Abstract
Background
Limited in-person visits during the COVID-19 pandemic, with liberal reimbursement policies, resulted in increased use of video conferencing (hereby described as telehealth) for patient care. To better understand the impact on pediatric surgeons and their patients, we surveyed members of the American Pediatric Surgical Association (APSA) regarding telehealth use prior to and during the pandemic.
Methods
:An iteratively developed survey was sent to all active, non-trainee surgeons within APSA during March 2021.
Results
Of 247 responses (23% response rate), 154 (62%) began using telehealth during the pandemic. In addition to the 101 (60.5%) respondents who felt telehealth had a positive impact on their clinical practice, 161 (74.2%) felt that it had a positive impact on their patients’ satisfaction. The most common barriers to telehealth use prior to COVID-19 were availability of technology (39.3%), patient access to technology (36.0%), and lack of reimbursement (32.0%). These barriers became less substantial during the pandemic. Most respondents (95.3%) indicated they would continue using telehealth post-pandemic if it remains appropriately reimbursed.
Conclusions
The majority of pediatric surgeons implemented telehealth during the COVID-19 pandemic and endorsed a positive effect on their clinical practice as well as on patient satisfaction. An overwhelming majority would continue using this technology if reimbursement policies remain favorable.
Keywords: COVID-19, Telehealth, Reimbursement, Public policy, Patient satisfaction
Abbreviations: COVID-19, coronavirus disease 2019; APSA, American pediatric surgical association; AAP, American academy of pediatrics; IQR, interquartile range; CMS, centers for medicare & medicaid services; HHS, health and human services; HPIAA, health insurance portability and accountability act
1. Introduction
Over the last two decades, telehealth, defined as two-way audiovisual communication to deliver health care services, has increased access to care for underprivileged populations and others who have barriers to traditional care models [1]. While telehealth has existed since the late 1950s, many challenges have limited its usefulness in daily practice [2]. Some of those challenges include access to technology, malpractice concerns, and limitations in the ability to perform comprehensive physical exams. Despite telehealth care commanding similar clinician resources and time as in-person care, and possibly improving the care of patients, Medicare/Medicaid and many commercial insurance companies have been unwilling to reimburse telehealth care altogether, or instead, reimburse telehealth at lower rates than in-person care.
The COVID-19 pandemic led to a rapid increase in telehealth utilization to limit unnecessary person-to-person interactions and spread of disease while maintaining access to healthcare systems and providers. Legislation was expeditiously approved nationally to temporarily ensure similar rates of reimbursement for telehealth as in-person visits [3]. While studies in adult populations demonstrated that expanded telehealth reimbursement led to improved access and patient satisfaction, data evaluating outcomes among pediatric populations is limited [4], [5], [6]. We therefore surveyed the American Pediatric Surgical Association (APSA) general membership to determine (1) how telehealth was utilized prior to and during the COVID-19 pandemic among pediatric surgeons, (2) the impact of telehealth on clinical practice, and (3) how clinicians view the impact of telehealth on patient satisfaction. Furthermore, we attempted to identify mechanisms for professional organizations such as APSA and the American Academy of Pediatrics (AAP) to support future telehealth use in pediatric surgery.
2. Methods
2.1. Survey development
Survey development followed previously published APSA protocols [7]. A panel to develop and review the survey was formed including members from the Division of Pediatric Surgery at Rush University Medical Center and members from the AAP Delivery of Surgical Care Committee. The initial meeting focused on developing the aims of the survey including: (1) to determine the clinician-perceived impact of telehealth on their practice as well as on their patients, (2) to determine barriers to implementation of telehealth, and (3) to determine how professional organizations such as APSA and AAP could support the implementation and utilization of telehealth.
