Abstract
Mortality associated with pancreatic cancer is among the highest of all malignancies, with a 5-year overall survival of 5–10%. Immunotherapy, represented by the blocking antibodies against programmed cell death protein 1 or its ligand 1 (anti-PD-(L)1), has achieved remarkable success in a number of malignancies. However, due to the immune-suppressive tumor microenvironment, the therapeutic efficacy of anti-PD-(L)1 in pancreatic cancer is far from expectation. To address such a fundamental issue, chemotherapy, radiotherapy, targeted therapy and even immunotherapy itself, have individually been attempted to combine with anti-PD-(L)1 in preclinical and clinical investigation. This review, with a particular focus on pancreatic cancer therapy, collects current anti-PD-(L)1-based combination strategy, highlights potential adverse effects of accumulative combination, and further points out future direction in optimization of combination, including targeting post-translational modification of PD-(L)1 and improving precision of treatment.
Keywords: Pancreatic cancer, Immune checkpoint inhibitor, PD-1, PD-L1, Combinational therapy, Systematic treatment, Post-translational modification, Precision therapy
Background
Mortality associated with pancreatic cancer (PC) is among the highest of all cancers, with a 5-year overall survival (OS) of only 5–10% and the highest incidence-to-mortality ratio of any solid tumor [1, 2]. It is anticipated that it will be the second greatest cause of cancer-related death by 2030 [3]. Because of the difficulties of early detection, the invasion of major blood vessels, aggressive biology characterized by early metastasis, and the wasting syndrome cachexia, the majority of patients with PC cannot undergo surgical resection, or relapse after surgery [4, 5]. Therefore, effective systemic treatments are urgently required. Although the mainstay of treatments for locally advanced or metastatic PC rely on systemic combination chemotherapy, specifically gemcitabine plus nab-paclitaxel or FOLFIRINOX (fluorouracil, leucovorin, irinotecan, and oxaliplatin) or modified FOLFIRINOX, survival has remained poor because of chemotherapeutic resistance, poor performance in patients, and the lack of biomarkers to match patients who tend to benefit from specific chemotherapeutic agents [6, 7].
Cancer immunotherapy has proved to be remarkably efficacious in a variety of malignancies. Traditionally, it aims to activate and increase the anti-tumor immune response in terms of both quantity and quality, which are generally categorized into two strategies [8]. The first category is passive immunotherapy, in which effector cells or molecules of the immune system directly attack tumor cells. Antibody-targeted therapy, antibody-drug conjugates, adoptive immune cell therapies, and engineered T cells such as chimeric antigen receptor (CAR) T cell and T cell receptor (TCR) T cell therapies are typical strategies [9, 10]. The second category is active immunotherapy, in which endogenous immune regulatory mechanisms are modulated to enhance anti-tumor immune activation. Using cancer vaccines and other agents are typical strategies, that enhance antigen uptake, processing, and presentation to T cells by antigen-presenting cells (APCs), enhancing the activation and expansion of naive T cells and effector T cells (Teffs) [11].
Over the last decade, monoclonal antibodies targeting programmed cell death protein 1 (PD-1, also known as PDCD1 and CD279) or programmed cell death ligand 1 (PD-L1, also known as CD274 and B7-H1) to restore tumor-induced immune deficiency have emerged as a promising treatment. Unlike previous immune enhancement strategies, anti-PD-(L)1 therapies block cancer immune evasion mechanisms, thereby promoting anti-tumor immune normalization [12]. Physiologically, the PD-L1-PD-1 axis attenuates the local T cell response and maintains immune homeostasis, signaling that cancers exploit to evade the anti-tumor immune response, and to facilitate tumor growth, progression, and metastasis [13, 14]. Therefore, blocking PD-(L)1 harnesses the endogenous anti-tumor response to fight cancer. This strategy has achieved a higher objective response rate (ORR) with considerably fewer immune-related adverse events (irAEs) in patients [8].
The PD-1 inhibitors currently approved by the US Food and Drug Administration (FDA) include pembrolizumab, nivolumab, and cemiplimab-rwlc. PD-L1 inhibitors approved by the FDA include atezolizumab, avelumab, and durvalumab [15]. These represent monoclonal antibodies that have demonstrated treatment efficacy against various solid and hematologic malignancies, including melanoma, non-small-cell lung cancer, head and neck squamous cell carcinoma, renal cell carcinoma, Hodgkin lymphoma, bladder cancer, and Merkel cell carcinoma [16, 17]. Nevertheless, the majority of PCs are resistant to anti-PD-(L)1 therapy due to their non-inflamed phenotype, namely immune-desert and immune-excluded phenotypes [18]. These tumors are characterized by a suppressive tumor microenvironment (TME) with low infiltration of Teffs combined with high infiltration of regulatory T cells (Tregs), tumor-associated macrophages (TAMs), and myeloid-derived suppressor cells (MDSCs). In addition, the dense fibrous stroma of a PC tumor impedes drug delivery and access of Teffs to its interior [11, 19]. A multicenter phase I trial in 2012 treated 207 cancer patients with an anti-PD-L1 antibody. Of 14 PC patients, no objective response was observed [20]. Another phase I trial which aimed to validate anti-PD-L1 (MPDL3280A) therapy included 1 PC patient who did not respond [21]. The greatest efficacy for the treatment of PC was reported from a phase I trial of pembrolizumab alone in which one patient achieved disease-free progression for 20 weeks [22]. Therefore, to overcome resistance to anti-PD-(L)1 monotherapy and integrate different anti-tumor therapeutic mechanisms, a variety of preclinical and clinical studies have been conducted to validate combining an anti-PD-(L)1 agent with chemotherapy, radiotherapy, targeted therapies, or other immunotherapies. The mechanisms and the details of preclinical trials, cases, and clinical trials (Table 1), including ongoing trials (Table 2), of various combinations are reviewed hereafter.
Table 1.
Published clinical trials using anti-PD-(L)1 combination therapy
| Publication year | Study phase | PC stage | Treatment line | Treatment regimens | Number of PC pts | Efficacy |
|---|---|---|---|---|---|---|
| Combination with chemotherapy | ||||||
| 2017 | Ib/II | metastatic | 1 / 2 | pembrolizumab + gemcitabine, nab-paclitaxel | 17 | (Among the 11 chemotherapy naïve pts.) DCR 100%; mPFS 9.1 m, mOS 15.0 m |
| 2020 | I | locally advanced / metastatic | 1 / 2 | nivolumab + gemcitabine, nab-paclitaxel | 50 | (Among the 50 chemotherapy naïve pts.) ORR 18%, DCR 64%; mPFS 5.5 m, mOS 9.9 m |
| 2020 | / (case) | metastatic | 1 | toripalimab + gemcitabine, nab-paclitaxel | 1 | PR for at least 8 cycles |
| Combination with radiotherapy | ||||||
| 2019 | I/II | borderline resectable / locally advanced | 2 | durvalumab + stereotactic ablative radiotherapy | 15 | 6 underwent R0 resection |
| 2018 | I | metastatic | ≥ 2 | pembrolizumab + hypofractionated radiotherapy | 4 | all PD |
| 2017 | Ib/II (randomized controlled study) | resectable / borderline resectable | 1 | pembrolizumab + radiation + capecitabine | 22 (14 pts. in the triple therapy arm) | 71% underwent surgery (compared to 50% in the arm only receiving capecitabine and radiation) |
| Combination with molecularly targeted therapy | ||||||
| 2019 | II | metastatic | 1 | nivolumab + gemcitabine, nab-paclitaxel, cisplatin + paricalcitol | 24 | 19 PR, 2 SD and 2 PD; mPFS 8.17 m, mOS 15.3 m |
| 2018 | I | locally advanced / metastatic | M7824 (a bifunctional fusion protein of anti-PD-L1 antibody fused to the extracellular domain of TGF-β receptor II) | 5 | 1 durable PR (with dMMR), 1 prolonged SD | |
| 2019 | Ib | metastatic | durvalumab + galunisertib (TGF-β receptor I kinase inhibitor) | 32 | 1 PR, 7 SD; mPFS 1.9 m | |
| 2017 | I | advanced | ≥ 2 | nivolumab + cabiralizumab (anti-CSF1R antibody) | 31 | 3 PR (293, 275+, and 168+ days on study), 1 prolonged SD (182 d); 6-month DCR 13%, ORR 10% |
| 2018 | Ib/II | advanced | spartalizumab (anti-PD-1 antibody) + lacnotuzumab (anti-CSF1R antibody) | 30 | 1 PR (on study for 346 d), 2 durable SD (on study for 328 d and 319 d) | |
| 2021 | Ib | metastatic | 1 | nivolumab + APX005M (sotigalimab, CD40 agonist) + gemcitabine, nab-paclitaxel | 12 | 8 PR, 3 SD; mPFS 10.8 m (0.1 mg/kg APX005M) / 12.4 m (0.3 mg/kg APX005M) |
| 2020 | I/II | metastatic | 3 mean lines of prior treatment | pembrolizumab + NOX-A12 (CXCL12 inhibitor) | 9 | (among 11 colorectal cancer pts. and 9 PC pts.) 25% SD; mPFS 1.87 m, 6-month OS 42%, 12-month OS 22% |
| 2019 | IIb | metastatic | 2 mean lines of prior treatment | pembrolizumab + BL-8040 (CXCR4 antagonist) | 15 | 1 PR, 2 SD, DCR 21.4%; mOS 7 m |
| 2020 | IIa | metastatic | ≥ 2 | pembrolizumab + BL-8040 (CXCR4 antagonist) | 37 | (Among the 29 chemotherapy-resistant evaluable pts.) 1 PR, 9 SD, DCR 34.5%; mOS 3.3 m |
| 2 | pembrolizumab + BL-8040 (CXCR4 antagonist) + liposomal irinotecan, fluorouracil, leucovorin | 22 | ORR 32%, DCR 77%; median duration of response 7.8 m | |||
| 2018 | I | ? | pembrolizumab + defactinib (FAK inhibitor) + gemcitabine | 8 | 1 PR; median time on treatment 127 d | |
| 2020 | II (randomized controlled study) | locally advanced / metastatic | ≥ 2 | pembrolizumab + acalabrutinib (BTK inhibitor) | 77 (40 pts. in the combination therapy arm) | ORR 7.9%, DCR 21.1% |
| 2017 | Ib | advanced | BGB-A317 (anti-PD-1 antibody) + BGB-290 (PARP 1 / 2 inhibitor) | ? (38 pts. in all, including ovarian, breast, prostate, pancreatic cancers, etc.) | (among PC pts.) 1 PR, 2 SD (received the combination therapy for 189 d and 281 d) | |
| 2019 | Ib | advanced | dostarlimab (PD-1 inhibitor) + niraparib (PARP inhibitor) + bevacizumab | ? | 1 SD in a PC pt | |
| Combination with immunotherapy | ||||||
| 2020 | / (cases) | relapsed / refractory | complicated | nivolumab + ipilimumab | 5 | (among 3 evaluable pts.) 1 CR (with BRCA1), 1 PR (with RAD51C) |
| 2019 | II | metastatic | ≥ 2 | nivolumab + ipilimumab + radiation | 25 | ORR 13%, DCR 20% |
| 2018 | II (randomized controlled study) | metastatic | ≥ 2 | durvalumab + tremelimumab | 64 (32 pts. in the combination therapy arm) | DCR 9.4%; mPFS 1.5 m, mOS 3.1 m |
| 2018 | II | metastatic | 1 | durvalumab + tremelimumab + gemcitabine, nab-paclitaxel | 11 | PR 73%, DCR 100%; mPFS 7.9 m, 6-month survival 80% |
| 2018 | I | advanced | ≥ 2 | pembrolizumab + epacadostat (IDO1 inhibitor) | 1 | PR (on treatment at 21 w) |
| 2019 | I | advanced | atezolizumab + navoximod (IDO1 inhibitor) | 1 | PR | |
| 2015 | / | metastatic | 2 | antigen-primed MoDCs modified by PD-L1 blockade | 10 | 5 pts. (didn’t respond to MoDC alone) achieved secondary stabilization (4 m to 8 m) by using MoDCs modified by PD-L1 blockade |
| 2016 | / | metastatic | nivolumab + antigen-primed MoDCs | 7 | 2 PR | |
| 2019 | Ib | advanced | 2 | pembrolizumab + pelareorep (oncolytic reovirus) + chemotherapy | 11 | (among 10 efficacy-evaluable pts.) 1 PR for 17.4 m, 2 SD lasting 9 m and 4 m |
Abbreviations: BTK, Bruton’s tyrosine kinase; CSF1R, colony-stimulating factor 1 receptor; CXCL12, CXC-chemokine ligand 12; CXCR4, CXC-chemokine receptor 4; DCR, disease control rate; dMMR, mismatch repair-deficient; FAK, focal adhesion kinase; IDO1, indoleamine 2,3-dioxygenase 1; MoDC, monocyte-derived dendritic cell; ORR, overall response rate; OS, overall survival; PARP, poly ADP-ribose polymerase; PC, pancreatic cancer; PD, progressive disease; PD-(L)1, programmed cell death (ligand) 1; PFS, progression-free survival; PR, partial response; pts., patients; SD, stable disease; TGF-β, transforming growth factor-β
Table 2.
