ABSTRACT
Despite recommendations and their occupational risk to influenza infection vaccine hesitancy remains a challenge among healthcare workers (HCWs). No studies have been conducted in Lebanon to assess the influenza vaccine’s acceptance among HCWs. We conducted a survey to assess factors associated with vaccine uptake and practices among HCWs in Lebanon. Only 40.4% of the HCWs reported receiving the 2018–2019 seasonal vaccine and 1 out 5 routinely received the seasonal vaccine. One-third of the HCWs reported having free access to the influenza vaccine. The willingness to receive the vaccine decreased had it been offered for a fee. Self, family and community protection (55.5%) was a key vaccination enabler. While, viral evolution, concerns regarding vaccine efficacy and side effects, and cost of vaccine ranked as top vaccination barriers. The majority of the HCWs (75%) recommended the vaccine to their patients. Past influenza vaccination (Odds ratio (OR) = 2.37, CI 1.48,3.79), willingness to receive the vaccine for free (OR = 6.93, CI 4.27–11.34) or having diagnosed influenza (OR = 1.81, CI 1.12–2.92) were significantly associated with HCWs’ willingness to recommend the vaccine to patients. Better knowledge about influenza and vaccination was strongly associated with the willingness to receive and recommend the vaccine (p < .001). The vaccination rate among HCWs in Lebanon was suboptimal despite the positive attitudes toward the influenza vaccine. Interventions that enhance vaccine accessibility and knowledge are warranted to improve vaccination coverage among HCWs.
KEYWORDS: Health care workers, vaccination, influenza, acceptance, knowledge, Lebanon
Introduction
Seasonal influenza represents a significant burden worldwide, in terms of disease morbidity and mortality. The annual global attack rate of influenza is estimated at 5–10% in adults and 20–30% in children resulting in three to five million hospitalizations and 290,000 to 650,000 associated respiratory deaths.1,2 Influenza virus is highly contagious and can spread easily from person to person by droplets and aerosols.2,3 The World Health Organization (WHO) recommends influenza vaccination for high-risk groups including pregnant women at any stage of pregnancy, children (6 months to 5 years of age), people with underlying medical conditions, and healthcare workers (HCWs).3 HCWs are at an increased risk of contracting influenza in their workplace not only from patients, but also from infected coworkers. This compromises patients’ safety as HCWs can transmit the influenza infection to vulnerable patients who may be at high risk for complications and severe illness.4–6 Influenza outbreaks among HCWs and patients are well documented and posing risk to staff and patients alike.7–9
Influenza vaccination of HCWs is an essential preventive measure to protect them, their families, and their patients.10,11 In this context, Amodio et al. demonstrated that the decrease in vaccination rate among HCWs during seven consecutive influenza seasons (2005–2012) was associated with an increase in the number of patients experiencing nosocomial influenza-like illness.12
Therefore, the WHO considers HCWs a priority high-risk group for receiving influenza vaccination to protect themselves, their patients, and ensure continuity of healthcare services.13 We recently reported that 14 countries in the Eastern Mediterranean Region (EMR) having influenza immunization policies during the 2015/2016 influenza season, included HCWs as a priority group for vaccination.14 Based on vaccine dose distribution, vaccination coverage in Lebanon among the whole population is estimated at 6%.15 However, data are scarce regarding the uptake rate of the influenza vaccine among HCWs in the EMR, including Lebanon. Additionally, there is a limited understanding of HCWs’ knowledge, attitudes, and practice toward influenza vaccination.16 A study among a group of Lebanese family physicians reported a clear deficiency in adult pneumococcal and influenza immunization awareness and practices.17 Consequently, examining vaccination coverage rates as well as understanding the knowledge and attitudes toward the seasonal influenza vaccine among HCWs is essential for developing interventions that could enhance the acceptance of influenza vaccination among HCWs. The lack of knowledge on influenza vaccines and hesitancy to take it by HCWs might also be a barrier for them to recommend it for their patients.18 Filling information gaps about influenza and its vaccine may enable an informed and evidence-based approach to improve vaccine uptake rates by the HCWs and their patients. Thus, this study aims to examine the uptake rates and to assess the knowledge, attitudes, and practices toward seasonal influenza vaccination among HCWs in Lebanon.
Methods
Study tool and design
We evaluated uptake rates, knowledge, attitudes, and practices (KAP) toward seasonal influenza vaccination among HCWs through a cross-sectional mixed-design survey. This study was conducted during the first six months of 2019 on a convenience sample of HCWs at health care institutions in three governorates of Lebanon: Beirut, North, and Bekaa. The survey locations were chosen based on the feasibility of gaining approval to conduct the survey and having students rotating at the facility. The self-administered questionnaire consisted of four open-ended and 24 closed-ended questions in English language.19 The questions were divided into three sections. The first section addressed the general sociodemographic characteristics of the subject such as age, gender, occupation, educational level and experience. The second part examined the flu vaccination history, in addition to the general knowledge and attitudes about influenza and influenza vaccines. The last section of the questionnaire addressed the HCWs’ knowledge, attitudes, and practices related to influenza disease and its vaccine in patient care. The open-ended questions focused on the top reasons for accepting/and recommending or refusing/and not recommending the influenza vaccine.
Ethics
The research proposal of this cross-sectional mixed-design study was reviewed and approved by the Lebanese International University and the American University of Beirut ethical bodies. An oral or electronic informed consent was obtained from every participant. The participants were assured of the confidentiality of the collected information, and the involvement in the study was voluntary.
