Abstract
Background
Brazil has been disproportionately affected by COVID-19, placing a high burden on ICUs.
Research Question
Are perceptions of ICU resource availability associated with end-of-life decisions and burnout among health care providers (HCPs) during COVID-19 surges in Brazil?
Study Design and Methods
We electronically administered a survey to multidisciplinary ICU HCPs during two 2-week periods (in June 2020 and March 2021) coinciding with COVID-19 surges. We examined responses across geographical regions and performed multivariate regressions to explore factors associated with reports of: (1) families being allowed less input in decisions about maintaining life-sustaining treatments for patients with COVID-19 and (2) emotional distress and burnout.
Results
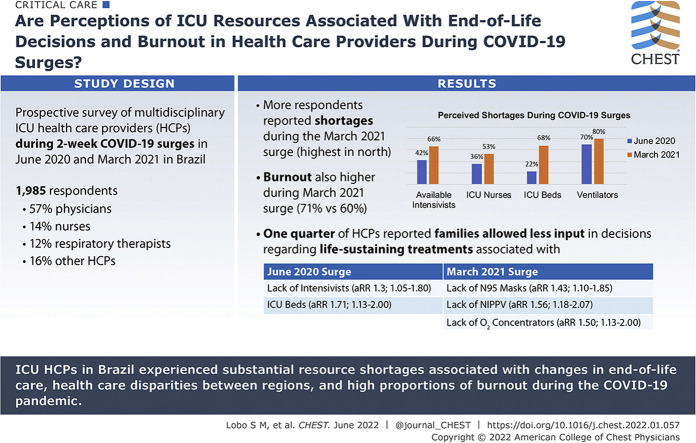
We included 1,985 respondents (57% physicians, 14% nurses, 12% respiratory therapists, 16% other HCPs). More respondents reported shortages during the second surge compared with the first (P < .05 for all comparisons), including lower availability of intensivists (66% vs 42%), ICU nurses (53% vs 36%), ICU beds (68% vs 22%), and ventilators for patients with COVID-19 (80% vs 70%); shortages were highest in the North. One-quarter of HCPs reported that families were allowed less input in decisions about maintaining life-sustaining treatments for patients with COVID-19, which was associated with lack of intensivists (adjusted relative risk [aRR], 1.37; 95% CI, 1.05-1.80) and ICU beds (aRR, 1.71; 95% CI, 1.16-2.62) during the first surge and lack of N95 masks (aRR, 1.43; 95% CI, 1.10-1.85), noninvasive positive pressure ventilation (aRR, 1.56; 95% CI, 1.18-2.07), and oxygen concentrators (aRR, 1.50; 95% CI, 1.13-2.00) during the second surge. Burnout was higher during the second surge (60% vs 71%; P < .001), associated with witnessing colleagues at one’s hospital contract COVID-19 during both surges (aRR, 1.55 [95% CI, 1.25-1.93] and 1.31 [95% CI, 1.11-1.55], respectively), as well as worries about finances (aRR, 1.28; 95% CI, 1.02-1.61) and lack of ICU nurses (aRR, 1.25; 95% CI, 1.02-1.53) during the first surge.
Interpretation
During the COVID-19 pandemic, ICU HCPs in Brazil experienced substantial resource shortages, health care disparities between regions, changes in end-of-life care associated with resource shortages, and high proportions of burnout.
Key Words: Brazil, burnout, COVID-19, critical care resources, disparities, end-of-life care, health care disparities, resource utilization, surge
Graphical Abstract
Take-home Points.
Study Question: How has the COVID-19 pandemic impacted critical care resources and ICU health care provider (HCP) well-being in Brazil?
Results: During two COVID-19 surges in June 2020 and March 2021, participants reported substantial ICU resource shortages, which were lowest in the North. Reported availability of ICU staff, beds, and ventilators was significantly lower during the second surge. HCPs reported allowing families less input in end-of-life decisions for patients with COVID-19, which was associated with reporting resource shortages. Burnout rates were high (60% vs 71%; P < .001) and were associated most strongly with witnessing colleagues contract COVID-19 during both surges.
Interpretation: During the COVID-19 pandemic, ICU HCPs in Brazil experienced substantial resource shortages, witnessed health care disparities among regions, experienced changes in end-of-life care associated with resource shortages, and experienced high proportions of burnout.
The Brazilian COVID-19 health care crisis has been described as a “humanitarian catastrophe” by Médicins Sans Frontières.1 Brazil accounts for the second highest death and third highest case count of COVID-19 worldwide.2 The burden on ICUs has been immense: between February and August 2020, 38% of hospitalized patients with COVID-19 were admitted to an ICU, with ICU mortality ranging from 49% to 79%.3 In late 2020, the P1 (gamma) variant emerged, resulting in a devastating second surge in early 2021.4, 5, 6
Managing surge capacity and resource needs while ensuring provider safety and well-being are essential to balancing the demands of patients in the ICU and maintaining a healthy workforce. Studies have demonstrated a high psychological burden among ICU health care providers (HCPs) during the pandemic,7, 8, 9, 10, 11, 12, 13 with increasing rates of anxiety and burnout.14 Regions with limited resources have been underrepresented in prior assessments of ICU resource use and frontline provider experiences.9 , 10 , 15 , 16
In light of critical medication shortages and ICU bed occupancy levels of > 90% in most states, Brazilian HCPs face challenging decisions about starting or maintaining scarce life-sustaining therapies. Physicians may find themselves having to make such decisions based on available resources and having to limit family input in the shared decision-making process in favor of a more parental approach.
Given Brazil’s continental proportions and heterogeneous geographic distribution of ICU resources,17, 18, 19 the Brazilian Intensive Care Medicine Association (AMIB) has led Brazil’s COVID-19 response by facilitating networking among ICUs, guiding development of consistent protocols, and advocating for resources and support with policymakers. To assess the interplay between critical care shortages, resource use, and provider distress, AMIB distributed a survey to ICU HCPs during the initial COVID-19 surge in June 2020 and the subsequent surge resulting from the P1 (gamma) variant in March 2021.
Our objectives were: (1) to assess HCPs’ perceptions of availability and use of ICU resources during two surges and across all five regions, (2) to evaluate changes in end-of-life decisions and self-reported emotional distress and burnout among HCPs, and (3) to examine the associations among resource availability, end-of-life decisions, and HCP burnout.
Study Design and Methods
Survey Design
A multidisciplinary team of physicians, nurses, and respiratory therapists at the University of Washington designed an electronic survey to elicit perceptions of ICU resource shortages and provider concerns related to COVID-19. This survey was distributed worldwide between April 23 and May 7, 2020, and results were reported previously.10 , 11 The same survey was translated into Brazilian Portuguese for the present study (supplement) and entered into the Institute of Translational Health Sciences’ Research Electronic Data Capture database.20 The survey was pilot tested by 30 multidisciplinary HCPs in Brazil. These responses were not included in the analysis. The study was deemed exempt by the University of Washington Institutional Review Board. Respondents were informed that the survey was anonymous and that summary results would be shared with the scientific community.
Survey Distribution
Our target population included HCPs in Brazil self-attesting to caring directly for patients with COVID-19 hospitalized in an ICU. Respondents who completed only demographic information were excluded. The survey was disseminated via e-mail by the AMIB and its Associates Registry and was posted on AMIB’s website and social media (Twitter, Instagram, and Facebook). With 5,250 members, AMIB is Brazil’s largest medical society, as well as being its only national critical care society. We distributed the survey during two time frames, with the intention of capturing data during COVID-19 surges: (1) June 10 through 24, 2020 (first surge) and (2) March 17 through 31, 2021 (second surge).21 , 22 Additional questions about provider concerns were added for the second survey based on feedback from Brazilian HCPs.
