Abstract
Caregiving and other interpersonal interactions often require accurate perception of others’ pain from nonverbal cues, but perceivers may be subject to systematic biases based on gender, race, and other contextual factors. Such biases could contribute to systematic under-recognition and under-treatment of pain. In two experiments, we studied the impact of perceived patient sex on lay perceivers’ pain estimates and treatment recommendations. In Experiment 1 (N = 50), perceivers viewed facial video clips of female and male patients in chronic shoulder pain and estimated patients’ pain intensity. Multi-level linear modeling revealed that perceivers under-estimated female patients’ pain compared with male patients, after controlling for patients’ self-reported pain and pain facial expressiveness. Experiment 2 (N = 200) replicated these findings, and additionally found that 1) perceivers’ pain-related gender stereotypes, specifically beliefs about typical women’ s vs. men’ s willingness to express pain, predicted pain estimation biases; and 2) perceivers judged female patients as relatively more likely to benefit from psychotherapy, whereas male patients were judged to benefit more from pain medicine. In both experiments, the gender bias effect size was on average 2.45 points on a 0–100 pain scale. Gender biases in pain estimation may be an obstacle to effective pain care, and experimental approaches to characterizing biases, such as the one we tested here, could inform the development of interventions to reduce such biases.
Keywords: Sex, gendergender bias, pain estimation, pain treatment recommendations, pain-related gender role expectation, stereotypes
Accurate estimation of others’ pain from nonverbal cues is an essential aspect of interpersonal communication45. It forms part of the foundation for empathy57 and caregiving15. With the high pain prevalence in the U.S.33 and worldwide40, recognizing others’ pain is an increasingly valuable interpersonal skill for both clinicians and laypersons. Though pain can often be assessed through pain sufferers’ self-reports, which serve as the current “gold standard” for pain assessment in clinical contexts, recognizing pain facial expressions is an integral part of pain assessment as well 31,56
As pain expressions are communicative behaviors, observers’ interpretations of those expressions are a crucial aspect of pain communication45. Those interpretations are affected not only by the characteristics of pain expressions, but by observers’ knowledge and biases about pain, and the characteristics of pain sufferers13, 18, 26.
The perceived sex of pain sufferers has been found to be particularly influential on estimation of others’ pain. Biases based on perceived sex, operationalized for the present study as the tendency to perceive women as in less or more pain than men for a given level of pain self-report and expressiveness, is particularly important for understanding disparities in clinical and lay settings in terms of pain assessment and treatment. A number of studies have found that providers are more likely to recommend psychological treatment for females than males24, 27, and analgesics more frequently for males than females38, 56, 63. Female patients also wait longer to receive analgesic medication and are less likely to receive opioid analgesics7. Importantly, however, there are some studies on sex biases in pain treatment that show the opposite pattern or no sex differences25, 55. For example, Raftery and colleagues48 found that female emergency room patients received more pain medication and stronger analgesics than male patients, however, in this study increased pain treatment to female patients is likely because those female patients reported more pain and were perceived by providers to experience more pain than male patients48.
Despite clinical evidence of underestimation and undertreatment of female patients’ pain, laboratory findings on sex bias in pain estimation have been inconsistent10, 26, 36, 51, 52. In some studies, females have been judged as being in more pain than males based on their facial expressions of pain51, 52. In other studies, participants have judged female patients to be in less pain than males10, 56, but as higher in catastrophizing32 and exaggeration of pain56 than male patients. It seems that the inconsistency in the direction of the sex bias in pain assessment stems from whether pain facial expressions are taken into account. If females are believed to be more expressive at the same level of pain as men, then controlling for pain facial expressiveness could actually result in a reversal of a sex bias in pain assessment from females to males being perceived to be in more pain.
Sex biases in pain estimation and treatment may arise in part from gender stereotypes about pain. Hoffman and Tarzian28 provided several examples of these pain stereotypes including that, “Women complain more than men; women are not accurate reporters of their pain; men are more stoic so that when they do complain of pain, ‘it’s real’; and women are better able to tolerate pain or have better coping skills than men.” Robinson and colleagues50 formalized measurement of gender stereotypes about pain in others in the Gender Role Expectations of Pain measure (GREP). The GREP asks about perceptions of typical man’s and woman’s sensitivity to, endurance of, and willingness to report pain. Studies using the GREP have reported that women are viewed as more willing to report pain, more sensitive to pain and less able to endure pain than men. These gender pain stereotypes may represent mechanisms underlying gender biases in pain assessment and treatment.
Here, we attempt to resolve conflicting findings over gender biases in pain estimation and understand their underlying mechanisms by extending previous work in three critical respects. First, we compared the differences in pain estimates of women and men at the same level of pain expressiveness by controlling for patients’ self-reported pain and pain facial expressiveness both during stimulus selection and in our analyses. This is necessary because 1) the amount of pain experienced across patients is highly variable, 2) pain facial response is one of the most salient cues perceivers use to estimate pain2, 19, 26, 67, 68, and 3) patients’ expressivity can affect perceivers’ estimates and their empathic accuracy68. Additionally, women are believed to be more expressive than men28. Controlling both factors enables us to verify that differences in pain estimates reflect inaccurate bias, rather than accurate estimation of true sex differences in pain experience and/or expressiveness.
Second, we investigated perceivers’ pain estimation by using real chronic pain patients. Most previous studies have used stimuli depicting experimentally induced pain in healthy participants51, 57, individuals acting as if they are in pain8, 67, or computer-generated avatars1, 26, 27. These studies are valuable, but real chronic pain is likely to be expressed, and perceived, differently62.
Critically, it also remains unclear to what extent gender stereotypes in pain are accurate (reflect the reality of a given cultural context). For example, it may be true that women are more facially expressive than men in the same amount of pain in some cultures. If so, it would be adaptive to use sex and gender information to bias estimates of pain, so as to achieve a more accurate pain estimate. To investigate this, we tested for perceived sex bias in “pain prediction errors” – the difference between self-reported pain and perceived pain. A perceived sex bias in pain prediction errors would indicate a systematic inaccuracy in pain estimates due to perceived sex.
We also extended these analyses to investigate perceived sex biases in lay perceptions of pain treatment recommendations. While there is substantial evidence of perceived sex and gender biases in pain assessment and treatment in clinical settings, fewer studies have investigated these phenomena in lay perceivers. Yet, much of the management of everyday pain complaints and clinical pain conditions takes place in home settings or community-led, group-based self-management programs for chronic pain conditions5, 37. Thus, understanding biases in pain assessment and treatment recommendations by non-medical perceivers will provide needed additional information on the pervasiveness and mechanisms of biases outside of clinical settings.
Experiment 1
Objectives and hypotheses
The objective of Experiment 1 was to test whether patients’ perceived sex affects perceivers’ pain estimation. We hypothesized that female patients would be perceived to be in more pain than male patients without controlling for pain facial expression intensity and patients’ self-reported pain51, 52, but that male patients would be perceived to be in more pain than female patients at equivalent levels of pain facial expression intensity and patients’ self-reported pain32, 56.
Methods
Participants.
50 volunteers (30 females, 20 males, mean age = 22.3 years, age range 18–53 years) recruited from Boulder, Colorado participated in the study. All participants reported having no diagnosed psychiatric or neurologic disorders and no chronic pain conditions. The study was approved by the Institutional Review Board at the University of Colorado Boulder. All participants gave written informed consent and were paid for their time.
Sex and gender.
Gender has been recently defined as the “socially constructed roles, behaviors, expressions and identities of … diverse people”9. It is “usually conceptualized as a binary (girl/woman and boy/man) yet there is considerable diversity in how individuals and groups understand, experience, and express it”. Sex refers to a “set of biological attributes … primarily associated with physical and physiological features including chromosomes, gene expression, hormone levels and function, and reproductive/sexual anatomy.”9, 3. While sex and gender are distinct, “perceived sex” and “perceived gender” cannot be meaningfully distinguished with the stimuli used in this study. Participants inferred both sex and gender together from observable characteristics (e.g., facial and body morphology, hair, clothing, and makeup) in brief videos, and were provided no direct information about sex or gender of target patients. We have opted to use the term “perceived sex” because it perhaps more closely captures the perception that a target patient is male or female. We use the term “gender bias” because it is most prevalent in recent literature referring to disparities in treatment of males and females6, 23, 49 and because discrepancies in perceived pain and other aspects of health are likely to reflect “socially constructed roles, behaviours, expressions and identities” that “influences how people perceive themselves and each other, how they act and interact, and the distribution of power and resources in society”, in accord with recent definitions of gender9.