Statistical analysis
For the summary of the data, descriptive statistics were used, such as counts and percentages for the categorical variables and means and standard deviations for the continuous ones. The responses of the open-ended questions were reviewed by two investigators who then defined the themes captured by the responses. The responses were then merged by theme and the frequencies of each theme were calculated. Chi-square (χ2) and independent t-tests were used to calculate the association between categorical and continuous variables respectively. Simple and multiple logistic regression analyses were applied to determine which socio-demographic and work-related characteristics of the study sample are associated with the odds to receive or recommend influenza vaccination. In the regression models, socio-demographic and work-related variables, including age, gender, occupation, specialty, the average number of patients seen per day and work experience were all used as independent variables. The willingness to receive (for free) or recommend influenza vaccination were each used as the dependent variable. All socio-demographic and work-related variables that showed statistical significance in the simple logistic model were included in the final multiple logistic regression model as independent variables, to adjust for possible confounders. Odds ratios and their respective 95% confidence intervals were calculated. A vaccine guidelines knowledge index was calculated to assess the knowledge of HCWs in groups to whom the vaccine is recommended according to WHO (supplementary Table S1), whereby correct answers were given 1-point and zero-point for incorrect answers. Finally, a knowledge index was created to assess its association with the willingness to receive or recommend the influenza vaccine (Supplementary Table S2). The index was computed by summing 11 variables related to knowledge. Correct answers were given 1-point and zero-point for incorrect answers. The median index with the interquartile range (IQR) was reported and the Mann-Whitney U test was used to assess the relationship between knowledge about influenza and influenza vaccine and the willingness to receive or recommend the vaccine. All reported p-values were based on two-sided tests and were compared with a significance level of 5%. Statistical Package for Social Sciences (SPSS) software V.24.0 for windows program was used to analyze the data.
Results
A total of 429 HCWs filled the questionnaire. The majority of HCWs were from Beirut (62.7%). The sample population comprised respondents from four age groups: 18–24 years old (21.7%), 25–34 (41.5%), 35–49 (21.7%) and ≥ 50 (15.2%), with 256 (59.7%) being males and 173 (40.3%) females. Nurses were the largest captured group (42.7%), followed by physicians and residents (28.7 and 11.0%, respectively). Most of the participants worked in the general internal medicine department (22.3%). The majority of the participants (57.5%) reported seeing 11 to 30 patients per day. Furthermore, 39.2% of the participating HCWs had less than five years of experience in healthcare and 34.9% have 5 to 14 years of experience (Table 1).
Table 1.
Characteristics of the study participants
| Characteristics | Category | Frequency (%) |
|---|---|---|
| Health facility site | Beirut | 269 (62.7) |
| n = 429* | Bekaa | 101 (23.5) |
| Tripoli | 59 (13.8) | |
| Age (years) | 18–24 | 93 (21.7) |
| n = 429 | 25–34 | 178 (41.5) |
| 35–49 | 93 (21.7) | |
| ≥50 | 65 (15.2) | |
| Gender | Male | 256 (59.7) |
| n = 429 | Female | 173 (40.3) |
| Profession | Nurse | 183 (42.7) |
| n = 429 | Physician | 123 (28.7) |
| Resident | 47 (11.0) | |
| Intern | 34 (7.9) | |
| Pharmacist | 5 (1.2) | |
| Other | 37 (8.6) | |
| Specialty | General/internal medicine | 95 (22.3) |
| n = 429 | ||
| Emergency department | 12 (2.8) | |
| Obstetrics/ gynecology | 19 (4.5) | |
| Adults Intensive Care Unit | 42 (9.9) | |
| Neonatal Intensive Care Unit | 10 (2.3) | |
| Pediatrics | 49 (11.5) | |
| Radiology | 14 (3.3) | |
| Surgery | 35 (8.2) | |
| Other | 150 (35.2) | |
| Average number of patients (per day) | ≤10 | 138 (32.8) |
| n = 421 | 11–30 | 242 (57.5) |
| >30 | 41 (9.7) | |
| Experience (years) | <5 | 168 (39.6) |
| n = 424 | 5–14 | 148 (34.9) |
| 15–24 | 57 (13.4) | |
| ≥25 | 51 (12.0) |
*, number of responses
In terms of vaccination practices, more than half of the participants have previously been vaccinated at least once against influenza (61.5%) in the past. Out of 292 HCWs who answered this question, 118 (40.4%) reported receiving the influenza vaccine in the 2018–2019 season. Furthermore, regarding the influenza vaccination history in the previous five years, 20.5% of the respondents were vaccinated five times, 30.1% were vaccinated between two to four times, and 25.3% were vaccinated only once. One hundred forty participants (33.3%) reported that the vaccine is available for free in their healthcare facility. Two-thirds of respondents (67.2%) reported that they would be willing to receive the vaccine if it is available for free, whereas the willingness to receive the vaccine decreased to 46.7% when asked if they would buy the influenza vaccine. More than three in four participants (76.8%) indicated that they would recommend the vaccine for their patients (Table 2). The majority of the HCWs (87.6%) correctly stated that the influenza vaccine should be administered annually.
Table 2.
Attitudes toward influenza vaccination
| Attitude toward vaccination | Frequency (%) | |
|---|---|---|
| History of influenza vaccination | Yes | 264 (61.5) |
| n = 429* | No | 142 (33.1) |
| I don’t remember | 23 (5.4) | |
| Number of influenza vaccines taken in past 5 years | Once | 74 (25.3) |
| n = 292 | 2–4 times | 88 (30.1) |
| 5 times | 60 (20.5) | |
| I don’t remember | 70 (24.0) | |
| Vaccinated this season | Yes | 118 (40.4) |
| n = 292 | No | 162 (55.5) |
| I don’t remember | 12 (4.1) | |
| Vaccine available for free in healthcare facility | Yes | 140 (33.3) |
| n = 421 | No | 198 (47.0) |
| I don’t know | 83 (19.7) | |
| Taking the vaccine for free | Yes | 287 (67.2) |
| n = 427 | No | 116 (27.2) |
| I don’t know | 24 (5.6) | |
| Taking the vaccine purchased | Yes | 193 (46.7) |
| n = 413 | No | 158 (38.3) |
| I don’t know | 62 (15.0) | |
| Recommend the vaccine for patients | Yes | 328 (76.8) |
| n = 427 | No | 51 (11.9) |
| I don’t know | 48 (11.2) | |
| Frequency of influenza vaccination | Every 6 months | 27 (6.3) |
| n = 428 | Every year | 375 (87.6) |
| Every 5 years | 2 (0.5) | |
| Once in a lifetime | 5 (1.2) | |
| Never | 19 (4.4) |
*, number of responses
More than half (55.5%) of the participants reported that they receive the influenza vaccine to protect themselves and their surrounding community or family. Furthermore, boosting immunity and decreasing the severity of the infection and the risk of complications (20.5%) and being at high risk of exposure to infection (6.5%) were the top reasons for being vaccinated (Figure 1(a)). On the other hand, some participants reported that the virus evolution and efficacy concerns (32.9%), side effects (16.4%), existing immunity (12.1%), and cost (expensive or not free) (11.4%) would discourage them from receiving the vaccine (Figure (b)). The participants reported relying on various sources for vaccine recommendations, including international organizations (e.g., WHO), the ministry of health, and their workplace (Figure 2).