Data Collection
Survey topics included: (1) critical care resource availability (ICU staff, beds, oxygen supplies, testing capacity, and personal protective equipment [PPE]), (2) critical care resource use, and (3) provider concerns, including self-reported emotional distress and burnout. Self-reported emotional distress and burnout were assessed as a single-item question (yes or no). We followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for the reporting of cross-sectional studies.23 To compare respondents’ perceptions against empiric data, AMIB collected data regarding ICU resources and number of COVID-19 cases and deaths from the Instituto Brasileiro de Geografia e Estatística,23 Agência Nacional de Saúde,24 and Datasus.25
Statistical Analysis
We used descriptive statistics to report survey responses across regions, and McNemar’s χ2 test to compare responses between the surges. Brazilian states were categorized into five geographic regions: North, Northeast, Center West, Southeast, and South (e-Table 1). We conducted univariate regression and multivariate log-binomial regression to examine factors associated with two prespecified outcomes: (1) report that patients’ families were allowed less input in critical decisions about maintaining life-sustaining treatments for patients with COVID-19 and (2) emotional distress and burnout. Exposure variables that were statistically significant in the univariate regression (P < .05) were considered for inclusion in multivariate models.26 We conducted a missing data analysis for both surveys to assess how demographics and reported resource availability differed among those who completed the full survey and those who did not. Analyses were conducted using R software (R Foundation for Statistical Computing).
Results
Respondent Characteristics
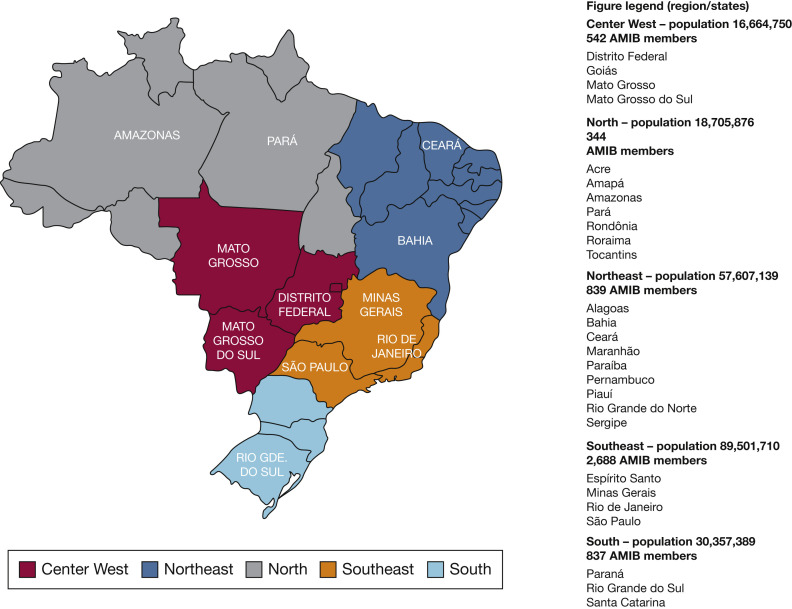
We received 3,007 responses; 671 responses were excluded (n = 301 reported not directly caring for patients with critical illness with COVID-19, n = 370 only completed demographic information) (e-Fig 1). We included 2,336 completed surveys from 1,985 unique respondents in all 27 states (Fig 1 ). Of these, 991 respondents completed the survey during the first surge, 1,345 completed the survey during the second surge, and 351 reported completing both surveys.
Figure 1.
Map of Brazil divided by regions and states.
Most respondents were from the Southeast region (54%), followed by the Northeast (18%), South (15%), Center West (8%), and North (7%). Respondents were physicians (57%), nurses (14%), respiratory therapists (12%), and other providers (16%). Among all participants, the mean ± SD number of years in practice was 13 ± 9.2, 62% were women, and 55% reported caring for > 50 patients with critical illness with COVID-19 (Table 1 ). Most physicians (68%) and 28% of nurses listed critical care as their primary subspecialty. During the second surge, a higher proportion of respondents were physicians (55% vs 63%; P < .001) and more HCPs reported caring for > 50 patients with critical illness with COVID-19 (37% vs 74%; P < .001). Survey responses were similar among those who reported completing the survey twice and completing it only once (e-Table 2).
Table 1.
HCP Characteristics by Survey Perioda
| Characteristic | All Participants (N = 1,985) | Survey 1: First Surge, June 2020 (n = 991) | Survey 2 (All): Second Surge, March 2021 (n = 1,345) | Survey 2: Completed Both Surveys (n = 351) |
|---|---|---|---|---|
| Sex, female | 1,226 (62) | 620 (63) | 802 (60) | 196 (56) |
| Institution | ||||
| Public | 1,004 (51) | 474 (48) | 674 (51) | 144 (42) |
| Private | 782 (40) | 407 (42) | 555 (42) | 180 (52) |
| University | 174 (9) | 98 (10) | 97 (7) | 21 (6) |
| Region | ||||
| Center West | 168 (8) | 86 (9) | 114 (8) | 32 (9) |
| North | 142 (7) | 73 (7) | 84 (6) | 15 (4) |
| Northeast | 353 (18) | 176 (18) | 235 (17) | 58 (17) |
| South | 300 (15) | 125 (13) | 233 (17) | 58 (17) |
| Southeast | 1,022 (54) | 531 (54) | 679 (50) | 188 (54) |
| Qualificationb | ||||
| Attending physician | 761 (38) | 376 (38) | 579 (43) | 194 (55) |
| Physician in training | 382 (19) | 172 (17) | 276 (20) | 66 (19) |
| Nurse | 276 (14) | 150 (15) | 145 (11) | 19 (5) |
| Respiratory therapist | 274 (12) | 148 (15) | 138 (10) | 39 (11) |
| Othersc | 322 (16) | 148 (15) | 207 (10) | 33 (9) |
| Years in practice | 13.1 ± 9.21 | 14.0 ± 9.42 | 13.1 ± 9.21 | 15.6 ± 9.54 |
| Specialization | ||||
| Physiciansd | ||||
| Intensive care | 774 (68) | 424 (77) | 586 (69) | 218 (84) |
| Internal medicine | 245 (21) | 110 (20) | 178 (21) | 43 (17) |
| Cardiology | 121 (11) | 65 (12) | 80 (9) | 2 (8) |
| Emergency medicine | 79 (7) | 35 (6) | 60 (7) | 15 (6) |
| Pulmonology | 40 (3) | 22 (4) | 27 (3) | 12 (5) |
| Anesthesiology | 38 (3) | 15 (3) | 30 (4) | 18 (7) |
| Other | 79 (7) | 35 (6) | 61 (7) | 16 (6) |
| Nurses | ||||
| Intensive care | 235 (28) | 126 (28) | 126 (26) | 17 (89) |
| No. of patients with COVID-19 cared forb | ||||
| < 10 | 284 (14) | 216 (22) | 82 (6) | 14 (4) |
| 10-50 | 613 (31) | 408 (41) | 261 (19) | 56 (16) |
| > 50 | 1,088 (55) | 367 (37) | 1,001 (74) | 280 (80) |
Data are presented as No. (%) or mean ± SD. HCP = health care provider.
No. of respondents in each category vary slightly because some responses are optional; multiple responses are possible per respondent regarding area of specialization, so most frequent subspecialties are listed. A full list of HCP specializations is available in e-Appendix 1. Years in clinical practice includes years in training. Physicians in training include residents and fellows.
P < .05 between surveys 1 and 2
Attending physicians and physicians in training.
Speech therapists, pharmacists, nutritionists, dentists, psychologists, technicians, and research coordinators.
Empiric data show that the number of ICU beds per population and ventilators per population were lowest in the North and Northeast regions during both surges (Table 2 ). The number of COVID-19 cases per population was highest in the Center West and North regions during the first surge and highest in the South and Center West regions during the second surge.
Table 2.
