Abstract
Background
COVID-19 may play a role in various immune-related dermatologic conditions. The relationship between COVID-19 and alopecia areata remains unclear.
Objective
To review the existing literature for clinical studies and reports investigating the association between new-onset alopecia areata or the exacerbation of preexisting alopecia areata following infection with SARS-CoV-2.
Methods
A systematic review of the literature was performed using PubMed, Embase, and MEDLINE databases from inception to October 2021. Included articles assessed alopecia areata following infection with SARS-CoV-2.
Results
Of 402 total articles, 9 were identified as meeting the inclusion criteria. Six articles described case reports of 7 patients with new-onset alopecia areata following confirmed infection with SARS-CoV-2, and 3 articles reported on alopecia areata recurrence or exacerbation following SARS-CoV-2 infection in patients with preexisting disease. Studies investigating the exacerbation or recurrence of alopecia areata following infection reported mixed findings.
Limitations
A majority of the included studies were case reports. The heterogeneity of articles precluded data synthesis.
Conclusion
Alopecia areata may be a dermatologic manifestation of COVID-19, with cases most often appearing 1 to 2 months following infection. Additional research is necessary to better elucidate the relationship and draw conclusions.
Key words: AA, alopecia areata, COVID-19, inflammation, SARS-CoV-2
Capsule Summary.
-
•
This study synthesizes various independent reports of patient experience with alopecia areata following infection with SARS-CoV-2.
-
•
Assessing the existing literature of alopecia areata following infection with SARS-CoV-2 may assist dermatologists in identifying patients at risk for alopecia areata and educating these patients on seeking dermatologic care should hair loss occur.
Introduction
COVID-19, caused by viral infection of SARS-CoV-2, is characterized by systemic activation of the immune system. Research over the past 2 years has elucidated the relationship between COVID-19 and various immune-related dermatologic conditions.1,2 Alopecia areata is an autoimmune disease characterized by nonscarring hair loss of the scalp, face, or body that can cause severe psychologic distress and affects approximately 2% of the population.3 Currently, the relationship between COVID-19 and alopecia areata remains unclear. A study in Turkey assessing the number of alopecia areata cases in an outpatient dermatology clinic following the COVID-19 outbreak reported an increase in the percentage of patients with alopecia areata from 0.97% before the pandemic to 1.48% 2 months after the pandemic. Given that alopecia areata can worsen in response to both immune dysregulation and psychosocial stress, the lack of data collected in the study on infection rates makes it challenging to decipher whether this increase is related to emotional distress or the virus itself.4
The pathophysiology of alopecia areata is not well understood; however, current theories involve the loss of immune privilege within the hair follicle, leading to a dysregulated immune response.5 Viruses such as SARS-CoV-2 may play an important role in the development, recurrence, or exacerbation of alopecia areata in infected patients. In better elucidating the association, if any, between alopecia areata and COVID-19, clinicians will have the tools to focus their history taking, increase the accuracy of diagnoses, and, ultimately, improve patient outcomes. The purpose of this systematic review was to review the existing literature for clinical studies and reports investigating the development of new-onset alopecia areata or the exacerbation of preexisting alopecia areata following infection with SARS-CoV-2.
Methods
This systematic review followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. To identify literature from inception to October 23, 2021, the following search strategy was used within the PubMed, Embase, and MEDLINE databases: (“COVID-19” OR “coronavirus” OR “2019-nCoV” OR “SARS-CoV-2”) AND (“alopecia”). Studies were included if they assessed the development of alopecia areata following infection with SARS-CoV-2 or the deterioration or recurrence of preexisting alopecia areata following infection. Articles assessing types of nonscarring alopecia (ie, telogen effluvium, androgenetic alopecia) and scarring alopecia were not included. Studies were excluded if they were the wrong publication type (ie, letter to the editor, reviews) or in a language other than English. An independent reviewer (R.E.C.) screened titles and abstracts, followed by full-text articles. The following data were extracted from articles meeting inclusion criteria when available: study design, new-onset or exacerbation of alopecia areata, patient gender, patient age, COVID-19 symptoms, treatment received for COVID-19, time to alopecia areata diagnosis following COVID-19, clinical presentation of alopecia areata, treatment received for alopecia areata, time to alopecia areata improvement, family history of alopecia areata, and patient medical history. An independent reviewer (R.E.C.) assessed risk of bias in the included studies using the National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies and the Joanna Briggs Institute Critical Appraisal Checklist for Case Reports.