Figure 1.
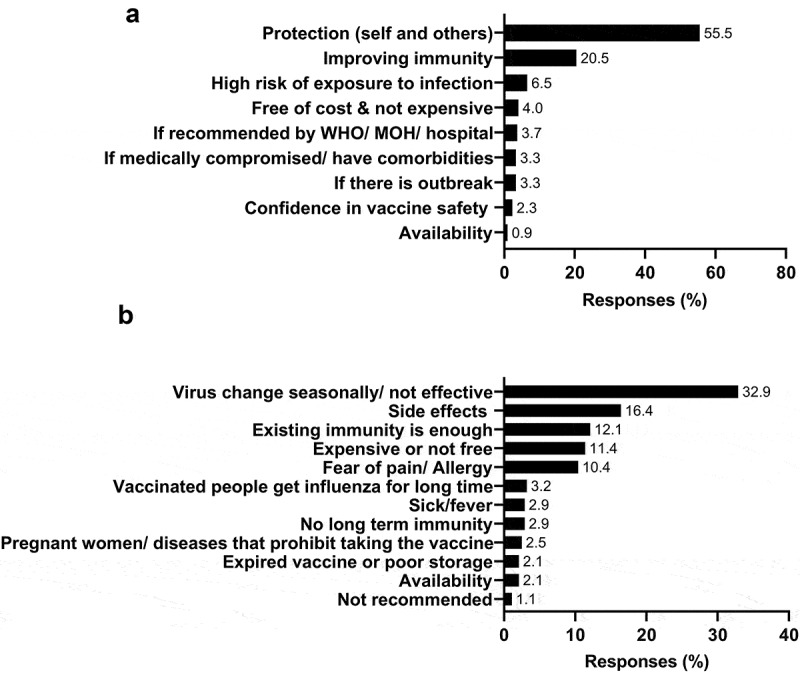
Enablers and barriers of influenza vaccination. (a) Reasons for vaccine acceptance. (b) Reasons for vaccine refusal.
Figure 2.
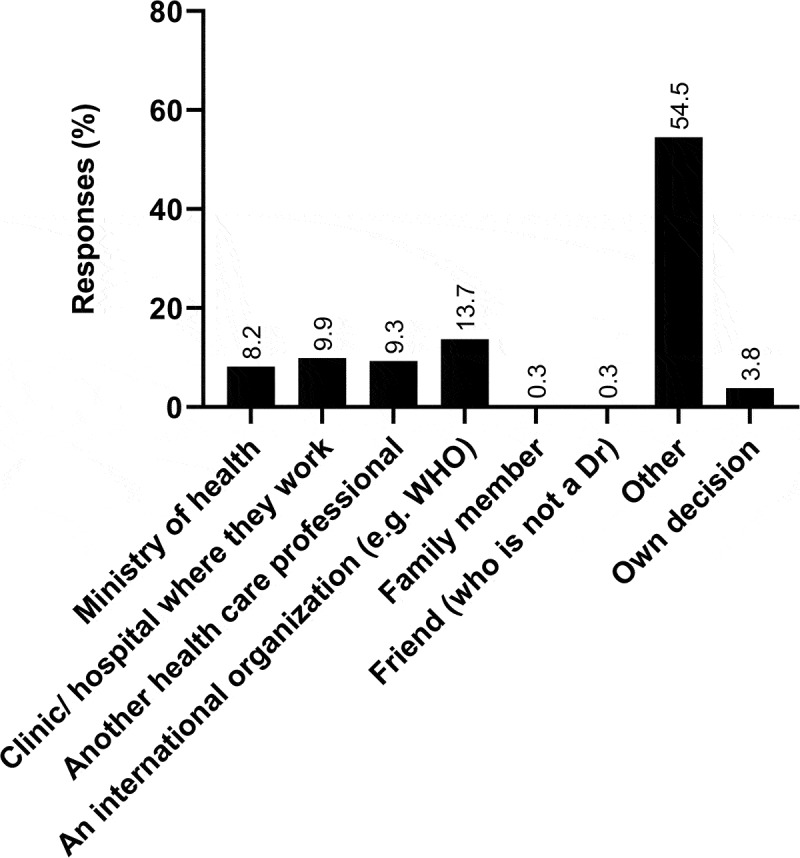
Sources of recommendation or advice for taking the vaccine.
In terms of knowledge in guideline recommendations, the majority of the participants (85.8%) correctly identified HCWs as a target group for vaccination, 80.9% elderly, 77.8% people with chronic medical conditions, and 66.3% children from 6–59 months. More than half (60%) of the participants correctly identified at least half of the high-risk groups recommended to receive the vaccine according to WHO guidelines, and only 29.6% correctly identified all the high-risk groups (Figure 3). The median guidelines’ knowledge score was 5.0 (IQR: 3.0–7.0).
Figure 3.
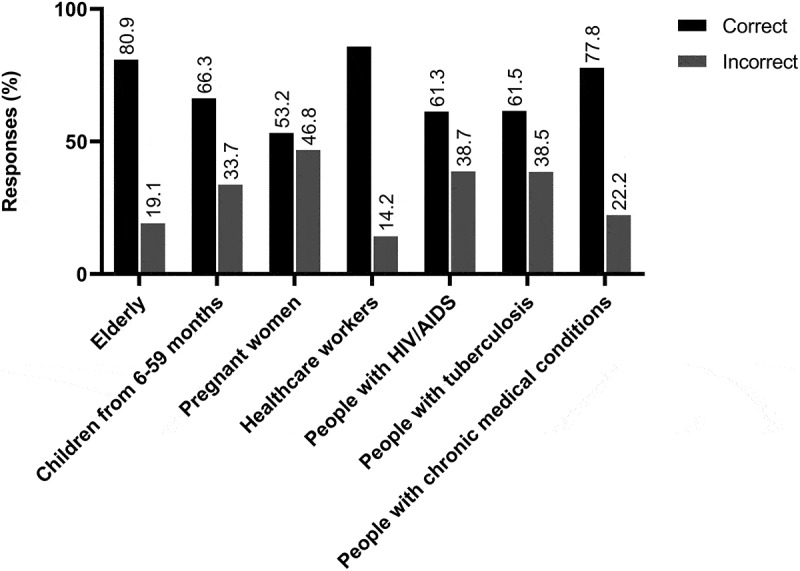
Guideline recommendations for influenza vaccination.