ICU and COVID-19-Related Metrics During Both Surges
| Variable | Center West | North | Northeast | South | Southeast | Overall |
|---|---|---|---|---|---|---|
| First surge (June 2020) | ||||||
| Population | 16,539,298 | 18,705,876 | 57,427,252 | 30,227,208 | 89,118,906 | 212,018,540 |
| % of total population | 7.18 | 8.81 | 27.03 | 14.24 | 42.91 | 100 |
| Share of national GDP | 9.92 | 5.53 | 14.35 | 17.07 | 53.13 | 100 |
| No. of total ICU beds | 5,027 | 2,911 | 11,639 | 7,540 | 27,628 | 54,745 |
| ICU beds per population × 1,000 | 0.30394277 | 0.15561955 | 0.20267381 | 0.24944414 | 0.31001278 | 0.25820855 |
| No. of ventilators | 7,341 | 4,598 | 15,787 | 11,171 | 40,910 | 79,807 |
| Vents per population × 1,000 | 0.44385197 | 0.24580511 | 0.27490433 | 0.36956771 | 0.45904962 | 0.37641519 |
| COVID-19 cases | 497,551 | 543,272 | 1,168,042 | 506,241 | 1,494,506 | 4,209,612 |
| Cases per population × 1,000 | 30.0829576 | 29.0428526 | 20.3395071 | 16.7478584 | 16.7697974 | 19.854924 |
| Accumulated deaths | 10,827 | 14,059 | 35,648 | 10.335 | 58,556 | 119,100 |
| Deaths per population × 1,000 | 0.65462271 | 0.75158202 | 0.62075058 | 0.00034191 | 0.65705474 | 0.56174491 |
| Second surge (March 2021) | ||||||
| Population | 16,664,750 | 18,849,628 | 57,607,139 | 30,357,389 | 89,501,710 | 212,980,616 |
| % of total population | 7.79 | 8.83 | 26.99 | 14.4 | 41.99 | 100 |
| Share of national GDP | 9.92 | 5.53 | 14.35 | 17.07 | 53.13 | 100 |
| No. of total ICU beds | 5,818 | 4,333 | 14,634 | 9,915 | 32,868 | 67,568 |
| ICU beds per population × 1,000 | 0.34912015 | 0.22987191 | 0.25403102 | 0.32660912 | 0.36723321 | 0.31724953 |
| No. of ventilators | 11,516 | 5,682 | 17,846 | 12,766 | 45,541 | 93,351 |
| Vents per population × 1,000 | 0.69103947 | 0.30143831 | 0.30978799 | 0.42052365 | 0.50882827 | 0.43830749 |
| COVID-19 cases | 1,608,006 | 1,546,943 | 3,588,235 | 2,946,490 | 5,754,761 | 15,444,435 |
| Cases per population × 1,000 | 96.4914565 | 82.0675612 | 62.2880265 | 97.0600601 | 64.2977771 | 72.5156838 |
| Accumulated deaths | 40,680 | 39,524 | 88,504 | 64,921 | 188,053 | 421,682 |
| Deaths per population × 1,000 | 2.44108072 | 2.09680531 | 1.53633736 | 2.13855678 | 2.10111069 | 1.97990788 |
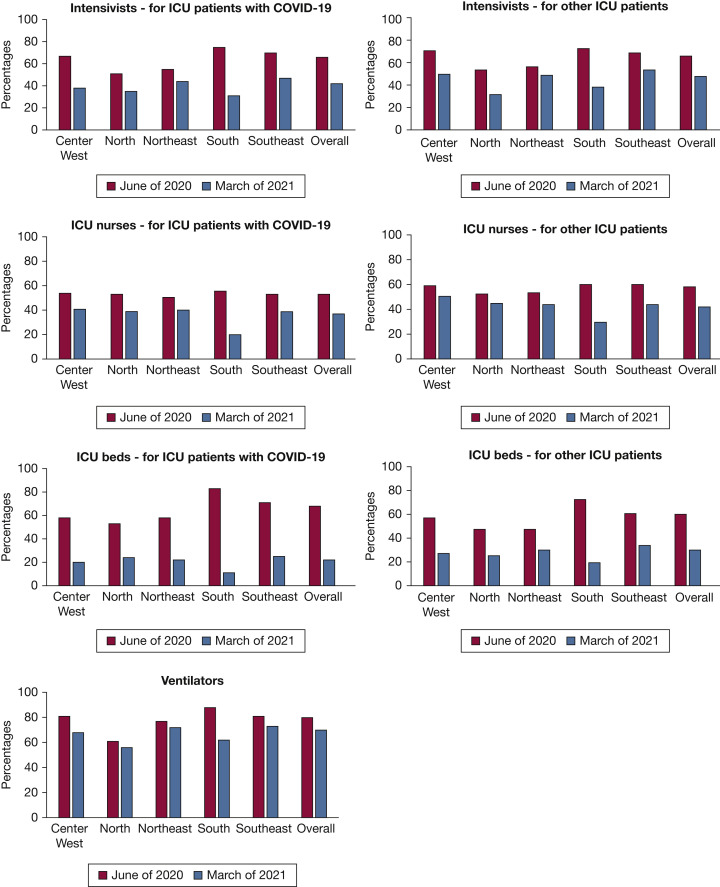
Critical Care Resource Availability
Compared with the first surge in June 2020, a greater proportion of respondents reported shortages during the second surge in March 2021 (Table 3 ). Specifically, during the second surge, respondents reported lower availability of intensivists (patients with COVID-19: 66% vs 42% [P = .002]; other ICU patients: 69% vs 50% [P = .5682]), ICU nurses (53% vs 36% [P < .001] and 59% vs 42% [P < .001], respectively), ICU beds (68% vs 22% [P < .001] and 60% vs 31% [P < .001], respectively), and ventilators (80% vs 70% [P < .001]). Reported availability of intensivists, ICU nurses, and ICU beds were lowest in the North and Northeast during the first surge. During the second surge, shortages were reported most commonly in the South and North (Fig 2 , e-Table 3). Reported lack of ventilators was highest in the North during both surges.
Table 3.
Survey Responses by Period: ICU Resources, ICU Resource Use, and Provider Concerns
| Variable | Survey 1: First Surge, June 2020 (n = 991) | Survey 2: Second Surge, March 2021 (n = 1,345) | P Value |
|---|---|---|---|
| ICU resource availability | |||
| Sufficient no. of intensivists (COVID-19) | 659 (66) | 567 (42) | .002 |
| Sufficient no. of intensivists (other ICU patients) | 688 (69) | 678 (50) | .568 |
| Sufficient no. of ICU nurses (COVID-19) | 529 (53) | 480 (36) | < .001 |
| Sufficient no. of ICU nurses (other ICU patients) | 583 (59) | 563 (42) | < .001 |
| Space | |||
| Sufficient no. of ICU beds (COVID-19) | 515 (68) | 209 (22) | < .001 |
| Sufficient no. of ICU beds (other ICU patients) | 455 (60) | 294 (31) | < .001 |
| Oxygen supplies, available for all patients | |||
| Ventilators | 672 (80) | 770 (70) | < .001 |
| NIPPV | 386 (46) | 503 (46) | .113 |
| HFNC | 234 (28) | 228 (21) | < .001 |
| Oxygen concentrator | 403 (48) | 447 (40) | .736 |
| Oxygen tank oxygen | 796 (95) | 1,022 (92) | .012 |
| Testing, always available | |||
| For patients | 316 (33) | 634 (49) | .8666 |
| For providers | 215 (23) | 475 (37) | < .001 |
| PPE, always available | |||
| Surgical mask | 685 (74) | 1,023 (82) | < .001 |
| Eye protection | 567 (62) | 726 (58) | < .001 |
| Face shield | 552 (60) | 710 (57) | < .001 |
| N95 | 429 (47) | 714 (57) | < .001 |
| PAPR | 231 (25) | 330 (26) | < .001 |
| Sterile gowns | 473 (51) | 772 (62) | < .001 |
| Gloves | 852 (93) | 1,145 (91) | < .001 |
| ICU resource use | |||
| Staffing | |||
| Nonintensivist care for ICU patients with COVID-19 | 314 (82) | 737 (88) | .002 |
| Nonintensivist care for other ICU patients | 177 (46) | 378 (45) | .568 |
| Non-ICU nursing care for ICU patients with COVID-19 | 354 (72) | 741 (81) | < .001 |
| Non-ICU nursing care for other ICU patients | 200 (40) | 388 (42) | < .001 |
| ICU nursing care for more patients at the same time | 135 (27) | 291 (32) | < .001 |
| Space | ... | ... | . . . |
| ICUs have to transfer ICU patients with COVID-19 | 122 (20) | 277 (23) | < .001 |
| ICUs have to transfer other ICU patients | 131 (22) | 240 (20) | < .001 |
| ICUs have to decline transfer requests for patients with COVID-19 | 146 (24) | 583 (49) | < .001 |
| ICUs have to decline transfer requests for other ICU patients | 153 (26) | 432 (36) | < .001 |
| Critical care intervention used for ICU patients with COVID-9 | |||
| Proning | 799 (81) | 1,093 (81) | .697 |
| ECMO | 131 (13) | 271 (20) | < .001 |
| Renal replacement therapy | 695 (70) | 949 (71) | .823 |
| Palliative care consultation | 287 (37) | 367 (36) | .202 |
| MV | |||
| Limiting MV for patients with COVID-19 | 98 (12) | 145 (13) | .36 |
| CPR in patients with COVID-19 | |||
| Unchanged compared with before COVID-19 | 202 (24) | 412 (37) | < .001 |
| New CPR policy | 437 (52) | 417 (38) | ... |
| No new policy, but changed CPR practices | 198 (24) | 279 (25) | ... |
| CPR decisions | |||
| No CPR in patients with COVID-19 | 16 (2) | 5 (0) | .001 |
| Determined by physicians | 571 (68) | 723 (65) | ... |
| Determined by families | 248 (30) | 380 (34) | ... |
| Family input for critical decisions in patients with COVID-19 | |||
| Less compared with before COVID-19 | 223 (27) | 281 (25) | < .001 |
| Provider concerns | n = 728 | n = 903 | ... |
| Insufficient access to PPE | 200 (28) | 132 (15) | < .001 |
| Hospital unable to keep providers safe | 162 (22) | 145 (16) | < .001 |
| Poor communication from supervisors | 159 (22) | 156 (17) | < .001 |
| Worries about my own health | 449 (62) | 462 (51) | < .001 |
| Worries about transmitting COVID-19 to my family or community | 572 (78) | 654 (72) | .001 |
| Experiencing social stigma outside of the hospital | 140 (19) | 142 (16) | < .001 |