Stimuli.
36 facial video clips (three each for six male patients and six female patients) were selected from the UNBC-McMaster Shoulder Pain Expression Archive Database35 (Figure S1). The database contains 200 videos of 25 shoulder pain patients captured while they were performing a series of range-of-motion tests to their affected and unaffected limbs. Each test was recorded on digital videotape with the camera focused on the face47. Throughout the paper we use the term “perceived sex” was used which was actually referred to the target’s perceived sex because pain perceivers were left to form impressions of the target’s demographic categories based on targets’ appearance.
The database further contains information about facial pain expressiveness35. In brief, each video frame was action unit (AU) coded by certified Facial Action Coding System (FACS)14 coders and composite facial pain expression scores for each frame were calculated according to the Prkachin and Solomon Pain Intensity (PSPI) formula, which combined scores from four actions: brow lowering (AU4), orbital tightening (AU6 and AU7), levator contraction (AU9 and AU10) and eye closure (AU43). These four actions are thought to show sufficient consistency to be considered a “core” expression of pain44, 47. We used peak PSPI score in each video as the metric of the pain facial expressiveness for that video.
In addition to FACS scores, the UNBC-McMaster database also provides patients’ self-report of their pain during each sequence based on a visual analog scale (VAS) ranging from 0–10 (from “No pain” to “Pain as bad as could be”) and ratings from independent observers ranging from 0–5 (from “No pain” to “Strong pain”). We chose three video clips for each patient, one at each of three intensity levels (low, medium, or high). We determined video intensity level categorizations based on the combination of patient self-reported pain and observer ratings provided by the database (for details, please see Table S1). Ultimately, as we were not able to model a random effect for patient in our mixed effects model due to a lack of a sufficient number of patient exemplars, we chose to average across the three videos of each patient to ensure independence of observations.
Video sequences were edited to 6 s duration centered approximately at the frame with the highest PSPI so as to show both the neutral expressions before and immediately after shoulder movement and the intense pain expressions during movement.
Procedure.
Perceivers completed 36 trials (12 targets with 3 videos each, presented in fully randomized order). In each trial, a fixation cross was presented first for 3–8 s. Then a 6s video clip was displayed. After a 2–6 s delay, perceivers were asked to rate how much pain the patients were experiencing, using a horizontal visual analogue scale (VAS). The scale was anchored at 0, labeled as “absolutely no pain” and 100, labeled as “worst pain possible”.
Analysis.
The data were analyzed with a multi-level GLM testing both within- and between-subject effects, implemented in a freely available toolbox (glmfit_multilevel function in CanlabCore; https://github.com/canlab/CanlabCore). We first estimated one model for each subject across trials. The dependent variable in the within-subject model was perceivers’ pain intensity estimates. Pain estimates of the three trials from each patient were averaged to ensure independence of observations, yielding 12 observations per perceiver. These within-subject models included three predictors: patient perceived sex (male or female), pain facial expressiveness (continuous), and patient self-reported pain (continuous). Parameter estimates from the within-subject models were then submitted to a between-subject model including an intercept term, which tested for reliable effects of these predictors across participants, and a term for participant self-reported gender (male or female) as a moderator.
To estimate effect sizes, we examined “pain prediction errors” – the difference between perceivers’ pain estimates and patients’ self-reported pain, controlling for pain facial expressiveness. To operationalize this, we repeated the above analyses but without a term for perceived patient sex. That is, the within-subject models predicted perceiver pain intensity estimates from self-reported pain and facial expressiveness. We then extracted the model residuals (the pain prediction errors) and tested for effects of perceived patient sex on these residuals.
Results
Gender bias in pain estimation.
Female and male patients were not perceived to be in differing amounts of pain (female mean = 34.10, male mean = 33.39) before controlling for patient pain facial expressiveness and self-report pain, t(49) = 1.53, p = 0.13, which is counter to our hypothesis that females would be perceived to be in more pain in this case. Pain estimates (without controlling for other factors) under each intensity level are shown in Table S2. Consistent with our hypothesis about the effects of controlling for both pain facial expressiveness and self-reported pain, female patients were perceived to be in less pain than male patients, t(49) = 4.11, p < 0.001, when controlling for these two variables. In other words, female patients were perceived to be in less pain than male patients at the same level of pain expressiveness and pain self-report. As expected, increased pain facial expressiveness predicted significantly increased perceiver pain estimates, t(49) = 8.43, p < 0.001. However, in this model, we did not find a significant effect of patient self-reported pain on perceiver pain estimates, t(49) = 1.7, p = 0.1. This is likely because pain facial expressiveness and patient self-reported pain were correlated (within-person r = 0.44, p < 0.05), and variance in pain estimation related to patient self-reported pain was likely largely explained by pain facial expressiveness. Finally, perceivers’ sex did not moderate their estimation of patients’ pain, t(49) = −0.19, p = 0.85, i.e. male and female perceivers did not differ in the estimates of male and female patients’ pain.
To estimate the gender bias effect size, we tested for effects of perceived sex on “pain prediction errors” – the difference between estimated and self-reported pain, operationalized as model residuals. We found a 2.23-point difference between male and female patients, on a 0–100 pain scale (Figure 1), with male patients’ pain overestimated / female patients’ pain underestimated.
Fig. 1.
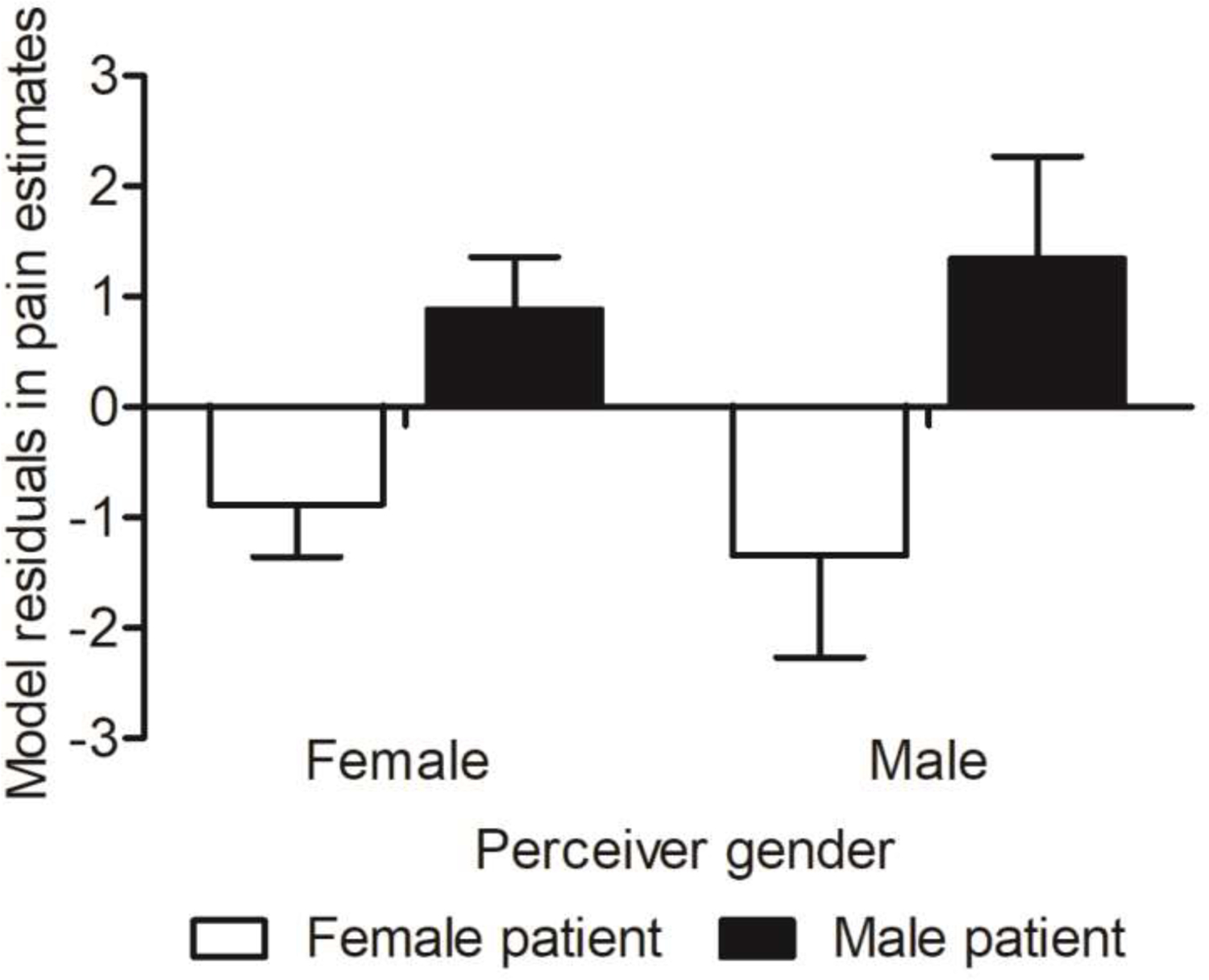
Gap in pain estimates at the same pain cues in Experiment 1. The y axis shows residuals in perceivers’ pain estimates on a 0–100 scale when controlling for patients’ pain facial expressiveness and self-reported pain. The error bars reflect the within-subject standard error of the mean.
