Abstract
Objectives:
Access to substance use disorder (SUD) treatment is complex, and more so for pregnant women and mothers who experience unique barriers. This scoping systematic review aimed to summarize contemporary findings on gateways, facilitators, and barriers to treatment for pregnant women and mothers with SUD.
Methods:
We used the scoping review methodology and a systematic search strategy via MEDLINE/PubMed and Google Scholar. The search was augmented by the similar article lists for sources identified in PubMed. Scholarly and peer-reviewed articles that were published in English from 1996 to 2019 were included. A thematic analysis of the selected studies was used to summarize pathways to SUD treatment and to identify research gaps.
Results:
The analysis included 41 articles. Multiple gateway institutions were identified: health care settings, social service agencies, criminal justice settings, community organizations, and employers. Some of the identified facilitators and barriers to SUD treatment were unique to pregnant women and mothers (e.g., fear of incarceration for child abuse). Both personal (emotional support and social support) and child-related factors (loss of children, suspension or termination of parental rights, the anticipation of reuniting with children) motivated women to seek treatment. Major access barriers included fear, stigma, charges of child abuse, inconvenience, and financial hardship.
Conclusions:
There has been progress in implementing different types of interventions and treatments for that were attentive to pregnant women and mothers’ needs. We developed a conceptual model that characterized women’s pathways to treatment by deciphering women’s potential engagement in gateway settings.
Keywords: Substance-Related Disorders, Addiction, Women’s Health, SBIRT, Treatment barriers
1. Introduction
Substance use disorder (SUD) treatment utilization remains low among pregnant women; only 8.5% of pregnant women with SUD received treatment in 2017.1 Pregnant women and mothers (or parenting women) experience additional barriers to SUD treatment such as childcare and the legal implications of substance use during pregnancy. Many pregnant women and mothers are afraid of disclosing their substance use which is considered child abuse in some states, and parental drug use has been associated with losing child custody.2 Given that health care providers can report suspected parental SUD that may lead to charges of child abuse or neglect, the fear that women have to disclose substance use in health care settings is not surprising.3
Examining specific mechanisms and pathways that facilitate SUD treatment during pregnancy and motherhood can pose opportunities to inform screening and treatment efforts. One potentially fruitful area for study is examining the roles of diverse organizations, such as health, social service, and criminal justice (CJ) agencies in facilitating pregnant women and mothers to access treatment. However, analysis of the gateways and referral pathways to accessing SUD treatment for pregnant women and mothers remains limited, and the literature has not been marshalled into a coherent, comprehensive model of treatment access. We first note which settings have been marked and studied as gateways for pregnant women and mothers in the literature. Second, we organize previous findings on the study settings and treatment referral settings, identify agencies that operated as gateways to refer pregnant women and mothers into treatment, and clarify the role of these institutions in engaging these individuals to treatment. Next, we explore how these identified settings may enable or impede women’s referral to treatment services in both clinical and non-clinical settings. We scrutinize the gateways, facilitators, and barriers to treatment access and retention for pregnant women and mothers with SUD, and the effectiveness of interventions. Finally, we develop a conceptual model of SUD treatment access and barriers for pregnant women and mothers across gateways. The model addresses the complexity of potentially modifiable opportunities and barriers in the community for accessing SUD treatment access.
2. Methods
The scoping systematic review strategy was undertaken to focus on summarizing common elements in the literature about the gateways, facilitators, and barriers to SUD treatment services.
2.1. Search strategy
The literature search was conducted using the electronic search engines MEDLINE/PubMed, Scopus, and Google Scholar for publications from 1996 to 2019 after Weisner and Schmidt called for the expansion of the frame of SUD health services research in 1995 (Appendix).4 References were also pulled from the “similar article” list in PubMed. We searched the reference lists of collected papers for additional papers.
2.2. Article screening and systematic extraction process
We included papers of United States samples that reported on subjects related to SUD treatment utilization among pregnant women or mothers between ages 15 to 44 who have children. We focused on studies of alcohol, cocaine, and opioid use disorder (OUD) and excluded nicotine use disorder because currently, SUD treatment programs focus on alcohol and other drugs, generally excluding nicotine. We excluded studies that report only on the outcomes of the children since we focused on women’s access to treatment. Furthermore, we excluded studies that did not document details on gateways, facilitators, or barriers to SUD treatment utilization. We removed duplicate records and conducted a full-text review. During the full-text review, we recorded the exclusion reasons and extracted information from the articles (Table 1). A flow chart of the literature search and selection process was developed (Figure 1). Two authors reviewed articles and when disagreements on study inclusion occurred, and when consensus could not be reached, a third reviewer was asked to determine the inclusion.
Table 1.
Full text article screening data extraction elements
| Extracted elements | Presented in main analysis |
|---|---|
| Study population (e.g., Pregnant women, women with children (mothers), or both) | X |
| Intervention description or main explanatory variable | |
| Sample size (N) | X |
| Geographic region (e.g., National, state, organization) | X |
| Study setting (e.g., Drug court, tertiary hospital, addiction outpatient treatment, CPS, N/A) | X |
| Referral setting (e.g., Drug court, tertiary hospital, addiction outpatient treatment, CPS, N/A) | X |
| Study design | X |
| Study objective(s) | X |
| Time period | |
| Main findings | X |
| Observed outcomes | |
| Process variables | |
| Policy factors | |
| Implementation factors | |
| Conceptual model used | |
| Name of the dataset used, if any | |
| Referral, access, retention, or effectiveness theme | X |
Figure 1.
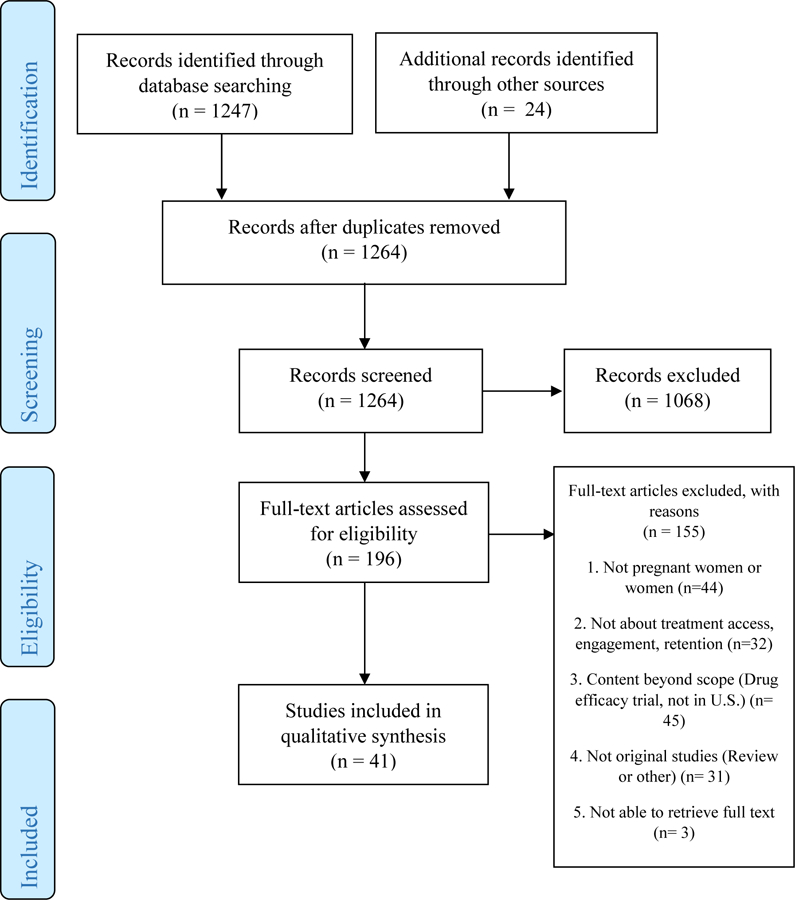
Article screening using PRISMA
2.3. Analysis
For the analysis, we identified treatment settings and gateways. We identified the results in relation to the domains of gateways, facilitators, and barriers to treatment access and retention for pregnant women and mothers with SUD. After the thematic analysis, we developed a SUD treatment access model for pregnant women and mothers across multiple referral settings that demonstrated the key barriers relevant to each gateway (Figure 2).
