Abstract
Background and Objectives
Prior work examining the role of older adult home care service use in alleviating strain in family caregivers has resulted in contradictory findings. However, prior research has been entirely limited to caregivers who live within close geographical proximity to their care recipients. Long-distance caregivers are a unique caregiving subgroup that has remained understudied. Guided by the stress process model, this study examined if the association between primary caregiving stressors (the care recipient’s functional and cognitive status) and secondary stressors (perceived role strains related to work and to other family responsibilities) in long-distance caregivers was mediated by the care recipient’s utilization of home care services.
Research Design and Methods
The sample included 166 long-distance caregivers in the United States who provide and manage care to a community-dwelling care recipient living 2 or more hours away. Participants reported on their care recipient’s cognitive and functional status, perceived interference of caregiving with work and other family responsibilities, and the care recipient’s use of home care services.
Results
Path analyses show that home care use by the care recipient fully mediated the association between care recipients’ functional impairment and caregiver strains (work and family). Furthermore, home care use partially mediated the effects of care recipients’ cognitive impairment on caregiver strains.
Discussion and Implications
Results indicate that the care recipient’s home care service utilization may serve as a protective factor against care-related strain in long-distance caregivers. These findings can be used to inform intervention efforts focused on a family-centered care approach that can be specifically tailored to long-distance caregivers.
Keywords: Caregiving, Distance caregivers, Formal care, Geographically distant caregivers, Long-term services and supports
Empirical research on family caregiving has resulted in a well-documented knowledge base regarding potential consequences for caregivers, including adverse physical and mental health, which can result from care-related stress. Given that approximately 83% of support given to older adults is provided by unpaid caregivers (Garvey et al., 2019), substantial research has examined the caregiving experience to understand how caregivers can be better supported to effectively provide care and to circumvent or delay placement of the care recipient in a long-term care facility. Findings in this arena have been used to inform intervention efforts to promote psychosocial well-being among family members who care for a care recipient with chronic illness and/or disability. However, research has also demonstrated significant heterogeneity in the family caregiving experience and trajectory, as well as differential outcomes resulting from care-related stress (Schulz et al., 2020). This variability can limit the effectiveness of interventions designed to alleviate caregiver burden, as “one size does not fit all.” Furthermore, most research has involved geographically proximate caregivers. Individuals who provide and facilitate care from a distance are a unique subgroup of caregivers that have remained understudied and are virtually absent from inclusion in intervention efforts aiming to mitigate caregiver strain.
The Long-Distance Caregiving Experience
Although little is known about the long-distance caregiving experience, accelerating societal mobilization, workplace globalization, and increased population migration are among a number of factors that have contributed to the increase in long-distance caregivers providing care to an older adult with chronic illness (Bei et al., 2020; Horowitz & Boerner, 2017). Roughly 11%–15% of family caregivers provide care from a distance (Douglas et al., 2016), with one fourth of these individuals serving as the primary or only caregiver for a care recipient (National Alliance for Caregiving (2009)). The limited research in this area indicates that the types of assistance provided by long-distance caregivers are relatively similar to the care activities carried out by geographically proximate caregivers (Roff et al., 2007; Vezina & Turcotte, 2010). To support their care recipient’s needs, long-distance caregivers engage in a wide variety of care-related activities, including the provision of financial assistance, care management, and emotional support (Cagle & Munn, 2012; Douglas et al., 2016; Parker et al., 2006; Vezina & Turcotte, 2010). In fact, approximately three fourths of long-distance caregivers assist with instrumental activities of daily living (ADLs), including arranging transportation and medication management (Bei et al., 2020; Koerin & Harrigan, 2015). Although these caregivers are geographically removed from the care environment, providing care from a distance has been associated with feelings of anxiety, stress, helplessness, guilt, and uncertainty (Douglas et al., 2016; Mazanec, 2012). Furthermore, distance adds an extra layer of complexity to the caregiving role, which could intensify care-related stress and burden. Not surprisingly, research has shown that long-distance caregivers report equal or greater levels of emotional distress compared to proximate caregivers (Thompsell & Lovesone, 2002). However, most interventions targeting the reduction of caregiver burden have focused solely on geographically close caregivers. Alternatively, long-distance caregivers have little to no resources available, with the exception of Internet websites and popular press articles, to support them as they navigate the care role from afar (Douglas et al., 2016).
The geographical barriers faced by long-distance caregivers not only prevent the provision of consistent hands-on care, but also makes monitoring their care recipient’s health, as well as communicating with and receiving information from long-term services and support (LTSS) providers, difficult. Our previous work found that long-distance caregivers tend to be dissatisfied with the quality and frequency of communication with formal care providers, particularly in long-term care (Falzarano et al., 2020). In addition to issues surrounding communication, like many proximate caregivers, long-distance caregivers are likely to experience conflicts stemming from the need to fulfill caregiving obligations while fulfilling work responsibilities and responsibilities to other family members. These so-called interrole conflicts emerge when there are conflicting pressures and expectations stemming from work and family roles (Greenhaus & Beutell, 1985). Interrole conflicts can be bidirectional in nature (e.g., work responsibilities interfere with family obligations and vice versa) and can exacerbate feelings of caregiver strain and burden. Long-distance caregivers may be more likely to experience work-to-family conflicts and family-to-work conflicts because they are more likely to be employed full time when compared to geographically proximate caregivers (National Alliance for Caregiving (2009)). Furthermore, interrole conflicts may be a common experience for long-distance caregivers because close to 50% of employed distance caregivers report having to rearrange work schedules to accommodate caregiving activities and travel, and one third report consistently missing days of work in order to fulfill their caregiving obligations (Douglas et al., 2016).