Based on these aims, a descriptive survey was iteratively developed using SurveyMonkey (San Mateo, CA, Appendix). The survey was subsequently reviewed and approved by the APSA Outcomes Committee. Once the survey was developed, institutional review board approval was obtained from Rush University Medical Center (IRB#: 21,012,503-IRB01). To improve the survey response rate, all interested respondents could opt into a raffle for a $150 online gift certificate. No personal health information or identifiable information was collected as part of the survey, except for the optional disclosure of an e-mail address used for the raffle. This identifiable information was maintained separately from the remaining survey data used in subsequent analyses. APSA trainee members were excluded as their telehealth utilization would reflect practices employed by their attending staff, and, therefore, may have led to duplicated and skewed results.
2.2. Survey validation
The survey was validated utilizing two methods. The first was an attempt to ensure test-retest reliability by sending the survey twice to a small group of pediatric surgeons (n = 5) roughly 1 month apart to ensure that their responses did not change over time. The second method was an attempt to ensure that there were no issues with survey comprehension or literacy. For this, the survey was sent to members of the APSA Outcomes Committee who had not been involved in survey development. These external reviewers were provided an opportunity to take the survey and provide open commentary regarding additional concerns and recommendations.
2.3. Variables and statistical analysis
As there is a large amount of variation in the definition of an “academic” practice, we used “working with residents” as an approximation of working in an academic setting. Practice setting was defined as rural (<10,000 people), suburban (10,000–100,000 people), and urban (>100,000 people). Salary type was also broken down as purely salaried, fee-for-service, or mixed model. The diagnoses appropriate for telehealth and the barriers to telehealth utilization were chosen by the panel a priori based on commonly utilized pediatric surgical procedures and commonly discussed barriers to telehealth utilization. These selections were then edited by the APSA Outcomes Committee. Most questions also had an open-ended section for free text responses. The survey was initially disseminated on March 1, 2021. Reminders were sent on March 16, 2021 and March 24, 2021. Standard summary statistics were used to describe all responses among all respondents. Missing data was dropped from the analysis for the specific question involved (not for all responses from the individual). R (version 4.0.2, R Foundation for Statistical Computing, Vienna, Austria) was used to compile and report all results.
3. Results
3.1. Demographics
The survey was sent to 1060 individuals identified as regular members of APSA. Of 250 respondents, 247 consented and were included in final analyses (response rate: 23.3%). The vast majority of the respondents were based in the United States (n = 220, 89.1%) and the median time from training completion was 11 years (interquartile range [IQR]: 6, 22, Table 1 ). The overwhelming majority were academic (n = 213, 89.5%). Most respondents were purely salaried (n = 168, 68.0%) as opposed to fee-for-service (n = 9, 3.6%) or mixed model (n = 51, 20.6%).
Table 1.
Baseline demographics of survey respondents.
| Variable | Outcome |
|---|---|
| N | 247 |
| Years Since Fellowship | 11 (6, 21.8) |
| Primary Practice Location (Country) | |
| North America (Not US) | 11 (4.5%) |
| Outside of North America | 7 (2.8%) |
| United States | 220 (89.1%) |
| Unknown | 9 (3.6%) |
| Practice Involving Residents | 213 (89.5%) |
| Practice Setting Type | |
| Rural (<10,000 people) | 1 (0.4%) |
| Suburban (10,000 - 1000,000 people) | 79 (32.0%) |
| Urban (>1000,000 people) | 158 (64.0%) |
| Unknown | 9 (3.6%) |
| Percentage of Patients on Medicaid | 50% (40%, 65%) |
| Percentage of Patients where English is Not First Language | 20% (10%, 30%) |
| Salary Type | |
| Fee-for-service | 9 (3.6%) |
| Mixed | 51 (20.6%) |
| Purely salaried | 168 (68.0%) |
| Other | 6 (2.4%) |
| Unknown | 13 (5.3%) |
Continuous variables are recorded as median (interquartile range) while categorical variables are listed as frequency (percentage).
