g/d (48.0% of total saturated fat intake), and sodium was 1669 mg/d (45.5% of total sodium intake) (Table 2). Overall, sugar-sweetened beverages (SSBs) were the highest contributor to total sugar intake from junk foods in 2015–2018 (22.2 g/d; 41% of total sugar deriving from junk foods; Table 3). Sandwiches, burgers, and pizzas were the highest food group contributor to energy [221 kcal/d (21%); Table 4], saturated fat [4.4 g/d (31%); Supplemental Table 3], and sodium intake [465 mg/d (28%); Supplemental Table 4] deriving from junk foods. Collectively, confectionery, desserts, and SSBs contributed ∼75% of total sugar intake deriving from junk foods (Table 3). Bread, ready-to-eat cereals, and processed meat, poultry, and fish contributed 25% of sodium intake collectively (Supplemental Table 4).
TABLE 2.
Nutrient intake in US adults deriving from junk food sources overall and by demographic subgroup, NHANES 2015–20181
| Per capita energy intake from junk food | Per capita total sugar intake from junk food | Per capita sodium intake from junk food | Per capita saturated fat intake from junk food | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | No. junk food items/d | Mean intake (kcal/d) | % total energy intake | Mean intake (g/d) | % total sugar intake | Mean intake (mg/d) | % total sodium intake | Mean intake (g/d) | % total saturated fat intake | |
| All adults, ≥19 y | 10,001 | 4.8 | 1043 | 47.1 | 54.4 | 75.0 | 1669 | 45.5 | 14.4 | 48.0 |
| Age group | ||||||||||
| 19–29 y | 1771 | 4.7 | 1122 | 50.1 | 56.2 | 79.5 | 1887 | 48.6 | 15.8 | 51.3 |
| 30–59 y2 | 4735 | 4.9 | 1082 | 47.0 | 58.5 | 74.3 | 1721 | 45.8 | 14.7 | 47.7 |
| ≥60 y | 3495 | 4.9 | 9113 | 45.13 | 45.23 | 73.23 | 14083 | 42.43 | 12.93 | 46.03 |
| Sex | ||||||||||
| Male2 | 4850 | 5.0 | 1218 | 48.3 | 62.6 | 76.5 | 2004 | 47.1 | 17.0 | 49.6 |
| Female | 5151 | 4.7 | 8804 | 46.04 | 46.84 | 73.74 | 13564 | 43.94 | 12.04 | 46.44 |
| Household income | ||||||||||
| <185% federal poverty level2 | 4062 | 4.7 | 1039 | 47.2 | 57.9 | 75.0 | 1651 | 45.7 | 14.0 | 47.6 |
| 185–350% federal poverty level | 2273 | 4.9 | 1066 | 48.2 | 58.9 | 75.7 | 1692 | 46.2 | 14.7 | 48.8 |
| >350% federal poverty level | 2598 | 4.9 | 1033 | 46.4 | 49.24 | 74.64 | 1668 | 44.9 | 14.6 | 47.7 |
| Race/ethnicity | ||||||||||
| Mexican American | 1554 | 4.6 | 9823 | 43.63 | 48.93 | 77.7 | 1576 | 40.5 | 13.4 | 45.0 |
| Non-Hispanic white2 | 3467 | 5.0 | 1081 | 48.8 | 56.6 | 75.0 | 1734 | 47.7 | 15.1 | 49.0 |
| Non-Hispanic black | 2238 | 5.1 | 1132 | 52.1 | 62.3 | 80.4 | 1755 | 49.3 | 15.0 | 53.4 |
1Results have been weighted to be nationally representative.
2Reference group.
3Different to all groups (P < 0.01).
4Different to reference group (P < 0.01).
TABLE 3.