Figure 2.
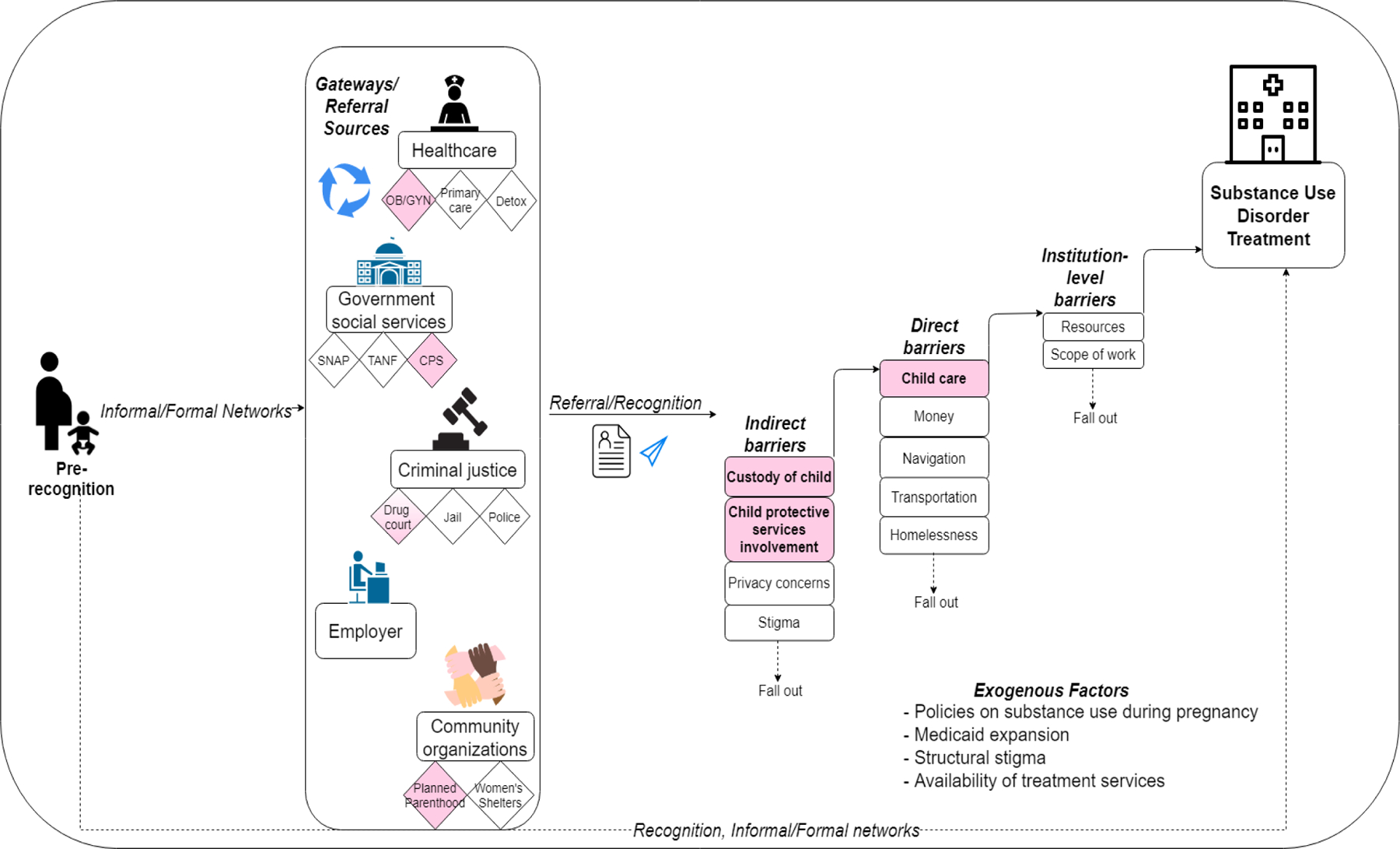
Conceptual model of substance use disorder treatment access and barriers for pregnant women and mothers across gateways and referral settings
Note: Pink denotes mother-specific settings or barriers
3. Results
Of the 196 articles selected for full-text examination, 155 were excluded, resulting in a final sample of 41 articles (Figure 1).
3.1. Trends in studies
Subjects of the studies showed a greater interest in pregnant women and treatment access than of women with children. Of 41 articles, 26 focused on samples of pregnant women, 4 focused on samples of women with children, and 11 articles focused on both pregnant women and women with children. There was a decline in the number of studies that involved community organizations or agencies from 1996 to 2019. Most of the research focused on associations between women’s characteristics and treatment referral, access, and retention in SUD treatment, and examined the unmet service needs of pregnant women with SUD. Many of the interventions focused on assisting women to be engaged in treatment. Research before 2012 includes a greater variety of referral settings, and studies published after 2012 focused more on health care settings. We observed a shift from identifying the treatment need in social welfare agencies to women’s health clinics. Studies published after 2012 have been taking place in other non-SUD hospital-based units such as obstetrics and gynecology5–9 or primary care.10,11
Increasing access for pregnant women and mothers was still an important issue in the post-2012 studies. Socially vulnerable subgroups, such as women involved in the CJ system and/or the CPS, have been studied sporadically throughout the studied periods.12–16 The number of studies on pregnant women and mothers with SUD increased dramatically in 2018, during the opioid epidemic, when the availability of fentanyl and overdose deaths increased.17 Likewise, studies that focused on women with OUD proliferated during the past decade due to the opioid epidemic. We began to see innovations like computer-delivered interventions targeting women with SUD in reproductive health clinics in 2018.7,8
3.2. Gateways to treatment
We examined the gateways of treatment utilization for pregnant women and mothers to examine where access to the treatment system begins. We observed that pregnant women and mothers with SUD were referred to treatment from healthcare settings (i.e., obstetric clinics),8,14 social service agencies (i.e., CPS, Supplemental Nutrition Program for Women, Infants and Children (SNAP-WIC), Temporary Assistance for Needy Families (TANF)),14,16,18–23 CJ settings,14,24,25 community-based organizations (i.e., shelters or Planned Parenthood that offer child care, housing assistance, or jobs for women in need),12,26 and employers (i.e., employment assistance services).21 We did not find studies that focused on evaluating the comparative effectiveness of referral sources (using a comparison group) for this population. All studies analyzed data from a single referral source or listed the source of referrals at the study setting.
