Abstract
Background
To enable services to be provided at a distance during the COVID-19 pandemic, outpatient pharmacy services in Australia underwent near-immediate reform by moving to telehealth, including telephone and video consults.
Objective
To investigate how telehealth was used in a metropolitan outpatient pharmacy setting before and after the start of the COVID-19 restrictions and the various influences on the uptake of phone and video modalities.
Methods
A multi-methods approach was used including: (1) quantifying administrative activity data between July 2019 to December 2020 and, (2) semi-structured interviews with key stakeholders (n = 34).
Results
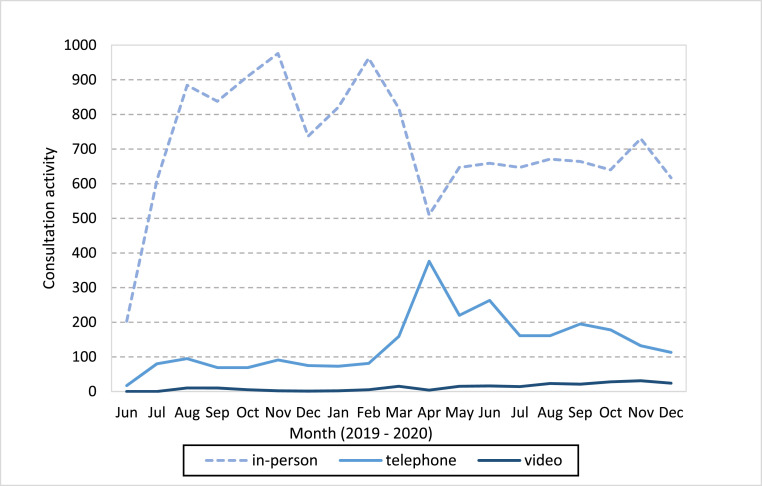
Activity data: Between July 2019 to December 2020 16,377 outpatient pharmacy consults were provided. Of these, 13,543 (83%) were provided in-person, 2,608 (16%) by telephone and 226 (1.4%) by video consult. COVID-19 impacted how these services were provided with telephone activity more than four-times higher in April 2020 than March 2020 and slight increases in video consults. Pharmacists have heavily favoured using the telephone despite the recommendation that video consults be used as the primary mode of contact and that telephone only be used when a video consult was not possible. As soon as COVID-19 restrictions eased, clinicians gradually returned to in-person appointments, maintaining some use of telephone and very limited use of video consult. Semi-structured interviews: Whilst clinicians recognised the potential benefits of video consults, challenges to routine use included the additional administrative and planning work required pre-consult, perceptions that patients were unable to use the technology, and the belief that in-person care was ‘better’ and that the telephone was easier.
Conclusion
Organisational strategies that encouraged the use of video over telephone (e.g. through financial incentives) did not appear to influence clinicians’ choice of care modality. Implementation studies are required to co-develop solutions to embed telehealth options into outpatient pharmacy settings that provide the best experience for both patients and clinicians.
Keywords: COVID-19, Telehealth, Videoconferencing, Outpatient pharmacist
Author contributions
Project conception: Dr Centaine Snoswell and A/Prof Michael Barras.
Procuring funding: Dr Centaine Snoswell.
Ethics and governance: Dr Centaine Snoswell and A/Prof Michael Barras.
Experimental design: Dr Centaine Snoswell.
Data collection: Monica Taylor and Dr Centaine Snoswell.
Data analysis: Dr Emma Thomas, Dr Soraia De Camargo Catapan, Dr Helen Haydon and Dr Centaine Snoswell.
Writing and editing the paper: Dr Emma Thomas, Dr Soraia De Camargo Catapan, Dr Helen Haydon, Dr Centaine Snoswell and A/Prof Michael Barras.
1. Introduction
Pharmacists play a key role in medication management both in hospitals and the community,1, 2, 3 and increasingly in outpatient specialist clinics.4 , 5 27 In 2020, Australia, like many countries, saw a rapid change in the way that healthcare was delivered, with many clinicians swapping in-person consultations for synchronous telehealth (telephone or video consults) to reduce the risk of COVID-19 transmission.6 , 7 Many outpatient pharmacy services underwent near-immediate reform as services were required to physically distance patients and staff, this meant changing in-person services to telehealth where appropriate.
Despite Government recommendations that video consults be used as the primary mode of telehealth contact and that telephone only be used when video consults were not possible,8 approximately 90% of all Australian telehealth consultations in 2020 (including general practitioners, allied health, specialist and nursing services) occurred using the telephone.9 While the long-term effects of these changes remain to be seen, the COVID-19 pandemic has presented an exceptional natural experiment where clinician adoption of telehealth can be observed.
In the 2019–2020 financial year, the Princess Alexandra Hospital (PAH) executive made a multi-million-dollar investment by adding new outpatient pharmacist roles across renal, cancer, mental health, surgery, general medical, and emergency medicine, as well as rehabilitation services. It was expected that the addition of a pharmacist to these teams would enhance medication compliance, prevent medication-related harm, and improve patient outcomes. This research was conducted as part of the overall evaluation for these clinical roles.27 , 28 This paper explores the changes to the modality of care across pharmacist outpatient clinics at a large metropolitan hospital during and immediately after the peak COVID-19 restrictions that occurred between March and May 2020 in Queensland, Australia. At this hospital, clinicians have access to telehealth support, software, and infrastructure to conduct video consults.
Using complimentary administrative activity data and qualitative interviews with pharmacists, their team leaders, managers, and other clinical staff from the outpatient clinics, this paper examines the influences on choosing the mode of delivery in lieu of in-person consultations. Specifically, this paper aims to: (1) determine the proportion of outpatient pharmacy appointments that were delivered via telephone and video consult before and after the start of the COVID-19 restrictions; and (2) understand the perceived clinician, service, and broader contextual challenges to using video consults within the outpatient pharmacy setting.
