Abstract
Objective
To evaluate the correlation between the TIMI frame count, IMR, and CFR in coronary microvascular disease (slow flow phenomenon).
Methods
TFC and IMR were recorded in the nitroglycerin and ATP administration states, and the relationship between TFC, IMR, and CFR in specific states was analyzed.
Results
A total of 41 patients with baseline TFC >25 frames on coronary angiography were enrolled, and nitroglycerin reduced TFC by 50% from baseline in 24 (58.54%) patients; 16 of the remaining 17 patients were able to achieve a 50% reduction in TFC by further intracoronary ATP injection. 10 patients were further tested for IMR, and the results showed significant correlations between baseline TFC and IMR (r = 0.775, P=0.008), TFC and IMR after nitroglycerin (r = 0.875, P=0.001), and the minimal TFC and IMR that could be obtained with nitroglycerin or ATP administration (r = 0.890, P=0.001). There was also a significant correlation between the proportional improvement in TFC and CFR before and after nitroglycerin injection (r = 0.685, P=0.029). In addition, we observed a lower IMR measured after nitroglycerin than after ATP in three patients, suggesting that CMD may be dominated by NO-sensitive vascular such as prearterioles and that an extensive analysis of the target site of CMD may be achieved by stepwise drug administration.
Conclusion
Induction of TFC in different states by a stepwise drug approach may serve as a potential primary screening method for coronary microcirculatory dysfunction, thereby reducing the need for further IMR or CFR testing.
1. Introduction
Coronary microvascular dysfunction (CMD) is a clinical phenomenon that causes myocardial ischemia due to functional or structural abnormalities of the microvascular and is considered one of the causes of nonobstructive coronary heart disease [1]. The invasive diagnostic criteria for CMD mainly include coronary slow flow (CSF) phenomenon presenting as TIMI frame count (TFC) >25 frames, index of microcirculatory resistance (IMR) >25, or coronary flow reserve (CFR) <2.0 [2]. Some studies have shown that there is no significant correlation between the three indices, suggesting that these three indices are measured from different dimensions [3, 4]. TFC evaluates the state of CMD at the baseline status; IMR evaluates the state when the microcirculation is fully dilated, focusing more on structural CMD; and CFR reflects the reserve capacity of coronary microcirculation. From this, we can also see that the difference between the three is related to different states at the time of testing, in addition to different testing methods. Therefore, we envisage that it is possible to find a connection between the three and even to substitute each other to some extent if the tests are performed in the same state. Due to the huge differences in the complexity of the detection methods, it is worth discussing whether TFC, a relatively easy-to-implement detection method, can replace the complex detection methods of IMR and CFR after its process improvement to achieve the goal of simplifying the CMD assessment process.
2. Method
2.1. Patient Enrollment
Patients with coronary angiography showing slow flow were enrolled consequently. CSF was defined as the TIMI frame count >25 frames at 15 frames per second (fps). The clinical diagnosis in all patients favored microvascular angina, i.e., coronary angiography showed no >50% stenosis or significant thrombotic, dissection lesions in the large epicardial vessels; also, there was no evidence of typical variant angina-epicardial large vessel spasm.
2.2. Coronary Angiography, Intracoronary Drug Administration, and TIMI Frame Count
Coronary angiography was performed using a 5 F TIG catheter through the radial artery. The contrast medium was injected manually by the same operator, and it was required to ensure satisfactory filling of the intravascular contrast medium and clear display of the vessel contour. The image acquisition frequency was standard 15 frames per second (fps), with a blank phase, and the image acquisition was maintained until the last branch of the distal coronary artery was visualized [5]. LAD was selected for all patients. The TFC result is obtained by subtracting the number of frames of the opening from the most distal branch. Each patient will undergo 2-3 steps of TIMI counting. In the first step, baseline TIMI frame (TFCBase) will be recorded without any intracoronary medication; in the second step, TIMI frame (TFCNIT) will be recorded after intracoronary injection of 200 μg of nitroglycerin; if the decrease in TFCNIT compared to TFCBase is less than 50%, then the third step is followed—inject 100 μg of adenosine triphosphate intracoronarily and record the TFC once again (TFCATP). It is important to note that there should be at least a 2-minute interval between the nitroglycerin and ATP injections and to confirm that the TFC returns to baseline levels to ensure complete elution of the nitroglycerin effect.
