ABSTRACT
Vaccine hesitancy regarding the coronavirus disease 2019 (COVID-19) vaccine is widespread during the COVID-19 pandemic. Many recent studies have reported that the confidence of the vaccination and perceived risk were associated with vaccination intent, yet few studies have focused on other psychological factors. This study aimed to clarify the trends in COVID-19 vaccination intent and to identify the association between the 5C psychological antecedents and COVID-19 vaccination intent by sex and age in Japan. This was a longitudinal study conducted through an Internet-based survey from January 2021 to April 2021 before and after vaccine distribution in Japan, including 2,655 participants recruited by quota sampling. Participants were asked to indicate how likely they were to get vaccinated against COVID-19. In the second survey, the participants responded to questions regarding the 5C psychological antecedents: confidence, complacency, constraints (structural and psychological barriers), calculation (engagement in extensive information searching), and collective responsibility (willingness to protect others). Multiple logistic regression analysis was performed to clarify the association between the 5C psychological antecedents and COVID-19 vaccination intent in the second wave survey. COVID-19 vaccination intent improved from 62.1% to 72.4% after vaccine distribution, but no significant difference was found in young men. Confidence and collective responsibility were positively associated with vaccination intent, and calculation was negatively associated among all generations. COVID-19 vaccination intent may be affected not only by confidence and constraints but also by calculation and collective responsibility, and further research is needed.
KEYWORDS: Coronavirus disease, vaccine hesitancy, public health, epidemiology, personal protective measure
Introduction
As of May 2021, the coronavirus disease 2019 (COVID-19) pandemic remains active. While effective vaccines are highly anticipated, vaccine hesitancy regarding COVID-19 vaccines is globally widespread.1–4 Vaccine hesitancy, as defined by the SAGE Working Group on Vaccine Hesitancy, is a delay in acceptance or refusal of vaccination despite the availability of vaccination services.5 Many previous studies on vaccine hesitancy on COVID−19 vaccines have reported that vaccine acceptance of COVID−19 differs by sociodemographic factors such as sex, age, educational level, income level, and race.1,6–11 Recent systematic reviews have also reported that COVID−19 vaccine acceptance is lower in women and young adults than men and older adults, respectively.2,3,4
One of the reasons why vaccine hesitancy differs by age and sex is the difference in attitudes toward COVID−19 infection and vaccines.12,13 The SAGE working group on vaccine hesitancy highlights three categories, namely, confidence, complacency, and convenience, referred to as 3Cs, as psychological factors that are associated with vaccine hesitancy.5 Confidence refers to trust in the efficacy and safety of vaccines, health services, policy makers, and so on.5 Complacency exists where the perceived risks of vaccine-preventable diseases are low and vaccination is not deemed a necessary preventive action.5 Convenience is a significant factor when physical availability, affordability and willingness-to-pay, geographical accessibility, ability to understand (language and health literacy), and appeal of immunization services affect uptake.5
Additionally, Betsch et al. proposed the 5C psychological antecedents of vaccination, which add two psychological factors, namely, calculation and collective responsibility, to the three psychological factors.14 Calculation refers to individuals’ engagement in extensive information searching, and it is assumed that individuals high in calculation evaluate the risks of infections and vaccination to derive a good decision.14 Collective responsibility is defined as the willingness to protect others by one’s own vaccination through herd immunity.14 Regarding COVID−19 vaccine hesitancy, although many studies have reported an association between the 3Cs and vaccine hesitancy,1,6–8,15–18 only a few studies have evaluated the association of vaccine hesitancy with calculation and collective responsibility,10,17,18 especially about calculation.16
When considering interventions for populations with low vaccine acceptance, it is important to clarify the status of psychological factors in the target population and to conduct an evidence-informed educational campaign.19 Regarding the COVID-19 vaccine, it is necessary to clarify the status of psychological factors among high vaccine hesitancy population groups such as women and younger age groups to reach high vaccination coverage.2 In Japan, the distribution of the COVID-19 vaccine has just begun among healthcare workers in February 2021, and vaccination for citizens, in April 2021.20 Japan has one of the lowest vaccine confidence indexes in the world, which may be due to the incident in 2013,21 where the Japanese Ministry of Health, Labor and Welfare suspended proactive recommendation of the human papillomavirus vaccine because of safety concerns raised by the general public.22 Naturally, there are concerns regarding COVID-19 vaccine acceptance in the country. However, few studies have been conducted on COVID-19 vaccination intent among ordinary citizens in Japan,10,23 and to the best of our knowledge, no study has clarified the vaccination intent after the start of vaccination.
Therefore, the aim of this study was to clarify the trends in COVID-19 vaccination intent from pre- to post-COVID-19 vaccine distribution and to identify the association between the 5C psychological antecedents of vaccination and COVID-19 vaccination intent by sex and age in Japan.