3.2. Use of telehealth
Only 49 (19.8%) respondents endorsed using telehealth prior to the COVID-19 pandemic, while 154 (62.3%) began using telehealth during the pandemic. A small number, 20 (8.1%), never used telehealth either before or after the pandemic began. Lastly 24 (9.7%) respondents left that question blank. Among those using telehealth prior to the pandemic, the vast majority used it for some post-operative visits (n = 41, 87.2%) and some long-term follow-ups (n = 39, 83.0%) as compared to some initial consults (n = 28, 60.9%). However, these clinicians only used it for a small number of these visits (a median of 10% [IQR: 5%, 20%] of post-operative appointments, a median of 5% [IQR: 0%, 5%] of initial consults and a median of 5% [IQR: 1%, 10%] of long-term follow-ups). Since the pandemic began, among those using telehealth, the median percentage of post-operative visits seen via telehealth was 30% (IQR: 10%, 60%); 10% (IQR: 5%, 25%) for initial consults, and 20% (IQR: 5%, 40%) for long-term follow-ups.
3.3. Diagnoses appropriate for telehealth
The most common diagnoses pediatric surgeons were willing to see via telehealth for the initial consult did not necessarily require a physical exam, such as cholelithiasis (55.1% [n = 136]), and port-a-cath placement (51.8% [n = 128], Table 2 ). Conversely, only 41.7% (n = 103) of respondents would see a hernia consult via telehealth, while 23.9% (n = 59) said they would not. Other diagnoses respondents said they would see for initial consults included fetal counseling (n = 18), gastrostomy tubes/reflux (n = 12), umbilical issues (n = 7), routine lumps/bumps (n = 11), and hormonal implants (n = 7). Other diagnoses respondents said they would NOT see included undescended testicles (n = 15), anorectal malformations (n = 5), pilonidal disease (n = 3), soft tissue masses (n = 6), or any patient with complex medical problems (n = 3).
Table 2.
Diagnoses that pediatric surgeons are willing to see and those that they are not via telehealth for the initial consult.
| Diagnosis | Okay for Telehealth | Not Okay for Telehealth |
|---|---|---|
| Cholelithiasis | 136 (55.1%) | 10 (4.0%) |
| Ports | 128 (51.8%) | 4 (1.6%) |
| Congenital Lung Malformations | 105 (42.5%) | 24 (9.7%) |
| Hernias | 103 (41.7%) | 59 (23.9%) |
| Pectus Excavatum | 94 (38.1%) | 20 (8.1%) |
3.4. Barriers to telehealth utilization
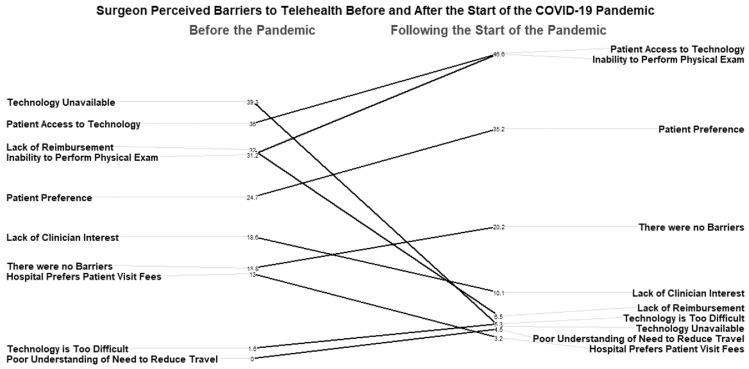
When evaluating barriers to the use of telehealth prior to the pandemic, unavailability of technology (n = 97, 39.3%), patient access to technology (n = 89, 36.0%), lack of reimbursement (n = 79, 32.0%), and inability to perform physical exam (n = 77, 31.2%) were among the most frequent barriers identified (Fig. 1 ). After the beginning of the COVID-19 pandemic, the dominant barriers to telehealth utilization were inability to perform a physical exam (n = 115, 46.6%), patient access to technology (n = 115, 46.6%), and patient preference (n = 87, 35.2%). Notably, the lack of reimbursement as a barrier to telehealth utilization dropped in importance from being identified by 32.0% (n = 79) of respondents prior to the pandemic to only 6.5% (n = 16) after. Lack of technology availability also dropped as a barrier to telehealth utilization from 39.3% (n = 97) prior to the start of the pandemic to only 4.9% (n = 12) afterward.
