Abstract
Background:
Due to invasive treatments and stressors related to heart health, adults with congenital heart defects (CHDs) may have an increased risk of post-traumatic stress disorder (PTSD), anxiety, and/or depressive disorders. Our objectives were to estimate the prevalence of these disorders among individuals with CHDs.
Methods:
Using IBM® MarketScan® Databases, we identified adults age 18–49 years with ≥2 outpatient anxiety/depressive disorder claims on separate dates or ≥1 inpatient anxiety/depressive disorder claim in 2017. CHDs were defined as ≥2 outpatient CHD claims ≥30 days apart or ≥1 inpatient CHD claim documented in 2007–2017. We used log-binomial regression to estimate adjusted prevalence ratios (aPR) and 95% confidence intervals (CI) for associations between CHDs and anxiety/depressive disorders.
Results:
Of 13,807 adults with CHDs, 12.4% were diagnosed with an anxiety or depressive disorder. Adults with CHDs, compared to the 5,408,094 without CHDs, had higher prevalence of PTSD (0.8% vs. 0.5%; aPR: 1.5 [CI: 1.2–1.8]), anxiety disorders (9.9% vs. 7.5%; aPR: 1.3 [CI: 1.3–1.4]), and depressive disorders (6.3% vs. 4.9%; aPR: 1.3 [CI: 1.2–1.4]). Among individuals with CHDs, female sex (aPR range: 1.6–3.3) and inpatient admission (aPR range 1.1–1.9) were associated with anxiety/depressive disorders.
Conclusion:
Over 1 in 8 adults with CHDs had diagnosed PTSD and/or other anxiety/depressive disorders, 30–50% higher than adults without CHDs. PTSD was rare, but three times more common in women with CHDs than men. Screening and referral for services for these conditions in people with CHDs may be beneficial.
Keywords: anxiety, congenital heart, depression, MarketScan, post-traumatic stress disorder
1 |. INTRODUCTION
Congenital heart defects (CHDs) affect approximately 1% of births, and range in severity and treatment invasiveness (Stout et al., 2019; Warnes et al., 2008a). Approximately 90% of those born with CHDs are expected to survive into adulthood (Moons, Bovijn, Budts, Belmans, & Gewillig, 2010; Tennant, Pearce, Bythell, & Rankin, 2010), with the population of U.S. adults living with CHDs estimated at over 1.4 million (Gilboa et al., 2016; Gilboa, Salemi, Nembhard, Fixler, & Correa, 2010). Adults with CHDs may require additional surgeries and procedures (Nasr, Faraoni, Valente, & DiNardo, 2017; Warnes et al., 2008a), experience cardiac events at higher rates than the general population (Warnes et al., 2008a), and have higher risk of neurocognitive dysfunction (Cohen & Earing, 2018; Heinz et al., 2018; Ilardi, Ono, McCartney, Book, & Stringer, 2017; Jackson, Misiti, Bridge, Daniels, & Vannatta, 2015). Many children with CHDs experience significant mental distress, including anxiety and depression (Gonzalez et al., 2021), potentially contributing to mental health concerns as adults.
Due to childhood experiences, stressors related to worsening heart health (Gurvitz et al., 2020), need for surgical intervention in adulthood (Berghammer, Karlsson, Ekman, Eriksson, & Dellborg, 2013; Bromberg, Beasley, D’Angelo, Landzberg, & DeMaso, 2003; Deng et al., 2016; Kovacs et al., 2009), and potential limitations in cognitive functioning and employment potential (Cohen & Earing, 2018; Jackson et al., 2015; Kamphuis et al., 2002), adults living with CHDs may have an increased risk of anxiety and/or depressive disorders (Jackson, Leslie, & Hondorp, 2018; Kovacs et al., 2009; Warnes et al., 2008b). Post-traumatic stress disorder (PTSD) is a trauma- or stress-related disorder that can occur after experiencing threatened death or serious injury (American Psychiatric Association, 2013, 2020). Invasive medical treatments experienced in childhood and adulthood might also increase the risk of PTSD in adults with CHDs (Meentken, van Beynum, Legerstee, Helbing, & Utens, 2017).
Increased levels of mood and anxiety disorders among adults with CHDs compared to the general population have been observed (Bromberg et al., 2003; Gleason et al., 2019; Horner, Liberthson, & Jellinek, 2000; Kovacs et al., 2009; Westhoff-Bleck et al., 2016). However, only two clinic-based studies have examined prevalence of PTSD in adults with CHDs (Deng et al., 2016; Eslami, 2017). Most individuals with CHDs fall out of specialized cardiac care in young adulthood, limiting the generalizability of previous findings (Gurvitz et al., 2013). Outside of specialized cardiac care, the burden of mental health conditions, including PTSD, and patterns of mental health treatment in adults with CHDs are not well understood (Agarwal et al., 2019; Khanna et al., 2019). We analyzed 2017 healthcare claims data for privately insured individuals with and without CHDs, to assess the prevalence of diagnosed PTSD, anxiety, and depressive disorders. Our objectives were to determine if the prevalence of these conditions among adults with CHDs is higher than adults without CHDs, examine factors associated with diagnosed anxiety and depressive disorders, and examine patterns of mental health treatment.
2 |. METHODS
We used claims data from the IBM® MarketScan® Commercial Research Database. Healthcare encounter claims from January 1, 2007 through December 31, 2017 were used to identify individuals with a diagnosis of CHDs or chromosomal anomaly. Claims from January 1, 2017 through December 31, 2017 were used to identify cohort members with anxiety, which includes PTSD, and depressive disorders. These data include inpatient and outpatient encounters with diagnosis and procedure codes, outpatient pharmacy claims, and enrollment data from large employers and health plans across the United States who provide healthcare coverage for approximately 40 million individuals and their dependents, on average, each year. Limited demographic characteristics are provided. Because the data are deidentified, the Centers for Disease Control and Prevention deemed this study to be research not involving human subjects and therefore did not need review by an institutional review board.
We included individuals aged 18–49 years at the beginning of 2017 who were enrolled for at least 11 months in an employer sponsored health plan with complete prescription drug and mental health/substance abuse records in 2017. We limited our sample to individuals <50 years of age to minimize misclassification of acquired heart disease coded as CHDs. Individuals were excluded from this sample if they had a diagnosed chromosomal anomaly (International Classification of Diseases, Ninth/Tenth Revision, Clinical Modification [ICD-9-CM]: 758.**; ICD-10-CM: Q90–Q99) at any point between 2007 and 2017, if they had no inpatient or outpatient healthcare encounters during 2017, or if they had a diagnosis of only an atrial septal defect (ICD-9-CM: 745.5; ICD-10-CM: Q21.1) or CHDs of “other” severity at any point between 2007 and 2017, as identified by Glidewell et al. (2018), as these nonspecific codes have been found to have lower positive predictive values than codes for more severe CHDs (Broberg et al., 2015; Khan et al., 2018; Steiner et al., 2018).
We considered an individual to have CHDs if, between January 2007 and December 2017, he or she had at least one inpatient claim with ICD-9-CM or ICD-10-CM CHD codes or at least two outpatient claims with such codes that were more than 30 days apart (Tables S1 and S2) (Downing et al., 2020; Grosse, Boulet, Grant, Hulihan, & Faughnan, 2014; Halasa et al., 2007; Woods, Boulet, Texter, Yates, & Kerlin, 2019). We classified individuals as having severe or nonsevere CHDs. Severe CHDs were those that generally require invasive interventions in the first year of life (Tables S1 and S2, Supporting Information) (Glidewell et al., 2018).