Materials and methods
Study sample and data collection
This was a longitudinal study conducted through an Internet-based survey. A baseline survey was conducted on January 14–18, 2021. At the time of the baseline survey, the COVID-19 vaccine had not yet been distributed in Japan, and the number of confirmed COVID-19 cases in Japan had significantly increased; consequently a state of emergency was declared by the Japanese government on January 7, 2021 for the second time since April 2020.24 The study participants were recruited from the registrants of a Japanese Internet research service company called MyVoice Communication, Inc., which had approximately 1.12 million registered persons as of February 2021. We aimed to collect data from 3,000 men and women aged 20–79 years from all regions of Japan. Quota sampling based on age, sex, and residential area was used to ensure that percentage distribution was the same as the results of the national survey in Japan. We stratified the 3,000 participants according to sex, age (five-year age groups), and residential area (i.e., Hokkaido, Tohoku, Kanto, Chubu, Kinki, Chugoku, Shikoku, and Kyushu regions) and set a target number of respondents for each group.
The Internet research service company randomly chose potential respondents from its registrants (n = 13,191) and invited them to participate in the survey by e-mail on January 14, 2021. The questionnaires were placed in a secured section of a website, and potential respondents received a specific uniform resource locator (URL) in their invitation e-mail. When the number of persons who responded to the questionnaire voluntarily reached the target number of respondents for each group, the responses were no longer accepted for that group. The survey was concluded on January 18, 2021, when the target number of respondents was reached for all groups. The company then invited 3,000 respondents from the baseline survey to participate in a second wave survey by e-mail on April 28, 2021. At that time in Japan, the initiation of the COVID-19 vaccine for healthcare workers had started in February, and had been introduced in older adults of the general population in April.20 The number of fully vaccinated persons on the starting date of this study was 995,758, which accounted for approximately 0.8% of the Japanese population.20 On the other hand, the number of confirmed COVID-19 cases in Japan had increased significantly again, and a third state of emergency was declared on April 25, 2021. The questionnaires were placed in a secure section of a website, and potential respondents received a specific URL in their invitation e-mail. The 3,000 respondents to the baseline survey responded to the questionnaire voluntarily, and the response cutoff date was May 6. Reward points valued at 80 yen and 50 yen were provided as incentives for participation in the baseline and second wave survey, respectively (approximately 0.8 and 0.5 US dollars as of January, 2021). This study was approved by the Ethics Committee of Tokyo Medical University, Tokyo, Japan (No: T2019-0234). Informed consent was obtained from all respondents.
Assessment of participants’ COVID-19 vaccination intent
In the baseline survey, at the time when COVID-19 vaccination was not yet started in Japan, we asked the participants to indicate how likely they were to get vaccinated for COVID-19, once a vaccine was available to the public. With reference to a previous study, five response options were provided: very unlikely, somewhat unlikely, somewhat likely, very likely, and unsure.9 At the time of the second survey, COVID-19 vaccine distribution had started in Japan.20 The COVID-19 vaccination program in Japan is designed as such that the public health center contacts the target individuals, and the COVID-19 vaccine is provided for those individuals who wish to receive it.20 Therefore, the participants first responded whether they had received contact from health centers regarding COVID-19 vaccination, and we asked only participants who had not been contacted, to the above questionnaire. We then asked participants who were contacted by health centers whether they planned to be vaccinated or not, to which three options were provided: yes, no, and already vaccinated.
Assessment of 5C psychological antecedents of vaccination
In the second wave survey, we assessed the 5C psychological antecedents of vaccination using a questionnaire based on the 5C scale.14 The 5C scale consists of three subscales for each of the five psychological antecedents, namely, confidence, complacency, constraints (same as convenience in the 3Cs model), calculation, and collective responsibility, for a total of 15 questions.14 The range of values for the possible responses for these items was between 1 and 7. With reference to a previous study, we coded each attitude and belief variable so that higher values indicated greater levels of that construct.14 Although the original 5C scale assesses vaccines in general,14 it is recommended that the wording of the items are modified to make them vaccine-specific when the 5C scale builds the basis of an intervention.25 Therefore, we revised the wording of the original 15 questions to be specific to the COVID-19 vaccine. The survey items were translated into Japanese, which was proofread by a professional editor for translation accuracy. Supplementary Material 1 shows the questions translated from Japanese to English.
Assessment of sociodemographic factors
Participants reported their sex, age, underlying diseases, including heart diseases, respiratory diseases, kidney diseases, diabetes, and hypertension (yes or no), marital status (married or not married), employment status (working or not working), residential area (47 prefectures), and living arrangement (living alone or with others).
The research company provided categorized data on educational attainment (university graduate or above/below) and annual personal income level (less than 2 million yen [approximately 19,000 USD], 2–4 million yen [19,000–38,000 USD], 4–6 million yen [38,000–57,000 USD], 6 million yen or more [57,000 USD or more]).
Statistical analysis
Participants who responded to both the baseline and the second wave surveys and completed all questions were included in the analysis. All analyses were performed according to sex and age (i.e., sex [men and women] and age 20–39, 40–59, 60–79 years old], for a total of six categories). We defined “a participant having COVID-19 vaccination intent” as an individual who met one of the following two criteria: (1) pertaining to the question on how likely they were to get vaccinated for COVID-19, the participant responded “very likely” or “somewhat likely;9 and (2) pertaining to the question on whether they planned to be vaccinated or not, the participant responded “yes” or “already vaccinated.” We clarified the proportion of participants with COVID-19 vaccination intent on the baseline and second wave surveys. The McNemar test was performed to compare the proportion of participants with COVID-19 vaccination intent between the baseline and follow-up surveys.