Results
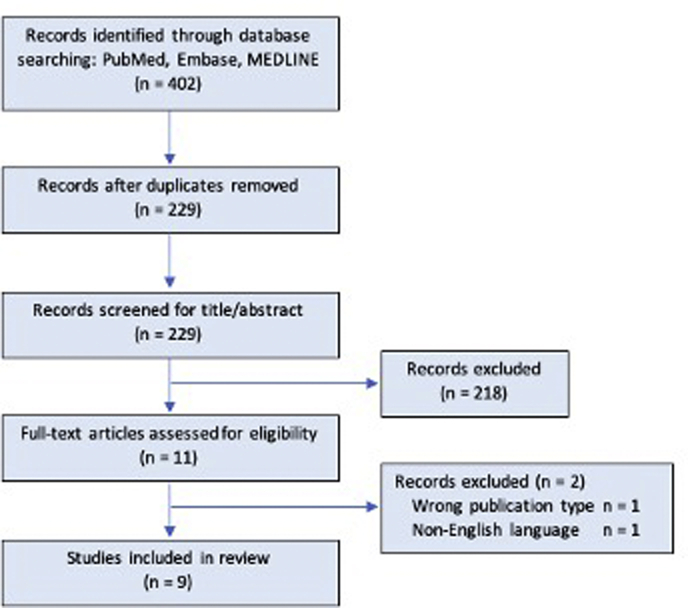
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram is available in Fig 1. In total, 402 records were identified and, after the removal of duplicates, 229 were screened. Overall, 9 articles met the inclusion criteria and were summarized in this review. Six articles described case reports of 7 patients with new-onset alopecia areata following confirmed infection with SARS-CoV-2, and 3 articles reported on alopecia areata recurrence or exacerbation following SARS-CoV-2 infection in patients with preexisting disease. Included studies were published between November 2020 and September 2021, with 89% published in 2021. Four studies were from Italy, 2 from Turkey, and 1 each from the United States, Brazil, and Poland.
Fig 1.
Flow diagram of the systematic study selection process.
Individual patient characteristics for reports of new-onset alopecia areata following SARS-CoV-2 infection are outlined in Table I.6, 7, 8, 9, 10, 11 The average age of the patients was 37 years (range, 13-56 years). Four patients (57%) were female, and 3 patients (43%) were male. No patients had a personal or family history of alopecia areata. In 3 cases for which COVID-19 severity was assessed, 100% of patients experienced mild respiratory symptoms. One patient experienced the loss of taste and smell and began experiencing hair loss while symptomatic. In 3 cases for which COVID-19 treatment was assessed, 1 patient received paracetamol alone, 1 received paracetamol and azithromycin, and 1 received a 7-day course of hydroxychloroquine.
Table I.