Experiment 2
Objectives and hypotheses
In Experiment 2 we had three objectives: (1) to replicate gender biases observed in Experiment 1 with an enlarged patient and perceiver sample, (2) to examine whether perceived patient sex would also impact treatment recommendations regarding medication and psychotherapy, and (3) to examine whether pain-related gender stereotypes helped to explain biases in pain estimation and treatment.
We predicted that 1) male patients would be estimated to be in more pain than female patients when controlling for pain facial expressiveness and patient self-reported pain (replicating Experiment 1); 2) male patients would be prescribed greater doses of pain medicine, whereas female patients would be prescribed more sessions of psychotherapy27, 56; 3) pain medicine would be seen as more helpful for male patients whereas psychotherapy would be seen as more helpful for female patients; 4) the gender biases in pain estimation and pain treatment would be influenced by the pain-specific gender stereotypes perceivers held.
Methods
Participants.
200 participants were tested via Amazon Mechanical Turk using Qualtrics software (Qualtrics, Provo, UT, USA. http://www.qualtrics.com). More than half (108 out of 200) of them have or had at least one chronic pain condition such as back pain, arthritis, migraine, etc., or acute pain conditions such as accidents, injuries, surgeries, etc. Only three out of the 200 participants had worked in healthcare. One participant failed to follow the study instructions (giving the same rating to all pain video stimuli) and was therefore excluded. Two participants chose their gender identity as “other”. Given that there were only two participants with non-binary gender, we chose to exclude them from the analysis as it would not have been possible to conduct a meaningful test of whether this group differed from those identifying as male and female in our sample. Data from the remaining 197 perceivers (81 females, 116 males, mean age = 32.3, age range 19–55 years old) were included in the analyses. The study was approved by the Institutional Review Board at the University of Colorado Boulder. Online informed consent was provided by all participants.
Stimuli.
Two different video clips of the facial expressions of each of 25 (13 females, 12 males) patients from the whole UNBC-McMaster Shoulder Pain Expression Archive Database35 were selected and edited to 6s in the same manner as in Experiment 1. We divided stimuli into two stimulus sets, with one video of each patients randomly assigned to each set. We controlled for any potential differences between the two stimulus sets by controlling for pain facial expressiveness and patient pain self-report in all of our models. We used this approach to reduce the influence of idiosyncrasies in individual patient videos while ensuring independence of observations. Each stimulus set was tested with 100 perceivers, yielding N = 98 (43 female) for stimulus set 1 and N = 99 (38 female) for stimulus set 2 (total N=197) analyzed for each stimulus set, with random assignment of participants to a stimulus set.
Procedure.
The online survey opened with the consent form and a demographic questionnaire. Experiment instructions (see supplementary materials for detailed instructions) and a practice trial were provided prior the main task. In each trial of the main task, perceivers first watched a 6s video clip and then estimated the patient’s pain on a horizontal VAS from 0 (“absolutely no pain”) to 100 (“worst pain possible”), as in Experiment 1. The videos were presented in a unique random order to each perceiver.
Following the main task, perceivers were then asked to prescribe pain treatments for each patient as if they were doctors (see supplementary materials for detailed instructions). A still frame from the video showing neutral facial expression was presented along with the prescription questions. Three questions were asked: 1) “If you were to prescribe pain medicine, what dose would you prescribe to this patient?”, 2) “If you were to prescribe psychotherapy, how many sessions would you prescribe?”, and 3) “What do you think would help the patient more, pain medicine or psychotherapy?” Since we believed most perceivers would not have medical training (confirmed in our sample with only 3 out of 200 with health care work experience), response ranges for the first two questions were made on a VAS from 0 (minimal dose or sessions) to 100 (maximal dose or sessions), rather than using a more specific clinical unit. For the third question, perceivers were required to make a forced choice between pain medicine and psychotherapy.
Lastly, perceivers were asked to complete the Gender Role Expectation of Pain Questionnaire (GREP)64, which measures gender-related stereotypic attributions about sensitivity to pain, endurance of pain, and willingness to report pain. The 9 questionnaire items were: “What is the typical woman’s sensitivity to pain/endurance of pain/willingness to report pain?”, “What is the typical man’s sensitivity to pain/endurance of pain/willingness to report pain?”, and “What is your sensitivity to pain/endurance of pain/willingness to report pain?”. These questions reflect the modified version of the GREP64, which was simplified from the original version50, to remove comparison statements, e.g., “compared with the typical woman, the typical man’s sensitivity to pain is.” Questions were rated on a visual analogue scale (VAS) scale from 0 (not at all sensitive, no endurance at all, or not at all willing) to 100 (most sensitive imaginable, most endurance imaginable, or most willing imaginable). For the present study, we focused on the 6 questions about the typical woman and man.
The experiment took 21 minutes on average to complete. Each perceiver was compensated $2.
Analysis.
We ran three sets of analyses corresponding to our three objectives. The first set of analyses tested for gender bias in pain estimation using a multi-level general linear model (GLM) in the same manner as Experiment 1.
The second set of analyses tested for gender biases in pain treatment recommendations using two different analyses. First, we tested for biases in treatment recommendations (doses of medicine or sessions of psychotherapy) using separate multi-level GLMs, also in the same manner as Experiment 1. Second, we tested for biases in treatment preference by calculating the proportion of the 25 trials in which medicine vs. psychotherapy was prescribed across both male and female patients, and to male and female patients separately. To test overall treatment preference, we conducted a one-sample t-test against a null hypothesis of 0.5, which would indicate an equal proportion of patients for which each of the two pain treatments was selected and thus no treatment preference. To test for gender biases in treatment preference, we performed paired t-tests on proportions for males vs. females.
The third set of analyses tested whether observed gender biases in pain estimation and treatment recommendations were moderated by the pain-related gender role expectations of perceivers. We used a two-step process in which we first screened for pain-related gender role expectations that showed some relationship with pain estimation or treatment recommendations by computing Pearson’s correlations between pain-related gender role expectations and each of the two variables of interest: (a) participants’ average pain estimation for female and male patients, and (b) hypothetical prescriptions of pain treatment recommendations for female patients and male patients. For the second step, we included any pain-related gender role expectations showing significant correlations with pain estimation and/or treatment variables in the multilevel GLM as moderators in the form of pain-related gender role stereotype scores. The pain-related gender role stereotype scores were created for each item by subtracting each perceiver’s beliefs about typical women from those for typical men, resulting in 3 scores ranging from −100 (strongest bias in favor of thinking the typical man has higher pain sensitivity/ endurance/ or willingness to report than the typical women) to 100 (strongest bias in favor of thinking the typical woman has higher pain sensitivity/ endurance/ or willingness than the typical man).
Results
Gender bias in pain estimation.
Female patients were perceived to be in less pain than male patients before controlling for other factors, t(196) = 3.27, p = 0.001, which is counter to our hypothesis that females would be perceived to be in more pain in this case but consistent with our findings in Experiment 1 after controlling for pain facial expressiveness and self-reported pain. Also consistent with the findings of Experiment 1, increased pain facial expressiveness predicted significantly increased pain estimates when controlling for self-reported pain, t(196) = 19.98, p < 0.001. Increased self-reported pain also independently, significantly predicted increased pain estimates controlling for pain facial expressiveness, t(196) = 6.04, p < 0.001. More importantly, when controlling for both pain facial expressiveness and patient self-reported pain, female patients were estimated to be in less pain than male patients, consistent with our hypothesis and the findings of Experiment 1, t(196) = 4.13, p < 0.001. In other words, as in Experiment 1, female patients were perceived to be in less pain than male patients at the same level of pain expressiveness and pain self-report. This bias was not moderated by perceivers’ gender, t(196) = −0.3, p = 0.76. In other words, male and female perceivers did not differ in the relative amount of pain they perceived in males and females.