Hand washing and wearing a face mask were the most frequently reported protective measures that the participating HCWs would consider if they were dealing with a patient diagnosed with influenza (Figure 4). Besides, 32.6% of the participants would take the vaccine, and 14.2% would take an antiviral drug to protect themselves from infection after contacting a patient diagnosed with influenza.
Figure 4.
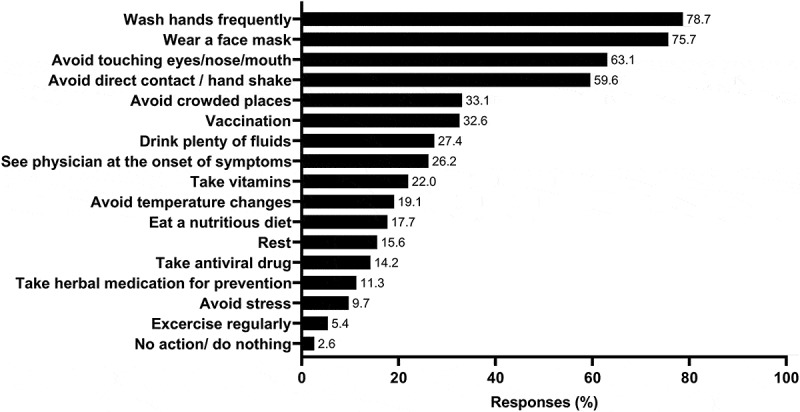
Measures to prevent influenza after diagnosing a patient with influenza.
Regarding the association between demographics or occupation and willingness to receive influenza vaccination, interns had significantly lower odds (OR = 0.41, 95% CI 0.19–0.89) for receiving influenza vaccination compared to physicians (Table 3). However, HCWs in the pediatrics department had significantly higher odds for willing to receive influenza vaccine as compared to those working in the general/internal medicine department (OR = 2.24, 95% CI 1.02–4.93). This is also the case for those in the obstetrics/ gynecology department (OR = 3.46, 95% CI 0.94–12.71). The association between demographics or occupation and willingness to recommend influenza vaccination was also studied (Table 3). Residents, interns, and nurses were significantly less likely to recommend the vaccine compared to physicians (OR = 0.38, 95% CI 0.17–0.83; OR = 0.29, 95% CI 0.13–0.69; OR = 0.51, 95% CI 0.28–0.91). Whilst, none of the other variables were found to be significantly associated with willingness to recommend the influenza vaccination.
Table 3.
Association between demographics and willingness to receive/recommend the influenza vaccine
| Willingness to receive the vaccine |
Willingness to recommend the vaccine |
|||||||
| Characteristics |
N * |
N(%) |
Adjusted OR [95%CI) |
P |
N |
N(%) |
Adjusted OR [95%CI) |
P |
| Age (years) | ||||||||
| 18–24 | 92 | 68 (23.7) | Ref | 82 | 70 (21.3) | Ref | ||
| 25–34 | 178 | 118 (41.1) | 0.69 [0.40,1.21] | 0.201 | 155 | 129 (39.3) | 0.88 [0.49,1.57] | 0.672 |
| 35–49 | 92 | 57 (19.9) | 0.57 [0.31,1.08] | 0.084 | 87 | 77 (23.5) | 1.58 [0.77,3.23] | 0.209 |
| ≥50 | 65 | 44 (15.3) | 0.74 [0.37,1.49] | 0.397 | 55 | 52 (15.9) | 1.42 [0.65,3.12] | 0.378 |
| Sex | ||||||||
| Female | 173 | 110 (38.3) | Ref | 158 | 130 (39.6) | Ref | ||
| Male | 254 | 177 (61.7) | 1.32 [0.87,1.98] | 0.188 | 221 | 198 (60.4) | 1.17 [0.74,1.84] | 0.500 |
| Occupation | ||||||||
| Physician | 123 | 84 (29.3) | Ref | 114 | 104 (31.7) | Ref | ||
| Resident | 46 | 28 (9.8) | 0.72 [0.36,1.46] | 0.365 | 38 | 31 (9.5) | 0.38 [0.17,0.83] | 0.015 |
| Intern | 34 | 16 (5.6) | 0.41 [0.19,0.89] | 0.025 | 27 | 21 (6.4) | 0.29 [0.13,0.69] | 0.005 |
| Nurse | 182 | 124 (43.2) | 0.99 [0.61,1.62] | 0.976 | 159 | 133 (40.5) | 0.51 [0.28,0.91] | 0.024 |
| Other | 42 | 35 (12.2) | 2.32 [0.95,5.69] | 0.065 | 41 | 39 (11.9) | 1.78 [0.57,5.57] | 0.321 |
| Specialty | ||||||||
| General/ internal medicine | 94 | 57 (20.1) | Ref | 79 | 71 (21.8) | Ref | ||
| Pediatrics | 49 | 38 (13.4) | 2.24 [1.02,4.93] | 0.045 | 46 | 43 (13.2) | 2.46 [0.93,6.49] | 0.070 |
| Obstetrics/ gynecology | 19 | 16 (5.6) | 3.46 [0.94,12.71] | 0.061 | 19 | 19 (5.8) | - | - |
| Other | 262 | 173 (60.9) | 1.26 [0.78,2.05] | 0.349 | 232 | 193 (59.2) | 0.98 [0.57,1.68] | 0.936 |
| Average number of patients seen per day | ||||||||
| ≤10 | 137 | 94 (33.5) | Ref | 123 | 106 (33.1) | Ref | ||
| 11–30 | 241 | 163 (58.0) | 0.96 [0.61,1.50] | 0.845 | 208 | 178 (55.6) | 0.87 [0.53,1.41] | 0.567 |
| >30 | 41 | 24 (8.5) | 0.65 [0.31,1.32] | 0.233 | 40 | 36 (11.2) | 2.17 [0.79,6.00] | 0.134 |
| Experience (years) | ||||||||
| <5 | 167 | 114 (40.4) | Ref | 144 | 123 (38.1) | Ref | ||
| 5–14 | 147 | 97 (34.4) | 0.90 [0.56,1.45] | 0.688 | 133 | 111 (34.4) | 1.13 [0.68,1.87] | 0.642 |
| 15–24 | 57 | 36 (12.8) | 0.80 [0.42,1.49] | 0.480 | 53 | 48 (14.9) | 2.19 [0.96,4.99] | 0.061 |
| ≥25 | 51 | 35 (12.4) | 1.02 [0.52,1.99] | 0.961 | 44 | 41 (12.7) | 1.50 [0.69,3.24] | 0.303 |
* N totals for each factor may not sum to the total N since missing responses (i.e. respondent indicated “I don’t know” or “I don’t remember” or skipped the question) are not included in Table 3 calculations.