Mean total sugar intake (g/d) and proportion of total sugar intake deriving from junk foods consumed by US adults in NHANES 2015–2018
| All adults (n = 10,001) | Male (n = 4850) | Female (n = 5151) | Mexican American (n = 1554) | Non-Hispanic white (n = 3467) | Non-Hispanic black (n = 2238) | Age 19–29 y (n = 1771) | Age 30–59 y (n = 4735) | Age ≥60 y (n = 3495) | <185% federal poverty level (n = 4062) | 185–350% federal poverty level (n = 2273) | >350% federal poverty level (n = 2598) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Breads | 0.6 (1.1%) | 0.7 (1.1%) | 0.6 (1.3%) | 0.7 (1.4%) | 0.6 (1.1%) | 0.9 (1.4%) | 0.5 (0.9%) | 0.6 (1.0%) | 0.9 (2.0%)1 | 0.6 (1.0%) | 0.6 (1.0%) | 0.7 (1.4%) |
| Cheese and cheese products | 0.0 (0.0%) | 0.0 (0.0%) | 0.0 (0.0%) | 0.0 (0.0%) | 0.0 (0.0%) | 0.0 (0.0%) | 0.0 (0.0%) | 0.0 (0.0%) | 0.0 (0.0%) | 0.0 (0.0%) | 0.0 (0.0%) | 0.0 (0.0%) |
| Confectionery | 4.8 (8.8%) | 5.0 (8.0%) | 4.7 (10.0%) | 4.7 (9.6%) | 5.3 (9.4%) | 5.0 (8.0%) | 4.8 (8.5%) | 5.1 (8.7%) | 4.4 (9.7%) | 4.3 (7.4%) | 4.4 (7.5%) | 5.5 (11.2%) |
| Dairy with added sugar | 0.5 (0.9%) | 0.5 (0.8%) | 0.6 (1.3%) | 0.5 (1.0%) | 0.6 (1.1%) | 0.1 (0.2%)2 | 0.6 (1.1%) | 0.6 (1.0%) | 0.5 (1.1%) | 0.7 (1.2%) | 0.5 (0.8%) | 0.4 (0.8%) |
| Desserts | 12.6 (23.2%) | 13.5 (21.6%) | 11.8 (25.2%)3 | 12.4 (25.4%) | 12.8 (22.6%) | 12.9 (20.7%) | 9.0 (16.0%)4 | 12.1 (20.7%) | 16.2 (35.8%)1 | 12.1 (20.9%) | 14.5 (24.6%) | 11.9 (24.2%) |
| Processed meat, poultry, and fish | 0.3 (0.6%) | 0.4 (0.6%) | 0.2 (0.4%)3 | 0.2 (0.4%) | 0.3 (0.5%) | 0.2 (0.3%) | 0.2 (0.4%) | 0.3 (0.5%) | 0.4 (0.9%) | 0.3 (0.5%) | 0.3 (0.5%) | 0.2 (0.4%) |
| Ready-to-eat cereals | 2.0 (3.7%) | 2.3 (3.7%) | 1.8 (3.8%) | 1.3 (2.7%)5 | 2.3 (4.1%) | 2.2 (3.5%) | 2.2 (3.9%) | 2.1 (3.6%) | 1.7 (3.8%) | 2.3 (4.0%) | 2.4 (4.1%) | 1.6 (3.3%) |
| Salty snacks | 0.2 (0.4%) | 0.3 (0.5%) | 0.2 (0.4%) | 0.2 (0.4%) | 0.3 (0.5%) | 0.2 (0.3%) | 0.3 (0.5%) | 0.2 (0.3%) | 0.2 (0.4%) | 0.2 (0.3%) | 0.2 (0.3%) | 0.3 (0.6%) |
| Sandwiches, burgers, and pizzas | 1.4 (2.6%) | 1.9 (3.0%) | 1.0 (2.1%)3 | 1.0 (2.0%)2 | 1.6 (2.8%) | 1.5 (2.4%) | 1.8 (3.2%) | 1.5 (2.6%) | 1.2 (2.7%) | 1.5 (2.6%) | 1.5 (2.5%) | 1.3 (2.6%) |
| Sugar-sweetened beverages | 22.2 (40.8%) | 27.6 (44.1%) | 17.1 (36.5%)3 | 20.7 (42.3%) | 22.9 (40.5%) | 26.7 (42.9%) | 26.0 (46.3%) | 25.7 (43.9%) | 12.6 (27.9%)1 | 27.7 (47.8%) | 25.0 (42.4%) | 16.4 (33.3%)6 |
| All other foods | 9.4 (17.3%) | 10.3 (16.5%) | 8.6 (18.4%) | 6.7 (13.7%)5 | 9.8 (17.3%) | 12.4 (19.9%) | 10.8 (19.2%) | 10.1 (17.3%) | 7.1 (15.7%)1 | 8.1 (14.0%) | 9.0 (15.3%) | 10.7 (21.7%)6 |
| All food | 54.4 | 62.6 | 46.8 | 48.9 | 56.6 | 62.3 | 56.2 | 58.5 | 45.2 | 57.9 | 58.9 | 49.2 |
Different to age 19–29 y and age 30–59 y (P < 0.01).
Different to non-Hispanic white (P < 0.01).
Different to males (P < 0.01).
Different to age 30–59 y and age ≥60 y (P < 0.01).
Different to non-Hispanic white and non-Hispanic black (P < 0.01).
Different to <185% federal poverty level and 185–350% federal poverty level (P < 0.01).
TABLE 4.