2. Method
To achieve the study aims, a multi-methods approach was used including administrative activity data analysis and semi-structured interviews with key stakeholders. Ethics approval for this study was obtained from the Metro South Human Research Ethics Committee (approval HREC/2020/QMS/61133). Verbal or written consent was provided by all participants. Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist guided the report qualitative findings (Appendix A).11
2.1. Setting
Participants were recruited from the PAH, in Brisbane, Australia. The PAH is a large metropolitan teaching hospital and prior to 2020 it conducted the highest annual volume of hospital telehealth consults in the state. Telehealth activity at the PAH is supported by a dedicated Telehealth Centre where equipment, consulting rooms, booking services, training and other assistance are available to all clinical services within the hospital. Reimbursement of outpatient services at this public hospital are primarily through the activity-based funding (ABF) model. ABF payments are dependent on the clinical classification (e.g. Tier 2), clinician provider type, service delivery mode and relative volume of activity provided by the hospital.10 In regard to delivering care via different modalities, a service delivered via telephone is reimbursed at a lower rate (approximately 80% less) than the provision of care via video consult or in-person.
2.2. Administrative activity data
Administrative activity data was collected retrospectively from June 2019 to December 2020 as part of the evaluation of the new outpatient pharmacist roles. The dataset collected included the number of outpatient pharmacist consultations delivered through different modalities (in-person, telephone or video consult), that were conducted in each calendar month, and combines both new and review (i.e. follow-up) consults. This period captures nine months before (June 2019–February 2020) and after (April 2020–December 2020) initial COVID-19 restrictions in Brisbane, Australia (March 2020). These data were used secondarily to compare (1) service volume, and (2) modality of care in the outpatient pharmacist departments. Descriptive data for pharmacist consultation activity was presented in a tabular and graphical format. For the pre- and post-COVID periods the total consults, mean monthly consults and standard deviation of monthly consult counts for each modality were calculated. These were compared using a t-test to test the hypothesis that the mean monthly consults for each modality were different in the post-COVID period compared to the pre-COVID period.
2.3. Semi-structured interviews
2.3.1. Participant recruitment
During March to May 2020, all pharmacists, their team leaders and managers, and other clinical staff (medical and nursing) from the outpatient clinics were invited to participate in an interview regarding the outpatient clinic pharmacist roles. Potential participants were approached (by author CS) through team meetings and staff emails, and any non-pharmacist clinicians were invited via active snowball sampling. The recruitment of non-pharmacists was to provide additional perspectives on the new pharmacist roles from non-pharmacy team members. Patients were not approached or invited to participate. No incentives to participate were provided. Recruitment ceased once data saturation was reached.
2.3.2. Interview data collection
All participants were sent an information and consent form, and a demographics questionnaire ahead of their interviews. If they were unable to return these prior to the interview, verbal consent was obtained at the start of the interview. Interviews were conducted in June–July 2020, via telephone, video conference, or in-person depending on the availability of the participant and in line with the physical distancing restrictions in effect at the time. An independent female research assistant (MT), who is experienced in qualitative research and works separately from the pharmacy department and was not known to the participants, conducted all interviews. No one else was present besides the participant and researcher. The full interviews explored the benefits, enablers and challenges of the new pharmacist outpatient roles. Interviews were expected to take 20–30 min, but generally ranged between 30 and 60 min (median 33:44 min). Repeat interviews were not carried out nor were transcripts or findings returned to the participants for comment. Here, we analyse a subset of questions related to a change in modality of care due to the COVID-19 pandemic. This subset comprised participant answers and comments related to the last two questions of the interview guide: (1) How have your outpatient clinics changed as a result of the COVID-19 pandemic? (Prompt: the physical distancing restriction); (2) Many services have swapped to telephone or video consult as a result of COVID-19 pandemic. Have you been using either of these? (Prompt: how was the transition? How has it been working? If not, why not?). Each interview was audio-recorded and transcribed verbatim.
2.3.3. Interview analyses
Interviews were audio recorded and automatically transcribed using Happy Scribe software (happyscribe.com). Transcripts were then checked for accuracy and deidentified by a member of the research team. As guided by Saldaña,12 the qualitative analysis was divided into two cycles of coding and an intermediate step. The choice of codes for each cycle was guided by the research question. In the first cycle, descriptive codes, which summarise data extracts into short words or phrases, were combined with structural codes, which compared the data back to the interview questions and either realigned or created new codes. After the first cycle, the codes were revised, adjusted, grouped and the main essence of the identified codes was described. In the second cycle of coding, we adopted the axial coding strategy to organise and reassemble data, selecting the best representative categories that corresponded to the two themes: 1) COVID-19 - the sudden disruptor, and 2) influences on choice of telehealth modality. Throughout the whole coding process, analytic memos (e.g. emerged patterns, code choice, inter-relations) were taken to enable a reflexive analysis on the data set.12 A sample of 15% and 30% of the data set were coded by two independent researchers to ensure that coding reflected consistent and appropriate interpretation. Four peer-debriefing and consensus meetings were conducted during the data analysis stage to discuss the developing themes, analysis process and data saturation. NVivo for Mac version 12.6 was used to organise data analyses.
2.3.4. Trustworthiness and rigour
According to Guba (1981),13 trustworthiness of qualitative research has four constructs: credibility, transferability, dependability and confirmability. Credibility of the study was enhanced by three of the authors (CS, SC, MB) being clinical pharmacists with hospital pharmacy expertise, two of which were employed by the study site (CS, MB). While these pharmacists were knowledgeable about the setting in which the study took place, they were not involved in clinical pharmacy activities at the time of the study. Transferability within the pharmacy setting can be enhanced by including other health professionals.14 This study involved 34 staff from 16 unique clinics and included pharmacists, team leaders, nurses, and doctors. The inclusion of a range of perspectives from different pharmacy clinics, disciplines and staff seniority enabled the collection of broader viewpoints. Dependability was ensured by employing an independent research assistant (MT) to conduct the interviews who was not a member of the hospital team or familiar with any of the participants. Likewise, analyse of the transcripts was undertaken by researchers independent of the pharmacy department (SC, ET). Confirmability was established through peer debriefing sessions as discussed above.
