ABSTRACT
Background
In response to the coronavirus disease 2019 (COVID-19) pandemic, many countries have implemented mitigating non-pharmaceutical interventions. We investigated the impact of these interventions and changes in public behavior on the incidences of selected vaccine-preventable diseases (VPDs) during the COVID-19 pandemic in the eastern of China.
Methods
From routine monitoring data collected in the capital of eastern China’s Jiangsu Province, we extracted and analyzed the incidences of influenza; hand, foot and mouth disease (HFMD); varicella; mumps; pertussis; and hepatitis B. We also investigated the changes in public behavior during the COVID-19 pandemic through telephone interviews and questionnaire surveys.
Results
Compared with the baseline (2017–2019), the incidences of all VPDs except influenza declined significantly in 2020 (HFMD decreased by 79.92%, varicella decreased by 7.71%, mumps decreased by 2.03%, pertussis decreased by 78.91%, and hepatitis B decreased by 0.31%). The reduction in reported cases in children (0–14 years) was greater than that in adults, and pertussis had the largest reduction (approximately 80%) in children. Influenza peaks in winter; in the three years before the COVID-19 pandemic, Influenza rates took an average of 10 weeks to recede to their lowest levels after the Spring Festival, while in 2020, this took only 1 week. A total of 366 outbreaks with 20,205 cases were reported during the COVID-19 pandemic. Among the participants in the study, 94.2% of the interviewees avoided going to high-risk areas, 82.4% avoided going to crowded places, 92.9% wore masks when going out,88.4% washed their hands frequently, and 67.9% maintained social distance.
Conclusions
Our study showed significant reductions in the incidences of VPDs after the implementation of a series of non-pharmaceutical interventions during the COVID-19 pandemic.
KEYWORDS: COVID-19, novel coronavirus, social distancing, wearing masks, incidence
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has spread all over the world, and it has imposed a substantial health burden. To date (May 14, 2021), Jiangsu Province has successfully controlled COVID-19, with only 721 confirmed cases recorded. Vaccination is still the most effective way to prevent disease, but in the absence of a vaccine and effective drugs, a series of non-pharmaceutical measures taken by the Chinese government became vital. These included the cancellation of all public transportation, the prohibition of all public gatherings, and the requirement for all residents to stay at home. When they go out to places where people gathered, please wear medical surgical masks, and maintain social distance. During the epidemic, schools and factories were in the suspension stage. When the epidemic is controlled, we were returning to work and school, medical surgical masks were required and health registrations were required every day. Generally, residents must show their health codes and wear medical surgical masks when taking public transportation, otherwise they will be prohibited from getting on the bus. Residents who violate the provisions of the Law on Prevention and Control of Infectious Diseases, will be punished accordingly. With increasing evidence that wearing masks, washing hands, and practicing social distancing are effective at mitigating the spread of COVID-19, these measures are currently the best ways to protect ourselves and our society from this dangerous disease.1–3 These measures are actually not uncommon; in past influenza epidemics, they were used to curb human-to-human transmission and thereby reduce morbidity and mortality to a certain extent. The population of Jiangsu Province were aware of the impact of the pandemic and adhere to the national guidelines established to reduce the spread of the virus, which has been a key factor in the province’s success in controlling the spread of COVID-19. These traditional infection control practices, including wearing masks, washing hands, and maintaining social distance, are widely accepted and adopted in Jiangsu Province. We also observed that the number of cases of VPDs decreased significantly during the COVID-19 pandemic.
China is located in the Northern Hemisphere, and Jiangsu Province is located in the eastern part of mainland China. It has four distinct seasons, and it is one of the most densely populated provinces in China. We speculated that the changes in individual behavior due to the implementation of control and prevention strategies during the COVID-19 pandemic may have led to the reductions in the incidences of VPDs among Jiangsu residents. Therefore, we investigated the impact of non-pharmaceutical interventions on the incidences of VPDs in Jiangsu Province during the COVID-19 pandemic with the aid of data from the National Notifiable Disease Reporting System (NNDRS).