| Witnessing colleagues in my hospital contract COVID-19 | 405 (55) | 387 (43) | < .001 |
| Hearing in the media about HCPs contract COVID-19 | 250 (34) | 249 (27) | < .001 |
| Emotional distress and burnout | 438 (60) | 638 (71) | < .001 |
| Worries about finances | 149 (21) | 172 (19) | < .001 |
| Living situation | |||
| Living away from family to protect my family | 123 (17) | 95 (11) | < .001 |
| Live in the same my house, but completely isolated | 34 (5) | 24 (3) | ... |
| Partially isolated from family members | 129 (18) | 123 (14) | ... |
| Do not isolate, but take extra precautions | 353 (49) | 498 (55) | ... |
| No precautions | 88 (12) | 163 (18) | ... |
Data are presented as No. (%), unless otherwise indicated. ECMO = extracorporeal membrane oxygenation; HCP = health care provider; HFNC = high-flow nasal cannula; MV = mechanical ventilation; NIPPV = noninvasive positive pressure ventilation; PAPR = powered air purifying respirator; PPE = personal protective equipment.
Figure 2.
A-D, Bar graphs showing the proportion of respondents who reported a sufficient number of intensivists (A), ICU nurses (B), ICU beds (C), and ventilators (D) at their institution.
During both surges, the proportion of HCPs reporting availability of COVID-19 testing for all patients (33% vs 49%) and all providers (23% vs 37%) was low. Shortages of PPE were reported during both surges (Table 3), most notably for powered air purifying respirators (reported as always available by only 25% vs 26%). During the second surge, more respondents reported availability of surgical masks (74% vs 82%), N95 masks (47% vs 57%), and sterile gowns (51% vs 62%; P < .05 for all comparisons). Shortages of PPE were reported most commonly in the North and Northeast during both surges (e-Table 3).
Critical Care Resource Use
Response to Resource Shortages
Most HCPs who reported shortages indicated that nonintensivists (82% in June 2020 vs 88% in March 2021) and non-ICU nurses (72% vs 81%, respectively) were caring for ICU patients with COVID-19 (Table 3); both proportions were higher during the second surge (P < .05 for both comparisons). The proportion of nonintensivists (46% vs 45%) and non-ICU nurses (40% vs 42%) reported to be caring for other ICU patients were similar between both surges. During the second surge, a higher proportion of respondents reported having to decline transfer requests from other hospitals for patients with critical illness with COVID-19 (24% vs 49%) and other patients in the ICU (26% vs 36%) because of ICU bed shortages (P < .05 for both comparisons). All these measures were reported most commonly in the North during the first surge and in the South during the second surge (e-Table 4).
Critical Care Interventions
Most HCPs reported using prone ventilation in ICU patients with COVID-19 (81% during both surges) and administering renal replacement therapy (71% during both surges). Extracorporeal membrane oxygenation use was reported more frequently during the second surge (13% vs 20%; P < .001) (Table 3). The proportion of HCPs reporting these treatments was lowest in the North during both surges. Approximately one-third of respondents reported consulting palliative care specialists regarding ICU patients with COVID-19 (37% vs 36%; lowest in the North at 23% vs 25%).
Mechanical Ventilation
More than one in 10 respondents (12% vs 13%) reported having to limit mechanical ventilation in patients with critical illness with COVID-19, with the highest proportion (25%) in the North during the first surge and in the North and South (17%) during the second surge. Respondents reported that ventilators were allocated based on disease severity (70% vs 73%), age (26% vs 24%), comorbidities (21% vs 24%), and patient’s insurance or financial status (5% vs 3%).
CPR
A substantial proportion reported changes in CPR policies (52% vs 38%) or practices (24% vs 25%) for ICU patients with COVID-19. Two thirds reported that CPR decisions were determined by physicians (68% vs 65%), rather than based on families’ preferences (30% vs 34%). During the second surge, a higher proportion of respondents from the North (7% vs 30%), and a lower proportion from the South (42% vs 32%) reported that families determined CPR decisions. Respondents reported that the main factors influencing decisions to limit CPR were disease severity (51% vs 57%), comorbidities (44% during both surges), and age (36% during both surges).
Shared Decision-making for Patients With COVID-19
During both surges, about one-quarter of respondents (27% vs 25%) reported that families were allowed less input in critical decisions about maintaining life-sustaining treatments for patients with COVID-19; this was highest in the North (40% vs 45%).
Provider Concerns
The most commonly reported concerns among HCPs were transmitting COVID-19 to one’s family or community (78% vs 72%), worries about their own health (62% vs 51%), and experience of emotional distress and burnout (60% vs 71%). Most provider concerns were lowest in the North during both surges (e-Table 5). A substantial minority (17% vs 10%) reported living away from their families to protect them.
Most provider concerns were reported less frequently during the second surge compared with the first (Table 3), including worries about their own health, finances, insufficient access to PPE, and social stigma outside the hospital (P < .05 for all comparisons). However, self-reported burnout (60% vs 71%; P < .001) was significantly higher during the second surge. In March 2021, 86% of respondents reported feeling more burned out compared with 6 months prior, and 90% reported feeling more burned out than before the pandemic. Respondents listed the following as factors contributing to their burnout: increased workload (79%), recurring surges (75%), poor patient outcomes (74%), emergence of new variants (66%), social isolation (52%), resource shortages (47%), limited family visitation (45%), and witnessing social disparities in patient care (32%). Emotional distress and burnout were lowest in the North and highest in the South during both surges (e-Table 5).
Associations Between Resource Shortages and Shared Decision-making
In multivariate regressions (Table 3), reporting less family input in critical decisions for patients with COVID-19 during the first surge was associated with reporting a shortage of intensivists (adjusted relative risk [aRR], 1.37; 95% CI, 1.05-1.80) and shortage of noninvasive positive pressure ventilation (aRR, 1.56; 95% CI, 1.18-2.07) (Table 4 ). During the second surge, this outcome was associated with report of palliative consultations for ICU patients with COVID-19 (aRR, 1.50; 95% CI, 1.12-2.01) and lack of ICU beds (aRR, 1.71; 95% CI, 1.16-2.62), N95 masks (aRR, 1.43; 95% CI, 1.10-1.85), and oxygen concentrators (aRR, 1.50; 95% CI, 1.13-2.00) (Table 5 ).
Table 4.
