COVID-19 placed unprecedented strain on the US health care system and revealed critical deficits in resources and planning. Beginning with a shortage of adequate personal protective equipment (PPE) and continuing with shortages of staff, supplies, and space, all hospitals faced crisis conditions that placed patients and staff at risk. Three related issues in addressing these crisis conditions hold key lessons:
-
•
Crisis standards of care (CSC) principles1., 2., 3. were often applied during shortages, but written plans and assumptions usually failed to meet the needs of the situation.4
-
•
COVID-19 disproportionately affected already-underserved communities.5 Rural areas and communities of color were particularly affected, forcing attention on how to improve equity and access to care before and during disasters.
-
•
Providers often suffered the severe moral distress of bedside rationing decisions, as well as working under physical and cognitive load conditions that increased the odds for error. Modeling suggests that surge conditions in hospitals caused a nearly 25% increase over expected COVID-19 mortality.6
In this article, we review some of the key gaps in planning and provide recommendations for hospitals that can help ensure the ability to respond effectively and justly across the range of conventional, contingency, and crisis conditions (Box 1).2
Box 1. Definitions of Conventional, Contingency, and Crisis Care.
Conventional care: Usual resources and level of care provided through maximal use of the facility's usual beds, staff, and resources.
Contingency care: Care provided is adapted from usual practices to expand capacity (for example, boarding critical care patients in postanesthesia care areas), but the quality of care provided to patients remains functionally equivalent to usual care.
Crisis care: Inadequate resources are available to provide usual quality of care for all patients—care is provided to the level possible given the resource gap. Significant increased risk of morbidity and mortality defines the care provided in this phase—this risk can be minimized by implementing consistent proactive resource use strategies.
Alt-text: Unlabelled box
These apparently discrete tiers actually exist across a continuum in practice. The three tiers are useful conceptually for planning and triggering use of specific strategies and requests for assistance, but the degradation in quality of care may be difficult to categorize, particularly between contingency and crisis. The emphasis on planning should be to extend the contingency phase as much as possible before crisis requires active triage of resources. This may involve deliberate changes in staffing, conservation of resources, redeployment of resources, and other mitigation strategies.
The transition zone between contingency and crisis can still be complicated for providers. For example, if a patient with a transient ischemic attack is discharged to an expedited outpatient workup because no inpatient beds are available, does this represent late contingency or early crisis care? Because these decisions are being made due to the need to triage resources, these care decisions should be regarded as crisis conditions, and every attempt should be made to equalize the risk to patients across the facility and within the surrounding region.
Lessons Learned from COVID-19
CSC plans in place at the time of COVID-19 often assumed a rapid descent into pervasive crisis conditions from a catastrophic disaster. Although US hospitals often experience temporary crisis conditions from a no-notice incident, these are usually rapidly mitigated by sending resources to and transferring patients from the affected facility or area. No prior disaster, to our knowledge, has required state “declarations” or formal activation of CSC.
COVID-19, a protracted and international disaster, has been very different. Staffing, PPE, ICU space, vaccines, antiviral, and many other shortages have ebbed and flowed, requiring rapid adaptation and frequently revised guidance. Resource conditions often fluctuated from day to day such that dialysis or staffing was felt to be in contingency mode (not presenting significant risk for patients) on some shifts and in crisis (substantial risk to patients) on others.
Communication, information sharing, and the ability to adapt policies and practices in a timely manner and consistent with community practice proved essential to providing the best care possible. Engagement with elected leaders and the executive branch of state government was unprecedented, leading to the largest number of disaster declarations related to health care service delivery in US history. In many cases, however, state government did not acknowledge or address crisis conditions. This was problematic for hospitals that were relying on state actions to enable activation of their CSC plans.
Within many hospitals, a breakdown in understanding between “boardroom and bedside” led to significant provider frustrations that crisis conditions were not being recognized and addressed. Sometimes, these conditions clearly represented a threat to patient safety. At other times, the caregiver burdens (physical and mental) met their personal definition of placing patients at risk—even if incident command did not regard the strategies being used as consistent with a crisis situation. There is no easy way to categorize these situations, but the perception that state and facility leadership was not understanding the level of stress or supporting the providers in crisis was problematic.