3.3. Barriers and facilitators for treatment access
3.3.1. Healthcare
Women who were admitted to managed withdrawal programs (detoxification) reported that acceptability and accessibility were the most common barriers to follow-up treatment.27 Acceptability captured multiple psychological barriers like the perception of the treatment environment, stigma, fear of losing children, self-denial, and pre-knowledge about treatment. For the treatment of an OUD, the rise of using buprenorphine in office-based treatment in settings such as primary care increased women’s access to treatment.11 Health care navigation issues such as delays in entering treatment,28 choosing a provider or making appointments,8 and child care12,14,29 interfered with women’s access to SUD treatment. Having other comorbid conditions such as mental health disorders can also be a barrier to treatment.13
3.3.2. Social services
Social service referrals raised concerns of privacy, stigma, and navigation difficulties that have been shown to hinder access.18,19 Women did not know what treatments were available and/or did not know how to access treatment.22 Women often faced the fear of disclosing their pregnancy and SUD status.30 We found that a woman’s relationship with a social service agency can be complicated, and research has shown mixed findings on the effects of women’s involvement with social service agents.
Women’s relationships with CPS can be both barriers and facilitators. A qualitative study that evaluated the perspectives of women revealed that their engagement with CPS led to participation in treatment programs in order to keep custody of their children and to avoid criminal investigations.12 Pregnant women with SUD also believed that participating in SUD treatment would help them keep their children or be reunited with their children more quickly.12,30,31 However, involvement with the CPS can turn women away from treatment; in one qualitative study, women mentioned both positive and negative experiences with their caseworkers and counselors.13 Some women stated they were not treated with respect, which was detrimental to their recovery. The participants described their positive and negative feelings toward CPS based on their encounters with caseworkers and counselors.13,16 Having a good relationship with experienced coordinators or counselors was a key facilitator that increased treatment accessibility.31,32
3.3.3. Criminal justice system
Treatment referral experience through the CJ system was bidirectional. For example, women who were referred by the CJ system were less likely to use MOUD24,25; however, a large proportion of public treatment utilizers were referred from the CJ system.15 Women seeking referrals from CJ settings can face the following barriers as well: stigma from their families and communities.24 Another barrier to SUD treatment care-seeking was women’s concerns of being reported to the CJ system, including the risk of criminal prosecution of child abuse14,16,24,25,28,33 and fear of losing custody of children.13,16,30
3.3.4. Employers
Accessing treatment from an employer also may hinder access to treatment due to unsolved transportation, navigation, child care issues.19,34 Employer services (employee assistance program) may pose fewer indirect barriers if employment assistance services can ensure confidentiality and anonymity.35
3.3.5. Community-based organizations
Due to women’s unwillingness to disclose their SUD, referrals from community-based organizations may face their own challenges in addition to privacy concerns, transportation, money, and navigation challenges. Stone discusses how women avoid treatment due to the risk of substance use detection.14 At the community-level, screening and referring women with SUD may be beyond the scope of work of these institutions or sectors.12
3.4. Structural factors
Contextual factors have been identified to affect women’s SUD treatment access as well. Structural stigma13,14 and policies on substance use during pregnancy such as mandatory reporting to CPS11 or risk of criminal prosecution of child abuse33 can hinder or exert pressure on women to access treatment services.36 These punitive policies can have different effects depending on which agency or gateway women enter. For example, these policies complicate the patient-provider, social worker-client, and caseworker-client relationships.24,30 Unavailability of treatment services was another barrier as SUD treatment services were limited in capacity and there is a shortage of buprenorphine prescribers.5,25,28 Conversely, state-funded programs that targeted pregnant women or offered priority access increased the availability of treatment services.25 Pregnancy can facilitate expedited enrollment in methadone treatment while waiting periods were longer between pregnancies.14 State policies like the Medicaid expansion directly increased the likelihood of insurance coverage among pregnant women for those living in the expansion states, increasing one’s SUD treatment access.33
3.5. Factors for retention
MOUD use at the time of conception was associated with a longer length of treatment for pregnant women.11 Involvement with the CJ system and external pressure36,37 were factors that increased treatment retention. Likewise, having custody of their children increased the likelihood of treatment retention.38 The availability of support groups was associated with treatment engagement,13 as was family support.37 On the other hand, social vulnerability factors such as homelessness,39 as well as mental health comorbidities, decreased the likelihood of treatment retention.37
3.6. Effectiveness of interventions
Multiple interventions reduced substance use5,31,32,34,40–42 and improved mental health and physical health outcomes.9,31,32,40–43 We examined an increase in different treatment modalities, but most programs strived to be convenient,5,44 practical,12,31 and emotionally supportive.13,31,32 The attention to enhanced convenience was evident in multiple treatment interventions: these program components included child care options,45 parenting education sessions, 29 case management,43 and treatment coordination.19,32,40 The treatment programs attended to the social and psychosocial needs of mothers by focusing on self-sufficiency,41 integrating family involvement and support,6 teaching parenting techniques,29,31,41 providing a linkage to social service agencies,12 and offering vocational education.19,34 Some programs focused on increasing access to clinical treatment, emphasizing outpatient treatment,19,45 offering MOUD,5,43 providing psychosocial support,40–42,45 and addressing comorbid diagnoses.9,13 Programs that allow women to keep their children or that help women regain custody of their children successfully motivated women to participate in treatment.12 Maintaining or regaining child custody motivated women to seek treatment, but for some, it deterred women from seeking treatment.13,30
3.7. Conceptual model
Based on the findings, we developed an empirically testable conceptual model that illustrates pregnant women’s and mother’s pathways to treatment by mapping gateways (Figure 2). In describing pregnant women and mothers’ access to treatment, we considered their informal or formal networks, gateways, and the referral itself. The model highlights the potential barriers women may encounter based on the use of gateways. We observed many individual-level indirect barriers to treatment including, privacy concerns, disbelief that treatment is effective, loss of intimate relationships and having a lack of social capital, medical comorbidities, stigma, potential CPS involvement, and legal concerns of keeping custody of their children. In the direct barrier domain, not having access to transportation, money, and child care for treatment, and having a hard time navigating the complex treatment system. Some of the identified barriers to SUD treatment were unique to pregnant women and mothers (e.g., potential CPS involvement or legal concerns). These indirect and direct barriers can be personal (e.g., emotional support, social support) and child-related factors (e.g., keeping custody, child care). The difference in characterizing by personal and child-related factors is conditional on whether the observed factors are organized around the needs and interests of the woman or the child. A detailed description of the model can be found in the Appendix.
