I read a recent article written by Dr. Toes-Zoutendijk et al. that described how the coronavirus disease (COVID)-19 pandemic affected colorectal cancer screening and its incidence in the Netherlands [1]. The impact of the COVID-19 pandemic on cancer diagnosis and treatment is a serious concern for healthcare providers, policymakers, and the general public since cancer deaths are the leading causes of death in many countries. The broad spectrum of oncological care was suspended to deal with critical COVID-19 patients in some COVID-19 high-burden countries such as the Netherlands [1,2]. This finding was totally compatible with a previous study from France, which reported decreased new case numbers of several cancers in 2020 [3]. Nonetheless, how the pandemic damaged cancer care in COVID-19 low-burden countries, such as Japan, has not been assessed as a nationwide research project.
This retrospective analysis using prospectively registered data was conducted. The hospital-based cancer registry that accumulates data from 849 hospitals, covers more than 70% of cancer cases in Japan [4]. This was initiated in 2007, and we were provided with data for 2016–2020.
Of the 24 registered cancers, the top 10 with the largest number of new cases were used for our analysis. The registry classified the treatments into 13 categories, including surgery, endoscopic surgery, radiotherapy, chemotherapy, and their combinations. These treatments that were administered within months in the hospital where the patient was diagnosed. In the present analysis, we present the number for surgery alone plus endoscopic surgery alone as “resected cases” since these treatment options were usually considered as radical treatment.
The number of diagnoses and resections, assuming no pandemic, was estimated with a regression line using the least squares method with only the year as an explanatory variable based on data from 2016 to 2019. The gap between the estimated and observed cases was regarded as the impact of the pandemic. The Thompson test was applied to evaluate whether the 2020 residual from the regression line was an outlier when the year 2020 had the largest negative residual. P = 0.05 was used as the criterion for statistical significance.
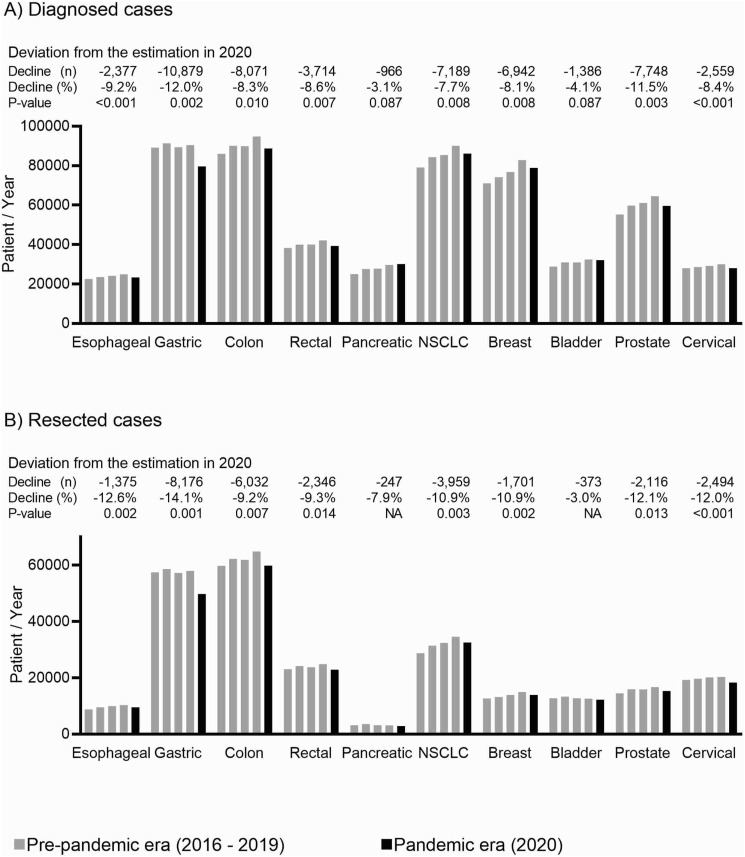
Of the 24 cancer types in the hospital-based cancer registry, the 10 cancers with the highest number of diagnoses are shown in Fig. 1 A. Compared to the estimation, the largest decreases in diagnosis were observed for gastric cancer (estimation 90,528; observed 79,649; deviation −10,879; −12.0%; P = 0.002) followed by colon cancer (estimation 96,765; observed 88,694; deviation −8071; −8.3%; P = 0.010). Prostate cancer diagnoses also declined by 11.5% (estimation 67,413; observed 59,665; deviation −7748; P = 0.003). We observed significant decreases in the incidence of esophageal, rectal, non-small cell lung, breast, and cervical cancers. The estimated total decrease in the diagnosis of the 10 cancers due to the pandemic was 51,829 (Fig. 1A). The lower-stage subgroups tended to have greater decreases in the estimation (Spearman's r = 0.58; P < 0.001).
