ABSTRACT
The development of safe and effective COVID-19 vaccines as well as their delivery to people’s arms are the best hope for ending the COVID-19 pandemic. However, the implementation of vaccination varies greatly across countries, with the developing countries lagging behind. This study investigates Indonesia’s vaccination experiences, challenges, and acceleration over the course of implementation period. This study provides simulations to estimate the vaccination rate using time-series forecasting machine learning. We use Administrative data and Survey results in our analysis. Our findings suggest limited vaccine availability had caused low-coverage vaccination implementation in the early stage of vaccination implementation period. However, following the increased availability of vaccine, the vaccination rate accelerates up to 600% times. The government of Indonesia utilized strategic public places, public and private offices, and engaging private sectors in the phase two implementation to accelerate the vaccination implementation. Indonesia might reach 63.1 million individuals vaccinated at the end of March 2022, or 35% of the targeted population with up to April 2021 vaccination rate. To accelerate, government introduced a number of new strategies including door-to-door persuasion through neighborhood association (RT), educating individuals, and providing transportation from their home to the vaccination facility. We expect new strategies could further improve vaccination speed by around 1.4 million to 3.5 million individuals per day.
KEYWORDS: COVID-19, vaccines, vaccination acceleration
Introduction
The novel Coronavirus Disease (COVID-19) has been haunting people across the globe, including people in Indonesia. COVID-19 crisis devastates not only public health but also the economy. This health crisis caused Indonesia an economic contraction of 2.2% (y-on-y) in 2020. The disruption to the growth of labor-intensive sectors is inevitable. Indonesia witnessed a deep contraction in a number of economic sectors, particularly sectors that require face-to-face interaction and/or mobility such as the transportation and warehousing sector which contracted by 13.4%, construction sector which contracted by 5.7%, and food and beverages sector which contracted by 8.9%. The poverty rate in September 2020 was recorded at 10.2% (27.55 million people), or an increase of 2.76 million people from September 2019.1,2 Its impact on public health and economy made COVID-19 the primary concern of all countries in the world, including Indonesia.
Vaccines had demonstrated as effective means to control various infectious diseases in the past.3–7 The success of a number of companies and research institutes in developing Covid-19 vaccines had become as a new hope to contain the virus in 2021. Vaccines that induce virus-neutralizing antibodies may optimally prevent COVID-19 infection and avoid unfavorable effects.8 Many studies show vaccines provide promising efforts on COVID-19 containment worldwide in the clinical phase and implementation phase. Clinical Development reported vaccine efficacy gives relative risk reductions of 95% for the Pfizer–BioNTech, 94% for the Moderna–NIH, 90% for the Gamaleya, 67% for the J&J, and 67% for the AstraZeneca–Oxford vaccines.9–11 BBC News shows four weeks after the first dose implementation, hospital admissions declined by 85% and 94% in the United Kingdom.12,13 Similar findings is also found in the United States, Italy, and many other countries worldwide.13–15 Therefore, the development of safe, effective COVID-19 vaccines and its delivery to people’s arms is a global priority. It brings hope for ending the COVID-19 pandemic.16,17
For it’s effective protection, vaccination must be administered well in advance of any natural exposure or infection.18 But, ensuring in-time vaccines availability can be ethically and logistically complex. The problems lie from vaccines limitation, competing priority groups to vaccine acceptabilities.19,20 Yet, the application of vaccination varies in different parts of the world. Despite the importance of the vaccination distribution, scant studies explore the vaccination implementation challenges and strategies to deliver it to people’s arms, primarily in developing countries. While some studies concern about differences in access to COVID-19 vaccines between rich and poor countries (Wouters et al., 2021; Yamey et al., 2020), they did not address the distribution issues which particularly relevant to the developing countries. So, even though developing countries can have access to vaccines, it does not necessarily mean they can administer the vaccination implementation swiftly. For example, poor or nonexistence of infrastructures, limited society health education, and the quality of the nation’s institutions are among factors potentially delay the vaccination implementation programs in developing countries.19,21–24
Lessons learned from Indonesia’s experiences and challenges in implementing the vaccination program, and it’s vaccination acceleration strategy could help other countries to speed up the COVID-19 vaccination rate. In February, some studies predict Indonesia’s vaccination could take more than ten years to cover 75% of its population.25,26 However, On April 24, two months later, Bloomberg reports Indonesia as the 12th largest vaccine implementation country that administered more than 18.5 million doses or 336 thousand doses daily on average.27 Those conflicting pieces of evidence suggest the dynamics in the Indonesia vaccination program in which the vaccine roll-out program have changed considerably.
This study investigates vaccination experiences in Indonesia. We discuss the challenges that Indonesia faces and the acceleration strategy it adopts. In this study, we provide simulations to estimate the vaccination rate in Indonesia taking into account the acceleration strategy. We take particularly close look at policy and vaccination implementation which is relevant for other developing countries.
Data and methodology
This study closely looks at vaccination policy, vaccination administration plan, and its implementation from the Indonesian government. Indonesia planned to provide free vaccination for 181 million people and divide it into four wave vaccination plans based on occupation types and age from January 2021 to March 2022. We construct daily vaccine arrival plans and daily vaccination administration plans for each occupation and age wave to understand their daily vaccination rate plan over time. We employ daily administered vaccine compiled in kawalcovid database from January 10, 2021 to April 24, 2021. Medical, education, science, research, technology, and mass communication volunteers help each other collect COVID-19 data in kawalcovid. Kawalcovid provides daily vaccination progress at an aggregate level or by occupation and the elderly vaccination progress up to date, but with a different starting point. They provide aggregate vaccination starting on the first day of the vaccination period. Vaccination progress for each occupation and the elderly group started on March 2, 2021. Daily vaccination administered is compared to the plan in order to understand the achievement rate. We complement kawalcovid vaccination data with COVID-19 cases data from Indonesia National Board for Disaster Management (BNPB) to analyze its trend before and after the vaccination period.