2. Material and methods
2.1. Study design and database
The numbers of cases and incidence rates of VPDs each year were obtained from the NNDRS. It is a nationwide database that provides epidemiological data on VPDs (hepatitis B, measles, rubella, mumps, varicella, pertussis, hand-foot-mouth disease [HFMD], influenza,etc.). Measles and rubella were not included in this analysis due to their low incidences in China since the implementation of the measles elimination program. We downloaded epidemiological data pertaining to VPDs from November 1, 2016, to December 31, 2020, from the NNDRS. We estimated the baseline weekly average incidences of the relevant VPDs from 2017 to 2019, and then we assessed the differences between those baseline values and the weekly incidences of the same VPDs in 2020.
We conducted a cross-sectional questionnaire and telephone survey among parents of children in Jiangsu Province from May 1st to 3rd, 2020. Volunteers for the telephone survey were recruited through random number dialing. Under normal circumstances, only one adult over 18 years old in a family will accept the questionnaire survey. However, in the offline electronic questionnaire survey, occasionally two family members will bring their children to the vaccination site together for vaccination. In this case, the two people will be investigated at the same time, but the proportion is very low.The questionnaire survey was mainly distributed by researchers through a WeChat mini-program. At the same time, each respondent was accompanied by a researcher who was only responsible for explaining the questions and did not express personal views on the questions. When we conducted the survey, it has been stated in the survey notice that only when the respondents completed the survey could they be rewarded with 5 yuan. The questionnaire and telephone survey items assessed the participants’ perception of risks related to COVID-19 and VPDs as well as the behavioral measures that they implemented to prevent disease transmission, including wearing masks, washing hands, practicing social distancing, etc.All the volunteers received unified training before the survey and could participate in the survey only after passing the training. Most of the volunteers were medical staff at the vaccination sites.
2.2. Key time point
The Spring Festival is an important event in China. It starts on New Year’s Eve and lasts for seven days. During the week-long holiday, most Chinese spend time with their families. On January 25, 2020, which was the start of the Spring Festival holiday, the Chinese government established a working group focused on the prevention and control of COVID-19. Therefore, we chose the Chinese New Years in 2017–2019 as the key time points (11 weeks before and 39 weeks after the key time point).
2.3. Statistical analysis
We used Excel 2010 to plot the monthly incidences based on the reported cases, and the data with 95% confidence intervals were analyzed by SPSS 22.0 (IBM, Armonk, New York, USA).
2.4. Ethical clearance
This study was approved by the Medical Ethics Committee of Jiangsu of the Jiangsu Provincial Center for Disease Control and Prevention (CDC),and all the participants gave verbal informed consent.The ethics committee reviews the privacy protection of the subjects during the entire research process. In addition, the questionnaire does not contain individual private information. At the same time, the subject numbers were used as the only identifiable information, and only allowed the researcher to contact and analyze the entire data.
3. Result
3.1. The incidence of VPD
The following six infectious diseases were included in our analysis: influenza, HFMD, varicella, mumps, pertussis, and hepatitis B. In total, 80,108 cases of influenza, 27,477 cases of HFMD, 92,891 cases of varicella, 8,998 cases of mumps, 31 cases of pertussis, and 14,021 cases of hepatitis B were reported between November 2019 and October 2020. Compared with the baseline (2017–2019), the incidences of all the VPDs except influenza declined significantly (HFMD decreased by 79.92%, varicella by 7.71%, mumps by 2.03%, pertussis by 78.91%, and hepatitis B by 0.31%)(see Table 2). The incidences of influenza, HFMD, varicella, mumps, pertussis, and hepatitis B from 11 weeks before to 39 weeks after the Chinese New Year in 2020 are shown in Figure 1. In the three years before the outbreak of COVID-19, the average numbers of reported cases of HFMD, varicella, mumps, pertussis, and hepatitis B began to decline 11 weeks before the Chinese New Year, but the numbers of reported cases rebounded rapidly after the Chinese New Year, with the incidences of the five diseases reaching the previous levels in 5–15 weeks.However, in 2020, when preventive public health interventions had been implemented, it took approximately 15–30 weeks for the numbers of reported cases to return to their original levels.In addition, the results showed an increase of 297.32% compared with the baseline, as influenza is a clearly seasonal disease that has a peak incidence at approximately the time of the Chinese New Year. In the three years before the COVID-19 pandemic, it took an average of 10 weeks for the incidence of influenza to recede to the lowest level after the Spring Festival, while in 2020, this occurred in only 1 week.
Table 2.