Fig. 1.
Slope chart demonstrating surgeon identified barriers to telehealth prior to and after the start of the COVID-19 pandemic.
3.5. Effects of telehealth on clinical practice
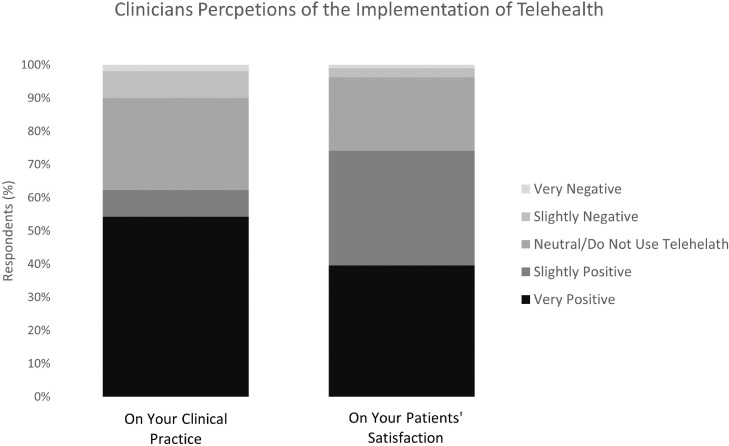
When investigating the effects of telehealth implementation on clinical practice, 60.5% (n = 101) of respondents said telehealth had a very positive or slightly positive impact on their clinical practice (Fig. 2 ). Only 9.9% (n = 16) of respondents felt that telehealth had a slightly negative or very negative effect on clinical practice. The positive impact on clinical practice was based on decreased exposure to infectious diseases (example: COVID-19, n = 134, 54.3%, Table 3 ), more flexible scheduling (n = 106, 42.9%), clinic efficiency (n = 71, 28.7%), less clinic “no shows” (n = 67, 27.1%), and less travel for multi-institutional surgeons (n = 63, 25.5%). With regards to negative effects on clinical practice, the most common reasons were difficulties with technology (n = 152, 61.5%) and the inability to diagnose or treat owing to the lack of a physical exam (n = 112, 45.3%).
Fig. 2.
Clinician perceptions of the effect of telehealth on clinical practice and patient satisfaction.
Table 3.
Surgeon perceived positive and negative effects on clinical practice and patient experience.
| What effects have you seen from the implementation of telehealth on your clinical practice? |
|||
|---|---|---|---|
| Positive Effects | Negative Effects | ||
Administrative
|
71 (28.7%) 46 (18.6%) 17 (6.9%) 106 (42.9%) 67 (27.1%) 26 (10.5%) 63 (25.5%) 31 (12.6%) 134 (54.3%) |
Administrative
|
152 (61.5%) 50 (20.2%) 60 (24.3%) 72 (29.1%) 112 (45.3%) 66 (26.7%) 33 (13.4%) 49 (19.8%) |
| What effects have you seen from the implementation of telehealth on your patients? | |||
| Positive Effects | Negative Effects | ||
Patient Quality of Life
|
153 (61.9%) 6 (2.4%) 160 (64.8%) 69 (27.9%) 104 (42.1%) 168 (68.0%) 99 (40.1%) 171 (69.2%) |
Barriers to Care
|
161 (65.2%) 59 (23.9%) 73 (29.6%) 83 (33.6%) 60 (24.3%) |
ER - Emergency Room. COVID – Coronavirus Disease.