3. Results
3.1. Administrative activity data
Since the implementation of the new outpatient pharmacy services in June 2019 and December 2020, 16,377 consults were conducted (Table 1 ). Of these, 13,543 (83%) were provided in-person, 2,608 (16%) were provided by telephone and 226 (1.4%) by video consults. In the 9-months preceding the COVID-19 restrictions in Brisbane, Australia (June 2019 to February 2020) the total number of consults (7626) provided by the service did not differ greatly from the 9-months after the restrictions (7,760 consults conducted between April 2020–December 2020), however, the modality of care by which these consults were delivered changed. There were approximately 950 in-person consults in February 2020, dropping to about 500 in April 2020.
Table 1.
Monthly outpatient pharmacist consult activity by modality from June 2019 to December 2020.
| 2019 |
2020 |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Modality | Jun | Jul | Aug | Sep | Oct | Nov | Dec | Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep | Oct | Nov | Dec | Total |
| In-person | 203 | 610 | 884 | 838 | 910 | 976 | 737 | 821 | 962 | 817 | 510 | 647 | 659 | 647 | 671 | 664 | 640 | 730 | 617 | 13,543 |
| Telephone | 17 | 80 | 95 | 69 | 69 | 91 | 75 | 73 | 81 | 159 | 376 | 220 | 263 | 161 | 161 | 195 | 178 | 132 | 113 | 2,608 |
| Video consult |
0 |
0 |
10 |
10 |
5 |
2 |
1 |
2 |
5 |
15 |
4 |
15 |
16 |
14 |
23 |
21 |
28 |
31 |
24 |
226 |
| Total | 220 | 690 | 989 | 917 | 984 | 1,069 | 813 | 896 | 1,048 | 991 | 890 | 882 | 938 | 822 | 855 | 880 | 846 | 893 | 754 | 16,377 |
Prior to the COVID-19 restrictions (June 2019 to February 2020) the clinic pharmacists conducted a mean of 771 in-person consults, 72 telephone consults and 4 video consults per month (Table 2 ). After the restrictions eased this makeup shifted significantly to 643, 128 and 16 consults of each type per month (p ≤ 0.0001 for all three means).
Table 2.
Pre and post COVID comparison of mean monthly consults by modality.
| Pre-COVID |
Post-COVID |
Difference between means | p-value | |||
|---|---|---|---|---|---|---|
| Modality | Total consults | Mean consults per month (SD) | Total consults | Mean consults per month (SD) | ||
| In-person | 6941 | 771 (242) | 5785 | 643 (78) | 128 | 0.0001 |
| Telephone | 650 | 72 (23) | 1799 | 200 (76) | 128 | 0.0001 |
| Video consult |
35 |
4 (4) |
176 |
20 (8) |
16 |
0.0001 |
| Total | 7626 | 7760 | 272 | |||
During peak COVID periods, multiple clinics had to stop completely or pause for a period of time. These service interruptions were due to the vulnerability of their patient cohort, if exposed to COVID-19, or cancellations of non-urgent care within the hospital (e.g. elective surgery). Care that was categorised as urgent such acute orthopaedic assessment and treatment continued in-person with social distancing restrictions. Telephone activity was two-fold higher in March than February, and more than four-times higher in April, gradually reducing over time as in-person services resumed. While video consults increased from approximately 4 monthly consultations prior to March 2020, to approximately 20 monthly consultations between April to December, they only made up a very small proportion of total consultations (Fig. 1 ).
Fig. 1.
Monthly outpatient pharmacist service consults by modality from June 2019 to December 2020.
3.2. Semi-structured interviews
3.2.1. Participant demographics
Of the 34 staff interviewed, 68% were female, 74% were aged 31–50 years and the cohort was comprised of: 16 outpatient pharmacists, 9 pharmacist team leaders, 5 nurses (clinical nurses, diabetes specialised, or telehealth navigators) and 4 doctors (specialist consultants and registrars) (Table 3 ). The interviewees represented the 18 outpatient clinics who added a pharmacist to their team in mid-2019.
Table 3.
Participant demographics.
| Characteristic | Categories | Count, n=34 (%) |
|---|---|---|
| Gender | Female | 23 (68) |
| Age (years) | 21–30 | 6 (18) |
| 31–50 | 25 (74) | |
| >50 |
3 (9) |
|
| Health professional position | Pharmacist | 16 (47) |
| Pharmacist and team leader | 9 (26) | |
| Specialist consultant or registrar | 4 (12) | |
| Nurse (clinical nurse, registered nurse or telehealth nurse navigator) |
5 (15) |
|
| Highest level of education | Bachelor | 13 (38) |
| Graduate certificate | 8 (24) | |
| Graduate Diploma | 6 (18) | |
| Masters | 6 (18) | |
| PhD |
1 (3) |
|
| Years practicing as a pharmacist or other health professional | Less than 1 year | 1 (3) |
| 1–5 years | 8 (24) | |
| 6–10 years | 8 (24) | |
| 11–15 years | 9 (26) | |
| 16–20 years | 5 (15) | |
| 21+ years |
3 (9) |
|
| Area of specialty | Rehabilitation | 3 (9) |
| Medical | 9 (26) | |
| Surgical | 8 (24) | |
| Renal | 4 (12) | |
| Cancer | 5 (15) | |
| Other (emergency, immunology, mental health, misc.) | 5 (15) |
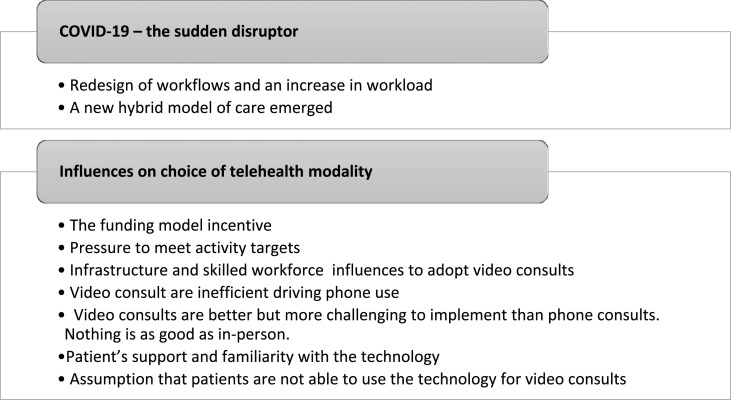
Two overall themes were identified and included: 1) COVID-19 - the sudden disruptor, and 2) influences on choice of telehealth modality. These themes along with their nine categories are listed in Fig. 2 and described in detail below with exemplars.