The incidences of all VPDsduring the study period (11 weeks before and 39 weeks after Chinese Spring Festival)
| Disease | 2017 N (/100,000) | 2018 N (/100,000) | 2019 N (/100,000) | Baseline (2017–2019) N (/100,000) | 2020 N (/100,000) |
|---|---|---|---|---|---|
| influenza | 6869 (8.59) | 15,991(19.99) | 37,625(47.03) | 20,162 (25.20) | 80,108(100.14) |
| HFMD | 105,594(131.99) | 186,255(232.82) | 118,676(148.35) | 136,842 (171.05) | 27,477(34.35) |
| varicella | 51,143(63.93) | 101,184(126.48) | 149,627(187.03) | 100,651 (125.81) | 92,891(116.11) |
| mumps | 5760(7.20) | 7309(9.14) | 14,482(18.10) | 9184 (11.48) | 8998(11.25) |
| pertussis | 57(0.07) | 123(0.15) | 261(0.33) | 147 (0.18) | 31(0.04) |
| hepatitis B | 13,791(17.24) | 13,800(17.25) | 14,603(18.25) | 14,065 (17.58) | 14,021(17.53) |
Figure 1.
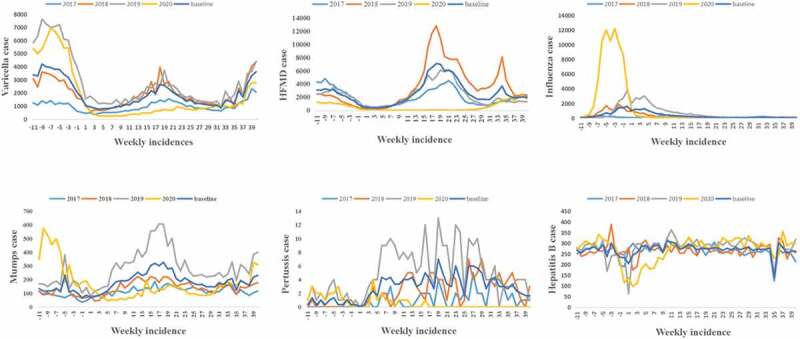
Weekly reported cases of VPD from NNDRS.We estimated the baseline weekly average incidences of the relevant VPDs from 2017 to 2019, and assessed the differences between those baseline values and the weekly incidences of the same VPDs in 2020. Meanwhile, we chose Chinese New Year in 2017–2019 as the key time point (11 weeks before and 39 weeks after the key time point).
3.2. The age distribution of VPD
Table 1 summarizes the age distributions across the six types of VPDs from week 11 to week 39 of the next year (2017–2020). The majority of patients with HFMD and pertussis were 0–4 years old, while most patients with varicella and mumps were between ages 5 and 14. The reduction in reported cases in children (0–14 years) was greater than that in adults, and pertussis had the largest reduction (approximately 80%) in children.
Table 1.
Age distribution of people with VPD during the study period (11 weeks before and 39 weeks after Chinese Spring Festival)
| Disease | Year |
||||
|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | Baseline (2017–2019) | 2020 | |
| Influenza, N | 6869 | 15,991 | 37,625 | 20,162 | 80,108 |
| 0–4 years,n(%) | 1512(22.01) | 3872(24.21) | 10,437(27.74) | 5274(26.16) | 17,080(21.32) |
| 5–14 years,n(%) | 3038(44.23) | 7379(46.14) | 12,255(32.57) | 7557 (37.48) | 43,082(53.78) |
| 15–24 years,n(%) | 475(6.92) | 833(5.21) | 2582(6.86) | 1297 (6.43) | 4978(6.21) |
| ≥25 years,n(%) | 1844(26.85) | 3907(24.43) | 12,351(32.83) | 6034 (29.93) | 14,968(18.68) |
