Lay Summary
Latinas at high risk for hereditary breast and ovarian cancer (HBOC) have low rates of genetic counseling and testing. Latinas may not have ready access to services like genetic counseling and testing, which need special solutions. One solution can involve training community health workers to bridge the gap between Latinas and genetic specialists. We developed an online and in person training program (ÁRBOLES Familiares or Family Trees) for English-Spanish bilingual community health workers that teaches them how to help Latinas get access to genetic services. We tested this program with a small group of community health workers. After the program, their HBOC knowledge, genetic literacy, and confidence to help Latinas get access to genetic services had improved. Trainees also made suggestions to improve the program, which will be used to help future trainees expand their knowledge and skills to work with Latinas at risk of HBOC.
Keywords: Cancer, Genetics, Inherited, Promotoras, Education
Abstract
Cancer health disparities remain a significant problem in the USA, compounded by lack of access to care, language barriers and systemic biases in health care. These disparities are particularly evident in areas such as genetics/genomics. For example, Latinas at high risk for hereditary breast and ovarian cancer (HBOC) have extremely low rates of genetic counseling/testing. Long-standing barriers and inequities in access to services such as genetic counseling and testing require innovative solutions. One solution can involve training community outreach and education professionals (CORE-Ps) to bridge the gap between underserved communities and genetic specialists. We sought to develop and pilot test a training program for English-Spanish bilingual CORE-Ps to reduce disparities in access to and uptake of genetic services among Latino populations. Guided by Adult Learning Theory and with input from multiple stakeholders, we developed ÁRBOLES Familiares (Family Trees), an in-person and online training program for bilingual CORE-Ps to facilitate identification, referral, and navigation of Latinas to genetic counseling/testing. We conducted a pilot test of 24 CORE-Ps recruited from across the United States and assessed knowledge, genetic literacy, and self-efficacy at baseline and follow-up. At follow-up, participants in the pilot with complete baseline and follow-up data (N = 15) demonstrated significant improvements in HBOC knowledge, genetic literacy, self-efficacy and reports of fewer barriers to identify/navigate Latinas (ps < .05). Qualitative assessment identified ways to improve the training curriculum. Pilot results suggest ÁRBOLES is a promising approach for training CORE-Ps to identify and refer high-risk Latinas to genetic services. Next steps involve further refinement of ÁRBOLES, development of an online toolkit, and adaptation for virtual delivery.
Implications.
Practice: Training bilingual community outreach and education professionals is a promising strategy for improving their abilities to identify, refer, and navigate Latinas at risk of hereditary breast and ovarian cancer to genetics services.
Policy: Effective training programs for promotoras should consider delivery method (online, in person, combination), interactive group content, and practical, applicable content and projects that enhance abilities to work with local Latina women and appropriate genetic services.
Research: Future research will be aimed at assessing long term outcomes of subsequent cohorts of promotoras with refinements made from pilot feedback, and will focus on developing an online toolkit for wide community use.
Introduction
Hereditary breast and ovarian cancers in Latinas
Among Latinas and Hispanic women (hereafter referred to as “Latinas”), breast cancer is the most common cancer [1] and despite lower incidence among Latinas compared to Non-Hispanic White women, the mortality rate among Latinas is higher [2]. The health disparities in breast cancer mortality by race and ethnicity are further evidenced by Latinas’ younger age at diagnosis and worse prognostic features, including more triple negative disease, compared to Non-Hispanic Whites [2–4]. In the overall population of women diagnosed with breast cancer, approximately 10–15% of cases are attributed to inherited pathogenic variants [5]. The most common cause of inherited breast and/or ovarian cancer is pathogenic variants in the BRCA1 and BRCA2 (BRCA1/2) genes, leading to hereditary breast and ovarian cancer (HBOC) [6]. Carrying a BRCA1/2 pathogenic variant results in a lifetime risk of breast cancer of up to 60%–70% and lifetime ovarian cancer risk of up to 40% [7]. The general population prevalence of pathogenic variants in the BRCA1/2 genes in Latinas is not well understood, especially compared with non-Hispanic white women [8, 9]. Prevalence estimates are limited to clinic-based samples and those with a personal or family history of HBOC [9, 10], restricting the ability to determine true population prevalence of pathogenic variants in the BRCA1/2 genes for Latinas.
Gaps in and need for genetic services for Latinas at risk of HBOC
According to National Health Interview Survey data, Latinas consistently had the lowest level of awareness about genetic testing for inherited cancer risk, compared to all other U.S. racial/ethnic groups [11, 12]. Furthermore, Latinas may face barriers to genetic testing such as less referral and access to services, lack of health insurance, socioeconomic and language barriers, and competing time demands [13, 14]. Disparities in the use of genetic counseling and testing may result in less awareness of the higher lifetime cancer risks of HBOC and thus an increased risk of mortality [15].
Despite these disparities and barriers, Latinas’ interest in genetic services has been demonstrated to be greater or equal to that of women of other ethnicities [13, 16]. Studies conducted in safety-net hospital settings (e.g., hospitals that provide care to uninsured patients or those covered by Medicaid) with predominately Latino patients suggest that when offered genetic counseling, most women (88%) [16] kept their appointments and nearly all (96%) had BRCA1/2 testing when recommended [17]. Other research suggests that once referred, Latinas are just as likely to undergo testing as other ethnic groups [18].