As in Experiment 1, we also tested the influence of perceived sex on pain prediction errors. Our results were consistent with Experiment 1, finding relatively more positive pain prediction errors for men (pain overestimation) and relatively more negative prediction errors for women (pain underestimation). Perceived sex introduced a bias of 2.67 points on a 0–100 pain scale (Figure 2).
Fig. 2.
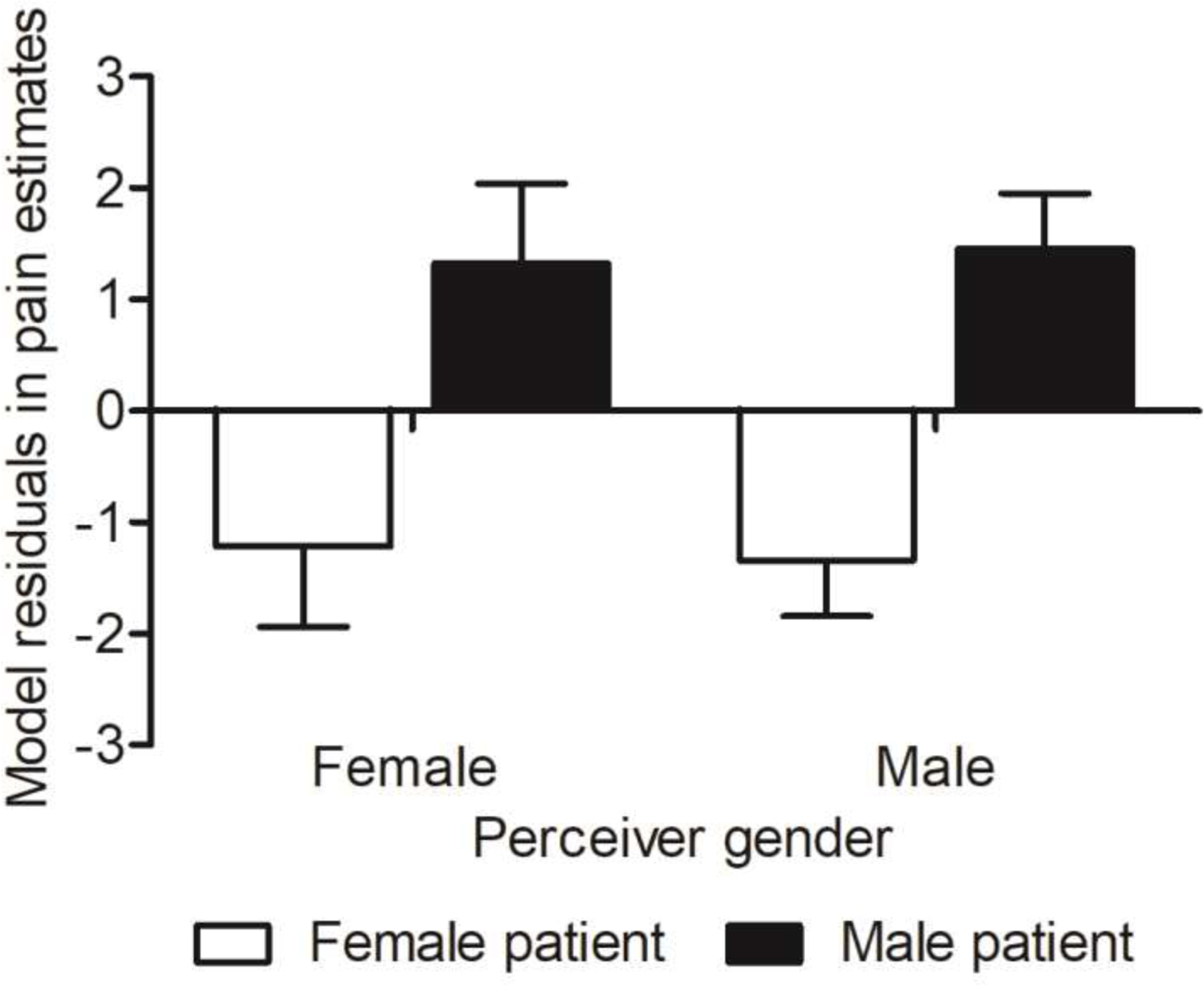
Gap in pain estimates at the same pain cues in Experiment 2. The y axis shows residuals in pain estimates on a 0–100 scale when controlling for pain facial expressiveness and self-reported pain, grouped by gender. Error bars show within-subject standard error of the mean.
Gender bias in pain treatment recommendations.
Contrary to our hypotheses the dose of pain medicine prescribed to female and male patients did not differ after controlling for pain facial expressiveness and patient self-reported pain, t(196) =0.13, p = 0.9. As expected, however, increased pain facial expressiveness significantly predicted increased doses of pain medicine, t(196) = 4.35, p < 0.001, but patient self-reported pain did not predict dose of pain medicine after controlling for expressiveness, t(196) = 0.18, p = 0.86.
Also contrary to our hypothesis the sessions of psychotherapy prescribed for female and male patients did not differ, t(196) = −0.46, p = 0.64, when controlling for pain facial expressiveness and patient self-reported pain. As with pain medicine, however, increased pain facial expressiveness significantly predicted prescription of more sessions of psychotherapy, t(196) = 2.67, p < 0.01, and we did not find an effect of patient self-reported pain on sessions of psychotherapy prescribed, t(196) = −0.71, p = 0.48.
Male and female perceivers also did not differ in the doses of pain medicine (p = 0.62) or sessions of psychotherapy they prescribed (p = 0.26). Importantly, the fact that patients’ pain facial expressiveness significantly predicted the dose of pain medicine and the sessions of psychotherapy prescribed suggested perceivers did not prescribe randomly, but likely based their management recommendations on their memory of patients’ pain expressiveness.
When perceivers were asked to make a forced-choice recommendation about which treatment would be more helpful for each patient, pain medicine was preferred over psychotherapy overall for both females (58% medicine vs. 42% psychotherapy) and males (62% medicine vs. 38% psychotherapy). The average number of trials for which each participant prescribed pain medicine was significantly greater than 50%, t(196) = −5.59, p < 0.001. However, a comparison of treatment preference for male and female patients revealed that psychotherapy was preferred for a higher proportion of female patients (42%) than male patients (38%). A paired t-test on the average number of trials for which each participant prescribed psychotherapy for females vs. males showed a significant difference; t(196) = 2.47, p < 0.05 (Figure 3).
Fig. 3.