The Centers for Medicare & Medicaid Services Chronic Conditions Data Warehouse (CCW) provides ICD-10-CM algorithms, which include valid ICD-10-CM codes and number/types of claims to qualify as having a depressive, anxiety, or PTSD disorder (Centers for Medicare & Medicaid Services, 2020). These algorithms require one inpatient or two other nondrug claims of any service type at least 1 day apart during a 2-year period (Centers for Medicare & Medicaid Services, 2020) (Table S3). The ICD-10-CM codes for PTSD were also included in the CCW definition of anxiety disorders. Individuals could therefore have ICD-10-CM codes for anxiety disorders, but not PTSD, but all individuals with PTSD diagnosis codes were also included among individuals with anxiety disorder diagnosis codes. Individuals who had only one outpatient claim, or more than one outpatient claim recorded on the same day during 2017 for anxiety or depressive disorders were excluded from the analysis.
Among all individuals with an anxiety or depressive disorder, we examined the percentage who filled one or more outpatient prescriptions for antianxiety or antidepressant medication in 2017 (Table S4). We additionally identified receipt of mental health services in 2017, using procedure codes indicating a diagnostic or therapeutic encounter (Table S5, referred to hereafter as receipt of “psychosocial treatment”).
We estimated the 2017 administrative prevalence of diagnosed PTSD, anxiety, and depressive disorders among individuals with and without CHDs, both overall and by severity of CHDs. We report distributions by age, sex, and region of residence. In addition, we report healthcare utilization in 2017, including outpatient encounters without receipt of psychosocial treatment (Table S5), any inpatient admissions, and inpatient or outpatient encounters with a surgical (typically occurring in an operating room and involving skin incision), catheterization (invasive, nonsurgical), or other noninvasive (e.g., imaging, stress testing) cardiovascular procedure code (Table S6). We used log-binomial regression to examine adjusted prevalence ratios (aPR) of diagnosed PTSD, anxiety disorders, and depressive disorders in 2017 comparing individuals with and without CHDs. Models were adjusted for categorical age (18–29 years, 30–39 years, 40–49 years), sex, and region of residence. To assess factors associated with diagnosed anxiety or depressive disorders among those with CHDs, we used log-binomial regression to estimate aPRs for the presence of a diagnosed anxiety or depressive disorder using patient characteristics and their healthcare utilization as the exposures. Models were adjusted for subsets of confounders based on the factor of interest: categorical age, sex, region, and total outpatient encounters without psychosocial treatment. Region of residence was missing for 0.3% of individuals; these individuals were kept in the analytic sample but were excluded from models that adjusted for region. Among all individuals with a diagnosed anxiety or depressive disorder, we assessed the percentage who filled a prescription for an antianxiety or antidepressant medication, had an outpatient encounter that included psychosocial treatment, or both, stratified by presence of CHDs.
Two supplemental analyses were conducted. First, we limited our analytic sample to individuals who, in 2017, were enrolled in a noncapitated health insurance plan. Capitated health insurance plans are those in which doctors or hospitals are paid a fixed amount per patient and are not always directly tied to the diagnoses and services an individual receives. Because of this, diagnosis and procedures may be coded less accurately in capitated, compared to fee-for-service insurance plans (Landon & Mechanic, 2017). Second, to identify potential differences by age, we conducted analyses stratified by age groups (18–29 years, 30–39 years, and 40–49 years). All analyses were conducted in SAS, Version 9.4 (SAS Institute, Cary NC).
3 |. RESULTS
We found 7,140,720 individuals aged 18 to 49 years who were enrolled for at least 11 months in a health plan with prescription drug and mental health/substance abuse claims inclusion in 2017. A total of 5,421,901 individuals met all remaining inclusion criteria and were included in the analytic sample (Figure 1). Of those, 13,807 (0.3%) individuals had eligible CHDs that met diagnosis criteria between 2007 and 2017, hereafter referred to as having “CHDs.” Among individuals with CHDs, 3,977 (28.8%) had severe CHDs (Table 1). Compared to individuals without CHDs, individuals with CHDs were younger, more likely to be male, more likely to reside in the Northeast region, have increased numbers of outpatient encounters without psychosocial treatment in 2017, were more likely to have an inpatient admission in 2017, and were more likely to have at least one surgical, catheterization, or noninvasive cardiovascular procedure in 2017 (Table 1). Compared to individuals with nonsevere CHDs, individuals with severe CHDs were more likely to be younger, reside in the North Central or South regions, and have at least one surgical, catheterization, or noninvasive cardiovascular procedure in 2017.
FIGURE 1.
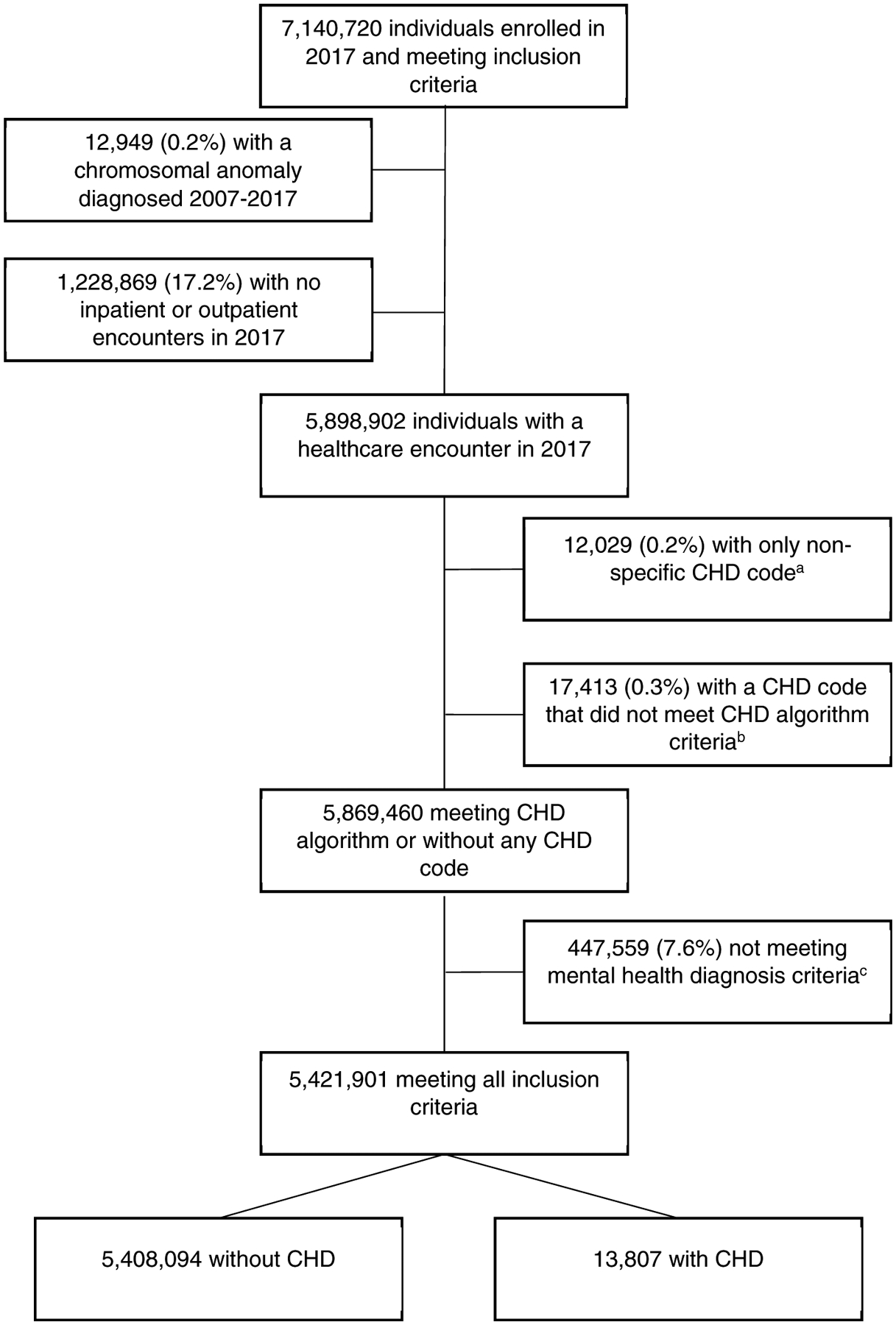
Counts of individuals meeting inclusion and exclusion criteria, IBM MarketScan® Commercial Databases, 2017. aCHD(s): Congenital heart defect(s), defined by ICD-9-CM or ICD-10-CM inpatient and outpatient codes between 2007 and 2017. bIndividuals were considered to have a CHD if they had at least two ICD codes more than 30 days apart in outpatient encounter data, or at least one ICD code in inpatient encounter data. cAt least one inpatient or 2 outpatient ICD-10-CM codes diagnosed on separate days for depressive or anxiety disorders diagnosed in 2017
TABLE 1.