Need for identification and referral-level competency training of CORE-Ps (community outreach and education professionals)
In 2001, the CDC outlined basic genomic competencies for all members of the public health workforce including abilities to: (a) demonstrate basic knowledge of the role that genomics plays in the development of disease; (b) identify the limits of his/her genomic expertise; and (c) make appropriate referrals to those with more genomic expertise [19]. Core competencies in genetics for non-physicians identified through a modified Delphi process include a similar demonstration of knowledge, abilities, and attitudes [20]. While multiple programs offer targeted cancer genetics education and training for clinical health care professionals such as physicians and nurses [21, 22], these trainings are generally focused on clinical genetics service delivery competencies, rather than those at the level of identification and referral.
Consistent evidence suggests that key knowledge and awareness barriers affect risk appropriate utilization of genetic services among Latinas at increased risk for HBOC [11, 12, 23, 24], but when education and access are provided in the community, Latinas are likely to participate in such services. Community outreach and education professionals (hereafter “CORE-Ps”), such as community health educators, promotoras, lay health advisors, and patient navigators, have been effective in improving cancer screening behaviors in underserved populations [25, 26]. However, limited research has evaluated the use of CORE-P education and support to increase Latinas’ awareness and utilization of cancer genetics services.
An innovative program to train CORE-Ps in identification and referral-level genetic competencies
Innovative educational models are urgently needed to address existing genomic disparities given the rapidly shifting demographics of the U.S. population (to about 30% Latino by 2060) [12–16]. As such, we developed a training program for CORE-Ps, entitled the Family Trees Program [Programa de ÁRBOLES Familiares: Assessing Risk of Breast Cancer through Outreach to Latinas with Education and Support]. Our target audience includes bilingual CORE-Ps employed by community-based organizations, clinics, and hospitals that provide direct education, outreach, or services to Latinos. The goal of the training program is to address the unmet need of developing a trained network of CORE-Ps with referral-level competence to identify those who may be at increased risk for hereditary cancer and facilitate risk-appropriate use of genetic services among Latinas at risk for HBOC. In this paper, we describe the specific elements of the program including content, recruitment, plans for evaluation and results of pilot testing to assess changes from pre- to immediate post-training knowledge, genetic literacy, and self-efficacy to identify, educate, and refer at-risk Latinas. We also include initial outcomes from the 12-month post-training assessment. We include pilot trainee feedback on refinements that can improve future training processes and content.
METHOD
Training program structure
We developed the ÁRBOLES Familiares curriculum based on Adult Learning Theory [27], which allows CORE-Ps to share personal experiences and see a direct application of a learned concept through the following principles: (a) learning should capitalize on the participants’ experience; (b) learning should be adapted to the limitations of the participant; (c) learners should be challenged to move to advanced stages of personal development; and (d) learners should have a choice in organizing the learning program. Table 1 describes the application of Adult Learning Theory to the ÁRBOLES training program. We combine principles of Adult Learning Theory with popular education techniques prominent in Latin America and community health education [28, 29].
Table 1.
Adult learning theory application
| Adult learning principle | ARBOLES training example |
|---|---|
| Learning should capitalize on the participants’ experience | - Eligibility of participants is based on their experience with and knowledge of the Latino community - Approaches and modalities used during in-person training are based on strategies that participants often use to teach their communities (e.g., activities, games, and role play) |
| Learning should be adapted to the limitations of the participant | - Curriculum is designed to use a step-wise didactic and skill building approach for those with minimal knowledge and skills related to identification and referral of individuals at increased risk of HBOC - Training offered in both English and Spanish to provide participants an opportunity to learn in their native/preferred language, but also gain the skills and practice to interface with non-bilingual genetic professionals - Training program places minimal financial and travel burden on participants by covering all expenses for in-person training - Online component of training allows participants to complete coursework on their own time |
| Adults should be challenged to move to advanced stages of personal development | - Training designed to impart additional knowledge and skills to help expand the educational content and support they provide to the community - Curriculum facilitates participants’ personal and professional growth by providing feedback and suggestions for improvement through use of practice presentations and other skill building activities |
| Adults should have choice in organizing the learning program | - Course content and activities are routinely adapted to meet participants’ needs by having an External Advisory Panel with representation of those delivering health education to Latinos, seeking regular feedback and evaluation, and assessing a pilot cohort. |
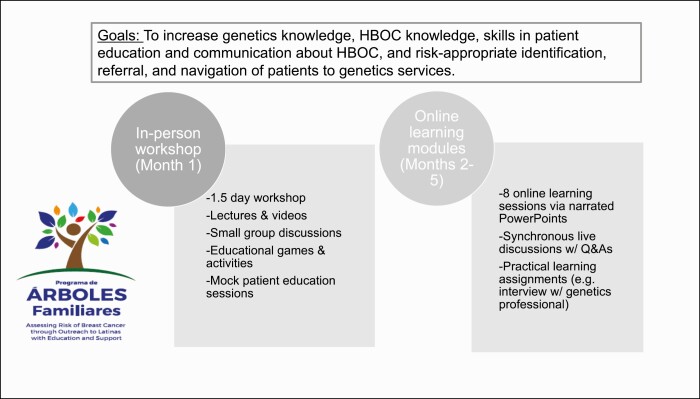
The ÁRBOLES Familiares training program uses multi-modal educational activities and approaches to increase CORE-Ps’ genetics knowledge, foundational knowledge regarding HBOC, skills in communication/patient education regarding HBOC, and risk-appropriate identification, referral, and navigation of patients to genetic services (Fig. 1). We designed the pilot program to include a 1.5-day in-person workshop followed by eight online learning sessions initiated within a month of the in-person workshop and completed once every two weeks over the course of four months. The in-person workshop includes lectures, videos, small group discussions, educational games/activities, mock patient education sessions, and individual and group learning activities (Fig. 1; Table 2). The pilot online learning sessions include a mix of online, didactic sessions, and synchronous (live) discussions. The online learning sessions include content modules via narrated PowerPoints addressing: identification of community member at-risk of HBOC, communication about genetic cancer risk through group and individual community education sessions, identification of local genetics professionals and services, access of resources to facilitate referral, and provision of referral and navigation of genetics services. Synchronous (live) discussions feature a 60-min session with a brief presentation followed by time for questions and answers, practical applications of materials and learning assignments, and case presentations. Practical learning assignments include interviews with genetics professionals and development of plans to: (a) identify community, regional, or national resources related to HBOC and (b) identify community members who are at-risk for HBOC. See Table 3 for a detailed description of the pilot online learning sessions. The training program covers all expenses, travel, and accommodations for the in-person workshop.