We simulate the Indonesian vaccination rate, and provide analysis on how to improve the vaccination rate. We use the time-series forecasting machine learning prophet library developed by Facebook to estimate vaccination implementation projections for March 2022. Facebook prophet library uses time as a repressor and fits several linear and nonlinear functions of time as regression components. We use python software to employ a time-series forecasting vaccination rate. We compared vaccination projection with vaccination plan to understand whether Indonesian current vaccination rate match the plan. We also utilize the National Socioeconomic Survey (SUSENAS) 2019 data to estimate the number of neighborhood association (RT) that could potentially mobilize to increase the vaccination rate in Indonesia. SUSENAS is a survey designed to collect relatively broad socio-economic data. The data collected in SUSENAS includes education, health/nutrition, housing, other socio-economic activities, socio-cultural activities, consumption/expenditure and household income, travel, and public opinion regarding their household’s welfare. The total number of neighborhood association (RT) is estimated from total households for each province from SUSENAS divided by the number of households per RT as stipulated in local government regulation, which is 20–50 households.
We construct an estimated health facility distance map for each district using Village Potential (PODES) 2018 data to understand vaccination challenges-related health facility heterogeneity. PODES is a village level survey to collect data and information on the specific potential at the lowest administrative level (villages). PODES data is essential for planning, implementing, controlling, and evaluating regional Development in general or even specifically according to specific regions. It is an area-based thematic data source that can describe the potential of a village-level area throughout Indonesia.
Results and discussion
Vaccination plan and implementation in Indonesia
Indonesian government COVID-19 vaccination plan is based on the Presidential decree number 99/2020 enacted on October 5, 2020, which provides legal basis for COVID-19 procurement and vaccination implementation. Minister of Health Regulations number 84/2020 on December 14, 2020, defines further the implementation plans that include vaccine types and vaccination targets.
The Government of Indonesia secured vaccine very early. The procurement was settled in 2020. This allows Indonesia’s government secures enough dose to reach herd immunity. The Government of Indonesia secured more than 426 million doses from Sinovac Biotech, Novavax, Vaccines from COVAX/GAVI, Pfizer, and AstraZeneca to vaccinate more than 181 million Indonesian citizens. Sinovac Biotech will provide more than 55% COVID-19 vaccines in Indonesia.
Furthermore, vaccination implementation strategy and mechanism was also set in 2020. Although Sinovac vaccine phase 1 and 2 clinical trials were conducted in China between April 16, 2020 to May 5, 2020,28 Indonesia is part of the Phase 3 Global Clinic Trial for the COVID-19 candidate from Sinovac carried out by four countries (Brazil, Chile, Indonesia and Turkey), with a total more than 20 thousand volunteers worldwide.29 The COVID-19 vaccine material from Sinovac arrived in Indonesia on July 19, 2020. As of August 16, 2020, a total of 1,866 Indonesia volunteers had registered to participate in the phase III clinical trials of the Sinovac Biotech30 and 1,620 of volunteers which met all the required volunteers’ criteria received the complete dose.31 The Sinovac vaccine, which showed an efficacy of 65.3% in Indonesia phase III clinical trials, is declared save.32 The National Food and Drug Supervisory Agency (POM Agency) issued Emergency Use of Authorization (EUA) on January 11, 2021. Also, the vaccination strategy and mechanism include real-time vaccine shipment tracking and centralized vaccination data. The Government of Indonesia allocated more than IDR 58 trillion (USD 4.1 billion) for vaccine procurement and vaccination implementation. In addition, earmarked additional IDR 6.5 trillion (USD 464 million) through local government for supporting vaccination implementation program is also secured.
Table 1 illustrates the Ministry of Health COVID-19 vaccination target and the related vaccination plan for the years 2021 and 2022 based vaccine arrival plan to Indonesia. Based on the plan, 1.46 million health workers will be vaccinated first followed by the elderly and public service workers, about 38.4 million. The third targeted group are those living in the High-Risk Areas. The remaining of the population will get their vaccines during the period of June 2021 to March 2022. Table 1 also suggests a higher population target in the later period which consequently requires a continuous vaccination acceleration plan.
Table 1.
Vaccination target and wave in Indonesia
| Period | Period I | Period II | Period III | Period IV |
|---|---|---|---|---|
| Vaccination targets | Health workers | Elderly and public service | Communities on high-risk areas | General population |
| Estimated population | 1.46 Million | 38.4 Million | 63.9 Million | 77.7 Million |
| Estimated time | January 2021–June 2021 | January 2021–June 2021 | June 2021– March 2022 | June 2021–March 2022 |
We construct cumulative daily vaccine arrival date and vaccination implementation plan based on the estimated vaccine arrival date and implementation plan from the Ministry of Health as in Figure 1. The figure suggests vaccination implementation plan follows closely the vaccine arrival plan. This indicates the government’s vaccination plan already taking into accounts vaccine availability throughout the vaccination period. Phase 1 vaccination started on January 13, 2021, to cover 1.46 million health workers or correspond to around 60,000 individuals vaccinated per day up to February 2021. Low coverage vaccination plan in the beginning period up to February 2021 follows the limited vaccines availability in early 2021. Vaccines arrival and implementation planned increase substantially from February 2021 which is sufficient to cover 38.4 million elderly and public services workers vaccinated or equivalent to 659 thousand individuals per day in the second wave to keep up with the plan (June 2021). This means 16 times the daily vaccination rate of first wave. Based on the plan, more than 408 million doses of Covid-19 vaccine will arrive during the period of June 2021 to March 2022 to vaccinate more than 141.6 million Indonesians. The vaccinators need to vaccinate more than 420 thousand individuals per day for about 335 days on these last two phases to keep up with the plan. Extra doses of vaccines would still be available to cover more Indonesian populations after June 2021.