Mean energy intake (kcal/d) and proportion of energy intake deriving from junk foods consumed by US adults in NHANES 2015–2018
| All adults (n = 10,001) | Male (n = 4850) | Female (n = 5151) | Mexican American (n = 1554) | Non-Hispanic white (n = 3467) | Non-Hispanic black (n = 2238) | Age 19–29 y (n = 1771) | Age 30–59 y (n = 4735) | Age ≥60 y (n = 3495) | <185% federal poverty level (n = 4062) | 185–350% federal poverty level (n = 2273) | >350% federal poverty level (n = 2598) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Breads | 62 (5.9%) | 68 (5.6%) | 56 (6.4%)1 | 70 (7.1%) | 58 (5.4%) | 70 (6.2%) | 49 (4.4%) | 61 (5.6%) | 74 (8.1%) | 60 (5.8%) | 57 (5.3%) | 66 (6.4%) |
| Cheese and cheese products | 8 (0.8%) | 9 (0.7%) | 6 (0.7%) | 5 (0.5%)2 | 9 (0.8%) | 7 (0.6%) | 8 (0.7%) | 9 (0.8%) | 6 (0.7%) | 8 (0.8%) | 9 (0.8%) | 7 (0.7%) |
| Confectionery | 52 (5.0%) | 54 (4.4%) | 50 (5.7%) | 49 (5.0%) | 56 (5.2%) | 48 (4.2%) | 53 (4.7%) | 55 (5.1%) | 45 (4.9%) | 46 (4.4%) | 46 (4.3%) | 60 (5.8%) |
| Dairy with added sugar | 7 (0.7%) | 7 (0.6%) | 7 (0.8%) | 6 (0.6%) | 9 (0.8%) | 1 (0.1%)2 | 8 (0.7%) | 7 (0.6%) | 6 (0.7%) | 9 (0.9%) | 7 (0.7%) | 6 (0.6%) |
| Desserts | 175 (16.8%) | 188 (15.4%) | 164 (18.6%)1 | 186 (18.9%) | 177 (16.4%) | 175 (15.5%) | 124 (11.1%)3 | 169 (15.6%) | 225 (24.7%)4 | 171 (16.5%) | 195 (18.3%) | 167 (16.2%) |
| Processed meat, poultry, and fish | 47 (4.5%) | 60 (4.9%) | 35 (4.0%)1 | 28 (2.9%)2 | 55 (5.1%) | 42 (3.7%) | 47 (4.2%) | 47 (4.3%) | 48 (5.3%) | 44 (4.2%) | 55 (5.2%) | 46 (4.5%) |
| Ready-to-eat cereals | 38 (3.6%) | 43 (3.5%) | 33 (3.8%) | 26 (2.6%)2 | 43 (4.0%) | 32 (2.8%)2 | 34 (3.0%) | 38 (3.5%) | 40 (4.4%) | 41 (3.9%) | 41 (3.8%) | 33 (3.2%) |
| Salty snacks | 86 (8.2%) | 96 (7.9%) | 77 (8.8%)1 | 71 (7.2%)5 | 91 (8.4%) | 93 (8.2%) | 96 (8.6%) | 90 (8.3%) | 70 (7.7%)4 | 79 (7.6%) | 96 (9.0%) | 85 (8.2%) |
| Sandwiches, burgers, and pizzas | 221 (21.2%) | 288 (23.6%) | 158 (18.0%)1 | 239 (24.3%) | 234 (21.6%) | 200 (17.7%) | 297 (26.5%)3 | 228 (21.1%) | 152 (16.7%)4 | 225 (21.7%) | 226 (21.2%) | 215 (20.8%) |
| Sugar-sweetened beverages | 98 (9.4%) | 122 (10.0%) | 76 (8.6%)1 | 94 (9.6%) | 101 (9.3%) | 119 (10.5%) | 113 (10.1%) | 114 (10.5%) | 56 (6.1%)4 | 119 (11.5%) | 108 (10.1%) | 77 (7.5%)6 |
| All other foods | 249 (23.9%) | 283 (23.2%) | 217 (24.7%)1 | 203 (20.7%) | 247 (22.8%) | 343 (30.3%)7 | 292 (26.0%) | 263 (24.3%) | 190 (20.9%)4 | 237 (22.8%) | 227 (21.3%) | 271 (26.2%)6 |
| All food | 1043 | 1218 | 880 | 982 | 1081 | 1132 | 1122 | 1082 | 911 | 1039 | 1066 | 1033 |
Different to males (P < 0.01).
Different to non-Hispanic white (P < 0.01).
Different to age 30–59 y and age ≥60 y (P < 0.01).
Different to age 19–29 y and age 30–59 y (P < 0.01).
Different to non-Hispanic white and non-Hispanic black (P < 0.01).
Different to <185% federal poverty level and >350% federal poverty level (P < 0.01).
Different to Mexican American and non-Hispanic white (P < 0.01).