Characteristics of adults with and without CHDs, MarketScan® Commercial Database, 2017
| Any CHDsa | No CHDsa | Chi square p-value | Severe CHDs | Nonsevere CHDs | Chi square p-value | ||
|---|---|---|---|---|---|---|---|
| Characteristics | Category | n (%) | n (%) | n (%) | n (%) | ||
| Total | 13,807 | 5,408,094 | 3,977 | 9,830 | |||
| Ageb | 18–29 | 6,101 (44.2) | 1,834,118 (33.9) | <.0001 | 2,005 (50.4) | 4,096 (41.7) | <.0001 |
| 30–39 | 3,731 (27.0) | 1,623,249 (30.0) | 1,157 (29.1) | 2,574 (26.2) | |||
| 40–49 | 3,975 (28.8) | 1,950,727 (36.1) | 815 (20.5) | 3,160 (32.1) | |||
| Sex | Female | 7,046 (51.0) | 3,014,883 (55.7) | <.0001 | 2,024 (50.9) | 5,022 (51.1) | .8348 |
| Male | 6,761 (49.0) | 2,393,211 (44.3) | 1,953 (49.1) | 4,808 (48.9) | |||
| Region of residence | Northeast | 3,412 (24.8) | 1,026,338 (19.0) | <.0001 | 848 (21.4) | 2,564 (26.2) | <.0001 |
| North Central | 3,176 (23.1) | 1,258,393 (23.3) | 1,007 (25.4) | 2,169 (22.1) | |||
| South | 5,039 (36.6) | 2,239,758 (41.5) | 1,480 (37.3) | 3,559 (36.3) | |||
| West | 2,137 (15.5) | 866,985 (16.1) | 632 (15.9) | 1,505 (15.4) | |||
| Missing | 43 (0) | 16,620 (0) | 10 (0) | 33 (0) | |||
| Outpatient encounters without mental health psychosocial treatmentc | 0 encounters | 26 (0.2) | 20,448 (0.4) | <.0001 | 6 (0.2) | 20 (0.2) | .5176 |
| 1–5 encounters | 5,232 (37.9) | 3,089,281 (57.1) | 1,468 (36.9) | 3,764 (38.3) | |||
| 6–10 encounters | 3,302 (23.9) | 1,136,957 (21.0) | 957 (24.1) | 2,345 (23.9) | |||
| 11–15 encounters | 1,862 (13.5) | 493,536 (9.1) | 532 (13.4) | 1,330 (13.5) | |||
| 16–20 encounters | 1,092 (7.9) | 255,469 (4.7) | 331 (8.3) | 761 (7.7) | |||
| More than 20 encounters | 2,293 (16.6) | 412,403 (7.6) | 683 (17.2) | 1,610 (16.4) | |||
| Inpatient admissionc | Yes | 1,738 (12.6) | 274,812 (5.1) | <.0001 | 539 (13.6) | 1,199 (12.2) | .0297 |
| No | 12,069 (87.4) | 5,133,282 (94.9) | 3,438 (86.4) | 8,631 (87.8) | |||
| Surgical cardiovascular encounterc,d | 0 | 13,538 (98.1) | 5,405,933 (100.0) | <.0001 | 3,888 (97.8) | 9,650 (98.2) | .1174 |
| 1+ | 269 (1.9) | 2,161 (0.04) | 89 (2.2) | 180 (1.8) | |||
| Catheterization cardiovascular encounterc,d | 0 | 13,305 (96.4) | 5,393,201 (99.7) | <.0001 | 3,686 (92.7) | 9,619 (97.9) | <.0001 |
| 1 | 390 (2.8) | 10,198 (0.2) | 222 (5.6) | 168 (1.7) | |||
| 2+ | 112 (0.8) | 4,695 (0.1) | 69 (1.7) | 43 (0.4) | |||
| Noninvasive cardiovascular encounterc,d | 0 | 5,799 (42.0) | 4,699,637 (86.9) | <.0001 | 1,057 (26.6) | 4,742 (48.2) | <.0001 |
| 1 | 4,204 (30.4) | 520,531 (9.6) | 1,350 (33.9) | 2,854 (29.0) | |||
| 2+ | 3,804 (27.6) | 187,926 (3.5) | 1,570 (39.5) | 2,234 (22.7) |
Note: Boldface indicates statistical significance at α < .05.
Abbreviation: CHD, congenital heart defect.
CHDs were defined using International Classification of Disease (ICD) 9 and 10 codes; Individuals were considered to have CHDs if they had at least two ICD codes separated by at least 30 days in outpatient encounter data, or at least one ICD code in inpatient encounter data. Individuals were considered to have severe CHDs if they had ICD codes for common truncus, transposition of the great arteries, complete transposition of the great arteries not otherwise specific, double outlet right ventricle or incomplete transposition of the great arteries, corrected transposition of the great arteries, other transposition of the great arteries, tetralogy of Fallot, single ventricle or cor triloculare, endocardial cushion defect, endocardial cushion defect unspecified, atrial septal defect primum, endocardial cushion defect other specified, pulmonary valve atresia or absence, tricuspid atresia, stenosis or absence, hypoplastic left heart syndrome, interrupted aortic arch, total anomalous pulmonary venous return.
Age as of January 1, 2017.
In 2017.
Any inpatient or outpatient encounter that included cardiovascular procedure code.