| HFMD, N | 105,594 | 186,255 | 118,676 | 136,842 | 27,477 |
| 0–4 years,n(%) | 86,808(82.21) | 155,505(83.49) | 92,763(78.16) | 111,692 (81.62) | 23,254(84.63) |
| 5–14 years,n(%) | 18,296(17.33) | 29,362(15.76) | 25,155(21.20) | 24,271 (17.74) | 3923(14.28) |
| 15–24 years,n(%) | 153(0.14) | 408(0.22) | 230(0.19) | 264 (0.19) | 101(0.37) |
| ≥25 years,n(%) | 337(0.32) | 980(0.53) | 528(0.44) | 615(0.45) | 199(0.72) |
| varicella, N | 51,143 | 101,184 | 149,627 | 100,651 | 92,891 |
| 0–4 years,n(%) | 10,571(20.67) | 21,672(21.42) | 32,143(21.48) | 21,462 (21.32) | 13,824(18.30) |
| 5–14 years,n(%) | 27,997(54.74) | 54,790(54.15) | 82,766(55.31) | 55,184 (54.83) | 53,564(55.95) |
| 15–24 years,n(%) | 5726(11.20) | 10,803(10.68) | 14,826(9.91) | 10,452 (10.38) | 12,537(12.18) |
| ≥25 years,n(%) | 6849(13.39) | 13,919(13.76) | 19,892(13.29) | 13,553 (13.47) | 12,966(13.57) |
| mumps, N | 5760 | 7309 | 14,482 | 9184 | 8998 |
| 0–4 years,n(%) | 1291(22.41) | 1481(20.26) | 1774(12.25) | 1515 (16.50) | 1397(15.52) |
| 5–14 years,n(%) | 3571(62.00) | 4940(67.59) | 10,538(72.77) | 6350 (69.14) | 6316(70.19) |
| 15–24 years,n(%) | 336(5.83) | 373(5.10) | 1261(8.71) | 657 (7.15) | 660(7.33) |
| ≥25 years,n(%) | 562(9.76) | 515(7.05) | 909(6.28) | 662(7.21) | 625(6.96) |
| pertussis, N | 57 | 123 | 261 | 147 | 31 |
| 0–4 years,n(%) | 55(96.49) | 119(96.75) | 246(94.25) | 140 (95.24) | 27(87.10) |
| 5–14 years,n(%) | 2(3.51) | 4(3.25) | 13(4.98) | 6 (4.08) | 3(9.68) |
| 15–24 years,n(%) | 0(0.00) | 0(0.00) | 0(0.00) | 0 (0.00) | 0(0.00) |
| ≥25 years,n(%) | 0(0.00) | 0(0.00) | 2(0.77) | 1 (0.68) | 1(3.22) |
| hepatitis B, N | 13,791 | 13,800 | 14,603 | 14,065 | 14,021 |
| 0–4 years,n(%) | 30(0.22) | 28(0.20) | 35(0.24) | 31 (0.22) | 25(0.18) |
| 5–14 years,n(%) | 52(0.38) | 43(0.31) | 49(0.34) | 48 (0.34) | 40(0.29) |
| 15–24 years,n(%) | 654(4.74) | 569(4.12) | 496(3.40) | 573(4.07) | 502(3.58) |
| ≥25 years,n(%) | 13,055(94.66) | 13,160(95.36) | 14,023(96.03) | 13,413 (95.37) | 13,454(95.96) |
3.3. The outbreak of VPD
A total of 366 outbreaks with 20,205 cases were reported during the COVID-19 pandemic (2020). Compared with 2019, the number of outbreaks decreased from 414to 366, a decrease of 11.59%. Except for influenza, the number of outbreak-related cases decreased significantly, HFMD decreased by 89.24%, varicella decreased by 14.91% and mumps decreased by 46.20% (Table 3).
Table 3.