Fig. 2.
Overall themes and categories identified from the semi-structured interviews.
3.3. COVID-19 – the sudden disruptor
3.3.1. Redesign of workflows and an increase in workload
In some clinics, because of the urgency to provide alternative ways for in-person care, new workflows had to be developed often resulting in an increased workload. While many consultations were made at a distance, when a patient was acutely unwell and needed an in-person consultation, a COVID-safe clinic was set up. A triage process (determined by management) was adopted to assess which patients would come in-person to the clinic depending on the severity and risk of each case, keeping chronic and stable patients for phone reviews. Some pharmacists modified their roles, reducing their clinics to an ad hoc basis (i.e. only when requested) so they had capacity to support elsewhere across the hospital service when needed.
Decisions to offer telephone reviews meant that in some instances the pre-COVID access to multidisciplinary team (MDT) assessments were removed. In this model, phone reviews were only completed by the doctors; pharmacist and nurses were no longer part of the consultation.
Participant 24 - … we changed our way of practice to do phone conversations by the doctors. So, the pharmacists and nurse couldn't really participate much.
Other clinics tried to maintain patient-clinician contact with all the MDT, however, this created administrative challenges. From an administrative perspective, the shift to phone consults made it difficult to schedule MDT appointments. During in-person clinics, the patient either meets with the whole MDT at once or moves from one room to another seeing a different clinician. During phone appointments, however, this patient flow is disrupted, and if one clinician is delayed, the next cannot connect with the patient or the patient cannot determine which clinician they are consulting with at the time. Also, phone adoption was perceived to increase administrative workload, as it generates extra tasks (emailing lists, collecting contact information, calling other sources, etc.) demanding more time than in-person consultations.
Participant 18 - And there's a whole lot of admin associated with it at the other end. So, you know, having to, send stuff out to the [patient] just having to envelope up new med lists, and get their correct address. And so, there's a little bit of extra admin as well, I think.
3.3.2. A new hybrid model of care emerged
Correlating with the administrative activity data, interviewees described a sudden decrease in patient numbers for in-person visits during the peak COVID-19 restrictions. Even after COVID-19 restrictions were relaxed in Queensland (May 2020), several clinics continued with telephone and video consult modalities of care, according to patients' needs and the specificity of each clinic. These modalities enabled care commensurate with physical distancing requirements and the limited physical spaces in the hospital's waiting rooms. An approach wherein one in every three consults would be in-person, and the other two would be performed by video or telephone, was one of the strategies adopted to cope with social distancing and decrease the number of patients coming for in-person consultations.
Another model adopted by some chronic conditions’ specialities, such as oncology and haematology, was to offer monthly phone consults for patient reviews, followed by couriered medication for oral therapies. This model appeared to be appealing and convenient for patients. However, one interviewee emphasised that for that model to be sustainable, it must provide both a financial benefit for the health system, as well as benefit for the patients. After the experience with this model, one interviewee feared that some patients might resist returning to in-person care; a concept they appeared resistant to due to the financial costs.
Participant 27 – And as soon as they have to start coming into the hospital once a month, they're like ‘this is ridiculous’. That sort of thing. So, I don't know if the patients feel like. (…) they've had a taste of what the public system really could do if we had unlimited funding.
3.4. Influences on choice of telehealth modality
3.4.1. The funding model incentive
Interviewees showed an awareness that the ABF model employed at their hospital determined that telephone calls are reimbursed at a rate seven times less than video consults. The adoption of phone calls as an alternative for in-person appointments placed a challenge on clinicians to sustain their roles and keep funding to run clinics during the COVID-19 period. Prior to COVID-19 it was expected that each pharmacist would bring in enough funding to cover their new role, however, there was a sense that the clinicians would not be directly impacted on this lack of funding because of the unusual circumstances.
Participant 3 – It's a massive decrease in ABF [activity-based funding] funding associated with that but in all honesty, executive kind of indicated this was going to be expected. And that wouldn't be … it wouldn't be held … it wouldn't be held against us, effectively.
However, when video consults were used instead of phone consults the cited motivation was to increase revenue, as these attracted the same reimbursement as in-person while a telephone was approximately 10–20%. Some interviewees believed the actual reimbursement amounts for telephone was not commensurate with what is beneficial for patients during COVID-19 restrictions. Likewise, some interviewees expressed frustration with the pressure to conduct video consults instead of telephone calls. However, the activity data suggests that this did not overly impact the choice of care modality given telephone was the dominate telehealth choice.
Participant 1 - There was push to do more video conference, otherwise the role would not be sustainable.
3.4.2. Pressure to meet activity targets
The need to meet weekly activity targets (which are directly linked to funding) to sustain the new outpatient pharmacy role also had a direct influence on clinical pharmacist routine practice and the chosen modality of care. For instance, one clinician reported trying to make multiple phone calls at the end of the week even though the clinical benefit may have been minimal. Pharmacists started to change their practices to incorporate less complex or less time-consuming interactions over the phone. For instance, interviewees described that rather than performing comprehensive medication reviews they simply enquired about the side effects of a new medication. One pharmacist described their frustration with their choice for phone review for less complex cases due to the pressure to increase the number of consults and meet activity targets.
Participant 19 – [It is] not my proudest moment to say, ‘oh yeah I pick easy patients to review,’ but when you get to like, three o'clock on a Thursday and you're three patients behind your weekly target, you just do what you have to do, which I think is a real drawback to the structure of the service and of the funding model of the service.