Findings by demographic subgroups
Race/ethnic groups
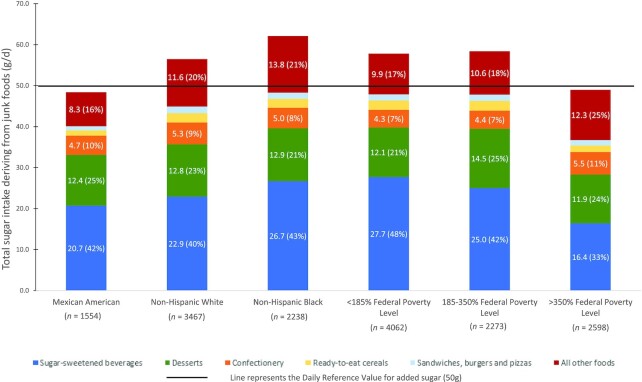
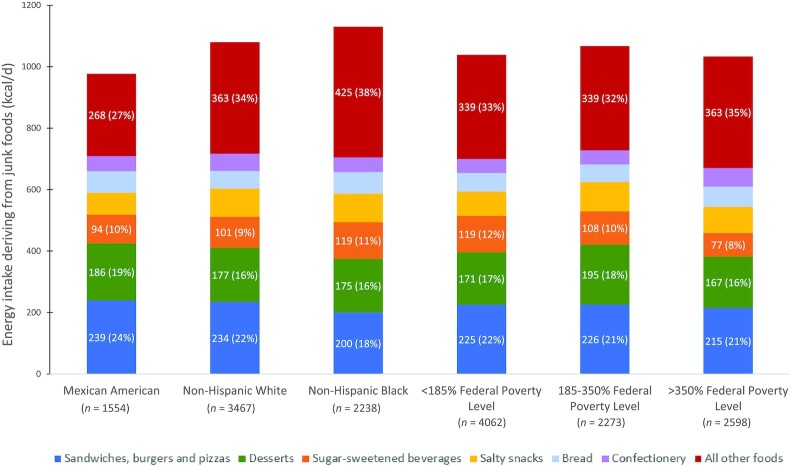
Non-Hispanic black adults had the highest mean energy, total sugar, and sodium intake deriving from junk foods, with non-Hispanic white adults reporting the highest saturated fat intake (Table 2). Mexican American adults had significantly lower energy intake (982 kcal/d) and total sugar intake (48.9 g/d) deriving from junk foods compared with non-Hispanic whites (1081 kcal/d and 56.6 g/d, respectively) and non-Hispanic blacks (1132 kcal/d and 62.3 g/d, respectively) (P < 0.01; Table 2). Differences between race/ethnic groups were driven by a few key food categories, namely SSB and salty snacks. Mexican Americans had significantly lower calorie and sodium intake deriving from junk food sources of salty snacks [71 kcal/d (7%) and 93 mg/d (6%)] compared with non-Hispanic whites [91 kcal/d (8%) and 129 mg/d (7%)] and non-Hispanic blacks [93 kcal/d (8%) and 122 mg/d (7%)] (P < 0.01 for all). Non-Hispanic black adults had the highest intake of total sugar deriving from junk food sources of SSBs [26.7 g/d (43%)], with SSBs representing >40% of total sugar intake deriving from junk food sources for all race/ethnic groups, while desserts were the other larger food group with 23% of overall sugar daily intake (Figure 1). Significant race/ethnic differences were observed in other sources of energy from junk food sources. Mexican Americans had a lower intake of total energy from desserts and salty snacks, whereas non-Hispanic black adults had a lower amount of energy deriving from desserts and a higher amount from sandwiches, burgers, and pizzas compared with non-Hispanic white adults (Figure 2).
FIGURE 1.
Mean total sugar intake deriving from junk foods consumed by 10,001 US adults in NHANES 2015–2018.
FIGURE 2.
Mean total energy intake deriving from junk foods consumed by 10,001 US adults in NHANES 2015–2018.
Age groups
The ≥60 y age group had significantly lower intake of energy, total sugar, saturated fat, and sodium deriving from junk foods compared with the 19–29 y and 30–59 y age groups (P < 0.01 for all; Table 2). Total sugar intake from SSBs was significantly lower in the ≥60 y age group compared with other age groups (P < 0.01; Table 3). Desserts was the only category for which the ≥60 y age group had a higher intake of energy [225 kcal/d (25%)], total sugar [16.2 g/d (36%)], and saturated fat [3.8 g/d (30%)] deriving from junk food sources compared with the other age groups.
Gender
Overall, females compared with males had significantly lower intakes of energy (880 compared with 1218 kcal/d), total sugar (46.8 compared with 62.6 g/d), saturated fat (12.0 compared with 17.0 g/d), and sodium (1356 compared with 2004 mg/d) (P < 0.01 for all; Table 2). The same trends were observed when examining results by food category.