Reports of new-onset alopecia areata after infection with SARS-CoV-2
| Case report | Age, y | Sex | Time to diagnosis after COVID-19 | Clinical presentation |
|---|---|---|---|---|
| Rossi et al6 | 29 | Female | 4 wk | Patchy hair loss on vertex and parietal regions progressing to the involvement of the total scalp |
| Hayran et al7 | 13 | Male | 4 wk | Single 1-cm alopecic patch on scalp |
| Capalbo et al8 | 38 | Male | 4 wk | Variously distributed, sharply demarcated alopecic patches of the beard |
| Flvenson9 | 56 | Female | 8 wk | Loss of >99% of all body hair |
| Sgubbi et al10 | 54 | Female | 8 wk | Rapid onset of multiple patches of alopecia on the tempero-parietal area of scalp |
| Temiz and Kutlu11 | 43 | Male | 6 wk | Not reported |
| Temiz and Kutlu11 | 39 | Female | 8 wk | Not reported |
Of the 3 articles that investigated the relationship between SARS-CoV-2 infection and exacerbation of preexisting alopecia areata, 1 was a retrospective analysis, 1 was a cross-sectional study, and 1 was a case report. Variability in reported data among articles made comparisons impractical. In their retrospective analysis of 32 patients with alopecia areata and COVID-19, Rudnicka et al12 found that patients experienced no significant worsening of alopecia areata symptoms as measured by the severity of alopecia tool score in the 6 months following their infection. Of note, a majority of patients included in the study were on active alopecia areata treatment at the time of SARS-CoV-2 infection. In a larger study, Rinaldi et al13 employed a questionnaire to assess the effects of COVID-19 on alopecia areata relapse. A total of 389 patients (of 475 invited patients) affected by alopecia areata in the past 2 years completed the survey between March and October 2020. Of the 34% of participants who reported contracting SARS-CoV-2, 44% reported a relapse of alopecia areata at a median of 2.14 months following infection compared with only 12% of COVID-19–negative patients reporting relapse. Finally, Berbert Ferreira et al14 reported a case of a 24-year-old woman with alopecia areata totalis, successfully managed with tofacitinib 5 mg twice a day for the past 12 months, who tested positive for SARS-CoV-2 after experiencing loss of smell and taste. Tofacitinib was discontinued for 2 weeks following diagnosis, at which point the patient experienced rapid-onset and severe anagen effluvium. After 2 weeks, tofacitinib was restarted; however, the patient did not show clinical improvement even after 3 months.
Discussion
This systematic review identified 9 published studies on the development or exacerbation of alopecia areata following infection with SARS-CoV-2. Seven case reports provide insight into the variability of patients who may experience new-onset alopecia areata following COVID-19. Studies investigating the exacerbation or recurrence of alopecia areata following infection report mixed findings. Overall, these results suggest that alopecia areata may be a dermatologic manifestation of COVID-19, with cases most often appearing 1 to 2 months following infection. However, the heterogeneity of study designs and a high proportion of case reports make it challenging to draw any conclusions, and further research is necessary to better elucidate the relationship between the clinical course of alopecia areata and COVID-19.
Worsening of alopecia areata is multifactorial. Physical stress on the body secondary to an infection, such as that with SARS-CoV-2, may have important implications in a patient’s deterioration. Likewise, a heavy psychosocial burden secondary to a major life stressor, such as a pandemic, may also play a central role in exacerbation of the underlying disease.15,16 This presents a major limitation in not only the existing literature presented in this review but also future research investigating the relationship between alopecia areata and COVID-19. Teasing apart these underlying factors, although difficult, is critical to understand this relationship.
In better understanding whether an association between alopecia areata and COVID-19 exists, dermatologists can be more prepared to diagnose and manage patients presenting with postinfection hair loss. Conversely, patients can be educated on the risk of the development of hair loss in the 1 to 2 months span following COVID-19 and encouraged to seek dermatologic care should this occur. Finally, the dermatologic manifestations of COVID-19 can cause significant anxiety, depression, and psychosocial stress in afflicted patients. A strong awareness among dermatologists, psychiatrists, and primary care physicians of the potential dermatologic diseases that can occur following COVID-19 provides an opportunity for these providers to screen for psychopathology and offer the appropriate services and support if necessary.
Limitations of the current study include the use of a single reviewer for article screening, risk of bias assessment, and data extraction. The current study also included a limited number of heterogeneous articles, with a high proportion of case reports. Despite the limited data available, this systematic review provides clinicians with an up-to-date compilation of all existing evidence that may prove useful when making diagnostic and treatment decisions. Moreover, increasing awareness of the possible link between alopecia areata and COVID-19 may ultimately increase the number of published reports in the literature.
Conclusion
Since the beginning of the COVID-19 pandemic in December 2019, various cases on the development of alopecia areata in the 2 months following COVID-19 have been reported. Other studies investigating the worsening of preexisting alopecia areata in afflicted patients are limited and have produced inconclusive results. An informed understanding of this relationship may improve patient outcomes both in terms of dermatologic treatment and psychologic well-being. Further research is required to definitively evaluate the association between COVID-19 and development or exacerbation of alopecia areata.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
Accepted for publication February 3, 2022.