Home Care Service Use and Caregiving Strain
To manage competing responsibilities and to keep the care recipient living at home for as long as possible, many caregivers need to defer to formal LTSS services to help provide care and assistance to care recipients. Among the many LTSS options available, home care services are the most widely used and preferred formal service options designed to provide assistance to frail older adults (e.g., personal care) and to support caregivers in managing care tasks (Martinez-Martin et al., 2012; Mensie & Steffan, 2010; O’Connell et al. 2012). Home care is provided by paid caregivers (i.e., home health aides, personal care attendants, or other direct care workers) who assist individuals with functional and cognitive impairments at home with daily tasks such as cooking, bathing, and medication management (Reckrey, 2020; Spetz et al., 2019). Home care can be provided full time, part time, or over certain periods of time based on the care recipient’s long-term care needs.
Empirical work examining the influence of home care utilization on caregiver outcomes, such as burden and strain, has produced somewhat contradictory findings (Garcés et al., 2010; Schoenmakers et al., 2010; Vandepitte et al., 2016; Zarit et al., 2017). Studies using quasi-experimental designs found that caregiver burden and distress was significantly reduced in individuals whose care recipient received formal home care (Kim & Kim, 2016; Reckrey, 2020). Additionally, other work has shown that caregivers were generally satisfied with home care and self-reported benefits including lower perceived burden, stress, and greater relief from the care role (Lethin et al., 2017; O’Connell et al., 2012; Vandepitte et al., 2019). This suggests that paid, formal care may positively affect the caregiver. However, systematic reviews have demonstrated small effects for home care use in reducing the burden and poor mental health (Kumamoto et al., 2006; Mason et al., 2007), while other research found no association between home care utilization and burden (Hawranik & Strain, 2000; Kim & Yeom, 2016; Maayan et al., 2014). Some studies even found that home care can exacerbate feelings of burden and stress in caregivers (Connors et al., 2019; Schoenmakers et al., 2010; Ward-Griffin et al., 2012). In addition to methodological challenges around measuring qualitatively different forms of home care services (e.g., respite care; Maayan et al., 2014), the mixed evidence on the influence of home care service use in reducing caregiver strain could most prominently be attributed to a lack of attention to different caregiving subgroups. Research into specific subgroups of caregivers, such as long-distance caregivers, may help to better elucidate the utility of home care service use in reducing caregiver strain.
The Current Study
Given the increasing population of individuals providing care from a distance and the likelihood that long-distance caregivers experience interrole conflicts, the investigation of home care utilization by care recipients of long-distance caregivers can make a unique contribution to the literature on the impact of formal service use in caregivers. Hence, the purpose of the current study was to examine if the care recipients’ use of home care services can reduce care-related role strain in long-distance caregivers. Research on geographically proximate caregivers has utilized the stress process model (Pearlin et al., 1990) as a theoretical framework to explain the differential ways by which care-related stress and stress appraisals can influence caregiver outcomes. In addition to background and contextual characteristics, the stress process model is divided into four domains: (a) primary stressors (e.g., stressors derived directly from the care environment, such as the care recipient’s functional and cognitive status), (b) secondary stressors (e.g., stressors that arise outside of the direct care role, including work and family interrole conflicts/role strains), (c) mediators (e.g., support), and (d) outcomes (e.g., emotional well-being). According to Pearlin et al. (1990), secondary stressors, such as role strains related to employment or other family responsibilities, develop based on primary stressors, and both types of stressors become interrelated. Research on geographically proximate caregivers demonstrated that both primary and secondary stressors can contribute to poorer outcomes (Bastawrous, 2013; Boumans & Durant, 2020). Furthermore, mediating factors, including the use of support (both formal and informal) and coping strategies, can influence the appraisal of primary stressors and subsequently alleviate some of the impacts of caregiving stressors. Thus, guided by the stress process model as a theoretical framework, the current study examines the relationship between primary and secondary stressors, and how use of home care may mediate this relationship. We first hypothesize that the cognitive and functional status (primary stressors) of the care recipient will be directly related to greater role strains experienced by long-distance caregivers with respect to work and other family responsibilities (secondary stressors). Additionally, we hypothesize that the association between primary stressors and secondary stressors will be mediated by the care recipients’ home care service utilization (formal support), such that home care service use will be associated with reduced role strains.
Method
Participants
The sample included in the current analysis represents a subsample of 166 individuals who participated in a larger national cross-sectional study (N = 304) that examined the experiences, challenges, and consequences of long-distance caregiving across the United States (PI: A. Horowitz: R21-AG050018). Approximately 45% of participants were recruited from aging service organizations, 41% from researchmatch.org (a national database of prospective research participants), and 14% were recruited from professional networks, participant referrals, and through an existing pool of participants enrolled in an ongoing aging study. Study participants comprised both English- and Spanish-speaking caregivers. A telephone screening was conducted prior to the interview to determine participant eligibility criteria, which required participants to (a) be a primary or coprimary caregiver responsible for the care of an older adult; (b) provide care for an individual who is functionally impaired and exhibits difficulty with two or more tasks of ADLs or is unable to do at least one without assistance; and (c) live at least 2 h or more in travel time away from the care recipient. The frequency and/or type of care provided was not an eligibility criterion in order to represent the full range of long-distance caregiving experiences. Those who met eligibility criteria provided consent and participated in a telephone interview lasting approximately 1 h.
