Abstract
There is a growing emphasis to use a transdisciplinary team approach to accelerate innovations in science to solve complex conditions associated with aging. However, the optimal organizational structure and process for how to accomplish transdisciplinary team science is unclear. In this forum, we illustrate our team’s experience using transdisciplinary approaches to solve challenging and persistent problems for older adults living in urban communities. We describe our challenges and successes using the National Institutes of Health four-phase model of transdisciplinary team-based research. Using a de-identified survey, the team conducted an internal evaluation to identify features that created challenges including structural incongruities, interprofessional blind spots, group function, and group dynamics. This work resulted in the creation of the team’s Transdisciplinary Conceptual Model. This model became essential to understanding the complex interplay between societal factors, community partners, and academic partners. Conducting internal evaluations of transdisciplinary team processes is integral for teams to move beyond the multi- and interdisciplinary niche and to reach true transdisciplinary success. More research is needed to develop measures that assess team transdisciplinary integration. Once the process of transdisciplinary integration can be reliably assessed, the next step would be to determine the impact of transdisciplinary team science initiatives on aging communities.
Keywords: Community-engaged research, Knowledge translation, Team science
The complexity of aging research and the systems associated with aging such as social networks, physical environment, community, and public policy requires that we develop a new integrative research model. Arguably, one that includes expertise that incorporates the social–ecological model with transdisciplinary principles to support innovations needed to solve complex aging issues (Callaghan, 2017; Golden et al., 2015; Rosenfield, 1992). The term “transdisciplinary” was introduced in the 1970s by the Swiss psychologist Jean Piaget who coined the term to describe a “higher stage of succeeding interdisciplinary relationships which would not only cover interactions or reciprocities between specialized research projects but would place these relationships within a total system without any firm boundaries between disciplines” (Bernstein & Bernstein, 2015; Piaget, 1972, p. 138). Conceptually, transdisciplinary approaches are envisioned as a way to find solutions for large societal problems such as health, education, policy, and socially responsible science. The goal of transdisciplinary research is to extend knowledge and generate new processes that go beyond individual disciplines, thereby creating novel practical solutions to advancing science (Bernstein & Bernstein, 2015; Thompson Klein, 2004).
The problems that intersect healthy aging and society are complex, and our ability to harness the power of Jean Piaget’s vision of transdisciplinary science is fundamental to our success to enact change. Given the growing emphasis on transdisciplinary team science in research, we need to understand how teams are accomplishing this process from theory to practice. This includes understanding (a) how do teams become transdisciplinary, (b) what are the features of transdisciplinary teams that create challenges, and (c) how can we measure the impact of transdisciplinary research in aging communities? To answer these questions, we must self-reflect and share lessons learned from teams attempting to achieve transdisciplinary team science.
Transdisciplinary teams go beyond multi- and interdisciplinary approaches. As such, they hold the greatest potential for systematically addressing complex health disparities occurring during older adulthood. However, attempting to transcend the multi- and interdisciplinary niche and reach true transdisciplinary status is not without its challenges (Black et al., 2019). Barriers noted in the literature include systems-based (i.e., organizational politics, disconnect between university and community), team-based (i.e., goal misalignment with team members, lack of deep knowledge integration, conflict resolution), and university-based policies (i.e., rewarding individual scientific accomplishments vs team-based research achievements) (Black et al., 2019; Harvey et al., 2015; Mazumdar et al., 2015; Thompson Klein, 2004). Moreover, the term transdisciplinary is frequently misapplied and misunderstood or used interchangeably with the word interdisciplinary (Archibald et al., 2018; Hall, Stokols, et al., 2012). To advance the understanding of transdisciplinary research, effective transdisciplinary teams must clearly articulate the process taken to achieve a shared understanding of knowledge translation between team members (Archibald et al., 2018). Our goal is to describe the development, conceptualization, and implementation of our transdisciplinary team and share what has and has not worked well.
Program Development Background
In 2012, the Richmond Health and Wellness Program (RHWP) was founded. RHWP is an interprofessional care coordination program that serves health disparate older adults (https://nursing.vcu.edu/community-engagement/rhwp/) living in low-income senior housing (Parsons et al., 2019). Many of the health and wellness issues affecting this population of residents are related to social determinants of health and health disparities (Coe et al., 2018; Parsons et al., 2019). Effectively addressing these issues requires coordinated efforts from service, teaching, and research across multiple disciplines. Health professions students and faculty staff attend weekly on-site wellness clinics in low-income senior apartment buildings to support aging in place and reduce preventable health care utilization (Parsons et al., 2019, 2020). RHWP has developed over time using continuous quality improvement processes to meet the needs of the community and learners with university support from Virginia Commonwealth University (VCU), an urban public research university. RHWP is aligned with the VCU mission to affect the lives of its students and the surrounding neighborhoods through community engagement and interdisciplinary education and scholarship.