In many hospitals there was confusion about who should be responsible for making scarce resource allocation decisions, what guidance to provide to bedside teams, and how triage decisions should be coordinated at the facility vs. the regional and state level. Further, providers often felt that the triage teams specified in many hospital plans were designed to address triage of ventilators and other resources irrelevant to the problems they were facing. The triage team concept was difficult to implement, often because it involved consultation with a large team of individuals and/or processes that could not render timely decisions.1 , 4
The lack of clinical guidance often resulted in ad hoc bedside decisions, which not infrequently resulted in “implicit triage,” in which the providers withheld interventions based on their interpretation of the likelihood of benefit vs. the resources available. These ad hoc rationing decisions risk being inconsistent with the actual resource situation and blur a key distinction between determining that a patient cannot benefit from care and withholding care that might benefit a patient due to resource shortages. These decisions often inflict severe moral distress as well as patient harm.
Despite more than a decade of work focused on preparing for catastrophic health emergencies, few state health departments, health care coalitions, or health care systems had planned for the process of implementing crisis care strategies, instead often concentrating on protocols for triaging specific interventions such as ventilators. Unfortunately, explicit CSC planning requirements under the US Department of Health and Human Services, Office of the Assistant Secretary for Preparedness and Response (HHS/ASPR) Hospital Preparedness Program (HPP) were scheduled as deliverables at the state level in 2020 and coalition level in 2021.7 The Joint Commission, the primary accrediting body of hospitals whose requirements shape the preparedness efforts at most facilities, did not include planning requirements for crisis conditions in their 2022 emergency management standards,8 though additions are under consideration.
In hospitals that had CSC plans prior to COVID-19, several common weaknesses emerged during the response. CSC plans were generally stand-alone annexes, disconnected from hospital disaster response plans and exercises, and not integrated well with facility surge strategies. Most focused on using triage teams to determine who received resources—most often ventilators, which never were in systemic shortage—but they did not describe processes for more frequent but more elastic decisions about resources such as staff or dialysis. Often, the Sequential Organ Failure Assessment (SOFA) score was proposed as a triage tool. Unfortunately, SOFA has inadequate prognostic accuracy and does not differentiate between acute and chronic renal failure and therefore (particularly in the setting of primary respiratory illness) biases scoring against those with preexisting disease.8 , 9 As the pandemic has progressed, emphasis9 has shifted from determining who would benefit most from resources to determining who might suffer the least harm if a resource that is in shortage were to be withheld (for example, restricting or withdrawing nonbeneficial care).10
Surges across cities and regions have presented equity concerns, starting with New York City, where facilities serving marginalized communities were overwhelmed compared to nearby facilities serving higher-income communities. There was no system to balance the load, and transfers were often difficult or refused. More recently, many states have experienced rural-urban equity issues when tertiary centers became saturated and did not accept referrals from smaller (often critical access) hospitals. Although telemedicine provided some support, patient care often suffered, as major delays for time-sensitive interventions such as surgery, endoscopy, and dialysis occurred. Load-balancing solutions, including statewide call centers,11 often helped find destinations for patients. However, when capacity became saturated there was often no policy or authority to compel facilities to accept transfers.
Finally, despite an early focus on alternate care sites, these locations generally failed to contribute meaningfully to capacity aside from a few smaller communities that had very high inpatient volumes—often due to large rural catchment areas.12 Alternate care locations on the hospital campus often were a better solution, although staffing these locations proved a major challenge.
Areas of Emphasis for Planning and Policy
Hospitals should use the pandemic learnings to ensure that emergency plans better address the spectrum of care delivery that ranges from conventional to crisis conditions based on availability of key resources (Box 1 and Table 1 14 , 19).
Table 1.
Action Steps for Hospitals
| Command |
|
| Coordination |
|
| Clinical |
|
| Staff13,14 |
|
| Space |
|
| Supplies |
|
| Services |
|
| Special |
|
EMS, emergency medical services; ESF, Emergency Support Function; MOCC, Medical Operations Coordination Cell; ECMO, extracorporeal membrane oxygenation.
1. Most hospital surge plans need revision. Plans should incorporate a scaled expansion of space and redeployments of staff, starting with conventional assets and continuing through contingency and then crisis, using a stepwise progression. As the number of patients increases, and the availability of staff and other key resources decreases, changes to the type of care that can be delivered and how it is delivered must be described. Conditions that define a crisis should be delineated whenever possible (for example, by using specific triggers, such as staff at > 200% of normal patient care ratios, or providers having to ration treatment in a way that puts patients at significant risk). Hospitals should have plans to rapidly implement regional assistance and coordination when these conditions arise.