4. Discussion
In this review, we explored various treatment gateways and treatment access concerns for pregnant women and mothers with SUD. Limited treatment availability poses a great concern since such specialty agencies serve a small part of the persons who use substances and need treatment.4 However, we observed that treatment settings began to encompass women’s socioeconomic needs and their social contexts. Many studies discussed strategies for increasing treatment participation for pregnant women such as offering vocational education, nutritional support, case management, and housing assistance.18,19,22 Treatment programs that integrated services had positive outcomes. Some patients attended parenting education sessions after their outpatient visit for medication treatment.29 The programs that offered parenting education were a collaborative effort among physicians, nurses, and child welfare training specialists.
Although there has been some interest in bridging the siloed behavioral and physical healthcare systems since the 2000s, the literature indicates that there is a dearth of literature on referrals, particularly from non-healthcare settings. However, studies conducted to improve screening and referral to treatment across settings may offer some insight. Less progress has been made to enhance the interrelationships between these women and existing social service institutions. A majority of women who enter SUD treatment were already receiving food assistance, housing assistance, and other government support.7,12,34,35 This suggests that a majority of women come into contact with social service providers before they are screened or referred to treatment by other sources. However, our findings raise the potential problems of identifying and referring women to treatment from welfare offices due to organizational inefficiency: for example, identification and referral services can burden the workers at welfare offices.46 In this case, aligning divergent priorities and goals of treatment providers and agency workers or social workers must be considered. This can be addressed by training providers as well as implementing policies that mandate the expansion of the role of social service agencies. In particular, social workers have a wide variety of practice possibilities when it comes to addressing the health needs of patients with SUD, from performing evidence-based psychosocial treatment to refer women elsewhere for treatment. However, the absence of SBIRT in social service organizations, and the absence of trained social workers in making a referral to appropriate alternative treatment sources is a concern.47 Increasing training opportunities in SBIRT and SUD can facilitate collaborative SUD care, only if organizational issues, such as job definitions and scopes of responsibility in social service agencies are changed. The role of agents has been known to greatly influence women’s motivation to enter treatment services.13 Therefore, more research to understand how to best train agents is desirable.
Articles that investigated the relationship between CJ referrals and treatment access show disparities in access to evidence-based treatment for pregnant women. In a study that examined pregnant women who have OUD, Black women were more than 10 times more likely to be reported to authorities after a positive urine screening compared to White women.24 Pregnant women who were referred from the CJ system to treatment were less likely to receive evidence-based treatment, such as MOUD.24,25 Inefficient or non-existent connections between the CJ system and treatment programs may explain why the criminal-justice referred women were less likely to receive MOUD.
Some gaps in the literature were identified. Referral settings are understudied, and more research should investigate the effectiveness and mechanisms of gateways that can promote pregnant women’s and mothers’ pathways to treatment. To facilitate referrals, future research should focus on assessing the feasibility of implementing interagency collaborations. Although screening and referring women with SUD may be beyond the scope of work at many institutions, the efforts of treating SUD can coincide with addressing the main missions of some public agencies. Patient-centered and integrated services can lessen potential duplications, and promote appropriate need-based care for women. Furthermore, the notion of coercion and the receipt of social welfare is complicated and warrants more research, at different socioecological levels like the individual, provider, organizational, state, and regional levels. Offering comprehensive and evidence-based interventions to address the stated needs of women across many settings can reduce the barriers to SUD treatment. Low-socioeconomic status – poverty, poor education, inadequate housing, unemployment, and difficulties with transportation and childcare – will need to be addressed to optimize treatment entry. Other community agencies like women’s shelters and Planned Parenthood26 that focus on reducing stigma and advocating for women’s rights can be utilized as entry settings to link women in need of treatment services. We were not able to find studies that evaluated referral patterns from these types of agencies, and more research is warranted in such community settings that are known to engage vulnerable pregnant women and mothers with SUD without stigma. Women’s prior experiences that may affect treatment access such as adverse childhood events, trauma, and interpersonal violence also have not been addressed. Adapting the interventions to meet essential socioeconomic and psychosocial needs can be an important step toward increasing access to effective SUD treatment for pregnant women and mothers.
There are limitations to this study. We started the search beginning in 1996, which may not be enough time to reflect the expansion of services. The literature search has been restricted to women, thus the results do not reflect the experience of trans-men, non-binary people, or others who do not identify as “women” or “mothers”, but can conceive and bear children. Men with SUD also have difficulties with access to care, but women have additional barriers and having children add more barriers on top of that. Publication bias may be present. Convenience bias is likely present, since women’s characteristics are captured in a setting in which they sought treatment. Limiting the review to the US settings can reduce generalizability. We have not identified non-peer-reviewed state reports or pilot program evaluations since we searched for peer-reviewed original investigations. Finally, our conceptual model shows a unidirectional relationship between a gateway and treatment access, but treatment pathways can be cyclical in reality.
Conclusions
This review revealed several research priorities to increase treatment access for women by developing women-focused interventions that account for economic and social needs. Our results indicate there are opportunities to leverage various social service programs as well as health care settings to address treatment needs; therefore, there is a need for innovative design and implementation of strategies to develop efficient referral avenues. Finally, we need more research that attends to the unique needs of individual women, in particular how to mobilize their social relationships and support network.
Supplementary Material
Table 2.