VCU launched the Institute for Inclusion, Inquiry, and Innovation (iCubed) in 2016, and invested $2.8 million to support the hiring of 22 faculty, postdoctoral fellows, and visiting scholars into eight transdisciplinary cores. Faculty are recruited from underrepresented faculty groups and provided support through a Pathways to Professoriate Program; 16 are racial or ethnic minorities and 13 are women. Furthermore, the iCubed’s Commonwealth Scholars Program (CSP) is designed to bridge the gap between access, opportunity, and engagement for highly talented minority students to be mentored by faculty specializing in inclusive community-engaged research. VCU iCubed includes stakeholders from diverse backgrounds, communities, and disciplines relying heavily on partnership equity between the university and various communities. Collectively, the core nurtures communities to enhance the social and health aspects of daily living across the life span. All core leadership members participate in team science, diversity and inclusion training.
RHWP took the opportunity to enhance its service, education programs, and scholarship components by applying to VCU’s iCubed initiative. This allowed members of RHWP to seek the expertise of disciplines outside of the health professions (gerontology, urban planning) to develop a successful proposal and soon after became the Health and Wellness in Aging (HWA) Populations Transdisciplinary Core in iCubed, to significantly affect the population we serve through research initiatives.
The HWA Populations Transdisciplinary Core focuses on issues affecting the health and welfare of an older adult population (https://icubed.vcu.edu/programs/aging-populations/). The core goal of HWA is to address health equity, health outcomes, and wellness across the life span. Members of HWA collaborate with community health professionals, academics, urban planners, policy experts, and community housing experts to create sustainable programs of research that translate to the community. Students across disciplines are included in all HWA-related projects, encouraging them to pursue careers focused on supporting underserved older adults as they experience working with a transdisciplinary team. The HWA core meets together with all iCubed cores to discuss the teams’ collective progress and solutions to overcome barriers and challenges within and outside of the university.
Team Development
While the most common process for research collaboration occurs as a response to a funding announcement (National Research Council, 2015), our strategy is to focus on recruiting faculty with the desire to employ transdisciplinary research approaches to solve persistent problems for aging urban communities. Cluster hiring of faculty is a practiced mechanism a university will use to enhance inclusion and innovation; we adopted this approach to bring scholars from outside the university to VCU. Through VCU iCubed core development support HWA added three tenure track (nursing, pharmacy, and gerontology), one term faculty (nursing), and two postdoctoral fellows (medicine and pharmacy) in 2017–2018 with diverse professional training, life experiences, and scholarly approaches. The current composition of the HWA core consists of community representatives from our low-income housing agency partners and academic researchers from nursing, pharmacy, gerontology, epidemiology, medicine, medical anthropology, and occupational therapy.
HWA works to anticipate and address institutional barriers to successful scholarship and career progression for its members through informal mentorship among team members and mentoring in formal training programs such as the National Center for Faculty Development and Diversity Faculty Success Program. We actively learn about and from each other’s expertise. Mentoring of faculty and trainees is critical to our success. The diverse disciplines are enhanced by the minority faculty who bring unique skill sets and views, and are more representative of the community we serve, thereby changing the way we engage with our community. Furthermore, HWA mentors minority students to participate in the iCubed CSP. The CSP mentorship program identifies students with the highest financial need and highest talent and connects them with research faculty specializing in community-engaged research, thereby bridging the gap for students to learn transdisciplinary research. Although not necessarily a new idea, the diversity and inclusion efforts of the CSP program go beyond past efforts, which typically focused on improving the social climate for underrepresented minority students. Instead, it prioritizes the academic or research climate and experience (Lopatto, 2007). The paradigmatic shift is in the exposure to research at multiple levels by working within transdisciplinary research teams that are composed of faculty from different disciplines, postdoctoral scholars, graduate students, and their fellow undergraduate CSP students (Goel & Zanjani, 2018).
Addressing the disparities affecting low-income older adults who are aging in place requires an authentic partnership with the community. As a part of our mission to address community concerns around race and culture to advance social equity, we developed a community Advisory Council. The Advisory Council meets to ensure the community’s voice is integrated into a sustainable program of research and service. Residents from the housing buildings and surrounding neighborhoods comprise the council, which meets quarterly at a location in the community. To support equity, compensation for Advisory Council members includes an honorarium, transportation, and lunch.