Regarding the 5C psychological antecedents of vaccination, with recommendations from a previous study, the mean of the three subscales for each psychological antecedent was calculated as the score for psychological antecedents.14 These scores were compared between participants with COVID-19 vaccination intent and those who did not, using the t-test.
Multiple logistic regression analysis was performed to clarify the association between the 5C psychological antecedents and COVID-19 vaccination intent in the second wave survey. The dependent variable was set as a dichotomous variable coded as “1” if the participant had COVID-19 vaccination intent at the time of the second wave survey and “zero” otherwise. The independent variable was the mean score of the five psychological antecedents. All variables were simultaneously placed in the model, and the model was adjusted for educational attainment and annual personal income, which was reported to be associated with vaccination intent in a recent systematic review.4 For the sensitivity analysis, these multiple logistic regression analyses were also performed only among participants who were not contacted by health centers regarding COVID-19 vaccination at the time of the second survey. Statistical analyses were performed using IBM SPSS Statistics for Windows, version 27 (IBM Japan, Tokyo, Japan). Two-sided p-values less than 0.05 were considered statistically significant.
Results
Of the 3,000 respondents in the baseline survey, 345 were excluded for the following reasons: not obtaining valid responses in the follow-up survey (n = 317) and incomplete data provided by the survey company (n = 28). Therefore, the analysis set consisted of 2,655 participants (Table 1). At the time of the second wave survey, compared with the baseline survey, the proportion of participants with COVID-19 vaccination intent had significantly increased from 62.1% to 72.4% among all participants (p value < .001). In all sex and age groups, the proportion of participants with COVID-19 vaccinate intent increased, but no statistically significant difference was found in men in their 20s and 30s (Figure 1).
Table 1.
Participants’ characteristics
| Men |
Women |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 20–39 years |
40–59 years |
60–79 years |
20–39 years |
40–59 years |
60–79 years |
|||||||
| N= 353 | N= 527 | N= 435 | N= 367 | N= 495 | N= 478 | |||||||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |||||||
| Marital status | ||||||||||||
| Married | 90 | (25.5) | 296 | (56.2) | 348 | (80.0) | 127 | (34.6) | 337 | (68.1) | 360 | (75.3) |
| Not married | 263 | (74.5) | 231 | (43.8) | 87 | (20.0) | 240 | (65.4) | 158 | (31.9) | 118 | (24.7) |
| Employment status | ||||||||||||
| Working | 279 | (79.0) | 475 | (90.1) | 222 | (51.0) | 253 | (68.9) | 287 | (58.0) | 103 | (21.5) |
| Not working | 74 | (21.0) | 52 | (9.9) | 213 | (49.0) | 114 | (31.1) | 208 | (42.0) | 375 | (78.5) |
| Residential area | ||||||||||||
| Tokyo metropolitan areaa | 103 | (29.2) | 175 | (33.2) | 134 | (30.8) | 118 | (32.2) | 151 | (30.5) | 155 | (32.4) |
| Other | 250 | (70.8) | 352 | (66.8) | 301 | (69.2) | 249 | (67.8) | 344 | (69.5) | 323 | (67.6) |
| Living arrangement | ||||||||||||
| Alone | 99 | (28.0) | 109 | (20.7) | 61 | (14.0) | 65 | (17.7) | 56 | (11.3) | 83 | (17.4) |
| With others | 254 | (72.0) | 418 | (79.3) | 374 | (86.0) | 302 | (82.3) | 439 | (89.7) | 395 | (82.6) |
| Educational attainment | ||||||||||||
| University graduate or above | 248 | (70.3) | 329 | (62.4) | 284 | (65.3) | 228 | (62.1) | 181 | (36.6) | 118 | (24.7) |
| Below university graduate level | 105 | (29.7) | 198 | (37.6) | 151 | (34.7) | 139 | (37.9) | 314 | (63.4) | 360 | (75.3) |
| Annual personal income | ||||||||||||
| <2 million yen [approximately 19,000 USD] | 123 | (34.8) | 87 | (16.5) | 93 | (21.4) | 210 | (57.2) | 366 | (73.9) | 385 | (80.5) |
| 2-<4 million yen [19,000 -< 38,000] | 96 | (27.2) | 114 | (21.6) | 202 | (46.4) | 114 | (31.1) | 87 | (17.6) | 70 | (14.6) |
| 4-<6 million yen [38,000 -< 57,000] | 92 | (26.1) | 136 | (25.8) | 89 | (20.5) | 28 | (7.6) | 34 | (6.9) | 14 | (2.9) |
| ≥6 million yen or more [57,000-] | 42 | (11.9) | 190 | (36.1) | 51 | (11.7) | 15 | (4.1) | 8 | (1.6) | 9 | (1.9) |
| Underlying diseasesb | ||||||||||||
| Yes | 49 | (13.9) | 143 | (27.1) | 249 | (57.2) | 27 | (7.4) | 92 | (18.6) | 194 | (40.6) |
| No | 304 | (86.1) | 384 | (72.9) | 186 | (42.8) | 340 | (92.6) | 403 | (81.4) | 284 | (59.4) |
aTokyo metropolitan area included Tokyo, Kanagawa, Saitama, and Chiba prefectures.
bUnderlying diseases included heart disease, respiratory disease, kidney disease, diabetes, and hypertension.