3.6. Effects of telehealth on patient satisfaction
With regards to the clinician's perception of their patient satisfaction of care, 74.2% (n = 161) reported that telehealth had a very positive or slightly positive effect on patient satisfaction, while only 3.7% (n = 8) felt that the effect was slightly negative or very negative. From the clinician's perspective, positive effects on patients were reduced exposure to other patients (69.2%, n = 171), less impact on patients’ days (such as time off work, 68.0%, n = 168), less money and/or time spent on transportation/parking (64.8%, n = 160), and ease of scheduling appointments (61.9%, n = 153). Once again, difficulty on the patients’ side with using technology (65.2%, n = 161) contributed to the negative impact of telehealth adoption.
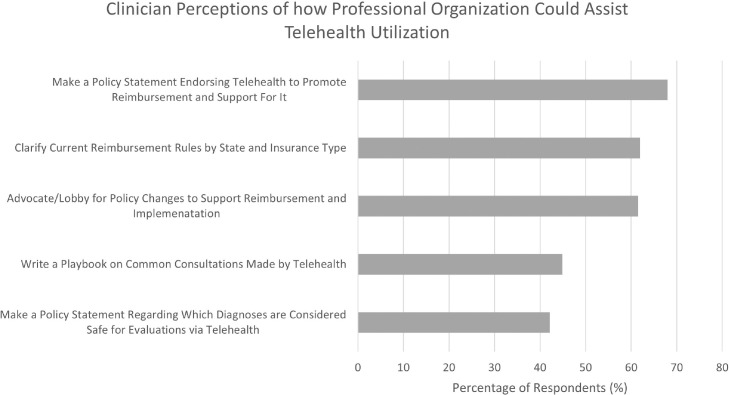
3.7. Preferred professional organization involvement
When asked how professional organizations such as APSA and AAP could reduce barriers to telehealth utilization, 68.0%, (n = 168) of respondents recommended a policy statement endorsing telehealth to promote reimbursement and support (Fig. 3 ). More than half of respondents also supported clarifying reimbursement rules by state and insurer type (61.9%, n = 153) and advocating for policy changes to support reimbursement and implementation (61.5%, n = 152). Writing a guide surrounding best practices for common telehealth consultations (44.9%, n = 111) and making a policy statement regarding safe diagnoses to make via telehealth (42.1%, n = 104) were less commonly selected. Other additional free text recommendations included supporting research into telehealth effectiveness (n = 1) and improving patient access to technology (n = 3). Lastly a few respondents mentioned the importance of a practice-wide discussion regarding the use of telehealth across state lines, both with regards to limiting the “poaching” of patients as telehealth expands, but also allowing easier use across state lines without needing a permit in the other state.
Fig. 3.
Clinician perceptions of how professional organizations could help reduce barriers to telehealth.
3.8. Future of telehealth utilization
Lastly, the vast majority of respondents (95.3%, n = 205) indicated they would continue to use telehealth after the pandemic ended if it remained reimbursable. Among these respondents, a median of 15% (IQR: 10%, 25%) of initial consults would be seen via telehealth, 50% (IQR: 25%, 75%) of post-operative follow-ups, and 30% (IQR: 16%, 50%) of long-term follow-up patients.
4. Discussion
This is the first study to survey pediatric surgeons on their attitudes on the rapid adoption of telehealth during the COVID-19 pandemic. While many studies have shown that telehealth in pediatric surgery is feasible, the widespread application of telehealth was limited prior to the COVID-19 pandemic [8], [9], [10]. The highly specialized nature of pediatric surgery combined with a limited number of physicians often concentrated in urban locations support that pediatric surgery is an optimal field for telehealth. In this study, we found that following the start of the pandemic, most pediatric surgeons began using telehealth. Furthermore, the use of telehealth has had an overwhelmingly positive impact on clinical practice and perceived patient satisfaction. Furthermore, 95% of surgeons would continue using telehealth if it remained appropriately reimbursed, demonstrating the need for policy changes to support this practice.