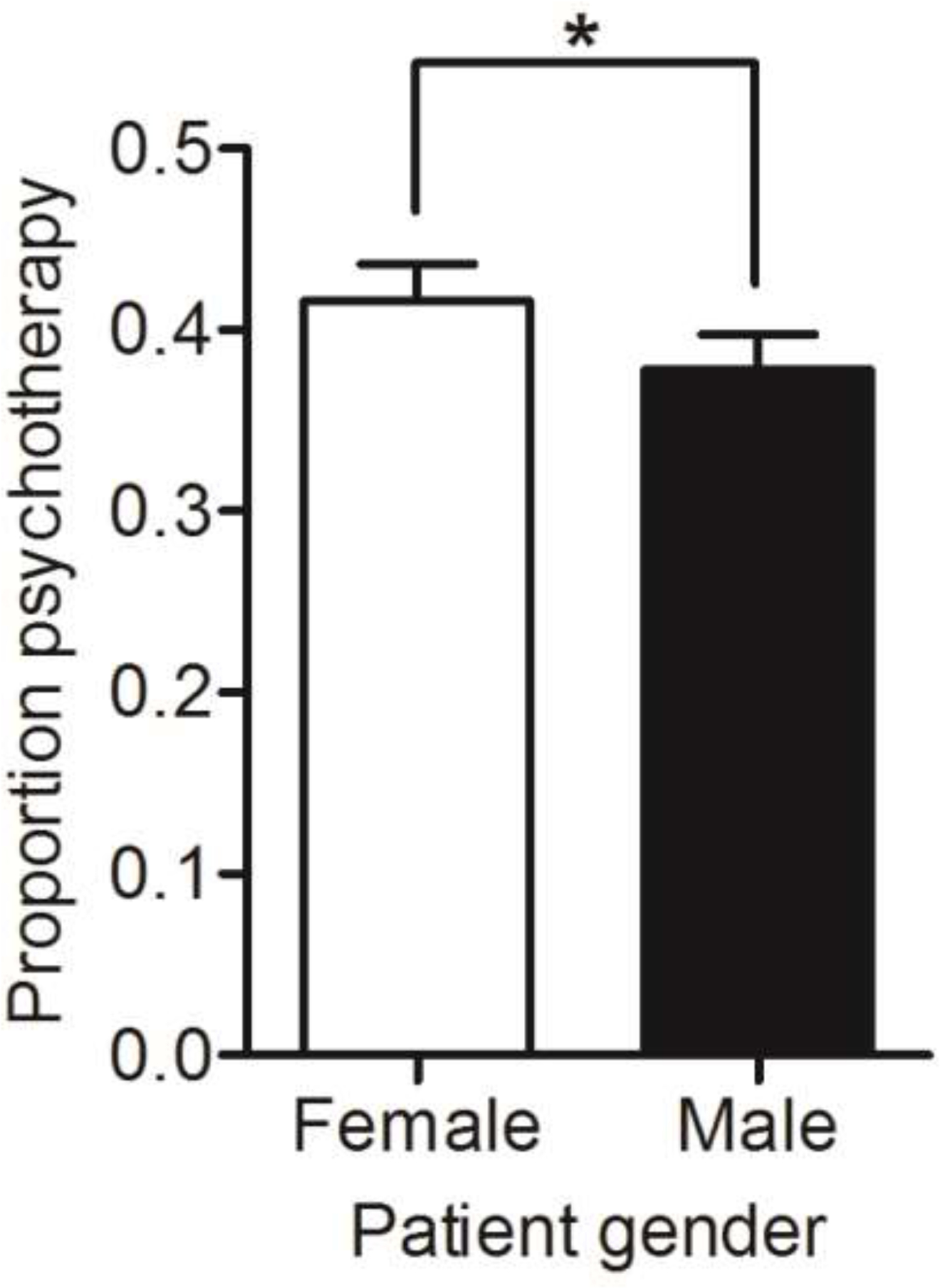
Pain treatment preference for psychotherapy vs. medication for male and female patients. Y axis values represent the proportion of the patients of a given gender in which perceivers indicated psychotherapy would be more helpful than pain medication in a forced-choice test. Proportion of pain medicine = 1- proportion of psychotherapy. Psychotherapy was preferred more often for female than for male patients whereas pain medication was preferred more often for male than female patients. Error bars reflect the standard error of the mean. *, p < 0.05.
Moderation of bias in pain estimation and pain treatment recommendations by pain-related gender role expectations.
We found a significant interaction between perceiver gender and typical gender ( F(1, 195) = 9.08, p < 0.01) showing that female perceivers believed that typical women have higher pain endurance than typical men (p < 0.001) and a main effect of typical gender, such that perceivers believed typical women to be substantially more willing to report pain than typical men, F(1, 195) = 76.24, p < 0.001 (See “Pain-related gender role expectations” in Supplementary Materials for full results). Because gender role expectations about pain endurance and willingness to report pain had previously been reported to account for variance in pain estimation26, 51, we tested whether these two expectations of perceivers were correlated with sex biases in pain estimation and pain treatment recommendations, and if yes, whether these items influenced pain estimation and pain treatment recommendations in our multilevel models.
Correlations between pain-related gender role expectations and both pain estimation and pain treatment recommendations are shown in Table 1. Perceivers’ expectations about the typical man’s ability to endure pain were associated with higher estimation of male patients’ pain, r(197) = 0.16, p = 0.02, and prescription of more pain medicine, r(197) = 0.18, p = 0.01. Perceivers’ expectation about the typical man’s willingness to report pain were also associated with higher estimation of male patients’ pain, r(197) = 0.14, p = 0.05, and prescription of both more pain medicine, r(197) = 0.21, p = 0.004, and psychotherapy, r(197) = 0.29, p < 0.001. (Participants selected a prescribed dose for each independently). In contrast, perceivers’ expectations about the typical woman’s ability to endure pain and willingness to report pain were not associated with their estimation of female patients’ pain or their prescriptions to female patients.
Table 1.
Correlation between pain-specific gender role expectations and pain estimation or treatment recommendations
| GREP | Pain estimation |
Pain medicine |
Psychotherapy |
|||
|---|---|---|---|---|---|---|
| FePat | MaPat | FePat | MaPat | FePat | MaPat | |
| TypWoEnd | 0.05 | — | −0.02 | — | 0.01 | — |
| TypMeEnd | — | 0.16* | — | 0.18* | — | 0.12 |
| TypWoWil | 0.1 | — | 0.11 | — | 0.09 | — |
| TypMeWil | — | 0.14# | — | 0.21** | — | 0.29*** |
Note. GREP, Gender Role Expectation of Pain Questionnaire. TypWoEnd, typical woman’s endurance of pain; TypMeEnd, typical man’s endurance of pain; TypWoWil, typical woman’s willingness to report pain; TypMeWil, typical man’s willingness to report pain. FePat, female patients; MaPat, male patients;
= p < 0.1;
= p < 0.05;
= p < 0.01;
= p < 0.001.
We added these gender stereotype scores for willingness to report pain and endurance of pain separately to our multilevel models as between-person moderators. For pain estimation, perceivers who believed typical women are more willing to report pain than men estimated female patients to be in less pain than men, t(196) = −2.45, p < 0.05. In contrast, gender stereotypes about endurance of pain did not moderate gender biases in pain estimation, t(196) = 0.75, p = 0.46. Importantly, female patients were still perceived to be in less pain than male patients after adding gender stereotypes about willingness to report pain to the model, t(196) = 4.43, p < 0.001, indicating that the average participant shows reasonably strong gender bias and that other factors such as additional pain stereotypes, or perceptual biases likely contribute to this bias. For pain treatment recommendations, neither gender stereotype moderated the gender bias in hypothetical prescriptions of medicine or psychotherapy.
Discussion
Accurate estimation of others’ pain is an important interpersonal skill in both clinical and everyday settings. We found that lay perceivers’ pain estimation and pain treatment recommendations were biased by perceived patient sex. Perceivers estimated female patients to be in less pain than male patients at the same level of pain expressiveness and pain self-report and underestimated women’s pain relative to their own self-report while overestimating men’s pain relative to their own self-report. Perceivers also indicated that female patients would benefit more than male patients from psychotherapy vs. medication. Furthermore, we found that perceivers pain-related gender stereotypes influenced their biases in pain estimation. The more willing perceivers believed women are report pain than men, the less pain they perceived female patients to be in. Importantly, these biases were observed while participants viewed actual patients in genuine clinical pain, and when controlling for pain facial expressiveness and patients’ self-reported pain.
Together, these findings suggest that women’s pain is underestimated compared to men’s and perceived to benefit more psychotherapy, and that perceivers’ pain-related stereotypes may be a source of these pain estimation and treatment biases. These findings add to a growing body of evidence of demographic biases in the estimation and treatment of others’ suffering in a wide range of societal domains from the medical field26, 27, 56, 65 to the justice system41 and point to stereotype education as a promising avenue for mitigating these biases.
Perceived sex effects on pain estimation and treatment recommendations
Male patients were perceived to be in more pain than female patients both before and after controlling for pain facial expressions and pain self-report in Experiment 2. This same pattern was only revealed after controlling for pain facial expressions and pain self-report in Experiment 1, with no perceived sex difference in pain estimates evident before controlling for these factors. The finding that men’s pain is over-estimated relative to women’s is consistent with other studies suggesting that males’ pain is perceived as more intense than female’s pain56, even in neonates10. However, our finding stands in contrast to an even larger number of studies that have found women to be estimated in more pain than men26, 36, 51. In addition, a substantial literature demonstrates that when sex or gender differences in pain report are present, women are almost always found to report more pain than men16, 20. Several factors may explain these discrepancies, including variability across studies in whether perceivers assess specific people vs. make normative judgments and the specific aspects of pain that are being judged. For example, perceivers may simultaneously believe that women experience more pain in response to a given stimulus, but under-value the actual indicators of pain in women. Our perceivers rated genuine pain expressions in clinical shoulder pain patients. Thus, the gender biases observed in the present study may be more similar to those seen in real-world clinical and lay pain evaluation contexts than in some previous studies.