Figure 1.
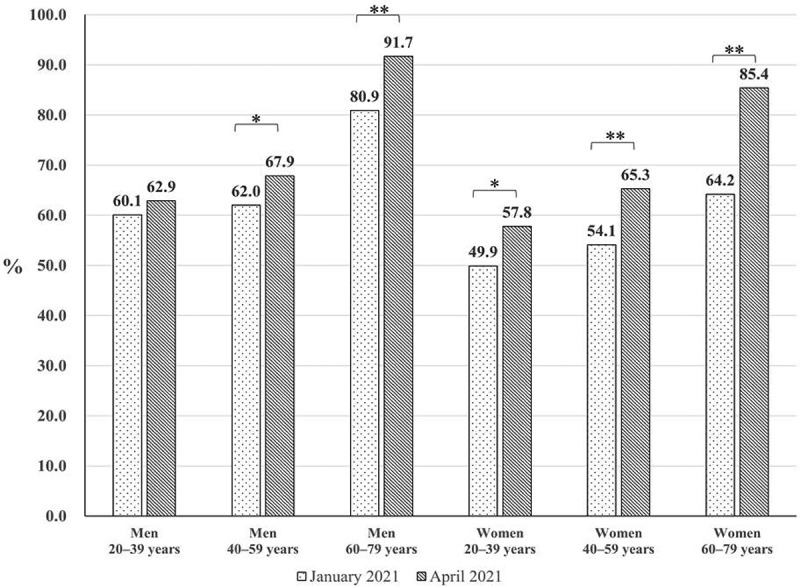
The proportion of participants who had COVID-19 vaccination intent during the baseline (January 2021) and second wave (April 2021) surveys. The McNemar test was performed to compare the prevalence (* p value < .05, ** p value < .001).
Table 2 shows the mean values of the 5C psychological antecedents of vaccination. In all groups, the mean value confidence and collective responsibility was significantly higher, and the mean value complacency and constraints was significantly lower among participants having COVID-19 vaccinate intent, compared with those who did not. In women aged 40–59 years and men aged 60–79 years, the mean value of calculation was significantly lower among participants having COVID-19 vaccinate intent, compared with those without intent.
Table 2.
Mean value of 5C psychological antecedents for age, sex, and vaccination intent
| Total | Participants having COVID-19 vaccination intent a | Participants not having COVID-19 vaccination intent | Total | Participants having COVID-19 vaccination intent | Participants not having COVID-19 vaccination intent | Total | Participants having COVID-19 vaccination intent | Participants not having COVID-19 vaccination intent | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men |
||||||||||||
| 20–39 years |
40–59 years |
60–79 years |
||||||||||
| n | 353 | 222 | 131 | 527 | 358 | 169 | 435 | 399 | 36 | |||
| (%) | (62.9) | (37.1) | (67.9) | (32.1) | (91.7) | (9.3) | ||||||
| Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | ||||
| |
(SD) |
(SD) |
(SD) |
p-value c |
(SD) |
(SD) |
(SD) |
p-value |
(SD) |
(SD) |
(SD) |
p-value |
| Confidence b | 4.42 | 4.81 | 3.77 | <0.001 | 4.32 | 4.73 | 3.46 | <0.001 | 4.95 | 5.05 | 3.85 | <0.001 |
| (1.06) | (0.90) | (0.99) | (1.15) | (0.95) | (1.05) | (0.95) | (0.88) | (0.98) | ||||
| Complacency b | 3.31 | 2.99 | 3.85 | <0.001 | 2.90 | 2.57 | 3.60 | <0.001 | 2.56 | 2.44 | 3.90 | <0.001 |
| (1.34) | (1.39) | (1.08) | (1.25) | (1.16) | (1.16) | (1.19) | (1.11) | (1.19) | ||||
| Constraints b | 3.64 | 3.32 | 4.19 | <0.001 | 3.28 | 3.00 | 3.87 | <0.001 | 2.51 | 2.38 | 3.99 | <0.001 |
| (1.26) | (1.31) | (0.94) | (1.15) | (1.16) | (0.86) | (1.17) | (1.10) | (0.91) | ||||
| Calculation b | 4.70 | 4.73 | 4.66 | 0.478 | 4.75 | 4.77 | 4.71 | 0.574 | 4.83 | 4.78 | 5.37 | 0.002 |
| (0.94) | (0.91) | (0.97) | (1.07) | (1.07) | (1.07) | (1.09) | (1.08) | (1.02) | ||||
| Collective responsibility b | 4.73 | 5.14 | 4.03 | <0.001 | 4.99 | 5.47 | 3.99 | <0.001 | 5.57 | 5.73 | 3.89 | <0.001 |
| |
(1.08) |
(1.06) |
(0.68) |
|
(1.19) |
(1.02) |
(0.86) |
|
(1.07) |
(0.93) |
(1.05) |
|
| Women |
||||||||||||
| 20–39 years |
40–59 years |
60–79 years |
||||||||||
| n | 367 | 212 | 155 | 495 | 323 | 172 | 478 | 408 | 70 | |||
| (%) | (57.8) | (42.2) | (65.3) | (34.7) | (85.4) | (14.6) | ||||||
| Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | Mean | ||||
| |
(SD) |
(SD) |
(SD) |
p-value c |
(SD) |
(SD) |
(SD) |
p-value |
(SD) |
(SD) |
(SD) |
p-value |
| Confidence | 4.20 | 4.68 | 3.55 | <0.001 | 4.34 | 4.70 | 3.66 | <0.001 | 4.87 | 5.06 | 3.70 | <0.001 |
| (1.04) | (0.84) | (0.93) | (1.01) | (0.79) | (1.01) | (0.94) | (0.79) | (0.92) | ||||
| Complacency | 3.16 | 2.95 | 3.44 | <0.001 | 2.98 | 2.64 | 3.61 | <0.001 | 2.62 | 2.43 | 3.70 | <0.001 |
| (1.13) | (1.21) | (0.94) | (1.17) | (1.12) | (1.00) | (1.13) | (1.03) | (1.08) | ||||