Most of the literature surrounding telehealth utilization in surgical specialties has focused on post-operative visits, visits with established patients, and counseling of patients [11]. This survey demonstrates that physicians still prefer in-person visits for conditions that require a physical exam to accurately diagnose patients. Examples included hernias, undescended testicles, and anorectal malformations. Surgeons appear to be more comfortable using telehealth when the physical exam is less critical in treatment decision making, such as cholelithiasis or port-a-cath placement. As technology improves and alternate models of telehealth mature, current limitations in physical examination may be addressed and allow surgeons to more comfortably use it for a broader expanse of diagnoses. For example, joint telehealth sessions while a patient is physically with a non-surgical clinician (e.g., primary care physician or advanced care provider) who are able to communicate physical exam findings in real-time with a surgeon may be a viable model to improve access and overall system efficiency. Interestingly, many existing payment structures reimburse at higher levels based on enumeration of thorough physical exams, leading practitioners to superfluously examine body parts that have little impact on the consultation diagnosis. More contemporary reimbursement is focused more on medical decision making and patient discussions, which may align well with the ability to fully renumerate telehealth visits.
At the start of the COVID-19 pandemic, the Centers for Medicare and Medicaid services (CMS) issued a temporary and emergency relaxation of telehealth rules via the 1135 waiver and the Coronavirus Preparedness and Response Supplemental Appropriations Act. This waiver established equivalent reimbursement for video telehealth visits and traditional in-person visits [3]. Additionally, the Health and Human Services (HHS) Office for Civil Rights relaxed enforcement of software-based violations of the Health Insurance Portability and Accountability Act (HIPAA) [12]. Combined, these efforts paved the way for clinicians to increase their use of telehealth, reducing a barrier to care that likely should have been implemented prior to the pandemic. Some states, such as Illinois, have already realized the importance of this legislation outside this emergency time-period and have made these changes permanent [13].
Several other barriers to telehealth use that were noted prior to the pandemic have diminished. The largest barriers to telehealth prior to the pandemic in addition to reimbursement included institutional unavailability of technology and difficulty with patient access to technology. Patient/family comfort with the use of technology for healthcare after the start of the pandemic may be reflective of increased utilization of video-based platforms in other aspects of life including school, work, and personal/social connections. Additionally, it is possible that once practitioners were forced to use this technology, benefits were realized that expanded its use. These theories are supported by other studies of telehealth implementation outside of pediatric surgery. Madden et al. surveyed providers of prenatal care visits early in the COVID-19 pandemic. They found large support with regards to convenience of telehealth for themselves and their patients, and the vast majority were motivated to continue using the technology in the future. However almost 40% felt that prior to the pandemic, they had no motivation to utilize this technology [14]. Furthermore the respondents felt that the technology was easy to implement, and there was not a substantial time spent learning how to use it.
While numerous studies have demonstrated patient satisfaction of telehealth, [8,10,11,[15], [16], [17], [18] our study addressed the clinicians’ perception of patient satisfaction. Like previous findings, respondents in our survey reported an overall positive perception on patient experience for ease of seeing the provider. Perhaps most importantly, it was felt patients could spend less money and time away from family/work and on transportation and parking, a finding supported by previous research [19]. These, and other barriers, may disproportionally affect patients and families from lower socioeconomic means, compounding the importance of increasing access to telehealth for pediatric patients. Telehealth utilization is also theoretically important for expanding access to specialized pediatric surgical care for patients in more rural areas [20,21].
At the request of the AAP Delivery of Surgical Care Committee and the APSA Outcomes Committee, we included a section in this survey of what clinicians thought the appropriate role of professional organizations is with regards to telehealth. The most commonly recommended actions were to develop policy statements endorsing telehealth and to advocate for policy changes to support telehealth reimbursement. This was followed closely by clarifying reimbursement by state and insurance type. These responses indicate a strong desire for professional organizations to help permanently reduce the financial barriers to telehealth, and to keep clinicians alerted to when those barriers return after the pandemic. As noted earlier, reimbursement was a major barrier to telehealth utilization prior to the pandemic, but emergency legislation diminished this barrier virtually overnight. As more than 90% of pediatric surgeons indicated they would like to continue using telehealth after the pandemic, professional organizations should view this specific request as a call to arms to assist.