The full sample (N = 304) included long-distance caregivers with care recipients residing in both residential care and the community; the subsample of participants included in the current analysis were 166 long-distance caregivers who provide and/or manage care to a community-dwelling older adult. The study was approved by the Institutional Review Boards of the respective institutions where the study was conducted.
Measures
Care recipient cognitive status
Cognitive impairment was assessed via a six-item measure (Galvin et al., 2005) asking participants to report on the severity of their care recipient’s cognitive status. Sample items include “Does [your care-recipient] have problems with judgement (e.g., problems making decisions, bad financial decisions, problems with thinking)?” and “Does [your care-recipient] repeat the same things over and over (e.g., questions, stories, or statements)?” Response options included “Yes, a major problem,” “Yes, somewhat of a problem,” and “No, not a problem.” Items were summed, with higher scores indicating greater cognitive impairment.
Care recipient functional status
Functional impairment was assessed via a 14-item scale asking participants to report on the care recipient’s level of difficulty with seven ADLs and seven instrumental ADLs using a 4-point Likert scale (Older Americans Resources and Services: Center for the Study of Aging and Human Development, 1975; Horowitz et al., 2005). Sample items include “Does [your care-recipient] have any difficulty with bathing him/herself, that is taking a bath, shower, or sponge bath?” and “Does [your care-recipient] have any difficulty preparing his/her own meals including cutting, mixing, and cooking food?” Response options ranged from “No difficulty” to “Can’t do without help,” with higher scores indicating greater functional impairment.
Perceived interference of caregiving with work and family
Participants were administered two items asking to rate how much caregiving interferes with (a) work activities and (b) responsibilities to other family members. Response options for each item ranged from 0 (No interference at all) to 10 (Extreme interference).
Home care utilization
Participants who indicated that their care recipient receives home care services were administered one open-ended item asking participants to indicate the number of hours per week home care services are provided to the care recipient. Participants with care recipients who did not receive home care services were coded as “0” hours.
Data Analyses
Descriptive statistics (means, standard deviations, and percentages) were computed for all demographic and study variables to ensure normality in the distribution of the data. Independent samples t-tests and chi-square tests were then conducted to examine differences in participants who have care recipients with and without home care on key study variables. Then, two path models were run to examine the mediating role of hours of home care services provided per week in the association between care recipient functioning, as measured by functional difficulty and cognitive impairment, on participants’ perceived interference with work and family responsibilities. Assessment of direct and indirect effects followed guidelines by Preacher and Hayes (2004) and Zhao et al. (2010). Bootstrapping, a nonparametric resampling technique with a replacement that can mitigate issues surrounding low power and non-normality, was used to derive 95% bias-corrected confidence intervals (CIs) with 5,000 bootstrapped resamples (Preacher & Hayes, 2008). Bootstrapping methods require no missing data, thus multiple imputation based on regression was used to address cases of missing data. Several fit indices were evaluated to assess model fit, including the chi-square statistic, chi-square ration (χ 2/df), the comparative fit index (CFI), and the root-mean-square error of approximation (RMSEA).
Results
Sample Characteristics
Descriptive statistics are presented in Table 1. Participants were between the ages of 25 and 86 years (Mage = 53.85, SD = 12.98). The majority of participants were female and reported to be adult-child caregivers. Nearly one third of participants were of racial/ethnic minority background. Of the participants included in the current analyses, 81 of the 166 participants reported that their care recipient received home care services. The average use of home care across the total sample was 30 h/week. Chi-square and independent samples t-tests were conducted to examine differences between long-distance caregivers of care recipients with and without home care on key study variables. Chi-square analyses on categorical variables including race, education, and relationship to care recipient revealed no significant differences between caregivers of those with and without home care, with one exception. Participants with care recipients who received home care were significantly more likely to have a dementia diagnosis: χ 2 (1, N = 166) = 6.26, p = .012. Independent samples t-tests revealed that participants with care recipients who received home care were significantly older (t (160) = −4.97, p < .001), had care recipients with worse cognitive (t (160) = −2.21, p = .002) and functional (t (160) = −8.65, p < .001) status. Furthermore, caregivers of those with home care reported significantly lower perceived interference with work (t (160) = 2.05, p = .016) and family responsibilities (t (160) = 2.57), p = .043).
Table 1.