| Constraints | 3.52 | 3.28 | 3.84 | <0.001 | 3.27 | 2.96 | 3.85 | <0.001 | 2.63 | 2.43 | 3.80 | <0.001 |
| (1.09) | (1.15) | (0.90) | (1.18) | (1.21) | (0.87) | (1.13) | (1.05) | (0.84) | ||||
| Calculation | 4.84 | 4.88 | 4.78 | 0.368 | 5.01 | 4.89 | 5.23 | <0.001 | 5.07 | 5.05 | 5.18 | 0.310 |
| (1.05) | (1.01) | (1.10) | (0.95) | (0.85) | (1.08) | (0.99) | (0.97) | (1.11) | ||||
| Collective responsibility | 4.77 | 5.27 | 4.09 | <0.001 | 5.00 | 5.51 | 4.05 | <0.001 | 5.54 | 5.80 | 4.01 | <0.001 |
| (1.06) | (0.97) | (0.77) | (1.14) | (0.92) | (0.87) | (1.07) | (0.87) | (0.77) | ||||
SD: standard deviation
aWe defined “a participant having COVID-19 vaccination intent” as meeting one of the following two criteria; 1) pertaining to the question on how likely they were to get vaccinated for COVID-19, the participant responded “very likely” or “somewhat likely, 2) pertaining to the question on whether they planned to be vaccinated or not, the participant responded “yes” or “already vaccinated”.
bAverage of the three subscales.
cp-value was calculated using t test.
Table 3 shows the results of logistic regression analysis. In all groups, high values of confidence and collective responsibility were significant factors for having COVID-19 vaccination intent. In all groups, a high value of calculation was a significant factor for not having COVID-19 vaccinate intent, whereas complacency was not associated with having a COVID-19 vaccination intent in all groups. A high value of constraints was a significant factor for not having COVID-19 vaccination intent among men. The sensitivity analysis showed relatively similar results (Supplementary Material 2).
Table 3.
Individual psychological factors associated with COVID-19 vaccination intent
| Odds ratioa | 95% confidence interval | p-value | Odds ratio | 95% confidence interval | p-value | Odds ratio | 95% confidence interval | p-value | |
|---|---|---|---|---|---|---|---|---|---|
| Men |
|||||||||
| |
20–39 years |
40–59 years |
60–79 years |
||||||
| Confidence | 3.90 | (2.45-6.22) | <0.001 | 3.16 | (2.16-4.61) | <0.001 | 2.47 | (1.21-5.06) | 0.014 |
| Complacency | 0.79 | (0.55-1.12) | 0.187 | 0.83 | (0.59-1.16) | 0.266 | 1.18 | (0.63-2.22) | 0.600 |
| Constraints | 0.66 | (0.44-0.99) | 0.043 | 0.69 | (0.47-1.00) | 0.048 | 0.38 | (0.21-0.71) | 0.002 |
| Calculation | 0.55 | (0.36-0.84) | 0.006 | 0.50 | (0.35-0.70) | <0.001 | 0.24 | (0.12-0.47) | <0.001 |
| Collective responsibility |
3.48 |
(2.02-5.97) |
<0.001 |
4.92 |
(2.90-8.36) |
<0.001 |
7.49 |
(2.81-20.00) |
<0.001 |
| Women |
|||||||||
| |
20–39 years |
40–59 years |
60–79 years |
||||||
| Confidence | 4.53 | (2.69-7.64) | <0.001 | 3.32 | (2.15-5.12) | <0.001 | 4.80 | (2.39-9.63) | <0.001 |
| Complacency | 1.17 | (0.78-1.74) | 0.451 | 0.81 | (0.56-1.16) | 0.249 | 0.71 | (0.40-1.25) | 0.236 |
| Constraints | 0.69 | (0.44-1.08) | 0.100 | 1.10 | (0.76-1.59) | 0.601 | 0.91 | (0.49-1.70) | 0.771 |
| Calculation | 0.41 | (0.27-0.61) | <0.001 | 0.31 | (0.20-0.46) | <0.001 | 0.52 | (0.33-0.83) | 0.006 |
| Collective responsibility | 5.48 | (2.93-10.23) | <0.001 | 8.82 | (5.01-15.51) | <0.001 | 9.09 | (4.24-19.48) | <0.001 |
The dependent variable was set as a dichotomous variable coded as “1” if the participant had COVID-19 vaccination intent in the second wave survey and “zero” otherwise. The independent variable was the mean score of the five psychological antecedents.