2.3. Measurement of IMR, CFR, and FFR
IMR, CFR, and fractional flow reserve (FFR) were evaluated in all patients who signed an informed consent form using a C12008 pressure wire (Abbott, Illinois, USA) following a standard procedure. Blood was flushed out of the system with saline prior to testing, and the pressure of the catheter system was equalized to the atmospheric pressure and the pressure of the catheter system before the pressure guide wire entered the catheter. The test was performed using a 6 F guide catheter, and the pressure guide wire was equalized to the system pressure when it reached the ostium of the LCA. The pressure guide wire was advanced as far as possible into the distal segment of the LAD while avoiding wall attachment or significant tension on the tip of the pressure guide wire.
After confirming that the guiding catheter and LCA ostium were well engaged, intracoronary bullet injections of 5 ml of room temperature saline were performed to obtain the mean transit time (Tmn), and mean distal pressure (Pd) was recorded simultaneously [6, 7]. Pd and Tmn were acquired in 3 specific states: baseline state (without any vasoactive drug), after intracoronary injection with 200 ug nitroglycerin, and during continuous intravenous pumping of adenosine triphosphate (160 ug/kg ∗ min). After each specific state is tested, the next state is waited for the TIMI frame count to return to baseline levels.
IMR was then calculated as Pd × Tmn. Base, NIT, and ATP were used as footnotes for the IMR in the corresponding states, which were presented as IMRBase, IMRNIT, and IMRATP. The lowest IMR that can be achieved after NIT or ATP treatment was represented by IMRMin.
CFR was calculated as the ratio of Tmn at rest to Tmn at the maximum hyperemic state. Use the footer to indicate the comparison of the two states in which the CFR occurs. For example, a comparison between the baseline state and the nitroglycerin-induced state is indicated as CFRBase/NIT.
FFR was calculated as Pd/Pa in the maximal hyperemic state. The maximal hyperemic state was obtained by intracoronary nitroglycerin injection with continuous intravenous pumping of adenosine triphosphate (160 ug/kg ∗ min).
2.4. Statistical Methods
Statistical analyses were performed using SPSS 26.0 software (IBM Corp., Armonk, NY, USA). For continuous variables, the Kolmogorov–Smirnov test was used to determine whether the data are normally distributed. Continuous variables were presented as mean ± standard deviation or median (quartile), whereas gender, past medical history, etc., were presented as percentages. Spearman's correlation analysis was used to analyze the correlation between parameters. A two-tailed P value <0.05 was considered statistically significant.
3. Results
3.1. General Data
A total of 41 patients were enrolled, including 28 males and 13 females, with a mean age of 59.02 ± 12.01. All patients were admitted with chest pain/discomfort, but not exertional. 24 had a history of hypertension, 17 had type 2 diabetes mellitus, 21 patients (51.22%) were current smokers, and the proportion of other comorbid diseases was low. The mean BMI was 25.01 ± 3.72 kg/m2 in males and 24.92 ± 3.24 kg/m2 in females, both meeting the criteria for overweight. Mean systolic blood pressure was 125.39 ± 16.89 mmHg, diastolic blood pressure was 75.95 ± 10.83 mmHg, and heart rate was 72.05 ± 11.39 bpm. Ancillary examinations showed that mean HbA1c was 6.80 ± 1.50%, NT-proBNP was 77 (5, 1871) pg/ml, and mean LVEF was 63.95 ± 6.47%. Detailed examination results are shown in Table 1.
Table 1.