Characteristics of included studies
| Study | Referral, Access, Retention, Or Effectiveness | Population Focus | Study Setting, Sample Size | Gateway or Referral source | Type of Substance Use Disorder | Study Design | Objective(s) | Key Results |
|---|---|---|---|---|---|---|---|---|
| Alemi et al., 199642 | Effectiveness | Pregnant women | Clinical setting, not specified (n=179) | Health care provider, not specified | Cocaine | Prospective cohort; Qualitative interview | Assess the intervention that used computer services to inform and motivate patients | • The intervention did not lead to significant change in patients’ health status, drug use, or utilization of services; however, it did increase SUD treatment engagement • SUD treatment engagement did not reduce drug or alcohol use |
| Messer et al., 199648 | Access | Pregnant women | Prenatal care clinic (n=182) | Health care provider | Alcohol or other drugs | Cross-sectional | Explore the characteristics of pregnant women who used SUD treatment service vs. women who declined to participate | • 51% of eligible pregnant women participated in the SUD treatment service • Among women with low SES, Black women, women with more children, women with greater severity of SUD, individuals who use cocaine, and women who have previously received SUD treatment were more likely to participate in this SUD treatment service |
| Klein and Zahnd, 199722 | Referral; Access | Pregnant women | Public agencies and community organizations (n=401) | Families with Dependent Children, health clinics, SNAP, refuges, jails, and programs for teenagers | Alcohol or other drugs | Qualitative interview | Explore alcohol and drug use patterns, and problems and unmet service needs (including treatment) | • More than half of the sample came from the Aid to Families with Dependent Children (AFDC), followed by health clinics, SNAP, and refuges, jails, and programs for teenagers • The following service needs were found: job placement, educational programs, and housing • 64% had not participated in formal treatment or 12 step program • Among women who were not in treatment, they did not want treatment due to: financial barriers, legal problems, did not know what treatment was available/how to get into treatment, and/or had no transportation or child care. |
| Whiteside et al., 199940 | Effectiveness | Pregnant women and mothers | SUD treatment (n=105) | N/A | Alcohol or other drugs | Prospective cohort | Assess the Arkansas Center for Addictions Research, Education, and Services (AR-CARES) | • The AR-CARES evolved over a 5-year period and responded to the needs of the target population (pregnant women and parenting women with SUD) • Added residential facilities, mental health counseling, child care, early intervention for children, and transportation to the treatment program • Decreased maternal substance use and lowered incidence of premature labor and maternal infections |
| Weisdorf et al., 199945 | Retention; Effectiveness | Pregnant women | SUD treatment (n=500) | N/A | Cocaine | Retro-spective cohort | Evaluate the Pregnancy Substance Abuse Program (PSAP) | • The PSAP increased treatment retention • Successful factors include: counselor continuity, treatment coordination and group continuity across levels of care, pregnancy and women specific treatment groups, child-care options, and increased emphasis on outpatient treatment |
| Kissin et al., 200149 | Access | Pregnant women | SUD treatment (n=240) | Social services | Opioid or cocaine | Cross-sectional | Explore the characteristics of pregnant women in SUD treatment | • Participants were likely to be Black, low income, urban women with opioid use disorder in their late twenties who voluntarily entered treatment • They were surrounded by others, often family members, with substance use disorder problems • They were less likely to have a full-time employment and many received income from the Department of Social Services |
| Nishimoto et al., 200138 | Retention | Pregnant women and Mothers | SUD treatment (n=252) | Child Protective Services (CPS), local hospitals, social services, self-referrals | Alcohol or other drugs | Randomized controlled trial | Examine the relationship between various indicators of coercion and treatment retention and whether those relationships vary by treatment modality | • 83% of the sample were referred from the CPS; 8% from local hospitals; 6% from social agencies; 2.8% were self-referrals • Women who had custody were more likely to stay in treatment compared to women who did not have custody |
| Hohman et al., 200320 | Referral | Pregnant women | SUD treatment (n=678) | CPS | Alcohol or other drugs | Retro-spective cohort | Describe the demographic, substance use, and treatment variables and to compare these variables based on CPS status | • Mandated status, unsatisfactory exit status, and cocaine use were associated with CPS referrals • CPS has additional requirements beyond the treatment requirements |
| Tuten et al., 200350 | Retention | Pregnant women | SUD treatment (n=235) | Social services | Alcohol or other drugs | Cross-sectional | Compare homeless and domiciled pregnant women with SUD on treatment outcomes | • Homeless women with SUD had lower retention rates, received only 65% of the social services income compared to domiciled women • Homeless pregnant women with SUD may be lacking resources compared to domiciled women |
| Grella et al., 2006 21 | Referral | Mothers | SUD treatment (n=4,156) | Healthcare provider, CPS, social services, employer | Alcohol or other drugs | Cross-sectional | Compare the characteristics of mothers in treatment who were and were not involved with child welfare services | • Women engaged in child welfare services were younger, had more children, had lower levels of addiction severity, but were more likely to be economically unstable compared to women not engaged in child welfare services • Women who were involved with child welfare services were less likely to cite an individual (i.e., self, family, or friends) or another treatment provider as the source of referral to treatment, and had a higher rate of being referred by another organization or service provider (i.e., health care provider, child welfare, social services, employer) |
| Conners et al., 2006 41 | Retention; Effectiveness | Pregnant women and mothers | SUD treatment (n=305) | Criminal justice system | Alcohol or other drugs | Prospective cohort | Evaluate AR-CARES program on women in the areas of substance use, consequences of use, employment, legal involvement, mental health symptoms, risky sexual behavior, and parenting attitudes. | • AR-CARES improved LOS and resulted in positive outcomes (lower substance use, higher self-sufficiency, improved parenting attitudes, and fewer symptoms of depression and PTSD) • About 33% of women were legally pressured to enter treatment • Most women entered treatment with a criminal record, and more than half (59.5%) were arrested in the year before intake, a quarter (24.3%) were rearrested after treatment |
| Pollack & Reuter, 2006 23 | Referral; Effectiveness | Pregnant women and mothers | National Survey | CPS, social services | Alcohol or other drugs | Retro-spective cohort | Evaluate the association between welfare receipt and treatment | • Welfare settings are important access points to treatment for low-income women (Temporary Assistance for Needy Families (TANF)) |
| O’Connor & Whaley, 2007 18 | Effectiveness; Referral | Pregnant women | Supplemental Nutrition Program (n=255) | Social services, Community programs | Alcohol | Randomized controlled trial | Examine the efficacy of brief intervention | • Brief intervention by nonmedical professionals (i.e., nutritionists) successfully increased pregnant women’s motivation to change alcohol drinking behavior • Community programs like Public Health Foundation Enterprises Management Solutions Special Supplemental Nutrition Program for Women, Infants, and Children (SNAP-WIC) can be instrumental in preventing alcohol-exposed pregnancies |