No. Of VPD outbreaks and outbreak-related cases during the study period (11 weeks before and 39 weeks afterChinese Spring Festival)
| No. of outbreaks (%) |
No. of outbreak-related cases (%) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Year | Influenza | HFMD | varicella | mumps | Total | Influenza | HFMD | varicella | mumps | Total |
| 2017 | 21(16.0) | 13(9.9) | 93(71.0) | 4(3.1) | 131(100.0) | 1010(26.7) | 314(8.3) | 2301(60.7) | 163(4.3) | 3788(100.0) |
| 2018 | 67(19.1) | 50(14.2) | 230(65.5) | 4(1.1) | 351(100.0) | 4109(33.6) | 1328(10.9) | 6612(54.1) | 184(1.5) | 12,233(100.0) |
| 2019 | 37(8.9) | 63(15.2) | 283(68.4) | 31(7.5) | 414(100.0) | 2156(14.4) | 1348(9.0) | 9225(61.8) | 2195(14.7) | 14,924(100.0) |
| 2020 | 127(34.7) | 7(1.9) | 213(58.2) | 19(5.2) | 366(100.0) | 11,029(54.6) | 145(0.7) | 7850(38.9) | 1181(5.8) | 20,205(100.0) |
3.4. Risk perception and behavioral responses
We selected a county with a population of 400,000 (Jingkou District, Zhenjiang City), and surveyed a total of 1050 people, accounting for 0.26% of the total population. A total of 550 people completed the electronic questionnaire (80% response rate) and 500 people participated in the telephone interviews (71% response rate). There were 502 males and 548 females, with an average age of 44.7 years. We found that respondents perceived the risk of COVID-19 to be much higher than that of VPDs.However, in response to the threat of COVID-19, their use of preventive measures increased significantly.The results showed that 94.2% of the interviewees avoided going to high-risk areas, 82.4% avoided going to crowded places, 75.2% avoided contact with people with respiratory symptoms,70.5% avoided visiting medical facilities,92.9% wore masks when going out,88.4% washed their hands frequently, and 67.9% maintained social distance (Table 4).
Table 4.
Risk perceptions and behavioral responses toward COVID-19 and VPD
| Questionnaire survey (550) (%; 95% CI) | Telephone survey (500) (%; 95% CI) | Total (%; 95% CI) | |
|---|---|---|---|
| Risk perception of COVID-19 | |||
| Perceived susceptibility to COVID-19 | 355 (64.5%; 60.4–68.5) | 270 (54.0%; 49.5–58.4) | 625 (59.5%; 56.5–62.5) |
| Perceived severity of COVID-19 | 500 (90.9%; 88.1–93.1) | 443 (88.6%; 85.4–91.2) | 943 (89.8%; 87.8–91.5) |
| Risk perception of VPD | |||
| Perceived susceptibility to VPD | 221 (40.2%; 36.1–44.4) | 179 (35.8%; 31.6–40.2) | 400 (38.1%; 35.2–41.1) |
| Perceived severity of VPD | 178 (32.4%; 28.5–36.5) | 202 (40.4%; 36.1–44.9) | 380 (36.2%; 33.3–39.2) |
| Preventive measures taken against COVID-19 and VPD | |||
| avoided going to crowded places | 425 (77.3%; 73.5–80.7) | 440 (88.0%; 84.8–90.7) | 865 (82.4%; 79.9–84.6) |
| avoided going to high risk areas* | 512 (93.1%; 90.6–95.0) | 477 (95.4%; 93.1–97.0) | 989 (94.2%; 92.6–95.5) |
| avoided contacting with people with respiratory symptoms | 387 (70.3%; 66.3–74.1) | 402 (80.4%; 76.6–83.7) | 789 (75.2%; 72.4–77.7) |
| avoided visiting medical institutions | 351 (63.8%; 59.6–67.8) | 389 (77.8%; 73.9–81.3) | 740 (70.5%; 67.6–73.2) |
| wearing masks | 502 (91.3%; 88.5–93.4) | 473 (94.6%; 92.1–96.3) | 975 (92.9%; 91.1–94.3) |
| washing hands | 440 (80.0%; 76.4–83.2) | 488 (97.6%; 95.7–98.7) | 928 (88.4%; 86.3–90.2) |
| social distancing | 335 (60.9%; 56.7–64.9) | 378 (75.6%; 71.6–79.3) | 713(67.9%; 64.9–70.7) |
*High risk areas: the cumulative number of cases exceeds 50, and cluster outbreaks occurred within 14 days.
4. Discussion
Figure 1 shows that in the three before the COVID-19 pandemic, the average numbers of reported cases of HFMD, varicella, mumps, pertussis, and hepatitis B decreased in the 11 weeks before the Chinese New Year, but they rebounded rapidly after the Chinese New Year. The main reason is that face-to-face contact is greatly reduced with the students’ holidays. Since the beginning of the COVID-19 pandemic, government authorities have implemented aggressive outbreak control measures; at the same time, reductions in the incidences of VPDs have been observed.Similar studies have recently been published in the US,4,5 where both hospitalizations for respiratory diseases and respiratory disease incidence rates have declined after the implementation of some strict measures. The results from other studies also showed reductions in the incidence of influenza after such measures were implemented.6–8There are many factors that influence morbidity, such as age, sex, maintenance of social distance, mask-wearing behavior, and the frequency of hand washing, and it is difficult to determine the effectiveness of these factors. However, the number of confirmed cases of COVID-19 in Jiangsu Province is relatively low. We believe that the range of non-pharmaceutical interventions not only controlled the spread of COVID-19 but also had a positive effect on the transmission of VPDs and that further research is needed to investigate the independent and combined effects of these measures. Other interventions may also help contain the epidemic, and further research is needed to clarify the effects of each intervention.