Of adults with CHDs, 12.4% had a diagnosed anxiety or depressive disorder in 2017, compared to 9.7% of adults without CHDs (aPR: 1.3, 95% confidence interval [CI]: 1.2–1.4; Table 2). Among adults with CHDs, 0.8% had a PTSD diagnosis, compared to 0.5% of adults without CHDs (aPR: 1.5, CI: 1.2–1.8). Additionally, 9.9% had an anxiety disorder diagnosis (vs. 7.5% of adults without CHDs; aPR: 1.3, CI: 1.3–1.4) and 6.3% had a depressive disorder diagnosis (vs. 4.9% of adults without CHDs; aPR: 1.3, CI: 1.2–1.4). Individuals with severe CHDs had similar prevalence of anxiety and depressive disorders as individuals with nonsevere CHDs (Table 2). Stratified analyses of individuals with severe and nonsevere CHDs (vs. no CHDs) yielded results that were similar to the main analyses that included all individuals with CHDs. Adults with severe CHDs had slightly higher aPRs for these outcomes than adults with nonsevere CHDs, but confidence intervals overlapped.
TABLE 2.
Association of CHDs with diagnosed anxiety, PTSD, and/or depressive disorder, MarketScan® Commercial Database, 2017
| No CHDs | Any CHDsa | Any severe CHDsa | Any nonsevere CHDs | Any CHDs aPRb | Severe CHDs aPRb | Nonsevere CHDsaPRb | |
|---|---|---|---|---|---|---|---|
| Condition | n (%) | n (%) | n (%) | n (%) | (95% CI) | (95% CI) | (95% CI) |
| Total N | 5,408,094 | 13,807 | 3,977 | 9,830 | |||
| Any anxiety or depressive disorderc | 523,022 (9.7) | 1,713 (12.4) | 513 (12.9) | 1,200 (12.2) | 1.3 (1.2–1.4) | 1.3 (1.2–1.5) | 1.3 (1.2–1.3) |
| Anxiety disorder | 403,164 (7.5) | 1,371 (9.9) | 398 (10.0) | 973 (9.9) | 1.3 (1.3–1.4) | 1.3 (1.2–1.5) | 1.3 (1.3–1.4) |
| Post-traumatic stress disorderc | 29,206 (0.5) | 110 (0.8) | 34 (0.9) | 76 (0.8) | 1.5 (1.2–1.8) | 1.6 (1.1–.2.2) | 1.4 (1.2–1.8) |
| Depressive disorder | 267,644 (4.9) | 871 (6.3) | 269 (6.8) | 602 (6.1) | 1.3 (1.2–1.4) | 1.4 (1.2–1.5) | 1.3 (1.2–1.4) |
Note: Boldface indicates statistical significance at α < .05.
Abbreviations: aPR, adjusted prevalence ratio; CHD, congenital heart defect; CI, confidence interval; PTSD, post-traumatic stress disorder.
CHDs were defined using International Classification of Disease (ICD) 9 and 10 codes; Individuals were considered to have CHDs if they had at least two ICD codes separated by at least 30 days in outpatient encounter data, or at least one ICD code in inpatient encounter data. Individuals were considered to have severe CHDs if they had ICD codes for common truncus, transposition of the great arteries, complete transposition of the great arteries not otherwise specific, double outlet right ventricle or incomplete transposition of the great arteries, corrected transposition of the great arteries, other transposition of the great arteries, tetralogy of Fallot, single ventricle or cor triloculare, endocardial cushion defect, endocardial cushion defect unspecified, atrial septal defect primum, endocardial cushion defect other specified, pulmonary valve atresia or absence, tricuspid atresia, stenosis or absence, hypoplastic left heart syndrome, interrupted aortic arch, total anomalous pulmonary venous return.
For all models comparison is adults without a congenital heart defect diagnosis; models are adjusted for categorical age at the beginning of 2017 (18–29 years, 30–39 years, 40–49 years), sex, and region of residence.
Any anxiety or depressive disorder includes any individual with a diagnosis of an anxiety or depressive disorder in 2017; the codes for post-traumatic stress disorder are also included in the codes used to identify individuals with anxiety disorder.
Among adults with CHDs, several factors were associated with increased prevalence of diagnosed PTSD (Table 3). Women were over three times as likely to have diagnosed PTSD compared to men (aPR: 3.3, CI: 2.1–5.1). Increasing outpatient encounters without psychosocial treatment and having a 2017 inpatient admission were associated with increased prevalence of PTSD. These patterns were observed for depressive disorders and anxiety disorders overall. Individuals with a surgical cardiovascular procedure had slightly elevated risk of any mental health disorders, depressive, and anxiety disorders, but associations were not significant.
TABLE 3.
Associations between mental health conditions and characteristics among adults with CHDs, MarketScan® Commercial Database, 2017
| Characteristics | Any anxiety or depressive disorder | Post-traumatic stress disordera | Anxiety disorder | Depressive disorder | ||||
|---|---|---|---|---|---|---|---|---|
| n (%) | aPRb (95% CI) | n (%) | aPRb (95% CI) | n (%) | aPRb (95% CI) | n (%) | aPRb (95% CI) | |
| Congenital heart defect severityc | ||||||||
| Severe CHDs | 513 (12.9) | 1.1 (1.0, 1.2) | 34 (0.9) | 1.1 (0.7, 1.7) | 398 (10.0) | 1.0 (0.9, 1.1) | 269 (6.8) | 1.1 (1.0, 1.3) |
| Nonsevere CHDs | 1,200 (12.2) | Ref | 76 (0.8) | Ref | 973 (9.9) | Ref | 602 (6.1) | Ref |
| Aged | ||||||||
| 18–29 | 756 (12.4) | 1.0 (0.9, 1.1) | 44 (0.7) | 0.9 (0.6, 1.5) | 619 (10.1) | 1.1 (0.9, 1.2) | 384 (6.3) | 1.0 (0.9, 1.2) |
| 30–39 | 454 (12.2) | 0.9 (0.8, 1.0) | 35 (0.9) | 1.1 (0.7, 1.7) | 368 (9.9) | 1.0 (0.8, 1.1) | 233 (6.2) | 0.9 (0.8, 1.1) |
| 40–49 | 503 (12.7) | Ref | 31 (0.8) | Ref | 384 (9.7) | Ref | 254 (6.4) | Ref |
| Sex | ||||||||
| Female | 1,067 (15.1) | 1.6 (1.5, 1.8) | 85 (1.2) | 3.3 (2.1, 5.1) | 868 (12.3) | 1.7 (1.5, 1.9) | 555 (7.9) | 1.7 (1.5, 2.0) |
| Male | 646 (9.6) | Ref | 25 (0.4) | Ref | 503 (7.4) | Ref | 316 (4.7) | Ref |
| Region of residence | ||||||||
| Northeast | 476 (14.0) | 1.2 (1.0, 1.4) | 27 (0.8) | 0.8 (0.5, 1.4) | 376 (11.0) | 1.2 (1.0, 1.4) | 228 (6.7) | 1.0 (0.8, 1.2) |
| North Central | 391 (12.3) | 1.1 (0.9, 1.3) | 32 (1.0) | 1.0 (0.6, 1.8) | 316 (9.9) | 1.1 (0.9, 1.3) | 211 (6.6) | 1.0 (0.8, 1.3) |
| South | 591 (11.7) | 1.0 (0.9, 1.2) | 28 (0.6) | 0.5 (0.3, 0.9) | 471 (9.3) | 1.0 (0.8, 1.2) | 285 (5.7) | 0.8 (0.7, 1.0) |