Figure 1.
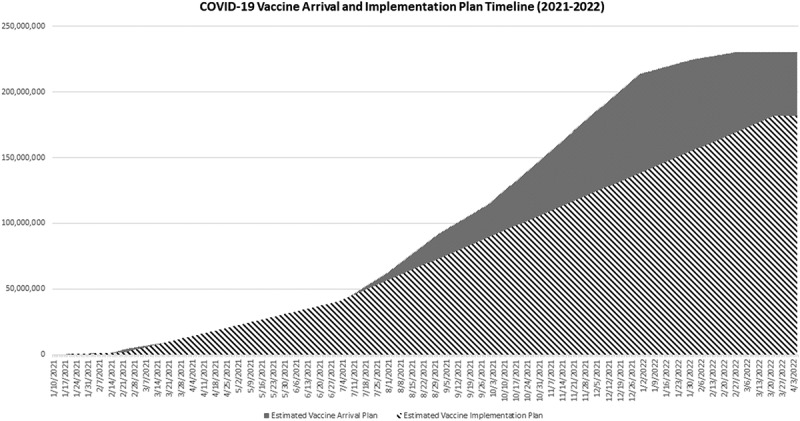
COVID-19 vaccine arrival and implementation plan timeline (2021–2022).
Figure 2 provides vaccination implementation and its plan up to April. 24th, 2021 in Indonesia. Gray shading is the estimated first dose vaccination plan, and a solid black line is its vaccination implementation. The dot pattern is the estimated second-dose vaccination plan, and the black dash line is its implementation. The flat estimated second dose vaccination plan from February 21 represents a 28-day second-dose waiting period after the first shots. Indonesia has administered 18.5 million doses with 11.7 million individuals for the first dose and 6.8 million individuals for the second dose on April 24, 2021. The figure suggests vaccination implementation is in line with its plan on vaccination wave 1, yet less catch-up its plan on wave 2. 80% of health workers’ target received the first dose, and 68% of them received the second dose on February 17, 2021, when wave two vaccination implementation started. Forty-nine thousand nine hundred twenty doses vaccines per day on average are administered to health workers on phase 1 from January 13 to February 17, 2021.
Figure 2.
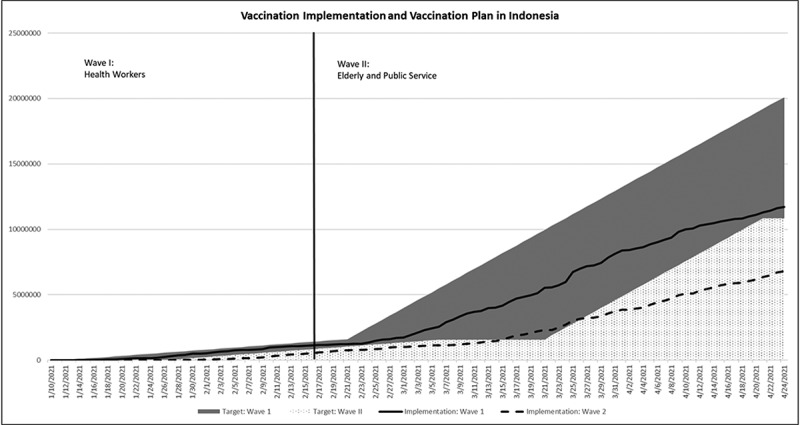
COVID-19 vaccination implementation in Indonesia.
Vaccination for elderly started earlier than the plan. While the vaccination to health workers continuous, the vaccination for the elderly and public service workers also began after February 17, five days earlier than the initial plan. We observe a more extensive vaccination implementation in the wave 2 vaccination period. On average, 316,000 doses per day are administered on phase two or 600% larger than the phase 1 daily vaccination implementation period. The acceleration of vaccination implementation in the phase 2 was made possible by utilizing strategic public places, public and private offices, and engaging private sectors to implement the vaccination. Drive-thru and walk-in vaccinations were also provided at particular places. For example, Istora Senayan, a football sport field, could provide vaccination rate up to 6 thousand doses per day. The authority also engages public transportation companies to provide transportation to the vaccination site.
Given vaccine supplies limitation at the beginning of vaccination period, vaccination implementation strategy focuses on the high-risk areas to overcome COVID-19. Java island received 70% vaccine allocation. Java contributes 68% of COVID-19 cases In Indonesia. Figure 3 provides ten provinces with the highest vaccination rate on the wave I and II in Indonesia. DKI Jakarta is the highest, administering more than 2.85 million doses or corresponds to 99% of its vaccination targets on waves I and II on April 24, 2021. Bali province administered 916 thousand doses or corresponded to 76% of its target on the wave I and II. Yogyakarta, Banten East Java, Central Java, and West Java vaccinate 59%, 47%, 38%, 39%, and 42% of its target on the wave I and II.