The association between attitudes toward influenza and willingness to recommend the influenza vaccine was studied using simple logistic regression (Table 4). HCWs who received the vaccine in the past were significantly more likely to recommend it to their patients (OR = 2.37, CI 1.48,3.79). Participants who reported willingness to receive the vaccine for free had significantly higher odds for recommending it (OR = 6.93, CI 4.27–11.34). Further, individuals reporting that the influenza vaccine is available for free at their health facility were more likely to offer the influenza vaccine for their patients (OR = 1.93, CI 1.12–3.34). HCWs who received the influenza vaccine between two to four times in the past five years are 2.83 times more likely to recommend the vaccine for their patients compared to those who reported receiving the influenza vaccine only once in the past five years (OR = 2.83, CI 1.35–5.90). Participants who were highly confident that the influenza vaccine can prevent influenza were significantly more likely to recommend the vaccine as well (OR = 4.66, CI 2.90–7.49). Finally, confirming the diagnosis of influenza through a laboratory test (OR = 1.81, CI 1.12–2.92) or clinically (OR = 2.01, 1.23–3.28) were significantly associated with the tendency to recommend or give the vaccine.
Table 4.
Association between attitudes toward influenza and willingness to recommend the influenza vaccine
| Question | N* | Willing to recommend or give influenza vaccination n (%) |
Crude OR (CI) |
P value | |
|---|---|---|---|---|---|
| Have you ever been vaccinated against influenza? | Yes | 263 | 216 (82.1) | 2.37 [1.48,3.79] | <0.001 |
| No | 141 | 93 (66) | Ref | ||
| Are you willing to receive free influenza vaccine? | Yes | 286 | 253 (88.5) | 6.93 [4.27,11.34] | <0.001 |
| No | 139 | 73 (52.5) | Ref | ||
| Is influenza vaccine available for free to you and other health workers at your health facility? | Yes | 140 | 117 (83.6) | 1.93 [1.12,3.34] | 0.018 |
| No | 196 | 142 (72.4) | Ref | ||
| Did you receive influenza vaccine last year? | Yes | 118 | 102 (86.4) | 1.71 [0.89,3.26] | 0.106 |
| No | 161 | 127 (78.9) | Ref | ||
| How many times did you receive influenza vaccine in the past 5 years? | 1 | 74 | 55 (74.3) | Ref | |
| 2–4 | 147 | 131 (89.1) | 2.83 [1.35,5.90] | 0.006 | |
| How confident are you that influenza vaccine can prevent influenza? $ | ≤3 (Low confidence) | 131 | 74(22.6) | Ref | |
| ≥4 (High confidence) | 296 | 254 (77.4) | 4.66 [2.90,7.49] | <0.001 | |
| Have you ever made a laboratory-confirmed diagnosis of influenza in a patient? | Yes | 211 | 173 (82.0) | 1.81 [1.12,2.92] | 0.016 |
| No | 176 | 126 (71.6) | Ref | ||
| Have you ever made a clinical, non-laboratory confirmed diagnosis of influenza in a patient? | Yes | 187 | 187 (100.0) | 2.01 [1.23,3.28] | 0.005 |
| No | 165 | 118 (71.5) | Ref |
*N totals for each question may not sum to the total N since missing responses (i.e. respondent indicated “I don’t know” or “I don’t remember” or skipped the question) are not included in Table 3 calculations.
$Likert scale; 1 being “not at all” and 5 being “very much.” Neutral answers were considered low confidence.
The association between knowledge about influenza and its vaccine, and the willingness to receive and recommend the influenza vaccine was also analyzed. The knowledge index for the HCWs ranged between 6 and 9, with a median of 8.0. Using Mann Whitney U test, the total knowledge score was significantly associated with both the willingness to recommend (p < .001) and to receive the influenza vaccine (p < .001) (Table 5). These associations were also found when dividing the knowledge index into two categories: knowledge about influenza and knowledge about influenza vaccine (data not shown).
Table 5.
Association between knowledge about influenza and influenza vaccine and willingness to receive or give influenza vaccination
| Total sample n = 402 | Knowledge index * Range [0–11] |
Mann Whitney U test | P-value | |
|---|---|---|---|---|
| Median [IQR] | 8.0 [6.0–9.0] | |||
| Willing to receive influenza vaccination | No | 6.0 [5.0–8.0] | 7485.5 | <0.001 |
| Yes | 8.0 [7.0–9.0] | |||
| Willing to recommend or give influenza vaccination | No | 6.0 [4.0–7.75] | 4673.0 | <0.001 |
| Yes | 8.0 [7.0–9.0] |
Discussion
Vaccination is the most effective method to prevent influenza and its subsequent complications. To our knowledge, this study is the first cross-sectional mixed-design study in Lebanon to investigate the uptake rates, knowledge, attitudes, and practices (KAP) toward seasonal influenza vaccination among HCWs.