| West | 252 (11.8) | Ref | 23 (1.1) | Ref | 206 (9.6) | Ref | 145 (6.8) | Ref |
| Outpatient encounters without mental health psychosocial treatmente | ||||||||
| 1–5 encounters | 280 (5.4) | Ref | 12 (0.2) | Ref | 209 (4.0) | Ref | 136 (2.6) | Ref |
| 6–10 encounters | 360 (10.9) | 2.0 (1.7, 2.3) | 17 (0.5) | 2.1 (1.0, 4.4) | 287 (8.7) | 2.2 (1.8, 2.6) | 155 (4.7) | 1.8 (1.4, 2.3) |
| 11–15 encounters | 288 (15.5) | 2.9 (2.4, 3.3) | 16 (0.9) | 3.3 (1.6, 7.1) | 228 (12.2) | 3.0 (2.5, 3.6) | 151 (8.1) | 3.1 (2.5, 3.9) |
| 16–20 encounters | 204 (18.7) | 3.4 (2.9, 4.1) | 11 (1.0) | 3.8 (1.7, 8.7) | 167 (15.3) | 3.8 (3.1, 4.6) | 109 (10.0) | 3.8 (2.9, 4.8) |
| More than 20 encounters | 571 (24.9) | 4.6 (4.0, 5.3) | 53 (2.3) | 8.8 (4.7, 16.6) | 472 (20.6) | 5.2 (4.4, 6.0) | 316 (13.8) | 5.3 (4.3, 6.4) |
| Inpatient admissionf | ||||||||
| Yes | 381 (21.9) | 1.1 (1.0, 1.3) | 41 (2.4) | 1.9 (1.2, 2.9) | 310 (17.8) | 1.1 (1.0, 1.3) | 223 (12.8) | 1.3 (1.1, 1.5) |
| No | 1,332 (11.0) | Ref | 69 (0.6) | Ref | 1,061 (8.8) | Ref | 648 (5.4) | Ref |
| Surgical cardiovascular encounterf,g | ||||||||
| 0 encounters | 1,649 (12.2) | Ref | 107 (0.8) | Ref | 1,318 (9.7) | Ref | 838 (6.2) | Ref |
| ≥1 encounter | 64 (23.8) | 1.2 (1.0, 1.5) | 3 (1.1) | 0.8 (0.2, 2.5) | 53 (19.7) | 1.3 (1.0, 1.6) | 33 (12.3) | 1.2 (0.9, 1.7) |
| Catheterization cardiovascular encounterf,g | ||||||||
| 0 encounters | 1,625 (12.2) | Ref | 105 (0.8) | Ref | 1,299 (9.8) | Ref | 824 (6.2) | Ref |
| 1 encounter | 62 (15.9) | 0.9 (0.7, 1.2) | 3 (0.8) | 0.6 (0.2, 1.9) | 50 (12.8) | 0.9 (0.7, 1.2) | 33 (8.5) | 0.9 (0.6, 1.3) |
| ≥2 encounters | 26 (23.2) | 1.1 (0.8, 1.5) | 2 (1.8) | 1.1 (0.3, 4.4) | 22 (19.6) | 1.1 (0.8, 1.7) | 14 (12.5) | 1.1 (0.7, 1.8) |
| Noninvasive cardiovascular encounterf,g | ||||||||
| 0 encounters | 622 (10.7) | Ref | 42 (0.7) | Ref | 496 (8.6) | Ref | 318 (5.5) | Ref |
| 1 encounter | 458 (10.9) | 0.9 (0.8, 1.0) | 24 (0.6) | 0.7 (0.4, 1.2) | 348 (8.3) | 0.9 (0.8, 1.0) | 232 (5.5) | 0.9 (0.8, 1.1) |
| ≥2 encounters | 633 (16.6) | 1.0 (0.9, 1.1) | 44 (1.2) | 0.9 (0.6, 1.4) | 527 (13.9) | 1.0 (0.9, 1.2) | 321 (8.4) | 0.9 (0.8, 1.1) |
Note: Boldface indicates statistical significance at α < .05.
Abbreviations: aPR, adjusted prevalence ratio; CHD, congenital heart defects; CI, confidence interval.
Post-traumatic stress disorder is a subset of anxiety disorders.
Adjusted prevalence ratios: Type of congenital heart defect and outpatient encounters without mental health counseling adjusted for categorical age (18–29 years, 30–39 years, 40–49 years), sex, and region; Age adjusted for sex and region; Sex adjusted for categorical age and region, Region adjusted for categorical age and sex; Inpatient admissions and Encounter with cardiovascular procedures adjusted for categorical age, sex, region, and total outpatient encounters without psychosocial treatment.
Individuals were considered to have severe CHDs if they had ICD codes for common truncus, transposition of the great arteries, complete transposition of the great arteries not otherwise specific, double outlet right ventricle or incomplete transposition of the great arteries, corrected transposition of the great arteries, other transposition of the great arteries, tetralogy of Fallot, single ventricle or cor triloculare, endocardial cushion defect, endocardial cushion defect unspecified, atrial septal defect primum, endocardial cushion defect other specified, pulmonary valve atresia or absence, tricuspid atresia stenosis or absence, hypoplastic left heart syndrome, interrupted aortic arch, total anomalous pulmonary venous return.
Age as of January 1, 2017.
Among individuals with at least one outpatient encounter without psychosocial treatment.
In 2017.
Any inpatient or outpatient encounter that included a cardiovascular procedure code.
Over 90% of adults with diagnosed anxiety or depressive disorders received psychosocial treatment and/or antianxiety and/or antidepressant medication dispensed in 2017, regardless of their CHDs status (Table 4). Over 97% of adults with CHDs and PTSD received some sort of treatment in 2017, higher than adults with anxiety or depression diagnoses (Table 4). Further, adults with PTSD and CHDs had slightly higher prevalence of both psychosocial treatment and antianxiety/antidepressant medication than adults without CHDs (not significant). Among adults with anxiety diagnoses, adults with CHDs were slightly more likely to have both psychosocial treatment and antianxiety/antidepressant medication than adults without CHDs, and slightly less likely to have only psychosocial treatment or antianxiety/antidepressant medication use.
TABLE 4.
Treatment characteristics of adults with a mental health diagnosis, MarketScan® Commercial Database, 2017
| Post-traumatic stress disordera | Anxiety | Depression | |||||||
|---|---|---|---|---|---|---|---|---|---|
| CHDsb | No CHDs | CHDsb | No CHDs | CHDsb | No CHDs | ||||
| Category | n (%) | n (%) | p-valuec | n (%) | n (%) | p-valuec | n (%) | n (%) | p-valuec |
| Total | 110 | 29,206 | 1,368 | 403,164 | 871 | 267,644 | |||
| Both psychosocial treatment and antianxiety/antidepressant medication | 76 (69.1) | 18,643 (63.8) | .2176 | 573 (41.8) | 152,437 (37.8) | .0224 | 458 (52.6) | 128,909 (48.2) | .0290 |
| Antianxiety/antidepressant only | 15 (13.6) | 3,191 (10.9) | 528 (38.5) | 166,682 (41.3) | 279 (32.0) | 90,188 (33.7) | |||
| Psychosocial treatment only | 16 (14.6) | 6,630 (22.7) | 176 (12.8) | 56,212 (13.9) | 98 (11.3) | 37,557 (14.0) | |||
| Neither psychosocial treatment or antianxiety/antidepressant medication | 3 (2.7) | 742 (2.5) | 94 (6.9) | 27,833 (6.9) | 36 (4.1) | 10,990 (4.1) | |||
Note: Boldface indicates statistical significance at α < .05.
Abbreviation: CHD, congenital heart defect.
Post-traumatic stress disorder is a subset of anxiety disorders.