Ongoing clinical trials using anti-PD-(L)1 combination therapiesa
| Anti-PD-(L)1 regimen | Combination regimens | PC stage | Treatment line | Primary outcomes | Study phase | Trial ID |
|---|---|---|---|---|---|---|
| nivolumab | FOLFIRINOX | resectable / borderline resectable | 1 | clinically relevant pancreatic fistula in the post-operative period, pCR | I/II | NCT03970252 |
| SBRT | locally advanced | 2 | incidence of TRAEs, incidence of laboratory abnormalities | I/II | NCT04098432 | |
| irreversible electroporation + CpG (toll-like receptor 9 ligand) | metastatic | ≥ 2 | TRAEs | I | NCT04612530 | |
| irreversible electroporation | ||||||
| SX-682 (CXCR1 / 2 inhibitor) | metastatic | ≥ 2 | MTD | I | NCT04477343 | |
| cabiralizumab (CSF1R inhibitor) + gemcitabine | metastatic | 2 | PFS | II | NCT03697564 | |
| APX005M (CD40 agonist) + GA | metastatic | 1 | number and percentage of subjects with AEs, SAEs, DLTs; OS | Ib/II | NCT03214250 | |
| entinostat (class I histone deacetylases inhibitor) | advanced | ORR | II | NCT03250273 | ||
| TPST-1120 (peroxisome proliferator activated receptor alpha antagonist) | advanced | incidence of DLTs, TEAEs; MTD | I | NCT03829436 | ||
| autologous dendritic cell vaccine loaded with personalized peptides + gemcitabine, capecitabine | resectable | number of cases for which vaccine is produced, AEs | Ib | NCT04627246 | ||
| KRAS peptide vaccine + ipilimumab | resected | number of participants experiencing DRTs, fold change in interferon-producing mutant-KRAS-specific CD8 and CD4 T cells at 16 w | I | NCT04117087 | ||
| GVAX + SBRT + cyclophosphamide | borderline resectable | no more than 1 month / cycle (28 days) of systemic therapy | CD8 count in the TME | II | NCT03161379 | |
| GVAX + cyclophosphamide | resectable | 1 | median IL-17A expression in vaccine-induced lymphoid aggregates found in surgically resected PC | I/II | NCT02451982 | |
| GVAX + urelumab (CD137 agonist) + cyclophosphamide | ||||||
| GVAX + BMS-813160 (CCR2 / CCR5 antagonist) + SBRT | locally advanced | 1 | number of participants experiencing DRTs, percentage of participants who achieve an immune response (> 80% increase of infiltration of CD8 + CD137+ T cells into the tumor) | I/II | NCT03767582 | |
| BMS-813160 + SBRT | ||||||
| ipilimumab + CRS-207 (live, attenuated Listeria monocytogenes-expressing mesothelin) + GVAX + cyclophosphamide | metastatic | ORR | II | NCT03190265 | ||
| ipilimumab + CRS-207 | ||||||
| GRT-C903 (shared neoantigen cancer vaccine prime) + GRT-R904 (shared neoantigen cancer vaccine boost) + ipilimumab | advanced | 2 | incidence of AEs, SAEs, DLTs; RP2D of GRT-C903 and GRT-R904; ORR in phase 2 | I/II | NCT03953235 | |
| pembrolizumab | INT230–6 (comprised of 3 agents: cisplatin, vinblastine sulfate, and a cell permeation enhancer) | advanced | no limit | rate and severity of ≥ grade 3 TEAEs | I/II | NCT03058289 |
| PEGPH20 | metastatic | 2 | PFS | II | NCT03634332 | |
| efineptakin alfa (NT-I7, long-acting human IL-7) | advanced | 2 | incidence, nature and severity of AEs, incidence and nature of DLTs, MTD and RP2D of NT-I7; ORR in phase IIa | Ib/IIa | NCT04332653 | |
| GB1275 (modulator of CD11b) | metastatic | incidence of DLTs, AEs; maximum plasma concentration, trough plasma concentration, time of maximum observed plasma concentration, terminal phase elimination half-life, area under the plasma concentration-time curve, oral clearance of GB1275; ORR in phase II | I/II | NCT04060342 | ||
| ENB003 (endothelin B receptor antagonist) | metastatic | ≥ 2 | incidence of TEAEs, ORR | Ib/IIa | NCT04205227 | |
| itacitinib (INCB039110, JAK1 inhibitor) | advanced | frequency, duration, and severity of AEs | Ib | NCT02646748 | ||
| INCB050465 (PI3K-delta inhibitor) | ||||||
| lenvatinib | advanced | ≥ 2 | ORR; percentage of participants who experience an AE or discontinue treatment due to an AE | II | NCT03797326 | |
| Debio 1143 (a second mitochondrial-derived activator of caspases mimetic designed to promote apoptosis) | Stage III or IV | ≥ 2 | MTD, RP2D, extension part ORR | I | NCT03871959 | |
| defactinib (focal adhesion kinase inhibitor) | advanced | ≥ 2 | AEs, MTD | I/IIa | NCT02758587 | |
| defactinib + gemcitabine | advanced | 2 | RP2D (determined from MTD) | I | NCT02546531 | |
| defactinib + chemotherapy | resectable | 1 | pCR rate | II | NCT03727880 | |
| olaparib (PARP inhibitor) + GAX-CI (gemcitabine, nab-paclitaxel, capecitabine, cisplatin, and irinotecan) | metastatic | 1 | PFS after 6 m | II | NCT04753879 | |
| ipilimumab + anetumab ravtansine (an anti-mesothelin antibody conjugated to the maytansinoid tubulin inhibitor DM4) | advanced | ≥ 2 | MTD | I | NCT03816358 | |
| anetumab ravtansine + gemcitabine | ||||||
| GVAX + IMC-CS4 (LY3022855, anti-CSF1R antibody) + cyclophosphamide | borderline resectable | CD8 T cell density in the primary tumor, number of participants experiencing DRTs | I | NCT03153410 | ||
| epacadostat + GVAX + cyclophosphamide | metastatic | ≥ 2 | recommended dose of epacadostat; 6-month survival | II | NCT03006302 | |
| epacadostat + CRS-207 (live, attenuated Listeria monocytogenes-expressing mesothelin) | ||||||
| GVAX + cyclophosphamide + SBRT | locally advanced | ≥ 2 | distant metastasis free survival | II | NCT02648282 | |
| p53MVA vaccine | advanced | ≥ 2 or refuse standard treatment | tolerability of the combination | I | NCT02432963 | |
| mRNA-5671/V941 | advanced | DLTs, AEs, discontinuations | I | NCT03948763 | ||
| pembrolizumab (local delivery via trans-artery or intra-tumor injection) | ipilimumab (local delivery via trans-artery or intra-tumor injection) | advanced | OS, CR rate before or at 6 m | II/III | NCT03755739 | |
| spartalizumab | NIS793 (anti-TGF-β antibody) | advanced | incidence of DLTs, AEs, SAEs, dose reductions/interruptions | I | NCT02947165 | |
| NIS793 + GA | metastatic | 1 | incidence of DLTs, incidence and severity of TEAEs and SAEs, dose interruptions / reductions, dose intensity; PFS | II | NCT04390763 | |
| canakinumab (ACZ885, anti-IL-1β antibody) + GA | metastatic | 1 | recommended phase 2 / 3 dose | Ib | NCT04581343 | |
| dostarlimab | niraparib (PARP inhibitor) | metastatic | 2 or 3 | DCR at 12w | II | NCT04493060 |
| sintilimab | mFOLFIRINOX | metastatic | 1 or 2 | OS | III | NCT03977272 |
| toripalimab | mFOLFIRINOX | borderline resectable / locally advanced | PFS | III | NCT03983057 | |
| anlotinib + nab-paclitaxel | locally advanced / metastatic | 2 | PFS | II | NCT04718701 | |
| camrelizumab | GA | metastatic | 1 | PFS | III | NCT04674956 |
| GA | metastatic | ORR, PFS | II | NCT04498689 | ||
| plerixafor (AMD3100, CXCR4 antagonist) | metastatic | ≥ 2 | ORR | II | NCT04177810 | |
| zimberelimab | AB680 (CD73 inhibitor) + GA | metastatic | number of participants with TEAEs | I | NCT04104672 | |
| unknown PD-1 antibody | radiotherapy | advanced | local control | II | NCT03374293 | |
| GA + manganese | locally advanced / metastatic | number of subjects with TRAEs, DCR | I/II | NCT03989310 | ||
| GA | ||||||
| LYT-200 (galectin-9 inhibitor) + GA | metastatic | incidence of TEAEs and DLTs, PFS, ORR | I/II | NCT04666688 | ||
| apatinib (VEGFR-2 tyrosine kinase inhibitor) + radiation | advanced | PFS | / | NCT04365049 | ||
| mutant KRAS G12V-specific TCR transduced autologous T cells + cyclophosphamide, fludarabine | advanced | frequency and severity of TRAEs, ORR | I/II | NCT04146298 | ||
| durvalumab | danvatirsen (antisense oligonucleotide targeting signal transducer and activator of transcription 3) | refractory / stage II / stage III / stage IV | incidence of AEs, SAEs; physiological parameters; incidence of TEAEs and deaths; PD-L1 expression; phosphorylated or total STAT3 expression levels; characterization of immune infiltrates; quantification and characterization of CD8 staining pattern; PD-L1 protein levels in the membrane of circulating tumor cells; physical examinations | II | NCT02983578 | |
| olaparib (PARP inhibitor) | advanced | changes in genomic and immune biomarkers | II | NCT03851614 | ||
| cediranib (inhibitor of VEGFR tyrosine kinases) | ||||||
| tremelimumab + SBRT | advanced | ≥ 2 | number of AEs with grade 1–5 | I/II | NCT02311361 | |
| SBRT | ||||||
| CV301 (poxviral-based vaccine) + capecitabine | metastatic | 2 | RP2D of durvalumab, 8.5-month PFS rate, 4-month PFS rate | I/II | NCT03376659 | |
| atezolizumab | BDB001 (Toll-like receptor agonist) + radiotherapy | metastatic | DCR within 24 w | II | NCT03915678 | |
| KY1044 (anti-ICOS antibody) | advanced | incidence and severity of AEs and SAEs; number of dose interruptions, reductions and dose intensity; ORR | I/II | NCT03829501 | ||
| personalized neoantigen tumor vaccines + mFOLFIRINOX | resectable | 1 | DRT | I | NCT04161755 | |
| LOAd703 (oncolytic adenovirus encoding TMZ-CD40L and 4-1BBL) + GA | advanced | number of patients with DLTs | I/IIa | NCT02705196 | ||
| avelumab | binimetinib (MEK inhibitor) + talazoparib (PARP inhibitor) | locally advanced / metastatic | 2 or 3 | DLT, confirmed objective response | Ib/II | NCT03637491 |
| binimetinib | ||||||
| ETBX-011 (vaccine inducing CEA-specific cytotoxic T-cell activity) + GI-4000 (vaccine expressing mutant Ras proteins) + haNK + ALT-803 (IL-15 superagonist) + bevacizumab + aldoxorubicin HCl, capecitabine, cyclophosphamide, fluorouracil, leucovorin, nab-paclitaxel, omega-3-acid ehtyl esters, oxaliplatin + SBRT | advanced | ≥ 2 | incidence of TEAEs and SAEs, ORR | Ib/II | NCT03387098b | |
| ETBX-011 + ETBX-021 (HER2) + ETBX-051 (Brachyury) + ETBX-061 (MUC1) + GI-4000 + GI-6207 (CEA yeast) + GI-6301 (Brachyury yeast) + haNK + ALT-803 + bevacizumab + aldoxorubicin HCl, capecitabine, cyclophosphamide, fluorouracil, leucovorin, nab-paclitaxel, oxaliplatin + SBRT | advanced | ≥ 2 | incidence of TEAEs and TESAEs, ORR | Ib/II | NCT03586869 | |
| LY3300054 (anti-PD-L1 antibody) | merestinib (multikinase inhibitor) | locally advanced / metastatic | 1 | number of participants with LY3300054 DLTs | I | NCT02791334 |
| SHR-1701 (PD-L1/TGF-β bsAb) | GA | advanced | 1 | RP2D, ORR | Ib/II | NCT04624217 |
| PD-L1/CTLA-4 bsAb | / | locally advanced / metastatic | 2 | ORR | I/II | NCT04324307 |
| GA | 1 | |||||
| FOLFIRINOX | 1 | |||||
| PD-L1 targeting haNK | N-803 (IL-15 superagonist) + SBRT + cyclophosphamide, gemcitabine, nab-paclitaxel, aldoxorubicin HCl | locally advanced / metastatic | ≥ 2 | PFS | II | NCT04390399 |
aAbbreviations: AE, adverse effect; bsAb, bispecific antibody; CR, complete response; DCR, disease control rate; DLT, dose-limiting toxicity; DRT, drug-related toxicity; FOLFIRINOX, fluorouracil, leucovorin, irinotecan, and oxaliplatin; GA, gemcitabine, nab-paclitaxel; GVAX, granulocyte-macrophage colony-stimulating factor-secreting PC vaccine; haNK, high-affinity natural killer; mFOLFIRINOX, modified FOLFIRINOX; MTD, maximum tolerated dose; ORR, overall response rate; OS, overall survival; PARP, poly (ADP-ribose) polymerase; PC, pancreatic cancer; pCR, pathologic complete response; PD-(L)1, programmed cell death (ligand) 1; PEGPH20, PEGylated recombinant hyaluronidase PH20; PFS, progression-free survival; RP2D, recommended phase 2 dose; SAE, severe adverse effect; SBRT, stereotactic body radiation therapy; TEAE, treatment-emergent adverse event; TESAE, treatment-emergent severe adverse event; TME, tumor microenvironment; TRAE, treatment-related adverse event; VEGFR, vascular endothelial growth factor receptor
bThis group also initiated 2 studies exploring combination therapies without aldoxorubicin HCl, or without aldoxorubicin HCl + omega-3-acid ethyl esters + SBRT (other regimens are the same; trial ID NCT03329248; NCT03136406)
Combination with chemotherapy
In patients with locally advanced or metastatic PC, gemcitabine plus nab-paclitaxel, FOLFIRINOX, and modified FOLFIRINOX are considered first-line treatment regimens for those with good performance status [23, 24]. While nab-paclitaxel has been shown to enhance the release of granzyme B by effector cells and cause the desmoplastic stroma to increase intratumoral gemcitabine penetration, gemcitabine can increase antigen presentation by upregulating major histocompatibility complex (MHC) class I expression and promote dendritic cell maturation [25, 26]. Moreover, FOLFIRINOX has been shown to reduce human leukocyte antigen-A defects, increase CD8+ cell numbers, and decrease Treg and M2 macrophage density [27]. The expression of the immunosuppressive gene CXCL5 has been shown to be reduced after delivering FOLFIRINOX [28]. These findings demonstrate that in addition to a direct cytotoxic effect on cancer cells, PC chemotherapy may promote immunogenic cell death (ICD), which provides the foundation for combination therapy with an anti-PD-(L)1 agent. Significantly, PD-L1 expression may be influenced by the type of chemotherapy and the response to treatment, which in return will influence the efficacy of an anti-PD-(L)1 combination therapy [29–31].
Preclinical studies have provided supporting evidence for combining anti-PD-(L)1 therapy with chemotherapy for PC. In a transgenic mouse model of resectable PC, a neoadjuvant PD-1 antagonist (150 mg/mouse at day 0, 3, 6; clone RMP1–14) with gemcitabine (100 mg/kg at day 0, 3, 6) resulted in significantly improved survival compared with neoadjuvant gemcitabine alone. Following combination therapy, tumor infiltration by neoantigen-specific CD8+ T lymphocytes against the marker neoepitope LAMA4-G1254V and CD103+CD8+ T cells increased, confirming local T cell activation [32]. In an additional study using a syngeneic subcutaneous PC mouse model, the anti-tumor properties of gemcitabine (60 μg/g Q3D, 0–2 weeks) were enhanced by combining with delayed 2-week PD-L1 blockade (0.3 mg TIW, 2–4 weeks). Furthermore, gemcitabine (using the same dosing strategy) with simultaneous and subsequent 4-week PD-L1 blockade (0.3 mg TIW, 0–4 weeks) displayed a substantial synergistic anti-tumor effect and resulted in complete response (CR) [33]. Moreover, in a syngeneic orthotopic PC mouse model, the combination of PD-L1 blockade (100 μg BIW for 2 weeks, clone 10F.9G2) with urokinase plasminogen activator receptor-targeted iron oxide nanoparticles loaded with cisplatin (10 mg/kg drug equivalent) decreased tumor burden by ~ 65% [34]. In a syngeneic subcutaneous PC mouse model, the combination of the novel taxoid DHA-SBT-1214 (25 mg/kg QW for 6 weeks) and anti-PD-L1 antibody (200 μg BIW for 3 weeks, clone 10F.9G2) also resulted in enhanced CD8+ T cell infiltration that provided therapeutic effects [35].
When used clinically, the addition of pembrolizumab to chemotherapy has displayed slightly improved efficacy. In a single-center phase Ib/II study, 11 chemotherapy-naive metastatic PC patients were administered gemcitabine (1000 mg/m2 on day 1 and 8 every 3 weeks), nab-paclitaxel (125 mg/m2 on day 1 and 8 every 3 weeks), and pembrolizumab (2 mg/kg Q3W). Their median progression-free survival (mPFS) and median overall survival (mOS) were 9.1 and 15.0 months, respectively. The disease control rate (DCR) was 100%, within which 3 patients displayed a partial response (PR) for 8+, ~ 11, and 15 months. In that study, DNA copy number instability was considered prognostic for OS [36]. However, disappointing outcomes were observed in a phase I study combining nivolumab (3 mg/kg on day 1 and 15 every 4 weeks) with gemcitabine (1000 mg/m2 on day 1, 8, 15 every 4 weeks) and nab-paclitaxel (125 mg/m2 on day 1, 8, 15 every 4 weeks) in patients with locally advanced or metastatic PC. Of the 50 treated patients, mPFS and mOS were 5.5 and 9.9 months, respectively. The ORR was 18% (1 CR and 8 PR) while DCR was 64%. These study results of efficacy did not support further investigation [37]. Additionally, PD-L1 positive expression was detected in liver metastases in a patient with metastatic PC who had received toripalimab (240 mg Q3W) and gemcitabine (1000 mg/m2 on day 1 and 8 every 3 weeks) plus nab-paclitaxel (125 mg/m2 on day 1 and 8 every 3 weeks). As a result, he experienced long-term PR (8 cycles at the time of the report) but did not suffer any grade 3 or higher toxicity [38]. A phase Ib/II study in which toripalimab, gemcitabine, and nab-paclitaxel were combined to treat patients with nonresectable PC was initiated by the same center (ChiCTR2000032293, [39]. Additionally, the author is conducting a study using sintilimab + mFOLFIRINOX for metastatic PC patients (NCT03977272), and a study using toripalimab + mFOLFIRINOX for borderline resectable or locally advanced PC patients (NCT03983057). The current ORRs are encouraging and primary endpoints are being followed up.
Tumor cells harness PD-L1 upregulation and antigen processing and presentation defects to evade immunosurveillance. Combining chemotherapies with anti-PD-(L)1 has been predicted to both induce ICD to promote antigen processing and presentation, and block the PD-L1-PD-1 interaction to improve T cell function [29]. However, the presence of rough PC TME, including dense fibrous stroma, high levels of carcinoma-associated fibroblasts (CAFs), MDSCs, and TAMs, impede the delivery and function of systemic therapeutics [40]. Optimization of the scheduling and sequencing of combination therapeutics, investigation of advanced targeting delivery systems, and testing local delivery methods are promising routes for improving the efficacy of therapies and reducing adverse effects (AEs). So far, published clinical studies that combine chemotherapies with anti-PD-(L)1 have been limited by relatively small sample sizes and the lack of comparator arms. The results of randomized controlled trials are anticipated to address the unmet clinical need in PC.
Combination with radiotherapy or other locoregional therapies
Radiotherapy (RT) is used in PC to sterilize vessel margins, promote margin-negative resection, prevent or delay local progression, palliate pain and bleeding, and relieve obstructive symptoms [41–43]. RT can induce an immune response via promotion of the production of the interferons (IFNs), cytokines, and chemokines, as well as the release of tumor antigens and damage-associated molecular patterns (DAMPs). However, the efficacy of RT alone is insufficient to radically eliminate the tumor. Combining RT with anti-PD-(L)1 may be synergistic for local and distant tumor control [44, 45].
In a preclinical study using a syngeneic orthotopic PC mouse model, the combination of anti-PD-1 antibodies (10 mg/kg) and hypofractionated RT (8 Gy × 3 fractions delivered daily for 3 days, at a dose rate of 3 Gy/minute) improved survival compared with anti-PD-1 or RT alone. The combination resulted in the greatest systemic IFN-γ response and the highest local expression of immune-activation genes, including CD28 and Icos, in all groups [46]. Azad et al. reported that the addition of anti-PD-L1 antibodies (10 mg/kg at day 0, 3, 6 and 9, administered immediately after RT; clone 10F.9G2) to high doses of RT (12 Gy or 5 × 3 Gy delivered daily until the mice were sacrificed) increased the delay in tumor growth in both KPC and Pan02-derived syngeneic subcutaneous PC mouse models. Radiosensitization following PD-L1 blockade was associated with reduced CD11b+Gr1+ myeloid cell infiltration and enhanced CD45+CD8+ T cell infiltration. T cell activation markers, including CD69, CD44, and FasL, and the CD8: Treg ratio also increased. The treatment of murine PC cells with RT upregulated PD-L1 expression in a JAK/STAT1-dependent manner [47]. Moreover, it has been reported that ablative RT promotes vessel normalization and enhances the delivery of anti-PD-L1 agents. Using a syngeneic orthotropic UN-KC6141 mouse model of PC, 67% of mice survived more than 30 days after tumor inoculation when using ablative RT (a single dose of 25 Gy) and anti-PD-L1 antibodies (10 mg/kg for 5 days), while the median survival time was 16.5 days within the control group. Furthermore, ablative RT was found to be more effective than conventional fractionated RT at recruiting T cells and combining an anti-PD-L1 agent [48]. Ataxia-telangiectasia mutated (ATM) is an apical kinase responding to ionizing radiation-induced DNA double-strand breaks. In a syngeneic subcutaneous PC mouse model, the efficacy of PD-L1 inhibition (100 μg/mouse Q3W) was demonstrated to be enhanced by the inhibition of ATM (by infecting the cells with shATM virus) and further potentiated by radiation (a single fraction of 8 Gy) with increased tumoral immunogenicity [49].
In a recent phase I/II clinic study, durvalumab (750 mg on day 1 Q2W) and stereotactic RT (6.6 Gy × 5 QOD beginning day 8) were administered to patients with locally advanced or borderline resectable PC. Of the 15 patients recruited to the study, 6 underwent surgery for whom the resections were all margin-negative, while 4 discontinued study treatments due to disease progression. No dose-limiting toxicity (DLT) was identified [50]. A case report has been published in which a patient with locally advanced PC received preoperative radiation (5 Gy × 5) and pembrolizumab (200 mg Q3W) for 4 months. After surgery, a near-complete pathological response was reported [51]. However, in a phase I trial combining pembrolizumab (200 mg Q3W, beginning 1 week before the radiation therapy) with hypofractionated radiotherapy, 4 patients with metastatic PC all displayed progressive disease (PD). Three received 8 Gy × 3 fractions while the other received a 17 Gy × 1 fraction. All RT target lesion sites metastasized within the liver rather than the pancreas [52]. The combination of chemoradiation and anti-PD-(L)1 has also been used clinically. In a randomized phase Ib/II study in which 22 patients with resectable or borderline resectable PC were recruited, 71% of patients that had received pembrolizumab (200 mg Q3W) and capecitabine (825 mg/m2 BID, Monday-Friday, on days of radiation only) with radiation (50.4 Gy in 28 fractions over 28 days) underwent surgery, compared with 50% of patients that received only capecitabine and radiation. No grade 4 toxicity was observed in the tri-combination [53].