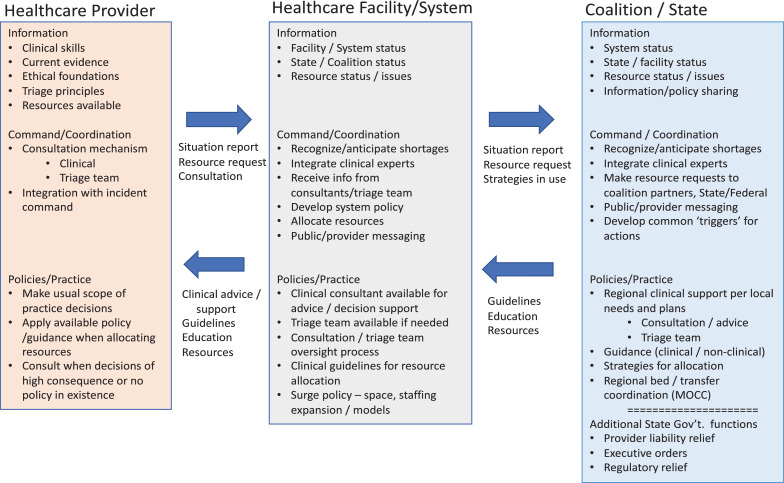
2. Crisis conditions will require both a facility and a regional response, whether or not they have been declared. Hospitals in crisis must adapt to the situation until it can be mitigated by bringing in resources or transferring patients. Key to this adaptation is the integration of the incident command team with both bedside providers and the health care coalition or emergency management agency coordinating the regional response. Roles and responsibilities should be understood across these domains, as each level both gives and receives information and support (Figure 1 4). Facility incident command should share information with regional partners and seek to mitigate shortages through resource requests as well as through development and circulation of recommended strategies. Ideally, development of these strategies should be consistent across the health care system and region with affirmation/endorsement by state public health agencies. In this way, shortages can be rapidly recognized, subject matter experts can be engaged to ensure the best care recommendations possible, and resources and response strategies can be coordinated across the area.
Figure 1.
Shown here are the key domains and requirements in crisis standards of care. Reprinted from Hick et al. with permission.
* This is a capsule summary of progression—the facility should include specific plans for consultation, triage team, and so on.
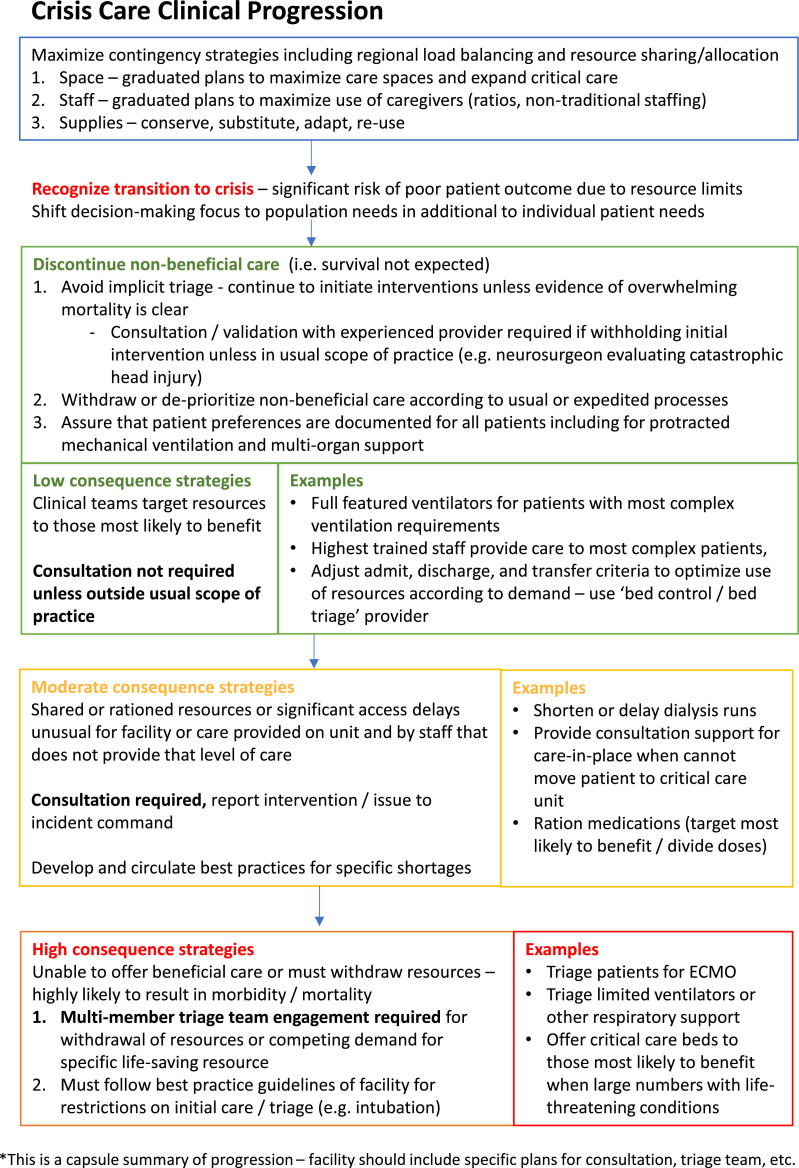
3. The hospital should plan clinical strategies that facilitate unit or service line adaptations to evolving conditions (Table 2 ). Raising thresholds for unit admission and lowering them for discharge from the unit, triaging patients to the most appropriate inpatient bed (bed triage), defining when triage teams are used and their components and activation, as well as considering how crisis conditions are documented in the medical record (for example, documenting why a patient was discharged who normally would be admitted) are all important components of hospital crisis response. Most crisis care adjustments will revolve around lack of specific beds (for example, critical care), staff (for example, respiratory therapy), or supplies (for example, medications). Decisions about reallocation of life support will be rare. Hospitals will face decisions and should have policies on withdrawal of futile care and for when to curtail nonbeneficial and inappropriate care based on the resource situation.15 As the risk of the rationing increases, so should the engagement of consultants and teams to assist with decision making (Figure 2 ). A review process for guidelines and triage team decisions is also required to ensure that they are operationally, medically, ethically, and equitably sound. Triage teams should conduct an individualized assessment of the patient using information from the treating provider as well