3.4.3. Infrastructure and skilled workforce influences to adopt video consults
Infrastructure to conduct video consults was available at this hospital which was perceived as a positive influence on its adoption. Staff had access to software and hardware with peripherals, as well as technical and administrative support. A designated and equipped telehealth room was considered necessary, especially if it was within the clinic's premises, to facilitate MDT work. A prepared workforce, with technical knowledge and the ability to perform a video consult was also mentioned as an enabler.
Participant 4 - So it was just a matter of getting the patient on board to kind of figure out how to do stuff.
On the other hand, the lack of flexibility in the use of the infrastructure and varied workforce skill were also quoted as barriers by other clinic pharmacists. Interviewees highlighted the importance of using the required hospital-endorsed platform to virtually connect with their patients, to ensure high levels of data security and privacy. However, some discussed struggling to use the platform. They also indicated that the lack of adequate technical support and logistic hurdles was impeditive to the shift to video consults. For those clinics who preferred in situ telehealth, rather than using the PAH telehealth centre (purpose-built telehealth rooms at the basement of the hospital), there were, at times difficulties finding an appropriate space within the clinic to conduct video consults. Also, lack of infrastructure on the other end, either the patients' lack of resources, devices or limited facilities infrastructure in prison settings were also reported to hinder the adoption of video consults.
3.4.4. Video consult are inefficient driving phone use
At first, in the transitioning stage, it takes more time to set up a video consult than an in-person one. Without initial adequate support to make video consults part of an efficient routine, it would take more time and energy. There was a perception that video consults would take a lot longer to set up than phone consultations and was therefore not appropriate in time-critical consults. For example, in the outpatient preadmission clinic, patients needed reviews before scheduled surgeries. In the example below, the interviewee cited the need to wait for three days before being able to set up a teleconference.
Participant 1 - But because of the time-critical nature of some of these instructions, sometimes I didn't have the ability to wait three days to be able to set up a teleconference with the correct people.
Participant 19 - We have to book into rooms here [for video consults] and I just found it much easier doing it over the phone, despite the lack of funding.
Conversely, interviewees described phone consults as their main modality choice when they needed to conduct consults virtually, as it was perceived to be easy and ready to use.
Participant 5 - But a lot of the other times, I've tried to do video … the and the patient said ‘Oh no thanks. I'd just rather have the phone’.
One of the factors described as favourable to the rapid shift to phone consults instead of video is the ability to access medical records via integrated electronic medical records (ieMR). Before the widespread adoption of ieMR, video consults were more advantageous than phone consults as an effective and secure way for the pharmacist to confirm the patient's prescribed medication. The patient could display their medicine on screen and tell how they were taking it. The access to up-to-date medicine information on ieMR has withdrawn this advantage. One pharmacist mentioned that:
Participant 14 - I think eHealth records is making a huge difference in terms of how we carry out phone reviews. And I think it might be a reason why telehealth [video consults] in the past was valued more because you know you weren't able to do that over the phone. But now, like having access to someone's records, somewhat sort of lessens the need to have a telehealth review with a patient.
There was also evidence to suggest that the modality of care used by doctors had a flow-on effect for the broader clinic. This peer influence appeared to impact the pharmacists’ willingness to implement video consults if doctors were only using the telephone.
Participant 5 - I have found it hard to implement Telehealth if I'm the only one doing it. Because the doctors have just been switching everything to a phone review.
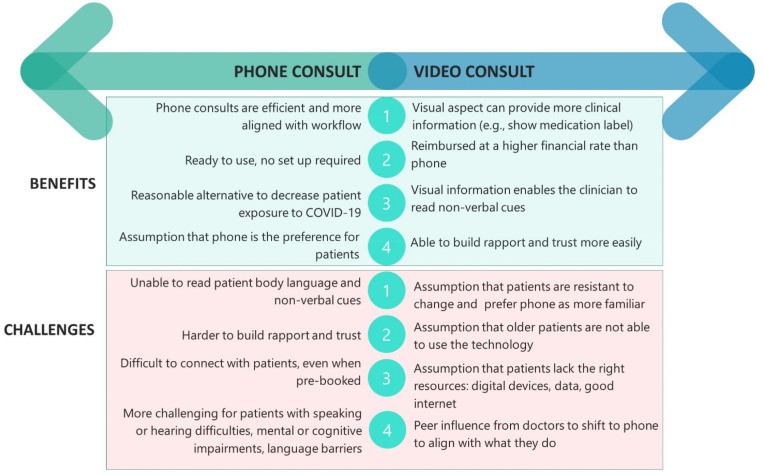
3.4.5. Video consults are better but more challenging to implement than phone consults. Nothing is as good as in-person
The overall opinions about different modalities of care differed. However, there did appear to be a developing hierarchy of effectiveness. Interviewees ranked video consults as more effective and sustainable than phone consults, but not as good as an in-person consult (Fig. 3 ). Although it was recognised that phone consults were a reasonable alternative to decrease potential exposure to COVID-19, interviewees described their limitations. For instance, the inability to visualise the patient, read their body language, and the increased difficulty to build rapport over the phone deemed phone calls as less effective than in-person consults.
Participant 34 - I mean, telephone interviews with mental health are useful but you know, it's not ideal either. We need to see the patient. Video link would have been a lot more sustainable.
Fig. 3.
Benefits and challenges of phone vs. video consults.
Interviewees also recognise the benefits when patients can observe their health care professional. Interviewees cited the importance of visual cues to establish a trustful relationship. Conversely, there is an implication that potential detachment in phone consultations make it easier for clients to end the call in a shorter amount of time.
Participant 21 - So I guess for mental health patients, phone reviews are difficult or harder to engage patients, as opposed to face to face. In particular because there's always intrinsic trust factors. A lot of patients with schizophrenia or schizophrenic, they, they may be paranoid and they don't know who you are. For them to disclose, to be more open about their concerns on medications or for abuse … to keep them on the phone for the same amount of time, sometimes could be difficult. And yeah. Yeah and there's harder to develop rapport over the phone as well.