Univariate and Multivariate Associations of Reporting Families Have Less Input in Decision-making During COVID-19
| Variable | RR (95% CI) | P Value | aRR (95% CI) | P Value |
|---|---|---|---|---|
| Survey 1: first surge, June 2020 | ||||
| Region | ||||
| Southeast | Reference | ... | Reference | ... |
| North | 1.55 (0.92-2.61) | .10 | 1.41 (0.89-2.23) | .14 |
| Center West | 0.73 (0.42-1.26) | .26 | 0.69 (0.39-1.23) | .21 |
| Northeast | 1.31 (0.90-1.89) | .16 | 1.16 (0.82-1.63) | .41 |
| South | 0.79 (0.51-1.23) | .30 | 0.82 (0.52-1.27) | .37 |
| Palliative care | 1.45 (1.07-1.96) | .02 | — | ... |
| Shortages reported | ||||
| Limited availability of N95 | 1.22 (0.93-1.59) | .15 | — | ... |
| Limited availability of PAPR | 1.30 (0.93-1.81) | .12 | — | ... |
| Insufficient intensivists | 1.49 (1.14-1.94) | < .01 | 1.37 (1.05-1.80) | .02 |
| Insufficient nurses | 1.32 (1.01-1.71) | .04 | — | ... |
| Insufficient ICU beds | 1.32 (0.99-1.76) | .06 | — | ... |
| Limited availability of mechanical ventilators | 1.41 (1.04-1.90) | .03 | — | ... |
| Limited availability of NIPPV | 1.66 (1.26-2.19) | < .01 | 1.56 (1.18-2.07) | < .01 |
| Limited availability of HFNC | 1.33 (0.97-1.83) | .07 | — | ... |
| Limited availability of oxygen concentrators | 1.37 (1.05-1.80) | .02 | — | ... |
| Limited availability of tank oxygen | 1.73 (1.07-2.81) | .03 | — | ... |
| Survey 2: second surge, March 2021 | ||||
| Region | ||||
| Southeast | Reference | ... | Reference | ... |
| North | 2.05 (1.38-3.05) | < .01 | 1.58 (0.99-2.53) | .05 |
| Center West | 0.96 (0.60-1.55) | .88 | 0.90 (0.54-1.47) | .66 |
| Northeast | 1.14 (0.82-1.57) | .44 | 1.01 (0.70-1.44) | .97 |
| South | 1.25 (0.91-1.73) | .16 | 1.15 (0.82-1.62) | .41 |
| Palliative care | 1.65 (1.25-2.19) | < .01 | 1.50 (1.12-2.01) | .01 |
| Shortages reported | ||||
| Limited availability of N95 | 1.49 (1.18-1.88) | < .01 | 1.43 (1.10-1.85) | .01 |
| Limited availability of PAPR | 1.65 (1.20-2.25) | < .01 | — | ... |
| Insufficient intensivists | 1.48 (1.15-1.90) | < .01 | — | ... |
| Insufficient nurses | 1.42 (1.09-1.84) | .01 | — | ... |
| Insufficient ICU beds | 1.98 (1.35-2.90) | < .01 | 1.71 (1.16-2.52) | .01 |
| Limited availability of mechanical ventilators | 1.42 (1.12-1.81) | < .01 | — | ... |
| Limited availability of NIPPV | 1.51 (1.18-1.93) | < .01 | — | ... |
| Limited availability of HFNC | 1.36 (0.99-1.87) | < .01 | — | ... |
| Limited availability of oxygen concentrators | 1.64 (1.27-2.12) | < .01 | 1.50 (1.13-2.00) | .01 |
| Limited availability of tank oxygen | 1.38 (0.94-2.03) | .10 | — | ... |
aRR = adjusted relative risk; — = not included in the model, not statistically significant in multivariate analyses; HCP = health care professional; HFNC = high-flow nasal cannula; NIPPV = noninvasive positive pressure ventilation; PAPR = powered air purifying respirator; RR = relative risk.
Table 5.
Univariate and Multivariate Associations of Reporting Emotional Distress and Burnout Among Health Care Providers in Brazil During COVID-19
| Variable | RR (95% CI) | P Value | aRR (95% CI) | P Value |
|---|---|---|---|---|
| Survey 1: first surge, June 2020 | ||||
| Sex | ||||
| Male | Reference | ... | Reference | ... |
| Female | 1.17 (0.98-1.43) | .11 | — | ... |
| Provider type | ||||
| Attending physicians | Reference | ... | Reference | ... |
| Physicians in training | 0.95 (0.73-1.24) | .71 | 0.95 (0.72-1.26) | .74 |
| Nurse | 1.03 (0.77-1.36) | .85 | 1.05 (0.78-1.41) | .75 |
| Respiratory therapist | 0.92 (0.68-1.25) | .60 | 1.12 (0.84-1.51) | .44 |
| Other | 1.03 (0.77-1.36) | .19 | 0.95 (0.69-1.31) | .74 |
| Region | ||||
| Southeast | Reference | ... | Reference | ... |
| North | 0.88 (0.60-1.30) | .53 | — | — |
| Center West | 1.04 (0.84-1.29) | .77 | 0.82 (0.56-1.21) | .31 |
| Northeast | 1.04 (0.84-1.29) | .73 | 0.93 (0.71-1.22) | .59 |
| South | 1.12 (0.91-1.38) | .35 | 1.04 (0.78-1.39) | .78 |
| Palliative care | 0.98 (0.81-1.19) | 0.84 | — | — |
| Shortages reported | ||||
| Limited availability of N95 | 1.13 (0.94-1.37) | .20 | — | — |
| Limited availability of PAPR | 1.17 (0.90-1.41) | .31 | — | — |
| Insufficient intensivists | 1.27 (1.05-1.53) | .02 | — | — |
| Insufficient nurses | 1.35 (1.11-1.63) | < .01 | 1.25 (1.02-1.53) | .03 |
| Insufficient ICU beds | 1.13 (0.93-1.38) | .21 | — | — |
| Limited availability of mechanical ventilators | 0.96 (0.75-1.23) | .76 | — | — |
| Limited availability of NIPPV | 1.02 (0.85-1.23) | .82 | — | — |
| Limited availability of HFNC | 1.17 (0.94-1.45) | .17 | — | — |
| Limited availability of oxygen concentrators | 1.04 (0.86-1.25) | .69 | — | — |
| Limited availability of tank oxygen | 0.99 (0.60-1.63) | .97 | — | — |
| Provider concerns | ||||
| Insufficient access to PPE | 1.23 (1.01-1.51) | .04 | — | — |
| Feel that hospital is unable to keep me safe | 1.30 (1.05-1.60) | .02 | — | — |
| Poor communication from supervisors | 1.32 (1.07-1.64) | .01 | — | — |
| Worries about own health | 1.37 (1.12-1.68) | < .01 | — | — |
| Worries about financial situation | 1.49 (1.21-1.84) | < .01 | 1.28 (1.02-1.61) | .03 |
| Worries about transmitting infection to my family and community | 1.53 (1.18-1.98) | < .01 | — | — |
| Social stigma from my community | 1.48 (1.19-1.83) | < .01 | 1.25 (1.02-1.53) | .06 |
| Witnessing colleagues at my hospital contract COVID-19 | 1.71 (1.39-2.08) | < .01 | 1.55 (1.25-1.93) | < .01 |
| Hearing about other providers contracting COVID-19 from news | 1.51(1.25-1.83) | < .01 | — | — |
| No. of patients with COVID-19 cared for | ||||
| < 10 | Reference | ... | ... | ... |
| ≥ 10 | 1.35 (1.04-1.75) | .03 | 1.36 (1.03-1.79) | .03 |
| Survey 2: second surge, March 2021 | ||||
| Sex | ||||
| Male | Reference | ... | Reference | ... |
| Female | 1.10 (0.94-1.29) | .23 | — | ... |
| Provider type | ||||
| Attending physicians | Reference | ... | Reference | ... |
| Physicians in training | 1.08 (0.88-1.32) | .48 | 1.06 (0.87-1.30) | .57 |
| Nurse | 1.13 (0.87-1.47) | .35 | 1.11 (0.85-1.44) | .45 |
| Respiratory therapist | 1.01 (0.76-1.32) | .96 | 0.97 (0.74-1.28) | .84 |
| Other | 0.81 (0.62-1.05) | .11 | 0.79 (0.60-1.03) | .08 |
| Region | ||||
| Southeast | Reference | ... | Reference | ... |
| North | 0.90 (0.61-0.77) | .61 | 0.91 (0.62-1.34) | .63 |
| Center West | 1.04 (0.61-1.33) | .77 | 1.03 (0.78-1.37) | .83 |
| Northeast | 1.04 (0.84-1.29) | .73 | 1.03 (0.83-1.28) | .81 |
| South | 1.12 (0.91-1.38) | .28 | 1.08 (0.88-1.34) | .46 |
| Palliative care | 1.00 (0.85-1.17) | .96 | — | — |
| Shortages reported | ||||
| Limited availability of N95 | 1.03 (0.88-1.21) | .68 | — | — |
| Limited availability of PAPR | 1.09 (0.91-1.32) | .35 | — | — |
| Insufficient intensivists | 1.09 (0.93-1.28) | .28 | — | — |
| Insufficient nurses | 1.13 (0.95-1.33) | .17 | — | — |
| Insufficient ICU beds | 1.27 (1.04-1.55) | .02 | — | — |
| Limited availability of mechanical ventilators | 1.05 (0.89-1.24) | .55 | — | — |
| Limited availability of NIPPV | 1.09 (0.94-1.28) | .26 | — | — |
| Limited availability of HFNC | 1.25 (1.02-1.54) | .04 | — | — |
| Limited availability of oxygen concentrators | 1.03 (0.88-1.21) | .42 | — | — |
| Limited availability of tank oxygen | 0.95 (0.70-1.28) | .72 | — | — |
| Provider concerns | ||||
| Insufficient access to PPE | 1.14 (0.92-1.40) | .23 | — | — |
| Feel that hospital is unable to keep me safe | 1.16 (0.95-1.42) | .15 | — | — |
| Poor communication from supervisors | 1.26 (1.04-1.52) | .02 | — | — |