Phases of Transdisciplinary Team-Based Research
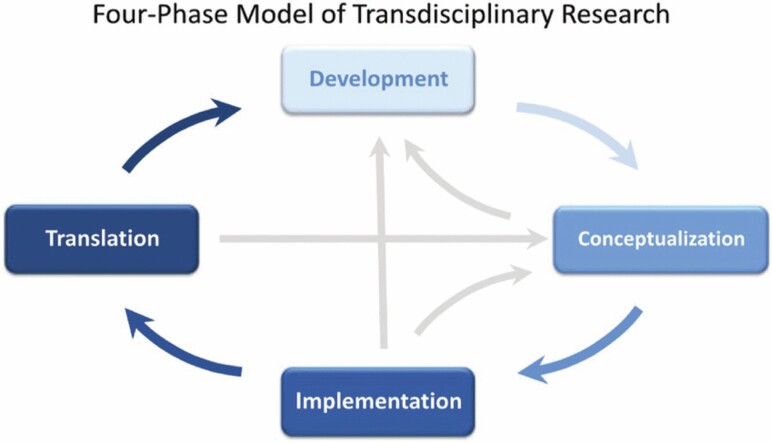
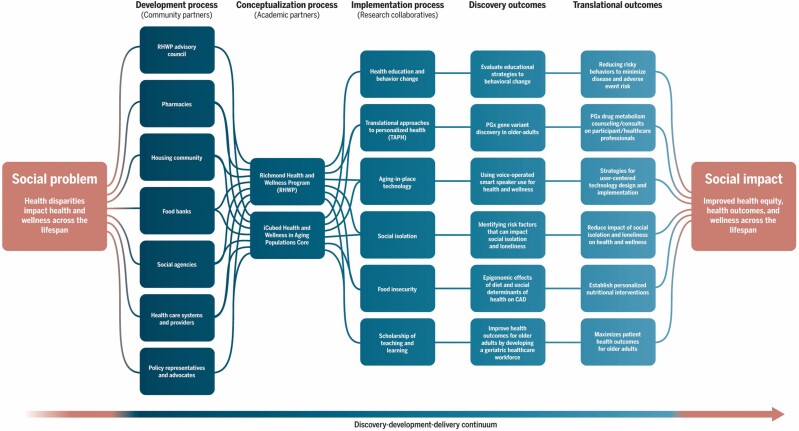
Our team has drawn upon the National Institutes of Health (NIH) four-phase model of transdisciplinary team-based research to operationalize our mission and goals (Hall, Vogel, et al., 2012). Below we describe our processes, challenges, and successes (see Figure 1). In a cyclical process, each time the team moved through the four phases, strategies emerged to address challenges and maximize successes. The four-phase model includes developmental and operational phases. In our case, the development and conceptualization team processes are the foundation for generating innovative ideas between academic researchers and community partners, and the operational phases included research implementation with discovery and translational outcomes (see Figure 2).
Figure 1.
Four-phase model of transdisciplinary team-based research. The four-phase model of transdisciplinary research supported by National Institutes of Health National Cancer Institute provides a foundation from which to operationalize transdisciplinary research (Hall, Vogel, et al., 2012). The team describes the process of developing a shared mission as a cyclical progression from development, conceptualization, implementation, and translation.
Figure 2.
Transdisciplinary Conceptual Model and Research Collaboratives. The model is driven by societal factors relevant to understanding minority health and health disparities. The lines represent the iterative process of communication that flows from the development phase to the conceptualization phase and then into the implementation process. There is a continuous flow of ideas back and forth between the three phases as research initiatives are generated. The findings from the discovery and translational outcomes may generate new research questions or interventions, which move back into the development and/or conceptualization process.
Development Process
Generating a Shared Mission and Critical Awareness
The process of developing a shared mission has been a complex nonlinear process with components of reflection, conflict, and growth. As a part of this process the HWA team reflected on and discussed the question, what does it mean to be transdisciplinary? In 2018, the team started a learning collaborative led by three members who further explored this question and developed a de-identified survey which was completed by all HWA members. The survey included two open-ended questions: (a) how would you describe your experience being a part of the HWA iCubed core (e.g., benefits, challenges, goals, motivations), and (b) what have you learned about the process of creating a transdisciplinary core? Two members compiled the responses as key features that create challenges (Harris et al., 2009). The themes from the survey were presented to the team for reflection and refinement. The team then identified responses to address the features that created challenges and determined indicators for success (see Table 1). Indicators for success were identified by the team as a place for continued evaluation of the teams’ collaborative effectiveness, transdisciplinary integration, and impact on the university and aging community.
Table 1.