Further, interviewees described the difficulty of connecting with their patients for phone consults, even when consults were pre-booked or scheduled in advance patients would not always answer or be free to talk. Additional patient-end challenges reported included patient hearing or communication difficulties, mental and cognitive impairments and those who spoke English as a second language and required an interpreter.
Despite these limitations of phone consults, they continued to be used at a much higher rate that video consults. The reason for this appeared to be largely due to the issues with implementation and ease of use. According to some interviewees, phone consults were more efficient, familiar, and easier than video consults.
Participant 32 - So, patients tend to like it [telephone reviews] because they don't have to come to hospital obviously, don't have to get parking … lots, lots of reasons … not having to hang around for ages, and it's quite efficient as well from our point of view. So, a lot of our job can be done from just looking at blood tests and talking to the patient. There's some things you can't do, but most times you can get away with just a phone review. So it is quite efficient. I quite like them.
3.4.6. Patient's support and familiarity with the technology
Patients require varying amounts of support to use the technology depending upon their familiarity with technology. In one of the endocrinology clinics, for example, patients were already using blood glucose readers and interacting with their health care professionals using an app before the COVID-19 pandemic. Consequently, for those patients the transition to follow-up video consults was smoother than other patients. Also, patients and professionals’ acceptability of video consults was attributed to the increased familiarity with video consults, resulting from the COVID-19 social distancing requirements.
The lack of technical onboarding support services to assist patients to setup a video consults, together with patient-end challenges with troubleshooting, was also mentioned as a barrier to adopting video consults. Queensland Health's website provides informative materials and direct line to support patients. However, often the technical support during the first contact using video remained with the health care professional, which adds an extra burden on them.
Participant 5 - But a lot of the other times, I've tried to do video … the patient wasn't able to troubleshoot it, or just changed their mind last minute. They said ‘Oh no thanks. I'd just rather have the phone’.
Participant 10 - We do rely probably on some of our patients with more significant cognitive impairments [to have] a family member or friend or someone that can facilitate the technology.
3.4.7. Assumption that patients are not able to use the technology for video consults
Some interviewees recognised that they might be underestimating the familiarity that older patients have with the technology and their ability to set up a video consult. Mostly, however, interviewees assumed that accessing video consults would be too difficult for their patients as a result of: the nature of their condition (i.e., mental health), their age, or cognitive impairment (patient eligibility). Further, there was a perception that older patients would not be able to use the technology.
P09 - Just the nature of the patients and being old and not able to use technology.
P24 – I guess because a large patient cohort status, that are all geriatric, they wouldn't be able to manage that. (…) So even if we booked a clinic with them initially, they agree. And yes, but there's no show, and often we have had a few occasions in the past year, which we think it's because of the patient age cohort. And also, they have limitations from family support. That's why it's not really practical for us to do any video consultation or anything high tech involved, for the geriatric type of patient.
Some clinicians stated that their patients had tried to use video consults and struggled, so they prefer to talk over the phone. Also, interviewees asserted that some patients do not have their own digital devices, enough data available and/or good connectivity to connect via video, and therefore they would still need to travel to use equipped facilities able to perform video consults, such as their local hospital or general practitioner.
4. Discussion
We investigated how telehealth was used in a metropolitan outpatient pharmacy setting before, during and after peak COVID-19 restrictions and the various influences on the uptake of phone and video modalities. In this setting, multiple factors were in place to support the use of video consults including the provision of technology, managerial support, and financial incentives that favoured the use of video over telephone. COVID-19 could have been the ‘perfect storm’ to accelerate video consult activity. Instead, what occurred was a rapid switch to the telephone and very limited use of video. The activity data demonstrates that as soon as COVID-19 restrictions eased, clinicians gradually returned to in-person appointments, maintaining some use of phone consults and very limited use of video consults. Australian data on other health professionals such as general practitioners also demonstrates a quick transition to telephone during the COVID-19 pandemic and limited uptake of video consults.7 Few studies, however, have begun to understand why this occurred and the various influences impacting upon clinicians' decisions. This study elucidates some of the perceived clinician and broader contextual challenges that led to the limited uptake of video consults including the additional administrative and planning work required, perceptions that patients were unable to use the technology, and the belief that in-person care was ‘better’.
Broader organisational influences to use telehealth appear to have a limited impact if clinicians are resistant or reluctant to use it. This phenomenon has previously been highlighted by Wade et al.15 , 16 A lack of clinician willingness can be further exacerbated by poor experiences with telehealth6 , 17 which reportedly occurred during the COVID-19 period given the rapid and unplanned transition. Fundamental to changing a clinician's behaviour and way of working must be a belief that the new way of working will provide additional benefit. Discussed another way by Abimbola et al.,18 is that the benefit of telehealth must outweigh the ‘transaction cost’ (i.e. the effort, time and costs required to complete a clinical interaction). This likely explains to some degree why telephone was so heavily favoured; the transaction cost was lower. Therefore, to increase use of video consults the process of delivering care remotely needs to be easier (e.g. simple for clinicians and patients to use, available technology, good connection and audio-visual quality) and the benefits made more obvious (e.g. improved care processes, patient satisfaction, improved access to patients and/or clinical outcomes). The best way of achieving this is likely though cooperative, participatory approaches that engage and work with clinicians, consumers, and administrators to determine where the telehealth value proposition lies.19 To get the most benefit out of these models of care, the designed digital solution (and workflows of use) should meet the needs of its intended users.20
The perceived relative advantage of telehealth differed between interviewees. Some pharmacists felt that telehealth offers opportunities to connect early with outpatient pharmacy patients and triage those at risk of medication errors and readmission. There were instances where clinicians persisted with using video consults even when the technology and infrastructure did not enable smooth experiences. These tended to be where clinicians perceived that the patient benefit would be high, and this benefit outweighed the additional effort required by the clinician. Examples included the preadmission clinic, mental health, and the diabetes clinics.