Sample Characteristics (N = 166)
| Total sample | Home care use (n = 81) | No home care use (n = 85) | t-test | χ 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | % | M | SD | % | M | SD | % | M | SD | ||
| Age | 53.85 | 12.98 | 58.35 | 12.16 | 49.52 | 12.31 | −4.97*** | ||||
| Gender (female) | 75.3 | 72.8 | 77.6 | 0.83 | |||||||
| Race/ethnicity | 4.11 | ||||||||||
| White | 72.1 | 78.8 | 65.9 | ||||||||
| Black/African American | 10.9 | 7.4 | 14.1 | ||||||||
| Hispanic | 9.7 | 8.6 | 10.6 | ||||||||
| Asian/Pacific Islander | 0.6 | 2.5 | 4.7 | ||||||||
| Other | 3.0 | 2.5 | 4.7 | ||||||||
| Education | 2.75 | ||||||||||
| GED/high school graduate | 0 | 0 | 0 | ||||||||
| Some college | 19.3 | 21.0 | 17.6 | ||||||||
| College graduate | 28.9 | 22.2 | 35.3 | ||||||||
| Graduate school or greater | 51.8 | 56.8 | 47.1 | ||||||||
| Relationship to care recipient | 22.30 | ||||||||||
| Spouse | 0 | ||||||||||
| Child | 75.3 | ||||||||||
| Sibling | 6.6 | ||||||||||
| Other | 18.1 | ||||||||||
| Caregiver employed (yes) | 68.7 | 66.7 | 70.6 | 0.77 | |||||||
| Care recipient dementia diagnosis (yes) | 28.7 | 37.5 | 20.2 | 6.26* | |||||||
| Distance from care recipient (miles) | 861.34 | 1,145.73 | 836.24 | 917.64 | 885.25 | 1,332.44 | 0.77 | ||||
| Travel time to care recipient (hours) | 6.24 | 6.63 | 6.65 | 8.17 | 5.90 | 4.78 | 0.48 | ||||
| Care recipient functional status | 30.52 | 11.57 | 37.22 | 10.60 | 24.31 | 8.62 | −8.65*** | ||||
| Care recipient cognitive status | 5.70 | 3.59 | 6.60 | 3.52 | 4.87 | 3.47 | −2.21** | ||||
| Perceived work interference | 7.97 | 2.40 | 6.58 | 2.51 | 6.78 | 2.19 | 2.05* | ||||
| Perceived family interference | 8.05 | 2.36 | 7.05 | 2.51 | 7.52 | 2.30 | 2.57* | ||||
| Home care hours per week | 63.98 | 65.16 | 0 | 0 | — | ||||||
Note: GED = General Educational Development.
*p < .05, **p < .01, ***p < .001.
Path Analysis 1: Perceived Interference With Family Responsibilities
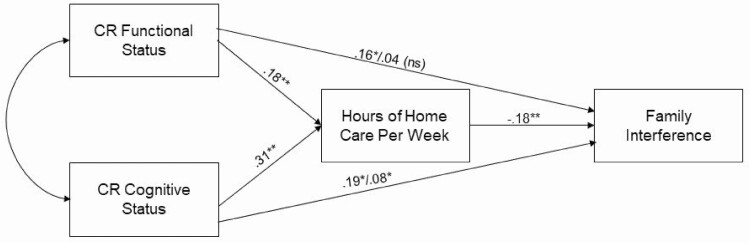
The first path model examined the association between care recipient functioning (cognitive status and functional status) and participants’ perceived interference with responsibilities to other family members (Figure 1) and demonstrated adequate model fit: (χ 2 (2) = 4.41; CFI = 0.982, RMSEA = 0.084). Inspection of direct effects indicated that both care recipient functional status (B = 0.16, p = .04) and cognitive status (B = 0.19, p = .02) were significantly associated with greater interference with participants’ family responsibilities.
Figure 1.
Path model examining care recipient functioning and perceived interference with family responsibilities as mediated by hours of home care provided to the care recipient per week. Note: CR = care recipient. Values before the “/” represent the total effects between CR functioning and family interference. Values after the “/” represent the direct effects after the addition of the mediators. *p < .05, **p < .001.
When assessing hours of home care services provided per week as a mediator, the association between care recipient functional status and family interference became nonsignificant (B = 0.04, p = .59), providing evidence that home care hours fully mediated this relationship. Inspection of indirect effects using 95% bootstrap bias (e.g., corrected for bias in the bootstrap distribution) corrected CIs confirmed evidence of mediation. The relationship between care recipient functional status and participants’ perceived interference with family responsibilities significantly operated through home care hours (indirect effect = −0.006, 95% CI [−0.015, −0.001], p = .005), indicating that greater functional impairment and more hours of home care per week predicted lower perceived interference. Inclusion of home care hours in the model as a mediator reduced the magnitude of the relationship between care recipient cognitive status and family interference; however, this association remained statistically significant (B = 0.08, p = .04), providing evidence for partial mediation. Inspection of indirect effects using 95% bootstrap bias-corrected CIs shows that the indirect effect was not significant.
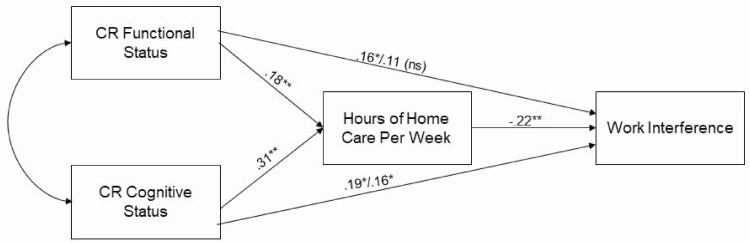
Path Analysis 2: Perceived Interference With Work Responsibilities
The second path model (Figure 2) examined the association between care recipient functioning (cognitive status and functional impairment) and long-distance caregivers’ perceived interference with work-related responsibilities. The model demonstrated good fit: (χ 2 (2) = 3.50; CFI = 0.989, RMSEA = 0.067). We found that care recipient functional (B = 0.16, p = .03) and cognitive status (B = 0.19, p = .02) significantly predicted greater perceived interference with work responsibilities.