Key Features, Goals, and Challenges of Transdisciplinary Team Science
| Features that create challenges | Feature examples | Team responses | Indicators for successa |
|---|---|---|---|
| Structural incongruities | - Expectations of each researcher’s home institution, variations in policies, workload, and methods for research. | - Recognize and respect these dynamic tensions. Find an effective platform to support the careers of all the transdisciplinary team members. - Share career goals and unit expectations among team members in a retreat format. |
- Issues brought to the attention of university leadership that impede transdisciplinary work are effectively addressed, including issues related to diversity and inclusion. - Faculty in the core achieve promotion/tenure. - Core’s academic units’ support faculty transdisciplinary work. - Diverse faculty recruited to the core are supported by the core and in their academic units. - Cross-core collaborations develop focusing on research, community engagement, and publication (eight established iCubed cores). |
| - University metrics used to evaluate faculty vary between schools and do not fit the team’s transdisciplinary goals. | - Use our unified goal to obtain funding to support infrastructure and independence. | - Funding support for a transdisciplinary center with sufficient resources to support the work. | |
| Interprofessional blind spots | - University and home institution pressures are creating transactional relationships where people are reduced to discipline and/or utility of skill. | - Instead of creating opportunities for cross-pollination which is more interdisciplinary in nature, use transdisciplinary approaches. Be aware of and capitalize on each other’s strengths, skills, goals, and career paths. | - Increased productivity, number of interprofessional proposals, and number and types of community partners within our projects over time. - Increased scholarship outcomes from students in the commonwealth scholars program. |
| - Unsure how to bring the individual components of expertise together to achieve the larger goal. | - Find ways to move beyond project management-styled meetings and promote idea formation and innovation. | - Demonstrate progress on effective collaboration, productive use of meeting time, and achieving transdisciplinary goals. | |
| High diversity of participation group function | - Unclear roles within the group and open membership creating fluidity vs consistency. | - Intentional discussion of individual strategic priority areas and roles (i.e., research, clinical practice, community outreach). | - Demonstrate increasing clarity of roles and strategic priority areas over time. |
| - Confusion about how community and university resources should play a role in the transdisciplinary team. | - Recognize the community-identified needs as a way to create transdisciplinary projects/collaboratives. | - Community partners indicate that community needs are addressed and the partnerships are successful. - Advisory board indicates that community-identified priority areas align with the strategic priorities of the core. - Advisory Committee membership is sustained and new members are recruited. - Active enrollment in community-engaged research with research findings disseminated back to the community for feedback and education. - Development of sustainable community coalitions. |
|
| High task dependency group dynamics | - Pressure to produce publications and grant funding is causing silos of research. | - Divide the conversation more equitably for everyone at the table and discuss individual priorities (i.e., research, clinical practice, community outreach) to find a common goal. | - Core members indicate that the team engages in equitable conversations. |
Note: aIndicators for success will be evaluated by the Health and Wellness in Aging (HWA) faculty in ongoing surveys.
The early development processes included using meeting time to discuss perceived roles/expectations of members, sharing leadership processes, handling conflict resolution, presenting individual research/expertise, and identifying collaborations. During our self-reflection process, HWA identified one feature—the changing composition of the team—that created challenges in developing a shared language and research agenda, as well as impaired the development of trusting relationships among members. Over time, the team adjusted to an influx of new faculty hires and a loss of members. Some members left the core when they felt the team’s focus was not aligned with their interests, others moved on to university administrative positions or retired, and a few faculty members’ academic units were unwilling to support their effort in the core. Although change in team composition is considered detrimental to team effectiveness, some instances have a positive effect and may enhance team performance and increase creative ideas (Gorman & Cooke, 2011; Gruenfeld et al., 2000). Alternatively, when a team member leaves who possesses unique knowledge and skills that others do not have, this can lead to deterioration of the team’s effectiveness. Barriers to successful integration and actions to retain valued members require regular reflection, discussion, and planning. To enhance the development process HWA reviewed the NIH team science framework, which is where many of the concepts in the four-phase model of transdisciplinary research originate (shared mental model and vision, group dynamics, processes, measures of success, etc.). Members of HWA were introduced to these concepts through the NIH team science training and the toolkit that core members of iCubed had an opportunity to participate in as part of the National Science Foundation Bridges study. Through team training, discussion, and evaluation of our transdisciplinary process, we continue to build an understanding of what makes an effective team and the processes for becoming a transdisciplinary team.
Externalizing Group Cognition
The team spent time creating a shared conceptual model by mapping the complex interplay between societal factors, community partners, and academic partners. Creating this model enabled the group to collectively envision the multiple levels of influence that shape the health disparities experienced by the community (Golden et al., 2015). Additionally, we developed a visual representation to identify the social and community networks involved in addressing these societal problems. This process prompted a shared vision for how to operationalize key elements of research into the social model. The resultant HWA Transdisciplinary Conceptual Model highlights how ideas to address societal problems are created between community partners and academic partners, thereby generating health and wellness initiatives for RHWP and/or research initiatives for the HWA core. Implementation of these initiatives becomes research collaboratives that integrate transdisciplinary perspectives to target the problem in innovative ways resulting in the discovery and translational outcomes to affect the local community (see Figure 2). A research collaborative consists of one or more of the HWA core members combined with experts in other disciplines (i.e., data managers, biostatisticians, additional academic, and community partners). The research collaboratives work to conduct the planned research and use separate meeting times to refine methods, recruitment, data collection, analysis, and dissemination of findings.