Although RT reprograms the PC TME to exert a potent antitumor immune response, it may enhance the infiltration of Tregs and MDSCs [44]. The transient accumulation of immunosuppressive CD4+ FoxP3+ Treg after irradiation was deemed to protect the local tissue against excessive inflammation-induced tissue damage [54]. Preclinical studies have shown that increased radiation dose may in turn weaken immunogenicity [55, 56]. Moreover, while single high-dose irradiation may enhance the immune response, fractionated RT may eliminate this effect [57]. Therefore, the radiotherapy dose, fractionation, in addition to the scheduling of combining anti-PD-(L)1 into the treatment, remain challenging.
Other locoregional therapies have also been investigated in combination with anti-PD-(L)1 agents. Irreversible electroporation (IRE) is a local ablation technique that uses short high-voltage electrical pulses to induce cell death through permanent membrane lysis or loss of homeostasis [58]. The combination of IRE and anti-PD-1 (100 μg per mouse at 30 min after IRE, then QOD for 6 total injections; clone J43) was reported to promote CD8+ T cell infiltration and significantly prolong survival in a syngeneic orthotopic PC mouse model, resulting in an immune response that had long-term memory [59]. In a phase Ib trial that treated 10 locally advanced PC patients with surgically-ablative IRE followed by nivolumab (240 mg Q2W), the probability of OS was 67% after 12 months and 33% after 18 months. No DLT was observed. A multicenter phase 2 adjuvant trial using this combination is currently underway [60].
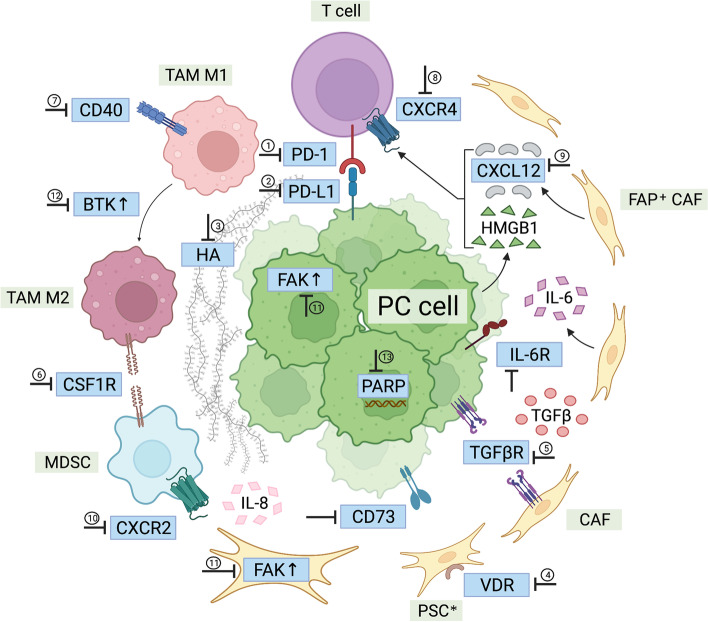
Combination with molecularly targeted therapy (Fig. 1)
Fig. 1.
Pancreatic cancer targeted therapies described in the review. ①nivolumab, pembrolizumab, toripalimab; ②durvalumab, avelumab, atezolizumab; ③PEGPH20; ④paricalcitol; ⑤galunisertib, M7824, LY2157299; ⑥cabiralizumab, lacnotuzumab; ⑦APX005M; ⑧BL-8040, AMD3100; ⑨NOX-A12; ⑩SX-682; ⑪defactinib; ⑫acalabrutinib; ⑬niraparib, BGB-290. BTK: Bruton’s tyrosine kinase; CAF: carcinoma-associated fibroblast; CSF1R: colony stimulating factor 1; CXCL12: CXC-chemokine ligand 12; CXCR2: CXC-chemokine receptor 2; CXCR4: CXC-chemokine receptor 4; FAK: focal adhesion kinase; FAP: fibroblast activation protein; HA: hyaluronic acid; HMGB1: high-mobility group protein B1; IL-6R: interleukin-6 receptor; MDSC: myeloid-derived suppressor cell; PARP: Poly (ADP-ribose) polymerase; PC: pancreatic cancer; PD-1: programmed cell death protein 1; PD-L1: programmed cell death ligand 1; PSC: pancreatic stellate cell; PSC*: activated pancreatic stellate cell; TAM: tumor-associated macrophage; TGFβR: transforming growth factor-β receptor; VDR: vitamin D receptor
Combination with agents targeting the extracellular stroma
PC is characterized by a dense fibrous stroma, consisting principally of collagen, hyaluronic acid (HA), and fibronectin [61]. It impedes blood flow, inhibits drug delivery, and suppresses the anti-tumor immune response [62]. In patients with PC, increased HA is associated with decreased survival. Depletion of HA using hyaluronidase diminishes collagen synthesis, depletes chondroitin sulfates, and remodels the stroma of the tumor [63]. In a preclinical model of cancer, the MH194 PC cell line was transfected with hyaluronan synthase-3 (HAS3) to generate a syngeneic PC mouse model with high levels of HA. By combining an anti-PD-L1 antibody (clone 10F.9G2) and PEGylated recombinant hyaluronidase PH20 (PEGPH20, 37.5 μg/kg, the human equivalent dose, 24 h prior to anti-PD-L1), inhibition of the growth of MH194/HAS3 tumors was enhanced (by 79%, p < 0.0001 compared with anti-PD-L1 or PEGPH20 alone). Similar findings were obtained when anti-PD-1 (clone RMP1–14) and PEGPH20 were combined (tumor growth inhibition: 56%, p = 0.020 and 0.017, respectively, compared with anti-PD-1 or PEGPH20 alone) [64]. The use of PEGPH20 to improve the delivery of anti-PD-1 antibodies and infiltration of cytotoxic T lymphocytes is being investigated in an ongoing clinical trial (3 μg/kg PEGPH20 QW with 200 mg pembrolizumab Q3W) for patients with HA-high refractory metastatic PC [65]. Considering the important role of HA in interstitium formation, AEs of such combination therapies, especially cardiovascular risks, should be closely monitored and evaluated.
Interleukin-6 (IL-6) is a cytokine instrumental for the progression of PC and a prognostic factor for outcome. It is produced principally by pancreatic stellate cells (PSCs) but also by tumor-associated myeloid cells [66, 67]. The IL-6/STAT3 axis can promote the expansion of immunosuppressive cells and alter the balance of T cell subsets [68, 69]. In mice bearing subcutaneous MT5 and Panc02 tumors, the combination blockade of anti-IL-6 antibody (200 μg/mouse, TIW for 2 weeks; clone MP5-20F3) and anti-PD-L1 antibody (200 μg/mouse, TIW for 2 weeks; clone 10F.9G2) was found to inhibit tumor volume (p < 0.05 compared with monotherapy using either) in CD8+ T cell-dependent approaches [70]. In addition, in mice bearing autochthonous KPC-derived pancreatic tumors, mOS increased with the combination of anti-IL-6 and anti-PD-L1 (25 days vs 11 days, p = 0.04, compared with mice administered equimolar control antibodies) [71]. While T cell infiltration into tumors is a major issue that anti-PD-(L)1 therapies face, combining anti-IL-6 may switch T cells to a Th1 phenotype and limit immune suppression [70]. Of note, IL-6 blocking antibodies have been approved in clinic to treat autoimmune diseases [72]. Therefore, whether this combination improves PC treatment efficacy still requires clinical verification.
Combination with agents targeting membrane receptors
PSCs are fibroblasts that become activated and express high levels of vitamin D receptors (VDRs) in the stroma of tumors in PC. Treatment with VDR ligands may convert activated PSCs to a quiescent state, inducing stromal remodeling and reducing tumor volume, thereby permitting greater delivery of chemotherapeutic agents [73]. A clinical trial that combined gemcitabine (1000 mg/m2, on day 1, 8, 22, and 29 of a 42-day cycle), albumin-bound paclitaxel (125 mg/m2, on day 1, 8, 22, and 29 of a 42-day cycle), cisplatin (25 mg/ m2, on day 1, 8, 22, and 29 of a 42-day cycle), nivolumab (240 mg, on day 1, 15, and 29 of a 42-day cycle), and paricalcitol (25 μg BIW) to study the treatment of metastatic PC found that among 24 patients that were evaluated, 19 displayed PR, 2 had stable disease (SD), and 2 exhibited PD. Median PFS was 8.17 months and mOS was 15.3 months. The most common drug-related, grade 3–4 AEs were thrombocytopenia (76%) and anemia (44%). Encouraging ORR values have resulted in an expansion of the trial [74]. Due to the lack of control groups, the role of paricalcitol in improving anti-tumor effects remains unknown. Additionally, considering the relatively heavy chemotherapeutic burden of this combined regimen, AEs require strict prevention and treatment.
Transforming growth factor-β (TGF-β) promotes the expression of fibrous extracellular matrix and enhances tumor immunosuppression, metastasis, and epithelial-to-mesenchymal transition (EMT )[75]. Preclinical trials in other tumors have demonstrated that the combined blockade of TGF-β signaling and PD-(L)1 checkpoint increases CD8+ T cell infiltration and reduces immune suppression [75, 76]. Wang and others used acidic tumor extracellular pH-responsive clustered nanoparticles (LYiClustersiPD-L1) to deliver TGF-β receptor inhibitors (LY2157299) and small interfering RNA (siRNA) molecules that targeted PD-L1 in PC. In a Panc02 orthotopic tumor model, tumor weight was found to significantly decline using LYiClustersiPD-L1 (~ 88% reduction, p < 0.001 compared with monotherapy of either). High serum levels of IFN-γ resulted in improved T cell activity [77]. M7824 (MSB0011359C) is a bifunctional fusion protein of anti-PD-L1 antibody fused to the extracellular domain of TGF-β receptor II (TGF-β trap). In a phase I trial of 5 advanced PC patients, one that was mismatch repair-deficient (dMMR) received M7824 at 3 mg/kg and achieved durable PR. The patient persisted in the study and experienced disease progression at 10.5 months. Another PC patient who received M7824 at 3 mg/kg displayed a prolongation of SD for 4.5 months [78]. Moreover, a combination of the TGF-β receptor I kinase inhibitor galunisertib (150 mg BID 14 days on/14 days off) and durvalumab (1500 mg Q4W) was assessed in recurrent or refractory metastatic PC patients in a phase Ib study. One patient experienced PR while 7 displayed SD in a trial of 32 patients, demonstrating a DCR of 25% and mPFS of 1.9 months [79]. Although combined blockade of TGF-β and PD-L1 may display nonredundant effects on the adaptive and innate immune systems, the clinical data were based on heavily pretreated patients and not comparable with chemotherapy.
TAMs and MDSCs actively suppress the anti-tumor immune response, promoting metastatic dissemination and imparting resistance to cytotoxic therapies in human tumors. Colony-stimulating factor 1 (CSF1) signaling regulates their differentiation and survival [80, 81]. While CSF1R blockade was found to upregulate PD-L1 expression, a combination of CSF1R inhibitor (GW2580 800 mg/kg in chow), PD-1 antagonist (200 μg/dose every 4 to 5 days; clone RMP1–14), and gemcitabine (50 mg/kg every 4 to 5 days) reduced tumor progression by more than 90% in a syngeneic orthotopic mouse model [80]. In a phase I study of 31 PC patients that combined the anti-CSF1R antibody cabiralizumab (mostly 4 mg/kg Q2W) and nivolumab (3 mg/kg Q2W), 3 experienced PR (continuing on the study for 293, 275+, and 168+ days) with microsatellite-stable status while 1 displayed prolonged SD (182 days). The 6-month DCR was 13% with an ORR of 10% [82]. A separate study of 30 PC patients that combined the anti-CSF1R antibody lacnotuzumab (MCS110) with the anti-PD-1 antibody spartalizumab (PDR001) resulted in one that experienced PR (continuing in the study for 346 days) and 2 that displayed durable SD (on the study for 328 and 319 days) [83]. Although CSF1 signaling can regulate both the number and the function of TAMs, the PC immunosuppressive microenvironment involves a complex regulatory network, which limits the efficacy of the combined regimen.
CD40 is a member of the tumor necrosis factor (TNF) receptor superfamily that allows dendritic cells (DCs) to promote antitumor T cell activation and re-educates macrophages to destroy the tumor stroma. Agonistic anti-CD40 antibodies and trimeric CD40 ligands were studied to determine whether they activated DCs and other APCs [84]. Using an orthotopic Pan02 tumor mouse model, combining the CD40 agonist (3 mg/kg on day 7, 14, 21, 28; clone FGK4.5) with PD-L1 blockade (10 mg/kg on day 7, 10, 14, 17, 21, 24; clone 10F.9G2) improved OS versus monotherapy with either agent. PD-L1 upregulation, systemic APC maturation, and memory T cell expansion were demonstrated after the use of a CD40 agonist [85]. Furthermore, in a syngeneic subcutaneous PC mouse model, the addition of anti-PD-1 antibodies (200 μg on day 0, 3, 6, 9, 12, 15, 18, and 21; clone RMP1–14) to the CD40 agonist (100 μg on day 3; clone FGK45) and gemcitabine (120 mg/kg on day 1) + nab-paclitaxel (120 mg/kg on day 1) doubled long-term survival compared with a CD40 agonist + gemcitabine + nab-paclitaxel (26% versus 12%). Furthermore, the addition of a cytotoxic T-lymphocyte antigen-4 (CTLA-4) antibody (200 μg on day 0, 3, and 6; clone 9H10) more than trebled long-term survival (39% versus 12%) [86]. In another study in which a genetically engineered PC mouse model was used, the combination of CD40 agonist (100 μg on day 11; clone FGK4.5), radiotherapy (20 Gy on day 8), anti-PD-1 antibodies (200 μg on day 5, 8, 11; clone RMP1–14), and anti-CTLA-4 antibodies (200 μg on day 5, 8, and 11; clone 9H10) eradicated primary and abscopal tumors, thereby providing long-term immunity. While radiotherapy triggers an early proinflammatory response and upregulates MHC class I and CD86 antigens on APCs, CD40 agonists prompt systemic and intratumoral myeloid compartment reorganization. Subsequent immune checkpoint blockade increases intratumoral T cell infiltration and increases the CD8 T cell: Treg ratio. This observation demonstrates that CD40 agonist and radiotherapy can functionally augment PC antitumor immunity [87]. In a clinical phase Ib study in which CD40 agonist APX005M (sotigalimab, 0.1 mg/kg or 0.3 mg/kg on day 3 or day 10), gemcitabine (1000 mg/m2 on day 1, 8, and 15 every 4 weeks), and nab-paclitaxel (125 mg/m2 on day 1, 8, and 15 every 4 weeks) were combined with nivolumab (240 mg on day 1 and 15 every 4 weeks) to treat 12 metastatic PC patients, 8 achieved PR while 3 displayed SD. Twenty one-day chemotherapy cycle and dose reduction (except for nivolumab) to manage toxicity were allowed. Median PFS was 10.8 months (in the cohort receiving 0.1 mg/kg APX005M) and 12.4 months (in the cohort receiving 0.3 mg/kg APX005M). It was established that the combination was tolerable and later-phase trials are anticipated [88]. Unlike blocking tumor progression or invasion signals in part, CD40 agonism is an “ignition” signal resulting in APC activation, macrophage tumoricidal activity, and CD8+ T cell-dependent antitumor immunity. Therefore, administration of a CD40 agonist several days after chemotherapy or radiotherapy may amplify the tumor antigen-induced immune responses. The development of novel drug delivery systems in PC may further improve efficacy.
To counter anti-tumor immunity, PC cells release high-mobility group protein B1 (HMGB1), which combines with CXC-chemokine ligand 12 (CXCL12) produced by fibroblast activation protein (FAP)-positive CAFs to activate CXC-chemokine receptor 4 (CXCR4) on Teffs [89]. In a syngeneic subcutaneous PC mouse model, the addition of anti-PD-L1 antibodies (160 μg QOD; clone 10F.9G2) to 90 mg/mL CXCR4 inhibitor AMD3100 (using an AZLET osmotic pump) was found to significantly decrease tumor volume (p < 0.01), identified by the loss of heterozygosity of the Trp53 gene [90]. In a study in which human PC specimens were harvested and analyzed by organotypic slice culture to test the effects of the combination of anti-PD-1 (20 mg/mL) and CXCR4 inhibitor AMD3100 (100 mg/mL), CD8+ T cell migration and induction of tumor cell apoptosis were observed [91]. In a Panc02 subcutaneous tumor mouse model, CXCR4 antagonist BL-8040 combined with anti-PD-1 and irinotecan, fluorouracil and leucovorin reduced tumor growth by 58% compared with chemotherapy alone. Although the triple combination treatment did not significantly change the number of CD8+ T cells in the tumor, it increased their activation state [92]. In a clinical study, administration of the CXCL12 inhibitor NOX-A12 and pembrolizumab resulted in 25% of patients experiencing SD in 11 metastatic colorectal cancer patients and 9 metastatic PC patients. Median PFS was 1.87 months, OS was 42% after 6 months and 22% after 12 months [93]. A similar DCR of 21.4% (1 PR + 2 SD) was achieved using BL-8040 (1.25 mg/kg for 2 weeks before pembrolizumab and on day 1, 4, 8, 11 combined with pembrolizumab in a 3-week cycle) and pembrolizumab (200 mg Q3W) in metastatic PC patients in a similar study [94]. Furthermore, in a phase IIa two-cohort study, 22 metastatic PC patients received BL-8040 (1.25 mg/kg on day 1–5 of week 1, then 1.25 mg/kg BIW from week 2), pembrolizumab (200 mg Q3W from day 10), liposomal irinotecan (70 mg/m2 Q2W from day 8), fluorouracil (2400 mg/m2 Q2W from day 8), and leucovorin (400 mg/m2 Q2W from day 8), finding that the ORR, DCR, and the median duration of response were 32, 77%, and 7.8 months, respectively. In a separate cohort, 37 patients with chemotherapy-resistant stage II-IV PC received BL-8040 (1.25 mg/kg on day 1–5 of week 1, then 1.25 mg/kg TIW from week 2) and pembrolizumab (200 mg Q3W). The investigators found a DCR of 34.5% in the study population with an mOS of 7.5 months in patients receiving the treatment as second-line therapy [95]. Blocking the CXCL12/CXCR4 pathway attempts to address the problem of geographic sequestration of Teffs, which emphasizes the sequestration of clonally expanded Teffs from the juxtatumoral compartment [91]. Combined with anti-PD-(L)1, it modulates different axes of immunosuppression in PC that demonstrates a synergistic effect.