An interesting answer also arose from the free text section regarding the role of professional organizations in regard to telehealth. There appeared to be concern regarding the use of telehealth across state lines. On one side of the issue, a respondent was concerned that other institutions would start “poaching” his/her patients. Alternatively, another wanted more clarity on the legality of using the technology across state lines when the practitioner was not certified in that state. Clearly this is an area of active discussion, and one that will need further dialogue in the future.
Our study has several limitations. First, our response rate was only 23%. Most APSA surveys have historically had similar response rates [22,23]. We attempted to increase response rates by offering a raffle for a $150 gift certificate, although it appears to have had little benefit. Second, we asked clinicians about their views of patient satisfaction but we did not perform a separate patient-facing survey. We therefore can only infer their satisfaction based upon clinicians’ viewpoints. We plan to perform a similar study on patients in the future. Lastly, a survey instrument, while useful, does not provide actual objective evidence with regards to changes in barriers to care such as money and time spent on visits or other parameters. Nonetheless, this survey provides a holistic view of changes in telehealth utilization practices by pediatric surgeons in the setting of the COVID-19 pandemic.
5. Conclusion
In this study, we have demonstrated that the implementation of telehealth during the COVID-19 pandemic has had a largely positive impact on both pediatric surgeons and perceived patient satisfaction. The reduction in barriers to utilization, specifically reimbursement and access/availability of technology, led to large increases in telehealth use. More than 90% of pediatric surgeons stated they will continue to use telehealth if it remains reimbursable at an equal rate as in-person visits. As evidenced by respondents’ desire for professional organizations such as APSA and AAP to continue to lobby and promote its use, legislation should be enacted to ensure reimbursement for telehealth visits.
Financial support
This work was supported by the American Academy of Pediatrics Delivery of Surgical Care Committee and the American Pediatric Surgical Association Outcomes Committee.
Level of evidence
V
Declaration of Competing Interest
None of the authors have any competing interests to declare.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jpedsurg.2022.01.048.
Appendix. Supplementary materials
References
- 1.Bashshur R.L., Shannon G.W. Mary Ann Liebert; New Rochelle, NY: 2009. History of telemedicine: evolution, context, and transformation. [Google Scholar]
- 2.Nesbitt, T.S. The evolution of telehealth: where have we been and where are we going? National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK207141/
- 3.HR 6074 - coronavirus preparedness and response supplemental appropriations act, 2020. www.congress.gov/bill/116th-congress/house-bill/6074. [Accessed on September 28, 2021].
- 4.Imlach F., McKinlay E., Middleton L., et al. Telehealth consultations in general practice during a pandemic lockdown: survey and interviews on patient experiences and preferences. BMS Fam Pract. 2020;21(1):269. doi: 10.1186/s12875-020-01336-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jeganathan S., Prasannan L., Blitz M.J., et al. Adherence and acceptability of telehealth appointments for high-risk obstetrical patients during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM. 2020;2(4) doi: 10.1016/j.ajogmf.2020.100233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Postuma R., Loewen L. Telepediatric surgery: capturing clinical outcomes. J Pediatr Surg. 2005;40(5):813–818. doi: 10.1016/j.jpedsurg.2005.01.049. [DOI] [PubMed] [Google Scholar]
- 7.Goldin A.B., Lariviere C., Arca M.J., et al. Guidelines for surveys of the American pediatric surgical association. J Pediatr Surg. 2011;46(10):2012–2017. doi: 10.1016/j.jpedsurg.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 8.Dean P., O'Donnell M., Zhou L., et al. Improving value and access to specialty medical care for families: a pediatric surgery telehealth program. Can J Surg. 2019;62(6):436–441. doi: 10.1503/cjs.005918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harting M.T., et al. Telemedicine in pediatric surgery. J Pediatr Surg. 2019;54:587–594. doi: 10.1016/j.jpedsurg.2018.04.038. [DOI] [PubMed] [Google Scholar]
- 10.Schmidtberg L.C., Grindle C., Hersh D.S., et al. Telehealth in pediatric surgical subspecialties: rapid adoption in the setting of COVID-19. Telemed J eHealth. 2021 doi: 10.1089/tmj.2021.0080. Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 11.Nandra K., Koenig G., DelMastro A., et al. Telehealth provides a comprehensive approach to the surgical patient. Am J Surg. 2019;218(3):476–479. doi: 10.1016/j.amjsurg.2018.09.020. [DOI] [PubMed] [Google Scholar]
- 12.Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html. [Accessed on September 28, 2021].