However, the incidence of influenza in 2020 was higher than in the three years before COVID-19. This was mainly because influenza is concentrated from November of one year to January of the next year in the Northern Hemisphere.9,10At that time, strict interventions had not yet been implemented in Jiangsu Province,11,12 and new test method (colloidal gold) has been adopted for national influenza surveillance since the end of 2019, greatly improving the detection sensitivity.13,14 Figure 1 shows the incidence of influenza in the 11 weeks before the Chinese New Year. It also shows that in the first week after the Chinese Lunar New Year, influenza cases in Jiangsu Province had dropped to the lowest level of all the years considered. Recent studies in Taiwan also showed a sharp drop in the incidence of influenza after the Chinese Lunar New Year.6
We also found that the degree of reduction in the incidences of VPDs was related to age, and the reductions in reported cases among children were greater than those in adults. The incidence of pertussis among children aged 0–14 in 2020 dropped by approximately 80% compared with the baseline level, which was similar to the reduction reported in a South Korean study.15 This may be because the implementation of non-pharmaceutical interventions among children is stronger than that among adults, and children are more compliant. Adults still need to work on site, and the resumption of schools has been postponed until the end of May, and the order of resumption is first high school, then middle school, and finally primary school and kindergarten.
The results of our questionnaire survey indicated that the participants perceived the risk of COVID-19 to be greater than that of VPDs (Table 3),and 82.4% of the participants avoided going to crowded places,94.2% avoided going to high-risk areas, and 92.9% of people wore masks when going out or in public places. A similar survey was conducted in Hong Kong, in which 99% of the respondents reported wearing masks during the COVID-19 pandemic in 2020,16 while only 10% reported wearing masks during the influenza epidemic in 2009.17 Our results also showed that 70.5% of the participants avoided visiting health care facilities. It is worth noting that fewer people maintained social distancing (67.9%) compared to higher reported avoiding crowded places. People of different nationalities and cultures have different spatial regions. Most English-speaking people will keep a certain distance when talking, while Asians, due to cultural reasons, seem to be unfriendly if they were too far away from each other, social distance was not highly compliant in China. Avoiding crowded places, which can effectively prevent the spread of the virus. This aspect does not involve Chinese culture, so compliance was better. Our results also showed that 70.5% of the participants avoided visiting health care facilities, the main reason is that this can reduce cross-infection in medical institutions, and at the same time cause the infection to be undiagnosed These behavioral changes indicate the level of people’s concern about COVID-19, but the cumulative effect of these changes in personal behavior requires further research to verify.
Nevertheless, we also observed that the incidences of VPDs had returned to nearly baseline levels 30 weeks after the end of the Chinese New Year, mainly because the COVID-19 outbreak was under control in China, and engagement in behaviors such social distancing, masking, frequent hand washing, etc. was less common, possibly also indicating some fatigue regarding the maintenance of these measures. Another reason for this phenomenon may be that as schools resumed classes, students were again exposed to their normal environments again.15,16Studies have suggested that the lack of immune stimulation due to reduced exposure to viruses or bacteria, as well as reduced vaccination, may have adverse consequences when these interventions are withdrawn in the late stages of epidemic control.This is mainly due to an increase in the proportion of “susceptible people” and a decline in herd immunity.
Our study also has some limitations. First, information was collected from passive surveillance that is likely to be incomplete; Second, during the COVID-19 epidemic, the decreases in the incidences of VPDs may be related to the reluctance to seek medical treatment, leading to reporting bias.Third, randomized controlled trials were not available, so the independent effects of each measure could not be assessed.Fourth, our survey respondents were parents of children who had attended vaccination clinics, possibly leading to selection bias and response bias. Fifth, in the survey, we used red envelopes as small gifts, which may have a selection bias on the results. Before the survey, we did not inform participants that there will be a red envelope reward for completing the survey, because this red envelope reward is randomly and automatically generated by the WeChat applet, rather than artificially set, and this had limited impact on the participation of people at different levels.