| Simons, 2008 37 | Retention | Pregnant women and mothers | SUD treatment (n=80) | N/A | Alcohol or other drugs | Retro-spective cohort | Measure differences in characteristics and outcomes between treatment completers versus non-completers | • Women who completed treatment had higher rates of alcohol consumption, arrests for public intoxication, family support, lower mental health problems, higher rates of childhood emotional neglect, and higher rates of medication. • Mental health comorbidity is a big barrier to treatment completion, especially among Black women |
| Morgenstern et al., 2009 19 | Effectiveness; Referral | Mothers | Temporary Assistance for Needy Families (TANF) (n=452) | Social services | Alcohol or other drugs | Randomized controlled trial | Evaluate the impact of intensive case management program among women with SUD receiving TANF. | • Intensive case management program increased abstinence rates through 24 months of follow-up, and improved full-time employment rates among women receiving TANF • Treatment likely improves abstinence, which impacts later employment |
| Dakof et al., 2010 31 | Effectiveness | Mothers | Drug court, (n=62) |
Criminal justice system, CPS | Alcohol or other drugs | Randomized controlled trial | Evaluate the Engaging Moms Program (EMP) intervention | • EMP increased the likelihood of positive child welfare dispositions • Decreased substance use • Increased family functioning and enhanced parenting practices • Improved maternal mental and physical health |
| Ondersma et al., 2010 36 | Retention | Pregnant women | SUD treatment, (n=200) | N/A | Alcohol or other drugs | Randomized controlled trial | Analyze external pressure on retention in treatment and substance use | • Pregnant women who had external pressure were more likely to remain in treatment, attend more treatment sessions, less likely to use substances (less tested positive or report fewer days of use) |
| Jackson and Shannon, 2012 27 | Access | Pregnant women | Tertiary hospital, detox (n=85) | Health care provider | Alcohol or other drugs | Cross-sectional | Identify barriers to treatment | • Over 80% of the sample reporting having experienced any barrier to treatment and the majority indicated having more than two barriers • The majority experienced acceptability and accessibility barriers |
| McCabe et al., 2012 26 | Access | Pregnant women | SUD treatment, (n=1,724,479) | Criminal justice system, health care provider | Alcohol or other drugs | Repeated cross-sectional | Characterize pregnant women entering SUD treatment | • Pregnant women were more likely to be younger, minority, never married, less educated, homeless, on public-assistance or have no income than nonpregnant women |
| Meyer et al., 2012 43 | Effectiveness | Pregnant women | Tertiary hospital, (n=149) | Health care provider | Opioids | Cross-sectional | Determine whether increased access to medication for opioid use disorder and improved coordination of ancillary services for pregnant women improved perinatal outcomes | • The number of pregnant women receiving treatment increased • Improved maternal and perinatal outcome in the nonurban setting • Development of coordinated team care may improve outcomes |
| Thompson et al., 2013 12 | Access | Mothers | CPS, (n=27) | CPS | Alcohol or other drugs | Qualitative interview | Evaluate the perspective of participants in the Parenting in Recovery (PIR) program | • Motivations behind participation include 1) the program would allow them to keep their children or be reunited with their children more quickly 2) to avoid a criminal investigation, arrest or jail |
| Kuo et al., 2013 13 | Access; Retention | Pregnant women and mothers | SUD treatment, (n=18) | Social services, CPS | Alcohol or other drugs | Qualitative interview | Explore factors impacting treatment outcomes and needs | • Self-motivation, pregnancy, navigating family relationships, availability of community support (support groups and program for outpatient treatment) can facilitate treatment • Social support does not always facilitate treatment; agencies like Department of Children, Youth, and Their Families (DCYF) can be facilitative or challenging • Programs that address dual-diagnoses are promising |
| Aklin et al., 2014 34 | Effectiveness | Pregnant women and mothers | SUD treatment, (n=40) | N/A | Opioids, cocaine | Randomized controlled trial | Evaluate the effects of a therapeutic workplace social business on drug abstinence and employment | • More cocaine- and opiate- negative urine samples than controls • Less money spent on drugs • More days employed • Higher employment income |
| Lee King et al., 2015 10 | Access; Retention | Pregnant women | Primary care, (n=2,729) | Health care provider | Alcohol or other drugs | Cross-sectional | Determine clinical profiles of pregnant women in treatment for co-occurring disorders with current interpersonal abuse | • Pregnant women more likely to demonstrate social vulnerability than nonpregnant women • Less income |
| Stone, 2015 14 | Referral; Access | Pregnant women and mothers | Community (Multiple settings including transportation hubs and healthcare settings) (n=30) | N/A | Alcohol or other drugs | Qualitative interview | Explore the experiences of substance-using mothers in health and criminal justice settings |
• Women managed their risk of detection by health or criminal justice authorities, including isolating themselves from others, skipping treatment appointments, or avoiding treatment altogether |
| Angelotta et al., 2016 24 | Access; Referral | Pregnant women | SUD treatment, (n=8,292) | Individual, Health care provider, Criminal justice system, Community | Opioids | Repeated cross-sectional | Analyze the relationship between the use of medication for opioid use disorder (MOUD) and state laws that criminalize substance use during pregnancy | • Half of pregnant women with opioid use disorder received MOUD • Pregnant women referred to treatment by the criminal justice system were least likely to receive MOUD |
| Kahn et al., 2017 29 | Effectiveness | Pregnant women and mothers | SUD treatment, (n=75) | N/A | Opioids | Qualitative interview | Evaluate parenting education at MAT clinic | • Educational content was useful • Participants appreciated the social support provided by the groups |
| Mittal et al., 2017 5 | Effectiveness | Pregnant women | Obstetric clinic, (n=14) | Health care provider | Opioids | Qualitative interview | Evaluate collaborative care treatment with buprenorphine | • Intervention is feasible • High retention rates • Only 6.9% had aberrant urine opioid screen at delivery |
| Hand et al., 2017 28 | Access | Pregnant women | SUD treatment, (n=8,656) | Criminal justice system | Alcohol or other drugs | Repeated cross-sectional | Characterize pregnant women entering treatment by geographical regions | • Women living in South are more likely to use benzos compared to those in other regions; less likely to use MOUD; less likely to use heroin and be injection drug users |
| Washio et al., 2018 15 | Access | Pregnant women | SUD treatment, (n=166,863) | Criminal justice system | Alcohol | Repeated cross-sectional | Characterize pregnant women who reported alcohol use entering treatment | • Pregnant women who use alcohol were more likely to be referred by the criminal justice system • Marijuana was the most popular co-used substance among pregnant women |
| Saia et al., 2017 6 | Access | Pregnant women | Obstetric clinic, (n=310) | Health care provider | Opioids | Cross-sectional | Describe prenatal care and neonatal outcomes after the implementation of buprenorphine treatment at the clinic | • Increase in the volume of pregnant women treated and children with neonatal abstinence syndrome over time |
| Brogly et al., 2018 35 | Access | Pregnant women | SUD treatment, (n=113) | N/A | Opioids | Cross-sectional | Characterize pregnant women with OUD entering treatment | • Over half had been incarcerated in the past, 30% currently involved in legal proceedings, 15% have unstable housing |