Figure 2.
Path model examining care recipient functioning and perceived interference with work responsibilities as mediated by hours of home care provided to the care recipient per week. Note: CR = care recipient. Values before the “/” represent the total effects between CR functioning and family interference. Values after the “/” represent the direct effects after the addition of the mediators. *p < .05, **p < .001.
When assessing hours of home care per week as a mediator, the direct relationship between care recipient functional status and work interference was no longer significant (B = 0.11, p = .10), indicating full mediation. Inspection of 95% bootstrap bias-corrected CIs showed that the indirect effect was significant (indirect effect = −0.007, 95% CI [−0.015 to −0.002], p = .005), suggesting that a greater number of home care hours provided per week accounted for the relationship between care recipient functional status and perceived work interference. While including home care hours as a mediator in the model reduced the magnitude of the direct association between care recipient cognitive status and work interference, this relationship remained statistically significant (B = 0.16, p = .04), providing evidence for partial mediation. Inspection of indirect effects using 95% bootstrap bias indicated that there was not a significant indirect effect.
Discussion
Research has only begun to examine the experiences of the growing population of long-distance caregivers providing and managing care for a care recipient living a significant distance away. To the best of our knowledge, our study is the first to provide insights into the relationship between primary and secondary stressors (role strains) in long-distance caregivers. Guided by the stress process model (Pearlin et al., 1990), we examined the influence of functional and cognitive impairment on caregivers’ perceived role strain due to work and other family responsibilities, and how this relationship may be mediated by the care recipients’ use of home care. Confirming our hypotheses, results indicate that more severe functional and cognitive impairments (primary stressors) were associated with greater perceived interference with both work and family responsibilities in long-distance caregivers (secondary stressors). Furthermore, we found that hours of home care use fully mediated the relationship between care recipient functional status and interference with both work and other family responsibilities. This suggests that long-distance caregivers whose care recipient used more hours of home care did not perceive their care recipient’s functional impairment to interfere with work and other family responsibilities. This is likely a result of home care aides providing assistance with ADLs and the caregiver not having to provide hands-on ADL assistance as frequently. We also identified evidence of partial mediation for home care in the relationship between the care recipient’s cognitive impairment and perceived interference with caregiving. This indicates that participants’ perceptions of how much their care recipient’s cognitive impairment negatively interfered with work and other family responsibilities were lessened because of the care recipient’s amount of home care. Full mediation of home care use in the relationship between cognitive status and interference with both work and other family responsibilities would likely not occur because of the more complex care needs of individuals with dementia. Although empirical work examining the associations between home care use and caregiving strain has been mixed (Garcés et al., 2010), our overall findings are consistent with the small pool of literature (Reckrey et al., 2020; Vandepitte et al., 2016) that has found evidence for the positive influence of home care service use in alleviating caregiver distress. Our specific contribution to this body of literature is evidence showing that home care service use by care recipients can alleviate family-to-work and work-to-family conflict in long-distance caregivers. Because a majority of long-distance caregivers are employed full time (National Alliance for Caregiving (2009)), connecting these individuals and their care partners to home care services could reduce the stress associated with role conflicts in this unique caregiving population.
Our findings regarding the benefit of home care use for long-distance caregivers could be attributed to the time point in the caregiving trajectory at which these caregivers seek out formal services. Geographically close caregivers usually resort to formal services, such as formal home care, when already at a crisis stage and when the burden is already too high to be mitigated by home care service use (Carretero et al., 2009). However, given the physical distance between the “care pair,” long-distance caregivers may draw on home care services in a preventative manner to ensure the care recipient is taken care of and may explain why the use of home care services in this study was shown to reduce perceived strain in long-distance caregivers.
It is important to note that providing care from a significant distance away poses barriers to the family caregiving role. Long-distance caregivers, who are often unable to be physically present at care plan meetings and appointments, may be left out of communications regarding their care recipient’s health status, which may create additional stressors while navigating the caregiving role when they are not receiving consistent communication from the care recipient’s health care team. As highlighted in prior work, the establishment of close, collaborative relationships with family members and formal caregivers are a fundamental aspect of the quality of and satisfaction with home care (Funk & Stajduhar, 2013). In direct contrast to the type and structure of care provided in acute and long-term care settings, the provision of home care requires a continuity of exchange between all members of the care team to ensure consistent and effective care (Sims-Gould & Martin-Matthews, 2010). It is possible that care provided in the home, which requires home care providers to be sensitive to the family’s space and needs and to the development of a mutual, trusting relationship among formal and family caregivers, may foster a more consistent stream of communication with long-distance caregivers regarding the care recipient’s health and condition and thus can contribute to alleviating feelings of strain and role conflict (Lindahl et al., 2011).
Study findings have implications for practice as they bolster support for a family-centered care approach that emphasizes the importance of integrating staff, care recipients, and caregivers as a care team. Caregivers, both distant and proximate, should be screened for sources of distress and personalized interventions should be designed to link unmet needs to relevant resources, such as home care, to alleviate caregiving-related stress. From a policy perspective, our results provide support for the increasing trend across U.S. states toward the development of “No Wrong Door” initiatives, which seeks to streamline access to LTSS formal service options and facilitate the integration of caregivers into the service system (Arc, 2017; Grossman et al., 2018). Awareness and knowledge of the unique experiences and challenges that long-distance caregivers face can inform the adaptation of such initiatives to ensure that they have equitable access to needed resources and beneficial formal supports that can alleviate the stress associated with caregiving from afar.