General data of patients enrolled.
| Indicator | Value |
|---|---|
| Age (y) | 59.02 ± 12.01 |
| Gender (female, %) | 31.71 (13/41) |
| BMI male (kg/m2) | 25.01 ± 3.72 |
| BMI female (kg/m2) | 24.92 ± 3.24 |
| HR (bpm) | 72.05 ± 11.39 |
| SBP (mmHg) | 125.39 ± 16.89 |
| DBP (mmHg) | 75.95 ± 10.83 |
| NT-proBNP (pg/ml) | 77 (5, 1871) |
| HbA1c (%) | 6.80 ± 1.50 |
| LDL-c (mmol/L) | 2.04 ± 0.58 |
| Triglyceride (mmol/L) | 1.50 (1.00, 2.19) |
| eGFR (ml/min ∗ kg) | 94.92 ± 12.64 |
| LVEF (%) | 63.95 ± 6.47 |
| IVS (mm) | 9.23 ± 1.37 |
| LVPW (mm) | 8.90 ± 1.10 |
| LVEDd (mm) | 45.66 ± 4.62 |
| Smoker (%) | 51.22 (21/41) |
| Hypertension (%) | 58.54 (24/41) |
| Type 2 diabetes (%) | 41.46 (17/41) |
| Obstructive sleep apnea syndrome (%) | 4.88 (2/41) |
3.2. Result of TFC Analysis
Mean TFCBase for all 41 patients was 38.12 ± 10.12 frames, and mean TFCNit was 19.34 ± 8.39 frames, with a mean reduction in TFCNit over TFCBase of 49.40 ± 15.91%. The proportion of patients with >50% reduction was 58.54% (24/41), and their baseline median frames were 37 (29, 41) frames, which decreased to 14 (12, 17) frames with nitroglycerin, with a median reduction of 60.49% (54.90%, 64.39%); the proportion of patients with ≦50% reduction was 41.46% (16/41), and their baseline median frames were 36 (29, 49) frames, which decreased to 25 (18, 34) frames with nitroglycerin, with a median decrease of 36.11% (32.35%, 40.01%). There was no statistically significant difference between the two groups of effective/ineffective nitroglycerin in TFCBase (P=0.519) (Figure 1).
Figure 1.
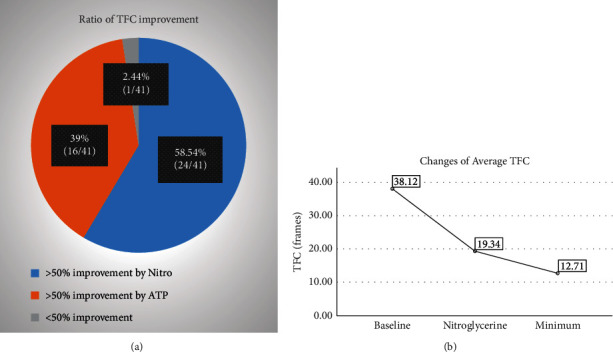
(a) The proportion of TFC improved by nitroglycerin or ATP; (b) the extent to which TFC can be reduced after intracoronary nitroglycerin injection and after sequential ATP injection.
For the 17 patients with <50% reduction in TFCBase induced by nitroglycerin, TFCATP was assayed after nitroglycerin elution, and the results were 11 (9, 15) frames with a median reduction of 69.44% (65.48%, 72.43%) compared to TFCBase. All patients could obtain more than 50% reduction in the TFC from baseline by nitroglycerin or ATP injection, except for 1 patient who had a reduction of less than 50% from baseline.
3.3. Result of Specific IMR
A total of 10 patients underwent examination with the pressure wire, and FFR was above 0.87 in all patients (0.87 to 0.96). Six of them had >50% reduction in the TFC induced by nitroglycerin, three had >50% reduction in the TFC induced by ATP, and one could not achieve >50% reduction in the TFC by both nitroglycerin and ATP. The results showed that the included patients had TFCBase of 32 (28, 39) frames and TFCNIT of 15 (12, 22) frames, and the minimum TFC induced by nitroglycerin or ATP (TFCMin) was 12 (10, 14) frames. IMRBase was 115.58 (111.67, 136.05), IMRNIT was 48.33 (18.28, 67.77), IMRATP was 23.10 (14.70, 37.55), and the minimum IMR induced by nitroglycerin or ATP (IMRMin) was 16.33 (13.83, 28.13). Three patients had IMRNit <25, six patients had IMRATP <25, and there was no correlation between IMRNit and IMRATP (Figure 2).