Fig 1.
ÁRBOLES Familiares pilot training program components.
Table 2.
Pilot 1.5-day in-person workshop activities and descriptions
| Pilot activity/topic | Description |
|---|---|
| Day 1 | |
| Welcome & making connections | • Trainees introduce themselves and then mingle & discuss questions on nametags (e.g., “What do you think are the biggest challenges to discussing cancer risk with Latinas?”) |
| Introduction & why is family history important? | • Sharing of a personal story by a Latina breast cancer survivor who tested positive with BRCA1 • Scripted role play between a Latina breast cancer survivor and her physician eliciting family history and introducing idea that patient’s cancer could be due to BRCA1/2 pathogenic variants • Group discussion with questions and answers followed by Spanish-language video about family history, genes, and HBOC |
| Genetics 101 | • Lecture on genetics designed to convey basic genetic concepts and appropriate for trainees with limited prior knowledge of genetics • Small group activity: create models of the double helix using candy to help reinforce concepts from genetics lecture |
| Hereditary breast & ovarian cancer | • Trainees instructed in how to draw family histories using pedigree symbols and then draw their own family tree; discussion of how certain traits and/or health conditions are passed between generations • Discuss case example of patient in the introductory role play to highlight importance of family history of breast and ovarian cancer • Trainees work in pairs to practice taking a fictitious family history. Pairs share experience with small group and discuss whether/why the family histories they provided are/are not suggestive of HBOC • Introduce/reinforce different concepts important in referral-level competencies related to HBOC including genetic counseling, genetic testing, initiating genetic testing in a proband, defining “affected” and “unaffected,” risk factors related to young age of cancer onset or triple negative breast cancer, and how other genes beyond BRCA1/2 may also be involved in HBOC. Concepts conveyed through case presentations of family pedigrees and provision of glossary with terms in English and Spanish |
| Introduction to HBOC risk management | • Introduce risk management approaches with presentation describing surveillance and prophylactic surgery options • Questions and answers with physician and genetic counselors who care for high risk Latina patients |
| Debrief day 1 experiences | • Breakout groups (of 6–7 trainees) to discuss and then report back to larger group to debrief from day 1 and elicit trainees’ professional experiences related to community education, risk assessment, referrals to specialists, and navigation with health services • Large group discussion of trainees’ prior experiences of working with patients with HBOC within their communities and organizations |
| Day 2 | |
| Greeting & ice breaker activity | • Place small signs on trainees’ backs that have words or definitions on them (e.g., affected/diagnosed with breast or ovarian cancer; proband/first person in the family to be tested.) Participants find the match of their word/definition by asking questions and providing hints to one another |
| Genetic Counseling and Testing | • Presentation about what genetic counseling is, the goals and typical components. Introduce concepts of panel testing vs. single-site testing • Lay-level presentation about current evidence related to population frequency of BRCA1/2 variants and other known deleterious variants related to breast cancer risk in Latinas |
| Risk assessment skills | • -Role play to demonstrate how promotora might initiate and conduct risk assessments • Overview, discussion and practice using risk assessment tools available in Spanish and English |
| Ethical, legal, & social issues | • Discuss ethical, legal, and social issues using case examples relevant to Latinas including: communication about family history and potential stigma of cancer or passing along deleterious pathogenic variants; sharing of genetic test results with family members living in woman’s country of origin; costs of testing and resources for women without insurance or high deductibles • Introduction to the Genetic Information & Nondiscrimination Act • Discussion of issues relevant to confidentiality |
| Making connections with- and navigation to- genetic resources | • Review different types of genetic services (genetic counseling, genetic education, genetic testing, panel testing) • Group discussion/Q&A about what happens during a genetic counseling appointment via panel of genetic counselors • Demonstration of navigating national online genetics resources |
| Communication about HBOC | • Group discussion of how trainees might apply the information and skills discussed during training • Discussion of training assignment for implementation of information and skills |
| Workshop evaluation & wrap-up | • Complete evaluation about satisfaction with content and format • Orient trainees to upcoming online learning sessions |
Table 3.