as diagnosis-specific prognostic factors. Validated clinical risk scores may provide decision support but should not be the dominant basis for decisions, and proactive efforts should be made to minimize the risk of bias in triage decisions.16 Triage teams and incident command should have a view of local and regional resource availability, and may need to engage regional consultation to support real-time decisions (for example, for services such as extracorporeal membrane oxygenation [ECMO]).
Table 2.
Clinical Prioritization by Phase of Care.
| Clinical Team/Provider | Organizational Support | |
|---|---|---|
| Initial Interventions | Restrict interventions only when:
|
|
| Admission/ transfer decision |
Adjust threshold for admission according to resources available.
|
|
| Ongoing care | Assess resources required vs. benefit.
|
|
ECMO, extracorporeal membrane oxygenation.
Figure 2.
This flowchart illustrates the clinical progression of crisis care. ECMO, extracorporeal membrane oxygenation.
4. Guidance and consultation should be available to clinicians facing unusual allocation decisions. Providers make frequent small allocation decisions in the course of usual practice, such as triaging waiting patients in the emergency department. But the allocation decisions required in a crisis can be much more consequential, complex, and distressing. CSC plans must establish a process for providing clinical guidance or consultation with specialists/colleagues when a clinician is forced to make a rationing decision that is not normally in their scope of practice but that does not require activation of a triage team. Examples include deciding whether to intubate a patient in the emergency department relative to other strategies, or how to best ration dialysis duration and timing.
Consultation and/or written clinical guidance for making allocation decisions protects the bedside team from moral distress and potential liabilities as well as facilitates consistent delivery of the best care possible under the circumstances. Relatedly, when conditions are such that clinicians must operate outside their scope of practice, the incident command team must be aware of these conditions.
By implementing and training on an emergency response plan, the hospital and its care providers gain a degree of legal protection as compared with having no plan and making ad hoc decisions in crisis. Hospital leadership must be engaged in the development of these plans and stand behind the processes and recommended clinical practices. Some states offer broader legal protections for providers and facilities during crisis conditions, while others offer few or no additional protections. Being familiar with the legal protections available is important when disaster strikes, but more important is providing care that is as consistent as possible with that provided in other facilities in the area and with common strategies.