Another factor that may help explain differences between our findings of biases in pain estimation and those in previous studies is whether pain expressiveness and self-report are controlled for. Women are consistently found to report higher levels of pain than men16, 20 and to be more expressive of pain than men22, 60. Perceivers may in turn get habituated to more frequent or more intense pain expressions in females and as a result reduce the pain they attribute to those expressions. A similar bias has been seen upon repeated exposure to pain facial expressions which has been found to reduce vicarious pain estimation21, 46. Thus, controlling for both factors is critical to test for the presence of a true bias, i.e. differences in pain estimates for male and female patients based on the same pain cues. Several previous studies in which women were perceived to be in more pain than men did not control for pain facial expression intensity, and to our knowledge, no prior studies controlled for the pain sufferer’s own pain reports, either alone or in combination with their pain facial expressions. Thus, some of those prior findings may not have reflected true biases in pain estimation. Furthermore, our findings of men being perceived in higher pain than women are consistent with biases in clinical pain treatment, which have demonstrated that men are more likely to receive analgesic treatment, in stronger forms, and more rapidly than women7, 24, 27.
A final factor that may contribute to the difference between our findings and those in previous studies is that some previous studies employed observers with medical training. In contrast, only 3/200 participants in Experiment 2 in the present study reported having healthcare work experience. Previous studies have suggested that medical training may influence how people perceive pain in others. For example, health professionals have been found to underestimate patients’ pain58. Although we do not know of any studies showing that medical training changes pain assessment and treatment biases related to patient demographics, this is also plausible.
Gender-related pain stereotypes contribute to perceived sex differences in pain estimation and treatment recommendations
Prior literature suggests the most likely source of gender biases in pain estimation are the norms and stereotypes perceivers hold about emotional expression and pain responses. Generally, boys are discouraged from expressing emotions, whereas girls are permitted to express them. These norms hold in many cultures and societies from a young age28, 43. As a result, men may be more reluctant to express pain and other vulnerabilities than women43. Thus, masculine gender norms are associated with high pain tolerance and stoicism whereas feminine gender norms are more permissive of expressing pain39, 61.
We found evidence of these pain-related gender stereotypes in the current study. Specifically, women were considered substantially more willing to report pain than men by both male and female perceivers, replicating prior work50, 53, 66. Additionally, female perceivers rated women as more willing to endure pain than men. Critically, individual differences in the beliefs regarding women’s higher willingness to report pain were directly linked to reduced pain estimates of female (compared to male) patients. Thus, it is plausible that male patients’ expressions of pain were seen as more credible whereas those of female patients were discounted during pain estimation, to correct for an assumed higher pain expressiveness of women. We found no statistically significant perceived sex differences in pain facial expressiveness in the present stimuli (see supplementary materials), but other studies suggest that females may indeed report and express higher pain than males17, 20, 22. In other words, our participants’ bias (stereotype) that women are more expressive of pain than men may well be accurate at the population level. However, it led them to misestimate pain in this study. Indeed, studies have shown that people use group-level stereotypes when information about the individual person is sparse30, as was the case for our stimuli and in many medical encounters.
Alternatively, perceivers may habituate to repeated and more frequent expressions of pain in females. Grégoire and colleagues21 showed that repeated exposure to others’ pain reduces vicarious pain intensity estimation. Using signal-detection techniques, Prkachin and colleagues46 similarly demonstrated that repeated exposure to pain facial expressions led to more conservative recommendations about pain estimation. Although in the present study there were no sex differences in pain facial expressiveness in video stimuli, it is possible that perceivers’ previous experiences of higher pain expressiveness by women compared to men made them less willing to attribute pain to female patients. If this was the case, our findings, together with evidence from other studies8, 11, 58, would suggest that frequent exposure to female patients’ intense pain facial expressions in clinical settings might contribute to underestimation of their pain and in turn may result in sub-standard treatment for them.
In contrast to our findings on willingness to report pain, gender stereotypes about endurance of pain did not moderate perceived sex biases in pain estimation. This finding may be in conflict with the findings of Robinson and Wise51 who report that both male and female gender pain stereotypes predict pain estimation for male and female patients. However, our use of a difference score between female and male gender pain stereotypes as a moderator of perceived sex effects on pain estimation is not directly comparable to the analyses in Robinson and Wise51. Our finding that female perceivers rated women as more willing to endure pain than men but male participants did not is consistent with the findings of Wandner and colleagues64 but inconsistent with the findings of Robinson and colleagues50 who found that both males and females rated women as less willing to endure pain than men. Finally, our finding that neither male nor female perceivers rated typical men and women to differ in pain sensitivity is in conflict with the findings of both Robinson and colleagues50 and Wandner and colleagues64, who both found that women were perceived to be less willing to endure pain and more sensitive to pain by both male and female perceivers. One factor that may explain the differences between our findings and those of Robinson and colleagues50 is that participants viewed patient pain videos prior to filling out questionnaires about their gender pain stereotypes in our study. Patient pain videos may have influenced our participants gender stereotypic pain views, at least in the short term.
Implications of underestimation and psychologization in treatment of women’s pain
A critical question for understanding the potential effects of gender biases in pain estimation is whether they are accurate at a population level. For example, if women in a given cultural context are more expressive relative to their level of pain compared to men, then perhaps a gender bias would be adaptive in forming accurate pain estimates at a population level. Taking self-reported pain as the ground truth, however, our analyses of pain prediction error in both experiments show that perceived sex introduces a systematic bias leading to inaccurate pain estimation, with underestimation of women’s pain and overestimation of men’s relative to their reports of their own pain.
Pain underestimation and psychologization in the treatment of women’s pain could both have detrimental effects on female patient’s health outcomes. For example, in the study of Schäfer and colleagues56, health care providers who believed female chronic pain patients were more likely to exaggerate their pain prescribed psychotherapy to female patients but opioids to male patients, presumably because providers attributed less pain to female patients. Yet, prior studies have not found consistent differences in the treatment efficacy of psychotherapy and opioids for female and male patients4, 34, 42, 59. Thus, the belief that psychotherapy is more helpful to female patients and opioids are more helpful to male patients that we observed in this study, likely represents a true bias, i.e. a deviation from the most efficacious treatment strategies. Our data cannot speak to the particular reason that participants were more likely to prefer psychotherapy for women, however. One possibility is that participants may believe that women’s pain is less nociceptive in origin. Another is that they may believe women will be more receptive to psychotherapy and benefit more from it. Other explanations may be possible as well.
Limitations
Our findings should be interpreted in light of several limitations. The size of the patient sample used in this study is limited (N = 12 in Experiment 1 and N = 25 in Experiment 2). Because of this limited sample size of patient stimuli our analyses treated patient as a fixed (non-random) effect. Therefore, future studies will need to test whether our findings generalize to other populations of male and female patient exemplars. Additionally, because the factors affecting the estimation and treatment of patient pain may differ across different pain conditions54, it is unclear whether our findings would generalize to pain disorders beyond shoulder pain. However, we did have similar findings across our two experiments.
Another aspect that potentially limits the generalizability of the findings to clinical settings is hardly any of the pain perceivers had medical training or healthcare work experience (3/200 in Experiment 2). However nearly half of them (92 out 200 in Experiment 2) reported past or current experiences with pain, thus they likely did have experience with considering treatments for their own pain and likely the pain of those in their families. Indeed, pain is a universal condition and many recommendations about pain and its management are made outside of medical care by members of the lay public. Even individuals with chronic pain conditions often make recommendations about their own pain treatment, striving for self-management5. Furthermore, lay-led, group-based self-management programs for patients with chronic pain have been developed, which entail the evaluation of pain and pain treatment by lay perceivers37. Therefore, understanding the biases that lay perceivers have in both pain assessment and treatment recommendations has value and potential clinical relevance.
The magnitude of the perceived sex bias in pain estimation revealed in this study was on average 2.45 points out of a 100-point scale. Further studies are needed to decide whether an effect of this size would be practically meaningful. Similarly, the correlations between perceived sex bias in pain estimation and gender role expectations in our studies, though small, are statistically significant. Also importantly, female patients were still perceived to be in less pain than male patients after adding gender stereotypes about willingness to report pain to the model.
This study was not able to address biases related to race and age (for studies, see Hollingshead and colleagues29) as the UNBC-McMaster Shoulder Pain Expression Archive Database does not systematically vary in race and age, nor does it provide demographic information for the patients. As studies with virtual agents have demonstrated that the perceived age and race/ethnicity of the target can also influence pain assessment and treatment29, 63, it is possible these factors could have influenced our results. However, the patients appear to be mostly middle-aged Caucasian adults. Therefore, we think race and age are unlikely to represent a major confound in findings. Generalization of our findings to other patient demographic groups will require further research with stimuli systematically varying in other demographic dimensions.