Pilot online learning session descriptions
| Session | Modality | Description/topic |
|---|---|---|
| 1 | Narrated PowerPoint |
CORE-P from an organization with an established approach to identifying those at increased risk for HBOC share experiences with implementation of procedures, facilitators and barriers to implementation, and approaches to follow-up among patients identified as increased risk |
| 2 | Synchronous | Discussion of trainees’ attempt(s) to apply approaches with individual patients or implement within their organizations |
| 3 | Narrated PowerPoint |
Participants will watch videos modeling community education and one-on-one patient education about HBOC |
| 4 | Synchronous | Role plays between CORE-Ps with one posing as educator and one as patient. |
| 5 | Narrated PowerPoint |
Focus on identification of local genetics services. A genetic counselor reviews the role of a genetic counselor and how to find genetic counselors |
| 6 | Synchronous | Discussion following an assignment to interview a genetics professional. |
| 7 | Narrated PowerPoint |
Focus on providing referrals and navigation related to genetics services |
| 8 | Synchronous | Discussion of trainee plans to implement their training in the context of their community education setting |
Participant eligibility and recruitment
Eligibility requirements include: (a) bilingual (English and Spanish); (b) CORE-P employed by or volunteer for an organization, clinic, institution, hospital, or agency providing direct education, outreach or health services to Latinas, and (c) have an electronic device with internet access. We recruit CORE-Ps from: community-based cancer resource organizations, national Latino cancer networks and summits, presentations at national, regional, and local professional or community meetings, trainee referral, and relationships with a diverse group of community and national partners. Recruitment strategies included email outreach, distribution through relevant listservs, hosting of tables at health fairs and relevant conferences, and word of mouth.
Interested trainees submit an online application including information about educational and professional background, workplace setting and demographics of the patient and community populations they serve, current educational and referral practices for HBOC, two personal and professional goals for the training, and assurances they can attend a 1.5-day in-person workshop, complete eight online learning sessions over four months, and complete 6- and 12-month follow-up surveys. We evaluate applications for gender, self-reported bilingual ability, geographic location, type of organization, and stated interest in the program. The highest ranked applicants are accepted into the program. In 2018, for the pilot cohort, we conducted purposeful recruitment to identify trainees from established organizations working with the Latino community; we received 30 inquiries of interest and invited 25 trainees for the pilot cohort. For subsequent cohorts, we follow recruitment as described above to recruit and enroll cohorts of 28–35 participants each or seven additional cohorts over the course of the 5-year funding period.
Assessment schedule and measures
Trainees complete an online pre-training baseline assessment survey prior to the workshop and then three post-training surveys: one immediately following completion of the in-person workshop, and then two assessments conducted after completion of the online training (“post-training,” conducted within 1–2 months of completion of the online training modules and approximately 4–5 months after the in-person workshop) and again at 12 months after completion of the online training component. We also assess programmatic milestones including number of applicants and number of completed trainees. Trainees are also asked to answer open-ended questions to obtain feedback related to their experiences during the training. Assessments can be completed in English or in Spanish. We used validated Spanish versions of the measures noted below, or, if not available, used a forward and backward translation approach by bilingual measures of the team. These measures were then reviewed by other team members for wording and accuracy. In the overall ÁRBOLES Familiares Training Program, we are assessing awareness and attitudes about genetic risk/genetic counseling, HBOC knowledge, genetic literacy, genetics knowledge, self-efficacy, and communication and behavioral outcomes. In the pilot study, we have results for a subset of these measures, indicated below.
ÁRBOLES Familiares measures: pilot study
Demographics include trainee age, race, ethnicity, gender, education, income, country of origin, years in US, professional role, and acculturation (Short Acculturation Scale, [30] including language use, media preferences, social relations).
HBOC (hereditary breast and ovarian cancer) knowledge is assessed with a 10-item true/false Spanish version of the National Human Genome Research Knowledge Scale [31] assessed pre- and post-training. Correct items are summed for a total possible score of 10. Cronbach’s alpha (alpha = 0.72) indicated the scale reached acceptable reliability.
Genetic health literacy is assessed using a validated Spanish-language genetic literacy tool, the Short REAL-G-Sp [32]. The adapted version is utilized to capture functional genetic literacy, assessed through key word familiarity and comprehension measures (rating the familiarity of words and completing fill-in-the-blank sentences with those words). The 8-item Familiarity section is scored as an average of the participants’ familiarity ratings (range 1–7) with the terms (e.g., genética (genetic), susceptibilidad (susceptibility)). Internal consistency reliability for the Familiarity section was alpha = 0.92. The 8-item Comprehension portion is scored as the sum of correct answers in response to the fill-in-the-blank sentences (range 0–8).
Genetics knowledge is assessed with an 8-item multiple choice questionnaire [32] on general genetic knowledge, including disease susceptibility, pathogenic variants, hereditability, etc. Correct items are summed for a total possible score of 8. Cronbach’s alpha indicated the scale had excellent reliability (alpha = 0.94).
Self-efficacy for identifying at-risk women, providing education, referral, and navigation services is assessed with items adapted from scales of self-efficacy for genetic counseling in non-English speaking patients [33]. This 7-item measure assesses self-efficacy on a 10-point Likert scale from “not at all confident” to “extremely confident.” The Likert responses for each of the seven items are summed for a possible total score of 70. Cronbach’s alpha indicated the scale had excellent reliability (alpha = 0.95).
Process measures. We also assessed process outcomes using quantitative and open-ended survey methods at the immediate post-training assessment. Participants answered questions with Likert scale response options ranging from “strongly agree” to “strongly disagree.” We assessed clarity of training objectives, whether information was understandable, trainees’ perceptions of both the personal value and professional value of the training program, and whether trainees understood the role of genetics in breast and ovarian cancer. In addition, we asked participants to rank order the specific learning sessions in the training in terms of their preferred sessions and then asked open-ended questions about the aspects of the training sessions that were most helpful, least helpful, and how they intended to use the information within their community.