Income groups
Few differences were observed between household income groups. No significant differences in intake of energy, saturated fat, or sodium deriving from junk food sources were observed (Table 2). The highest income group (>350% of the federal poverty level) had significantly lower intake of sugar deriving from junk food sources (49.2 g/d) compared with the lowest income group (<185% federal poverty level; 57.9 g/d) and the middle-income group (185–350% of the federal poverty level; 58.9 g/d) (P < 0.01 for all). This trend was driven solely by SSBs, with the highest income group having significantly lower intake of total sugar deriving from SSBs [16.4 g/d (33%)] compared with the lowest income group [27.7g/d (48%)] and the middle-income group [25.0 g/d (42%)] (P < 0.01 for all; Figure 1).
Discussion
We found that in 2015–2018, 47% of energy, 75% of total sugar, 46% of sodium, and 48% of saturated fat consumed by US adults derived from junk foods. SSBs were responsible for >40% of total sugar intake deriving from junk foods. Our results mirror those observed in a recent study in US children and adolescents which found that 56% of energy, 82% of total sugar intake, 55% of sodium, and 43% of saturated fat derived from junk food sources (23). These findings are also in line with other US studies showing a large proportion of energy intake derives from foods generally considered unhealthy (38–41). These results are important given that the US Dietary Guidelines identify sodium, saturated fat, and added sugars as food components of public health concern, as does WHO (42, 43).
Differences were observed between race/ethnic groups, with non-Hispanic black adults consuming the highest amount of energy, total sugar, and sodium from junk food sources compared with Mexican Americans and non-Hispanic whites. Non-Hispanic blacks also had the highest intake of energy and sugar deriving from SSBs in the current study. This is in line with existing US research showing that non-Hispanic black adults generally purchase and consume a higher amount of sugar compared with other race/ethnic groups in the United States (44, 45) and that non-Hispanic blacks have been shown to have a higher consumption of SSBs compared with other race/ethnic groups (38, 46). Few differences were observed between different age and income groups. One other notable difference observed was that the highest income group (>350% of the federal poverty level) had significantly lower intake of total sugar from junk foods compared with the other income groups, driven solely by the highest income group having significantly lower intake of SSBs.
An important finding in this study was that it is not only foods commonly considered junk food (e.g., confectionery, snack foods, and SSBs) that were not considered healthy using the Chilean criteria but also foods from other categories, such as sandwiches, processed meats, ready-to-eat cereals, and bread products that contributed to junk food intake (particularly sodium intake) in this sample of US adults. Much of the research to date has focused primarily on food and beverage categories generally considered to be junk food (e.g., confectionery, savory snacks, and grain-based desserts) (47), which given the results from the current study may not provide the full picture of where US consumers are deriving added sugars, sodium, and saturated fats. The Chilean regulation was implemented in 2016. Early research on the regulation showed that there was a decrease in the amount of sugars and sodium in a number of packaged food and beverage categories after its initial implementation (34). There is likely a need for a similar approach to be taken in the United States given the results from the current study showing not only that a large proportion of energy and nutrient intake derives from junk food sources but also that many food sources that are not commonly considered junk food may not be addressed under existing policies. Currently, there are many state-based policies attempting to reduce the purchase of, and hence consumption of, less healthy ultraprocessed products, especially SSBs (48). Despite evidence in the literature of consumption decreasing in recent years, intake of SSBs remains high and clear disparities exist between subgroups. The need exists for comprehensive national-level policies that help reduce amounts of added sugars, sodium, and saturated fat in packaged food and beverage products but that do not increase disparities between race/ethnic groups in the United States and that do not focus solely on food categories commonly thought of as junk foods. Such solutions may include a consistent easy-to-understand front-of-pack label (due to potential language difficulties in some subpopulations), advertisements/marketing regulations including warnings (along with enforcement), policies regarding what is allowed to be sold or to be available in schools, and even regulations regarding whether such products can be sold at checkouts of stores or take up more than a certain amount of shelf space (49–51).
This analysis had some limitations. Because our study was cross-sectional in nature, we cannot make robust conclusions about causality in the observed associations. Reported dietary data have limitations in misreporting, and they can vary by demographic variables such as gender and race/ethnicity (52). In addition, unhealthy foods, such as SSBs (53), are particularly prone to underreporting, so it is possible that some of the associations observed here might have been underestimated due to systematic measurement error associated with this. Another important point is that nutrient-based criteria such as those used in the Chilean model do not take into account all aspects of a food or beverage product (e.g., protein or dietary fiber), and the Chilean model is one of many approaches to support consumers in the identification of what would be considered junk food. The Chilean model also does not address alcohol, and given that the latest data suggest almost three-fourths of all US adults reported consuming alcohol in the past year (54), it would be important for future policymakers to also include guidance and policies in relation to alcohol consumption.