| Short et al., 2018 25 | Access; Referral | Pregnant women | SUD treatment, (n= 88,241) | Criminal justice system, self-referral | Opioids | Repeated cross-sectional | Analyze trends and disparities in receipt of MAT | • MOUD utilization is less likely among the employed, those in intensive outpatient or residential programs, referred from criminal justice or have co-occurring mental health illnesses |
| Falleta et al., 2018 16 | Access; Referral | Pregnant women | SUD treatment, (n= 16) | CPS | Opioids | Qualitative interview | Understand currently or recently pregnant women’s perceptions of CPS in treatment | • Both positive and negative feelings toward CPS exist • CPS is client-focused and provides support but needs are not met and resources are not provided • Patient and caseworker relationship is important |
| Ondersma et al., 2018 7 | Effectiveness | Pregnant women and mothers | Delivery unit, (n=500) | Health care provider | Prescrip-tion opioids, marijuana | Randomized controlled trial | Evaluate the efficacy of the computer-delivered brief intervention | • No evidence of efficacy for an indirect, single-session, computer-delivered, brief intervention designed as a complement to indirect screening |
| Martino et al., 2018 8 | Effectiveness; Referral | Pregnant women and mothers | Reproductive health clinic, (n=439) | Health care provider | Alcohol or other drugs | Randomized controlled trial | Evaluate the efficacy of electronic or clinician based screening and brief interventions for referral to treatment | • Both e-SBIRT and SBIRT significantly reduced days of primary substance use over the follow-up period compared to usual care • No interaction with pregnancy |
| O’Connor et al., 2018 11 | Retention | Pregnant women | Primary care, (n=190) | Health care provider | Alcohol or other drugs | Retro-spective Cohort | Characterize pregnant women’s treatment retention | • MOUD utilization before conception would likely improve treatment outcomes |
| Cochran et al., 2018 32 | Effectiveness | Pregnant women | SUD treatment, (n=21) | Health care provider | Opioids | Prospective cohort | Optimize and evaluate patient navigation intervention | • Significantly improved illicit opioid use abstinence and decreased in drug use and depression |
| Clemans et al., 2019 33 | Access | Pregnant women | Health care setting, (n=72,086) | Health care provider | Opioids | Retro-spective cohort | Analyze maternal and infant care, Medicaid costs, and outcomes related to maternal OUD | • 75% of women with OUD had at least some treatment related to substance use but treatment was not continuous • Health care costs were higher for women with OUD than those with other substance use disorders |
| Frazer et al., 2019 30 | Access | Pregnant women | SUD treatment, (n=20) | Friend/partner, Health care provider, Criminal justice system | Alcohol or other drugs | Qualitative interview | Identify motivators and barriers to treatment | • Motivators: readiness to stop using, concern for the baby’s health, concern about custody of the baby or other children, wanting to escape violent environments or homelessness, and seeking structure • Barriers: fear of loss of custody, not wanting to be away from children/partner, concern about stigma or privacy, and lack of childcare and transportation |
| Shenai et al., 2019 9 | Effectiveness | Pregnant women | Antepartum unit, (n=31) | Health care provider | Alcohol or other drugs | Prospective cohort | Evaluate the efficacy of a brief education session | • All women reported multiple lifetime traumatic experiences • Session improved their knowledge about diagnoses • Increased likelihood of pursuing further dual treatment |
Acknowledgments
Sources of support for the work reported/paper: National Institutes of Health (NIH) National Institute on Drug Abuse (NIDA) #1T32DA041898
Footnotes
Conflicts of interest: None
References
- 1.Substance Abuse and Mental Health Services Administration. Results from the 2017 National Survey on Drug Use and Health. Volume I Summary of National Findings 2018. [Google Scholar]
- 2.Marcenko MO, Kemp SP, Larson NC. Childhood experiences of abuse, later substance use, and parenting outcomes among low-income mothers. American Journal of Orthopsychiatry 2000. doi: 10.1037/h0087853 [DOI] [PubMed] [Google Scholar]
- 3.Haffajee RL, Faherty LJ, Zivin K. Pregnant Women with Substance Use Disorders — The Harm Associated with Punitive Approaches. New England Journal of Medicine 2021;384(25):2364–2367. doi: 10.1056/NEJMp2101051 [DOI] [PubMed] [Google Scholar]
- 4.Weisner C, Schmidt LA. Expanding the frame of health services research in the drug abuse field. Health Services Research 1995. [PMC free article] [PubMed] [Google Scholar]
- 5.Mittal L, Suzuki J. Feasibility of collaborative care treatment of opioid use disorders with buprenorphine during pregnancy. Substance abuse 2017;38(3):261–264. [DOI] [PubMed] [Google Scholar]
- 6.Saia K, Bagley S, Wachman E, Patel P, Nadas M, Brogly S. Prenatal treatment for opioid dependency: observations from a large inner-city clinic. Addiction science & clinical practice 2017;12(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ondersma SJ, Svikis DS, Thacker C, et al. Computer-delivered indirect screening and brief intervention for drug use in the perinatal period: A randomized trial. Drug and alcohol dependence 2018;185:271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martino S, Ondersma SJ, Forray A, et al. A randomized controlled trial of screening and brief interventions for substance misuse in reproductive health. American journal of obstetrics and gynecology 2018;218(3):322.e1–322.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shenai N, Gopalan P, Glance J. Integrated Brief Intervention for PTSD and Substance Use in an Antepartum Unit. Maternal and child health journal 2019;23(5):592–596. [DOI] [PubMed] [Google Scholar]
- 10.Lee King PA, Duan L, Amaro H. Clinical needs of in-treatment pregnant women with co-occurring disorders: implications for primary care. Maternal and child health journal 2015;19(1):180–187. [DOI] [PubMed] [Google Scholar]
- 11.O’Connor A, Uhler B, O’Brien LM, Knuppel K. Predictors of treatment retention in postpartum women prescribed buprenorphine during pregnancy. Journal of substance abuse treatment 2018;86:26–29. [DOI] [PubMed] [Google Scholar]
- 12.Thompson S, Roper C, Peveto L. Parenting in recovery program: participant responses and case examples. Child welfare 2013;92(1):139–157. [PubMed] [Google Scholar]
- 13.Kuo C, Schonbrun YC, Zlotnick C, et al. A qualitative study of treatment needs among pregnant and postpartum women with substance use and depression. Substance use & misuse 2013;48(14):1498–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stone R. Pregnant women and substance use: fear, stigma, and barriers to care. Health & Justice 2015. doi: 10.1186/s40352-015-0015-5 [DOI] [Google Scholar]
- 15.Washio Y, Mark K, Terplan M. Characteristics of Pregnant Women Reporting Cannabis Use Disorder at Substance Use Treatment Entry. Journal of addiction medicine 2018;12(5):395–400. [DOI] [PubMed] [Google Scholar]
- 16.Falletta L, Hamilton K, Fischbein R, Aultman J, Kinney B, Kenne D. Perceptions of child protective services among pregnant or recently pregnant, opioid-using women in substance abuse treatment. Child abuse & neglect 2018;79:125–135. [DOI] [PubMed] [Google Scholar]
- 17.Lee YW, Saia K. Caring for Pregnant Women with Opioid Use Disorder. Current Obstetrics and Gynecology Reports 2019. doi: 10.1007/s13669-019-0255-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Connor MJ, Whaley SE. Brief intervention for alcohol use by pregnant women. American Journal of Public Health 2007. doi: 10.2105/AJPH.2005.077222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morgenstern J, Neighbors CJ, Kuerbis A, et al. Improving 24-month abstinence and employment outcomes for substance-dependent women receiving temporary assistance for needy families with intensive case management. American Journal of Public Health 2009. doi: 10.2105/AJPH.2007.133553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hohman MM, Shillington AM, Baxter HG. A comparison of pregnant women presenting for alcohol and other drug treatment by CPS status. Child Abuse and Neglect 2003. doi: 10.1016/S0145-2134(03)00008-5 [DOI] [PubMed] [Google Scholar]