Attitudes toward genetic counseling/testing are assessed with a 17-item validated measure used with Latinas related to counseling/testing use in at-risk minority women [34]. Ten items assessed perceived benefits of genetic testing for cancer (internal consistency reliability Cronbach’s alpha = 0.92), nine items assessed perceived barriers to genetic testing for cancer risk (e.g., implications of positive test such as harm caused to family members, potential stigma of BRCA carrier status, etc.; internal consistency reliability Cronbach’s alpha = 0.78) and five items assessed concerns related to genetic counseling and testing (internal consistency reliability Cronbach’s alpha = 0.64).
Communication practices and skills related to genetics education and referral, adapted from our prior work on other training programs, assess communication with community members about HBOC and whether trainees identified, referred or navigated individuals at risk for HBOC to genetic services [35, 36].
Additional measures in overall ÁRBOLES Familiares training program evaluation
Awareness of cancer genetic risk and genetic counseling is assessed with the 4-item scale used in our prior work with Latinas [34]. This measure asks participants how much they have heard or read about genetically inherited diseases and genetic testing on a 4-point scale from almost nothing (1) to a lot (4).
Pilot method
We pilot tested the in-person and online training components of the ÁRBOLES program with one group of CORE-Ps. For the quantitative data assessed at baseline (“pre-training”) and immediately following the complete training, which included the in-person training workshop and the online modules (“post-training”), we conducted paired-samples t-tests to evaluate change in HBOC knowledge, genetic health literacy, genetics knowledge, and self-efficacy from pre-training to post-training among trainees with complete data at both timepoints (N = 15). For the qualitative data, responses to open-ended items assessed at post-training after completion of the online modules and at 12 months post-training; these comments were reviewed for commonalities across participants and representative quotes are presented below.
Pilot trainees
We accepted 25 trainees into the pilot training group, recruited primarily via email, distribution of flyers and outreach through advocacy groups and direct outreach to established community organizations working with Latino communities. For the pilot training, 24 out of 25 accepted CORE-Ps participated, including 23 women and one man (one accepted trainee was unable to attend). Ninety-six percent were Hispanic or Latino and were from either Washington, DC or four U.S. states: California, Texas, Florida, and New York. In terms of language, 41.7% of participants reported speaking and reading both English and Spanish equally, 33.3% more English than Spanish, 16.7% more Spanish than English, 4.2% preferred only Spanish, and 4.2% “other.” In terms of education, 4% of participants had a doctoral degree, 40% had a master’s, 28% had a bachelor’s, 16% completed some college, and 12% completed high school. In terms of professional role, 33.3% reported working or volunteering at a community-based organization, 33.3% at a cancer center, 20.8% at a university hospital, and 12.5% “other.” Finally, 85% of pilot participants completed requirements for all online modules and assignments; 15% dropped out during the online training portion, completing only some modules/assignments.
RESULTS
Pilot quantitative outcomes
Trainees reported a small increase in genetics knowledge from pre-training (M = 7.07, SD = 0.80) to post-training, although this was not a statistically significant increase (M = 7.20, SD = 0.68; t(14) = −0.81, p = .43). With a total possible score of 8, the pre-training scores indicate a possible ceiling effect, with little change in the genetics knowledge of participants at post-training. However, there was a statistically significant increase in HBOC knowledge from pre-training (M = 5.27, SD = 2.28) to post-training (M = 8.07, SD = 1.33; t(14) = −3.70, p = .002); knowledge remained high at 12 months (M = 7.11, SD = 1.16).
Genetic health literacy increased from pre-training to post-training for the Familiarity component (pre: M = 4.88, SD = 1.07; post: M = 6.5, SD = 0.435; t(14) = 5.99, p < .0001). Comprehension did not demonstrate a statistically significant change (pre: M = 7.07, SD = 0.80; post: M = 7.2, SD = 0.67; t(14)= −0.807, p = .433).
Self-efficacy for identifying at-risk women and providing education, referral, and navigation services demonstrated a statistically significant increase from pre-training (M = 44.60, SD = 16.94) to post-training (M = 63.27, SD = 6.35; t(14) = −4.76, p < .0001).
For attitudes toward genetic counseling/testing, trainees reports of perceived barriers to genetic counseling significantly decreased from pre- to post-training (t(14) = 2.2, p = 0.04), although perceived benefits of genetic counseling and concerns related to genetic counseling did not change from pre-training to post-training (p = 0.32).
For communication practices and skills related to genetics education and referral assessed at 12 months, 100% of trainees indicated they conduct at least one educational session with women about hereditary breast and ovarian cancer at least once a month or more; 20% indicated they conducted these sessions at least once a week or more and 80% indicated they conducted these sessions at least once a month or more. At 12 months, 60% of trainees indicated that they had helped a Latino community member access genetic services and of these, 35% indicate that they help a patient or community member access genetic services at least once a month.
Pilot process outcomes
At post-training, nearly all pilot participants (more than 95%) agreed or strongly agreed the training had: clear objectives, understandable information, and both personal and professional value. Most (66.7%) strongly agreed they felt more comfortable with genetics terms following the training. The majority (75%) reported that they understood the role of genetics in breast and ovarian cancer risk.
Immediately following the in-person workshop, participants described the most helpful aspects of the training via open-ended responses to a survey. Some discussed specific lectures and activities that were meaningful, with a handful of participants indicating that the “Genetics 101” (40%; 8/20 open-ended responses) and “Why is family history important?” (20%; 4/20) lectures were the most helpful. One said: “Genetics 101 explained very well all the terms we need to be comfortable with.” The associated “Genetics 101” activities were also frequently cited as helpful: “The [double helix] candy model in Genetics 101 provided valuable learning strategies.” One participant stated the most helpful aspects were “the discussions with the genetic counselors, and [learning] the differences between acquired and inherited risk.” One highlighted how the online sessions complemented the in-person training: “As far as the online/phone portion, it gave me the chance to read the material more thoroughly.” Another participant described a helpful assignment from the online training: “The assignment of interviewing a genetic counselor deepened this understanding in reviewing real cases.”