Psychological Safety
The concept of psychological safety is important for how a team operates, where members feel comfortable expressing independent thoughts, and debate about differences in world views and scientific methods, without judgment or retribution (Hall, Vogel, et al., 2012). Procedures for resolving conflict are written into the team’s grant proposal; the initial goal was to establish a safe environment for discussion of controversial issues built on a foundation of trust rather than of conflict or avoidance. When attempting to increase diversity of thought and life experience within a team, common understanding is expected to take time and effort to develop.
Engaging in collaboration planning as a way to evaluate team processes helps members identify ways to connect their individual needs with the collective team goals (Hall et al., 2019). While building trust takes time and consistent intentional engagement, implementation of this goal became challenging as group members adjusted to university and academic unit inconsistencies. One of the key features that the team recognized to create challenges is structural incongruities. The team reported misalignment between academic unit processes (i.e., faculty workload, grant submission policies) and the core’s goals. This feature is perpetuated by organizational cultures and differences in incentive systems (i.e., term faculty and tenure track policies) further contrasted with our community partners’ organizational culture. Structural incongruities are seen as leading to another feature identified as interprofessional blind spots. This is reflected in the group’s reporting of uncertainty on how to bring individual components of expertise together to achieve the larger goal and the feeling that organizational pressures created transactional relationships where people were reduced to discipline or skill. Unclear roles within the group are described as high diversity of participation. This included reports of confusion about individuals’ roles within the group, university, and community with questions on how to fuse information to make decisions, solve problems, or create new knowledge.
When the features were presented to the team for reflection and refinement, with further discussion, the analysis provided clarity and identified potential responses to address the features that created challenges (see Table 1). It will take time to manifest into a common understanding that members are acting in the interest of the team and community rather than individual self-interest. Onboarding new team members to this common understanding may require the team to consistently engage in team reflection.
Conceptualization Process
Shared Mission and Goals
The HWA core engages in research-informed practice and practice-informed research in a feedback loop with residents, researchers, and community partners. During the Fall 2017 Advisory Council meeting, stakeholders identified medication safety, adverse drug events, food insecurity, mental and sexual health, health service access, social isolation, cardiovascular disease, cognition, and diabetes among their topics of concerns (Zanjani et al., 2018). Themes identified from the Advisory Council meetings are used to advance our transdisciplinary team of scientists’ shared scholarship agenda. Our desire was to transcend the boundaries between the university and community by hiring individuals into the HWA core. One approach that we attempted, albeit unsuccessfully, was to create nontraditional faculty roles or shared community–faculty roles as part of our core. These roles had many challenges related to career progression, compensation, reporting structure/factors, and the barriers between academic and nonacademic culture were difficult to overcome. Currently, we function through bridges built with faculty serving as liaisons between academic researchers with the community and housing resident services coordinators collaborating with the core. In addition, following the principles of community-engaged research, our core appointed a community representative as an Affiliate Faculty to serve as a core member. One of the essential parts of our conceptual thinking was to have the individuals from our community partners as members of a transdisciplinary team. The intention was to create a shared language between scientists from different disciplines and community members by engaging nonacademic perspectives into the work. Our commitment to sustainability, especially in our relationship with the community, is different from many past university programs that came and went as a specific grant started and ended. Having our community partners on equal ground and working toward research goals collaboratively will require more than an advisory council and a representative on the HWA core. The development of sustainable community coalitions is one way we are working toward this vision of collaboration as a different model of engagement. This is a vision that the core agrees on and is still working to operationalize.
Operational Phase
Implementation Process
The HWA team meetings are held biweekly, to develop our shared research agenda and to address challenges to conducting research with the community. In the implementation process, launching of grant initiatives and ideas for collaborative research occurred early in the teams’ development phase. Research collaboratives have advanced based on the shared scholarship agendas identified by themes in the development process with community partners (see Figure 2). When an idea is generated, an individual or a team of researchers works to develop a research collaborative and carry out the research.
In reflecting on this process, the team that reported the discussion of research initiatives often dominated team meeting time. This group dynamic is identified as high task dependency, pressure within the group to produce publications and grant funding causing silos of research. The team discussed the desire to divide the agenda more equitably for everyone at the table and discuss individual priorities that represented all members (i.e., research, clinical, practice, community outreach) to find a common goal (see Table 1).
Research Collaboratives: Discovery and Translational Outcomes
The identified research collaboratives’ primary goal is to apply research that advances the discovery–development–delivery continuum process by providing innovative solutions to the stated societal problem, health disparities affect health and wellness across the life span (Hall, Vogel, et al., 2012). There are currently six collaboratives working to address the societal problems identified by our team (see Figure 2). Each research collaborative encompasses a discovery and translational outcome, thereby conceptualizing how the findings have an impact on health equity, health outcomes, and wellness across the life span.
1. Health Education/Behavior Change focuses on late-life health promotion through reducing risky behaviors to minimize disease and adverse-event risk. Behavior change is targeted through community health-promotion interventions presenting older adult-focused education, awareness, and motivational strategies. The discovery initiative is to evaluate behavioral change strategies. The translational goal is to evaluate the multidimensional health impact of community health-promotion interventions.