Figure 3.
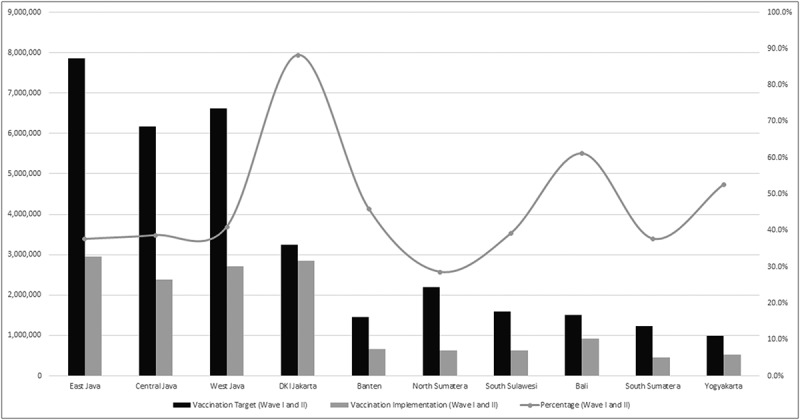
Provinces with highest vaccination rate.
Figure 4 provides COVID-19 daily confirmed cases for 10 Indonesian provinces from January 10, 2021, to April 24, 2021 (vaccination period). The figure suggests declining daily confirmed new cases trend for all provinces in Java Island, including Jakarta, East Java, Central Java, West Java, Banten, and Yogyakarta. Bali, North Sumatera, and South Sulawesi indicate declining COVID-19 cases trend as well. However, South Sumatera shows a declining trend at the beginning and an increasing trend after March 2021. Reduction of COVID-19 daily confirmed cases on most of the highest vaccination rate provinces indicates early vaccination hope to COVID-19 containment in Indonesia.
Figure 4.
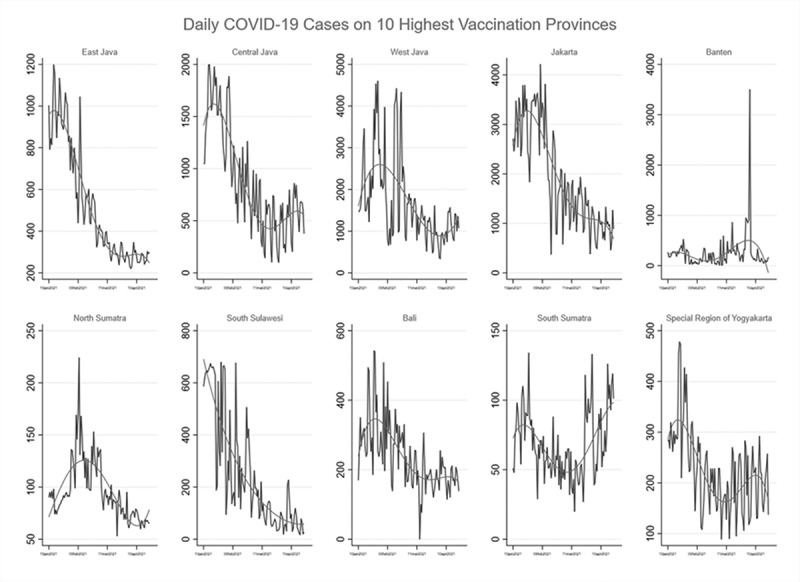
COVID-19 daily confirmed cases in Indonesia.
Vaccination challenges and the way forward
Despite Indonesia’s success story in accelerating vaccination implementation in phase 2, vaccination implementation challenges remain. The 600% vaccination rate acceleration in phase two is not sufficient to conclude the vaccination for herd immunity in March 2022. Indonesia needs further vaccination acceleration to achieve the required target since more vaccine supplies and vaccination targets in phase 3 and 4.
This study forecasts vaccination implementation in Indonesia up to March 2022 using the time-series forecasting machine learning prophet library developed by Facebook, as depicted in Figure 5. We forecast vaccination implementation at the mean and upper bound levels. The actual first dose vaccination implementation is shown before April 24, and the forecast implementation is shown after April 24. The gray shade is the vaccination plan, the solid line is a forecast vaccination at the mean level, and the dashed line is a forecast vaccination at the upper bound level. The figure suggests the current vaccination rate could reach 63.1 million individuals at the end of March 2022, or 35% of the targeted population. If the government can maintain the acceleration, it can improve vaccination coverage for up to 154 million people in March 2022.
Figure 5.
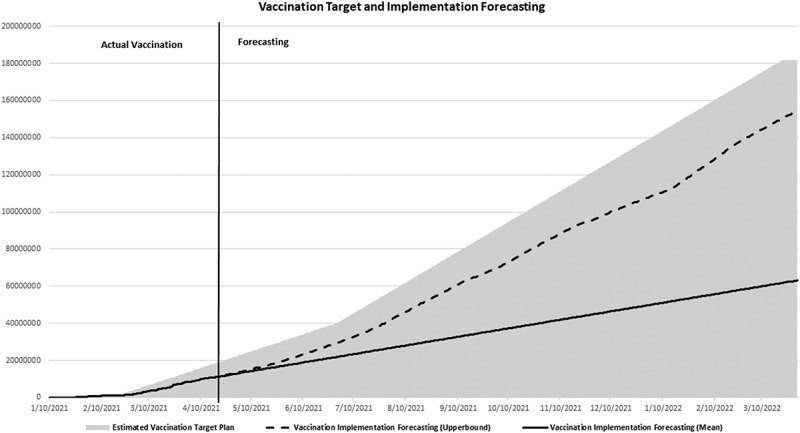
Forecasting vaccination implementation in Indonesia.