Merely, one in five of the participating HCWs in Lebanon reported regular influenza vaccine uptake during the past five seasons. This suggests a high rate of vaccination dropout and an opportunity for advocacy campaigns to sustain vaccine adherence. Only 40.4% of the surveyed HCWs reported receiving the influenza vaccine during the 2018–2019 season. This is nearly half the uptake coverage rate of the American HCWs (81.1%) during the same season,20 and well below the Healthy People 2020 target of 90% vaccination coverage for this risk group.21 Compared to neighboring EMR countries, the vaccine uptake rate among HCWs in Lebanon was better than that reported in the United Arab of Emirates (UAE; 32%) but lower than that reported in Oman (60% during the same season), Kuwait (67.2%), Qatar (67.7%), and Saudi Arabia (67.6%).19,22–25 Even though the optimal vaccination rate among HCWs is 100%, a minimum of 80% is considered effective in restraining the virus spread in healthcare settings.26 Thus, comprehensive strategies that take into consideration local barriers and enablers of vaccination should be implemented to enhance vaccine coverage among HCWs in Lebanon and the EMR in general.
The willingness to receive the influenza vaccine among the study participants increased by 44% (from 46.7% to 67.2%) if offered for free. In addition, the cost of the vaccine was the fourth most common barrier to vaccine acceptance. This suggests that enhancing vaccine accessibility and offering free vaccination can improve vaccine coverage. Consistently, a recent study from neighboring Qatar showed that free vaccination was associated with significant improvement in vaccine uptake among HCWs.27 Similar findings were also reported in the United States of America28,29 and Oman.19 Furthermore, a systematic review by Bish et al. reported that lower influenza vaccine costs are highly associated with the vaccination decision.30
Regarding vaccine enablers, our study revealed that self, family, and community protection against influenza are the key drivers of HCWs’ for vaccine acceptance. This was consistent with the findings of a study conducted in three Middle Eastern countries; the United Arab Emirates, Kuwait, and Oman.19,25 A recent study from the UAE reported that the majority (75%) of HCWs believed that influenza vaccination protected them and their families against infection.22 On the other hand, the concern about vaccine efficacy due to the rapid evolution of the virus was the most frequently reported barrier to vaccination among our study group. While this is a valid concern, it is well documented that vaccine mismatches and virus antigenic drifts do not fully abolish vaccine efficacy.31 Fear of side effects was also commonly cited as a barrier to vaccination in our study group. Similarly, studies from the EMR, the United States of America, and Europe assessing vaccine hesitancy among HCWs reported that side effects were their major concern.16,19,32,33 It is well documented that the majority of vaccine-related adverse events are mild and resolve spontaneously.34,35 Therefore, educating healthcare workers about influenza and vaccine efficacy and safety is warranted to alleviate such concerns and enhance uptake.
We demonstrated a varying level of knowledge about the risk groups for whom the influenza vaccine is recommended, with only one-third of the participants being aware of all the risk groups. Such variability in guidelines knowledge was in concordance with similar studies in Iran, India, Saudi Arabia, Oman, and the UAE.19,36–39 Importantly, the majority of HCWs in our and previous studies were aware of the recommendations to receive the influenza vaccine.19,36–39 Almost half of our study participants depend on vaccine recommendations from sources other than the ministry of health, international organizations (e.g. WHO) or other HCWs. Thus, more emphasis should be placed on communicating the recommendations for the influenza vaccine with HCWs particularly through the ministries of health. In Srinagar, India, 88% of HCWs thought that the seasonal influenza vaccine should be mandatory for those working in pediatrics wards.39 In our study, data showed that HCWs in the pediatrics department (OR = 2.24, p < .05) were more likely to receive the influenza vaccine. Moreover, receiving the vaccine by the HCWs was associated with an increased likelihood to recommend seasonal influenza vaccination to their patients. This is an important observation knowing that children are a high-risk group for influenza infection and complications. HCWs working with pediatrics might be more aware of vaccination recommendations as most vaccines are administered in this age group.
Similar to previous findings in Oman, Qatar, Saudi Arabia, and South Africa,19,23,24,33 the majority of surveyed HCWs in our study recommended the vaccine to their patients. In this study, a previous vaccination status, willingness to receive the vaccine by HCWs, and better knowledge about influenza and its vaccination were strongly associated with the tendency to recommend it to patients. In line with these findings, AlMarzooqi et al. reported that knowledge and attitudes to influenza vaccination among HCWs impact their decision to recommend it to patients in the UAE.37 The majority of study participants (85.7%) having a high knowledge level agreed to recommend the vaccine for their patients. These findings have important implications for pandemic preparedness as HCWs workers are the frontline of response during a pandemic and a trustable source of recommendation for patients. Higher knowledge scores were also associated with willingness to receive seasonal influenza vaccination in our study, which has important implications for pandemic preparedness. A review of HCWs’ compliance with pandemic influenza vaccination revealed that the receipt of seasonal influenza in previous seasons is a predictor of pandemic influenza vaccine acceptance.40 Moreover, Bonaccorsi et al. reported that pandemic influenza vaccine denial was higher among Italian HCWs who did not receive the seasonal vaccine in the previous season.41
The study had several limitations. First, the data collection relied on self-reported answers for practices, beliefs and knowledge. These answers could be subject to errors due to memory recall or social desirability bias. Second, the sample of HCWs considered in this study was conveniently selected from three governorates of Lebanon and therefore might not be nationally representative. Future studies are encouraged to survey a nationally representative sample of community HCWs from the six Lebanese governorates. Third, the response rate was not recorded. Finally, the cross-sectional mixed-design nature of the study prevented any inference about the change in beliefs, practices or knowledge over time among HCWs in the country.
In conclusion, vaccination rates among HCWs in Lebanon remain suboptimal. Nonetheless, in an encouraging observation, more HCWs expressed willingness to receive the vaccine if it was available for free. Importantly, HCWs who previously received the vaccine or those who expressed willingness to vaccinate were more likely to recommend it to their patients. Additionally, better knowledge about influenza and its vaccine was strongly associated with the willingness to recommend the vaccine. Thus, interventions that rely on improving vaccine accessibility and knowledge are poised to enhance the acceptance of vaccination and motivate HCWs to recommend it to their patients. Our study highlighted the opportunity to enhance vaccine awareness and uptake among HCWs (and potentially among the general population) through enhancing HCWs’ vaccine provision convenience and targeted educational campaigns.
Supplementary Material
Acknowledgments
We are grateful to all the HCWs who took part in this study. We thank Margaret McCarron for the discussions and input on the study and Malak Al-Ibrahim for technical help.