2. Translational Approach to Personalized Health engages in research focused on the discovery and translation of pharmacogenomic data to improve health outcomes. The collaborative addresses health disparities by utilizing pharmacogenomics (PGx) to study how genes affect an individual’s response to medications and determine if certain genetic differences are common in older African American adults, a population that is underrepresented in PGx research. The discovery initiative is to further characterize genotype differences for African Americans and identify new biomarkers for PGx. The translational component of our work is to use the PGx findings to improve therapeutic outcomes provided through medication management, education, and counseling for participants and health care providers.
3. Aging-in-place technology collaborative uses health monitoring technology to maintain healthy and independent living and improve access to health care among low-income, community-dwelling older adults. The discovery initiative includes understanding how to promote health and wellness through smart speakers and health monitoring technology. The translational initiative uses strategies for user-centered technology design and implementation to meet the needs of low-income senior housing residents.
4. Social isolation and loneliness collaborative focuses on the impact of social isolation and loneliness on health and wellness and understanding the factors that may affect morbidity and mortality. The RHWP program provides a platform for discovery and translation, including identifying risk factors that may be modifiable and providing opportunities to design and test interventions that can alleviate adverse outcomes of social isolation and loneliness on health and wellness.
5. Food insecurity collaborative focuses on addressing food insecurity and related social determinants of health affecting low-income urban communities. The discovery initiative includes uncovering the epigenomic effects of diet and social determinants of health on cardiovascular disease risk factors. The translational initiative is to establish personalized nutritional interventions tailored to individuals’ dietary patterns, social determinants of health, and sociocultural backgrounds.
6. Scholarship of teaching and learning collaborative focuses on advancing the quality of health care for older adults through interprofessional student and faculty development. The discovery initiative focuses on innovative programs that enhance education and training with transformative clinical and interprofessional experiences for health care trainees as well as community partnerships that engage older adults and caregivers in health promotion programs. The translational initiative focuses on developing a health care workforce that maximizes patient and family engagement and improves health outcomes for older adults by enhancing the gerontological perspective across the health care continuum.
The collaboratives are all funded and in the early phases of recruitment, data collection, and analysis. The majority of funding for the collaboratives has been obtained through foundations and internal funding to support the group’s federal funding goals. In order to translate findings into real-world applications, the core will continue to broaden its expertise to incorporate partners whose work influences policy, health organizations, and public health practitioners.
Discussion
Transdisciplinary teams are needed to create sustainable solutions for addressing the complexity of social health problems for older adults (Grigorovich et al., 2019; Rajapakse et al., 2020). For transdisciplinary team science to flourish institutions need to have a process for evaluating team science that includes traditional measures and nontraditional measures of shared scholarship, such as evidence of team science training, shared impact of research, and transdisciplinary integration (Mâsse et al., 2008). Measures of transdisciplinary collaborations should include evidence of the team’s shared understanding of knowledge translation (i.e., conceptual model), thereby going beyond the counts of shared grants, publications, and programs of research (Archibald et al., 2018; Hall, Stokols, et al., 2012; Mazumdar et al., 2015). We recognize that transdisciplinary methods of counting scholarship such as coauthorship instead of first authorship and multiple principal investigator status or team acronyms for grant submission are in conflict with traditional metrics used to evaluate faculty for promotion and tenure. These may be structural incongruities to address in a larger university policy platform. We strongly urge our fellow university administrators and colleagues to reduce structures preventing us from achieving transformative transdisciplinary research needed to solve complex aging issues. Our team anticipated challenges in authorship order and are attempting to discuss preemptively while working on supporting early career faculty.
Building truly integrated transdisciplinary teams takes time and resources. Our program has some potentially unique characteristics allowing the HWA core to emerge as a transdisciplinary team. These include (a) community engagement is highly valued as a part of the university’s strategic plan, (b) four of the core’s faculty have 75% time and effort funded by the university for iCubed-related research initiatives which fosters collaboration by reducing burden on grant budgets, and (c) strategic partners of iCubed include the Virginia Commonwealth University Office of the President, Office of the Provost and Vice President for Academic Affairs, Office of the Vice President for Health Sciences, Office of Research and Innovation, and Division for Inclusive Excellence. Our university’s investment in faculty development around community engagement, funding to support faculty workload dedication to research, and senior administrative support increases the likelihood for success.
Funding should support teams wanting to achieve transdisciplinary status for building an infrastructure to address persistent complex social, policy, and health problems. Funding calls and reviewers should take caution and examine the team and their transdisciplinary processes. In order to achieve Jean Piaget’s vision of transdisciplinary teams existing in “a total system without any firm boundaries between disciplines” (Piaget, 1972, p. 138), universities, discipline-specific home institutions, and community organizations have to find creative ways to address structural incongruencies as a key feature that creates challenges for transdisciplinary teams. For example, the metrics used for evaluation should be more inclusive and supportive for members of a transdisciplinary team.