| Worries about own health | 1.19 (1.02-1.39) | .03 | — | — |
| Worries about financial situation | 1.31 (1.09-1.58) | < .01 | — | — |
| Worries about transmitting infection to my family and community | 1.34 (1.11-1.62) | < .01 | 1.21 (0.98-1.48) | .07 |
| Social stigma from my community | 1.29 (1.06-1.57) | .01 | — | — |
| Witnessing colleagues at my hospital contract COVID-19 | 1.40 (1.20-1.63) | < .01 | 1.31 (1.11-1.55) | < .01 |
| Hearing about other providers contracting COVID-19 from news | 1.34 (1.14-1.58) | < .01 | — | — |
| No. of patients with COVID-19 cared for | ||||
| < 10 | Reference | ... | — | — |
| ≥ 10 | 1.33 (0.90-1.95) | .15 | — | — |
aRR = adjusted relative risk; HCP = health care professional; HFNC = high-flow nasal cannula; NIPPV = noninvasive positive pressure ventilation; PAPR = powered air purifying respirator; PPE = personal protective equipment; RR = relative risk.
Associations Between Resource Shortages and Provider Distress
In multivariate regressions, reporting emotional distress and burnout during the first surge was associated most strongly with reporting worries about witnessing colleagues contract COVID-19 (aRR, 1.55; 95% CI, 1.25-1.93), it was also associated with reporting concerns about finances (aRR, 1.49; 95% CI, 1.21-1.84), experiencing social stigma from one’s community (aRR, 1.28; 95% CI, 1.02-1.61), lack of ICU nurses (aRR, 1.25; 95% CI, 1.02-1.53), and caring for more than 10 ICU patients with COVID-19 (aRR, 1.36; 95% CI, 1.03-1.79). During the second surge, reporting emotional distress and burnout again was associated most strongly with reporting worries about witnessing colleagues contract COVID-19 (aRR, 1.31; 95% CI, 1.11-1.55) (Table 3), as well as transmitting COVID-19 infection to one’s family or community (aRR, 1.21; 95% CI, 0.98-1.48).
Missing Data Analysis
We found a drop-off in responses by the end of the questionnaire, leading to missing data in provider concerns (27% and 33% in the first and second surveys, respectively). Therefore, we completed a missing data analysis to assess patterns in the missing observations (e-Table 6). In the first surge, participants who completed the full survey were more likely to be men, to be physicians, to be from the Center West region, to specialize in critical care or internal medicine, and to report caring for > 50 patients with COVID-19. In the second surge, participants who completed the full survey were similar to those who did not in terms of sex, geographic region, and number of patients with COVID-19 cared for, but were more likely to be physicians, to work in private institutions, and to specialize in critical care. In both surges, participants who completed the surveys were more likely to report shortages of ICU staff and beds, whereas other resources were similar between those who did and did not complete the full survey.
Discussion
In this survey, exploring perceptions of 1,985 Brazilian ICU HCPs during two COVID-19 surges, we found (1) lower reported availability of intensivists, ICU nurses, ICU beds, and ventilators during the second surge; (2) disparities in critical care resource availability and use among regions, with respondents from the North and Northeast reporting the highest shortages; (3) HCPs reported allowing families less input when making decisions about maintenance of life-sustaining treatments for patients with COVID-19, which was associated with reporting resource shortages; and (4) high burnout rates, with significantly higher proportions during the second surge, and reporting burnout was associated most strongly with reports of witnessing colleagues contract COVID-19 during both surges.
HCPs reported substantial resource shortages and the need for drastic resource use measures. When comparing the results of this survey with responses from the same survey distributed worldwide in April 2020, the following shortages all were substantially higher in Brazil: intensivists, ICU nurses, ICU beds, mechanical ventilators, testing availability, and PPE. Challenges encountered during the initial Brazilian COVID-19 response included poor coordination among federal, state, and municipal governments; inconsistencies in leadership, miscommunications to the public, causing distrust and misinformation; insufficient lockdowns; lack of opportunities for physical distancing in vulnerable populations; and pursuit of medications with unproven efficacy. These problems are not unique to Brazil and have contributed to worsening spread and recurring surges in many other countries. The emergence of the P1 (gamma) variant in Manaus in late 2020 with higher transmissibility and reinfection potential resulted in a more devastating second surge.4, 5, 6 Initially underestimated, delayed response and fulminant spread led to an overwhelmed health care system and highly publicized scenes of mass grave burials in early 2021. Lessons learned from these two surges can inform the global pandemic response for future surges, especially as variants continue to emerge worldwide.
The pandemic has exacerbated social disparities in Brazil,27 resulting in a collapse of the fragile regional health care systems serving vulnerable populations in the North and Northeast. A retrospective analysis of outcomes in patients with COVID-19 between February and August 2020 demonstrated the highest ICU mortality in the North (79%) and Northeast (66%) compared with other regions (49%-53%).3 Long-standing inequalities and socioeconomic differences among regions predate COVID-1917, 18, 19 , 28 and are reflected in the heterogeneous distribution of federal resources and quality of regional health services.29 Disproportionate shortages of critical resources, lack of organizational structure, and poor adherence to best practices30, 31, 32 likely contribute to worse outcomes in disadvantaged regions. Additionally, racial disparities in Brazil have been magnified further by the pandemic,33 with higher in-hospital COVID-19 mortality and differences in resource use among patients of color, who are represented more frequently in the North and Northeast. An effective pandemic response and sustainable change in the health care system can be achieved only when prioritizing and supporting its most vulnerable populations.
The shared decision-making process between physicians and families may be affected by lack of ICU resources, as suggested by respondents reporting less family input in end-of-life decisions in association with perceived resource shortages. Best practices for end-of-life decisions, including interdisciplinary collaboration and shared decision-making, are essential components of ICU care and have been shown to impact patient and family outcomes, as well as provider well-being.34 , 35 Prior studies suggest that end-of-life decisions and limitations of life-sustaining treatments are less common in Latin America compared with Europe and the United States.36, 37, 38 However, families increasingly have been involved in end-of-life decisions in Brazil over the past decades.39 , 40 The pressure of having to allocate scarce resources among an overwhelming number of patients with critical illness may result in pursuit of a more unilateral approach, in effect reverting to a paternalistic model in the absence of the formal invocation of crisis standards of care41 and protections inherent in this process to the community and the HCPs.