However, maintaining the current acceleration rate or higher might face more complex challenges, including cold chain, distribution to remote areas, areas and population heterogeneities, people mobilization, and implementation financing. Lessons learned could be drawn from current vaccination implementation in Indonesia. The availability of health facility and health workers varies across regions. This contributes to different vaccination speeds across the regions, with outer java islands and rural areas tend to have lower vaccination speed. Figure 6 maps the nearest distance to any hospital or public health facility (Puskesmas) for each district in Indonesia. Darker shades suggest a longer travel distance to the nearest hospital or public health facility. The distance map is constructed from an average self-reported from a village official to the nearest hospital or public health facility on a district using PODES 2018. The figure suggests that individuals living in outer Java Island require longer travel time to health facility than people living in Java Island, primarily in Kalimantan and Papua islands. For Sumatera and Sulawesi, the average distance to the nearest hospital is around 25–30 km, and the average distance to the nearest public health facility is around 3–4 km. Longer travel distance is faced by individuals living in Kalimantan and Papua who have to travel between 41 and 60 km to the nearest hospital and is 4–15 km to the nearest public health facilities. This implies that people in Kalimantan and Papua will need transportation assistance to the nearest vaccination center in Indonesia.
Figure 6.

Distance to nearest hospital and public health facility in Indonesia.
The next challenge is reaching out to certain target group since each target group could have different characteristics that correlate with the vaccination rate. For example, vaccination is a crucial means to the elderly to protect them from morbidity and mortality.33 However, they also lack the resources, knowledge, and skills to obtain medical care.34 Figure 7 shows the vaccination implementation of waves 1 and 2 by target groups (health workers, elderly, and public service workers). The implementation of vaccination for health workers has reached 1.48 million people (100% of the target) for the first dose and 1.34 million people (91% of the target) for the second dose or a total of 2.8 million doses administered to health workers. The implementation of vaccination for public officers has reached 7.8 million people (45% of target) for the first dose and 4.2 million people (24% of the target) for the second dose or 12 million doses administered to public officers. In contrast, lower achievement rate for the elderly that the implementation of vaccination for the elderly has reached 2.38 million people or correspond 11% of the target for the first dose and 1.26 million people (5.8% of the target) for the second dose or total 3.6 million doses for the elderly on April 24, 2021. A considerable achievement gap of vaccination rate between public service workers and the elderly implies more considerable challenges to vaccinate the elderly. However, the latter group represents a higher fatality risk.
Figure 7.
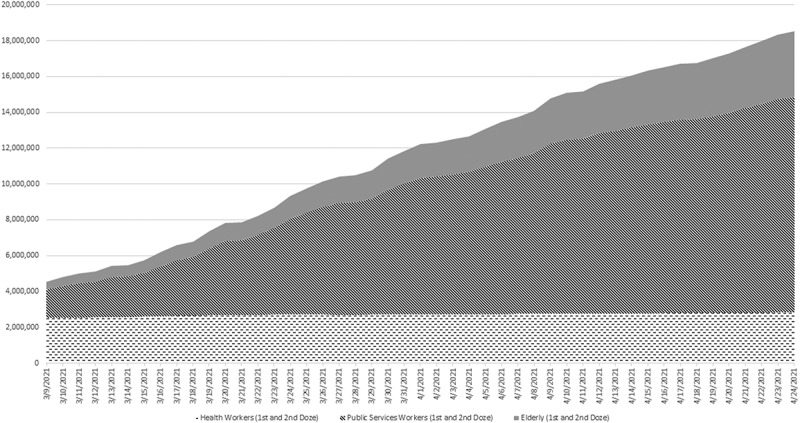
Vaccination Implementation by target group.
Addressing the challenge to vaccinate the elderly people, Indonesian government roll out the plan to accelerate the vaccination implementation to the elderly population with more intensified socialization and conducting a door-to-door vaccination persuasion through neighborhood association (RT), educating the elderly about the importance of vaccination, and providing transportation from their home to the vaccination facility. The neighborhood association is a unique lowest-level customary institution in Indonesia. While there is no publicly available neighborhood association administrative data, local government regulation indicates each neighborhood association usually manages 20–50 households in an area.35,36 Figure 8 estimates the number of neighborhood associations for each province in Indonesia. The solid bar is the estimated number of RT if one RT manages 20 households, and the dot bar is the estimated number of RT if one RT manages 50 households. The figure suggests there are 1.4 million to 3.5 million RT available all across Indonesia. Door-to-door vaccination persuasion through RT could potentially increase vaccination speed further if government mobilize RT to persuade elderly in their neighborhood to get vaccination. For example, suppose one RT could persuade one elderly per day and manage their transportation to the nearest vaccination center, this would lead to vaccination rate at least 1.4 million doses per day.
Figure 8.