CXCR2 is a G-protein-coupled receptor that regulates neutrophil and MDSC migration in the TME of PC, which drives tumor invasion and metastasis. In an experiment using KPC mice, one group firstly received the CXCR2 inhibitor AZ13381758 100 mg/kg BID for 2 weeks to increase T cell infiltration into the tumor, followed by the administration of anti-PD-1 antibodies (10 mg/kg BIW) while AZ13381758 continued. They experienced survival that was significantly extended compared with mice treated with vehicle plus anti-PD-1 [96]. In addition, using the KP2 orthotopic PC mouse model, triple therapy with the CXCR1/2 inhibitor SX-682, FOLFIRINOX, and checkpoint inhibition (anti-PD-1/anti-CTLA-4) resulted in significantly increased survival compared with other groups [97]. Considering that CXCR2 is principally upregulated in neutrophils and MDSCs rather than in cancer cells, its inhibition in combination with anti-PD-(L)1 may be used with standard chemotherapy to improve efficacy.
CD73 is an ectoenzyme that catalyzes the hydrolysis of adenosine monophosphate (AMP) to immune-suppressive adenosine (ADO). It curtails T cell activation and is associated with a worsening prognosis in malignancies. In C57BL/6 J mice bearing established KP4662-G12C tumors, coadministration of CD73 inhibitor A0001421 (30 mg/kg QD) and anti-PD-1 antibodies (10 mg/kg BIW; clone RMP1–14) was superior to anti-PD-1 alone in limiting PC growth [98]. KRAS mutation is one of the most common oncogenic drivers in PC, which significantly upregulates CD73 expression and results in a worsening prognosis. In addition, PD-1 nonresponsive mice express higher levels of ADO pathway genes, including CD73 and CD39. Therefore, inhibiting CD73 together with PD-(L)1 is hoped to provide a significant anti-tumor effect, especially in PC [98–100].
Combination with agents targeting intracellular regulators
Focal adhesion kinases (FAKs, including FAK1 and PYK2) are non-receptor tyrosine kinases that translate signals from the extracellular matrix into intracellular pro-inflammatory pathway regulation and cytokine production. Wound healing and pathological fibrosis both involve FAK signaling [101, 102]. FAK activity is elevated in human PC tissue and correlates with increased fibrosis and poor CD8+ cytotoxic T cell infiltration. Using both syngeneic and genetic animal models, FAK inhibitor VS-4718 (50 mg/kg BID) was found to promote responsiveness to a PD-1 antagonist (200 μg every 4–5 days; clone RMP1–14), demonstrated by reduced tumor burden and improved OS. The maximum response was observed when FAK inhibition was provided in combination with low-dose gemcitabine (25 mg/kg every 4–5 days) [102]. In a phase I study that combined the FAK inhibitor defactinib, pembrolizumab, and gemcitabine, PR was observed in a patient who had progressed when treated with gemcitabine and nab-paclitaxel. The median duration of patient treatment was 127 days in a cohort of 8 PC patients, the longest duration being 290 days. The combination regimen was found to be well-tolerated, and recruitment of additional patients to the cohort (PC only) is ongoing [103]. Considering the immunosuppressive TME and the uniquely desmoplastic stroma, FAK inhibition is particularly promising in PC. However, FAK inhibition and anti-PD-(L)1 both have strong molecule-targeting capabilities and general killing effects, and so still require treatment based on chemotherapy.
Bruton’s tyrosine kinase (BTK) is a non-receptor enzyme of the Tec kinase family expressed by B cells and macrophages. In a murine model of PC, BTK inhibitor ibrutinib was shown to convert M2-like macrophages to an M1-like phenotype, resulting in the promotion of CD8-mediated T cell cytotoxicity [104]. A phase II study evaluated the BTK inhibitor acalabrutinib (100 mg BID) alone or in combination with pembrolizumab (200 mg Q3W) in 77 advanced PC patients. The ORR and DCR values of 0 and 14.3% were observed with monotherapy, and 7.9 and 21.1% for combination therapy. An exceptional responder treated with this combination therapy experienced a PR with near-resolution of bulky peritoneal disease. An additional exceptional responder that had initially been prescribed acalabrutinib alone exhibited SD for 7.5 months, and on crossover demonstrated SD in response to combination therapy, remaining on combination therapy for 8.7 months before progression. The combination of acalabrutinib and pembrolizumab was well tolerated but demonstrated limited clinical effectiveness [105]. The enrolled patients had failed a median of 3 prior lines of therapy, possibly leading to a clonal expansion of a kinase inhibitor-resistant phenotype likely to eliminate the oncogenic drivers responsive to BTK inhibition [106]. For this kinase-targeted therapy, the difficulty of patient selection limits its clinical efficacy.
Poly (ADP-ribose) polymerase (PARP) recognizes and binds to single-stranded DNA breaks, and recruits proteins to perform DNA damage repair (DDR). PARP inhibitors prevent DDR, probably via trapping PARP on the DNA and preventing the progression of the replication fork. Cancer cells with mutations that prevent homologous recombination repair via other pathways, such as loss-of-function mutations in BRCA1/2, are often more sensitive to PARP inhibitors because of the substantially reduced capacity for DDR [6]. A study in which PARP 1/2 inhibitor BGB-290 was combined with the anti-PD-1 antibody BGB-A317 to treat advanced PC patients found that 1 subject experienced PR while 2 achieved SD. They had received BGB-290 + BGB-A317 for 189 and 281 days, respectively [107]. Furthermore, SD in PC patients was also observed when the PD-1 inhibitor dostarlimab, the PARP inhibitor niraparib, and bevacizumab were administered as a combination therapy in another study [108]. Because of the lack of control groups, whether the patients who did not derive benefit or were resistant to either PARP inhibition or anti-PD-(L)1 alone could have benefitted from the combination strategy is unknown. In addition, the underlying biological mechanisms of the combination strategy await elucidation to determine whether the agents should be restricted to DDR tumors or used more broadly.
Combination with immunotherapy
Combination with agents targeting other immune checkpoints
PD-(L)1 blockade and anti-CTLA-4 therapy operate in different phases of the immune response, which explains the basis of their combined mechanism of action. PD-1 is mostly expressed on late effector phase CD4+ helper T cells and CD8+ cytotoxic T cells in peripheral tissues. Anti-PD-1 treatment targets the effector phase of T cell activation in this periphery. CTLA-4 is among the first negative regulators to be induced and directly competes with CD28 for the ligands CD80 and CD86, thereby interfering with positive costimulatory signals. Anti-CTLA-4 treatments mostly result in changes in secondary lymphoid organs during the initial phase of naive T cell activation [16, 17, 109, 110]. In a clinical study of 3 refractory PC patients that received nivolumab and ipilimumab (ipilimumab 1 mg/kg and nivolumab 3 mg/kg Q3W followed by nivolumab 240 mg Q2W), 1 patient expressing BRCA1 achieved CR and thereafter received nivolumab on maintenance for 17 months. A second patient that expressed RAD51C achieved PR but continued to improve in terms of pain and tumor markers [111]. A phase II study in which nivolumab (240 mg Q2W) and ipilimumab (1 mg/kg Q6W) were combined with radiation (8 Gy × 3 at cycle 2 QOD) to treat metastatic microsatellite stable PC patients, found a DCR of 20% (5/25) with an ORR of 13% (3/25) via intention to treat analysis [112]. The addition of durvalumab to tremelimumab (durvalumab 1.5 g + tremelimumab 75 mg Q4W × 4 doses → durvalumab 1.5 g Q4W) for the treatment of metastatic PC patients found that more ≥ grade 3 treatment-related AEs were observed (22% with the combination therapy, 6% with durvalumab alone), while mPFS (both 1.5 months) and mOS (3.1 months in combination, 3.6 months for durvalumab alone) did not change [113]. A phase II study combined gemcitabine (1000 mg/m2 on day 1, 8, 15 every 4 weeks), nab-paclitaxel (125 mg/m2 on day 1, 8, 15 every 4 weeks), durvalumab (1500 mg on day 1 Q4W), and tremelimumab (75 mg on day 1 Q4W) as the first-line therapy to treat metastatic PC patients. A total of 8/11 patients (73%) achieved PR with a DCR of 100%. Median PFS was 7.9 months while the 6-month survival rate was 80% [114]. High-dimensional single-cell profiling was used to profile the response of T cell populations to anti-PD-(L)1 monotherapy, anti-CTLA-4 monotherapy, or their combination. It was shown that the majority of the effects of monotherapies are additive in the context of combination therapy, while combination therapy mediates a switch from an expansion of phenotypically exhausted CD8 T cells to an expansion of activated effector CD8 T cells [115]. However, based on the results of clinical studies, chemotherapy remains the cornerstone of this immune checkpoint inhibitor (ICI) combination strategy.
The immune checkpoint target indoleamine 2,3-dioxygenase 1 (IDO1) is a rate-limiting metabolic enzyme that converts tryptophan into downstream kynurenines. IDO1 is activated in a variety of human cancers and demonstrates immunosuppression through the suppression of CD8+ Teffs and NKs, in addition to increased activity of Tregs and MDSCs [116, 117]. A phase I study in Japan combined the IDO1 inhibitor epacadostat (INCB024360, 25 mg or 100 mg BID) with pembrolizumab (200 mg Q3W) to treat advanced PC tumors. One patient achieved PR and remained on treatment for 21 weeks [118]. In another phase I study, one PC patient that received the IDO1 inhibitor navoximod (GDC-0919, 100 mg Q12H) and atezolizumab (1200 mg Q3W) experienced PR. The patient remained in the study for more than 650 days [119]. Based on the clinical results of adding IDO1 inhibition to anti-PD-(L)1 in various cancers, the purpose of improving clinical efficacy in unselected patients has not been achieved.
Combination with CAR-T therapy
Chimeric antigen receptor (CAR) T cells recognize tumor-associated antigens in an MHC-restricted manner, thereby becoming activated to kill cancer cells. CARs usually consist of an extracellular ligand recognition domain fused to the cytoplasmic domains of one or more costimulatory domains (such as CD28 or 4-1BB) and CD3 zeta [120, 121]. A CAR comprising the extracellular domain of PD-1 not only recognizes the ligands of PD-1 expressed on cancer cells, but also interferes in the interactions of PD-1/PD-L1 that attenuate immune inhibition. In a subcutaneous Pan02 tumor mouse model, chimeric PD-1 T cells were found to significantly reduce tumor burden and increase survival compared with wild-type PD-1 T cells [122]. Another research group developed both PD1ACR (involving a PD-1-CD28–4-1BB activating chimeric receptor) T cells and PDL1CAR T cells using third-generation CARs. In syngeneic PC models, the adoptive transfer of both enhanced T cell persistence and induced CFPAC1 cancer regression by > 80% [123]. Distinct from monoclonal antibody therapies, although CAR T cells have not persisted over the long-term in tumor-surviving mice, they induced a long-lived tumor-antigen-specific host memory responses which protected against the rechallenge of the same tumor. It is worth noting that the host immune response was specific for tumor antigens instead of PD-1 ligands [122, 123]. Moreover, clinical trials investigating CAR T cells targeting mesothelin, carcinoembryonic antigen, mucin 1, and human epidermal growth factor receptor 2 found mixed efficacy in PC [124–128]. These once again demonstrated that a fundamental issue with CAR T cell therapy in PC is the lack of an ideal single-antigen target, which requires further investigation.
Combination with cancer vaccines
The combination of cancer vaccines and ICIs is likened to revving an engine and releasing the brakes. Cancer vaccines induce the infiltration of Teffs into tumors and create immune checkpoint signals. ICIs further attenuate tumor immune suppression [129]. Cancer vaccines include DC vaccines, whole-cell vaccines, peptide-based vaccines, mRNA vaccines, and DNA vaccines (plasmid vaccines, virus-based vaccines, bacterial vectors, and yeast-based recombination vaccines). DCs are a key member of the family of APCs, which efficiently present antigens to CD4+ and CD8+ T cells in addition to secreting cytokines such as IL-12, IL-15, IFN-γ, and TNF. DC vaccines can be activated by tumor antigens and promote a cytotoxic T cell response. Blocking PD-L1 on DC may improve the efficacy of DC therapy [130–132]. A recent study used antigen-primed monocyte-derived dendritic cells (MoDCs) alone or in combination with PD-L1 blockade to treat metastatic PC tumors. PD-L1 blockade was performed by adding soluble CD80 or anti-PD-L1 to MoDCs. As a result, 5/10 patients who did not respond to MoDC therapy alone achieved secondary stabilization (4 to 8 months) by the use of MoDCs modified using PD-L1 blockade [132]. Additionally, the same group studied the safety and efficacy of combining antigen-primed MoDCs with nivolumab (1–2 mg/kg 1 day before the DC vaccine). Two of 7 metastatic PC patients achieved PR. The majority of patients tolerated the therapy well with only mild AEs following therapy with nivolumab [133]. Furthermore, a phase Ib study combined a personalized autologous DC vaccine, standard of care adjuvant chemotherapy followed by nivolumab in 3 resectable PC patients. The personalized neoantigen peptides were identified through a proteo-genomics antigen discovery pipeline for each patient. The study described optimal conditions for incorporation into long peptides for manufacture into vaccine products [134]. It was shown in the preclinical study that DCs loaded with a PD-L1 immunogen could induce anti-PD-L1 antibodies and a T cell response in vivo. The PD-L1-specific cytotoxic T cells displayed cytolytic activity against PD-L1+ tumor cells. This provided a novel concept for combining DC vaccines and anti-PD-(L)1. Without the repeated administration of anti-PD-(L)1 antibodies, this novel PD-L1 vaccination persistently produced anti-PD-L1 antibodies and T cell responses. This strategy may benefit not only cancer treatment but immune prevention of carcinogenesis in healthy individuals at high risk of developing cancer, in addition to the prevention of cancer recurrence [135].
GVAX is a human whole-cell granulocyte-macrophage colony-stimulating factor (GM-CSF)-secreting PC vaccine, consisting of allogeneic PC cell lines engineered to secrete the factor. It significantly upregulated the expression of PD-L1 on the membrane following treatment of tumor-bearing mice. In a syngeneic metastatic PC mouse model, combination therapy with GVAX (on day 4, 7, 14, and 21) and anti-PD-1 G4 antibodies (100 μg BIW) improved murine survival compared with anti-PD-1 antibody monotherapy or GVAX therapy alone [136]. The addition of anti-CD137 antibodies (20 μg BIW for 4 weeks; clone BMS-469452) to GVAX (on day 4, 7, 14, and 21) and anti-PD-1 antibodies (100 μg BIW for 4 weeks; clone 4H2) further improved survival in a syngeneic liver-metastatic PC mouse model. The expression of the costimulatory molecules CD137 and OX40 on CD4+PD-1+ and CD8+PD-1+ T cells increased, suggesting activation of the T cells [137]. Moreover, the addition of the CD40 agonistic antibody to GVAX and anti-PD-1 also increased the survival of mice with syngeneic metastatic PC [138]. In terms of the dose and schedule for anti-PD-(L)1 and vaccines, it has been shown that both PD-1 and PD-L1 appear rapidly following exposure to IFN, which emphasizes the early application of PD-(L)1 blockade [134].
Combination with oncolytic virus
Oncolytic virus (OV) immunotherapy involves three major mechanisms: direct infection of cancer cells, endothelial cells, and subsequent oncolysis; indirect effects of necrosis or apoptosis of uninfected cancer cells and their associated cells within the TME; improved antigen cross-priming and recruitment of immune cells into the TME. When combined with ICIs, OVs prime, boost, and recruit Teffs into the TME, where ICIs enhance the potency of lymphocytes to infiltrate tumors via the removal of inhibitory signals [139, 140]. In a preclinical study using a KPC syngeneic PC mouse model, Wang et al. found that oVV-LZ8 (where the oVV-gene is an oncolytic vaccinia virus platform and LZ8 is an immunomodulatory protein isolated from Reishi, capable of promoting cell proliferation and IL-2 production in T cells) enhanced the tumor inhibitory effects of anti-PD-1 antibody in vivo. It was associated with increased numbers of NK, CD8+, and CD4+ T cells in addition to increased secretion of anti-tumor cytokines, including IFN-α, IFN-γ, and IL-2 [141]. VVL-21 is an oncolytic vaccinia virus carrying IL-21, a regimen that inhibits PI3Kδ to prevent viral uptake by macrophages so that intravenous delivery is enhanced, with viral B5R protein modification to improve viral spread within and between tumors. By combining VVL-21 with anti-PD-1, tumor growth was found to be significantly inhibited compared with the virus alone in a syngeneic subcutaneous DT6606 tumor mouse model. Enhanced IFN-γ induction and a more significant CD8+ T cell response resulted in more greatly increased OS [142]. Moreover, CF33-hNIS-antiPDL1 is a genetically engineered chimeric orthopoxvirus equipped with human sodium iodide symporter (hNIS) and anti-PD-L1 antibody. In a syngeneic peritoneal carcinomatosis nude mouse model of PC, a single dose of CF33-hNIS-antiPDL1 produced functional anti-PD-L1 antibody, reduced tumor burden, and prolonged survival [143].
In a clinical study, the combination of the oncolytic reovirus pelareorep with pembrolizumab and chemotherapy resulted in 1 PC patient achieving PR for 17.4 months, while 2 experienced SD for 9 and 4 months. Viral replication was observed in biopsies of the tumor. High peripheral T cell clonality and changes in the expression of immune genes were observed in patients, resulting in clinical benefit. The combination therapy did not display any significant toxicity [144].
The immunosuppressive PC TME poses a double-edge sword in OV immunotherapy. It helps with viral replication that promotes direct oncolysis, but also impedes the following antitumor immune responses and limits durable immunity. Methods to regulate the TME to manipulate this balance may determine the optimal clinical efficacy of OV. Moreover, the mechanisms of primary, adaptive, and acquired resistance to OV immunotherapy remain to be elucidated. Combining anti-PD-(L)1 with OV may partly overcome the resistance but has not demonstrated a radical improvement. Drugs regulating the TME can be either physically delivered or encoded by a recombinant OV to access the tumor to maximize the efficacy of this combination.