Participants also relayed aspects of the training that were least helpful and made suggestions for improvement. Two participants made suggestions for improvement pertaining to the practical applicability of session content for their particular community or organization, such as “…maybe the least helpful was the risk assessment referral because it might be different depending on which state or area the family is living.” Similarly, another said: “…it would be beneficial to have an example of how to implement something like this in an organization, how should we go about using this information.” Quite a few (50%; 9/18 open-ended responses) stated that it would be helpful to extend the length of the in-person training. One said: “[Add] more time or extra day. Too much information to sink in, especially the first day.” Several of those responses also suggested allowing more time for interaction with other participants: “More time to do hands on activities. The topics were excellent, but more time to do networking with the others.” Some comments (22.2%; 4/18) suggested that slides should be provided to participants. For example, “provide all presentation slides in binders for note taking.” At the post-training assessment we solicited suggestions about the online training components and assignments. One said: “Too many online sessions. Live [online] sessions were not doable for me.” Another mentioned the utility of the online training: “Some of the online training felt very repetitive and quite honestly was not helpful. The discussions on the sidebar—during the live training—from people we’d met, was very helpful.” One felt that approaching a genetic counselor for an interview was challenging: “It was difficult to do cold calling/contacting a genetic counselor not involved/aware of this training. I think it would have been helpful to receive a list of genetic counselors who have been informed about this training and who have agreed to be available for interviews.” Based on this feedback, we identified opportunities for refining the training program, described below.
DISCUSSION AND CONCLUSION
Discussion
ÁRBOLES is a new training program providing education about genetics and hereditary breast and ovarian cancer to bilingual (Spanish–English) community outreach and education professionals. Face-to-face learning followed by online sessions are meant to engage participants across the training. Results suggested that the pilot training workshop was successful in terms of educational content, participant engagement, and improvements in knowledge, genetic literacy and self-efficacy.
Guided by Adult Learning Theory and elements from popular education, ÁRBOLES seeks to increase knowledge and self-efficacy pertaining to hereditary breast and ovarian cancer and genetic risk in order to increase identification, referral, and navigation of high-risk Latina patients to genetic counseling and testing. We continue to iteratively refine the content and format of the training program for CORE-Ps in order to meet trainees needs and ultimately improve the effectiveness of trainees’ skills out in the community.
Program refinements following the pilot
Based on pilot participant feedback, we have revised and adapted ÁRBOLES Familiares. Adaptations include changes to both the format and content of the training. In terms of format refinements, we have extended the in-person workshop from 1.5 to 2.5 days to spread out the cognitive load of complex genetics information and allow trainees more time for networking, discussion, and small group activities. We have also refined our recruitment information and application process to clarify to potential applicants the time commitment and expected amount and timing of assignments so that they can make informed decisions about the fit of the program with their time and interests. Format changes also include a reduction in the number of homework assignments. For example, in substitution for the assignment to interview a genetic counselor, trainees can instead ask questions to two genetic counselors during one of the synchronous sessions. We have replaced the original assignments with one final “ÁRBOLES Action Project” that serve as a personalized guide for working with each participant’s community members and include resources and referral sources tailored to their at-risk Latina community members. CORE-P trainees now submit action projects at the conclusion of the online component. We have added resources and examples of projects to help support trainees in the development of their action projects, along with additional time to discuss and view the examples. We also now provide trainees with printed slides from the in-person didactic sessions so that they are better able to follow content as it is presented or take notes during lectures. In terms of the format for the online component, we have reduced the number of online didactic sessions after the in-person workshop from eight modules to six modules to decrease repetitiveness and focus on the most important content. There are now four main didactic sessions and two synchronous sessions. We have also adapted synchronous (live session) scheduling to account for participants’ differing time zones. We will move two of the online sessions to be completed before the in-person workshop with goals of introducing trainees to the overall topic, ensuring everyone has the same basic knowledge and orienting them to the structure and content of the ÁRBOLES training. In addition, we will add Spanish subtitles for all online trainings.
Content refinements to the training included the addition of more case examples to different sessions, expansion of interactive group activities to increase trainees’ knowledge and skills related to the HBOC and family history, and review of content at the end of the in-person workshop through games, discussion, and reflection.
This study has several weaknesses that cannot be addressed through program refinements. Although our long-term goal is to increase genetic services for Latina women at high risk of HBOC, the ÁRBOLES program only indirectly addresses this aim through training for CORE-Ps in areas that will enhance access to genetic services for those they serve. Although we do measure trainees’ reports of outreach to members in their community, we are unable to assess the direct impact of the training program on high-risk Latina women. In addition, ceiling effects may have dampened results from pre- to post-test. Furthermore, although our pre-test-post-test observational design allows us to assess changes over time in our trainees, future work can rigorously evaluate the efficacy of the ÁRBOLES Familiares training program in a randomized controlled trial to examine the effectiveness for both trainees and the community members that the trainees serve. In future studies, additional outcomes can be assessed, such as the frequency with which trainees use their knowledge, the number and types of interactions trainees have with individuals in the community, and the overall number of women who are appropriately referred to genetic counseling and testing.