In conclusion, our study showed significant reductions in the incidences of VPDs after the implementation of a series of non-pharmaceutical interventions during the COVID-19 pandemic.In addition, with effective control of the domestic COVID-19 epidemic and continued implementation of non-pharmaceutical interventions, further research is needed to determine whether this related downward trend will continue.
Appendix.
居民对COVID-19和VPD的风险认知和行为反应调查问卷
Residents’ risk perception and behavioral response questionnaire to COVID-19 and VPDs
您好!为更好地了解居民对新冠病毒 (COVID-19) 和疫苗可预防疾病 (VPD) 的风险认知和行为反应, 我们诚邀您参与一项调查, 将花费您几分钟的时间。本次调查不记名, 我们不会泄露任何与您个人情况相关的信息。感谢您的配合!
Hello! In order to better understand residents’ risk perceptions and behavioral responses to the new coronavirus (COVID-19) and vaccine preventable diseases (VPD), we sincerely invite you to participate in a survey that will take you a few minutes. This investigation is anonymous, and we will not disclose any information related to your personal situation. Thank you for your cooperation!
1.您的年龄段?(Age)
| 1□18-25 | 2□26-30 | 3□31-40 | 4□41-50 | 5□51-60 | 6□61以上 |
2.您的性别? (Sex)
| 1□男 (male) | 2□女 (female) |
3.您的文化程度? (Degree of education)
| 1□小学primary school | 2□中学middle school | 3□大学 college |
4□研究生及以上postgraduate |
4. 您认为以下疾病的易感性 (Susceptibility to COVID-19 and VPD)
| COVID-19 | 1□是(Yes) | 2□否(NO) | 3□不确定(UN) |
| VPD | 1□是(Yes) | 2□否(NO) | 3□不确定(UN) |
5. 您认为以下疾病的严重性 (Severity of COVID-19 and VPD)
| COVID-19 | 1□是(Yes) | 2□否(NO) | 3□不确定(UN) |
| VPD | 1□是(Yes) | 2□否(NO) | 3□不确定(UN) |
6. 预防COVID-19和VPD的措施?(Preventive measures taken against COVID-19 and VPD)
| 是否保持一定社交距离避免去人多的地方 | avoided going to crowded places | 1□是(Yes) | 0□否(NO) |
| 是否保持一定社交距离避免去高风险区 | avoided going to high risk areas | 1□是(Yes) | 0□否(NO) |
| 是否保持一定社交距离避免接触有呼吸道症状的患者 | avoided contacting with people with respiratory symptoms | 1□是(Yes) | 0□否(NO) |
| 是否保持一定社交距离避免前往医疗机构 | avoided visiting medical institutions | 1□是(Yes) | 0□否(NO) |
| 是否戴口罩 | wearing masks | 1□是(Yes) | 0□否(NO) |
| 是否勤洗手 | washing hands | 1□是(Yes) | 0□否(NO) |
| 是否保持一定社交距离 | social distancing | 1□是(Yes) | 0□否(NO) |
Funding Statement
This work was supported by Chinese Foundation for Hepatitis Prevention and Control under grant number YGFK20190027.
Authors’ contributions
Conceived and designed the experiments: XS, FT. Analysed the data: XS,YX. Wrote and revised the paper: XS, YX, YZ.All authors read and approved the final manuscript.
Disclosure of potential conflicts of interest
The authors declare that they have no competing interests.