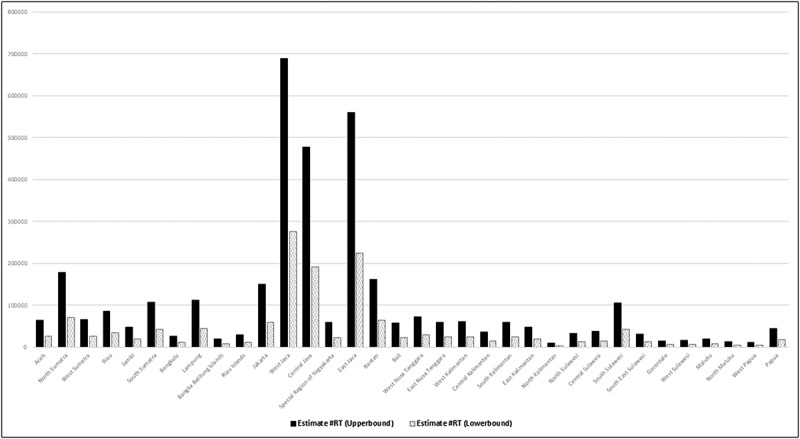
Estimate number of neighborhood association (RT) in Indonesia.
The challenge is how to finance society mobilization and transportation provision. Mobilizing society and providing transportation for 1.4 million to 3.5 million individuals per day requires a substantial amount of money. Currently, the government of Indonesia had allocated more than Rp 58 T for vaccine procurement and vaccination implementation which includes vaccine purchase and vaccination operational to cover distributions cost, vaccine infrastructures, medical devices for health workers, and vaccinators’ incentives. However, it does not yet cover society mobilization and transportation cost for people to get to the vaccination center. Fortunately, in the Indonesian budgetary system, budget allocated to regional government, term as Transfer to Regional Budget and Village fund program can be used as an alternative financing solution. Village fund program in particular is the allocated budget to the smallest unit of governance at the village level from the State Revenue and Expenditure Budget (APBN). The allocated to Villages is transferred through the Regency Regional Revenue and Expenditure Budget (APBD) to finance government administration, development implementation, community development, and empowerment program at the village level. In 2021, the village fund program focuses on the national economic recovery under the village’s authority. The village government can form the Covid-19 village’s command center, whose funding sources are obtained from village funds.
Conclusion and discussion
The development of safe, effective COVID-19 vaccines and their delivery to people’s arms is a global priority that can bring hope to end the COVID-19 pandemic. Yet, the implementation of these vaccines can be different across countries. This study closely looks at vaccination policy, vaccination administration plan, and its implementation in Indonesia which might be relevant for other developing countries. Supply bottleneck is among the problems faced by developing countries,37,38 including Indonesia, particularly at the beginning of the vaccination period due to relatively low coverage vaccination plan. Supply constraints from the manufacturers is one of the biggest challenges in the early period of vaccination when only 3 million doses arrived in Indonesia up to January 2021 although Indonesia had procured the vaccine as early as October 2020. Therefore, Indonesia’s phase 1 vaccination implementation focus on covering 1.46 million health workers. Nepal provides a similar solution with Indonesia39 since prioritization of target groups can increase the effectiveness of vaccines when vaccine supply is insufficient.6,19
Indonesia’s early vaccination procurement plan allows Indonesia to secure more vaccines supply over time to cover enough population to get herd immunity. With the continuous supply from manufacturers, phase two vaccination rate accelerates up to 600% of phase 1 daily vaccination rate. The use of strategic public places such as stadiums, public and private offices, engaging private sectors, employing drive-thru, and walk-in vaccination methods are among the key to successful vaccination in Indonesia. Time-series forecasting machine learning suggests that vaccination implementation could reach 63.1 million to 154 million individuals at the end of March 2022 if the government maintain the acceleration. Therefore, the Indonesian government requires continuous acceleration strategies, or they could face interrupted vaccination implementation. Ensuring cold chain equipment sufficiently installed to address storage gaps should be the priority40 as more vaccines will arrive in the future. Continuous evaluation of vaccine distribution loop is required to improve delivery efficiency, primarily in eastern part of Indonesia that has dispersed population and challenging terrains. For example, outsourced vaccine logistics to private transporters and vaccine delivery redesign in Africa and Gaza could ensure efficient vaccine transport and cost reduction.40 Access to a vaccine is usually via physician6 in public health centers and large private centers to ensure infrastructure readiness. However, large-scale vaccination programs may need to team up with private doctors, rural midwives, and any individual health workforce to fill the health center gap in underdeveloped areas. Appropriate training and incentives for them are required to prepare them for providing vaccination.
Large populations are waiting despite the rapid acceleration rate, and there are different acceleration rates between target groups. A study shows COVID-19 vaccine acceptance in Indonesia varies between 67% and 95%.41 The communication strategy should be continuously refined, including vaccine information, patient invitation, and recall system19 to address vaccination demand’s problems. Door to door persuasion through neighborhood association (RT), educating elderly about the importance of vaccination, and provision of transportation from their home to the vaccination facility strategies could potentially improve vaccination speed to around 1.4 million to 3.5 million individuals per day if one RT could persuade one individual per day and manage their transportation to the nearest vaccination center. Central government, local government, health authorities and international organizations must work together19 to achieve the strategy.