Our findings complement prior studies reporting high rates of burnout among ICU HCPs during the pandemic.8 , 12 , 14 Although a direct comparison is limited by differences in respondent selection and methodology, the proportion of ICU HCP burnout in our study is higher compared with studies in Brazil42 and globally43, 44, 45, 46 before the pandemic. Self-reported burnout also was higher in this study (60%-71%) than identified previously in the same survey among ICU HCPs worldwide (52%; highest in the United States at 58%) in April 2020.10 , 11 Although reporting burnout was associated most strongly with witnessing colleagues contract COVID-19 in Brazil, the predominant factors associated with burnout in the United States were insufficient access to PPE and poor communication from supervisors.11 In both countries, reporting burnout was associated with experience of social stigma outside the hospital, highlighting the juxtaposition of HCPs being praised as heroes while facing isolation and anger from the public. The relationship between psychological strain, resource availability, and socioeconomic factors is highly complex and requires further investigation. Perception and reporting of burnout may be influenced by cultural differences, social norms, and stigma around mental health. Interestingly, the regions reporting the highest resource shortages (North and Northeast) also were the least likely to report burnout in Brazil, and providers from regions with long-standing resource shortages may be more accustomed to the pressure of having to allocate scarce resources.
The pandemic has caused enormous strain among HCPs worldwide, with many leaving their profession because of exhaustion, frustration, and disheartening experiences. We found an association between lack of ICU nurses and burnout among all HCPs, emphasizing the importance of valuing and investing in excellent nursing care. Also, our findings suggest that financial concerns negatively impact the mental well-being of HCPs. Supporting the health of frontline staff, validating their efforts, and rapidly responding to mitigate their challenges early on are critical facets of strengthening our health care system during routine and emergency care.
Our study has several limitations. First, HCP perceptions about resource shortages may not reflect true resource availability. However, survey responses generally were aligned with empiric data.3 , 27 Second, our convenience sampling and inability to capture an accurate response rate introduce a risk of response and sampling bias and may limit generalizability of our results. Our survey response captured only a small proportion of ICU HCPs in Brazil and may not represent experiences of the entire critical care community. In addition, respondents who completed survey questions regarding provider concerns were more likely to report shortages of ICU staff and ICU beds than those with missing data, which might have overestimated burnout. Furthermore, we cannot assess demographics of individuals who saw the survey, but declined to complete it. Third, the ability to compare responses between the two surges is limited because we conducted two cross-sectional surveys, and respondents mostly were different. Furthermore, we conducted many statistical comparisons in this exploratory analysis, which increases the likelihood of false-positive findings. Therefore, we focused qualitatively on the trends across surges. Fourth, the cross-sectional nature of this study allowed us to assess association, but not to assign causality. Fifth, our assessment of provider burnout was based on a single item, rather than a validated scale.47 Finally, practices are changing rapidly as HCPs continue to adjust to the pandemic, and many facets of the pandemic were not captured in our survey.
Interpretation
Our results highlight how severely the COVID-19 pandemic has burdened HCPs. Findings of critical resource shortages, disparities in resource availability among regions with different social economic status, the need to make end-of-life decisions based on resource shortages, and burnout among HCPs underscore the challenges imposed by the pandemic and the personal sacrifices made by HCPs. Initiatives to invest in the health care system, achieve health care equity, and support the providers on the frontline are needed urgently as we continue to confront the pandemic.
Acknowledgments
Author contributions: On behalf of all authors, the corresponding author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained. S. M. L., S. W., M. S., and C. J. C. had full access to all of the data and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed substantially to the study design, data acquisition and analysis, as well as interpretation. M. S. performed the statistical analysis. S. M. L., S. W., M. S., and C. J. C. wrote the manuscript, and all authors edited the manuscript.
Financial/nonfinancial disclosures: None declared.
Other contributions: The authors thank all of their colleagues around the world who have taken the time to participate in their survey while being very busy caring for patients in the ICU. Specifically, we thank Mr. Jonny Suyama (AMIB), for his assistance with survey distribution via AMIB portals.
Additional information: The e-Appendix, e-Figure, and e-Tables are available online under "Supplementary Data."
Footnotes
Drs Wahlster and Sharma share last authorship.
FUNDING/SUPPORT: M. S. received support from the National Institute of Mental Health [Grant K01MH115789]. C. J. C. is supported by the National Institute of Neurological Disorders and Stroke [Grant NS09942]. E. A. is supported by the National Institutes of Health [Grant 1K23NS119794], the Hellman Fellows Fund, the Regents of the University of California Resource Allocation Program, the CURE Epilepsy Foundation Taking Flight Award, a Zoll Foundation Grant, and the American Heart Association [Grant 20CDA35310297].
Supplementary Data
References
- 1.Médecins Sans Frontières (MSF) International Failed coronavirus response drives Brazil to humanitarian catastrophe. https://www.msf.org/failed-coronavirus-response-drives-brazil-humanitarian-catastrophe Médecins Sans Frontières (MSF) International website.
- 2.CSSEGISandData/COVID-19. https://github.com/CSSEGISandData/COVID-19 GitHub website.
- 3.Ranzani O.T., Bastos L.S.L., Gelli J.G.M., et al. Characterisation of the first 250 000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respir Med. 2021;9(4):407–418. doi: 10.1016/S2213-2600(20)30560-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sabino E.C., Buss L.F., Carvalho M.P.S., et al. Resurgence of COVID-19 in Manaus, Brazil, despite high seroprevalence. Lancet. 2021;397(10273):452–455. doi: 10.1016/S0140-6736(21)00183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang P., Casner R.G., Nair M.S., et al. Increased resistance of SARS-CoV-2 variant P.1 to antibody neutralization. Cell Host Microbe. 2021;29(5):747–751.e4. doi: 10.1016/j.chom.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faria N.R., Mellan T.A., Whittaker C., et al. Genomics and epidemiology of the P.1 SARS-CoV-2 lineage in Manaus, Brazil [published online ahead of print May 21, 2021]. Science. https://doi.org/10.1126/science.abh2644 [DOI] [PMC free article] [PubMed]
- 7.Azoulay E., Cariou A., Bruneel F., et al. Symptoms of anxiety, depression, and peritraumatic dissociation in critical care clinicians managing patients with COVID-19. A cross-sectional study. Am J Respir Crit Care Med. 2020;202(10):1388–1398. doi: 10.1164/rccm.202006-2568OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Azoulay E., De Waele J., Ferrer R., et al. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care. 2020;10(1):110. doi: 10.1186/s13613-020-00722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kleinpell R., Ferraro D.M., Maves R.C., et al. Coronavirus disease 2019 pandemic measures: reports from a national survey of 9,120 ICU clinicians [published online ahead of print July 6, 2020]. Crit Care Med. https://doi.org/10.1097/CCM.0000000000004521 [DOI] [PMC free article] [PubMed]
- 10.Wahlster S., Sharma M., Lewis A.K., et al. The coronavirus disease 2019 pandemic’s effect on critical care resources and health-care providers: a global survey. Chest. 2021;159(2):619–633. doi: 10.1016/j.chest.2020.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma M., Creutzfeldt C.J., Lewis A., et al. Healthcare professionals’ perceptions of critical care resource availability and factors associated with mental well-being during COVID-19: results from a US survey [published online ahead of print September 2, 2020]. Clin Infect Dis Off Publ Infect Dis Soc Am. https://doi.org/10.1093/cid/ciaa1311 [DOI] [PMC free article] [PubMed]
- 12.Miller A.G., Roberts K.J., Smith B.J., et al. Prevalence of burnout among respiratory therapists amidst the COVID-19 pandemic. Respir Care. 2021;66(11):1639–1648. doi: 10.4187/respcare.09283. [DOI] [PubMed] [Google Scholar]
- 13.Morgantini L.A., Naha U., Wang H., et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: a rapid turnaround global survey. PloS One. 2020;15(9) doi: 10.1371/journal.pone.0238217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kerlin M.P., Silvestri J.A., Klaiman T., Gutsche J.T., Jablonski J., Mikkelsen M.E. Critical care clinician wellness during the COVID-19 pandemic: a longitudinal analysis [published online ahead of print August 16, 2021]. Ann Am Thorac Soc. https://doi.org/10.1513/AnnalsATS.202105-567RL [DOI] [PMC free article] [PubMed]
- 15.Kaplan L.J., Kleinpell R., Maves R.C., Doersam J.K., Raman R., Ferraro D.M. Critical care clinician reports on coronavirus disease 2019: results from a national survey of 4,875 ICU providers. Crit Care Explor. 2020;2(5) doi: 10.1097/CCE.0000000000000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vranas K.C., Golden S.E., Mathews K.S., et al. The influence of the COVID-19 pandemic on ICU organization, care processes, and frontline clinician experiences: a qualitative study. Chest. 2021;160(5):1714–1728. doi: 10.1016/j.chest.2021.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Amaral P.V., Rocha T.A.H., Barbosa A.C.Q., Lein A., Vissoci J.R.N. Spatially balanced provision of health equipment: a cross-sectional study oriented to the identification of challenges to access promotion. Int J Equity Health. 2017;16(1):209. doi: 10.1186/s12939-017-0704-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Global Burden of Disease 2016 Brazil Collaborators Burden of disease in Brazil, 1990-2016: a systematic subnational analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10149):760–775. doi: 10.1016/S0140-6736(18)31221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Szwarcwald C.L., de Souza Júnior P.R.B., Marques A.P., da S de Almeida W., Montilla D.E.R. Inequalities in healthy life expectancy by Brazilian geographic regions: findings from the National Health Survey, 2013. Int J Equity Health. 2016;15:141. doi: 10.1186/s12939-016-0432-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Research Electronic Data Capture. ITHS. https://www.iths.org/investigators/forms-templates/citation-information/ Research Electronic Data Capture website.