Reasons for different levels of uptake within the literature include; different visions, skills, fears, and opportunities, and being influenced by a diversity of intentions such as those to collaborate, solve problems, and improve efficiencies.21 In our study, the motivation of the clinician appeared to be strongly influenced by experiences of success and improved efficiencies (e.g. ensuring a patient being transferred from a correctional facility to hospital for surgery was well-prepared and necessary medications had been stopped avoiding a failed surgery and costly transfer). Further, it appeared that some practitioners were more motivated by financial incentives than others. Unsurprisingly, those in managerial positions that were required to directly report on activity numbers appeared more aware of the financial effects of activity, but this did not necessarily result in additional video consults (which attracted greater funding than phone). Previous studies have also identified a disconnect between policy pressures and actual use of video consults.22
The clinicians described how in their experience video consults led to new workflows and at times additional workload. They described issues with technology and this experience led to a belief that telehealth was less efficient than in-person care. There was also a reported increase in the administrative workload related to planning and supporting telehealth. The literature also supports that the use of both phone and video consults can increase workload.6 , 23 Additionally, since offering video consults was new for most pharmacists, learning the location of resources and infrastructure while providing ongoing care posed a challenge. These barriers did not exist in the same way for phone consults. In some instances, new ways of reorganising the service resulted in unintended consequences such as the exclusion of pharmacists from MDT appointments which were swapped to doctor-patient phone consults. The exclusion of the pharmacist from this patient consultation may have limited the early identification of medication-related issues. While telephone was described as easier to adopt, there was recognition that video consults would in many instances provide enhanced information that may lead to a better clinical outcome. In-person care, however, was viewed as the ‘gold-standard’ by many clinicians, aligned with other studies.24 Implementation of video consults into busy outpatient hospital settings has previously been described as complex and time-consuming25; the COVID-19 pandemic appeared to further exacerbate these challenges as the workflow and modality changes were required near-immediately.
There was a strong assumption that patients would not be able to use the technology. Strategies to support patients through the process (e.g. education, pre-testing, having a family member or support person) appeared limited. Clinicians also did not report routinely checking patients' access and confidence to using technology prior to determining the modality of care of the appointment. Rather, clinicians assumed accessing a video consult would be too difficult for older patients or for those with particular health conditions (e.g. cognitive impairment or mental health). These assumptions are not necessarily supported by the evidence with older patients being able to use telehealth innovations when supported.26
5. Strengths and limitations
This study was strengthened by the inclusion of multiple outpatient pharmacy clinics and stakeholder perspectives. The timing of the project also enabled a unique insight into what occurred before, during and after the peak COVID-19 restrictions. As the study was only conducted in hospital, findings may not be applicable to other settings. Additionally, the activity from the clinics varied between specialties. Further, the perspectives of consumers were not obtained which would have further strengthened the study. Some pharmacists described the selection of less complex patients for telephone and video consults. The pharmacist specialties and the routine activities they performed, such as medication history taking and medication counselling, have been described elsewhere.1 From the data available it was not possible to infer the pharmacists’ true motivations for changing their consult modality after the COVID restrictions commenced, although we expect that it was a complex interplay of patient complexity, pressure to meet key performance indicators and the local COVID-related social distancing policies.
6. Conclusion
Clinicians in the outpatient pharmacy setting discussed a hierarchy of preference of care modality as being in-person, then video, then telephone. However, the activity data showed a strong reliance on the telephone during the COVID-19 pandemic. Organisational strategies that encouraged the use of video over phone (e.g. through financial incentives) did not appear to influence clinician's choice of care modality. Despite not being able to see the patient, the telephone was reported to be easier to use (for both patients and clinicians), did not require a large change to the usual workflow, and aligned with what doctors were doing. Even though varying levels of support were needed for patients to transition to video depending on how familiar they were with technology, pharmacists discussed how patient capabilities were more assumed than known. In-person clinics are perceived as the best option for many clinicians and as physical distancing restrictions ease, clinicians are likely to gradually return to in-person modalities. Future studies should focus on quantifying patient benefits such as attendance rates between phone, video and in-person. Additionally, implementation studies are required to co-develop solutions to embed telehealth options into outpatient pharmacy settings that provide the best experience for both patients and clinicians.
Funding source statement
The study is funded by an early career researcher grant awarded to Dr Centaine Snoswell from The University of Queensland. Dr Emma Thomas is supported by a Postdoctoral Fellowship (#105215) from the National Heart Foundation of Australia.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank Monica Taylor for her assistance with conducting the interviews and for the Princess Alexandra Hospital Decision Support Unit who provided activity data.
Footnotes
Disclosure Statement / Conflict of interest: None to report.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sapharm.2022.02.003.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.Hume A.L., Pharm D., Kirwin J., et al. Improving care transitions : current practice and future American college of clinical pharmacy. Pharmacotherapy. 2012;32(11):326–337. doi: 10.1002/phar.1215. [DOI] [PubMed] [Google Scholar]
- 2.Tong E.Y., Roman C.P., Mitra B., et al. Reducing medication errors in hospital discharge summaries: a randomised controlled trial. Med J Aust. 2017;206(1):36–39. doi: 10.5694/mja16.00628. [DOI] [PubMed] [Google Scholar]
- 3.Wheeler A.J., Scahill S., Hopcroft D., Stapleton H. Reducing medication errors at transitions of care is everyone's business. Aust Prescr. 2018;41(3):73–77. doi: 10.18773/austprescr.2018.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hawes E.M., Maxwell W.D., White S.F., Mangun J., Lin F.C. Impact of an outpatient pharmacist intervention on medication discrepancies and health care resource utilization in posthospitalization care transitions. J Prim Care Commun Heal. 2014;5(1):14–18. doi: 10.1177/2150131913502489. [DOI] [PubMed] [Google Scholar]
- 5.Al-Qudah Msc R.A., Al-Badriyeh D., Al-Ali F.M., Altawalbeh S.M., Basheti I.A. Cost-benefit analysis of clinical pharmacist intervention in preventing adverse drug events in the general chronic diseases outpatients. J Eval Clin Pract. 2020;26:115–124. doi: 10.1111/jep.13209. [DOI] [PubMed] [Google Scholar]
- 6.Smith A.C., Thomas E., Snoswell C.L., et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020;26(5):309–313. doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Snoswell C.L., Caffery L.J., Haydon H.M., Thomas E.E., Smith A.C. Telehealth uptake in general practice as a result of the coronavirus (COVID-19) pandemic. Aust Health Rev. 2020;44(5):737–740. doi: 10.1071/AH20183. [DOI] [PubMed] [Google Scholar]
- 8.Australian Government, Department of Health Temporary COVID-19 MBS telehealth services – factsheet. Medicare Benefits Sched. 2020;(July):1–16. [Google Scholar]
- 9.Mehrotra A., Bhatia R.S., Snoswell C.L. Paying for telemedicine after the pandemic. JAMA. 2021;325(5):431–432. doi: 10.1089/tmj.2020.0176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Independent Hospital Pricing Authority Activity based funding. What we do. https://www.ihpa.gov.au/what-we-do/activity-based-funding# Published 2019. ∼:text=Activity Based Funding (ABF) is,patients%2C it receives more funding.