- 13.Illinois permanently expands access to telehealth. Healthcareitnews. https://www.healthcareitnews.com/news/illinois-permanently-expands-access- telehealth#:∼:text=Gov.&text=The%20bill%2C%20HB%203308%2C%20requires,to%20be%20covered%20through%202027. [Accessed on September 28, 2021].
- 14.Madden N., Emeruwa U.N., Friedman A.M., et al. Telehealth uptake in prenatal care and provider attitudes during the COVID-19 pandemic in New York city: a quantitative and qualitative analysis. Am J Perinatol. 2020;37(10):1005–1014. doi: 10.1055/s-0040-1712939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shivji S., Metcalfe P., Khan A., et al. Pediatric surgery telehealth: patient and clinician satisfaction. Pediatr Surg Int. 2011;27:523–526. doi: 10.1007/s00383-010-2823-y. [DOI] [PubMed] [Google Scholar]
- 16.Nanda M., Sharma R. A review of patient satisfaction and experience with telemedicine: a virtual solution during and beyond COVID-19 pandemic. Telemed J eHealth. 2021 doi: 10.1089/tmj.2020.0570. ahead of print. [DOI] [PubMed] [Google Scholar]
- 17.Dick P.T., Filler R., Pavan A. Participant satisfaction and comfort with multidisciplinary pediatric telemedicine consultations. J Pediatr Surg. 1999;34(1):137–141. doi: 10.1016/s0022-3468(99)90244-0. [DOI] [PubMed] [Google Scholar]
- 18.Abdulhai S., Glenn I.C., McNinch N.L., et al. Public perception of telemedicine and surgical telementoring in the pediatric population: results of a parental survey. J Laparoendosc Adv Surg Tech A. 2018;28(2):215–217. doi: 10.1089/lap.2017.0294. [DOI] [PubMed] [Google Scholar]
- 19.Bator E.X., Gleason J.M., Lorenzo A.J., et al. The burden of attending a pediatric surgical clinic and family preferences toward telemedicine. J Pediatr Surg. 2015;50:1776–1782. doi: 10.1016/j.jpedsurg.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 20.Miller G.G., Levesque K. Telehealth provides effective pediatric surgery care to remote locations. J Pediatr Surg. 2002;37:752–754. doi: 10.1053/jpsu.2002.32270. [DOI] [PubMed] [Google Scholar]
- 21.Kohler J.E., Falcone R.A., Fallat M.E. Rural health, telemedicine and access for pediatric surgery. Curr Opin Pediatr. 2019;31:391–398. doi: 10.1097/MOP.0000000000000763. [DOI] [PubMed] [Google Scholar]
- 22.Cost N.G., Aldrink J.H., Saltzman A.F., et al. Current state of renal tumor surgery among pediatric surgeons and pediatric urologists: a survey of the American pediatric surgical association (APSA) and society for pediatric urology (SPU) members. J Pediatr Urol. 2018;14(2):168e1–168e8. doi: 10.1016/j.jpurol.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 23.Trappey A.F., Galganski L., Saadai P., et al. Surgical management of pediatric rectal prolapse: a survey of the American pediatric surgical association (APSA) J Pediatr Surg. 2019;54(10):2149–2154. doi: 10.1016/j.jpedsurg.2019.02.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.