All variables were placed in the model simultaneously, and the model was adjusted for educational attainment (university graduate or above/below) and annual personal income (<19,000 USD /19,000–38,000 /38,000–57,000/≥57,000).
Discussion
In this study, we aimed to clarify the trends in COVID-19 vaccination intent from pre- to post-COVID-19 vaccine distribution and to identify the association between the 5C psychological antecedents of vaccination and COVID-19 vaccination intent by sex and age in Japan. Although the proportion of participants with COVID-19 vaccination intent increased on the whole after the start of vaccine distribution in Japan, COVID-19 vaccination intent among young adults remains low. Regarding the association between psychological factors and vaccination intent after the start of vaccine distribution, of the 5C psychological antecedents of vaccination, the results of multiple logistic regression analyses showed a positive association with confidence and collective responsibility (willingness to protect others), and negative association with calculation (engagement in extensive information searching) in all age and sex groups. Constraints (structural and psychological barriers) were negatively associated only among men. We believe findings from this study can be used to plan effective COVID-19 vaccine uptake campaigns among the general public.
Recent systematic reviews have reported that COVID-19 vaccine acceptance is lower in women and younger individuals than in other sex and age groups, respectively.2–4 One systematic review also reported that in addition to these two factors, the COVID−19 vaccination intent was lower in disadvantaged groups, such as those with lower income or education level and those belonging to an ethnic minority group, than in the other groups which may be caused by social inequality.26–28 To achieve high vaccination coverage, it is necessary to clarify the status of psychological factors among high vaccine hesitancy populations and to plan tailored communications.2 Among the sociodemographic factors associated with vaccine hesitancy, sex and age are relatively easier to acquire and target than other sociodemographic factors that may affect vaccination intent. Therefore, we clarified the COVID−19 vaccine acceptance situation, stratified by sex and age. As a result, COVID−19 vaccination intent in post- vaccine distribution improved overall compared to pre-vaccine distribution. However, despite there being some improvement, only a slight increase was found among men in their 20s and 30s, and women in their 20s and 30s, and the percentage of individuals having COVID−19 vaccination intent was still low. Several longitudinal studies in the United States have reported that COVID−19 vaccination intent declined over time from the early phase of the COVID−19 pandemic to late 2020.9,11 A systematic review by Robinson et al., which included 28 large nationally representative studies in 13 countries, also reported that the number of individuals expressing that they will refuse a COVID−19 vaccine have increased over time from March to October 2020.4 These studies reveal trends in COVID−19 vaccination intentions before the vaccine was distributed in Western countries. On the other hand, a recent study in the United States reported that the COVID−19 vaccination intent increased among citizens from September 2020, when the vaccine was not distributed, to December 2020, when it started, although it did not significantly increase among those aged 20–49 years old.29 Our results generally agree with these findings. This may indicate that COVID−19 vaccination intent among ordinary citizens might improve after vaccine distribution, but COVID−19 vaccination intent among young people remains low. To achieve high vaccination coverage, educational campaigns targeting young adults may be of particular importance.
We clarified the association between psychological factors and vaccination intent based on the 5C psychological antecedents of vaccination so that this could be utilized to plan an evidence-informed educational campaign according to age and sex. Confidence and collective responsibility were positively associated with COVID−19 vaccination intent among all age and sex groups. Many previous studies have reported a positive association between perceived safety and effectiveness of the COVID−19 vaccine, which are included in the concept of confidence, and vaccination intent.2,6,7,10,15 However, there are few studies on the association between collective responsibility and COVID−19 vaccination intent.10,16,17 Collective responsibility is defined as the willingness to protect others by one’s own vaccination through herd immunity.14 While people high in collective responsibility are willing to vaccinate in another person’s interest, having low values can indicate that a person does not know about herd immunity, does not care, or does not want to vaccinate for the benefit of others.14 A few previous studies have reported that higher levels of collective responsibility or altruism are associated with higher COVID−19 vaccination intent.10,16,17,18 A systematic review suggested that effective communication of herd immunity may increase general vaccination intent.30 Regarding COVID-19 vaccination, educational campaigns on herd immunity may be effective, as many citizens may not be aware or understand the concept.31
The current study showed that constraints were significantly associated with COVID-19 vaccination intent only among men in multiple logistic regression analyses. Kreps et al. reported that the impact of factors associated with COVID-19 vaccination intent on individual’s decision-making differs by sex in the United States.32 Our results may indicate that Japanese men emphasize vaccination convenience as part of decision-making during post-vaccine distribution, while women do not. In outreach activities to men, it may be important to improve the accessibility of vaccination services. Our results from the multiple logistic regression analyses also showed that complacency was not associated with COVID-19 vaccination intent in all groups. Perceived likelihood of a disease and perceived severity of a disease, which are included in the concept of complacency, are important factors for vaccination intent.5 Many recent studies have also reported an association between complacency and COVID-19 vaccine hesitancy,2,6,7,10,16 but few studies measured all factors of the 5C psychological antecedents.16 Our results may indicate that for the COVID-19 vaccine, which was developed rapidly, perceived safety of the vaccine and thoughts about collective responsibility were more important factors in vaccination intent than perceived risk of the disease in Japan at the time of post-COVID-19 vaccine distribution.
