Abstract
OBJECTIVES
Safety-net hospitals disproportionately care for people with substance use disorders (SUDs), yet little is known about trends in hospital admissions related to specific substances. This study uses electronic health record (EHR) data to describe trends in substance-specific admissions at a Midwest urban safety-net hospital.
METHODS
We included all admissions from 2008 through 2020 and defined them as non-SUD (N=154,477) or SUD-related (N=63,667). We described patient characteristics and trends in substance-specific admissions. We estimated the association of SUD diagnoses with discharge against medical advice (AMA) and length of stay (LOS) using logistic regression and generalized linear models.
RESULTS
Between 2008 and 2020, SUD-related admissions increased from 23.1% to 32.9% of total admissions. Admissions related to SUD had significantly more comorbidities than non-SUD-related admissions (4.7 vs 3.5, P<0.001). Among illicit substances, cocaine-related admissions were the most common in 2008 (3.9% of total admissions, 17.2% of SUD admissions) while psychostimulants (e.g., methamphetamines) were the most common in 2020 (7.8% of total admissions, 23.8% of SUD admissions). SUD-related hospitalizations had higher rates of AMA discharge (3.8%; 95% CI 3.6–3.9 vs 1.4%; 95% CI 1.3–1.4) and longer LOS (6.3 days; 95% CI: 6.2–6.3 vs 5.3 days; 95% CI: 5.3–5.4) than non-SUD-related admissions.
CONCLUSIONS
Over the study period, the proportion of admissions related to substance use rose to approximately one-third of all admissions, driven by a rapidly increasing share of psychostimulant-related admissions. Identifying substance use patterns quickly using EHR data can help safety-net hospitals meet the needs of their patients and improve outcomes.
Keywords: Substance use disorder, hospital admissions, length of stay
INTRODUCTION
Opioid use and related mortality have been the predominant focus of substance use disorder (SUD) policy and interventions over the last decade, but recent data indicate that overdose deaths related to other substances are rising.1,2 Overdose deaths increased from 38,329 in 2010 to an all-time high of 70,630 in 2019.3 Deaths related to cocaine and psychostimulants have been on the rise since 2009 and in 2019, the rate of psychostimulant deaths was higher than deaths due to prescription opioids.1,3 These data indicate rapidly shifting trends in substance use patterns, which may have important implications for hospital utilization and resources.
Safety-net hospitals disproportionately care for people with SUD, yet little is known about trends in hospital admissions and resource utilization related to SUD.4 Some studies have examined trends in isolated substances across a variety of hospital types, but granular data across substances within safety-net settings have not been reported.5 To guide resource allocation and inform policy during dynamic and unfolding crises, safety-net hospitals need timely data reflective of their patient population’s substance use patterns and healthcare utilization. Electronic health record (EHR) data are a rich source of analysis for substance use trends because they can update in real time and capture information for individuals who may be uninsured, a common problem among individuals with SUD.
In this study, we examined 12 years of EHR data at a Midwest urban safety-net hospital to describe trends in substance-specific admissions. We compared patient demographics, length of stay (LOS), and discharge against medical advice (AMA) between SUD and non-SUD-related hospitalizations.
METHODS
We included all admissions at Hennepin County Medical Center (HCMC), a large Midwestern tertiary care center and safety-net hospital, from January 1, 2008 to December 31, 2020. Admissions were defined as SUD-related using 9th and 10th revisions of International Classification of Diseases (ICD) codes identified in previous work.5,6 Specific substance categories included opioids, cannabis, alcohol, cocaine, psychostimulants, and sedatives. These categories were not mutually exclusive and concomitant substance use was examined. We described characteristics of the sample including age, sex, race/ethnicity, and year of admission. Medical complexity was estimated using an adjusted Elixhauser Comorbidity Index (ECI) that excluded SUD diagnoses, because SUD was our primary independent variable.7 Differences between groups regarding age, sex, and medical complexity were compared using Pearson χ2 tests.
We used a logistic regression model and a generalized linear model with gamma distribution and log-link function to examine the association of SUD diagnosis with discharges AMA and LOS, respectively. We controlled for race/ethnicity, age, gender, medical complexity, and year of admission. We also controlled for AMA discharge when examining LOS.