This study has a few limitations. Our time-series forecasting does not consider individual Indonesian province vaccination trends because of data limitations. The different regions could have different trajectories because of various regional characteristics such as transportation capabilities and vaccination health centers. Each health center could also specific experiences related to vaccination. We are unable to examine individual health center experiences to understand their challenges and opportunities better. For example, the particular health center may lack the internet required to implement a centralized vaccination system. Despite these limitations, our results provide valuable information on COVID-19 vaccination implementation acceleration in developing countries. This study is relevant and might encourage developing countries to improve distribution access to COVID-19 vaccination for accelerated vaccination program. No one safe until everyone safe. Vaccines are the hope to better manage COVID-19.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Indonesia S . Pertumbuhan Ekonomi Indonesia Triwulan II-2020; 2020. (17/02/Th. XXIV):1–12. [accessed 2021 May 5]. https://www.bps.go.id/pressrelease/2020/02/05/1755/ekonomi-indonesia-2019-tumbuh-5-02-persen.html
- 2.Indonesia S . STATISTIK Pertumbuhan Ekonomi Indonesia Triwulan I-2020; 2020. [accessed 2021 May 5]. https://www.bps.go.id/pressrelease/2020/02/05/1755/ekonomi-indonesia-2019-tumbuh-5-02-persen.html.
- 3.Kochhar S, Rath B, Seeber LD, Rundblad G, Khamesipour A, Ali M, Initiative VVS.. Introducing new vaccines in developing countries. Expert Rev Vaccines. 2013;12(12):1465–78. doi: 10.1586/14760584.2013.855612. [DOI] [PubMed] [Google Scholar]
- 4.Michelsen SW, Soborg B, Koch A, Carstensen L, Hoff ST, Agger EM, Lillebaek T, Sorensen HCF, Wohlfahrt J, Melbye M.. The effectiveness of BCG vaccination in preventing Mycobacterium tuberculosis infection and disease in Greenland. Thorax. 2014;69(9):851–56. doi: 10.1136/thoraxjnl-2014-205688. [DOI] [PubMed] [Google Scholar]
- 5.Purssell E. Reviewing the importance of the cold chain in the distribution of vaccines. Br J Community Nurs. 2015;20(10):481–86. doi: 10.12968/bjcn.2015.20.10.481. [DOI] [PubMed] [Google Scholar]
- 6.Smith J, Lipsitch M, Almond JW. Vaccine production, distribution, access, and uptake. Lancet. 2011;378(9789):428–38. doi: 10.1016/S0140-6736(11)60478-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wojda TR, Valenza PL, Cornejo K, McGinley T, Galwankar SC, Kelkar D, Sharpe RP, Papadimos TJ, Stawicki SP. The Ebola outbreak of 2014-2015: from coordinated multilateral action to effective disease containment, vaccine development, and beyond. J Glob Infect Dis. 2015;7(4):127. doi: 10.4103/0974-777X.170495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Speiser DE, Bachmann MF. COVID-19: mechanisms of vaccination and immunity. Vaccines. 2020;8(3):404. doi: 10.3390/vaccines8030404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.AstraZeneca . COVID-19 vaccine AstraZeneca confirms 100% protection against severe disease, hospitalisation and death in the primary analysis of phase III trials; 2021. [accessed 2021 Aug 10]. https://www.astrazeneca.com/media-centre/press-releases/2021/covid-19-vaccine-astrazeneca-confirms-protection-against-severe-disease-hospitalisation-and-death-in-the-primary-analysis-of-phase-iii-trials.html.
- 10.Olliaro P, Torreele E, Vaillant M. COVID-19 vaccine efficacy and effectiveness—the elephant (not) in the room. Lancet Micro. 2021;2:e279–e280. doi: 10.1016/S2666-5247(21)00069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pfizer . Pfizer and biontech conclude phase 3 study of COVID-19 vaccine candidate, meeting all primary efficacy endpoints; 2020. [accessed 2021 May 5]. https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-conclude-phase-3-study-covid-19-vaccine.
- 12.BBC . Covid vaccines - “spectacular” impact on serious illness; 2021. [accessed 2021 May 5]. https://www.bbc.com/news/health-56153600.
- 13.US News . Single dose of coronavirus vaccines reduces hospitalization in seniors, U.K. study finds; 2021. [accessed 2021 Aug 8]. https://www.usnews.com/news/health-news/articles/2021-03-02/single-dose-of-coronavirus-vaccines-reduces-hospitalization-in-seniors-uk-study-finds#:~:text=Justonedoseofthe,peopleover80yearsold.
- 14.MarketWatch . Single dose of AstraZeneca or Pfizer COVID-19 vaccine cuts hospitalization risk by more than 80%, study shows; 2021. [accessed 2021 Aug 8]. https://www.marketwatch.com/story/single-dose-of-astrazeneca-or-pfizer-covid-19-vaccine-cuts-hospitalization-risk-by-up-to-80-study-shows-11614688951.
- 15.Moghadas SM, Vilches TN, Zhang K, Wells CR, Shoukat A, Singer BH, Meyers LA, Neuzil KM, Langley JM, Fitzpatrick MC. The impact of vaccination on COVID-19 outbreaks in the United States. medRxiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.BBC . Covid: Biden promises vaccines for all US adults by end of May; 2021. [accessed 2021 May 5]. https://www.bbc.com/news/world-us-canada-56262687.