Tools and resources for facilitating transdisciplinary team science are becoming more robust and teams are starting to share strategies applied for successful team science initiatives (Gehlert et al., 2014; Hall et al., 2019). We encourage teams to engage in collaboration planning as described in this paper by using deliberate approaches to assess factors that may influence scientific and collaborative success (Hall et al., 2019). Internal evaluations of the transdisciplinary team process are integral for teams to move beyond the multi- and interdisciplinary niche and reach true transdisciplinary status. More research is needed to develop measures that assess transdisciplinary integration. Once the process of transdisciplinary integration can be reliably measured, the next step would be to determine the impact of transdisciplinary team science initiatives.
Acknowledgments
iCubed Health and Wellness in Aging Transdisciplinary Core, a group of the investigators and community advisory council within the Health and Wellness in Aging Populations core, contributed to the funding, design, and implementation of the work presented; as a transdisciplinary team, we take equal partnership in the scholarship of this project. We acknowledge Christopher Bickel, BA for the artistic support provided for Health and Wellness in Aging Populations Transdisciplinary Conceptual Model. We thank all of our community partners who help us enhance health and wellness services and research initiatives.
Funding
This work is supported by the Institute for Inclusion, Inquiry and Innovation at Virginia Commonwealth University, Presidential Research Quest Fund (PeRQ), African American Cardiovascular Pharmacogenetic Consortium (ACCOuNT) study (U54 MD010723, NIH-NIMHD), Alzheimer’s and Related Disease Research Award Fund, American Association of Retired Persons (AARP), Health and Resources and Services Administration (HRSA), and Center for Clinical and Translational Research (UL1TR002649).
Conflict of Interest
None declared.
References
- Archibald, M. M., Lawless, M., Harvey, G., & Kitson, A. L. (2018). Transdisciplinary research for impact: Protocol for a realist evaluation of the relationship between transdisciplinary research collaboration and knowledge translation. BMJ Open, 8(4), e021775. doi: 10.1136/bmjopen-2018-021775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein, J. H., & Bernstein, J. H. (2015). Transdisciplinarity: A review of its origins, development, and current issues. Journal of Research Practice, 11. http://academicworks.cuny.edu/kb_pubshttp://jrp.icaap.org/index.php/jrp/article/view/510/412 [Google Scholar]
- Black, D., Scally, G., Orme, J., Hunt, A., Pilkington, P., Lawrence, R., & Ebi, K. (2019). Moving health upstream in urban development: Reflections on the operationalization of a transdisciplinary case study. Global Challenges (Hoboken, NJ), 3(4), 1700103. doi: 10.1002/gch2.201700103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan, C. W. (2017). Developing the transdisciplinary aging research agenda: New developments in big data. Current Aging Science, 11(1), 33–44. doi: 10.2174/1874609810666170719100122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coe, A. B., Moczygemba, L. R., Ogbonna, K. C., Parsons, P. L., Slattum, P. W., & Mazmanian, P. E. (2018). Low-income senior housing residents’ emergency department use and care transition problems. Journal of Pharmacy Practice, 31(6), 610–616. doi: 10.1177/0897190017734763 [DOI] [PubMed] [Google Scholar]
- Gehlert, S., Hall, K., Vogel, A., Hohl, S., Hartman, S., Nebeling, L., Redline, S., Schmitz, K., Thornquist, M., Patterson, R., & Thompson, B. (2014). Advancing transdisciplinary research: The transdisciplinary research on energetics and cancer initiative. Journal of Translational Medicine & Epidemiology, 2(2), 1032. http://www.ncbi.nlm.nih.gov/pubmed/25356437 [PMC free article] [PubMed] [Google Scholar]
- Goel, N., & Zanjani, F. (2018). iCubed’s Commonwealth Scholars Program: Bridging the gap between access and opportunity—VCU iCubed. https://icubed.vcu.edu/stories/icubed-stories/commonwealth-scholars/
- Golden, S. D., McLeroy, K. R., Green, L. W., Earp, J. A., & Lieberman, L. D. (2015). Upending the social ecological model to guide health promotion efforts toward policy and environmental change. Health Education & Behavior, 42(1 Suppl.), 8S–14S. doi: 10.1177/1090198115575098 [DOI] [PubMed] [Google Scholar]
- Gorman, J. C., & Cooke, N. J. (2011). Changes in team cognition after a retention interval: The benefits of mixing it up. Journal of Experimental Psychology: Applied, 17(4), 303–319. doi: 10.1037/a0025149 [DOI] [PubMed] [Google Scholar]