Discussion
Anti-PD-(L)1 monotherapy has not achieved satisfactory clinical outcomes in PC, due to the immunosuppressive TME and its intrinsically non-immunogenic nature. Mechanisms to evoke the response of PC to ICIs include increasing initial T cell priming, neutralizing immunosuppressive elements within the TME, enhancing innate and other adaptive immune cell effector functions, and inhibition of compensatory T cell anergy and exhaustion [109, 145]. Various systemic and locoregional therapies have been investigated for combination with anti-PD-(L)1 therapy founded on this concept, but the efficacy and AEs of these combinations vary widely.
In terms of mechanisms, targeted therapies have strong specificity, while their anti-tumor effects may be mediocre. It may be due to the multi-faceted roles of the drug targets, which probably regulate the PC TME through a variety of cell types and pathways that do not simply suppress the tumor. Immunotherapies are highly dependent on the specific PC TME, which is complex for different tumors, displaying various responses. Chemotherapies powerfully induce tumor cell death, release tumor-associated antigens, and initiate a following immune response. However, chemotherapy alone tends to induce drug resistance, which leads to a subsequent poor response to other types of anti-tumor treatment.
In preclinical studies, cell and mouse models inadequately recapitulate the whole genomic heterogeneity and the TME of human PC. In particular, syngeneic subcutaneous PC mouse models are mostly used in current preclinical studies, but are relatively deficient in the host immune responses and have low disease complexity. Using humanized mouse models can help elevate the validity of evidence [146, 147]. In addition, animal samples are often limited to a small size. The dose, schedule, and sequence of drug administration vary greatly across different preclinical studies, resulting in significant differences in efficacy and survival. Moreover, the monitoring of AEs in animals is relatively scarce, restricting toxic dose limitation and dose adjustment.
In clinical studies, a number of researchers have selected patients based on predictive biomarkers or genetic profiling, while others have not investigated specific molecular characteristics. Some have excluded patients who had used the same types of drug, while others have not. The treatment lines of different combinations also vary widely. This has resulted in significant heterogeneity among enrolled patients. Focusing on a subgroup that did not derive benefit or was resistant to either monotherapy may be challenging but have meaningful conclusions. Moreover, some clinical studies are single-arm trials without control groups. The dosing and scheduling of drugs differ greatly across studies, as determined by preclinical protocols or clinical experience, and still require adjustments and optimization based on sequential tumor biopsies and serial blood collection.
A notable problem with combination therapies is whether AEs exceed acceptable clinical limits. When combining pembrolizumab (2 mg/kg Q3W) with gemcitabine (1000 mg/m2 on day 1 and 8 every 3 weeks) and nab-paclitaxel (125 mg/m2 on day 1 and 8 every 3 weeks) for the treatment of PC, 70.6% of patients experience grade 3–4 treatment-emergent adverse events (TEAEs), which declines following mandatory premedication with dexamethasone [36]. A separate study that tested nivolumab (3 mg/kg on day 1 and 15 every 4 weeks) + gemcitabine (1000 mg/m2 on day 1, 8, 15 every 4 weeks) and nab-paclitaxel (125 mg/m2 on day 1, 8, 15 every 4 weeks) reported that 98% of patients either experienced ≥1 grade 3–4 TEAE (96%) or discontinued treatment due to TEAEs (36%). That study deemed that the drugs were tolerable but the observed efficacy did not support further investigation. The combination was not characterized by additional immune-related AEs, and the reported AEs were consistent with those of each agent [37]. The tri-combination of pembrolizumab (200 mg Q3W), capecitabine (825 mg/m2 BID, Monday-Friday, on days of radiation therapy only), and radiation (50.4 Gy in 28 fractions over 28 days) treatment was relatively well-tolerated with no grade 4 toxicity or major surgical complications 30 days postoperatively [53]. As for AEs due to combining molecularly targeted agents with anti-PD-(L)1, dose-escalation of the TGF-β receptor I kinase inhibitor galunisertib (150 mg BID 14 days on/14 days off) did not display DLTs, at the maximum dose of 150 mg BID that was selected. Adding it to durvalumab (1500 mg Q4W) led to no more than 7 grade ≥ 3 related AEs in 32 PC patients [79]. When combining the anti-CSF1 antibody lacnotuzumab with spartalizumab, grade ≥ 3 AEs increased, such as elevated aspartate aminotransferase (12%), asthenia (10%), and hyponatremia (10%) [83]. The combination of sotigalimab (CD40 agonistic antibody, 0.1 mg/kg or 0.3 mg/kg on day 3 or day 10), gemcitabine (1000 mg/m2 on day 1, 8, and 15 every 4 weeks) plus nab-paclitaxel (125 mg/m2 on day 1, 8, and 15 every 4 weeks), and nivolumab (240 mg on day 1 and 15 every 4 weeks) was found to cause grade 3 or 4 treatment-related AEs in 94% of patients, but which were clinically manageable. One death due to septic shock occurred due to neutropenia. Toxicity was deemed chemotherapy-related and synergistic toxicity was not apparent when combining sotigalimab with nivolumab [88]. Most common grade ≥ 3 AEs using gemcitabine (1000 mg/m2 on day 1, 8, 15 every 4 weeks), nab-paclitaxel (125 mg/m2 on day 1, 8, 15 every 4 weeks), durvalumab (1500 mg on day 1 Q4W), and tremelimumab (75 mg on day 1 Q4W) were hypoalbuminemia (45%), abnormal lipase (45%), and anemia (36%) [114]. Combining anti-PD-(L)1 with anti-CTLA-4 was found to increase, predate, and raise the severity of AEs in various cancers [148, 149]. The use of the oncolytic reovirus pelareorep with pembrolizumab and chemotherapy was observed to cause grade 3–4 treatment-related AEs in 18% of patients [144]. Thus, the occurrence of AEs when combining anti-PD-(L)1 with different agents is variable but closely associated with drug dosage. Whether there is greater risk and earlier onset of AEs requires practical analysis. Systemic glucocorticoids should be used with caution. Clinicians and scientists need to perform a baseline evaluation before treatment, a comprehensive examination during treatment, a close follow-up after treatment, in addition to an individualized treatment [150].
Future perspectives
In addition to the challenging discovery and development of new drugs, drug repurposing has been recognized as an attractive investigation proposition, with fewer development costs, shorter development timelines, and lower safety risks [151]. With the focusing of research on the post-translational modifications (PTMs) of PD-(L)1, various traditional chemotherapeutic and targeted drugs have been found to regulate the PTMs of PD-(L)1, thus demonstrating the prospect of combining with anti-PD-(L)1. Gemcitabine and paclitaxel have been shown to induce PD-L1 expression via the JAK/STAT pathway, and attenuated by a JAK2 inhibitor [31]. The epidermal growth factor (EGF) receptor tyrosine kinase inhibitor gefitinib phosphorylates PD-L1 to induce its degradation. Gefitinib has been combined with PD-1 blockade, displaying enhanced therapeutic efficacy in a syngeneic mouse cancer model [152]. Anti-IL-6 inhibits JAK1 activation to promote the degradation of PD-L1, when combined with an ICI, demonstrated enhanced anti-tumor efficacy compared with the ICI alone [153]. The PTMs of PD-(L)1 restrict the synergistic effects of combination therapies mentioned above. However, combination therapies with drugs targeting the PTMs of PD-L1 have scarcely been studied for PC, although these have emerged as potential strategies for cancer treatments over recent years (Fig. 2).
Fig. 2.
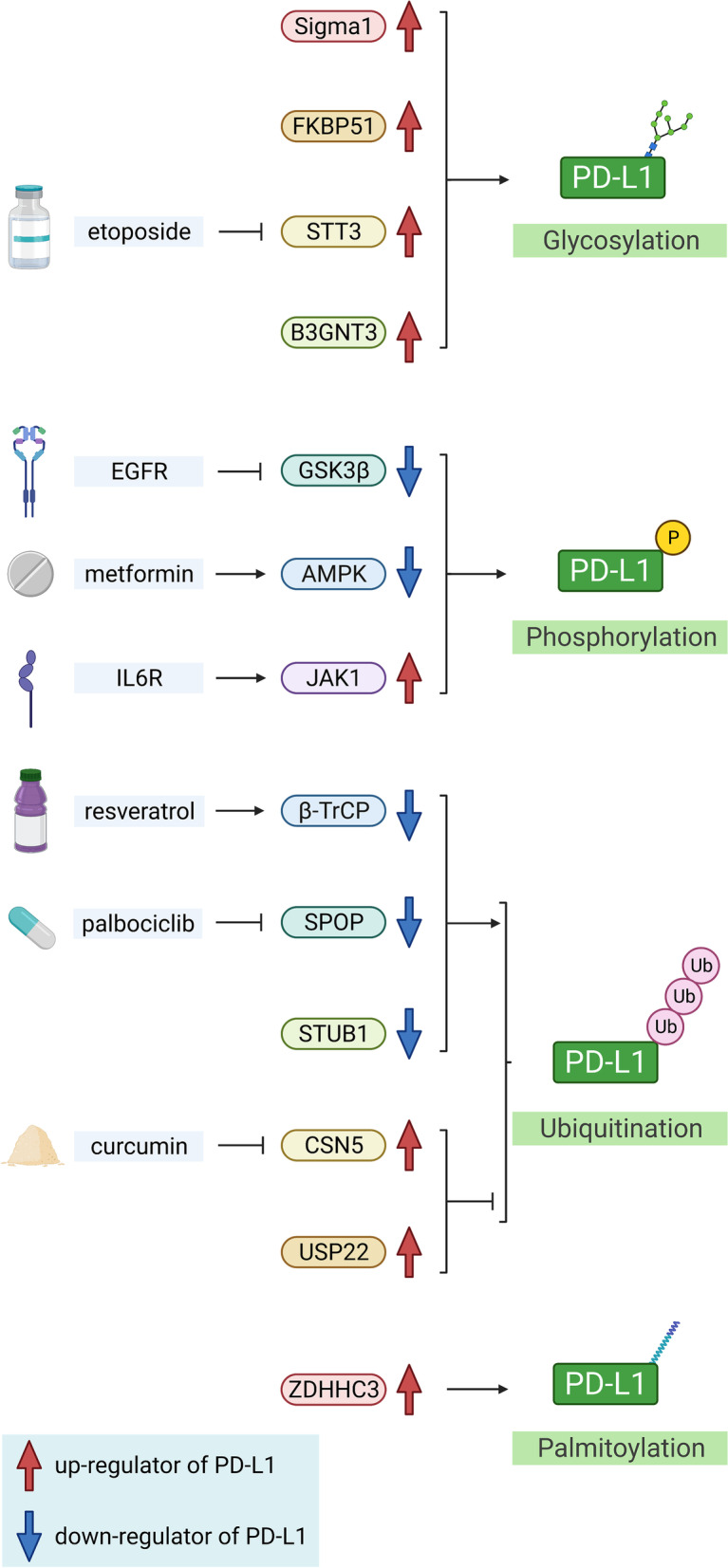
Post-translational modifications of PD-L1 described in the review. AMPK: adenosine-5′-monophosphate-activated protein kinase; B3GNT3: β-1,3-N-acetylglucosaminyl transferase; CSN5: COP9 signalosome complex subunit 5; EGFR: epidermal growth factor receptor; FKBP51: FK506 binding protein 51; GSK3β: glycogen synthase kinase 3β; IL6R: interleukin-6 receptor; JAK1: Janus kinase 1; PD-L1: programmed cell death ligand 1; Sigma1: sigma nonopioid intracellular receptor 1; SPOP: speckle-type POZ protein; STT3: staurosporine temperature sensitivity 3; STUB1: STIP1 homology and U-box containing protein 1; USP22: ubiquitin-specific protease 22; ZDHHC3: zinc-finger DHHC-type-containing 3; β-TrCP: β-transducin repeat-containing protein
Targeting the PTMs of PD-L1
The PTMs of PD-L1 are important mechanisms that regulate protein stability, translocation, and protein-protein interactions. Glycosylation, phosphorylation, ubiquitination, and palmitoylation are the four major PTMs of PD-L1. N-linked glycosylation protects PD-L1 from glycogen synthase kinase 3β (GSK3β)-mediated 26S proteasome machinery engagement [152, 154]. It also enriches PD-L1 in cancer stem cells and regulates PD-L1/PD-1 interaction, thus suppressing the T cell anti-tumor response [155, 156]. Chaperone sigma nonopioid intracellular receptor 1 (Sigma1) and cochaperone FK506 binding protein 51 (FKBP51) facilitate PD-L1 glycosylation and stabilization in the endoplasmic reticulum (ER). Inhibition of Sigma1 or FKBP51 has been demonstrated to reduce PD-L1 expression and activate T cells in vitro in prostate cancer, triple-negative breast cancer (TNBC), and glioblastoma models [157, 158]. Staurosporine temperature sensitivity 3 (STT3) is the catalytically active subunit of oligosaccharyltransferase in cancer stem cells that increases PD-L1 glycosylation. Antagonism of STT3 by etoposide has been shown to destabilize PD-L1 and sensitize cancer cells to T cell immunoglobulin mucin-3 (TIM3) antagonists in syngeneic mouse models of TNBC and colon cancer [155]. β-1,3-N-acetylglucosaminyl transferase (B3GNT3)-mediated poly-N-acetyllactosamine is required for the interaction between PD-L1 and PD-1. Anti-glycosylated PD-L1 antibodies induce PD-L1 internalization and degradation in lysosomes, based on which a new antibody-drug conjugate (anti–gPD-L1-MMAE) has been formed that helps eradicate TNBC cells [156, 159].
Phosphorylation regulates the conformation, activity, and interactions of proteins. GSK3β is a serine/threonine kinase that phosphorylates PD-L1’s extracellular domain, which promotes the interaction of PD-L1 with E3 ligase β-transducin repeat-containing protein (β-TrCP) and subsequent PD-L1 degradation [152]. The inhibition of EGF signaling, which is upstream of GSK3β, downregulates PD-L1 and enhances the therapeutic efficacy of PD-1 blockade in syngeneic mouse cancer models [152, 160]. Adenosine-5′-monophosphate-activated protein kinase (AMPK) is an additional serine/threonine kinase that phosphorylates PD-L1 to induce abnormal PD-L1 glycosylation and its ER-associated degradation (ERAD). The AMPK agonist metformin facilitates the ERAD of PD-L1 that promotes antitumor immunity [161]. Moreover, IL-6/JAK1 phosphorylates PD-L1 to facilitate STT3 formation in the ER that induces the glycosylation of PD-L1 and promotes its stabilization. The combination of anti-IL-6 and anti-TIM3 antibodies has been demonstrated to improve the anti-tumor efficacy of CD8+ T cells, compared with anti-TIM3 monotherapy [153].
The ubiquitin-mediated proteasome degradation pathway extensively regulates PD-L1 expression, suggesting that there is a prospect of combining PD-L1 polyubiquitination regulators with ICIs as a potential therapy. E3 ligase β-TrCP catalyzes PD-L1 ubiquitination that degrades nonglycosylated PD-L1. Induction of β-TrCP expression by resveratrol reduces PD-L1 expression in vitro [152]. Speckle-type POZ protein (SPOP) is an E3 ubiquitin ligase that promotes the polyubiquitination and downregulation of PD-L1 through cyclin D-cyclin-dependent kinase 4 (CDK4). In a syngeneic mouse model of colon cancer, the CDK4/6 inhibitor palbociclib increases PD-L1 expression and synergizes with anti-PD-1 therapy to enhance therapeutic efficacy [162]. CKLF-like MARVEL transmembrane domain-containing 6 (CMTM6) prevents PD-L1 from undergoing polyubiquitination by E3 ubiquitin ligase STIP1 homology and U-box containing protein 1 (STUB1, [163, 164]. Conversely, COP9 signalosome complex subunit 5 (CSN5) is a deubiquitinase that inhibits the degradation of PD-L1, thereby enhancing PD-L1/PD-1 interactions that promote immune escape. Inhibition of CSN5 by curcumin reduces chronic inflammation-mediated PD-L1-based immunosuppression and synergizes with anti-CTLA-4 therapy in syngeneic mouse models of TNBC, melanoma, and colon cancer [165]. Ubiquitin-specific protease 22 (USP22) is a deubiquitinase that directly interacts with the C terminus of PD-L1. Genetic depletion of USP22 inhibits liver cancer growth, increases tumor immunogenicity, and improves the therapeutic efficacy of anti-PD-L1 therapy [166].
Palmitoylation is a recently discovered PTM of lipids that blocks PD-L1 ubiquitination and increases its stability. It has been found that zinc-finger DHHC-type-containing 3 (ZDHHC3) catalyzes the linking of palmitate to C272 on PD-L1. Inhibition of palmitoyltransferase by 2-bromopalmitate (2-BP) sensitizes tumor cells to destruction by T cells and inhibition of tumor growth [167, 168]. In summary, PTMs of PD-L1 that are targeted by drugs have displayed promise in preclinical trials. Whether they can represent candidates in combination therapies with anti-PD-(L)1 clinically still requires investigation.
Precision medicine
Traditional drug-centered clinical trials for treatments of PC tend to identify patients with the same type of histology and provide specific drug regimens, while paying limited attention to the baseline characteristics, genomic subgroups, and tumor microenvironments of patients. Additional improvements in therapy require patient-centered trials in which patients with specific genetic and epigenetic information, RNA profiling, proteomic data, and immune markers are identified, allowing precision combination therapies [169, 170]. The molecular profiling of tissue and blood should be performed and evaluated both at the time of diagnosis and during treatment, to identify variable genetic and epigenetic diversity and monitor the response and resistance. Improved bioinformatics analysis is required to recognize key drivers of carcinogenesis. In PC, the interaction between tumor and stroma is also a significant factor influencing the efficacy of therapies, which require individualized analysis to identify molecular identity [171, 172]. Regarding precision therapy, optimization may require the use of treatment combinations that destroy PC using different mechanisms. Agents targeting KRAS, TP53, CDKN2A, and SMAD4, the four common mutations in PC, are still under development or under clinical investigation [172]. Considering the different modes of action of agents, their optimal dose, schedule, and sequence of administration will have to be determined scientifically and meticulously. Drug delivery, drug metabolism, and AEs for specific patients are also individual factors about which precision therapy will be considered [62].
Conclusions
In the complex PC TME, combining anti-PD-(L)1 with chemotherapy, radiotherapy, molecularly targeted therapies or immunotherapies is challenged by the different characteristics of the different mechanisms and constraints in the TME. The mouse models, study sizes, and drug administration schedules varied across preclinical studies do not faithfully replicate the real world. Different patient selection, treatment dosing, and study designs have been used in clinical studies, resulting in distinctions in efficacy and AEs, which still require adjustment and optimization. For new combination strategies, drug repurposing proposes a promising direction with fewer development costs, shorter development timelines, and lower safety risks. Targeting post-translational modifications of PD-(L)1 has been investigated in preclinical trials and may be combined with anti-PD-(L)1 to improve future treatments. Moreover, precision medicine based on individualized genetic and epigenetic information, RNA profiling, proteomic data, and immune markers can help identify patients who will benefit from anti-PD-(L)1 and provide individually targeted combination strategies.