Kwok et al. reported that in March 2020, during the early phase of the COVID-19 pandemic, they evaluated the association between the 5C psychological antecedents of vaccination and COVID-19 vaccination intent in nurses and found that more confidence, less complacency, and more collective responsibility were positively associated with intent, whereas constrains and calculation were not associated with intent.16 On the other hand, the present study shows that high calculation was associated with low COVID-19 vaccination intent. This may mean that individuals who are enthusiastic about collecting information have a lower COVID-19 vaccination intent. Under ordinary circumstances, it is assumed that individuals high in calculation evaluate the risks of infection and vaccination to derive a good decision.14 However, the Internet provides anti-vaccination activists with an opportunity to spread their message,33 and anti-vaccination contents on the Internet includes words that are consumer-orientated.34 Therefore, it is likely that the more people search for information about vaccines, the more critical information about vaccines they will find.35 Regarding COVID-19 infections and vaccines, misleading information and misinformation are spread in various media, especially social media.36 Previous studies conducted in Western countries reported that susceptibility to misinformation is associated with a lower likelihood of getting vaccinated for COVID-19.37 Our results may imply that increased exposure to misinformation as a result of individuals’ engagement in extensive information searching may have reduced the willingness of those susceptible to misinformation to be vaccinated. Therefore, providing correct information using consumer-friendly messages on various media platforms, including participatory Internet platforms, and increasing opportunities for ordinary citizens to interact with pro-vaccine information may be necessary.
The strengths of our study include the large sample size and the selection of participants from all regions of Japan using quota sampling. However, the limitations of this study must be considered. First, participants were recruited from a single Internet research company, and these results may have been affected by selection bias. Second, although the original 5C scale referred to in this study is a validated questionnaire, which also provides guidance on how to adapt the 5C scale in another language,14,25 we lacked time for preparation and therefore were unable to follow this guidance completely. Third, although there was a negative association between calculation on the 5C psychological antecedents and COVID-19 vaccination intent in this study, calculation is thought to be associated with a deliberative cognitive style of decision making.14 It is possible that a deliberative cognitive style of decision-making lead to avoidance of the new and rapidly developed COVID-19 vaccine, but this point was unclear in this study. Fourth, in this study, the 5C psychological antecedents of vaccination were not measured at the baseline survey. As with vaccination intent, the 5C psychological antecedents of vaccination may have changed from pre- to post-COVID-19 vaccine distribution, and these changes may have influenced the vaccination intent in the second wave survey. Fifth, our results did not clarify the reason why COVID-19 vaccination intent differs by sex and age in Japan, since the main purpose of our study was to reveal the trends in COVID-19 vaccination intent from pre- to post-COVID-19 vaccine distribution and to identify the association between the 5C psychological antecedents of vaccination and COVID-19 vaccination intent by sex and age. Future research may be needed to clarify the association between sociodemographic factors, such as sex, age, educational level, income level, and race, and psychological factors related to vaccination intent. Despite these limitations, to the best of our knowledge, this study is one of the first studies to clarify the trends in COVID-19 vaccination intent from pre- to post-COVID-19 vaccine distribution and to identify the association between the 5C psychological antecedents of vaccination and COVID-19 vaccination intent in Japan.
In conclusion, the vaccination intent among ordinary citizens in Japan increased after vaccine distribution, but improvement was poor among young men. COVID-19 vaccination intent may be affected not only by confidence and constraints but also by calculation and collective responsibility among all generations. Further research on COVID-19 vaccination intent focusing on the 5C psychological antecedents and COVID-19 vaccination intent may be needed.
Supplementary Material
Acknowledgments
We would like to express our sincere gratitude to all the participants who enrolled in this study.
Funding Statement
This research was supported by the Tokyo Medical University Research Grant [2021].
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
SUPPLEMENTAL DATA
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2021.1968217.
References
- 1.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A.. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–28. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin C, Tu P, Beitsch LM.. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines. 2021;9:16. doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021;39(15):2024–34. doi: 10.1016/j.vaccine.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–64. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 6.Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38(42):6500–07. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38(45):7002–06. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, Fang H. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines (Basel). 2020;8(3):482. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Szilagyi PG, Thomas K, Shah MD, Vizueta N, Cui Y, Vangala S, Kapteyn A. National trends in the US public’s likelihood of getting a COVID-19 vaccine—April 1 to December 8, 2020. JAMA. 2021;325(4):396–98. doi: 10.1001/jama.2020.26419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Machida M, Nakamura I, Kojima T, Saito R, Nakaya T, Hanibuchi T, Takamiya T, Odagiri Y, Fukushima N, Kikuchi H, et al. Acceptance of a COVID-19 vaccine in Japan during the COVID-19 pandemic. Vaccines. 2021;9(3):210. doi: 10.3390/vaccines9030210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daly M, Robinson E. Willingness to vaccinate against COVID-19 in the U.S.: representative longitudinal evidence from April to October 2020. Am J Prev Med. 2021;60(6):766–73. doi: 10.1016/j.amepre.2021.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Parental vaccine safety concerns in 2009. Pediatrics. 2010;125(4):654–59. doi: 10.1542/peds.2009-1962. [DOI] [PubMed] [Google Scholar]
- 13.Bish A, Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol. 2010;15(4):797–824. doi: 10.1348/135910710X485826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Bohm R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018;13:e0208601. doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leng A, Maitland E, Wang S, Nicholas S, Liu R, Wang J. Individual preferences for COVID-19 vaccination in China. Vaccine. 2021;39(2):247–54. doi: 10.1016/j.vaccine.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwok KO, Li -K-K, Wei WI, Tang A, Wong SYS, Lee SS. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. 2021;114:103854. doi: 10.1016/j.ijnurstu.2020.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Head KJ, Kasting ML, Sturm LA, Hartsock JA, Zimet GD. A national survey assessing SARS-CoV-2 vaccination intentions: implications for future public health communication efforts. Sci Commun. 2020:1075547020960463. doi: 10.1177/1075547020960463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210–e21. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Betsch C, Rossmann C, Pletz MW, Vollmar HC, Freytag A, Wichmann O, Hanke R, Hanke W, Heinemeier D, Schmid P, et al. Increasing influenza and pneumococcal vaccine uptake in the elderly: study protocol for the multi-methods prospective intervention study Vaccination60+. BMC Public Health. 2018;18(1):885. doi: 10.1186/s12889-018-5787-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prime minister of Japan and his cabinet . Novel coronavirus vaccines. [accessed 24 May 2021] https://japan.kantei.go.jp/ongoingtopics/vaccine.html.