Limitations and Future Directions
The results of the current study should be considered within the context of its limitations. A majority of participants were recruited using convenience sampling, limiting the generalizability of our findings. Sample selectivity may have influenced the findings, such that individuals willing to participate in research may represent a specialized group of caregivers who actively seek out services and resources, and thus the sample may not be representative of all long-distance caregivers. Furthermore, the current study was limited by a lack of information on the care recipient (i.e., age, specific chronic diseases), and future work should examine the long-distance caregiving experience in relation to care recipient characteristics. In addition, we only assessed one indicator of home care use, which was the number of home care hours received per week. Future research, therefore, should focus on assessing whether various types of home care differentially affect long-distance caregiving outcomes. Another limitation relates to inconsistencies in defining and conceptualizing long-distance caregiving. The current study defined distance caregiving as living at least 2 h away from the care recipient; however, there is still a lack of consensus on an adequate definition for long-distance caregiving (Douglas et al., 2016). Research would also benefit from additional exploration into the nature of the relationship between long-distance caregivers and home care providers, affordability of and types of home care used, the assistance provided that is perceived as helpful, and investigate how the interplay of these factors contribute to reduced strain in this caregiving population.
Despite the noted limitations, our study provides novel insights into caregiving strain in a sample of long-distance caregivers, and how the provision of formal home care can be used as a strategy to help mitigate the impact of interrole conflicts. The implications of the current study underscore the need to raise awareness among caregivers and home care providers regarding the benefits of home care use, so that a larger number of long-distance caregivers have knowledge of and access to home care services as a means of formal support to mitigate the unique stress associated with caregiving from afar.
Funding
This work was supported by the National Institute on Aging (NIA; PI: A. Horowitz: R21-AG050018). F. Falzarano acknowledges support from an NIA-funded T32 Training Program grant (AG049666).
Conflict of Interest
None declared.
References
- Arc. (2017). 2015–2017 Family Support Research and Training (FSRTC) state coalition report. Author.
- Bastawrous, M. (2013). Caregiver burden—A critical discussion. International Journal of Nursing Studies, 50(3), 431–441. doi: 10.1016/j.ijnurstu.2012.10.005 [DOI] [PubMed] [Google Scholar]
- Bei, E., Rotem-Mindali, O., & Vilchinsky, N. (2020). Providing care from afar: A growing yet understudied phenomenon in the caregiving field. Frontiers in Psychology, 11, 681. doi: 10.3389/fpsyg.2020.00681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boumans, N. P., & Dorant, E. (2020). The relationships of job and family demands and job and family resources with family caregivers’ strain. Scandinavian Journal of Caring Sciences, 35(2), 567–576. doi: 10.1111/scs.12873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagle, J. G., & Munn, J. C. (2012). Long-distance caregiving: A systematic review of the literature. Journal of Gerontological Social Work, 55(8), 682–707. doi: 10.1080/01634372.2012.703763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carretero, S., Garcés, J., Ródenas, F., & Sanjosé, V. (2009). The informal caregiver’s burden of dependent people: Theory and empirical review. Archives of Gerontology and Geriatrics, 49(1), 74–79. doi: 10.1016/j.archger.2008.05.004 [DOI] [PubMed] [Google Scholar]
- Center for the Study of Aging and Human Development. (1975). Multidimensional functional assessment: The OARS methodology (1st ed.). Duke University Medical Center. [Google Scholar]
- Connors, M. H., Seeher, K., Teixeira‐Pinto, A., Woodward, M., Ames, D., & Brodaty, H. (2019). Dementia and caregiver burden: A three‐year longitudinal study. International Journal of Geriatric Psychiatry, 35(2), 250–258. doi: 10.1002/gps.5244 [DOI] [PubMed] [Google Scholar]
- Douglas, S. L., Mazanec, P., Lipson, A., & Leuchtag, M. (2016). Distance caregiving a family member with cancer: A review of the literature on distance caregiving and recommendations for future research. World Journal of Clinical Oncology, 7(2), 214–219. doi: 10.5306/wjco.v7.i2.214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falzarano, F., Cimarolli, V. R., Minahan, J., & Horowitz, A. (2020). Long-distance caregivers: What are their experiences with formal care providers? Clinical Gerontologist, 1–12. doi: 10.1080/07317115.2020.1783043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk, L., & Stajduhar, K. (2013). Analysis and proposed model of family caregivers’ relationships with home health providers and perceptions of the quality of formal services. Journal of Applied Gerontology, 32(2), 188–206. doi: 10.1177/0733464811408699 [DOI] [PubMed] [Google Scholar]