Acknowledgments
The authors sincerely thank the support of funding, and thank www.biorender.com for figure preparation. Especially, the author L.L. expresses thanks to Dr. Diyu Chen (Zhejiang University) for his ideological inspiration, and Dr. Qinglong Zeng (Zhejiang University) for his critical comments and constructive suggestions for improving this manuscript.
Abbreviations
- ADO
Adenosine
- AE
Adverse effect
- AMP
Adenosine monophosphate
- AMPK
Adenosine-5′-monophosphate-activated protein kinase
- APC
Antigen-presenting cell
- ATM
Ataxia-telangiectasia mutated
- BTK
Bruton’s tyrosine kinase
- B3GNT3
β-1,3-N-acetylglucosaminyl transferase
- CAF
Carcinoma-associated fibroblasts
- CAR
Chimeric antigen receptor
- CDK4
Cyclin D-cyclin-dependent kinase 4
- CMTM6
CKLF-like MARVEL transmembrane domain-containing 6
- CR
Complete response
- CSF1
Colony-stimulating factor 1
- CSN5
Complex subunit 5
- CTLA-4
Cytotoxic T-lymphocyte antigen-4
- CXCL12
CXC-chemokine ligand 12
- CXCR4
CXC-chemokine receptor 4
- DAMP
Damage-associated molecular pattern
- DC
Dendritic cell
- DCR
Disease control rate
- DDR
DNA damage repair
- DLT
Dose-limiting toxicity
- dMMR
Mismatch repair-deficient
- EGF
Epidermal growth factor
- EMT
Epithelial-to-mesenchymal transition
- ER
Endoplasmic reticulum
- ERAD
ER-associated degradation
- FAK
Focal adhesion kinase
- FAP
Fibroblast activation protein
- FDA
Food and drug administration
- FKBP51
FK506 binding protein 51
- FOLFIRINOX
Fluorouracil + leucovorin + irinotecan + oxaliplatin
- GM-CSF
Granulocyte-macrophage colony-stimulating factor
- GSK3β
Glycogen synthase kinase 3β
- HA
Hyaluronic acid
- HAS3
Hyaluronan synthase-3
- HMGB1
High-mobility group protein B1
- hNIS
Human sodium iodide symporter
- ICI
Immune checkpoint inhibitor
- IDO1
Indoleamine 2,3-dioxygenase 1
- IFN
Interferon
- IL-6
Interleukin-6
- irAE
Immune-related adverse event
- IRE
Irreversible electroporation
- MDSC
Myeloid-derived suppressor cell
- MHC
Major histocompatibility complex
- MoDC
Monocyte-derived dendritic cell
- ORR
Objective response rate
- OS
Overall survival
- OV
Oncolytic virus
- PARP
Poly ADP-ribose polymerase
- PC
Pancreatic cancer
- PD
Progressive disease
- PD-1
Programmed cell death protein 1
- PD-L1
Programmed cell death ligand 1
- PEGPH20
PEGylated recombinant hyaluronidase PH20
- PFS
Progression-free survival
- PR
Partial response
- PSC
Pancreatic stellate cell
- PTM
Post-translational modification
- RT
Radiotherapy
- SD
Stable disease
- Sigma1
Sigma nonopioid intracellular receptor 1
- siRNA
Small interfering RNA
- SPOP
Speckle-type POZ protein
- STT3
Staurosporine temperature sensitivity 3
- STUB1
STIP1 homology and U-box containing protein 1
- TAM
Tumor-associated macrophage
- TCR
T cell receptor
- TEAE
Treatment-emergent adverse event
- Teff
Effector T cell
- TGF-β
Transforming growth factor-β
- TIM3
T cell immunoglobulin mucin-3
- TME
Tumor microenvironment
- TNBC
Triple-negative breast cancer
- TNF
Tumor necrosis factor
- Treg
Regulatory T cell
- USP22
Ubiquitin-specific protease 22
- VDR
Vitamin D receptor
- ZDHHC3
Zinc-finger DHHC-type-containing 3
- β-TrCP
β-transducin repeat-containing protein
- 2-BP
2-bromopalmitate
Authors’ contributions
X.B. and T.L. guided the preparation of this manuscript; L.L. and X.H. wrote and edited the manuscript; F.S., J.S., C.G., and J.Y. discussed and revised the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (81871925 and 82071867 to X.B.), the Fundamental Research Funds for the Zhejiang Provincial Universities (2021XZZX031 to X.B.), and the Key Research and Development Program of Zhejiang Province (2020C03117 to X.B.).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lingyue Liu and Xing Huang contributed equally to this work.
Contributor Information
Tingbo Liang, Email: liangtingbo@zju.edu.cn.
Xueli Bai, Email: shirleybai@zju.edu.cn.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 3.Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74(11):2913–2921. doi: 10.1158/0008-5472.CAN-14-0155. [DOI] [PubMed] [Google Scholar]
- 4.Grossberg AJ, Chu LC, Deig CR, Fishman EK, Hwang WL, Maitra A, et al. Multidisciplinary standards of care and recent progress in pancreatic ductal adenocarcinoma. CA Cancer J Clin. 2020. [DOI] [PMC free article] [PubMed]
- 5.Mizrahi JD, Surana R, Valle JW, Shroff RT. Pancreatic cancer. Lancet. 2020;395(10242):2008–2020. doi: 10.1016/S0140-6736(20)30974-0. [DOI] [PubMed] [Google Scholar]
- 6.Nevala-Plagemann C, Hidalgo M, Garrido-Laguna I. From state-of-the-art treatments to novel therapies for advanced-stage pancreatic cancer. Nat Rev Clin Oncol. 2020;17(2):108–123. doi: 10.1038/s41571-019-0281-6. [DOI] [PubMed] [Google Scholar]
- 7.Lai E, Puzzoni M, Ziranu P, Pretta A, Impera V, Mariani S, et al. New therapeutic targets in pancreatic cancer. Cancer Treat Rev. 2019;81:101926. doi: 10.1016/j.ctrv.2019.101926. [DOI] [PubMed] [Google Scholar]
- 8.Sanmamed MF, Chen L. A paradigm shift in Cancer immunotherapy: from enhancement to normalization. Cell. 2018;175(2):313–326. doi: 10.1016/j.cell.2018.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morrison AH, Byrne KT, Vonderheide RH. Immunotherapy and prevention of pancreatic Cancer. Trends Cancer. 2018;4(6):418–428. doi: 10.1016/j.trecan.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weiner GJ. Building better monoclonal antibody-based therapeutics. Nat Rev Cancer. 2015;15(6):361–370. doi: 10.1038/nrc3930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sahin IH, Askan G, Hu ZI, O'Reilly EM. Immunotherapy in pancreatic ductal adenocarcinoma: an emerging entity? Ann Oncol. 2017;28(12):2950–2961. doi: 10.1093/annonc/mdx503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sznol M, Chen L. Antagonist antibodies to PD-1 and B7-H1 (PD-L1) in the treatment of advanced human cancer--response. Clin Cancer Res. 2013;19(19):5542. doi: 10.1158/1078-0432.CCR-13-2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun C, Mezzadra R, Schumacher TN. Regulation and function of the PD-L1 checkpoint. Immunity. 2018;48(3):434–452. doi: 10.1016/j.immuni.2018.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma P, Allison JP. The future of immune checkpoint therapy. Science. 2015;348(6230):56–61. doi: 10.1126/science.aaa8172. [DOI] [PubMed] [Google Scholar]
- 15.Gong J, Chehrazi-Raffle A, Reddi S, Salgia R. Development of PD-1 and PD-L1 inhibitors as a form of cancer immunotherapy: a comprehensive review of registration trials and future considerations. J Immunother Cancer. 2018;6. [DOI] [PMC free article] [PubMed]
- 16.Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27(4):450–461. doi: 10.1016/j.ccell.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharpe AH, Pauken KE. The diverse functions of the PD1 inhibitory pathway. Nat Rev Immunol. 2018;18(3):153–167. doi: 10.1038/nri.2017.108. [DOI] [PubMed] [Google Scholar]
- 18.Feng M, Xiong G, Cao Z, Yang G, Zheng S, Song X, et al. PD-1/PD-L1 and immunotherapy for pancreatic cancer. Cancer Lett. 2017;407:57–65. doi: 10.1016/j.canlet.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 19.Gong J, Hendifar A, Tuli R, Chuang J, Cho M, Chung V, et al. Combination systemic therapies with immune checkpoint inhibitors in pancreatic cancer: overcoming resistance to single-agent checkpoint blockade. Clin Transl Med. 2018;7(1):32. doi: 10.1186/s40169-018-0210-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455–2465. doi: 10.1056/NEJMoa1200694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herbst RS, Soria JC, Kowanetz M, Fine GD, Hamid O, Gordon MS, et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014;515(7528):563–567. doi: 10.1038/nature14011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patnaik A, Kang SP, Rasco D, Papadopoulos KP, Elassaiss-Schaap J, Beeram M, et al. Phase I study of Pembrolizumab (MK-3475; anti-PD-1 monoclonal antibody) in patients with advanced solid tumors. Clin Cancer Res. 2015;21(19):4286–4293. doi: 10.1158/1078-0432.CCR-14-2607. [DOI] [PubMed] [Google Scholar]
- 23.Conroy T, Desseigne F, Ychou M, Bouche O, Guimbaud R, Becouarn Y, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817–1825. doi: 10.1056/NEJMoa1011923. [DOI] [PubMed] [Google Scholar]
- 24.Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691–1703. doi: 10.1056/NEJMoa1304369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Von Hoff DD, Ramanathan RK, Borad MJ, Laheru DA, Smith LS, Wood TE, et al. Gemcitabine plus nab-paclitaxel is an active regimen in patients with advanced pancreatic cancer: a phase I/II trial. J Clin Oncol. 2011;29(34):4548–4554. doi: 10.1200/JCO.2011.36.5742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weiss GJ, Waypa J, Blaydorn L, Coats J, McGahey K, Sangal A, et al. A phase Ib study of pembrolizumab plus chemotherapy in patients with advanced cancer (PembroPlus) Br J Cancer. 2017;117(1):33–40. doi: 10.1038/bjc.2017.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Michelakos T, Cai L, Villani V, Sabbatino F, Kontos F, Fernandez-Del Castillo C, et al. Tumor microenvironment immune response in pancreatic ductal adenocarcinoma patients treated with neoadjuvant therapy. J Natl Cancer Inst. 2021;113(2):182–191. doi: 10.1093/jnci/djaa073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu MY, Shen M, Xu MD, Yu ZY, Tao M. FOLFIRINOX regulated tumor immune microenvironment to extend the survival of patients with resectable pancreatic ductal adenocarcinoma. Gland Surg. 2020;9(6):2125–2135. doi: 10.21037/gs-20-828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown JS, Sundar R, Lopez J. Combining DNA damaging therapeutics with immunotherapy: more haste, less speed. Br J Cancer. 2018;118(3):312–324. doi: 10.1038/bjc.2017.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sheng J, Fang W, Yu J, Chen N, Zhan J, Ma Y, et al. Expression of programmed death ligand-1 on tumor cells varies pre and post chemotherapy in non-small cell lung cancer. Sci Rep. 2016;6:20090. doi: 10.1038/srep20090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Doi T, Ishikawa T, Okayama T, Oka K, Mizushima K, Yasuda T, et al. The JAK/STAT pathway is involved in the upregulation of PD-L1 expression in pancreatic cancer cell lines. Oncol Rep 2017;37(3):1545–54. [DOI] [PubMed]
- 32.Brooks J, Fleischmann-Mundt B, Woller N, Niemann J, Ribback S, Peters K, et al. Perioperative, spatiotemporally coordinated activation of T and NK cells prevents recurrence of pancreatic cancer. Cancer Res. 2018;78(2):475–488. doi: 10.1158/0008-5472.CAN-17-2415. [DOI] [PubMed] [Google Scholar]
- 33.Nomi T, Sho M, Akahori T, Hamada K, Kubo A, Kanehiro H, et al. Clinical significance and therapeutic potential of the programmed death-1 ligand/programmed death-1 pathway in human pancreatic cancer. Clin Cancer Res. 2007;13(7):2151–2157. doi: 10.1158/1078-0432.CCR-06-2746. [DOI] [PubMed] [Google Scholar]
- 34.Bozeman EN, Gao N, Qian W, Wang A, Yang L. Synergistic effect of targeted chemotherapy delivery using theranostic nanoparticles and PD-L1 blockade in an orthotopic mouse pancreatic cancer model. Cancer Immunol Res. 2015;3(10 Supplement):A60. [Google Scholar]
- 35.Ahmad G, Mackenzie GG, Egan J, Amiji MM. DHA-SBT-1214 Taxoid Nanoemulsion and anti-PD-L1 antibody combination therapy enhances antitumor efficacy in a syngeneic pancreatic adenocarcinoma model. Mol Cancer Ther. 2019;18(11):1961–1972. doi: 10.1158/1535-7163.MCT-18-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weiss GJ, Blaydorn L, Beck J, Bornemann-Kolatzki K, Urnovitz H, Schutz E, et al. Phase Ib/II study of gemcitabine, nab-paclitaxel, and pembrolizumab in metastatic pancreatic adenocarcinoma. Invest New Drugs. 2018;36(1):96–102. doi: 10.1007/s10637-017-0525-1. [DOI] [PubMed] [Google Scholar]
- 37.Wainberg ZA, Hochster HS, Kim EJ, George B, Kaylan A, Chiorean EG, et al. Open-label, phase 1 study of Nivolumab combined with nab-paclitaxel plus gemcitabine in advanced pancreatic Cancer. Clin Cancer Res. 2020. [DOI] [PubMed]
- 38.Shui L, Cheng K, Li X, Shui P, Li S, Peng Y, et al. Durable response and good tolerance to the triple combination of Toripalimab, gemcitabine, and nab-paclitaxel in a patient with metastatic pancreatic ductal adenocarcinoma. Front Immunol. 2020;11:1127. doi: 10.3389/fimmu.2020.01127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shui L, Cheng K, Li X, Shui P, Zhou X, Li J, et al. Study protocol for an open-label, single-arm, phase Ib/II study of combination of toripalimab, nab-paclitaxel, and gemcitabine as the first-line treatment for patients with unresectable pancreatic ductal adenocarcinoma. BMC Cancer. 2020;20(1). [DOI] [PMC free article] [PubMed]
- 40.Hosein AN, Brekken RA, Maitra A. Pancreatic cancer stroma: an update on therapeutic targeting strategies. Nat Rev Gastroenterol Hepatol. 2020;17(8):487–505. doi: 10.1038/s41575-020-0300-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tempero MA. NCCN guidelines updates: pancreatic Cancer. J Natl Compr Canc Ne. 2019;17(5):603–605. doi: 10.6004/jnccn.2019.5007. [DOI] [PubMed] [Google Scholar]
- 42.Toesca DAS, Koong AJ, Poultsides GA, Visser BC, Haraldsdottir S, Koong AC, et al. Management of Borderline Resectable Pancreatic Cancer. Int J Radiat Oncol Biol Phys. 2018;100(5):1155–1174. doi: 10.1016/j.ijrobp.2017.12.287. [DOI] [PubMed] [Google Scholar]
- 43.Mellon EA, Hoffe SE, Springett GM, Frakes JM, Strom TJ, Hodul PJ, et al. Long-term outcomes of induction chemotherapy and neoadjuvant stereotactic body radiotherapy for borderline resectable and locally advanced pancreatic adenocarcinoma. Acta Oncol. 2015;54(7):979–985. doi: 10.3109/0284186X.2015.1004367. [DOI] [PubMed] [Google Scholar]
- 44.Weichselbaum RR, Liang H, Deng L, Fu YX. Radiotherapy and immunotherapy: a beneficial liaison? Nat Rev Clin Oncol. 2017;14(6):365–379. doi: 10.1038/nrclinonc.2016.211. [DOI] [PubMed] [Google Scholar]
- 45.Sharabi AB, Lim M, DeWeese TL, Drake CG. Radiation and checkpoint blockade immunotherapy: radiosensitisation and potential mechanisms of synergy. Lancet Oncol. 2015;16(13):e498–e509. doi: 10.1016/S1470-2045(15)00007-8. [DOI] [PubMed] [Google Scholar]
- 46.Fujiwara K, Saung MT, Jing H, Herbst B, Zarecki M, Muth S, et al. Interrogating the immune-modulating roles of radiation therapy for a rational combination with immune-checkpoint inhibitors in treating pancreatic cancer. J Immunother Cancer. 2020;8(2). [DOI] [PMC free article] [PubMed]
- 47.Azad A, Yin Lim S, D'Costa Z, Jones K, Diana A, Sansom OJ, et al. PD-L1 blockade enhances response of pancreatic ductal adenocarcinoma to radiotherapy. EMBO Mol Med. 2017;9(2):167–180. doi: 10.15252/emmm.201606674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee YH, Yu CF, Yang YC, Hong JH, Chiang CS. Ablative radiotherapy reprograms the tumor microenvironment of a pancreatic tumor in favoring the immune checkpoint blockade therapy. Int J Mol Sci. 2021;22(4). [DOI] [PMC free article] [PubMed]
- 49.Zhang Q, Green MD, Lang X, Lazarus J, Parsels JD, Wei S, et al. Inhibition of ATM increases interferon signaling and sensitizes pancreatic Cancer to immune checkpoint blockade therapy. Cancer Res. 2019;79(15):3940–3951. doi: 10.1158/0008-5472.CAN-19-0761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tuli R, Nissen N, Lo S, Tighiouart M, Placencio V, Hendifar A. A phase I/II study of durvalumab and stereotactic radiotherapy in locally advanced pancreatic cancer. Cancer Res. 2019;79(24).