Funding Statement
This research was funded by the WHO Regional Office for the Eastern Mediterranean; World Health Organization (WHO).
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2021.1948783.
References
- 1.World Health Organization . Influenza [Internet]. WHO2017. [accessed 2021. Feb 2]. http://www.who.int/biologicals/vaccines/influenza/en/.
- 2.Iuliano AD, Roguski KM, Chang HH, Muscatello DJ, Palekar R, Tempia S, Cohen C, Gran JM, Schanzer D, Cowling BJ, et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet Lond Engl. 2018;391:1285–300. doi: 10.1016/S0140-6736(17)33293-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . Seasonal Influenza Fact Sheet [Internet]. 2018. [accessed 2021 May 17]. https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal).
- 4.Stott DJ, Kerr G, Carman WF.. Nosocomial transmission of influenza. Occup Med Oxf Engl. 2002;52:249–53. doi: 10.1093/occmed/52.5.249. [DOI] [PubMed] [Google Scholar]
- 5.Salgado CD, Farr BM, Hall KK, Hayden FG.. Influenza in the acute hospital setting. Lancet Infect Dis. 2002;2:145–55. doi: 10.1016/S1473-3099(02)00221-9. [DOI] [PubMed] [Google Scholar]
- 6.Parkash N, Beckingham W, Andersson P, Kelly P, Senanayake S, Coatsworth N. Hospital-acquired influenza in an Australian tertiary Centre 2017: a surveillance based study. BMC Pulm Med. 2019;19:79. doi: 10.1186/s12890-019-0842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oguma T, Saito R, Masaki H, Hoshino K, Zaraket H, Suzuki Y, Caperig-Dapat I, Dapat C, Baranovich T, Kuroki R, et al. Molecular characteristics of outbreaks of nosocomial infection with influenza A/H3N2 virus variants. Infect Control Hosp Epidemiol. 2011;32:267–75. doi: 10.1086/658671. [DOI] [PubMed] [Google Scholar]
- 8.Wilson KE, Wood SM, Schaecher KE, Cromwell KB, Godich J, Knapp MH, Sklar MJ, Ewing D, Raviprakash K, Defang G, et al. Nosocomial outbreak of influenza A H3N2 in an inpatient oncology unit related to health care workers presenting to work while ill. Am J Infect Control. 2019;47:683–87. doi: 10.1016/j.ajic.2018.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eibach D, Casalegno J-S, Bouscambert M, Bénet T, Regis C, Comte B, Kim B-A, Vanhems P, Lina B. Routes of transmission during a nosocomial influenza A(H3N2) outbreak among geriatric patients and healthcare workers. J Hosp Infect. 2014;86:188–93. doi: 10.1016/j.jhin.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Influenza (Seasonal) [Internet] . [accessed 2019 Dec 28]. https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal).
- 11.Influenza Vaccination Coverage Among Health Care Personnel — United States , 2017–18 Influenza Season | MMWR [Internet]. [accessed 2019 Dec 28]. https://www.cdc.gov/mmwr/volumes/67/wr/mm6738a2.htm.
- 12.Amodio E, Restivo V, Firenze A, Mammina C, Tramuto F, Vitale F. Can influenza vaccination coverage among healthcare workers influence the risk of nosocomial influenza-like illness in hospitalized patients? J Hosp Infect. 2014;86:182–87. doi: 10.1016/j.jhin.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization . Vaccines against influenza WHO position paper – november 2012 [Internet]. 2012. [accessed 2021 Mar 1]. https://www.who.int/wer/2012/wer8747.pdf?ua=1.
- 14.Abubakar A, Melhem N, Malik M, Dbaibo G, Khan WM, Zaraket H. Seasonal influenza vaccination policies in the Eastern Mediterranean Region: current status and the way forward. Vaccine. 2019;37:1601–07. doi: 10.1016/j.vaccine.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 15.7th MENA-ISN study group; Al Awaidi S, Abusrewil S, AbuHasan M, Akcay M, Aksakal FNB, Bashir U, Elahmer O, Esteghamati A, Gahwagi M, et al. Influenza vaccination situation in Middle-East and North Africa countries: report of the 7th MENA Influenza Stakeholders Network (MENA-ISN). J Infect Public Health. 2018;11:845–50. doi: 10.1016/j.jiph.2018.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zaraket H, Melhem N, Malik M, Khan WM, Dbaibo G, Abubakar A. Review of seasonal influenza vaccination in the Eastern Mediterranean Region: policies, use and barriers. J Infect Public Health. 2019;12:472–78. doi: 10.1016/j.jiph.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 17.Romani MH, Musharrafieh UM, Lakkis NA, Hamadeh GN. Family physicians beliefs and attitudes regarding adult pneumococcal and influenza immunization in Lebanon. Fam Pract. 2011;28:632–37. doi: 10.1093/fampra/cmr038. [DOI] [PubMed] [Google Scholar]
- 18.Maisa A, Milligan S, Quinn A, Boulter D, Johnston J, Treanor C, Bradley DT. Vaccination against pertussis and influenza in pregnancy: a qualitative study of barriers and facilitators. Public Health. 2018;162:111–17. doi: 10.1016/j.puhe.2018.05.025. [DOI] [PubMed] [Google Scholar]
- 19.Awaidy STA, K Al Mayahi Z, Kaddoura M, Mahomed O, Lahoud N, Abubakar A, Zaraket H. Influenza vaccination hesitancy among healthcare workers in South Al Batinah Governorate in Oman: a cross-sectional study. Vaccines. 2020;8:661. doi: 10.3390/vaccines8040661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Influenza Vaccination Information for Health Care Workers | CDC [Internet] . [accessed 2019 Dec 28]. https://www.cdc.gov/flu/professionals/healthcareworkers.htm.