In conclusion, US adults are consuming a large proportion of energy and sugar from junk food sources. In 2015–2018, 47% of total energy, 48% of saturated fat intake, 75% of sugar intake, and 46% of sodium intake among US adults derived from junk food. Future research should examine how other factors influence junk food intake, such as social and family aspects, exposure to unhealthy food marketing, and physical activity levels. This study found differences between sociodemographic subgroups, highlighting the need for policies or programs that both help reduce junk food consumption for the US population overall and also consider race/ethnic disparities in the population. Continued efforts to reduce intake of SSBs should be encouraged to improve the cardiometabolic health of the US population.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Karen Ritter for assistance with the data management. We also thank Euridice Martinez, School of Public Health, University of Sao Paulo, whose software allowed us to calculate all the Chilean ingredient criteria for 2015–2018. The authors’ responsibilities were as follows—EKD, BP, and SWN: designed and conducted the research; EKD: analyzed data and drafted the manuscript; and all authors: had joint primary responsibility for final content and read and approved the final manuscript.
Notes
This work was primarily funded by Arnold Ventures with additional support from the Carolina Population Center (NIH grant P2C HD050924 ).
Author disclosures: The authors report no conflicts of interest.
Supplemental Tables 1–4 and Supplemental Figure 1 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/jn/.
Contributor Information
Elizabeth K Dunford, Food Policy Division, The George Institute for Global Health, University of New South Wales, Sydney, Australia; Department of Nutrition, Gillings Global School of Public Health, The University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Barry Popkin, Department of Nutrition, Gillings Global School of Public Health, The University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; Carolina Population Center, The University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Shu Wen Ng, Department of Nutrition, Gillings Global School of Public Health, The University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; Carolina Population Center, The University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
References
- 1. Hales CM, Fryar CD, Carroll MD, Freedman DS, Aoki Y, Ogden CL. Differences in obesity prevalence by demographic characteristics and urbanization level among adults in the United States, 2013–2016. JAMA. 2018;319:2419–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315:2284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. [DOI] [PubMed] [Google Scholar]
- 4. GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet North Am Ed. 2020;396:1204–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mpofu JJ, de Moura L, Farr SL, Malta DC, Iser BM, Ivata Bernal RT, Robbins CL, Lobelo F. Associations between noncommunicable disease risk factors, race, education, and health insurance status among women of reproductive age in Brazil—2011. Prev Med Rep. 2016;3:333–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hussain A, Mahawar K, Xia Z, Yang W, El-Hasani S. Obesity and mortality of COVID-19: meta-analysis. Obes Res Clin Pract. 2020;14:295–300. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 7. Popkin BM, Du S, Green WD, Beck MA, Algaith T, Herbst CH, Alsukait RF, Alluhidan M, Alazemi N, Shekar M. Individuals with obesity and COVID-19: a global perspective on the epidemiology and biological relationships. Obes Rev. 2020;21(11):e13128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lane MM, Davis JA, Beattie S, Gómez-Donoso C, Loughman A, O'Neil A, Jacka F, Berk M, Page R, Marx W et al. Ultraprocessed food and chronic noncommunicable diseases: a systematic review and meta-analysis of 43 observational studies. Obes Rev. 2020;22(3):e13146. [DOI] [PubMed] [Google Scholar]
- 9. Nardocci M, Polsky JY, Moubarac JC. Consumption of ultra-processed foods is associated with obesity, diabetes and hypertension in Canadian adults. Can J Public Health. 2020;112(3):421–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yang Q, Zhang Z, Steele EM, Moore LV, Jackson SL. Ultra-processed foods and excess heart age among U.S. adults. Am J Prev Med. 2020;59(5):e197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. World Cancer Research Fund . Diet, nutrition, physical activity and cancer: a global perspective. [Internet]. [cited 10 January, 2021]. Available from: https://www.wcrf.org/dietandcancer. [Google Scholar]