- 51.McCarthy PM, Rendo MJ, Uy MD, Adams AM, O'Shea AE, Nelson DW, et al. Near complete pathologic response to PD-1 inhibitor and radiotherapy in a patient with locally advanced pancreatic ductal adenocarcinoma. Onco Targets Ther. 2021;14:3537–3544. doi: 10.2147/OTT.S311661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maity A, Mick R, Huang AC, George SM, Farwell MD, Lukens JN, et al. A phase I trial of pembrolizumab with hypofractionated radiotherapy in patients with metastatic solid tumours. Br J Cancer. 2018;119(10):1200–1207. doi: 10.1038/s41416-018-0281-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Katz MHG, Varadhachary GR, Bauer TW, Acquavella N, Merchant NB, Le TM, et al. Preliminary safety data from a randomized multicenter phase Ib/II study of neoadjuvant chemoradiation therapy (CRT) alone or in combination with pembrolizumab in patients with resectable or borderline resectable pancreatic cancer. J Clin Oncol 2017;35(15_suppl):4125-.
- 54.Wirsdorfer F, Cappuccini F, Niazman M, de Leve S, Westendorf AM, Ludemann L, et al. Thorax irradiation triggers a local and systemic accumulation of immunosuppressive CD4+ FoxP3+ regulatory T cells. Radiat Oncol. 2014;9:98. doi: 10.1186/1748-717X-9-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vanpouille-Box C, Alard A, Aryankalayil MJ, Sarfraz Y, Diamond JM, Schneider RJ, et al. DNA exonuclease Trex1 regulates radiotherapy-induced tumour immunogenicity. Nat Commun. 2017;8:15618. doi: 10.1038/ncomms15618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Han CY, Liu QY, Sheng LJ. Advances in mechanism and overview of clinical trials of combined radiotherapy and immunotherapy. Chinese journal of cancer prevention and treatment. 2019;26(18):1317–1322. [Google Scholar]
- 57.Chen ZT, Cao K, Li WH. Progress of radiotherapy combined with immune checkpoint inhibitors in advanced non-small cell lung cancer. J Cancer Control Treat. 2019;32(1):86–92. [Google Scholar]
- 58.Jiang C, Davalos RV, Bischof JC. A review of basic to clinical studies of irreversible electroporation therapy. IEEE Trans Biomed Eng. 2015;62(1):4–20. doi: 10.1109/TBME.2014.2367543. [DOI] [PubMed] [Google Scholar]
- 59.Zhao J, Wen X, Tian L, Li T, Xu C, Wen X, et al. Irreversible electroporation reverses resistance to immune checkpoint blockade in pancreatic cancer. Nat Commun. 2019;10(1):899. doi: 10.1038/s41467-019-08782-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.O'Neill C, Hayat T, Hamm J, Healey M, Zheng Q, Li Y, et al. A phase 1b trial of concurrent immunotherapy and irreversible electroporation in the treatment of locally advanced pancreatic adenocarcinoma. Surgery. 2020;168(4):610–616. doi: 10.1016/j.surg.2020.04.057. [DOI] [PubMed] [Google Scholar]
- 61.Christenson ES, Jaffee E, Azad NS. Current and emerging therapies for patients with advanced pancreatic ductal adenocarcinoma: a bright future. Lancet Oncol. 2020;21(3):e135–ee45. doi: 10.1016/S1470-2045(19)30795-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Looi CK, Chung FF, Leong CO, Wong SF, Rosli R, Mai CW. Therapeutic challenges and current immunomodulatory strategies in targeting the immunosuppressive pancreatic tumor microenvironment. J Exp Clin Cancer Res. 2019;38(1):162. doi: 10.1186/s13046-019-1153-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Blair AB, Kim VM, Muth ST, Saung MT, Lokker N, Blouw B, et al. Dissecting the stromal signaling and regulation of myeloid cells and memory effector T cells in pancreatic Cancer. Clin Cancer Res. 2019;25(17):5351. doi: 10.1158/1078-0432.CCR-18-4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rosengren S, Clift R, Zimmerman SJ, Souratha J, Thompson BJ, Blouw B, et al. PEGylated recombinant hyaluronidase PH20 (PEGPH20) enhances checkpoint inhibitor efficacy in syngeneic mouse models of cancer. Cancer Res. 2016;76(14 Supplement):4886. [Google Scholar]
- 65.Chiorean EG, Ritch PS, Zhen DB, Poplin E, George B, Hendifar AE, et al. PCRT16-001: phase II study of PEGPH20 plus pembrolizumab for patients (pts) with hyaluronan (HA)-high refractory metastatic pancreatic ductal adenocarcinoma (mPDA). J Clin Oncol 2020;38(4_suppl):TPS785-TPS.
- 66.Zhang Y, Yan W, Collins MA, Bednar F, Rakshit S, Zetter BR, et al. Interleukin-6 is required for pancreatic cancer progression by promoting MAPK signaling activation and oxidative stress resistance. Cancer Res. 2013;73(20):6359–6374. doi: 10.1158/0008-5472.CAN-13-1558-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Goumas FA, Holmer R, Egberts JH, Gontarewicz A, Heneweer C, Geisen U, et al. Inhibition of IL-6 signaling significantly reduces primary tumor growth and recurrencies in orthotopic xenograft models of pancreatic cancer. Int J Cancer. 2015;137(5):1035–1046. doi: 10.1002/ijc.29445. [DOI] [PubMed] [Google Scholar]
- 68.Fisher DT, Appenheimer MM, Evans SS. The two faces of IL-6 in the tumor microenvironment. Semin Immunol. 2014;26(1):38–47. doi: 10.1016/j.smim.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Corcoran RB, Contino G, Deshpande V, Tzatsos A, Conrad C, Benes CH, et al. STAT3 plays a critical role in KRAS-induced pancreatic tumorigenesis. Cancer Res. 2011;71(14):5020–5029. doi: 10.1158/0008-5472.CAN-11-0908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mace TA, Shakya R, Pitarresi JR, Swanson B, McQuinn CW, Loftus S, et al. IL-6 and PD-L1 antibody blockade combination therapy reduces tumour progression in murine models of pancreatic cancer. Gut. 2018;67(2):320–332. doi: 10.1136/gutjnl-2016-311585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ferrer M, Connell C, Flint T, Biasci D, Janowitz T. Combined administration of anti-IL6 and anti-PDL1 antibodies prevents ketogenic failure, reduces tumour progression, and increases overall survival in an autochthonous murine pancreatic cancer model. J Cachexia Sarcopenia Muscle. 2018;9(6):1170. [Google Scholar]
- 72.Narazaki M, Tanaka T, Kishimoto T. The role and therapeutic targeting of IL-6 in rheumatoid arthritis. Expert Rev Clin Immunol. 2017;13(6):535–551. doi: 10.1080/1744666X.2017.1295850. [DOI] [PubMed] [Google Scholar]
- 73.Sherman MH, Yu RT, Engle DD, Ding N, Atkins AR, Tiriac H, et al. Vitamin D receptor-mediated stromal reprogramming suppresses pancreatitis and enhances pancreatic cancer therapy. Cell. 2014;159(1):80–93. doi: 10.1016/j.cell.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Borazanci EH, Jameson G, Korn RL, Caldwell L, Ansaldo K, Hendrickson K, et al. A phase II pilot trial of nivolumab (N) + albumin bound paclitaxel (AP) + paricalcitol (P) + cisplatin (C) + gemcitabine (G) (NAPPCG) in patients with previously untreated metastatic pancreatic ductal adenocarcinoma (PDAC). Cancer Res. 2019;79(13 Supplement) CT152.
- 75.Mariathasan S, Turley SJ, Nickles D, Castiglioni A, Yuen K, Wang Y, et al. TGFbeta attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature. 2018;554(7693):544–548. doi: 10.1038/nature25501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tauriello DVF, Palomo-Ponce S, Stork D, Berenguer-Llergo A, Badia-Ramentol J, Iglesias M, et al. TGFbeta drives immune evasion in genetically reconstituted colon cancer metastasis. Nature. 2018;554(7693):538–543. doi: 10.1038/nature25492. [DOI] [PubMed] [Google Scholar]
- 77.Wang Y, Gao Z, Du X, Chen S, Zhang W, Wang J, et al. Co-inhibition of the TGF-beta pathway and the PD-L1 checkpoint by pH-responsive clustered nanoparticles for pancreatic cancer microenvironment regulation and anti-tumor immunotherapy. Biomater Sci. 2020;8(18):5121–5132. doi: 10.1039/d0bm00916d. [DOI] [PubMed] [Google Scholar]
- 78.Strauss J, Heery CR, Schlom J, Madan RA, Cao L, Kang Z, et al. Phase I trial of M7824 (MSB0011359C), a bifunctional fusion protein targeting PD-L1 and TGFbeta. Advanced Solid Tumors Clin Cancer Res. 2018;24(6):1287–1295. doi: 10.1158/1078-0432.CCR-17-2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Melisi D, Hollebecque A, Oh DY, Calvo E, Varghese AM, Borazanci EH, et al. A phase Ib dose-escalation and cohort-expansion study of safety and activity of the transforming growth factor (TGF) β receptor I kinase inhibitor galunisertib plus the anti-PD-LI antibody durvalumab in metastatic pancreatic cancer. J Clin Oncol. 2019;37. [DOI] [PMC free article] [PubMed]
- 80.Zhu Y, Knolhoff BL, Meyer MA, Nywening TM, West BL, Luo J, et al. CSF1/CSF1R blockade reprograms tumor-infiltrating macrophages and improves response to T-cell checkpoint immunotherapy in pancreatic cancer models. Cancer Res. 2014;74(18):5057–5069. doi: 10.1158/0008-5472.CAN-13-3723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Brahmer J, Rasco D, Chen M, Masteller E, Qazi I, Rogers S, et al. A phase 1a/1b study of FPA008 in combination with nivolumab in patients with selected advanced cancers. Cancer immunology. Research. 2016;4(1).
- 82.Wainberg Z, Piha-Paul S, Luke J, Kim E, Thompson J, Pfanzelter N, et al. First-in-human phase 1 dose escalation and expansion of a novel combination, anti-CSF-1 receptor (cabiralizumab) plus anti-PD-1 (nivolumab), in patients with advanced solid tumors. Journal for ImmunoTherapy of. Cancer. 2017;5.
- 83.Calvo A, Joensuu H, Sebastian M, Naing A, Bang Y-J, Martin M, et al. Phase Ib/II study of lacnotuzumab (MCS110) combined with spartalizumab (PDR001) in patients (pts) with advanced tumors. J Clin Oncol 2018;36(15_suppl):3014-.
- 84.Vonderheide RH. CD40 agonist antibodies in Cancer immunotherapy. Annu Rev Med. 2020;71:47–58. doi: 10.1146/annurev-med-062518-045435. [DOI] [PubMed] [Google Scholar]
- 85.Luheshi NM, Coates-Ulrichsen J, Harper J, Mullins S, Sulikowski MG, Martin P, et al. Transformation of the tumour microenvironment by a CD40 agonist antibody correlates with improved responses to PD-L1 blockade in a mouse orthotopic pancreatic tumour model. Oncotarget. 2016;7(14):18508–18520. doi: 10.18632/oncotarget.7610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Winograd R, Byrne KT, Evans RA, Odorizzi PM, Meyer AR, Bajor DL, et al. Induction of T-cell immunity overcomes complete resistance to PD-1 and CTLA-4 blockade and improves survival in pancreatic carcinoma. Cancer Immunol Res. 2015;3(4):399–411. doi: 10.1158/2326-6066.CIR-14-0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rech AJ, Dada H, Kotzin JJ, Henao-Mejia J, Minn AJ, Twyman-Saint Victor C, et al. Radiotherapy and CD40 activation separately augment immunity to checkpoint blockade in Cancer. Cancer Res. 2018;78(15):4282–4291. doi: 10.1158/0008-5472.CAN-17-3821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.O'Hara MH, O'Reilly EM, Varadhachary G, Wolff RA, Wainberg ZA, Ko AH, et al. CD40 agonistic monoclonal antibody APX005M (sotigalimab) and chemotherapy, with or without nivolumab, for the treatment of metastatic pancreatic adenocarcinoma: an open-label, multicentre, phase 1b study. Lancet Oncol. 2021;22(1):118–131. doi: 10.1016/S1470-2045(20)30532-5. [DOI] [PubMed] [Google Scholar]
- 89.Neoptolemos JP, Kleeff J, Michl P, Costello E, Greenhalf W, Palmer DH. Therapeutic developments in pancreatic cancer: current and future perspectives. Nature Reviews Gastroenterology and Hepatology. 2018;15(6):333–348. doi: 10.1038/s41575-018-0005-x. [DOI] [PubMed] [Google Scholar]
- 90.Feig C, Jones JO, Kraman M, Wells RJ, Deonarine A, Chan DS, et al. Targeting CXCL12 from FAP-expressing carcinoma-associated fibroblasts synergizes with anti-PD-L1 immunotherapy in pancreatic cancer. Proc Natl Acad Sci U S A. 2013;110(50):20212–20217. doi: 10.1073/pnas.1320318110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Seo YD, Jiang X, Sullivan KM, Jalikis FG, Smythe KS, Abbasi A, et al. Mobilization of CD8+ T cells via CXCR4 blockade facilitates PD-1 checkpoint therapy in human pancreatic Cancer. Clin Cancer Res. 2019;25(13):3934. doi: 10.1158/1078-0432.CCR-19-0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Peled A. Combination of BL-8040, anti PD-1 and chemotherapy significantly reduced pancreatic tumor growth and changed the balance between CD4+/FOXP3+ cells and CD8+ cells in the tumor. Journal for ImmunoTherapy of. Cancer. 2019;7.
- 93.Halama N, Williams A, Suarez-Carmona M, Schreiber J, Hohmann N, Pruefer U, et al. Phase I/II study with CXCL12 inhibitor NOX-A12 and pembrolizumab in patients with microsatellite-stable, metastatic colorectal or pancreatic cancer. Ann Oncol. 2020;31:S944. [Google Scholar]
- 94.Fogelman D, Overman M, Wolff R, Javle M, Pant S, Varadhachary G, et al. A phase IIB study of pembrolizumab plus BL-8040 in metastatic pancreatic cancer: clinical outcomes and biological correlates. Journal for ImmunoTherapy of. Cancer. 2019;7.
- 95.Bockorny B, Semenisty V, Macarulla T, Borazanci E, Wolpin BM, Stemmer SM, et al. BL-8040, a CXCR4 antagonist, in combination with pembrolizumab and chemotherapy for pancreatic cancer: the COMBAT trial. Nat Med. 2020;26(6):878–885. doi: 10.1038/s41591-020-0880-x. [DOI] [PubMed] [Google Scholar]
- 96.Steele CW, Karim SA, Leach JDG, Bailey P, Upstill-Goddard R, Rishi L, et al. CXCR2 inhibition profoundly suppresses metastases and augments immunotherapy in pancreatic ductal adenocarcinoma. Cancer Cell. 2016;29(6):832–845. doi: 10.1016/j.ccell.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ullman NA, Ruffolo LI, Jackson KM, Chacon A, Georger M, Jewell R, et al. CXCR1/2 blockade to enhance response to immune checkpoint inhibition in an aggressive orthotopic pancreatic adenocarcinoma model. J Clin Oncol 2020;38(5_suppl):19-.
- 98.Le TM, Udyavar A, Kim W, Cho AE, Li L, DiRenzo D, et al. CD73 inhibition enhances the effect of anti-PD-1 therapy on KRAS-mutated pancreatic cancer model. Cancer Immunol Res. 2020;8(3 Supplement):A46. [Google Scholar]
- 99.Turiello R, Capone M, Giannarelli D, Morretta E, Monti MC, Madonna G, et al. Serum CD73 is a prognostic factor in patients with metastatic melanoma and is associated with response to anti-PD-1 therapy. J Immunother Cancer. 2020;8(2). [DOI] [PMC free article] [PubMed]
- 100.Allard B, Pommey S, Smyth MJ, Stagg J. Targeting CD73 enhances the antitumor activity of anti-PD-1 and anti-CTLA-4 mAbs. Clin Cancer Res. 2013;19(20):5626–5635. doi: 10.1158/1078-0432.CCR-13-0545. [DOI] [PubMed] [Google Scholar]
- 101.Zhao XK, Cheng Y, Liang Cheng M, Yu L, Mu M, Li H, et al. Focal adhesion kinase regulates fibroblast migration via integrin beta-1 and plays a central role in fibrosis. Sci Rep. 2016;6:19276. doi: 10.1038/srep19276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jiang H, Hegde S, Knolhoff BL, Zhu Y, Herndon JM, Meyer MA, et al. Targeting focal adhesion kinase renders pancreatic cancers responsive to checkpoint immunotherapy. Nat Med. 2016;22(8):851–860. doi: 10.1038/nm.4123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wang-Gillam A, Lockhart AC, Tan BR, Suresh R, Lim K-H, Ratner L, et al. Phase I study of defactinib combined with pembrolizumab and gemcitabine in patients with advanced cancer. J Clin Oncol 2018;36(15_suppl):2561-.
- 104.Gunderson AJ, Kaneda MM, Tsujikawa T, Nguyen AV, Affara NI, Ruffell B, et al. Bruton tyrosine kinase-dependent immune cell cross-talk drives pancreas Cancer. Cancer Discov. 2016;6(3):270–285. doi: 10.1158/2159-8290.CD-15-0827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Overman M, Javle M, Davis RE, Vats P, Kumar-Sinha C, Xiao L, et al. Randomized phase II study of the Bruton tyrosine kinase inhibitor acalabrutinib, alone or with pembrolizumab in patients with advanced pancreatic cancer. J Immunother Cancer. 2020;8(1). [DOI] [PMC free article] [PubMed]
- 106.Hong D, Rasco D, Veeder M, Luke JJ, Chandler J, Balmanoukian A, et al. A phase 1b/2 study of the Bruton tyrosine kinase inhibitor Ibrutinib and the PD-L1 inhibitor Durvalumab in patients with pretreated solid tumors. Oncology. 2019;97(2):102–111. doi: 10.1159/000500571. [DOI] [PubMed] [Google Scholar]
- 107.Friedlander M, Meniawy T, Markman B, Mileshkin LR, Harnett PR, Millward M, et al. A phase 1b study of the anti-PD-1 monoclonal antibody BGB-A317 (A317) in combination with the PARP inhibitor BGB-290 (290) in advanced solid tumors. J Clin Oncol 2017;35(15_suppl):3013-.
- 108.Gabrail NY, Bessudo A, Hamilton EP, Sachdev JC, Patel MR, Rodon Ahnert J, et al. IOLite: multipart, phase 1b, dose-finding study of the PD-1 inhibitor dostarlimab in combination with the PARP inhibitor niraparib ± bevacizumab (bev), or with platinum-based chemotherapy ± bev for advanced cancer. J Clin Oncol 2019;37(15_suppl):2560-.