Figure 2.
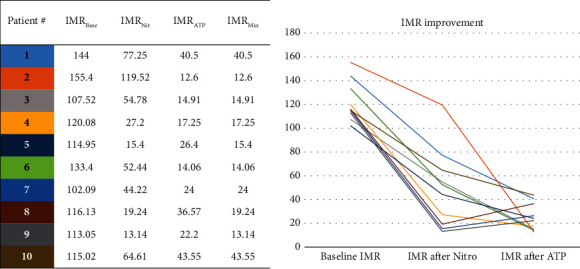
10 cases underwent IMR examination. The baseline IMR (IMRBase) was distributed between 100 and 160, and 3 patients had higher IMR induced by ATP (IMRATP) than IMR induced by nitroglycerin (IMRNit), suggesting difference in the position of functional microcirculatory insufficiency.
3.4. Correlation of TFC with Specific IMR
After treatment with nitroglycerin or ATP, IMRMin decreased to below 25 in 8 patients. The other 2 patients had IMRMin of 40.50 and 43.55, respectively, and their corresponding TFCMin was 16 and 15 frames, respectively. Spearman's correlation analysis showed that TFCBase was significantly correlated with IMRBase (r = 0.775, P=0.008), but not with IMRNIT, IMRATP, or IMRMin. TFCNit was significantly correlated with IMRNit (r = 0.875, P=0.001), and TFCMin was significantly correlated with IMRMin (r = 0.890, P=0.001) (Figure 3).
Figure 3.
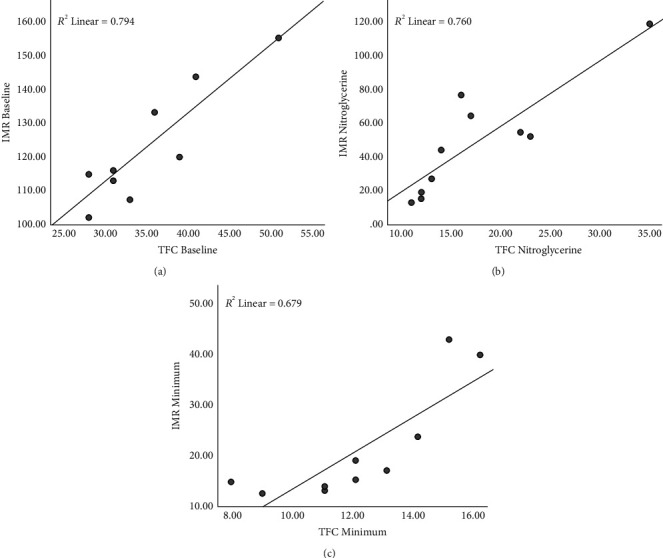
Correlation between IMR and TFC. (a) TFCBase was significantly correlated with IMRBase (r = 0.775, P=0.08). (b) TFCNit was significantly correlated with IMRNit (r = 0.875, P=0.001). (c) TFCMin was significantly correlated with IMRMin (r = 0.890, P=0.001).
3.5. Correlation of TFC and CFR
The value of the decrease in TFCNit compared to TFCBase was not significantly correlated with the value of the decrease in IMRNit compared to IMRBase (r = 0.549, P=0.100) (Figure 4(a)), while the value of the decrease in TFCMin compared to TFCBase was significantly correlated with the value of the decrease in IMRNit compared to IMRBase (r = 0.926, P < 0.001) (Figure 4(b)).
Figure 4.