Lastly, averaging the pain estimates of the three trials from each patient, though ensuring the independence of observation, obscures potential interactions with painful stimulus intensity that could further inform interventions aimed at mitigating gender disparities in pain treatment. Similarly, as we only included pain facial expressions we were not able to test the specificity of the biases we observed to pain. The degree to which our findings generalize across different levels of observed pain intensity and different facial expressions should be addressed in future studies.
Conclusions
The present study demonstrates a perceived sex bias in lay perceivers’ pain estimation and pain treatment recommendations. Women’s pain was viewed as less intense and as benefiting more from psychotherapy than men’s pain and perceivers’ gender role stereotypes about willingness to report pain explained some of this bias in pain estimation. These findings suggest that gender biases in pain estimation may be an obstacle to effective pain care, and that experimental approaches to characterizing biases, such as the one we tested here, could inform the development of interventions to reduce such biases.
Supplementary Material
Highlights.
In two studies, perceivers under-estimated female patients’ pain compared with males’ pain.
Perceivers’ pain-related gender stereotypes predicted pain estimation biases.
Perceivers prescribed more psychotherapy for female and more pain medicine for male patients.
Perspective:
This study identifies a bias towards underestimation of pain in female patients, which is related to gender stereotypes. The findings suggest caregivers’ or even clinicians’ pain stereotypes are a potential target for intervention.
Acknowledgement
The authors would like to acknowledge Daniel Kusko, Daniel Weflen and Philip Kragel for their help on participant recruitment, code debugging and helpful discussion.
Funding:
This work was supported by grant R01DA035484 to T.D.W.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Multilevel General Linear Model code is available at: https://github.com/canlab. All data and analyses from the two experiments are available here: https://github.com/zhang2lan/Gender-bias-in-pain-estimation. The authors have no potential conflicts of interest to declare.
References
- [1].Bartley EJ, Boissoneault J, Vargovich AM, Wandner LD, Hirsh AT, Lok BC, Heft MW, Robinson ME: The influence of health care professional characteristics on pain treatment recommendations. Pain Med 16: 99–111, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Bijlstra G, Holland RW, Wigboldus DH: The social face of emotion recognition: Evaluations versus stereotypes. J Exp Soc Psychol 46, 657–663, 2010. [Google Scholar]
- [3].Boerner KE, Chambers CT, Gahagan J, Keogh E, Fillingim RB, Mogil JS: Conceptual complexity of gender and its relevance to pain. Pain 159: 2137–2141, 2018. [DOI] [PubMed] [Google Scholar]
- [4].Broderick JE, Keefe FJ, Schneider S, Junghaenel DU, Bruckenthal P, Schwartz JE, Kaell AT, Caldwell DS, McKee D, Gould E: Cognitive behavioral therapy for chronic pain is effective, but for whom? Pain 157: 2115–2123, 2016. [DOI] [PubMed] [Google Scholar]
- [5].Campbell C, Cramb G: ‘Nobody likes a back bore’–exploring lay perspectives of chronic pain: revealing the hidden voices of nonservice users. Scand J Caring Sci 22: 383–390, 2008. [DOI] [PubMed] [Google Scholar]
- [6].Carlana M: Implicit stereotypes: Evidence from teachers’ gender bias. Q J Econ 134: 1163–1224, 2019. [Google Scholar]
- [7].Chen EH, Shofer FS, Dean AJ, Hollander JE, Baxt WG, Robey JL, Sease KL, Mills AM: Gender disparity in analgesic treatment of emergency department patients with acute abdominal pain. Acad Emerg Med 15: 414–418, 2008. [DOI] [PubMed] [Google Scholar]
- [8].Cheng Y, Lin C-P, Liu H-L, Hsu Y-Y, Lim K-E,Hung D, Decety J: Expertise modulates the perception of pain in others. Curr Biol 17: 1708–1713, 2007. [DOI] [PubMed] [Google Scholar]
- [9].CIHR: Canadian Institutes of Health Research, Institute of Gender and Health. What is gender? What is sex? Available at: http://www.cihr-irsc.gc.ca/e/48642.html. 2021.
- [10].Cohen LL, Cobb J, Martin SR: Gender biases in adult ratings of pediatric pain. Child Health Care 43: 87–95, 2014. [Google Scholar]
- [11].Decety J, Yang C-Y, Cheng Y: Physicians down-regulate their pain empathy response: an event-related brain potential study. Neuroimage 50: 1676–1682, 2010. [DOI] [PubMed] [Google Scholar]
- [12].Denisco RA, Chandler RK, Compton WM: Addressing the intersecting problems of opioid misuse and chronic pain treatment. Exp Clin Psychopharm 16: 417, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ely B, Dampier C, Gilday M, O’Neal P, Brodecki D: Caregiver report of pain in infants and toddlers with sickle cell disease: reliability and validity of a daily diary. J Pain 3: 50–57, 2002. [DOI] [PubMed] [Google Scholar]
- [14].Ekman P, Friesen WV: Manual for the facial action coding system Consulting Psychologists Press. 1978. [Google Scholar]
- [15].Esteve R, Marquina-Aponte V, Ramírez-Maestre C: Postoperative pain in children: association between anxiety sensitivity, pain catastrophizing, and female caregivers’ responses to children’s pain. J Pain 15: 157–168, 2014. [DOI] [PubMed] [Google Scholar]
- [16].Fillingim RB: Sex, gender, and pain: women and men really are different. Curr Rev Pain 4: 24–30, 2000. [DOI] [PubMed] [Google Scholar]
- [17].Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL: Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain 10: 447–485, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Goubert L, Craig KD, Vervoort T, Morley S, Sullivan M, de CAC W, Cano A, Crombez G: Facing others in pain: the effects of empathy. Pain 118: 285–288, 2005. [DOI] [PubMed] [Google Scholar]
- [19].Green AD, Tripp DA, Sullivan MJL, Davidson M: The relationship between empathy and estimates of observed pain. Pain Med 10: 381–392, 2009. [DOI] [PubMed] [Google Scholar]
- [20].Greenspan JD, Craft RM, LeResche L, Arendt-Nielsen L, Berkley KJ, Fillingim RB, Gold MS, Holdcroft A, Lautenbacher S, Mayer EA: Studying sex and gender differences in pain and analgesia: a consensus report. Pain 132: S26–S45, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Grégoire M, Coll M, Tremblay M, Prkachin K, Jackson P: Repeated exposure to others’ pain reduces vicarious pain intensity estimation. Eur J Pain 20: 1644–1652, 2016. [DOI] [PubMed] [Google Scholar]
- [22].Guinsburg R, de Araújo Peres C, de Almeida MFB, Balda RdCX, Berenguel RC, Tonelotto J, Kopelman BI: Differences in pain expression between male and female newborn infants. Pain 85: 127–133, 2000. [DOI] [PubMed] [Google Scholar]
- [23].Hamberg K: Gender bias in medicine. Women’s health, 4: 237–243, 2008. [DOI] [PubMed] [Google Scholar]
- [24].Hamberg K, Risberg G, Johansson EE, Westman G: Gender bias in physicians’ management of neck pain: a study of the answers in a Swedish national examination. J Women Health Gen-B 11: 653–666, 2002. [DOI] [PubMed] [Google Scholar]
- [25].Heins JK, Heins A, Grammas M, Costello M, Huang K, Mishra S: Disparities in analgesia and opioid prescribing practices for patients with musculoskeletal pain in the emergency department. J Emerg Nurs 32: 219–224, 2006. [DOI] [PubMed] [Google Scholar]
- [26].Hirsh AT, George SZ, Robinson ME: Pain assessment and treatment disparities: a virtual human technology investigation. Pain 143: 106–113, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Hirsh AT, Hollingshead NA, Matthias MS, Bair MJ, Kroenke K: The influence of patient sex, provider sex, and sexist attitudes on pain treatment decisions. J Pain 15: 551–559, 2014. [DOI] [PubMed] [Google Scholar]
- [28].Hoffmann DE, Tarzian AJ: The girl who cried pain: a bias against women in the treatment of pain. J Law Med Ethics 28: 13–27, 2001. [DOI] [PubMed] [Google Scholar]