Conclusions and practice implications
We have developed a highly innovative training program for CORE-Ps working in the Latino community, combining in-person and online delivery of carefully considered content. Pilot results demonstrate improvements in HBOC knowledge, genetic literacy and self-efficacy, and highlight the most helpful and practical training components, as well as aspects that needed improvement. Participant feedback and a lower-than expected retention rate of the pilot cohort resulted in modifications to session length, structure, and content (including didactic lessons, activities, and practical assignments). The ÁRBOLES Familiares Program addresses a critical disparity among community health educators’ awareness of- and patient referral to- appropriate genetic services among Latinas at increased risk for HBOC. We will evaluate the long-term effect of the ÁRBOLES Familiares training as additional cohorts complete the training.
Recruitment of subsequent cohorts is ongoing and will continue over the course of the funding period. Upon completion of the ÁRBOLES program we will develop training materials and resources that will be available via an online ÁRBOLES Familiares Program Toolkit. Development of toolkits for community use is an approach successfully applied in the past in similar contexts [37]. The ÁRBOLES toolkit will include access to the web-based lectures from the curriculum, suggestions for interactive training activities, and identification of available resources. We also plan to develop a physical toolkit that could be used by different community agencies in conjunction with the online training tools. In addition, we will develop a condensed version of the training program that could be appropriate for delivery in collaboration with other local or national programs that provide training and education for CORE-Ps, including a planned expansion of the ÁRBOLES training program to Latin America.
Acknowledgments:
We appreciate the involvement of our trainees and affiliated ARBOLES faculty.
Funding: This work is funded through an award from the National Cancer Institute, R25CA217723 (Graves, Vadaparampil, MPIs), with additional support from P30CA051008 (Weiner, PI) and the Biostatistics Core Facility at Moffitt Cancer Center under the Cancer Center Support Grant (NCI P30 CA076292, PI: Cleveland).
Compliance with Ethical Standards
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Human Rights: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. (IRB# 00000790).
Informed Consent: The IRB determined this study met the criteria for a waiver of consent.
Transparency Statement: This study was not formally registered. The analysis plan was not formally pre-registered. De-identified data from this study are not available in a public archive. De-identified data from this study will be made available (as allowable according to institutional IRB standards) by emailing the corresponding author. Analytic code used to conduct the analyses presented in this study are not available in a public archive. They may be available by emailing the corresponding author. Materials used to conduct the study are not publicly available.
REFERENCES
- 1. Society AC. Cancer facts & figures for Hispanics & Latinos 2015–2017. 2018; Available at https://www.cancer.org/research/cancer-facts-statistics/hispanics-latinos-facts-figures.html Accessed September 1, 2020.
- 2. Zavala VA, Bracci PM, Carethers JM, et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. 2021;124(2): 315–332. doi: 10.1038/s41416-020-01038-6. Epub 2020 Sep 9. PMID: 32901135; PMCID: PMC7852513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Miranda PY, Wilkinson AV, Etzel CJ, et al. Policy implications of early onset breast cancer among Mexican-origin women. Cancer. 2011;117(2):390–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lara-Medina F, Pérez-Sánchez V, Saavedra-Pérez D, et al. Triple-negative breast cancer in Hispanic patients: high prevalence, poor prognosis, and association with menopausal status, body mass index, and parity. Cancer. 2011;117(16):3658–3669. doi: 10.1002/cncr.25961. Epub 2011 Mar 8. PMID: 21387260. [DOI] [PubMed] [Google Scholar]
- 5. Ellsworth RE, Decewicz DJ, Shriver CD, Ellsworth DL. Breast cancer in the personal genomics era. Curr Genomics. 2010;11(3):146–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Euhus DM, Robinson L. Genetic predisposition syndromes and their management. Surg Clin North Am. 2013;93(2):341–362. [DOI] [PubMed] [Google Scholar]
- 7. Antoniou A, Pharoah PD, Narod S, et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: A combined analysis of 22 studies. Am J Hum Genet. 2003;72(5):1117–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dutil J, Golubeva VA, Pacheco-Torres AL, Diaz-Zabala HJ, Matta JL, Monteiro AN. The spectrum of BRCA1 and BRCA2 alleles in Latin America and the Caribbean: a clinical perspective. Breast Cancer Res Treat. 2015;154(3):441–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lynce F, Graves KD, Jandorf L, et al. Genomic disparities in breast cancer among Latinas. Cancer Control. 2016;23(4):359–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Weitzel JN, Clague J, Martir-Negron A, et al. Prevalence and type of BRCA mutations in Hispanics undergoing genetic cancer risk assessment in the southwestern United States: A report from the Clinical Cancer Genetics Community Research Network. J Clin Oncol. 2013;31(2):210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vadaparampil ST, Wideroff L, Breen N, Trapido E. The impact of acculturation on awareness of genetic testing for increased cancer risk among Hispanics in the year 2000 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2006;15:618–623. [DOI] [PubMed] [Google Scholar]
- 12. Wideroff L, Vadaparampil ST, Breen N, Croyle RT, Freedman AN. Awareness of genetic testing for increased cancer risk in the year 2000 National Health Interview Survey. Community Genet. 2003;6(3):147–156. [DOI] [PubMed] [Google Scholar]
- 13. Jagsi R, Griffith KA, Kurian AW, et al. Concerns about cancer risk and experiences with genetic testing in a diverse population of patients with breast cancer. J Clin Oncol. 2015;33(14):1584–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Suther S, Kiros GE. Barriers to the use of genetic testing: a study of racial and ethnic disparities. Genet Med. 2009;11(9):655–662. [DOI] [PubMed] [Google Scholar]
- 15. Randall TC, Armstrong K. Health Care disparities in hereditary ovarian cancer: Are we reaching the underserved population? Curr Treat Options Oncol. 2016;17(8):39. [DOI] [PubMed] [Google Scholar]
- 16. Ricker C, Lagos V, Feldman N, et al. If we build it. will they come?—Establishing a cancer genetics services clinic for an underserved predominantly Latina cohort. J Genet Couns. 2006;15(6):505–514. [DOI] [PubMed] [Google Scholar]
- 17. Komenaka IK, Nodora JN, Madlensky L, et al. Participation of low-income women in genetic cancer risk assessment and BRCA 1/2 testing: The experience of a safety-net institution. J Community Genet. 2016;7(3): 177–183. doi: 10.1007/s12687-015-0257-x. Epub 2015 Dec 21. PMID: 26690931; PMCID: PMC4960024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Woodson AH, Profato JL, Park M, et al. Service delivery model and experiences in a cancer genetics clinic for an underserved population. J Health Care Poor Underserved. 2015;26(3):784–791. [DOI] [PubMed] [Google Scholar]
- 19. CDC. Genomic workforce competencies 2001. 2001. 2019-01-17T08:12:56Z/; Available at https://www.cdc.gov/genomics/translation/competencies/index.htm. Accessed September 1, 2020.