- Galvin, J. E., Roe, C. M., Powlishta, K. K., Coats, M. A., Muich, S. J., Grant, E., Miller, J. P., Storandt, M., & Morris, J. C. (2005). The AD8: A brief informant interview to detect dementia. Neurology, 65(4), 559–564. doi: 10.1212/01.wnl.0000172958.95282.2a [DOI] [PubMed] [Google Scholar]
- Garcés, J., Carretero, S., Ródenas, F., & Alemán, C. (2010). A review of programs to alleviate the burden of informal caregivers of dependent persons. Archives of Gerontology and Geriatrics, 50(3), 254–259. doi: 10.1016/j.archger.2009.04.012 [DOI] [PubMed] [Google Scholar]
- Garvey, J. M., Dalton, J. M., & Magny-Normilus, C. (2019). A conceptual–theoretical–empirical structure for the study of Alzheimer informal caregivers and home health care nursing services. Home Health Care Management & Practice, 31(4), 231–238. doi: 10.1177/1084822319844263 [DOI] [Google Scholar]
- Greenhaus, J. H., & Beutell, N. J. (1985). Sources of conflict between work and family roles. Academy of Management Review, 10(1), 76–88. doi: 10.5465/amr.1985.4277352 [DOI] [Google Scholar]
- Grossman, B. R., Magaña, S., Abdelrahim, R., & Vanegas, S. (2018). Research on family caregiving support in the United States: A strategic plan. Family Support Research and Training Center, Institute of Disability and Human Development, University of Illinois at Chicago. [Google Scholar]
- Hawranik, P., & Strain, L. A. (2000). Health of informal caregivers: Effects of gender, employment, and use of home care services. University of Manitoba, Centre on Aging. [Google Scholar]
- Horowitz, A., & Boerner, K. (2017). Long-distance caregiving: Unique challenges and service needs. In Wilmoth J. & Silverstein M. (Eds.), Later-life social support and service provision in diverse and vulnerable populations: Understanding networks of care (pp. 136–154). Routledge. [Google Scholar]
- Horowitz, A., Reinhardt, J. P., & Boerner, K. (2005). The effect of rehabilitation on depression among visually disabled older adults. Aging & Mental Health, 9(6), 563–570. doi: 10.1080/13607860500193500 [DOI] [PubMed] [Google Scholar]
- Kim, J., & Kim, H. (2016). Effects of home care services use by older adults on family caregiver distress. Journal of Korean Academy of Nursing, 46(6), 836–847. doi: 10.4040/jkan.2016.46.6.836 [DOI] [PubMed] [Google Scholar]
- Kim, E. Y., & Yeom, H. E. (2016). Influence of home care services on caregivers’ burden and satisfaction. Journal of Clinical Nursing, 25(11–12), 1683–1692. doi: 10.1111/jocn.13188 [DOI] [PubMed] [Google Scholar]
- Koerin, B. B., and Harrigan, M. M. P. (2015). PS I love you: Long-distance caregiving. In Howe J.(Ed.), Older people and their caregivers across the spectrum of care (pp. 77–96). Routledge. [Google Scholar]
- Kumamoto, K., Arai, Y., & Zarit, S. H. (2006). Use of home care services effectively reduces feelings of burden among family caregivers of disabled elderly in Japan: Preliminary results. International Journal of Geriatric Psychiatry, 21(2), 163–170. doi: 10.1002/gps.1445 [DOI] [PubMed] [Google Scholar]
- Lethin, C., Renom-Guiteras, A., Zwakhalen, S., Soto-Martin, M., Saks, K., Zabalegui, A., & Challis, D. J. (2017). Psychological well-being over time among informal caregivers caring for persons with dementia living at home. Aging & Mental Health, 21(11), 1138–1146. doi: 10.1080/13607863.2016.1211621 [DOI] [PubMed] [Google Scholar]
- Lindahl, B., Lidén, E., & Lindblad, B. M. (2011). A meta-synthesis describing the relationships between patients, informal caregivers and health professionals in home-care settings. Journal of Clinical Nursing, 20(3–4), 454–463. doi: 10.1111/j.1365-2702.2009.03008.x [DOI] [PubMed] [Google Scholar]
- Maayan, N., Soares‐Weiser, K., & Lee, H. (2014). Respite care for people with dementia and their carers. Cochrane Database of Systematic Reviews, (1), CD004396. doi: 10.1002/14651858.CD004396.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Martin, P., Rodriguez-Blazquez, C., & Forjaz, M. J. (2012). Quality of life and burden in caregivers for patients with Parkinson’s disease: Concepts, assessment and related factors. Expert Review of Pharmacoeconomics & Outcomes Research, 12(2), 221–230. doi: 10.1586/erp.11.106 [DOI] [PubMed] [Google Scholar]
- Mason, A., Weatherly, H., Spilsbury, K., Arksey, H., Golder, S., Adamson, J., Drummond, M., & Glendinning, C. (2007). A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers. Health Technology Assessment, 11(15), 1–157. doi: 10.3310/hta11150 [DOI] [PubMed] [Google Scholar]
- Mazanec, P. (2012). Distance caregiving a parent with cancer. Seminars in Oncology Nursing, 28(4), 271–278. doi: 10.1016/j.soncn.2012.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mensie, L. C., & Steffen, A. M. (2010). Depressive symptoms and use of home-based respite time in family caregivers. Home Health Care Services Quarterly, 29(3), 120–137. doi: 10.1080/01621424.2010.511514 [DOI] [PubMed] [Google Scholar]