- 21.Grella CE, Hser YI, Huang YC. Mothers in substance abuse treatment: Differences in characteristics based on involvement with child welfare services. Child Abuse and Neglect 2006. doi: 10.1016/j.chiabu.2005.07.005 [DOI] [PubMed] [Google Scholar]
- 22.Klein D, Crim D, Zahnd E. Perspectives of pregnant substance-using women: Findings from the california perinatal needs assessment. Journal of Psychoactive Drugs 1997. doi: 10.1080/02791072.1997.10400170 [DOI] [PubMed] [Google Scholar]
- 23.Pollack HA, Reuter P. Welfare receipt and substance-abuse treatment among low-income mothers: The impact of welfare reform. American Journal of Public Health 2006. doi: 10.2105/AJPH.2004.061762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Angelotta C, Weiss CJ, Angelotta JW, Friedman RA. A Moral or Medical Problem? The Relationship between Legal Penalties and Treatment Practices for Opioid Use Disorders in Pregnant Women. Women’s Health Issues 2016;26(6):595–601. doi: 10.1016/j.whi.2016.09.002 [DOI] [PubMed] [Google Scholar]
- 25.Short VL, Hand DJ, MacAfee L, Abatemarco DJ, Terplan M. Trends and disparities in receipt of pharmacotherapy among pregnant women in publically funded treatment programs for opioid use disorder in the United States. Journal of substance abuse treatment 2018;89:67–74. [DOI] [PubMed] [Google Scholar]
- 26.McCabe JE, Arndt S. Demographic and substance abuse trends among pregnant and non-pregnant women: Eleven years of treatment admission data. Maternal and Child Health Journal 2012;16(8):1696–1702. doi: 10.1007/s10995-011-0872-z [DOI] [PubMed] [Google Scholar]
- 27.Jackson A, Shannon L. Barriers to receiving substance abuse treatment among rural pregnant women in Kentucky. Maternal and Child Health Journal 2012;16(9):1762–1770. doi: 10.1007/s10995-011-0923-5 [DOI] [PubMed] [Google Scholar]
- 28.Hand DJ, Short VL, Abatemarco DJ. Substance use, treatment, and demographic characteristics of pregnant women entering treatment for opioid use disorder differ by United States census region. Journal of Substance Abuse Treatment 2017. doi: 10.1016/j.jsat.2017.01.011 [DOI] [PubMed] [Google Scholar]
- 29.Kahn LS, Mendel WE, Fallin KL, et al. A parenting education program for women in treatment for opioid-use disorder at an outpatient medical practice. Social work in health care 2017;56(7):649–665. [DOI] [PubMed] [Google Scholar]
- 30.Frazer Z, McConnell K, Jansson LM. Treatment for substance use disorders in pregnant women: Motivators and barriers. Drug and Alcohol Dependence 2019. doi: 10.1016/j.drugalcdep.2019.107652 [DOI] [PubMed] [Google Scholar]
- 31.Dakof GA, Cohen JB, Henderson CE, et al. A randomized pilot study of the Engaging Moms Program for family drug court. Journal of Substance Abuse Treatment 2010;38(3):263–274. doi: 10.1016/j.jsat.2010.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cochran GT, Hruschak V, Abdullah W, et al. Optimizing Pregnancy Treatment Interventions for Moms (OPTI-Mom): A Pilot Study. Journal of addiction medicine 2018;12(1):72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clemans-Cope L, Lynch V, Howell E, et al. Pregnant women with opioid use disorder and their infants in three state Medicaid programs in 2013–2016. Drug and alcohol dependence 2019;195:156–163. [DOI] [PubMed] [Google Scholar]
- 34.Aklin WM, Wong CJ, Hampton J, et al. A therapeutic workplace for the long-term treatment of drug addiction and unemployment: eight-year outcomes of a social business intervention. Journal of substance abuse treatment 2014;47(5):329–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brogly SB, Saia KE, Werler MM, Regan E, Hernández-Díaz S. Prenatal Treatment and Outcomes of Women With Opioid Use Disorder. Obstetrics and gynecology 2018;132(4):916–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ondersma SJ, Winhusen T, Lewis DF. External pressure, motivation, and treatment outcome among pregnant substance-using women. Drug and Alcohol Dependence 2010;107(2–3):149–153. doi: 10.1016/j.drugalcdep.2009.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Simons L. Characteristics of drug-abusing women with children in residential treatment: A preliminary evaluation of program retention and treatment completion. Journal of Ethnicity in Substance Abuse 2008. doi: 10.1080/15332640802055616 [DOI] [PubMed] [Google Scholar]
- 38.Nishimoto RH, Roberts AC. Coercion and drug treatment for postpartum women. American Journal of Drug and Alcohol Abuse 2001. doi: 10.1081/ADA-100103125 [DOI] [PubMed] [Google Scholar]
- 39.Tuten M, Svikis DS, Keyser-Marcus L, O’Grady KE, Jones HE. Lessons learned from a randomized trial of fixed and escalating contingency management schedules in opioid-dependent pregnant women. American Journal of Drug and Alcohol Abuse 2012;38(4):286–292. doi: 10.3109/00952990.2011.643977 [DOI] [PubMed] [Google Scholar]
- 40.Whiteside-Mansell L, Crone CC, Conners NA. The development and evaluation of an alcohol and drug prevention and treatment program for women and children: The AR-CARES program. Journal of Substance Abuse Treatment 1999. doi: 10.1016/S0740-5472(98)00049-X [DOI] [PubMed] [Google Scholar]
- 41.Conners NA, Grant A, Crone CC, Whiteside-Mansell L. Substance abuse treatment for mothers: Treatment outcomes and the impact of length of stay. Journal of Substance Abuse Treatment 2006. doi: 10.1016/j.jsat.2006.06.001 [DOI] [PubMed] [Google Scholar]
- 42.Alemi F, Stephens RC, Javalghi RG, Dyches H, Butts J, Ghadiri A. A randomized trial of a telecommunications network for pregnant women who use cocaine. Medical Care 1996. doi: 10.1097/00005650-199610003-00002 [DOI] [PubMed] [Google Scholar]
- 43.Meyer M, Benvenuto A, Howard D, et al. Development of a substance abuse program for opioid-dependent nonurban pregnant women improves outcome. Journal of Addiction Medicine 2012;6(2):124–130. doi: 10.1097/ADM.0b013e3182541933 [DOI] [PubMed] [Google Scholar]
- 44.O’Connor A, Alto W, Musgrave K, et al. Observational study of buprenorphine treatment of opioid-dependent pregnant women in a family medicine residency: Reports on maternal and infant outcomes. Journal of the American Board of Family Medicine 2011;24(2):194–201. doi: 10.3122/jabfm.2011.02.100155 [DOI] [PubMed] [Google Scholar]
- 45.Weisdorf T, Parran T V., Graham A, Snyder C. Comparison of pregnancy-specific interventions to a traditional treatment program for cocaine-addicted pregnant women. Journal of Substance Abuse Treatment 1999. doi: 10.1016/S0740-5472(98)00006-3 [DOI] [PubMed] [Google Scholar]
- 46.Metsch LR, Pollack HA. Welfare reform and substance abuse. Milbank Quarterly 2005. doi: 10.1111/j.0887-378X.2005.00336.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wamsley M, Satterfield JM, Curtis A, Lundgren L, Satre DD. Alcohol and Drug Screening, Brief Intervention, and Referral to Treatment (SBIRT) Training and Implementation: Perspectives from 4 Health Professions. Journal of addiction medicine 2018. doi: 10.1097/ADM.0000000000000410 [DOI] [PubMed] [Google Scholar]
- 48.Messer K, Clark KA, Martin SL. Characteristics associated with pregnant women’s utilization of substance abuse treatment services. American Journal of Drug and Alcohol Abuse 1996. doi: 10.3109/00952999609001668 [DOI] [PubMed] [Google Scholar]
- 49.Kissin WB, Svikis DS, Morgan GD, Haug NA. Characterizing pregnant drug-dependent women in treatment and their children. Journal of Substance Abuse Treatment 2001. doi: 10.1016/S0740-5472(01)00176-3 [DOI] [PubMed] [Google Scholar]
- 50.Tuten M, Jones HE, Svikis DS. Comparing homeless and domiciled pregnant substance dependent women on psychosocial characteristics and treatment outcomes. Drug and Alcohol Dependence 2003. doi: 10.1016/S0376-8716(02)00229-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