- [29].Hollingshead NA, Matthias MS, Bair MJ, Hirsh AT: Impact of race and sex on pain management by medical trainees: A mixed methods pilot study of decision making and awareness of influence. Pain Med 16: 280–290, 2015. [DOI] [PubMed] [Google Scholar]
- [30].Jussim L, Crawford JT, Rubinstein RS: Stereotype (in) accuracy in perceptions of groups and individuals. Curr Dir Psychol Sci 24: 490–497, 2015. [Google Scholar]
- [31].Kappesser J, Williams ACdC: Pain estimation: asking the right questions. Pain 148: 184–187, 2010. [DOI] [PubMed] [Google Scholar]
- [32].Keefe FJ, Lefebvre JC, Egert JR, Affleck G, Sullivan MJ, Caldwell DS: The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: the role of catastrophizing. Pain 87: 325–334, 2000. [DOI] [PubMed] [Google Scholar]
- [33].Kennedy J, Roll JM, Schraudner T, Murphy S, McPherson S: Prevalence of persistent pain in the US adult population: new data from the 2010 national health interview survey. J Pain 15: 979–984, 2014. [DOI] [PubMed] [Google Scholar]
- [34].Kest B, Sarton E, Dahan A, Fisher DM: Gender Differences in Opioid-Mediated Analgesia: animal and human studies. The Journal of the American Society of Anesthesiologists 93: 539–547, 2000. [DOI] [PubMed] [Google Scholar]
- [35].Lucey P, Cohn JF, Prkachin KM, Solomon PE, Matthews I: Painful data: The UNBC-McMaster shoulder pain expression archive database. Face and Gesture 2011: 57–64. IEEE, 2011. [Google Scholar]
- [36].Martel MO, Thibault P, Sullivan MJL: Judgments about pain intensity and pain genuineness: the role of pain behavior and judgmental heuristics. J Pain 12: 468–475, 2011. [DOI] [PubMed] [Google Scholar]
- [37].Mehlsen M, Hegaard L, Ørnbøl E, Jensen JS, Fink P, Frostholm L: The effect of a lay-led, group-based self-management program for patients with chronic pain: a randomized controlled trial of the Danish version of the Chronic Pain Self-Management Programme. Pain 158: 1437, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Michael GE, Sporer KA, Youngblood GM: Women are less likely than men to receive prehospital analgesia for isolated extremity injuries. Am J Emerg Med 25: 901–906, 2007. [DOI] [PubMed] [Google Scholar]
- [39].Myers CD, Riley III JL, Robinson ME: Psychosocial contributions to sex-correlated differences in pain. Clin J Pain 19: 225–232, 2003. [DOI] [PubMed] [Google Scholar]
- [40].Nahin RL: Estimates of pain prevalence and severity in adults: United States, 2012. J Pain 16: 769–780, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Paradis CM, Horn L, Yang C-M, O’Rourke T: Ethnic differences in assessment and treatment of affective disorders in a jail population. J Offender Rehabil 28: 23–32, 1999. [Google Scholar]
- [42].Parker G, Blanch B, Crawford J: Does gender influence response to differing psychotherapies by those with unipolar depression? J Affect Disorders 130, 17–20, 2011. [DOI] [PubMed] [Google Scholar]
- [43].Pollack W. 1998: Real boys: Rescuing our sons from the myths of boyhood New York: Henry Holt and Company. Inc [Google Scholar]
- [44].Prkachin KM: The consistency of facial expressions of pain: a comparison across modalities. Pain 51: 297–306, 1992. [DOI] [PubMed] [Google Scholar]
- [45].Prkachin KM, Berzins S, Mercer SR: Encoding and decoding of pain expressions: a judgement study. Pain 58: 253–259, 1994. [DOI] [PubMed] [Google Scholar]
- [46].Prkachin KM, Mass H, Mercer SR: Effects of exposure on perception of pain expression. Pain 111: 8–12, 2004. [DOI] [PubMed] [Google Scholar]
- [47].Prkachin KM, Solomon PE: The structure, reliability and validity of pain expression: Evidence from patients with shoulder pain. Pain 139: 267–274, 2008. [DOI] [PubMed] [Google Scholar]
- [48].Raftery KA, Smith-Coggins R, Chen AH: Gender-associated differences in emergency department pain management. Ann Emerg Med 26: 414–421, 1995. [DOI] [PubMed] [Google Scholar]
- [49].Rivera LA, Tilcsik A: Scaling down inequality: Rating scales, gender bias, and the architecture of evaluation. Am Sociol Rev 84: 248–274, 2019. [Google Scholar]
- [50].Robinson ME, Riley III JL, Myers CD, Papas RK, Wise EA, Waxenberg LB, Fillingim RB: Gender role expectations of pain: relationship to sex differences in pain. J pain 2: 251–257, 2001. [DOI] [PubMed] [Google Scholar]
- [51].Robinson ME, Wise EA: Gender bias in the observation of experimental pain. Pain 104: 259–264, 2003. [DOI] [PubMed] [Google Scholar]
- [52].Robinson ME, Wise EA: Prior pain experience: influence on the observation of experimental pain in men and women. J Pain 5: 264–269, 2004. [DOI] [PubMed] [Google Scholar]
- [53].Robinson ME, Wise EA, Gagnon C, Fillingim RB, Price DD: Influences of gender role and anxiety on sex differences in temporal summation of pain. J Pain 5: 77–82, 2004. [DOI] [PubMed] [Google Scholar]
- [54].Robinson ME, Wise EA, Riley JL III, Atchison JW: Sex differences in clinical pain: A multisample study. J Clin Psychol Med S 5: 413–424, 1998. [Google Scholar]
- [55].Safdar B, Heins A, Homel P, Miner J, Neighbor M, DeSandre P, Todd KH: Impact of physician and patient gender on pain management in the emergency department—a multicenter study. Pain med 10: 364–372, 2009. [DOI] [PubMed] [Google Scholar]
- [56].Schäfer G, Prkachin KM, Kaseweter KA, de C Williams AC: Health care providers’ judgments in chronic pain: the influence of gender and trustworthiness. Pain 157: 1618–1625, 2016. [DOI] [PubMed] [Google Scholar]
- [57].Singer T, Seymour B, O’doherty J, Kaube H, Dolan RJ, Frith CD: Empathy for pain involves the affective but not sensory components of pain. Science 303: 1157–1162, 2004. [DOI] [PubMed] [Google Scholar]
- [58].Solomon P: Congruence between health professionals’ and patients’ pain ratings: a review of the literature. Scand J Caring Sci 15: 174–180, 2001. [DOI] [PubMed] [Google Scholar]
- [59].Staczan P, Schmuecker R, Koehler M, Berglar J, Crameri A, von Wyl A, Koemeda-Lutz M, Schulthess P, Tschuschke V: Effects of sex and gender in ten types of psychotherapy. Psychother Res 27: 74–88, 2017. [DOI] [PubMed] [Google Scholar]
- [60].Sullivan MJ, Tripp DA, Santor D: Gender differences in pain and pain behavior: the role of catastrophizing. Cognitive Ther Res 24: 121–134, 2000. [Google Scholar]
- [61].Thorn BE, Clements KL, Ward LC, Dixon KE, Kersh BC, Boothby JL, Chaplin WF: Personality factors in the explanation of sex differences in pain catastrophizing and response to experimental pain. Clin J Pain 20: 275–282, 2004. [DOI] [PubMed] [Google Scholar]
- [62].Vachon-Presseau E, Roy M, Woo C-W, Kunz M, Martel M-O, Sullivan MJ, Jackson PL, Wager TD, Rainville P: Multiple faces of pain: effects of chronic pain on the brain regulation of facial expression. Pain 157: 1819, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Wandner LD, Heft MW, Lok BC, Hirsh AT, George SZ,Horgas AL, Atchison JW, Torres CA, Robinson ME: The impact of patients’ gender, race, and age on health care professionals’ pain management decisions: an online survey using virtual human technology. Int J Nurs Stud 51: 726–733, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Wandner LD, Scipio CD, Hirsh AT, Torres CA, Robinson ME: The perception of pain in others: how gender, race, and age influence pain expectations. J Pain 13: 220–227, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Weisse CS, Sorum PC, Sanders KN, Syat BL: Do gender and race affect recommendations about pain treatment? J Gen Intern Med 16: 211–217, 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Wise EA, Price DD, Myers CD, Heft MW, Robinson ME: Gender role expectations of pain: relationship to experimental pain perception. Pain 96: 335–342, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Xu X, Zuo X, Wang X, Han S: Do you feel my pain? Racial group membership modulates empathic neural responses. J Neurosci 29: 8525–8529, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Zaki J, Bolger N, Ochsner K: It takes two: The interpersonal nature of empathic accuracy. Psychol sci 19: 399–404, 2008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