- 21.National Vaccine Advisory Committee . Strategies to achieve the healthy people 2020 annual influenza vaccine coverage goal for health-care personnel: recommendations from the national vaccine advisory committee. Public Health Rep Wash DC 1974 2013;128:7–25. [PMC free article] [PubMed] [Google Scholar]
- 22.Abu Hammour W, Al-Saleh S. Knowledge, attitudes, and practice of healthcare workers toward influenza vaccination at Al Jalila Children’s Specialty Hospital (AJCH), Dubai, UAE. Int J Pediatr Adolesc Med. 2019;6:16–20. doi: 10.1016/j.ijpam.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alshammari TM, Yusuff KB, Aziz MM, Subaie GM. Healthcare professionals’ knowledge, attitude and acceptance of influenza vaccination in Saudi Arabia: a multicenter cross-sectional study. BMC Health Serv Res. 2019;19:229. doi: 10.1186/s12913-019-4054-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alhammadi A, Khalifa M, Abdulrahman H, Almuslemani E, Alhothi A, Janahi M. Attitudes and perceptions among the pediatric health care providers toward influenza vaccination in Qatar: a cross-sectional study. Vaccine. 2015;33:3821–28. doi: 10.1016/j.vaccine.2015.06.082. [DOI] [PubMed] [Google Scholar]
- 25.Abu-Gharbieh E, Fahmy S, Rasool BA, Khan S. Influenza vaccination: healthcare workers attitude in Three Middle East Countries. Int J Med Sci. 2010;7:319–25. doi: 10.7150/ijms.7.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salgado CD, Giannetta ET, Hayden FG, Farr BM. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Infect Control Hosp Epidemiol. 2004;25:923–28. doi: 10.1086/502321. [DOI] [PubMed] [Google Scholar]
- 27.Mustafa M, Al-Khal A, Al Maslamani M, Al Soub H. Improving influenza vaccination rates of healthcare workers: a multipronged approach in Qatar. East Mediterr Health J Rev Sante Mediterr Orient Al-Majallah Al-Sihhiyah Li-Sharq Al-Mutawassit. 2017;23:303–10. [DOI] [PubMed] [Google Scholar]
- 28.Kung YM. A quality improvement project to increase influenza vaccination in healthcare personnel at a university health center. J Am Assoc Nurse Pract. 2014;26:148–54. doi: 10.1002/2327-6924.12060. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC) . Interventions to increase influenza vaccination of health-care workers--California and Minnesota. MMWR Morb Mortal Wkly Rep 2005;54:196–99. [PubMed] [Google Scholar]
- 30.Bish A, Yardley L, Nicoll A, Michie S. Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine. 2011;29:6472–84. doi: 10.1016/j.vaccine.2011.06.107. [DOI] [PubMed] [Google Scholar]
- 31.Russell K, Chung JR, Monto AS, Martin ET, Belongia EA, McLean HQ, Gaglani M, Murthy K, Zimmerman RK, Nowalk MP, et al. Influenza vaccine effectiveness in older adults compared with younger adults over five seasons. Vaccine. 2018;36:1272–78. doi: 10.1016/j.vaccine.2018.01.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karafillakis E, Dinca I, Apfel F, Cecconi S, Wűrz A, Takacs J, Suk J, Celentano LP, Kramarz P, Larson HJ. Vaccine hesitancy among healthcare workers in Europe: a qualitative study. Vaccine. 2016;34:5013–20. doi: 10.1016/j.vaccine.2016.08.029. [DOI] [PubMed] [Google Scholar]
- 33.McAnerney JM, Walaza S, Cohen AL, Tempia S, Buys A, Venter M, Blumberg L, Duque J, Cohen C. Effectiveness and knowledge, attitudes and practices of seasonal influenza vaccine in primary healthcare settings in South Africa, 2010–2013. Influenza Other Respir Viruses. 2015;9:143–50. doi: 10.1111/irv.12305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meijer WJ, Wensing AMJ, Bos AA, Kuiphuis JCF, Hagelen EMM, Wilschut JC, De Vries MJT, Riezebos-Brilman A. Influenza vaccination in healthcare workers; comparison of side effects and preferred route of administration of intradermal versus intramuscular administration. Vaccine. 2017;35:1517–23. doi: 10.1016/j.vaccine.2017.01.065. [DOI] [PubMed] [Google Scholar]
- 35.Coleman BL, McNeil SA, Langley JM, Halperin SA, McGeer AJ. Differences in efficiency, satisfaction and adverse events between self-administered intradermal and nurse-administered intramuscular influenza vaccines in hospital workers. Vaccine. 2015;33:6635–40. doi: 10.1016/j.vaccine.2015.10.095. [DOI] [PubMed] [Google Scholar]
- 36.Alshammari TM, AlFehaid LS, AlFraih JK, Aljadhey HS. Health care professionals’ awareness of, knowledge about and attitude to influenza vaccination. Vaccine. 2014;32:5957–61. doi: 10.1016/j.vaccine.2014.08.061. [DOI] [PubMed] [Google Scholar]
- 37.AlMarzooqi LM, AlMajidi AA, AlHammadi AA, AlAli N, Khansaheb HH. Knowledge, attitude, and practice of influenza vaccine immunization among primary healthcare providers in Dubai health authority, 2016-2017. Hum Vaccines Immunother. 2018;14:2999–3004. doi: 10.1080/21645515.2018.1507667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khazaeipour Z, Ranjbarnovin N, Hoseini N. Influenza immunization rates, knowledge, attitudes and practices of health care workers in Iran. J Infect Dev Ctries. 2010;4:636–44. doi: 10.3855/jidc.1152. [DOI] [PubMed] [Google Scholar]
- 39.Bali NK, Ashraf M, Ahmad F, Khan UH, Widdowson M, Lal RB, Koul PA. Knowledge, attitude, and practices about the seasonal influenza vaccination among healthcare workers in Srinagar, India. Influenza Other Respir Viruses. 2013;7:540–45. doi: 10.1111/j.1750-2659.2012.00416.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bellia C, Setbon M, Zylberman P, Flahault A. Healthcare worker compliance with seasonal and pandemic influenza vaccination. Influenza Other Respir Viruses. 2013;7:97–104. doi: 10.1111/irv.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bonaccorsi G, Lorini C, Santomauro F, Guarducci S, Pellegrino E, Puggelli F, Balli M, Bonanni P. Predictive factors associated with the acceptance of pandemic and seasonal influenza vaccination in health care workers and students in Tuscany, Central Italy. Hum Vaccines Immunother. 2013;9:2603–12. doi: 10.4161/hv.26036. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