CHDs were defined using International Classification of Disease (ICD) 9 and 10 codes; Individuals were considered to have CHDs if they had at least two ICD codes separated by at least 30 days in outpatient encounter data, or at least one ICD code in inpatient encounter data.
Chi-square p-value.
When we excluded 566,768 individuals with capitated health insurance plans from the analysis, results were similar to those from the main analysis (Tables S7–S9). When examining any anxiety or depressive disorders stratified by age, aPRs in all age strata had similar estimated associations between CHDs and anxiety or depressive disorders (aPR point estimates ranged from 1.2 to 1.4; individuals aged 30–39 years with severe CHDs had slightly higher prevalence of depressive disorders [aPR: 1.5; CI: 1.2, 1.8]) (Supplemental Table 12). However, when examining PTSD, individuals aged 18–29 years had lower estimated aPRs (range 1.0 to 1.5) compared to individuals aged 30–39 (range 1.5 to 2.3) and aged 40–49 (range 1.4–2.1) (Table S12). When examining factors associated with anxiety and depressive disorders among individuals with CHDs, similar patterns were present for most factors in all age groups (Tables S13–S15). There were some exceptions: having an inpatient admission in 2017 was associated with a lower prevalence of anxiety disorders (aPR: 0.7; CI: 0.5, 0.9) and depressive disorders (aPR: 0.7, CI: 0.5, 0.9) among individuals aged 30–39 years compared to individuals aged 18–29 and 40–49 years (aPR ranges 1.3–1.8) (Tables S13 and S14). Surgical, catheterization, and noninvasive procedures had higher aPRs in age stratified analyses compared to the main analysis, but to achieve model convergence, could not be adjusted for the same confounders as in the main analysis.
4 |. DISCUSSION
Our study of privately insured adults indicated that 12% of adults with CHDs had diagnosed anxiety disorders, including PTSD, or depressive disorders and they were more likely to have these disorders compared to adults without CHDs. This increased prevalence persisted when examining PTSD with or without codes for depressive and other anxiety disorders (CHDs: 0.8%; no CHDs 0.5%), anxiety disorders with or without codes for depressive disorders (CHDs: 9.9%; no CHDs 7.5%) and depressive disorders with or without codes for anxiety disorders (CHDs: 6.3%; no CHDs: 4.9%). Among individuals with a diagnosed anxiety or depressive disorder, almost all received treatment. Among adults with CHDs, increasing numbers of outpatient healthcare encounters and hospitalization in 2017 were associated with increased prevalence of PTSD, anxiety disorders and depressive disorders. Additionally, women with CHDs were more likely than men to have anxiety and depressive disorders, most strikingly for PTSD, with over three times the prevalence of a PTSD diagnosis. This finding aligns with others that indicate women have higher rates of most mental illness and PTSD compared to men, possibly due to increased lifetime experience of associated risk factors (Olff, 2017; Riecher-Rossler, 2017).
Few studies have investigated the frequency of PTSD in adults with CHDs. Invasive medical CHDs treatment and hospitalization in childhood and adolescence may be stressful and contribute to persistent stress reactions throughout childhood and into adulthood (Meentken et al., 2017). Additionally, the cumulative burden of treatment and cardiac health could contribute to the development of PTSD in adults (Alonzo, 2000). In a study of 134 adults with CHDs treated at an adult CHDs clinic in the United States, Deng et al. (2016) found that 11% met criteria for elevated PTSD symptoms related to their CHDs or its treatment and that 21% met criteria for elevated PTSD symptoms overall. In a hospital-based study of 347 adults with CHDs from Iran, Eslami reported that 52% met criteria for likely PTSD (vs. 48% of adults without CHDs) (Eslami, 2017). Our analysis of over 13,000 privately insured individuals found increased prevalence among adults with CHDs. We observed a much lower prevalence of diagnosed PTSD, indicating differences in prevalence of PTSD among adults receiving congenital cardiac care compared to adults with CHDs in the general population, or an underdiagnosis of the condition in administrative data.
Our findings can be considered alongside at least two other U.S.-based studies, neither of which examined PTSD individually. In a cohort of adults with CHDs ascertained from medical records and claims data between 2011 and 2013, Khanna et al. (2019) identified mental health encounters over a three-year period. Over 33% of adults with CHDs had a mental health encounter. Among adults with CHDs, having at least two cardiac procedures between 2011 and 2013 was associated with increased prevalence of anxiety (odds ratio [OR]: 3.4, CI: 2.9–4.0) and mood disorders (OR: 3.6, CI: 3.1–4.2). Unlike our study, Khanna et al. did not have a comparison group of adults without CHDs. Agarwal et al. used MarketScan data from 2010–2016 to identify adults aged 18–64 with one or more CHDs-related ICD codes and matched them to adults without CHDs. Psychiatric disorders were 1.5 times higher (95% CI: 1.35–1.65) among adults with CHDs (Agarwal et al., 2019). However, they did not examine PTSD or anxiety, examined depression and psychosis as a single outcome, and did not examine mental health treatment. Our study adds to the literature by assessing prevalence and risk factors for PTSD, anxiety and depressive disorders in the adult CHDs population as compared with a group of adults without CHDs, using a more specific CHDs case definition, and examining mental health treatment.
This analysis benefitted from a large, nationwide sample of over 13,000 individuals with CHDs. This allowed us to examine the rarely investigated (in this population) outcome of diagnosed PTSD, and allowed comparisons between individuals with and without CHDs, and by severity. However, MarketScan data are a convenience sample of privately insured individuals and their dependents, and we limited our sample to those with employer sponsored health plans, mental health coverage, prescription coverage, and at least 11 months of enrollment, so our results may not be generalizable to U.S. populations lacking commercial health insurance. Moreover, persons with CHDs likely have higher healthcare utilization than those without CHDs, giving more opportunities for mental health disorders to be detected, diagnosed, and treated. The increased prevalence of anxiety and depressive disorders could be partially explained by detection bias. An important limitation is that use of administrative data can lead to misclassification of both the exposure, and the outcome (Khan et al., 2018). Further, there could be additional life events and stressors not documented in administrative data that contribute to the development of PTSD, depression, or anxiety disorders in people with CHDs.
While our estimate of the prevalence of depressive disorders among adults without CHDs is similar to the past-year prevalence of a major depressive episode reported by the National Institute of Mental Health (NIMH), our estimate of the prevalence of anxiety disorders is lower than that reported by the NIMH (National Institute of Mental Health, 2017, 2019). This could suggest anxiety disorders may not be captured as well as depressive disorders in administrative data. Additionally, individuals seeking mental health care could be paying out of pocket, which would not be captured in these data. The use of ICD codes to identify adults with CHDs can incorrectly classify adults without CHDs as having CHDs. In particular, singular outpatient codes may have a positive predictive value as low as 50% (Khan et al., 2018). For this reason, we required at least two outpatient codes to identify CHDs, and excluded individuals with nonspecific codes. Our algorithm identified 0.3% of the privately insured analytic sample with inpatient or outpatient care to have CHDs, similar to other publications using administrative data (Glidewell et al., 2021), but less than the estimated 0.6% of U.S. adults estimated to be living with CHDs (Gilboa et al., 2016). This could indicate that our algorithm missed individuals with CHDs, or that individuals with CHDs did not have their CHD documented at their healthcare encounters or were not using healthcare, or had insurance other than what was included here.