- 11.Booth A., Hannes K., Harden A., Noyes J., Harris J., Tong A. In: Guidelines for Reporting Health Research : A Users Manual. Moher D., Altman D.G., Schulz K.F., Simera I., Wager E., editors. John Wiley & Sons Ltd.; 2014. COREQ (consolidate criteria for reporting qualitative studies) pp. 214–226. [DOI] [Google Scholar]
- 12.Saldaña J. In: The Coding Manual for Qualitative Researchers. 3 ed. Seaman Jai., editor. SAGE Publications Ltd.; 2016. [Google Scholar]
- 13.Guba E.G. Criteria for assessing the trustworthiness of naturalistic inquiries. Educ Commun Technol ERIC/ECTJ Annu Rev Pap. 1981;29(2):75–91. [Google Scholar]
- 14.Amin M.E.K., Nørgaard L.S., Cavaco A.M., et al. Establishing trustworthiness and authenticity in qualitative pharmacy research. Res Soc Adm Pharm. 2020;16(10):1472–1482. doi: 10.1016/j.sapharm.2020.02.005. [DOI] [PubMed] [Google Scholar]
- 15.Wade V.A., Eliott J.A., Hiller J.E. Clinician acceptance is the key factor for sustainable telehealth services. Qual Health Res. 2014;24(5):682–694. doi: 10.1177/1049732314528809. [DOI] [PubMed] [Google Scholar]
- 16.Wade V.A., Taylor A.D., Kidd M.R., Carati C. Transitioning a home telehealth project into a sustainable, large-scale service: a qualitative study. BMC Health Serv Res. 2016;16(1):1–10. doi: 10.1186/s12913-016-1436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas EE, Haydon HM, Mehrotra A, et al. Building on the momentum: sustaining telehealth beyond COVID-19. J Telemed Telecare. Published online 2020. doi:10.1177/1357633X20960638. [DOI] [PubMed]
- 18.Abimbola S., Keelan S., Everett M., et al. The medium, the message and the measure: a theory-driven review on the value of telehealth as a patient-facing digital health innovation. Health Econ Rev. 2019;9(1) doi: 10.1186/s13561-019-0239-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dixon-Woods M., Amalberti R., Goodman S., Bergman B., Glasziou P. Problems and promises of innovation: why healthcare needs to rethink its love/hate relationship with the new. BMJ Qual Saf. 2011;20(Suppl.1):47–51. doi: 10.1136/bmjqs.2010.046227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clemensen J., Rothmann M.J., Smith A.C., Caffery L.J., Danbjorg D.B. Participatory design methods in telemedicine research. J Telemed Telecare. 2017;23(9):780–785. doi: 10.1177/1357633X16686747. [DOI] [PubMed] [Google Scholar]
- 21.Orlikowski W.J. Using technology and constituting structures: a practice lens for studying technology in organizations. Organ Sci. 2000;11(4):404–428. doi: 10.1287/orsc.11.4.404.14600. [DOI] [Google Scholar]
- 22.Brant H., Atherton H., Ziebland S., McKinstry B., Campbell J.L., Salisbury C. Using alternatives to face-to-face consultations: a survey of prevalence and attitudes in general practice. Br J Gen Pract. 2016;66(648):e460–e466. doi: 10.3399/bjgp16X685597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Newbould J., Abel G., Ball S., et al. Evaluation of telephone first approach to demand management in English general practice: observational study. BMJ. 2017;358 doi: 10.1136/bmj.j4197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O'Cathail M., Ananth Sivanandan M., Diver C., Patel P., Christian J. The use of patient-facing teleconsultations in the national health service: scoping review. JMIR Med Informatics. 2020;8(3) doi: 10.2196/15380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Greenhalgh T., Shaw S., Wherton J., et al. Real-world implementation of video outpatient consultations at macro, meso, and micro levels: mixed-method study. J Med Internet Res. 2018;20(4) doi: 10.2196/jmir.9897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quinn C.C., Shardell M.D., Terrin M.L., et al. Mobile diabetes intervention for glycemic control in 45- to 64-year-old persons with type 2 diabetes. J Appl Gerontol. 2016;35(2):227–243. doi: 10.1177/0733464814542611. [DOI] [PubMed] [Google Scholar]
- 27.Snoswell Centaine L., De Guzman Keshia, Barras Michael. Pharmacists reducing medication risk in medical outpatient clinics: a retrospective study of 18 clinics. Intern Med J. 2021 doi: 10.1111/imj.15504. [DOI] [PubMed] [Google Scholar]
- 28.Snoswell Centaine L., Draper Megan J., Barras Michael. An evaluation of pharmacist activity in hospital outpatient clinics. J Pharm Pract Res. 2021;51(4):328–332. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.