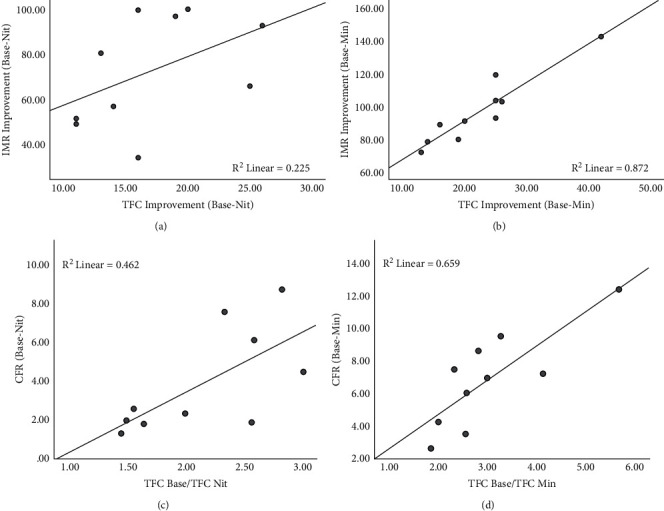
Correlation between the improvement of TFC and IMR. (a) No significant correlation in the actual value improvement between TFCBase-Nit and IMRBase-Nit (r = 0.549, P=0.10). (b) A significant correlation between the actual value improvement between TFCBase-Min and IMRBase-Min (r = 0.926, P < 0.001). (c, d) A significant correlation between the ratio of TFCBase/Nit and CFRBase/Nit (r = 0.685, P=0.029) as well as between TFCBase/Min and CFRBase/Min (r = 0.758, P=0.011). ∗Base: baseline; Nit: measured after nitroglycerin injection; ATP: measured after ATP injection; Min: measured after sequenced nitroglycerin and ATP injection.
We calculated the ratio of TFC (TFCBase/Nit) and CFR (CFRBase/Nit) for the coronary nitroglycerin-injected state compared with the baseline state and the maximum ratio of TFC (TFCBase/Min) and CFR (CFRBase/Min) that could be obtained for the nitroglycerin-injected or ATP state compared with the baseline state. The results showed median TFCBase/Nit of 2.17 (1.55, 2.54) and median CFRBase/Nit of 2.43 (1.84, 6.39), showing a significant correlation (r = 0.685, P=0.029) (Figure 4(c)). Median TFCBase/Min was 2.70 (2.25, 3.49), and median CFRBase/Min was 7.09 (4.08, 8.82), and there was a significant correlation between them (r = 0.758, P=0.011) (Figure 4(d)).
4. Discussion
CMD includes both functional and structural types, and some patients have both of these types, which are called mixed types. The incidence of structural abnormality is relatively low and is commonly caused by various causes of myocardial hypertrophy and atherosclerosis; functional CMD is relatively common and mainly results from vasospasm caused by various abnormalities in vasodilation and contraction regulation, which can usually be reversed using vasodilator drugs. Although there are differences in the technical principles of TFC, IMR, and CFR, what is more important is the difference in patient status at the time of testing. TFC is the state of CMD at baseline without medication and may contain both functional and structural factors, IMR is the state of maximal hyperemia induced by medication and retains only structural factors, whereas CFR evaluates the effect of medication and corresponds to the weighting of functional factors. Therefore, it is not reasonable to directly compare the three parameters and obtain results without correlation in previous studies. A more reasonable approach would be to compare the clinical values of the three parameters in the same hyperemic state.
In the present study, TFC and IMR were recorded separately for baseline and drug-induced maximum hyperemic states. Under the same state, TFC and IMR showed a good correlation, and there was also a significant correlation between improvement in TFC and CFR. Since TFC is a simpler method than CFR and IMR, the above results suggest a possible initial screening of coronary microcirculatory function by the results of TFC in different states to exclude the majority of patients with functional CMD. Only patients with insufficient drug effect require further IMR. To achieve this, there are still some issues that need further work to be addressed.
To further ensure the consistency of TFC and IMR in terms of measurement status, the choice of the target artery to be measured may have to be changed. The LAD was used in this study, which may not be a good choice. Since TFC is usually measured using an angiographic catheter, while IMR requires a guiding catheter, and the morphology of the LCA ostium and the diameter of the LM are highly variable, there are differences in the engagement of the LCA ostium between the two catheters, further affecting the coaxiality and filling speed of the contrast in the LAD. RCA, on the contrary, has relatively few problems in this regard and may be a more appropriate choice. Of course, this choice can only be made if it is not a significant left dominant, and RCA also shows a significant slow flow. The use of an extension catheter for the LAD with larger internal diameters may also be an option. This problem mainly affects the stability and reproducibility of the assay and is also present in the IMR measurement process.