- 109.Kabacaoglu D, Ciecielski KJ, Ruess DA, Algul H. Immune checkpoint inhibition for pancreatic ductal adenocarcinoma: current limitations and future options. Front Immunol. 2018;9:1878. doi: 10.3389/fimmu.2018.01878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12(4):252–264. doi: 10.1038/nrc3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Terrero G, Pollack T, Sussman DA, Lockhart AC, Hosein PJ. Exceptional responses to ipilimumab/nivolumab (ipi/nivo) in patients (pts) with refractory pancreatic ductal adenocarcinoma (PDAC) and germline BRCA or RAD51 mutations. J Clin Oncol 2020;38(4_suppl):754-.
- 112.Parikh A, Clark J, Wo J, Yeap B, Allen J, Blaszkowsky L, et al. Proof of concept of the abscopal effect in MSS GI cancers: A phase 2 study of ipilimumab and nivolumab with radiation in metastatic pancreatic and colorectal adenocarcinoma. Annals of oncology : official journal of the European Society for Medical Oncology. 2019;30(Suppl 4):iv128. [Google Scholar]
- 113.O'Reilly EM, Oh D-Y, Dhani N, Renouf DJ, Lee MA, Sun W, et al. A randomized phase 2 study of durvalumab monotherapy and in combination with tremelimumab in patients with metastatic pancreatic ductal adenocarcinoma (mPDAC): ALPS study. J Clin Oncol. 2018;36(4_suppl):217. [Google Scholar]
- 114.Renouf DJ, Dhani NC, Kavan P, Jonker DJ, AC-c W, Hsu T, et al. The Canadian Cancer trials group PA.7 trial: results from the safety run in of a randomized phase II study of gemcitabine (GEM) and nab-paclitaxel (nab-P) versus GEM, nab-P, durvalumab (D), and tremelimumab (T) as first-line therapy in metastatic pancreatic ductal adenocarcinoma (mPDAC) J Clin Oncol. 2018;36(4_suppl):349. [Google Scholar]
- 115.Wei SC, Anang NAS, Sharma R, Andrews MC, Reuben A, Levine JH, et al. Combination anti-CTLA-4 plus anti-PD-1 checkpoint blockade utilizes cellular mechanisms partially distinct from monotherapies. Proc Natl Acad Sci U S A. 2019;116(45):22699–22709. doi: 10.1073/pnas.1821218116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Prendergast GC, Malachowski WP, DuHadaway JB, Muller AJ. Discovery of IDO1 inhibitors: from bench to bedside. Cancer Res. 2017;77(24):6795–6811. doi: 10.1158/0008-5472.CAN-17-2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zhai L, Ladomersky E, Lenzen A, Nguyen B, Patel R, Lauing KL, et al. IDO1 in cancer: a Gemini of immune checkpoints. Cell Mol Immunol. 2018;15(5):447–457. doi: 10.1038/cmi.2017.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Fujiwara Y, Shitara K, Shimizu T, Yonemori K, Matsubara N, Ohno I, et al. INCB024360 (Epacadostat) monotherapy and in combination with pembrolizumab in patients with advanced solid tumors: primary results from first-in-Japanese phase I study (KEYNOTE-434) Mol Cancer Ther. 2018;17(1 Supplement):A204. [Google Scholar]
- 119.Jung KH, LoRusso P, Burris H, Gordon M, Bang Y-J, Hellmann MD, et al. Phase I study of the Indoleamine 2,3-dioxygenase 1 (IDO1) inhibitor Navoximod (GDC-0919) administered with PD-L1 inhibitor (Atezolizumab) in advanced solid tumors. Clin Cancer Res. 2019;25(11):3220. doi: 10.1158/1078-0432.CCR-18-2740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kershaw MH, Westwood JA, Darcy PK. Gene-engineered T cells for cancer therapy. Nat Rev Cancer. 2013;13(8):525–541. doi: 10.1038/nrc3565. [DOI] [PubMed] [Google Scholar]
- 121.Kershaw MH, Westwood JA, Slaney CY, Darcy PK. Clinical application of genetically modified T cells in cancer therapy. Clin Transl Immunology. 2014;3(5):e16. doi: 10.1038/cti.2014.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Parriott G, Deal K, Crean S, Richardson E, Nylen E, Barber A. T-cells expressing a chimeric-PD1-Dap10-CD3zeta receptor reduce tumour burden in multiple murine syngeneic models of solid cancer. Immunology. 2020;160(3):280–294. doi: 10.1111/imm.13187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yang CY, Fan MH, Miao CH, Liao YJ, Yuan RH, Liu CL. Engineering chimeric antigen receptor T cells against immune checkpoint inhibitors PD-1/PD-L1 for treating pancreatic Cancer. Mol Ther Oncolytics. 2020;17:571–585. doi: 10.1016/j.omto.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Beatty GL, O'Hara MH, Lacey SF, Torigian DA, Nazimuddin F, Chen F, et al. Activity of Mesothelin-specific chimeric antigen receptor T cells against pancreatic carcinoma metastases in a phase 1 trial. Gastroenterology. 2018;155(1):29–32. doi: 10.1053/j.gastro.2018.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Thistlethwaite FC, Gilham DE, Guest RD, Rothwell DG, Pillai M, Burt DJ, et al. The clinical efficacy of first-generation carcinoembryonic antigen (CEACAM5)-specific CAR T cells is limited by poor persistence and transient pre-conditioning-dependent respiratory toxicity. Cancer Immunol Immunother. 2017;66(11):1425–1436. doi: 10.1007/s00262-017-2034-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Posey AD, Jr, Schwab RD, Boesteanu AC, Steentoft C, Mandel U, Engels B, et al. Engineered CAR T cells targeting the Cancer-associated Tn-Glycoform of the membrane mucin MUC1 control adenocarcinoma. Immunity. 2016;44(6):1444–1454. doi: 10.1016/j.immuni.2016.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Feng K, Liu Y, Guo Y, Qiu J, Wu Z, Dai H, et al. Phase I study of chimeric antigen receptor modified T cells in treating HER2-positive advanced biliary tract cancers and pancreatic cancers. Protein Cell. 2018;9(10):838–847. doi: 10.1007/s13238-017-0440-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Henze J, Tacke F, Hardt O, Alves F, Al RW. Enhancing the efficacy of CAR T cells in the tumor microenvironment of pancreatic Cancer. Cancers (Basel). 2020;12(6). [DOI] [PMC free article] [PubMed]
- 129.Kleponis J, Skelton R, Zheng L. Fueling the engine and releasing the break: combinational therapy of cancer vaccines and immune checkpoint inhibitors. Cancer Biol Med. 2015;12(3):201–208. doi: 10.7497/j.issn.2095-3941.2015.0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Luo WH, Yang G, Luo WT, Cao Z, Liu YZ, Qiu JD, et al. Novel therapeutic strategies and perspectives for metastatic pancreatic cancer: vaccine therapy is more than just a theory. Cancer Cell Int. 2020;20(1). [DOI] [PMC free article] [PubMed]
- 131.Palucka K, Ueno H, Fay J, Banchereau J. Dendritic cells and immunity against cancer. J Intern Med. 2011;269(1):64–73. doi: 10.1111/j.1365-2796.2010.02317.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Nesselhut J, Marx D, Cillien N, Lange H, Regalo G, Herrmann M, et al. Dendritic cells generated with PDL-1 checkpoint blockade for treatment of advanced pancreatic cancer. J Clin Oncol 2015;33(15_suppl):4128-.
- 133.Nesselhut J, Marx D, Lange H, Regalo G, Cillien N, Chang RY, et al. Systemic treatment with anti-PD-1 antibody nivolumab in combination with vaccine therapy in advanced pancreatic cancer. J Clin Oncol. 2016;34(15_suppl):3092. [Google Scholar]
- 134.Bassani-Sternberg M, Digklia A, Huber F, Wagner D, Sempoux C, Stevenson BJ, et al. A phase Ib study of the combination of personalized autologous dendritic cell vaccine, aspirin, and standard of care adjuvant chemotherapy followed by Nivolumab for resected pancreatic adenocarcinoma-a proof of antigen discovery feasibility in three patients. Front Immunol. 2019;10:1832. doi: 10.3389/fimmu.2019.01832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Chen J, Liu H, Jehng T, Li Y, Chen Z, Lee KD, et al. A novel anti-PD-L1 vaccine for Cancer immunotherapy and Immunoprevention. Cancers (Basel). 2019;11(12). [DOI] [PMC free article] [PubMed]
- 136.Soares KC, Rucki AA, Wu AA, Olino K, Xiao Q, Chai Y, et al. PD-1/PD-L1 blockade together with vaccine therapy facilitates effector T-cell infiltration into pancreatic tumors. J Immunother. 2015;38(1):1–11. doi: 10.1097/CJI.0000000000000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Muth ST, Saung MT, Blair AB, Henderson MG, Thomas DL, Zheng L. CD137 agonist-based combination immunotherapy enhances activated, effector memory T cells and prolongs survival in pancreatic adenocarcinoma. Cancer Lett. 2020. [DOI] [PMC free article] [PubMed]
- 138.Ma HS, Torres ER, Poudel B, Robinson T, Christmas B, Cruz K, et al. Combination CD40 agonist and PD-1 antagonist antibody therapy enhances vaccine induced T cell responses in non-immunogenic cancers. Cancer Res. 2018;78(13 Supplement):4936. [Google Scholar]
- 139.Guo ZS, Liu Z, Kowalsky S, Feist M, Kalinski P, Lu B, et al. Oncolytic immunotherapy: conceptual evolution, current strategies, and future perspectives. Front Immunol. 2017;8:555. doi: 10.3389/fimmu.2017.00555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Raja J, Ludwig JM, Gettinger SN, Schalper KA, Kim HS. Oncolytic virus immunotherapy: future prospects for oncology. J Immunother Cancer. 2018;6(1):140. doi: 10.1186/s40425-018-0458-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wang S, Yang C, Xie S, Tong X. Pancreatic cancer therapy with PD-1 blockade and anti-tumor immunity of a novel oncolytic vaccinia virus expressing immunoregulatory protein LZ-8 in murine model. Eur J Immunol. 2019;49:1784. [Google Scholar]
- 142.Marelli G, Chard Dunmall LS, Yuan M, Di Gioia C, Miao J, Cheng Z, et al. A systemically deliverable vaccinia virus with increased capacity for intertumoral and intratumoral spread effectively treats pancreatic cancer. J Immunother Cancer. 2021;9(1). [DOI] [PMC free article] [PubMed]
- 143.Woo Y, Zhang Z, Yang A, Chaurasiya S, Park AK, Lu J, et al. Novel chimeric Immuno-oncolytic virus CF33-hNIS-antiPDL1 for the treatment of pancreatic Cancer. J Am Coll Surg. 2020;230(4):709–717. doi: 10.1016/j.jamcollsurg.2019.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Mahalingam D, Wilkinson GA, Eng KH, Fields P, Raber P, Moseley JL, et al. Pembrolizumab in combination with the oncolytic virus Pelareorep and chemotherapy in patients with advanced pancreatic adenocarcinoma: a phase Ib study. Clin Cancer Res. 2020;26(1):71–81. doi: 10.1158/1078-0432.CCR-19-2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Bear AS, Vonderheide RH, O'Hara MH. Challenges and opportunities for pancreatic Cancer immunotherapy. Cancer Cell. 2020;38(6):788–802. doi: 10.1016/j.ccell.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Peyraud F, Italiano A. Combined PARP inhibition and immune checkpoint therapy in solid tumors. Cancers (Basel). 2020;12(6). [DOI] [PMC free article] [PubMed]
- 147.Day CP, Merlino G, Van Dyke T. Preclinical mouse cancer models: a maze of opportunities and challenges. Cell. 2015;163(1):39–53. doi: 10.1016/j.cell.2015.08.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Tawbi HA, Forsyth PA, Algazi A, Hamid O, Hodi FS, Moschos SJ, et al. Combined Nivolumab and Ipilimumab in melanoma metastatic to the brain. N Engl J Med. 2018;379(8):722–730. doi: 10.1056/NEJMoa1805453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Scherpereel A, Mazieres J, Greillier L, Lantuejoul S, Do P, Bylicki O, et al. Nivolumab or nivolumab plus ipilimumab in patients with relapsed malignant pleural mesothelioma (IFCT-1501 MAPS2): a multicentre, open-label, randomised, non-comparative, phase 2 trial. Lancet Oncol. 2019;20(2):239–253. doi: 10.1016/S1470-2045(18)30765-4. [DOI] [PubMed] [Google Scholar]
- 150.Postow MA, Sidlow R, Hellmann MD. Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med. 2018;378(2):158–168. doi: 10.1056/NEJMra1703481. [DOI] [PubMed] [Google Scholar]
- 151.Pushpakom S, Iorio F, Eyers PA, Escott KJ, Hopper S, Wells A, et al. Drug repurposing: progress, challenges and recommendations. Nat Rev Drug Discov. 2019;18(1):41–58. doi: 10.1038/nrd.2018.168. [DOI] [PubMed] [Google Scholar]
- 152.Li CW, Lim SO, Xia W, Lee HH, Chan LC, Kuo CW, et al. Glycosylation and stabilization of programmed death ligand-1 suppresses T-cell activity. Nat Commun. 2016;7:12632. doi: 10.1038/ncomms12632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Chan LC, Li CW, Xia W, Hsu JM, Lee HH, Cha JH, et al. IL-6/JAK1 pathway drives PD-L1 Y112 phosphorylation to promote cancer immune evasion. J Clin Invest. 2019;129(8):3324–3338. doi: 10.1172/JCI126022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Cha JH, Chan LC, Li CW, Hsu JL, Hung MC. Mechanisms controlling PD-L1 expression in Cancer. Mol Cell. 2019;76(3):359–370. doi: 10.1016/j.molcel.2019.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Hsu JM, Xia W, Hsu YH, Chan LC, Yu WH, Cha JH, et al. STT3-dependent PD-L1 accumulation on cancer stem cells promotes immune evasion. Nat Commun. 2018;9(1):1908. doi: 10.1038/s41467-018-04313-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Li CW, Lim SO, Chung EM, Kim YS, Park AH, Yao J, et al. Eradication of triple-negative breast Cancer cells by targeting glycosylated PD-L1. Cancer Cell. 2018;33(2):187–201 e10. doi: 10.1016/j.ccell.2018.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Maher CM, Thomas JD, Haas DA, Longen CG, Oyer HM, Tong JY, et al. Small-molecule Sigma1 modulator induces Autophagic degradation of PD-L1. Mol Cancer Res. 2018;16(2):243–255. doi: 10.1158/1541-7786.MCR-17-0166. [DOI] [PubMed] [Google Scholar]
- 158.D'Arrigo P, Russo M, Rea A, Tufano M, Guadagno E, Del Basso De Caro ML, et al. A regulatory role for the co-chaperone FKBP51s in PD-L1 expression in glioma. Oncotarget. 2017;8(40):68291–68304. doi: 10.18632/oncotarget.19309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Hsu JM, Li CW, Lai YJ, Hung MC. Posttranslational modifications of PD-L1 and their applications in Cancer therapy. Cancer Res. 2018;78(22):6349–6353. doi: 10.1158/0008-5472.CAN-18-1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Horita H, Law A, Hong S, Middleton K. Identifying regulatory posttranslational modifications of PD-L1: a focus on Monoubiquitinaton. Neoplasia. 2017;19(4):346–353. doi: 10.1016/j.neo.2017.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Cha JH, Yang WH, Xia W, Wei Y, Chan LC, Lim SO, et al. Metformin promotes antitumor immunity via endoplasmic-reticulum-associated degradation of PD-L1. Mol Cell. 2018;71(4):606–20 e7. doi: 10.1016/j.molcel.2018.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zhang J, Bu X, Wang H, Zhu Y, Geng Y, Nihira NT, et al. Cyclin D-CDK4 kinase destabilizes PD-L1 via cullin 3-SPOP to control cancer immune surveillance. Nature. 2018;553(7686):91–95. doi: 10.1038/nature25015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Mezzadra R, Sun C, Jae LT, Gomez-Eerland R, de Vries E, Wu W, et al. Identification of CMTM6 and CMTM4 as PD-L1 protein regulators. Nature. 2017;549(7670):106–110. doi: 10.1038/nature23669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Burr ML, Sparbier CE, Chan YC, Williamson JC, Woods K, Beavis PA, et al. CMTM6 maintains the expression of PD-L1 and regulates anti-tumour immunity. Nature. 2017;549(7670):101–105. doi: 10.1038/nature23643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Lim SO, Li CW, Xia W, Cha JH, Chan LC, Wu Y, et al. Deubiquitination and stabilization of PD-L1 by CSN5. Cancer Cell. 2016;30(6):925–939. doi: 10.1016/j.ccell.2016.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Huang X, Zhang Q, Lou Y, Wang J, Zhao X, Wang L, et al. USP22 Deubiquitinates CD274 to suppress anticancer immunity. Cancer Immunol Res. 2019;7(10):1580–1590. doi: 10.1158/2326-6066.CIR-18-0910. [DOI] [PubMed] [Google Scholar]
- 167.Yang Y, Hsu JM, Sun L, Chan LC, Li CW, Hsu JL, et al. Palmitoylation stabilizes PD-L1 to promote breast tumor growth. Cell Res. 2019;29(1):83–86. doi: 10.1038/s41422-018-0124-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Yao H, Lan J, Li C, Shi H, Brosseau JP, Wang H, et al. Inhibiting PD-L1 palmitoylation enhances T-cell immune responses against tumours. Nat Biomed Eng. 2019;3(4):306–317. doi: 10.1038/s41551-019-0375-6. [DOI] [PubMed] [Google Scholar]
- 169.Whiteside TL, Demaria S, Rodriguez-Ruiz ME, Zarour HM, Melero I. Emerging opportunities and challenges in Cancer immunotherapy. Clin Cancer Res. 2016;22(8):1845–1855. doi: 10.1158/1078-0432.CCR-16-0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Tsimberidou AM, Fountzilas E, Nikanjam M, Kurzrock R. Review of precision cancer medicine: evolution of the treatment paradigm. Cancer Treat Rev. 2020;86:102019. doi: 10.1016/j.ctrv.2020.102019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Malone ER, Oliva M, Sabatini PJB, Stockley TL, Siu LL. Molecular profiling for precision cancer therapies. Genome Med. 2020;12(1):8. doi: 10.1186/s13073-019-0703-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Herbst B, Zheng L. Precision medicine in pancreatic cancer: treating every patient as an exception. Lancet Gastroenterol Hepatol. 2019;4(10):805–10. doi: 10.1016/S2468-1253(19)30175-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.