5. Coordination across a state or region is imperative. This requires engagement and participation of all stakeholders in a regional response structure, promotion of information sharing (both subjective and objective), and coordination of response policies. Health care coalitions (which usually involve regional hospitals, emergency medical services, public health, and emergency management) are critical structures to accomplish this coordination. Integrated health care delivery systems must promote consistency within their system but also must interface with regional partners and plans. Understanding local processes, having visibility on available resources, and knowing where to go for resource assistance are critical to returning to conventional operations as rapidly as possible. Coordination may include patient transfers (load balancing) or moving staff or resources to hospitals in crisis from facilities that have more resources.
The COVID-19 response has demonstrated the value of Medical Operations Coordination Cells (MOCCs)11 or similar coordinating centers with access to current bed and capacity data.17 , 18 Efforts to load-balance overwhelmed hospitals or determine which patients should be moved to or from specialty centers (for example, trauma, burn, pediatric) are core disaster response functions facilitated by the MOCC or similar entity. Coordination requires integration of information, involvement of medical providers who can triage the patients for transfer, and engagement with state and local authorities as well as emergency medical services. MOCC functions should be integrated into the coalition / regional planning and exercises required as part of the HPP cooperative agreement.7 The MOCC may also coordinate regional access to limited resources such as ECMO.13 , 19
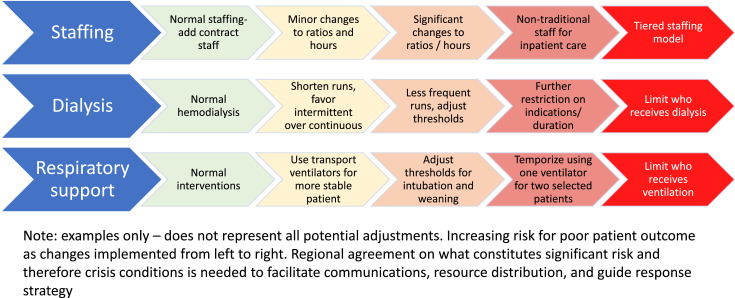
6. Consider documenting best practices for common resource challenges prior to an incident. Allocation decisions are frequent in health care. Whether the shortage is daily or disaster-related, if we have sound processes, develop clinical guidance, and provide consultation to clinicians, we can improve access, advance fairness, and decrease distress. Medication and other shortages that require rationing are an opportunity to use processes and develop guidance for contingency situations. Staffing, critical care space, blood products, and dialysis, burn, pediatric, and trauma surgery resources also lend themselves to proactive guidance development for contingency and crisis conditions (Figure 34). The HHS/ASPR HPP has requirements for all-hazard and specialty (burn, pediatric, infectious disease, radiation) regional response plans that can provide key support to developing these systems and strategies at the facility and health care coalition level.7
Figure 3.
Shown here is a sample progression of adaptive strategies for selected resources from conventional care to crisis care. Reprinted from Hick et al. with permission.
Conclusion
Surge capacity plans should include graded strategies for addressing shortages of space and staffing in particular, and when crisis conditions exist these must be implemented in a systematic fashion regardless of state or other actions. Surge plans should emphasize rapid care expansion to avoid crisis conditions by increasing capacity while maintaining contingency practices with minimal risk to patients. Facility plans must integrate with regional coordination and response strategies, including load-balancing mechanisms such as MOCC or transfer centers that have authorities and plans for when system capacity is reached.
Through planning, educating, and exercising, we can prepare our staff and systems to respond flexibly to the demands of a disaster while maximizing services and minimizing risk to patients and moral distress of providers. This “jazz band” approach of adapting to evolving conditions while staying in harmony both within the facility and with the community is inherently important in daily care as well as disaster care as conditions of scarcity become more and more common.
Acknowledgments
Conflicts of Interest
All authors report no conflicts of interest.