We applied algorithms to increase the specificity of classification mental health disorders (Centers for Medicare & Medicaid Services, 2020). However, we could have excluded individuals with depressive/anxiety disorders who did not meet the respective criteria. Although we excluded individuals with diagnostic codes for chromosomal anomalies, adults with CHDs and undiagnosed genetic conditions may have been included (Burchill, Greenway, Silversides, & Mital, 2011). We may have also inadvertently excluded individuals who received genetic testing during pregnancy or as part of a diagnostic workup. A final limitation is that variables unavailable in the MarketScan data (e.g., race/ethnicity, education, and socioeconomic status) may be important confounders or effect modifiers. Specifically, racial and ethnic minorities experience similar levels of mental illness as white adults, but have less access to and report lower utilization of mental health care (National Institute of Mental Health, n.d.; Substance Abuse and Mental Health Services Administration, 2015).
Current estimates suggest that over 1.4 million adults live with CHDs in the United States, and that population is expected to grow (Gilboa et al., 2016). Findings from this study are consistent with others that have observed a higher prevalence of mental illness in individuals with CHDs, and add to the existing literature by examining PTSD and mental health treatment. Future research should consider incorporating the impact of race and other social determinants of health on mental health outcomes in adults with CHDs. Understanding best practices for screening, diagnosis, and treatment of anxiety and depressive disorders in adults with CHDs, including ways to mitigate risk, especially before and after hospitalization, may help improve the mental health of this growing population.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to acknowledge Brittany Wright for her assistance with preparing the manuscript for submission. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. IBM MarketScan are trademarks of IBM Corporation in the United States, other countries, or both. The authors have no relevant financial or nonfinancial interests to disclose.
Footnotes
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of the article at the publisher’s website.
DATA AVAILABILITY STATEMENT
The authors cannot make data and study materials available to other investigators for purposes of reproducing the results because of licensing restrictions. Interested parties, however, could obtain and license the data by contacting IBM MarketScan Research Databases. SAS code is available upon request.
REFERENCES
- Agarwal A, Thombley R, Broberg CS, Harris IS, Foster E, Mahadevan VS, … Dudley RA (2019). Age- and lesion-related comorbidity burden among US adults with congenital heart disease: A population-based study. Journal of the American Heart Association, 8(20), e013450. 10.1161/JAHA.119.013450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alonzo AA (2000). The experience of chronic illness and post-traumatic stress disorder: The consequences of cumulative adversity. Social Science & Medicine, 50(10), 1475–1484. 10.1016/s0277-9536(99)00399-8 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association. (2020). What Is posttraumatic stress disorder? Retrieved from https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd
- Berghammer M, Karlsson J, Ekman I, Eriksson P, & Dellborg M (2013). Self-reported health status (EQ-5D) in adults with congenital heart disease. International Journal of Cardiology, 165(3), 537–543. 10.1016/j.ijcard.2011.10.002 [DOI] [PubMed] [Google Scholar]
- Broberg C, McLarry J, Mitchell J, Winter C, Doberne J, Woods P, … Weiss J (2015). Accuracy of administrative data for detection and categorization of adult congenital heart disease patients from an electronic medical record. Pediatric Cardiology, 36(4), 719–725. 10.1007/s00246-014-1068-2 [DOI] [PubMed] [Google Scholar]
- Bromberg JI, Beasley PJ, D’Angelo EJ, Landzberg M, & DeMaso DR (2003). Depression and anxiety in adults with congenital heart disease: A pilot study. Heart & Lung, 32(2), 105–110. 10.1067/mhl.2003.26 [DOI] [PubMed] [Google Scholar]
- Burchill L, Greenway S, Silversides CK, & Mital S (2011). Genetic counseling in the adult with congenital heart disease: What is the role? Current Cardiology Reports, 13(4), 347–355. 10.1007/s11886-011-0188-z [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. (2020). Chronic conditions data warehouse. Retrieved from https://www2.ccwdata.org/web/guest/condition-categories
- Cohen S, & Earing MG (2018). Neurocognitive impairment and its long-term impact on adults with congenital heart disease. Progress in Cardiovascular Diseases, 61(3–4), 287–293. 10.1016/j.pcad.2018.08.002 [DOI] [PubMed] [Google Scholar]
- Deng LX, Khan AM, Drajpuch D, Fuller S, Ludmir J, Mascio CE, … Kim YY (2016). Prevalence and correlates of post-traumatic stress disorder in adults with congenital heart disease. The American Journal of Cardiology, 117(5), 853–857. 10.1016/j.amjcard.2015.11.065 [DOI] [PubMed] [Google Scholar]
- Downing KF, Tepper NK, Simeone RM, Ailes EC, Gurvitz M, Boulet SL, … Farr SL (2020). Adverse pregnancy conditions among privately insured women with and without congenital heart defects. Circulation. Cardiovascular Quality and Outcomes, 13(6), e006311. 10.1161/CIRCOUTCOMES.119.006311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eslami B (2017). Correlates of posttraumatic stress disorder in adults with congenital heart disease. Congenital Heart Disease, 12(3), 357–363. 10.1111/chd.12452 [DOI] [PubMed] [Google Scholar]
- Gilboa SM, Devine OJ, Kucik JE, Oster ME, Riehle-Colarusso T, Nembhard WN, … Marelli AJ (2016). Congenital heart defects in the United States: Estimating the magnitude of the affected population in 2010. Circulation, 134(2), 101–109. 10.1161/CIRCULATIONAHA.115.019307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilboa SM, Salemi JL, Nembhard WN, Fixler DE, & Correa A (2010). Mortality resulting from congenital heart disease among children and adults in the United States, 1999 to 2006. Circulation, 122(22), 2254–2263. 10.1161/CIRCULATIONAHA.110.947002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleason LP, Deng LX, Khan AM, Drajpuch D, Fuller S, Ludmir J, … Kovacs AH (2019). Psychological distress in adults with congenital heart disease: Focus beyond depression. Cardiology in the Young, 29, 185–189. [DOI] [PubMed] [Google Scholar]
- Glidewell J, Book W, Raskind-Hood C, Hogue C, Dunn JE, Gurvitz M, … Riehle-Colarusso T (2018). Population-based surveillance of congenital heart defects among adolescents and adults: Surveillance methodology. Birth Defects Res, 110(19), 1395–1403. 10.1002/bdr2.1400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glidewell J, Farr SL, Book W, Botto LD, Li JS, Soim AS, … Crume TL (2021). Individuals aged 1–64 years with documented congenital heart defects at healthcare encounters, five U.S. surveillance sites, 2011–2013. American Heart Journal, 238, 100–108. 10.1016/j.ahj.2021.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez VJ, Kimbro RT, Cutitta KE, Shabosky JC, Bilal MF, Penny DJ, & Lopez KN (2021). Mental health disorders in children with congenital heart disease. Pediatrics, 147(2), e20201693. 10.1542/peds.2020-1693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosse SD, Boulet SL, Grant AM, Hulihan MM, & Faughnan ME (2014). The use of US health insurance data for surveillance of rare disorders: Hereditary hemorrhagic telangiectasia. Genetics in Medicine, 16(1), 33–39. 10.1038/gim.2013.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurvitz M, Dunn JE, Bhatt A, Book WM, Glidewell J, Hogue C, … Riehle-Colarusso T (2020). Characteristics of adults with congenital heart defects in the United States. Journal of the American College of Cardiology, 76(2), 175–182. 10.1016/j.jacc.2020.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurvitz M, Valente AM, Broberg C, Cook S, Stout K, Kay J, … Adult Congenital Heart Association. (2013). Prevalence and predictors of gaps in care among adult congenital heart disease patients: HEART-ACHD (The Health, Education, and Access Research Trial). Journal of the American College of Cardiology, 61(21), 2180–2184. 10.1016/j.jacc.2013.02.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halasa NB, Shankar SM, Talbot TR, Arbogast PG, Mitchel EF, Wang WC, … Griffin MR (2007). Incidence of invasive pneumococcal disease among individuals with sickle cell disease before and after the introduction of the pneumococcal conjugate vaccine. Clinical Infectious Diseases, 44(11), 1428–1433. 10.1086/516781 [DOI] [PubMed] [Google Scholar]