- 20. Tognetto A, Michelazzo MB, Ricciardi W, Federici A, Boccia S. Core competencies in genetics for healthcare professionals: Results from a literature review and a Delphi method. BMC Med Educ. 2019;19(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Blazer KR, Macdonald DJ, Culver JO, et al. Personalized cancer genetics training for personalized medicine: Improving community-based healthcare through a genetically literate workforce. Genet Med. 2011;13(9):832–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Masny A, Ropka ME, Peterson C, Fetzer D, Daly MB. Mentoring nurses in familial cancer risk assessment and counseling: Lessons learned from a formative evaluation. J Genet Couns. 2008;17(2):196–207. [DOI] [PubMed] [Google Scholar]
- 23. Mai PL, Vadaparampil ST, Breen N, McNeel TS, Wideroff L, Graubard BI. Awareness of cancer susceptibility genetic testing: The 2000, 2005, and 2010 National Health Interview Surveys. Am J Prev Med. 2014;46(5):440–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gammon AD, Rothwell E, Simmons R, et al. Awareness and preferences regarding BRCA1/2 genetic counseling and testing among Latinas and non-Latina white women at increased risk for hereditary breast and ovarian cancer. J Genet Couns. 2011;20(6):625–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Braun KL, Thomas WL Jr, Domingo JL. Reducing cancer screening disparities in Medicare beneficiaries through cancer patient navigation. J Am Geriatr Soc. 2015;63(2):365–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. O'Brien MJ, Halbert CH, Bixby R, Pimentel S, Shea JA. Community Health Worker intervention to decrease cervical cancer disparities in Hispanic Women. J Gen Intern Med. 2010;25(11):1186–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cross KP. Adults as Learners. Increasing Participation and Facilitating Learning. San Francisco, CA: Jossey-Bass; 1981. [Google Scholar]
- 28. Torres CA. Participatory action research and popular education in Latin America. Int J Qual Stud Educ. 2006;5(1):51–62. [Google Scholar]
- 29. Erwin DO, Treviño M, Saad-Harfouche FG, Rodriguez EM, Gage E, Jandorf L. Contextualizing diversity and culture within cancer control interventions for Latinas: Changing interventions, not cultures. Soc Sci Med. 2010;71(4):693–701. [DOI] [PubMed] [Google Scholar]
- 30. Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hispanic J Behav Sci. 1987;9(2):183–205. [Google Scholar]
- 31. Vadaparampil ST, Quinn GP, Small BJ, et al. A pilot study of hereditary breast and ovarian knowledge among a multiethnic group of Hispanic women with a personal or family history of cancer. Genet Test Mol Biomarkers. 2010;14(1):99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rodríguez SA, Roter DL, Castillo-Salgado C, Hooker GW, Erby LH. Translation and validation of a Spanish-language genetic health literacy screening tool. Health Psychology. 2019;34(2):120–129. [DOI] [PubMed] [Google Scholar]
- 33. Rivera YM, Moreno L, Briant KJ, et al. Developing sustainable cancer education programs: Training public health students to deliver cancer 101 in Puerto Rico. J Cancer Educ. 2018;33(1):128–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sussner KM, Thompson HS, Valdimarsdottir HB, Redd WH, Jandorf L. Acculturation and familiarity with, attitudes towards and beliefs about genetic testing for cancer risk within Latinas in East Harlem, New York City. J Genet Couns. 2009;18(1):60–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rush CL, Darling M, Elliott MG, et al. Engaging Latina cancer survivors, their caregivers, and community partners in a randomized controlled trial: Nueva Vida intervention. Qual Life Res. 2015;24(5):1107–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vadaparampil ST, Hutchins NM, Quinn GP. Reproductive health in the adolescent and young adult cancer patient: An innovative training program for oncology nurses. J Cancer Educ. 2013;28(1):197–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Watson-Johnson LC, Bhagatwala J, Reyes-Garcia C, et al. Refinement of an educational toolkit to promote cervical cancer screening among Hispanic immigrant women in rural southern Georgia. J Health Care Poor Underserved. 2012;23(4):1704–1711. [DOI] [PMC free article] [PubMed] [Google Scholar]