- 21.de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396(10255):898–908. doi: 10.1016/S0140-6736(20)31558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simms KT, Hanley SJB, Smith MA, Keane A, Canfell K. Impact of HPV vaccine hesitancy on cervical cancer in Japan: a modelling study. Lancet Public Health. 2020;5(4):e223–e34. doi: 10.1016/S2468-2667(20)30010-4. [DOI] [PubMed] [Google Scholar]
- 23.Yoda T, Katsuyama H. Willingness to receive COVID-19 Vaccination in Japan. Vaccines. 2021;9(1):48. doi: 10.3390/vaccines9010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prime minister of Japan and his cabinet . Press conference by the prime minister. [accessed 24 May 2021] https://japan.kantei.go.jp/99_suga/statement/202101/_00005.html.
- 25.Betsch C, Bach Habersaat K, Deshevoi S, Heinemeier D, Briko N, Kostenko N, Kocik J, Böhm R, Zettler I, Wiysonge CS, et al. Sample study protocol for adapting and translating the 5C scale to assess the psychological antecedents of vaccination. BMJ Open. 2020;10(3):e034869. doi: 10.1136/bmjopen-2019-034869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Galarce EM, Minsky S, Viswanath K. Socioeconomic status, demographics, beliefs and A(H1N1) vaccine uptake in the United States. Vaccine. 2011;29(32):5284–89. doi: 10.1016/j.vaccine.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 27.Endrich MM, Blank PR, Szucs TD. Influenza vaccination uptake and socioeconomic determinants in 11 European countries. Vaccine. 2009;27(30):4018–24. doi: 10.1016/j.vaccine.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 28.Corbie-Smith G. Vaccine hesitancy is a scapegoat for structural racism. JAMA Health Forum. 2021;2(3):e210434. doi: 10.1001/jamahealthforum.2021.0434. [DOI] [PubMed] [Google Scholar]
- 29.Nguyen KH, Srivastav A, Razzaghi H, Williams W, Lindley MC, Jorgensen C, Abad N, Singleton JA. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination — United States, September and December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(6):217–22. doi: 10.15585/mmwr.mm7006e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hakim H, Provencher T, Chambers CT, Driedger SM, Dube E, Gavaruzzi T, Giguere AMC, Ivers NM, MacDonald S, Paquette J-S, et al. Interventions to help people understand community immunity: a systematic review. Vaccine. 2019;37(2):235–47. doi: 10.1016/j.vaccine.2018.11.016. [DOI] [PubMed] [Google Scholar]
- 31.Korn L, Böhm R, Betsch C. Reply to Rabb et al.: Why promoting COVID-19 vaccines with community immunity is not a good strategy (yet). Proc Natl Acad Sci. 2021;118(14):e2102054118. doi: 10.1073/pnas.2102054118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kreps SE, Kriner DL. Factors influencing Covid-19 vaccine acceptance across subgroups in the United States: evidence from a Conjoint experiment. Vaccine. 2021;39(24):3250–58. doi: 10.1016/j.vaccine.2021.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kata A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm – an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine. 2012;30(25):3778–89. doi: 10.1016/j.vaccine.2011.11.112. [DOI] [PubMed] [Google Scholar]
- 34.Yiannakoulias N, Slavik CE, Chase M. Expressions of pro- and anti-vaccine sentiment on YouTube. Vaccine. 2019;37(15):2057–64. doi: 10.1016/j.vaccine.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 35.Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9:1763–73. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van Der Linden S, Roozenbeek J, Compton J. Inoculating against fake news about COVID-19. Front Psychol. 2020;11:566790. doi: 10.3389/fpsyg.2020.566790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roozenbeek J, Schneider CR, Dryhurst S, Kerr J, Freeman ALJ, Recchia G, van der Bles AM, Van Der Linden S. Susceptibility to misinformation about COVID-19 around the world. R Soc Open Sci. 2020;7(10):201199. doi: 10.1098/rsos.201199. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