We considered P<.05 to be statistically significant. We used a de-identified dataset therefore our study was determined to not be human subjects research by the Hennepin Healthcare Research Institute Institutional Review Board.
RESULTS
Our sample consisted of 218,144 unique admissions among 101,197 patients, ages 18 and older. Between 2008 and 2020 there were 63,667 admissions related to SUD, among 25,392 patients. The incidence of SUD-related admissions increased from 23.1% in 2008 to 32.9% of total admissions in 2020. Overall annual admissions for any reason declined from 18,808 in 2008 to 16,273 in 2019. The COVID-19 pandemic resulted in fewer total admissions (14,917) in 2020, consistent with national findings.8 SUD admissions increased from 4,343 in 2008 to 5,416 in 2019 and declined proportionally to total admissions in 2020 (4,905). During our 12-year study period, SUD-related admissions accounted for 29.2% of total admissions and increased from 23.1% in 2008 to 32.9% of total admissions in 2020.
Admissions with SUD tended to be younger (mean age 44.7 vs 50.8, P<.001), male (68.5% vs 44.9%, P<.001, and white (47.6% vs 46.1%, P<.001). Median ECI was higher in SUD-related admissions compared to those without an accompanying SUD diagnosis (4.7 vs 3.5, P<0.001).
Alcohol use disorder was the most common SUD in each study year (20.3% of total admissions and 61.7% of SUD-related admissions in 2020 [Figure 1]). Among illicit substances, cocaine-related admissions were the most common in 2008 (3.9% of total admissions, 17.2% of SUD admissions) while psychostimulants (e.g., methamphetamine) were the most common in 2020 (7.8% of total admissions, 23.8% of SUD admissions [Figure 2]). Opioid use was the second most common illicit SUD diagnosis in 2020 (19.6% of SUD admissions). Concurrent psychostimulant use increased from 0.3% to 43.5% among opioid-related admissions between 2008 and 2020.