- National Alliance for Caregiving . (2009). Caregiving in the U.S. 2009. Washington, DC: AARP Research. doi: 10.26419/ppi.00103.001 [DOI]
- O’Connell, B., Hawkins, M., Ostaszkiewicz, J., & Millar, L. (2012). Carers’ perspectives of respite care in Australia: An evaluative study. Contemporary Nurse, 41(1), 111–119. doi: 10.5172/conu.2012.41.1.111 [DOI] [PubMed] [Google Scholar]
- Parker, M. W., Church, W., & Toseland, R. W. (2006). Caregiving at a distance. In: Berkman B.(Ed.), Handbook on aging and social work (pp. 391–406). Haworth Press. [Google Scholar]
- Pearlin, L. I., Mullan, J. T., Semple, S. J., & Skaff, M. M. (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30(5), 583–594. doi: 10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Preacher, K. J., & Hayes, A. F. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36(4), 717–731. doi: 10.3758/BF03206553 [DOI] [PubMed] [Google Scholar]
- Preacher, K. J., & Hayes, A. F. (2008). Contemporary approaches to assessing mediation in communication research. In A. F. Hayes, M. D. Slater, & L. B. Snyder (Eds.), The Sage sourcebook of advanced data analysis methods for communication research (pp. 13–54). Sage. [Google Scholar]
- Reckrey, J. M. (2020). COVID-19 confirms it: Paid caregivers are essential members of the healthcare team. Journal of the American Geriatrics Society, 68(8), 1679–1680. doi: 10.1111/jgs.16566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reckrey, J., Bollens-Lund, E., Tsui, E., Boerner, K., & Ornstein, K. (2020). Dementia caregiving: The association between family caregiving strain and receipt of paid care. Innovation in Aging, 4(Suppl. 1), 572. doi: 10.1093/geroni/igaa057.1898 [DOI] [Google Scholar]
- Reckrey, J. M., Morrison, R. S., Boerner, K., Szanton, S. L., Bollens‐Lund, E., Leff, B., & Ornstein, K. A. (2020). Living in the community with dementia: Who receives paid care? Journal of the American Geriatrics Society, 68(1), 186–191. doi: 10.1111/jgs.16215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roff, L. L., Martin, S. S., Jennings, L. K., Parker, M. W., & Harmon, D. K. (2007). Long distance parental caregivers’ experiences with siblings: A qualitative study. Qualitative Social Work, 6(3), 315–334. doi: 10.1177/1473325007080404 [DOI] [Google Scholar]
- Schoenmakers, B., Buntinx, F., & DeLepeleire, J. (2010). Supporting the dementia family caregiver: The effect of home care intervention on general well-being. Aging and Mental Health, 14(1), 44–56. doi: 10.1080/13607860902845533 [DOI] [PubMed] [Google Scholar]
- Schulz, R., Beach, S. R., Czaja, S. J., Martire, L. M., & Monin, J. K. (2020). Family caregiving for older adults. Annual Review of Psychology, 71, 635–659. doi: 10.1146/annurev-psych-010419-050754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims‐Gould, J., & Martin‐Matthews, A. (2010). We share the care: Family caregivers’ experiences of their older relative receiving home support services. Health & Social Care in the Community, 18(4), 415–423. doi: 10.1111/j.1365-2524.2010.00913.x [DOI] [PubMed] [Google Scholar]
- Spetz, J., Stone, R. I., Chapman, S. A., & Bryant, N. (2019). Home and community-based workforce for patients with serious illness requires support to meet growing needs. Health Affairs, 38(6), 902–909. doi: 10.1377/hlthaff.2019.00021 [DOI] [PubMed] [Google Scholar]
- Thompsell, A., & Lovestone, S. (2002). Out of sight out of mind? Support and information given to distant and near relatives of those with dementia. International Journal of Geriatric Psychiatry, 17(9), 804–807. doi: 10.1002/gps.692 [DOI] [PubMed] [Google Scholar]
- Vandepitte, S., Van Den Noortgate, N., Putman, K., Verhaeghe, S., Verdonck, C., & Annemans, L. (2016). Effectiveness of respite care in supporting informal caregivers of persons with dementia: A systematic review. International Journal of Geriatric Psychiatry, 31(12), 1277–1288. doi: 10.1002/gps.4504 [DOI] [PubMed] [Google Scholar]
- Vandepitte, S., Putman, K., Van Den Noortgate, N., Verhaeghe, S., & Annemans, L. (2019). Effectiveness of an in-home respite care program to support informal dementia caregivers: A comparative study. International Journal of Geriatric Psychiatry, 34(10), 1534–1544. doi: 10.1002/gps.5164 [DOI] [PubMed] [Google Scholar]
- Vezina, M., & Turcotte, M. (2010). Caring for a parent who lives far away: The consequences. Statistics Canada. [Google Scholar]
- Ward-Griffin, C., Hall, J., DeForge, R., St-Amant, O., McWilliam, C., Oudshoorn, A., Forbes, D., & Klosek, M. (2012). Dementia home care resources: How are we managing?. Journal of Aging Research, 2012, 590724. doi: 10.1155/2012/590724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarit, S. H., Bangerter, L. R., Liu, Y., & Rovine, M. J. (2017). Exploring the benefits of respite services to family caregivers: Methodological issues and current findings. Aging & Mental Health, 21(3), 224–231. doi: 10.1080/13607863.2015.1128881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, X., LynchJr, J. G., & Chen, Q. (2010). Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research, 37(2), 197–206. doi: 10.1086/651257 [DOI] [Google Scholar]