- 17.Koff WC, Schenkelberg T, Williams T, Baric RS, McDermott A, Cameron CM, Cameron MJ, Friemann MB, Neumann G, Kawaoka Y. Development and deployment of COVID-19 vaccines for those most vulnerable. Sci Transl Med. 2021;13:579. doi: 10.1126/scitranslmed.abd1525. [DOI] [PubMed] [Google Scholar]
- 18.Cutler GJ. Vaccines and vaccination. In: Commercial chicken meat and egg production. Springer; 2002. p. 451–61. [Google Scholar]
- 19.Hessel L, Group EVM (EVM) IW . Pandemic influenza vaccines: meeting the supply, distribution and deployment challenges. Influenza Other Respi Viruses. 2009;3(4):165–70. doi: 10.1111/j.1750-2659.2009.00085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang H-C, Singh B, Morton DP, Johnson GP, Clements B, Meyers LA. Equalizing access to pandemic influenza vaccines through optimal allocation to public health distribution points. PloS One. 2017;12(8):e0182720. doi: 10.1371/journal.pone.0182720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gauri V, Khaleghian P. Immunization in developing countries: its political and organizational determinants. The World Bank; 2002. [Google Scholar]
- 22.Sankaranarayanan R. HPV vaccination: the promise & problems. Indian J Med Res. 2009;130:322–27. [PubMed] [Google Scholar]
- 23.Sherris J, Friedman A, Wittet S, Davies P, Steben M, Saraiya M. Education, training, and communication for HPV vaccines. Vaccine. 2006;24:S210–S218. doi: 10.1016/j.vaccine.2006.05.124. [DOI] [PubMed] [Google Scholar]
- 24.Streefland PH. Introduction of a HIV vaccine in developing countries: social and cultural dimensions. Vaccine. 2003;21(13–14):1304–09. doi: 10.1016/S0264-410X(02)00685-0. [DOI] [PubMed] [Google Scholar]
- 25.The Strait Times . Pandemic could end in 7 years at current pace of vaccination; 2021. Feb 6. [accessed 2021 May 5]. https://www.straitstimes.com/world/pandemic-could-end-in-7-years-at-current-pace-of-vaccination
- 26.Zainudin E. Bloomberg says > 10 years, but how many years is it actually? Nightingale; 2021. [accessed 2021 May 5]. https://medium.com/nightingale/bloomberg-says-10-years-but-how-many-years-is-it-actually-164c3c7c2732.
- 27.Bloomberg . Covid-19 tracker; 2021. [accessed 2021 May 5]. https://www.bloomberg.com/graphics/covid-vaccine-tracker-global-distribution/.
- 28.Zhang Y, Zeng G, Pan H, Li C, Hu Y, Chu K, Han W, Chen Z, Tang R, Yin W. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18–59 years: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect Dis. 2021;21(2):181–92. doi: 10.1016/S1473-3099(20)30843-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.voi . Clinical trials of COVID-19 vaccine in Indonesia enter the monitoring period; 2020. [accessed 2021 Aug 8]. https://voi.id/en/news/19637/clinical-trials-of-covid-19-vaccine-in-indonesia-enter-the-monitoring-period.
- 30.Antara . 110 Volunteers of Covid-19 vaccine trials in Bandung healthy: health office. Medcom.id; 2020. [accessed 2021 Aug 8]. https://www.medcom.id/english/national/5b2XO8aK-110-volunteers-of-covid-19-vaccine-trials-in-bandung-healthy-health-office.
- 31.Biofarma . The Covid-19 vaccine can be used in Indonesia; 2021. [accessed 2021 Aug 8]. https://www.biofarma.co.id/en/latest-news/detail/the-covid19-vaccine-can-be-used-in-indonesia.
- 32.Salma . The Sinovac vaccine, which showed an efficacy of 65.3 percent, is declared safe; 2021. [accessed 2021 Aug 8]. https://www.ugm.ac.id/en/news/20611-ugm-expert-having-an-efficacy-rate-of-65-3-percent-sinovac-vaccine-remains-safe.
- 33.Ciabattini A, Nardini C, Santoro F, Garagnani P, Franceschi C, Medaglini D. Vaccination in the elderly: the challenge of immune changes with aging. In: Seminars in immunology. Vol. 40. Elsevier; 2018. p. 83–94. [DOI] [PubMed] [Google Scholar]
- 34.Heydari A, Sharifi M, Bagheri Moghaddam A. Challenges and barriers to providing care to older adult patients in the intensive care unit: a qualitative research. Open Access Maced J Med Sci. 2019. Nov 15;7(21):3682–90. doi: 10.3889/oamjms.2019.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Indonesia M of HA . Lembaga Kemasyarakatan Desa Dan Lembaga Adat Desa. Indonesia; 2018. [Google Scholar]
- 36.Indonesia MM . Rukun Tetangga Dan Rukun Warga. Indonesia; 2012. [Google Scholar]
- 37.OECD . Coronavirus (COVID-19) vaccines for developing countries : an equal shot at recovery. 2021. Feb. p. 1–22.
- 38.Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, Jit M. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021;397:1023–34. doi: 10.1016/S0140-6736(21)00306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sah R, Shrestha S, Mehta R, Sah SK, Raaban AR, Dharma K, Rodriguez-Morales AJ. AZD1222 (Covishield) vaccination for COVID-19: experiences, challenges and solutions in Nepal. Travel Med Infect Dis. 2021;40:101989. doi: 10.1016/j.tmaid.2021.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vouking MZ, Mengue CMA, Yauba S, Edengue JM, Dicko M, Dicko HM, Wiysonge CS. Interventions to increase the distribution of vaccines in Sub-Saharan Africa: a scoping review. Pan Afr Med J. 2019;32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, Setiawan AM, Rajamoorthy Y, Sofyan H, Mudatsir M. Acceptance of a COVID-19 vaccine in Southeast Asia: a cross-sectional study in Indonesia. Front Public Health. 2020;8. [DOI] [PMC free article] [PubMed] [Google Scholar]