In-depth consideration is also needed in the selection of vasodilator drugs to achieve maximum hyperemia. The coronary microvasculature is a complex network that includes three components: prearterioles (200–400 um), arterioles (20–200 um), and capillaries. Both prearterioles and arterioles are the main regulatory vessels and can be classified as nitric oxide-dependent and nondependent, with differences in response to drugs. Adenosine/ATP acts mainly in 20–200 um vessels [8], whereas vessels in the 200–400 um diameter range are more sensitive to nitrates [9]. Depending on the vascular response to the drug, it can also be classified as endothelium-dependent dysfunction, nonendothelium-dependent dysfunction, or a combination of the two types. Of course, this functional classification is also related to the anatomical segment [10]. Although the classic approach to diagnosing CMD is to use adenosine/ATP alone, acetylcholine can identify endothelium-dependent dysfunction and increase diagnostic accuracy. However, there are risks associated with the process of acetylcholine-induced microcirculatory spasm [11, 12].
In this study, we used a stepwise administration strategy: (1) nitroglycerin was used instead of acetylcholine in patients with CSF to determine the presence of endothelium-dependent dysfunction; (2) nitroglycerin was first given to observe the effect of nitroglycerin on CSF, and ATP was given to patients who responded poorly to nitroglycerin. We observed a “biphasic” improvement in TFC, with nitroglycerin, which could reduce TFC by more than 50% in 58.54% of patients, suggesting that the CSF in this group of patients was mainly from the spasm of the prearterioles; and the phenomenon that ATP was effective suggests that the site of their coronary spasm may be located in the arterioles. The phenomenon of lower IMRNIT than IMRATP observed in some patients further suggests variability in the site of spasticity, the exact mechanism and clinical implications of which need to be further investigated. Thus, the stepwise administration strategy of nitroglycerin and ATP can be used to identify endothelium-dependent or nonendothelium-dependent, while a combination strategy of nitroglycerin and ATP/adenosine or the use of drugs such as nicorandil/fasudil that have a dilating effect covering the entire microvascular network may be relevant in determining the presence of structural dysfunction [13, 14]. Whether the use of stepwise administration allows for further refinement in locating the target vessels responsible for functional dysfunction and its clinical value requires further study.
4.1. Limitation
This study is only a preliminary exploratory study with a small sample size, which does not provide sufficient evidence for the generalizability of the results and is insufficient to analyze the factors associated with different phenotypes, and larger clinical studies are currently underway. In the follow-up study, the study process needs to be further improved, and it is proposed to perform TFC testing in both nitroglycerin and ATP states in all patients to further determine the proportion of different sites of microcirculatory abnormalities in the population and to analyze the associated factors. The clinical significance of the variability in response to drugs needs to be further explored.
5. Conclusion
CMD is a highly prevalent phenomenon, and the current diagnostic criteria for TFC, CFR, and IMR have significant overlap in terms of underlying theory. The preliminary results of the present study give a first insight into the association between the three parameters. Further clarification of this relationship through a larger study would be valuable to optimize the overall process of coronary microcirculation assessment and the diagnosis of CMD.
Acknowledgments
The authors are grateful to the staff at the Department of Cardiology, Peking University Third Hospital, for their invaluable help. This study was funded by the Coronary Microvascular Disease Innovation Fund (2018-CCA-CMVD-08) from XinXin Heart (SlP) Foundation, Hangzhou, China.
Contributor Information
Yanyang Mao, Email: 445011085@qq.com.
Liyun He, Email: hly26@126.com.
Data Availability
All the data generated or analyzed during this study are included in this published article.
Consent
Informed consent was obtained from the patients.
Disclosure
Xinye Xu and Jinbao Zhou are the co-first authors.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Authors' Contributions
Jinbao Zhou, Yanyang Mao, Liyun He, Yongzhen Zhang, Qian Li, and Xinye Xu carried out the studies and participated in the procedure conducting and data collecting. Jinbao Zhou and Xinye Xu drafted the manuscript. Xinye Xu designed the study and performed the statistical analysis. Liyun He and Lijun Guo helped to draft the manuscript. All authors read and approved the final manuscript.