- Heinz AJ, Meffert BN, Halvorson MA, Blonigen D, Timko C, & Cronkite R (2018). Employment characteristics, work environment, and the course of depression over 23 years: Does employment help foster resilience? Depression and Anxiety, 35(9), 861–867. 10.1002/da.22782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horner T, Liberthson R, & Jellinek MS (2000). Psychosocial profile of adults with complex congenital heart disease. Mayo Clinic Proceedings, 75(1), 31–36. 10.4065/75.1.31 [DOI] [PubMed] [Google Scholar]
- Ilardi D, Ono KE, McCartney R, Book W, & Stringer AY (2017). Neurocognitive functioning in adults with congenital heart disease. Congenital Heart Disease, 12(2), 166–173. 10.1111/chd.12434 [DOI] [PubMed] [Google Scholar]
- Jackson JL, Leslie CE, & Hondorp SN (2018). Depressive and anxiety symptoms in adult congenital heart disease: Prevalence, health impact and treatment. Progress in Cardiovascular Diseases, 61(3–4), 294–299. 10.1016/j.pcad.2018.07.015 [DOI] [PubMed] [Google Scholar]
- Jackson JL, Misiti B, Bridge JA, Daniels CJ, & Vannatta K (2015). Emotional functioning of adolescents and adults with congenital heart disease: A meta-analysis. Congenital Heart Disease, 10(1), 2–12. 10.1111/chd.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamphuis M, Vogels T, Ottenkamp J, Van Der Wall EE, Verloove-Vanhorick SP, & Vliegen HW (2002). Employment in adults with congenital heart disease. Archives of Pediatrics & Adolescent Medicine, 156(11), 1143–1148. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/12413345 [DOI] [PubMed] [Google Scholar]
- Khan A, Ramsey K, Ballard C, Armstrong E, Burchill LJ, Menashe V, … Broberg CS (2018). Limited accuracy of administrative data for the identification and classification of adult congenital heart disease. Journal of the American Heart Association, 7(2), e007378. 10.1161/JAHA.117.007378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna A, Duca L, Kay J, Shore J, Kelly S, & Crume R (2019). Prevalence of mental illness in adolescents and adults with congenital heart disease from the Colorado Congenital Heart Defect Surveillance System. The American Journal of Cardiology, 124, 618–626. 10.1016/j.amjcard.2019.05.023 [DOI] [PubMed] [Google Scholar]
- Kovacs AH, Saidi AS, Kuhl EA, Sears SF, Silversides C, Harrison JL, … Nolan RP (2009). Depression and anxiety in adult congenital heart disease: Predictors and prevalence. International Journal of Cardiology, 137(2), 158–164. 10.1016/j.ijcard.2008.06.042 [DOI] [PubMed] [Google Scholar]
- Landon BE, & Mechanic RE (2017). The paradox of coding—Policy concerns raised by risk-based provider contracts. The New England Journal of Medicine, 377(13), 1211–1213. 10.1056/NEJMp1708084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meentken MG, van Beynum IM, Legerstee JS, Helbing WA, & Utens EM (2017). Medically related post-traumatic stress in children and adolescents with congenital heart defects. Frontiers in Pediatrics, 5, 20. 10.3389/fped.2017.00020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moons P, Bovijn L, Budts W, Belmans A, & Gewillig M (2010). Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation, 122(22), 2264–2272. 10.1161/CIRCULATIONAHA.110.946343 [DOI] [PubMed] [Google Scholar]
- Nasr VG, Faraoni D, Valente AM, & DiNardo JA (2017). Outcomes and costs of cardiac surgery in adults with congenital heart disease. Pediatric Cardiology, 38(7), 1359–1364. 10.1007/s00246-017-1669-7 [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. (n.d.) Mental illness. Retrieved from https://www.nimh.nih.gov/health/statistics/mental-illness
- National Institute of Mental Health. (2017, November 2017). Any anxiety disorder. Retrieved from https://www.nimh.nih.gov/health/statistics/any-anxiety-disorder.shtml
- National Institute of Mental Health. (2019, February 2019). Major depression. Retrieved from https://www.nimh.nih.gov/health/statistics/major-depression.shtml
- Olff M (2017). Sex and gender differences in post-traumatic stress disorder: An update. European Journal of Psychotraumatology, 8, 1351204. 10.1080/20008198.2017.1351204 [DOI] [Google Scholar]
- Riecher-Rossler A (2017). Sex and gender differences in mental disorders. Lancet Psychiatry, 4(1), 8–9. 10.1016/S2215-0366(16)30348-0 [DOI] [PubMed] [Google Scholar]
- Steiner JM, Kirkpatrick JN, Heckbert SR, Habib A, Sibley J, Lober W, & Randall Curtis J (2018). Identification of adults with congenital heart disease of moderate or great complexity from administrative data. Congenital Heart Disease, 13(1), 65–71. 10.1111/chd.12524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, … Van Hare GF (2019). 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 139(14), e698–e800. 10.1161/CIR.0000000000000603 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2015). Racial/ethnic differences in mental health service use among adults. Retrieved from https://www.samhsa.gov/data/sites/default/files/MHServicesUseAmongAdults/MHServicesUseAmongAdults.pdf
- Tennant PW, Pearce MS, Bythell M, & Rankin J (2010). 20-year survival of children born with congenital anomalies: A population-based study. Lancet, 375(9715), 649–656. 10.1016/S0140-6736(09)61922-X [DOI] [PubMed] [Google Scholar]
- Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, … Webb GD (2008a). ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Journal of the American College of Cardiology, 52(23), e143–e263. 10.1016/j.jacc.2008.10.001 [DOI] [PubMed] [Google Scholar]
- Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, … Webb GD (2008b). ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines for the management of adults with congenital heart disease). Circulation, 118(23), 2395–2451. 10.1161/CIRCULATIONAHA.108.190811 [DOI] [PubMed] [Google Scholar]
- Westhoff-Bleck M, Briest J, Fraccarollo D, Hilfiker-Kleiner D, Winter L, Maske U, … Kahl KG (2016). Mental disorders in adults with congenital heart disease: Unmet needs and impact on quality of life. Journal of Affective Disorders, 204, 180–186. 10.1016/j.jad.2016.06.047 [DOI] [PubMed] [Google Scholar]
- Woods GM, Boulet SL, Texter K, Yates AR, & Kerlin BA (2019). Venous thromboembolism in chronic pediatric heart disease is associated with substantial health care burden and expenditures. Research and Practice in Thrombosis and Haemostasis, 3(3), 372–382. 10.1002/rth2.12205 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors cannot make data and study materials available to other investigators for purposes of reproducing the results because of licensing restrictions. Interested parties, however, could obtain and license the data by contacting IBM MarketScan Research Databases. SAS code is available upon request.