- 12. Hall KD. Ultra-processed diets cause excess calorie intake and weight gain: a one-month inpatient randomized controlled trial of ad libitum food intake. Cell Metab. 2019;30(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim H, Hu EA, Rebholz CM. Ultra-processed food intake and mortality in the USA: results from the Third National Health and Nutrition Examination Survey (NHANES III, 1988–1994). Public Health Nutr. 2019;22:1777–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Askari M, Heshmati J, Shahinfar H, Tripathi N, Daneshzad E. Ultra-processed food and the risk of overweight and obesity: a systematic review and meta-analysis of observational studies. Int J Obes. 2020;44:2080–91. [DOI] [PubMed] [Google Scholar]
- 15. Rauber F, Chang K, Vamos EP, da Costa Louzada ML, Monteiro CA, Millett C, Levy RB. Ultra-processed food consumption and risk of obesity: a prospective cohort study of UK Biobank. Eur J Nutr. 2020;60(4):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bonaccio M, Di Castelnuovo A, Costanzo S, De Curtis A, Persichillo M, Sofi F, Cerletti C, Donati MB, de Gaetano G, Iacoviello L. Ultra-processed food consumption is associated with increased risk of all-cause and cardiovascular mortality in the Moli-sani Study. Am J Clin Nutr. 2021;113(2):446–55. [DOI] [PubMed] [Google Scholar]
- 17. Pagliai G, Dinu M, Madarena MP, Bonaccio M, Iacoviello L, Sofi F. Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. Br J Nutr. 2021;125(3):308–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lawrence MA, Baker PI. Ultra-processed food and adverse health outcomes. BMJ. 2019;365:l2289. [DOI] [PubMed] [Google Scholar]
- 19. Poti JM, Mendez MA, Ng SW, Popkin BM. Is the degree of food processing and convenience linked with the nutritional quality of foods purchased by US households?. Am J Clin Nutr. 2015;101(6):1251–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kirkpatrick SI, Dodd KW, Reedy J, Krebs-Smith SM. Income and race/ethnicity are associated with adherence to food-based dietary guidance among US adults and children. J Acad Nutr Diet. 2012;112(5):624–35..e626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hiza HA, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet. 2013;113(2):297–306. [DOI] [PubMed] [Google Scholar]
- 22. Steele EM, Baraldi LG, da Costa Louzada ML, Moubarac J-C, Mozaffarian D, Monteiro CA. Ultra-processed foods and added sugars in the US diet: evidence from a nationally representative cross-sectional study. BMJ Open. 2016;6(3):e009892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dunford EK, Popkin BM, Ng SW. Recent trends in junk food intake in U.S. children and adolescents, 2003–2016. Am J Prev Med. 2020;59(1):49–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rodriguez Osiac L, Pizarro Quevedo T. [Law of food labelling and advertising: Chile innovating in public nutrition once again]. Rev Chil Pediatr. 2018;89(5):579–81. [DOI] [PubMed] [Google Scholar]
- 25. Corvalán C, Reyes M, Garmendia ML, Uauy R. Structural responses to the obesity and non-communicable diseases epidemic: update on the Chilean law of food labelling and advertising. Obes Rev. 2019;20(3):367–74. [DOI] [PubMed] [Google Scholar]
- 26. Endevelt R, Grotto I, Sheffer R, Goldsmith I, Golan M, Mendlovic J, Bar-Siman-Tov M. Policy and practice: regulatory measures to improve the built nutrition environment for prevention of obesity and related morbidity in Israel. Public Health Panorama. 2017;3(4):567–75. [Google Scholar]
- 27. Plataforma Digital Unica del Estado Peruano . Conoce las advertencias publicitarias (octógonos). [Internet]. 2019; [cited 17 May, 2021]. Available from: https://www.gob.pe/1066-ministerio-de-salud-conoce-las-advertencias-publicitarias-octogonos. [Google Scholar]
- 28. White M, Barquera S. Mexico adopts food warning labels, why now?. Health Systems Reform. 2020;6(1):e1752063. [DOI] [PubMed] [Google Scholar]
- 29. USDA, Foreign Agricultural Service. Brazil approves new regulations for food labeling. [Internet]. 2019; [cited 15 March, 2021]. Available from: https://www.fas.usda.gov/data/brazil-brazil-approves-new-regulations-food-labeling. [Google Scholar]
- 30. Perloff BP, Rizek RL, Haytowitz DB, Reid PR. Dietary intake methodology: II. USDA's Nutrient Data Base for Nationwide Dietary Intake Surveys. J Nutr. 1990;120(suppl 11):1530–4. [DOI] [PubMed] [Google Scholar]
- 31. Milani GP, Silano M, Pietrobelli A, Agostoni C. Junk food concept: seconds out. Int J Obes. 2017;41(5):669–71. [DOI] [PubMed] [Google Scholar]
- 32. Chapman G, Maclean H. “Junk food” and “healthy food”: meanings of food in adolescent women's culture. J Nutr Educ. 1993;25(3):108–13. [Google Scholar]
- 33. World Cancer Research Fund International . NOURISHING database. [Internet]. [cited 10 January, 2021]. Available from: https://www.wcrf.org/int/policy/nourishing-database. [Google Scholar]