References
- 1.Suwaidi J. A., Hamasaki S., Higano S. T., Nishimura R. A., Holmes D. R., Jr, Lerman A. Long-term follow-up of patients with mild coronary artery disease and endothelial dysfunction. Circulation . 2000;101(9):948–954. doi: 10.1161/01.cir.101.9.948. [DOI] [PubMed] [Google Scholar]
- 2.Ong P., Camici P. G., Beltrame J. F., et al. International standardization of diagnostic criteria for microvascular angina. International Journal of Cardiology . 2018;250:16–20. doi: 10.1016/j.ijcard.2017.08.068. [DOI] [PubMed] [Google Scholar]
- 3.Lee J. M., Jung J.-H., Hwang D., et al. Coronary flow reserve and microcirculatory resistance in patients with intermediate coronary stenosis. Journal of the American College of Cardiology . 2016;67(10):1158–1169. doi: 10.1016/j.jacc.2015.12.053. [DOI] [PubMed] [Google Scholar]
- 4.Fineschi M., Bravi A., Gori T. The “slow coronary flow” phenomenon: evidence of preserved coronary flow reserve despite increased resting microvascular resistances. International Journal of Cardiology . 2008;127(3):358–361. doi: 10.1016/j.ijcard.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Gibson C. M., Cannon C. P., Daley W. L., et al. TIMI frame count. Circulation . 1996;93(5):879–888. doi: 10.1161/01.cir.93.5.879. [DOI] [PubMed] [Google Scholar]
- 6.Ng M. K. C., Yeung A. C., Fearon W. F. Invasive assessment of the coronary microcirculation. Circulation . 2006;113(17):2054–2061. doi: 10.1161/circulationaha.105.603522. [DOI] [PubMed] [Google Scholar]
- 7.Fearon W. F., Balsam L. B., Farouque H. M. O., et al. Novel index for invasively assessing the coronary microcirculation. Circulation . 2003;107(25):3129–3132. doi: 10.1161/01.cir.0000080700.98607.d1. [DOI] [PubMed] [Google Scholar]
- 8.Conzen P. F., Habazettl H., Vollmar B., Christ M., Baier H., Peter K. Coronary microcirculation during halothane, enflurane, isoflurane, and adenosine in dogs. Anesthesiology . 1992;76(2):261–270. doi: 10.1097/00000542-199202000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Kanatsuka H., Eastham C. L., Marcus M. L., Lamping K. G. Effects of nitroglycerin on the coronary microcirculation in normal and ischemic myocardium. Journal of Cardiovascular Pharmacology . 1992;19:755–763. [PubMed] [Google Scholar]
- 10.Sara J. D., Widmer R. J., Matsuzawa Y., Lennon R. J., Lerman L. O., Lerman A. Prevalence of coronary microvascular dysfunction among patients with chest pain and nonobstructive coronary artery disease. JACC: Cardiovascular Interventions . 2015;8(11):1445–1453. doi: 10.1016/j.jcin.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 11.Knuuti J., Wijns W., Saraste A., et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. European Heart Journal . 2020;41(3):407–477. doi: 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 12.Rahman H., Demir O. M., Ryan M., et al. Optimal use of vasodilators for diagnosis of microvascular angina in the cardiac catheterization laboratory. Circulation: Cardiovascular Interventions . 2020;13 doi: 10.1161/CIRCINTERVENTIONS.120.009019.e009019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sadamatsu K., Tashiro H., Yoshida K., et al. Acute effects of isosorbide dinitrate and nicorandil on the coronary slow flow phenomenon. American Journal of Cardiovascular Drugs . 2010;10(3):203–208. doi: 10.2165/11537280-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 14.Sani H. D., Eshraghi A., Nezafati M. H., Vojdanparast M., Shahri B., Nezafati P. Nicorandil versus nitroglycerin for symptomatic relief of angina in patients with slow coronary flow phenomenon. Journal of Cardiovascular Pharmacology and Therapeutics . 2015;20(4):401–406. doi: 10.1177/1074248415571457. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data generated or analyzed during this study are included in this published article.