References
- 1.Lai S, Ruktanonchai NW, Zhou L, Prosper O, Luo W, Floyd JR, Wesolowski A, Santillana M, Zhang C, Du X, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020;585(7825):410–13. doi: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Teslya A, Pham TM, Godijk NG, Kretzschmar ME, Bootsma MCJ, Rozhnova G.. Impact of self-imposed prevention measures and short-term government-imposed social distancing on mitigating and delaying a COVID-19 epidemic: a modelling study. PLoS Med. 2020;17(7):e1003166. doi: 10.1371/journal.pmed.1003166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Y, Tian H, Zhang L, Zhang M, Guo D, Wu W, Zhang X, Kan G L, Jia L, Huo D, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Global Health. 2020;5(5):e002794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hatoun J, Correa ET, Donahue SMA, Vernacchio L.. Social distancing for COVID-19 and diagnoses of other infectious diseases in children. Pediatrics. 2020;146:e2020006460. [DOI] [PubMed] [Google Scholar]
- 5.Nolen LD, Seeman S, Bruden D, Klejka J, Desnoyers C, Tiesinga J, Singleton R. Impact of social distancing and travel restrictions on non-COVID-19 respiratory hospital admissions in young children in rural Alaska. Clin Infect Dis. 2021;72(12):2196–2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chiu NC, Chi H, Tai YL, Peng CC, Tseng CY, Chen CC, Tan BF, Lin C-Y. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: retrospective national epidemiological surveillance study. J Med Internet Res. 2020;22(8):e21257. doi: 10.2196/21257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed F, Zviedrite N, Uzicanin A. Effectiveness of workplace social distancing measures in reducing influenza transmission: a systematic review. BMC Public Health. 2018;18(1):518. doi: 10.1186/s12889-018-5446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yu D, Lin Q, Chiu AP, He D. Effects of reactive social distancing on the 1918 influenza pandemic. PloS One. 2017;12(7):e0180545. doi: 10.1371/journal.pone.0180545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang JW, Lai FY, Wong F, Hon KL. Incidence of common respiratory viral infections related to climate factors in hospitalized children in Hong Kong. Epidemiol Infect. 2010;138(2):226–35. doi: 10.1017/S0950268809990410. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Y, Wang X, Li Y, Ma J. Spatiotemporal Analysis of Influenza in China, 2005-2018. Sci Rep. 2019;9(1):19650. doi: 10.1038/s41598-019-56104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dai Q, Ma W, Huang H, Xu K, Qi X, Yu H, Deng F, Bao C, Huo X. The effect of ambient temperature on the activity of influenza and influenza like illness in Jiangsu Province, China. Sci Total Environ. 2018;645:684–91. doi: 10.1016/j.scitotenv.2018.07.065. [DOI] [PubMed] [Google Scholar]
- 12.Zhang J-C, Liu W-D, Liang Q, Hu J-L, Norris J, Wu Y, Bao C-J, Tang F-Y, Huang P, Zhao Y. Spatial distribution and risk factors of influenza in Jiangsu province, China, based on geographical information system. Geospat Health. 2014;8(2):429–35. doi: 10.4081/gh.2014.31. [DOI] [PubMed] [Google Scholar]
- 13.Kong MM, Yang B, Gong CJ, Wang H, Li X, Zhao KS, Li JJ, Wu F, Liu X, Hu Z, et al. Development of immunochromatographic colloidal gold test strip for rapid detection of Haemophilus influenzae in clinical specimens. J Appl Microbiol. 2017;123(1):287–94. doi: 10.1111/jam.13489. [DOI] [PubMed] [Google Scholar]
- 14.Tao Y, Hao H, Li J, Wang M, Wang Y, Zhang G, Hu Z. [Colloidal gold immunochromatographic strip for rapid detection of Haemophilus influenzae]. Sheng Wu Gong Cheng Xue Bao = Chin J Biotechnol. 2019;35:901–09. [DOI] [PubMed] [Google Scholar]
- 15.Huh K, Jung J, Hong J, Kim M, Ahn JG, Kim JH, Kang JM. Impact of non-pharmaceutical interventions on the incidence of respiratory infections during the COVID-19 outbreak in Korea: a nationwide surveillance study. Clin Infect Dis. 2021;72(7):e184–e191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cowling BJ, Ali ST, Ng TWY, Tsang TK, Li JCM, Fong MW, Liao Q, Kwan MY, Lee SL, Chiu SS. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5(5):e279–e88. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cowling BJ, Ng DM, Ip DK, Liao Q, Lam WW, Wu JT, Lau J, Griffiths S, Fielding R. Community psychological and behavioral responses through the first wave of the 2009 influenza A(H1N1) pandemic in Hong Kong. J Infect Dis. 2010;202(6):867–76. doi: 10.1086/655811. [DOI] [PubMed] [Google Scholar]