Fig. 1.
Impact of the COVID-19 pandemic on cancer diagnosis and resection in 2020. NSCLC: non-small cell lung cancer. NA: not available.
The number of resections, sum of regular surgeries and endoscopic surgeries, was lower than the estimation for all cancers, except pancreatic and bladder cancers (Fig. 1B). In 2020, we estimated that the pandemic prevented 28,817 resections for 10 cancers, including 8176 gastric cancers, 6032 colon cancers, and 3959 non-small cell lung cancers.
Similar to the observation in the Netherlands by Dr. Toes-Zoutendijk et al. [1], diagnosis of colon and rectal cancers were greatly decreased due to the pandemic in Japan. Besides, numbers of resection of colorectal cancers decreased (Fig. 1B). The same is true for other cancers including esophageal, gastric, non-small cell lung, breast, prostate, and cervical cancers (Fig. 1B). In 2020, 3492 patients died directly from COVID-19, and eight times as many cancer patients lost their chance for resection in the COVID-19 low-burden country (Fig. 1B). Diagnostic and treatment delays of malignancies caused by the pandemic will deteriorate patient survival [5]. Avoidable cancer deaths damage not only the patient health but the economics of the region [6]. A greater decline in the diagnosis in early-stage cancers suggests that suspended screening affected cancer diagnosis in 2020. Randomized trials and meta-analyses have shown that cancer screening, including low-dose CT for lung cancer [7], fecal occult blood for colorectal cancer [8], and Pap smear for cervical cancer [9] can reduce deaths. Mammography for breast cancer may also prevent deaths from cancers [10]. We should continue these cancer screening with infection control measures even during COVID-19 pandemic [10].
Author contribution
Nobuyuki Horita worked on conception, data acquisition, analysis, interpretation, drafting, revision, final approval, and accountability.
Funding
None.
Conflict of interest statement
Nothing to declare.
References
- 1.Toes-Zoutendijk E., Vink G., Nagtegaal I.D., et al. Impact of COVID-19 and suspension of colorectal cancer screening on incidence and stage distribution of colorectal cancers in The Netherlands. Eur J Cancer. 2022;161:38–43. doi: 10.1016/j.ejca.2021.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Riera R., Bagattini  M., Pacheco R.L., Pachito D.V., Roitberg F., Ilbawi A. Delays and disruptions in cancer health care due to COVID-19 pandemic: systematic review. JCO Glob Oncol. 2021;7:311–323. doi: 10.1200/GO.20.00639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kempf E., Lamé G., Layese R., et al. New cancer cases at the time of SARS-Cov2 pandemic and related public health policies: a persistent and concerning decrease long after the end of the national lockdown. Eur J Cancer. 2021;150:260–267. doi: 10.1016/j.ejca.2021.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cancer Information Service, National Cancer Center, Japan. Annual report of hospital-based cancer registries. Avilable at https://jhcr-cs.ganjoho.jp/hbcrtables/. Accessed on December 1, 2021.
- 5.Bardet A., Fraslin A.M., Marghadi J., et al. Impact of COVID-19 on healthcare organisation and cancer outcomes. Eur J Cancer. 2021;153:123–132. doi: 10.1016/j.ejca.2021.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gheorghe A., Maringe C., Spice J., et al. Economic impact of avoidable cancer deaths caused by diagnostic delay during the COVID-19 pandemic: a national population-based modelling study in England, UK. Eur J Cancer. 2021;152:233–242. doi: 10.1016/j.ejca.2021.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sadate A., Occean B.V., Beregi J.P., et al. Systematic review and meta-analysis on the impact of lung cancer screening by low-dose computed tomography. Eur J Cancer. 2020;134:107–114. doi: 10.1016/j.ejca.2020.04.035. [DOI] [PubMed] [Google Scholar]
- 8.Hewitson P., Glasziou P., Irwig L., Towler B., Watson E. Screening for colorectal cancer using the faecal occult blood test, Hemoccult. Cochrane Database Syst Rev. 2007;2007(1) doi: 10.1002/14651858.CD001216.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peirson L., Fitzpatrick-Lewis D., Ciliska D., Warren R. Screening for cervical cancer: a systematic review and meta-analysis. Syst Rev. 2013;2:35. doi: 10.1186/2046-4053-2-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.U.S. Preventive services task force. Recommendations. Available at: https://uspreventiveservicestaskforce.org/uspstf/. Accessed on December 1, 2021.