- Grigorovich, A., Fang, M. L., Sixsmith, J., & Kontos, P. (2019). Defining and evaluating transdisciplinary research: Implications for aging and technology. Disability and Rehabilitation: Assistive Technology, 14(6), 533–542. doi: 10.1080/17483107.2018.1496361 [DOI] [PubMed] [Google Scholar]
- Gruenfeld, D. H., Martorana, P. V., & Fan, E. T. (2000). What do groups learn from their worldliest members? Direct and indirect influence in dynamic teams. Organizational Behavior and Human Decision Processes, 82(1), 45–59. doi: 10.1006/obhd.2000.2886 [DOI] [Google Scholar]
- Hall, K. L., Stokols, D., Stipelman, B. A., Vogel, A. L., Feng, A., Masimore, B., Morgan, G., Moser, R. P., Marcus, S. E., & Berrigan, D. (2012). Assessing the value of team science: A study comparing center- and investigator-initiated grants. American Journal of Preventive Medicine, 42(2), 157–163. doi: 10.1016/j.amepre.2011.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall, K. L., Vogel, A. L., & Croyle, R. T. (Eds.). (2019). Strategies for team science success. Springer International Publishing. doi: 10.1007/978-3-030-20992-6 [DOI] [Google Scholar]
- Hall, K. L., Vogel, A. L., Stipelman, B., Stokols, D., Morgan, G., & Gehlert, S. (2012). A four-phase model of transdisciplinary team-based research: Goals, team processes, and strategies. Translational Behavioral Medicine, 2(4), 415–430. doi: 10.1007/s13142-012-0167-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey, G., Marshall, R. J., Jordan, Z., & Kitson, A. L. (2015). Exploring the hidden barriers in knowledge translation: A case study within an academic community. Qualitative Health Research, 25(11), 1506–1517. doi: 10.1177/1049732315580300 [DOI] [PubMed] [Google Scholar]
- Lopatto, D. (2007). Undergraduate research experiences support science career decisions and active learning. CBE Life Sciences Education, 6(4), 297–306. doi: 10.1187/cbe.07-06-0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mâsse, L. C., Moser, R. P., Stokols, D., Taylor, B. K., Marcus, S. E., Morgan, G. D., Hall, K. L., Croyle, R. T., & Trochim, W. M. (2008). Measuring collaboration and transdisciplinary integration in team science. American Journal of Preventive Medicine, 35(2 Suppl.), S151–S160. doi: 10.1016/j.amepre.2008.05.020 [DOI] [PubMed] [Google Scholar]
- Mazumdar, M., Messinger, S., Finkelstein, D. M., Goldberg, J. D., Lindsell, C. J., Morton, S. C., Pollock, B. H., Rahbar, M. H., Welty, L. J., Parker, R. A., & Biostatistics, Epidemiology, and Research Design (BERD) Key Function Committee of the Clinical and Translational Science Awards (CTSA) Consortium. (2015). Evaluating academic scientists collaborating in team-based research: A proposed framework. Academic Medicine, 90(10), 1302–1308. doi: 10.1097/ACM.0000000000000759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council . (2015). National Research Council: Enhancing the effectiveness of team science (Cooke N. J. & Hilton M. L., Eds.). The National Press. [PubMed] [Google Scholar]
- Parsons, P. L., Slattum, P. W., & Bleich, M. (2019). Mainstreaming health and wellness: The RHWP Innovation model to complement primary care. Nursing Forum, 54(2), 263–269. doi: 10.1111/nuf.12326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons, P. L., Slattum, P. W., Thomas, C. K., Cheng, J. L., Alsane D., & Giddens J. L. (2020). Evaluation of an interprofessional care coordination model: Benefits to health professions students and the community served. Advance online publication. doi: 10.1016/j.outlook.2020.09.007 [DOI] [PubMed]
- Piaget, J. (1972). The epistemology of interdisciplinary relationships. Interdisciplinarity: Problems of teaching and research in universities (pp. 127–139). OECD. [Google Scholar]
- Rajapakse, N., Sayre, M. H., & Pérez-Stable, E. J. (2020). Foreword: NIMHD transdisciplinary collaborative centers for health disparities research focused on precision medicine. Ethnicity and Disease, 30(Suppl. 1), 135–136. doi: 10.18865/ed.30.S1.135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfield, P. L. (1992). The potential of transdisciplinary research for sustaining and extending linkages between the health and social sciences. Social Science & Medicine (1982), 35(11), 1343–1357. doi: 10.1016/0277-9536(92)90038-r [DOI] [PubMed] [Google Scholar]
- Thompson Klein, J. (2004). Prospects for transdisciplinary. Futures, 36(4), 515–526. doi: 10.1016/j.futures.2003.10.007 [DOI] [Google Scholar]
- Zanjani, F., Falls, K., McQueen Gibson, E., Patel, K., Price, E., Sargent, L., Slattum, P., & Parsons, P. (2018). Richmond Health and Wellness Program: Community advisory council outcomes. Innovation in Aging, 2(Suppl. 1), 499–500. doi: 10.1093/geroni/igy023.1859 [DOI] [Google Scholar]