Figure 1:
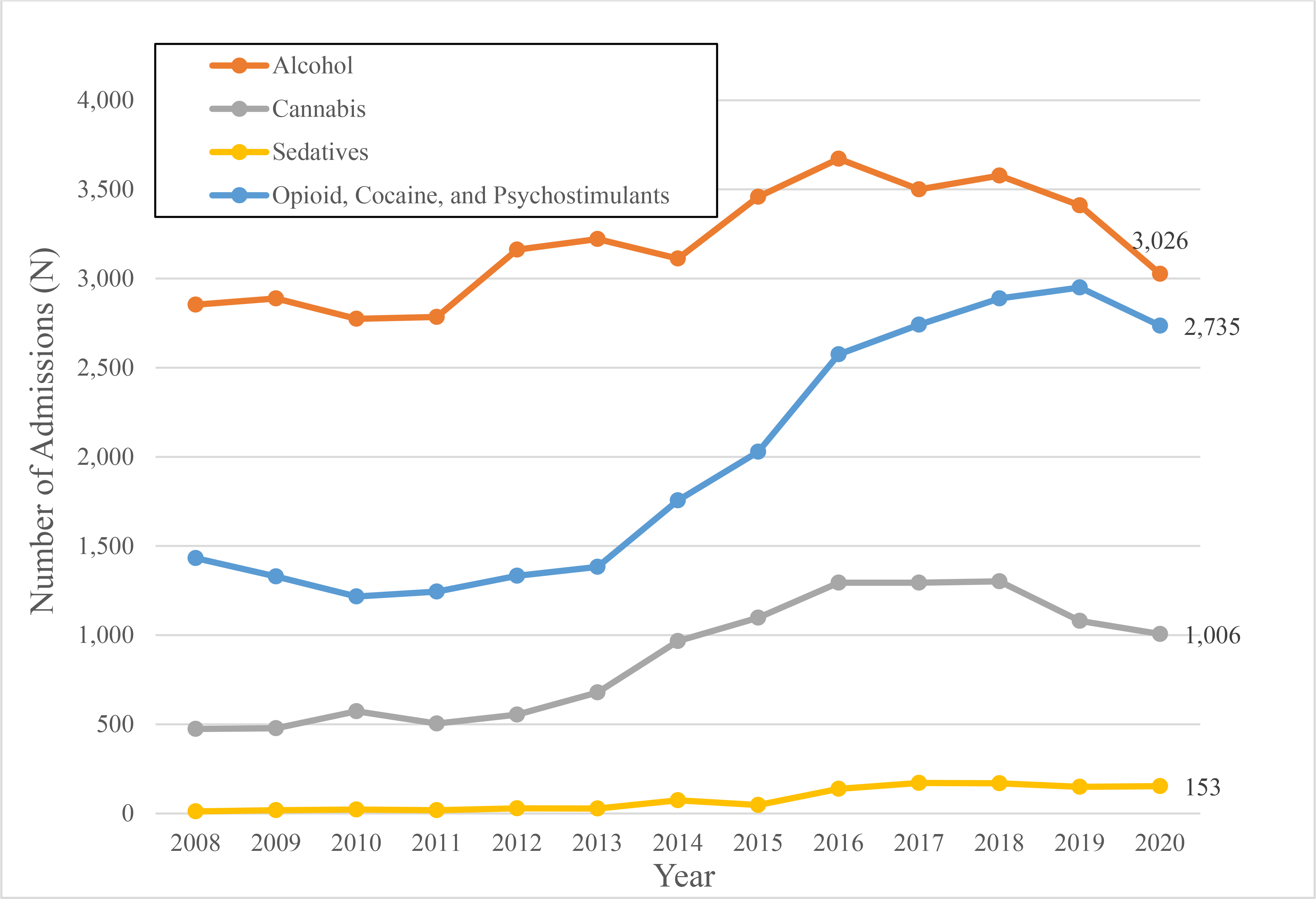
Hospital admissions associated with individual substances, 2008–2020 SUD diagnoses were not mutually exclusive. Admissions were often characterized by co-ingestion of multiple substances
Figure 2:
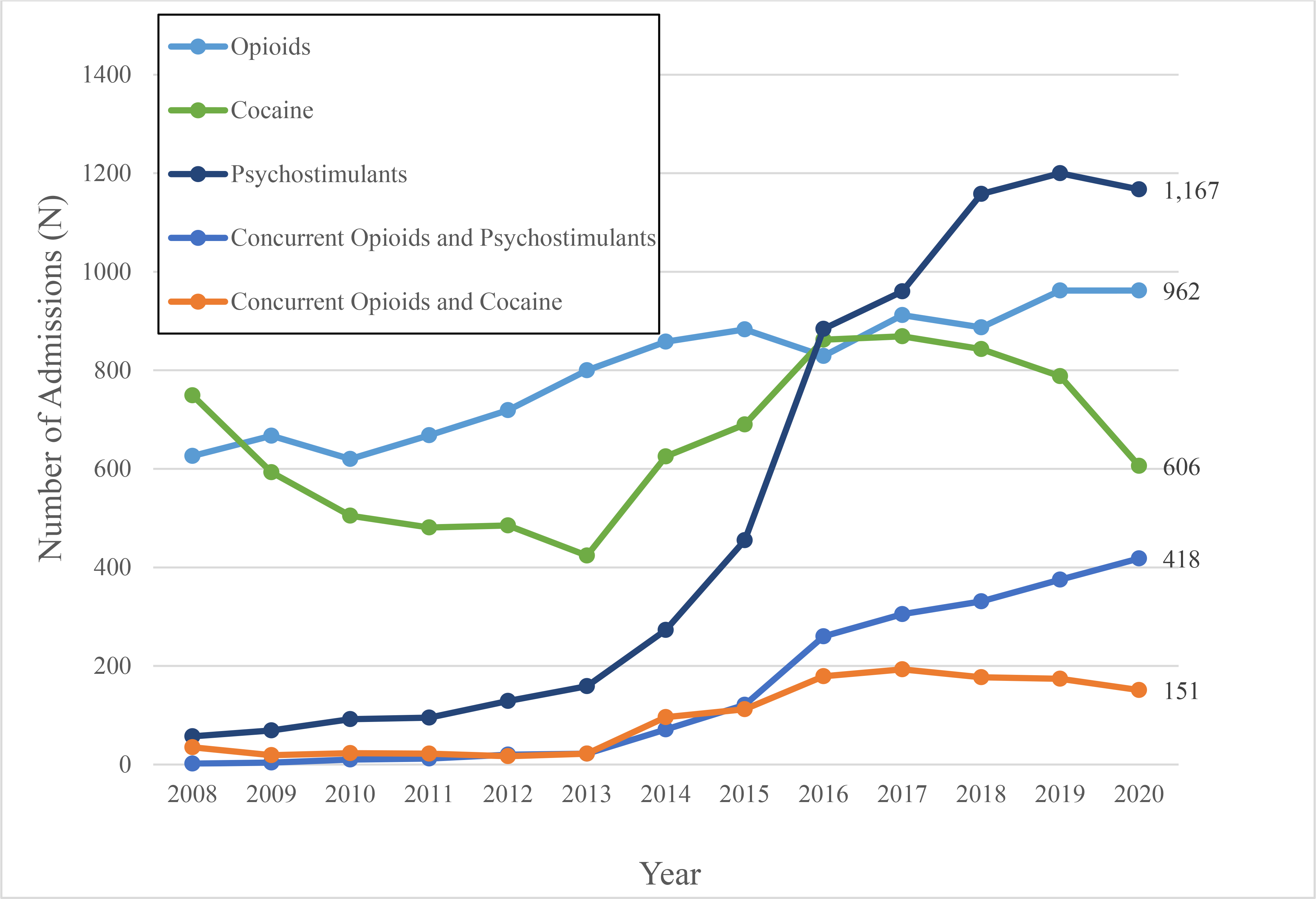
Hospital admissions associated with individual illicit substances, 2008–2020 SUD diagnoses were not mutually exclusive. Admissions were often characterized by co-ingestion of multiple substances. Simultaneous use was determined by the association of both Opioid and Psychostimulant/Cocaine ICD codes with the individual admission
After adjusting for covariates, SUD-related hospitalizations had higher rates of AMA discharge (3.8%; 95% CI 3.6–3.9 vs 1.4%; 95% CI 1.3–1.4) and longer mean LOS (6.3 days; 95% CI: 6.2–6.3 vs 5.3 days; 95% CI: 5.3–5.4) than non-SUD-related admissions. Psychostimulant-related admissions had the highest average LOS (8.0 days; 95% CI 7.7–8.3).
DISCUSSION
From 2008 to 2020, admissions at our institution related to any SUD increased by 42%, accounting for over one-third of total admissions in 2020. While opioid use remains a salient topic nationally, trends at our institution indicate that psychostimulant use is responsible for a rapidly increasing share of admissions. Additionally, concurrent use of both opioids and psychostimulants increased substantially during our study period. This is a concerning trend given increased rates of high-risk behaviors (e.g. intravenous administration) and poor health outcomes among this population.9 We also found that SUD-related admissions were associated with a significantly higher number of comorbidities. Current efforts to expand in-hospital addiction services have largely focused on opioids.10 In-hospital services that provide care for non-opioid SUDs, and address medical comorbidity, are vital to meeting the needs of this patient population.
We found that SUD was associated with increased odds of AMA discharge and higher LOS compared with non-SUD-related admissions. SUD-related hospitalizations are often complicated by psychiatric comorbidities and intoxication/withdrawal syndromes, which may increase AMA discharges and LOS.10 AMA discharge is consistently associated with increased acute hospital resource utilization and poor health outcomes.11 Previous work at our institution found that SUDs accounted for more than 80% of unreimbursed costs12. In-hospital addiction services could benefit patients and health systems by reducing AMA discharges and subsequent costs.13
Our study highlights the utility of EHR data to identify important trends in substance-related health care use. While SUD-related information is often hindered by lags in claims and mortality data, EHR data can enable health systems to adapt quickly to increasingly complex substance use patterns.
Our study’s limitations include reliance on provider documentation of SUD and the use of data from one safety-net hospital. However, National Survey on Drug Use and Health data show Minnesota has SUD trends that mirror national patterns, including decreases in alcohol use disorder and simultaneous rises in stimulant and opioid use since 2014.14 Given that SUD-related admission are more common in safety-net hospitals4, our findings may reasonably generalize to other safety-net hospitals, but are likely to be less generalizable to non-safety-net hospitals, reinforcing the need for ongoing surveillance of substance use trends within individual health systems.