References
- 1.Schwartzberg L.N., Advani S., Clancy D.C., Lin A., Jorizzo J.L. A systematic review of dermatologic manifestations among adult patients with COVID-19 diagnosis. Skin Health Dis. 2021;1(2) doi: 10.1002/ski2.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matar S., Oulès B., Sohier P., et al. Cutaneous manifestations in SARS-CoV-2 infection (COVID-19): a French experience and a systematic review of the literature. J Eur Acad Dermatol Venereol. 2020;34(11):e686–e689. doi: 10.1111/jdv.16775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee H.H., Gwillim E., Patel K.R., et al. Epidemiology of alopecia areata, ophiasis, totalis, and universalis: a systematic review and meta-analysis. J Am Acad Dermatol. 2020;82(3):675–682. doi: 10.1016/j.jaad.2019.08.032. [DOI] [PubMed] [Google Scholar]
- 4.Kutlu Ö, Aktaş H, İmren IG, Metin A. Short-term stress-related increasing cases of alopecia areata during the COVID-19 pandemic. J Dermatolog Treat. Published online June 19, 2020. 10.1080/09546634.2020.1782820 [DOI] [PubMed]
- 5.Zhou C., Li X., Wang C., Zhang J. Alopecia areata: an update on etiopathogenesis, diagnosis, and management. Clin Rev Allergy Immunol. 2021;61(3):403–423. doi: 10.1007/s12016-021-08883-0. [DOI] [PubMed] [Google Scholar]
- 6.Rossi A., Magri F., Michelini S., et al. New onset of alopecia areata in a patient with SARS-CoV-2 infection: possible pathogenetic correlations? J Cosmet Dermatol. 2021;20(7):2004–2005. doi: 10.1111/jocd.14080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hayran Y., Yorulmaz A., Gür G., Aktaş A. Different hair loss patterns in two pediatric patients with COVID-19-associated multisystem inflammatory syndrome in children. Dermatol Ther. 2021;34(2) doi: 10.1111/dth.14820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Capalbo A., Giordano D., Gagliostro N., et al. Alopecia areata in a COVID-19 patient: a case report. Dermatol Ther. 2021;34(2) doi: 10.1111/dth.14685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flvenson D. COVID-19: association with rapidly progressive forms of alopecia areata. Int J Dermatol. 2021;60(1):127. doi: 10.1111/ijd.15317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sgubbi P., Savoia F., Calderoni O., Longo R., Stinchi C., Tabanelli M. Alopecia areata in a patient with SARS-CoV-2 infection. Dermatol Ther. 2020;33(6) doi: 10.1111/dth.14295. [DOI] [PubMed] [Google Scholar]
- 11.Temiz S.A., Kutlu Ö. The development of dermatologic diseases in patients recovered from COVID-19. Dermatol Ther. 2021;34(2) doi: 10.1111/dth.14791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rudnicka L., Rakowska A., Waskiel-Burnat A., Kurzeja M., Olszewska M. Mild-to-moderate COVID-19 is not associated with worsening of alopecia areata: a retrospective analysis of 32 patients. J Am Acad Dermatol. 2021;85(3):723–725. doi: 10.1016/j.jaad.2021.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rinaldi F., Trink A., Giuliani G., Pinto D. Italian survey for the evaluation of the effects of coronavirus disease 2019 (COVID-19) pandemic on alopecia areata recurrence. Dermatol Ther (Heidelb) 2021;11(2):339–345. doi: 10.1007/s13555-021-00498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berbert Ferreira S., Gavazzoni Dias M.F.R., Berbert Ferreira R., Neves Neto A.C., Trüeb R.M., Lupi O. Rapidly progressive alopecia areata totalis in a COVID-19 patient, unresponsive to tofacitinib. J Eur Acad Dermatol Venereol. 2021;35(7):e411–e412. doi: 10.1111/jdv.17170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chrousos G.P. The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. N Engl J Med. 1995;332(20):1351–1362. doi: 10.1056/NEJM199505183322008. [DOI] [PubMed] [Google Scholar]
- 16.Azzawi S., Penzi L.R., Senna M.M. Immune privilege collapse and alopecia development: is stress a factor. Skin Appendage Disord. 2018;4(4):236–244. doi: 10.1159/000485080. [DOI] [PMC free article] [PubMed] [Google Scholar]