References
- 1.Institute of Medicine . National Academies Press; Washington, DC: 2012. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response, vol. 1: Introduction and CSC Framework.https://www.nap.edu/read/13351 Accessed Feb 21, 2022. [PubMed] [Google Scholar]
- 2.Hick JL, Barbera JA, Kelen GD. Refining surge capacity: conventional, contingency, and crisis capacity. Disaster Med Public Health Prep. 2009;3:S59–S67. doi: 10.1097/DMP.0b013e31819f1ae2. [DOI] [PubMed] [Google Scholar]
- 3.Maves RC, et al. Triage of scarce critical care resources in COVID-19: an implementation guide for regional allocation: an expert panel report of the Task Force for Mass Critical Care and the American College of Chest Physicians. Chest. 2020;158:212–225. doi: 10.1016/j.chest.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hick JL, et al. Crisis standards of care and COVID-19: what did we learn? How do we ensure equity? What should we do? NAM Perspect. 2021 Aug 30 doi: 10.31478/202108e. 2021:10.31478/202108e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manchanda EC, Couillard C, Sivashanker K. Inequity in crisis standards of care. N Engl J Med. 2020 Jul 23;383:e16. doi: 10.1056/NEJMp2011359. [DOI] [PubMed] [Google Scholar]
- 6.Kadri SS. Association between caseload surge and COVID-19 survival in 558 U.S. hospitals, March to August 2020. Ann Intern Med. 2021;174:1240–1251. doi: 10.7326/M21-1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.US Department of Health and Human Services, Office of the Assistant Secretary for Preparedness and Response. Hospital Preparedness Program (HHP). Sep 23, 2021. Accessed Feb 21, 2022. https://www.phe.gov/Preparedness/planning/hpp/Pages/default.aspx.
- 8.The Joint Commission. New and revised standards in emergency management. R3 Report, Issue 34. Dec 2021. https://www.jointcommission.org/-/media/tjc/documents/standards/r3-reports/final-r3-report-emergency-management.pdf.
- 9.US Department of Health and Human Services. SOFA Score: What It Is and How to Use It in Triage. (Updated: Dec 21, 2020.) Accessed Feb 21, 2022. https://files.asprtracie.hhs.gov/documents/aspr-tracie-sofa-score-fact-sheet.pdf.
- 10.Wynia MK, Sottile PD. Ethical triage demands a better triage survivability score. Am J Bioeth. 2020;20(7):75–77. doi: 10.1080/15265161.2020.1779412. [DOI] [PubMed] [Google Scholar]
- 11.US Department of Health and Human Services . 2nd ed. Medical Operations Coordination Cells Toolkit; Nov 2021. Office of the Assistant Secretary for Preparedness and Response; Technical Resources, Assistance Center, and Information Exchange.https://files.asprtracie.hhs.gov/documents/fema-mocc-toolkit.pdf Accessed Feb 21, 2021. [Google Scholar]
- 12.Breyre AM, et al. Establishment of an alternate care site (ACS) in Imperial County during COVID-19. West J Emerg Med. 2021 Mar 25;22:608–613. doi: 10.5811/westjem.2020.12.49237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prekker ME, et al. Regional planning for extracorporeal membrane oxygenation during coronavirus disease 2019. Chest. 2020;158:603–607. doi: 10.1016/j.chest.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Academies of Science, Engineering, and Medicine . National Academies Press; Washington, DC: 2020. Rapid Expert Consultation on Staffing Considerations for Crisis Standards of Care for the COVID-19 Pandemic (July 28, 2020)https://www.nap.edu/read/25890 Accessed Feb 21, 2022. [Google Scholar]
- 15.Nelson CM, Nazareth BA. Nonbeneficial treatment and conflict resolution: building consensus. Perm J. 2013;17(3):23–27. doi: 10.7812/TPP/12-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.US Department of Health and Human Services, Office for Civil Rights. Civil Rights and COVID-19. (Updated: Feb 4, 2022.) Accessed Feb 21, 2022. https://www.hhs.gov/civil-rights/for-providers/civil-rights-covid19/index.html.
- 17.Valin JP, et. al. Physician executives guide a successful COVID-19 response in Colorado. NEJM Catalyst. Epub 2021 Oct 15. Accessed Feb 21, 2022. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0402.
- 18.Villarroel L. Collaboration on the Arizona surge line: how COVID-19 became the impetus for private, public, and federal hospitals to function as one system. NEJM Catalyst. Epub. 2021 Jan 22 https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0595 Accessed Feb 21, 2022. [Google Scholar]
- 19.US Dept. of Health and Human Services . Healthcare Provider Shortages: Resources and Strategies for Meeting Demand; 2021. Office of the Assistant Secretary for Preparedness and Response; Technical Resources, Assistance Center, and Information Exchange (TRACIE)https://files.asprtracie.hhs.gov/documents/healthcare-workforce-strategies-for-managing-a-surge-in-healthcare-provider-demand.pdf Accessed Feb 21, 2022. [Google Scholar]