- 34. Reyes M, Smith Taillie L, Popkin B, Kanter R, Vandevijvere S, Corvalán C. Changes in the amount of nutrient of packaged foods and beverages after the initial implementation of the Chilean law of food labelling and advertising: a nonexperimental prospective study. PLoS Med. 2020;17(7):e1003220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Steele EM, Popkin BM, Swinburn B, Monteiro CA. The share of ultra-processed foods and the overall nutritional quality of diets in the US: evidence from a nationally representative cross-sectional study. Popul Health Metr. 2017;15(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Steele EM, Khandpur N, Sun Q, Monteiro CA. The impact of acculturation to the US environment on the dietary share of ultra-processed foods among US adults. Prev Med. 2020;141:106261. [DOI] [PubMed] [Google Scholar]
- 37. National Center for Health Statistics, CDC . Analytic and reporting guidelines: The National Health and Nutrition Examination Survey. [Internet]. 2005; [cited 17 May, 2021]. Available from: https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx. [Google Scholar]
- 38. Park S, Xu F, Town M, Blanck HM. Prevalence of sugar-sweetened beverage intake among adults—23 states and the district of Columbia, 2013. MMWR Morbid Mortal Wkly Rep. 2016;65(7):169–74. [DOI] [PubMed] [Google Scholar]
- 39. An R, Maurer G. Consumption of sugar-sweetened beverages and discretionary foods among US adults by purchase location. Eur J Clin Nutr. 2016;70(12):1396–400. [DOI] [PubMed] [Google Scholar]
- 40. An R. Beverage consumption in relation to discretionary food intake and diet quality among US adults, 2003 to 2012. J Acad Nutr Diet. 2016;116(1):28–37. [DOI] [PubMed] [Google Scholar]
- 41. Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary intake among us adults, 1999–2012. JAMA. 2016;315(23):2542–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. USDA and US Department of Health and Human Services . Dietary guidelines for Americans 2020–2025. [Internet]. [cited 17 May, 2021]. Available from: https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf. [Google Scholar]
- 43. WHO . Population nutrient intake goals for preventing diet-related chronic diseases. [Internet]. [cited 20 May, 2021]. Available from: https://www.who.int/nutrition/topics/5_population_nutrient/en. [Google Scholar]
- 44. Poti JM, Mendez MA, Ng SW, Popkin BM. Highly processed and ready-to-eat packaged food and beverage purchases differ by race/ethnicity among US households. J Nutr. 2016;146(9):1722–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lundeen EA, Park S, Pan L, Blanck HM. Daily intake of sugar-sweetened beverages among US adults in 9 states, by state and sociodemographic and behavioral characteristics, 2016. Prev Chronic Dis. 2018;15:E154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dunford EK, Popkin BM. Disparities in snacking trends in US adults over a 35 year period from 1977 to 2012. Nutrients. 2017;9(8):809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Liu J, Lee Y, Micha R, Li Y, Mozaffarian D. Trends in junk food consumption among US children and adults, 2001–2018. Am J Clin Nutr. 2021. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Huang Y, Pomeranz J, Wilde P, Capewell S, Gaziano T, O'Flaherty M, Kersh R, Whitsel L, Mozaffarian D, Micha R. Adoption and design of emerging dietary policies to improve cardiometabolic health in the US. Curr Atheroscler Rep. 2018;20(5):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Payne C, Niculescu M. Can healthy checkout end-caps improve targeted fruit and vegetable purchases? Evidence from grocery and SNAP participant purchases. Food Policy. 2018;79:318–23. [Google Scholar]
- 50. Ejlerskov KT, Sharp SJ, Stead M, Adamson AJ, White M, Adams J. Supermarket policies on less-healthy food at checkouts: natural experimental evaluation using interrupted time series analyses of purchases. PLoS Med. 2018;15(12):e1002712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Huitink M, Poelman MP, Seidell JC, Pleus M, Hofkamp T, Kuin C, Dijkstra SC. Can unhealthy food purchases at checkout counters be discouraged by introducing healthier snacks? A real-life experiment in supermarkets in deprived urban areas in the Netherlands. BMC Public Health. 2020;20:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Livingstone MB, Robson PJ, Wallace JM. Issues in dietary intake assessment of children and adolescents. Br J Nutr. 2004;92(suppl 2):S213–22. [DOI] [PubMed] [Google Scholar]
- 53. Börnhorst C, Huybrechts I, Ahrens W, Eiben G, Michels N, Pala V, Molnár D, Russo P, Barba G, Bel-Serrat S et al. Prevalence and determinants of misreporting among European children in proxy-reported 24 h dietary recalls. Br J Nutr. 2013;109(7):1257–65. [DOI] [PubMed] [Google Scholar]
- 54. Substance Abuse and Mental Health Services Administration,Center for Behavioral Health Statistics and Quality . 2019 national survey on drug use and health. [Internet]. 2020; [cited 26 May, 2021]. Available from: https://www.samhsa.gov/data/sites/default/files/reports/rpt29394/NSDUHDetailedTabs2019/NSDUHDetTabsSect2pe2019.htm#tab2-18b. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.