CONCLUSIONS
Our study highlights the large impact of the unfolding SUD crisis on safety-net health systems, with one-third of admissions now related to substance use. In addition, we show a rapidly increasing number of admissions related to psychostimulants. Identifying these patterns quickly using EHR data can help shape policy and programs at the health system and regional level that aim to improve patient outcomes.
ACKNOWLEDGEMENTS
This research was supported by the National Institutes of Health’s National Center for Advancing Translational Sciences, grant ULITR002494. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health National Center for Advancing Translational Sciences.
Footnotes
Conflict of interests: None declared.
REFERENCES
- 1.O’Donnell J Vital Signs: Characteristics of Drug Overdose Deaths Involving Opioids and Stimulants — 24 States and the District of Columbia, January–June 2019. MMWR Morb Mortal Wkly Rep. 2020;69. doi: 10.15585/mmwr.mm6935a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Han B, Cotto J, Etz K, Einstein EB, Compton WM, Volkow ND. Methamphetamine Overdose Deaths in the US by Sex and Race and Ethnicity. JAMA Psychiatry. Published online January 20, 2021. doi: 10.1001/jamapsychiatry.2020.4321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Institute on Drug Abuse. Overdose Death Rates. National Institute on Drug Abuse. Published October 19, 2020. https://www.drugabuse.gov/drug-topics/trends-statistics/overdose-death-rates. Accessed January 27, 2021. [Google Scholar]
- 4.Popescu I, Fingar KR, Cutler E, Guo J, Jiang HJ. Comparison of 3 Safety-Net Hospital Definitions and Association With Hospital Characteristics. JAMA Network Open. 2019;2(8). doi: 10.1001/jamanetworkopen.2019.8577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Winkelman TNA, Admon LK, Jennings L, Shippee ND, Richardson CR, Bart G. Evaluation of Amphetamine-Related Hospitalizations and Associated Clinical Outcomes and Costs in the United States. JAMA Netw Open. 2018;1(6):e183758. doi: 10.1001/jamanetworkopen.2018.3758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Owens PL, Fingar KR, McDermott KW, Muhuri PK, Heslin KC. Inpatient Stays Involving Mental and Substance Use Disorders, 2016. 2019. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb249-Mental-Substance-Use-Disorder-Hospital-Stays-2016.jsp. Accessed February 14, 2021. [PubMed]
- 7.Merchant E, Burke D, Shaw L, et al. Hospitalization outcomes of people who use drugs: One size does not fit all. Journal of Substance Abuse Treatment. 2020;112:23–28. doi: 10.1016/j.jsat.2020.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nourazari S, Davis SR, Granovsky R, et al. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am J Emerg Med Published online November 19, 2020. doi: 10.1016/j.ajem.2020.11.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shearer RD, Howell BA, Bart G, Winkelman TNA. Substance use patterns and health profiles among US adults who use opioids, methamphetamine, or both, 2015–2018. Drug and Alcohol Dependence. 2020;214:108162. doi: 10.1016/j.drugalcdep.2020.108162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Englander H, Patten A, Lockard R, Muller M, Gregg J. Spreading Addictions Care Across Oregon’s Rural and Community Hospitals: Mixed-Methods Evaluation of an Interprofessional Telementoring ECHO Program. J Gen Intern Med. 2021;36(1):100–107. doi: 10.1007/s11606-020-06175-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hwang SW, Li J, Gupta R, Chien V, Martin RE. What happens to patients who leave hospital against medical advice? CMAJ. 2003;168(4):417–420. [PMC free article] [PubMed] [Google Scholar]
- 12.Garrett N, Bikah Bi Nguema Engoang JA, Rubin S, et al. Health system resource use among populations with complex social and behavioral needs in an urban, safety-net health system. Healthc (Amst). 2020;8(3):100448. doi: 10.1016/j.hjdsi.2020.100448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thompson HM, Faig W, VanKim NA, Sharma B, Afshar M, Karnik NS. Differences in length of stay and discharge destination among patients with substance use disorders: The effect of Substance Use Intervention Team (SUIT) consultation service. PLoS One. 2020;15(10):e0239761. doi: 10.1371/journal.pone.0239761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. (2008–2018). National Survey on Drug Use and Health 2008–2018. Retrieved from https://datafiles.samhsa.gov/