- 21.World Health Organization WHO coronavirus disease (COVID-19) dashboard. World Health Organization website. https://covid19.who.int/
- 22.Institute for Health Metrics and Evaluation COVID-19 projections. Institute for Health Metrics and Evaluation website. https://covid19.healthdata.org/
- 23.von Elm E., Altman D.G., Egger M., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 24.Instituto Brasileiro de Geografia e Estatística Portal do Instituto Brasileiro de Geografia e Estatística. https://www.ibge.gov.br/ Instituto Brasileiro de Geografia e Estatística website.
- 25.Ministério da Saúde de Brasil. Informações de saúde (TABNET): DATASUS. https://datasus.saude.gov.br/informacoes-de-saude-tabnet/ Ministério da Saúde de Brasil website.
- 26.Barros A.J., Hirakata V.N. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3(1):21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ribeiro K.B., Ribeiro A.F., Veras M.A., de S.M., de Castro M.C. Social inequalities and COVID-19 mortality in the city of São Paulo, Brazil. Int J Epidemiol. 2021;50(3):732–742. doi: 10.1093/ije/dyab022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Machado F.R., Cavalcanti A.B., Bozza F.A., et al. The epidemiology of sepsis in Brazilian intensive care units (the Sepsis PREvalence Assessment Database, SPREAD): an observational study. Lancet Infect Dis. 2017;17(11):1180–1189. doi: 10.1016/S1473-3099(17)30322-5. [DOI] [PubMed] [Google Scholar]
- 29.Azevedo L.C.P., Park M., Salluh J.I.F., et al. Clinical outcomes of patients requiring ventilatory support in Brazilian intensive care units: a multicenter, prospective, cohort study. Crit Care Lond Engl. 2013;17(2):R63. doi: 10.1186/cc12594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nassar A.P., Zampieri F.G., Salluh J.I., et al. Organizational factors associated with target sedation on the first 48 h of mechanical ventilation: an analysis of checklist-ICU database. Crit Care. 2019;23(1):34. doi: 10.1186/s13054-019-2323-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Midega T.D., Bozza F.A., Machado F.R., et al. Organizational factors associated with adherence to low tidal volume ventilation: a secondary analysis of the CHECKLIST-ICU database. Ann Intensive Care. 2020;10(1):68. doi: 10.1186/s13613-020-00687-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Soares M., Bozza F.A., Angus D.C., et al. Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med. 2015;41(12):2149–2160. doi: 10.1007/s00134-015-4076-7. [DOI] [PubMed] [Google Scholar]
- 33.Peres I.T., Bastos L.S.L., Gelli J.G.M., et al. Sociodemographic factors associated with COVID-19 in-hospital mortality in Brazil. Public Health. 2021;192:15–20. doi: 10.1016/j.puhe.2021.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Curtis J.R., Vincent J.-L. Ethics and end-of-life care for adults in the intensive care unit. Lancet. 2010;376(9749):1347–1353. doi: 10.1016/S0140-6736(10)60143-2. [DOI] [PubMed] [Google Scholar]
- 35.Goldfarb M.J., Bibas L., Bartlett V., Jones H., Khan N. Outcomes of patient- and family-centered care interventions in the ICU: a systematic review and meta-analysis. Crit Care Med. 2017;45(10):1751–1761. doi: 10.1097/CCM.0000000000002624. [DOI] [PubMed] [Google Scholar]
- 36.Avidan A., Sprung C.L., Schefold J.C., et al. Variations in end-of-life practices in intensive care units worldwide (Ethicus-2): a prospective observational study. Lancet Respir Med. 2021;9(10):1101–1110. doi: 10.1016/S2213-2600(21)00261-7. [DOI] [PubMed] [Google Scholar]
- 37.Lobo S.M., De Simoni F.H.B., Jakob S.M., et al. Decision-making on withholding or withdrawing life support in the ICU: a worldwide perspective. Chest. 2017;152(2):321–329. doi: 10.1016/j.chest.2017.04.176. [DOI] [PubMed] [Google Scholar]
- 38.Soares M. End of life care in Brazil: the long and winding road. Crit Care. 2011;15(1):110. doi: 10.1186/cc9962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kipper D.J., Piva J.P., Garcia P.C.R., et al. Evolution of the medical practices and modes of death on pediatric intensive care units in southern Brazil∗. Pediatr Crit Care Med. 2005;6(3):258–263. doi: 10.1097/01.PCC.0000154958.71041.37. [DOI] [PubMed] [Google Scholar]
- 40.Fumis R.R.L., Deheinzelin D. Respiratory support withdrawal in intensive care units: families, physicians and nurses views on two hypothetical clinical scenarios. Crit Care. 2010;14(6):R235. doi: 10.1186/cc9390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Institute of Medicine (US) Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations. Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations: A Letter Report. Altevogt BM, Stroud C, Hanson SL, Hanfling D, Gostin LO, eds. National Academies Press; 2009. [PubMed]
- 42.de Aragão N.S.C., Barbosa G.B., Santos C.L.C., et al. Burnout syndrome and associated factors in intensive care unit nurses. Rev Bras Enferm. 2021;74(suppl 3) doi: 10.1590/0034-7167-2019-0535. [DOI] [PubMed] [Google Scholar]
- 43.Embriaco N., Azoulay E., Barrau K., et al. High level of burnout in intensivists. Am J Respir Crit Care Med. 2007;175(7):686–692. doi: 10.1164/rccm.200608-1184OC. [DOI] [PubMed] [Google Scholar]
- 44.Embriaco N., Papazian L., Kentish-Barnes N., Pochard F., Azoulay E. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. 2007;13(5):482–488. doi: 10.1097/MCC.0b013e3282efd28a. [DOI] [PubMed] [Google Scholar]
- 45.Poncet M.C., Toullic P., Papazian L., et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175(7):698–704. doi: 10.1164/rccm.200606-806OC. [DOI] [PubMed] [Google Scholar]
- 46.Azoulay E., Timsit J.F., Sprung C.L., et al. Prevalence and factors of intensive care unit conflicts: the Conflicus Study. Am J Respir Crit Care Med. 2009;180(9):853–860. doi: 10.1164/rccm.200810-1614OC. [DOI] [PubMed] [Google Scholar]
- 47.West C.P., Dyrbye L.N., Sloan J.A., Shanafelt T.D. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24(12):1318–1321. doi: 10.1007/s11606-009-1129-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.